Introduction
Bipolar disorder (BP) in youth has gained increasing attention in recent years. While DSM-IV criteria for depression and mania require that symptoms be associated with marked psychosocial impairment, little is known about psychosocial functioning among BP youth. BP among adults is associated with profound impairment in nearly every domain of functioning (Judd et al. 2005;Keck et al. 1998), with greater disability associated with depression than hypo/mania (Judd et al. 2005). Impairment among BP adults is not limited to symptomatic periods, but persists during periods of illness remission (Fagiolini et al. 2005;Morriss 2002).
Children and adolescents with BP also experience significant functional impairment. Geller and colleagues (2000) found that over half of hypo/manic BP youth were functioning poorly, and were more impaired than both ADHD and control youth on indices of social, familial, and academic functioning. Lewinsohn (1995) found that BP adolescents exhibited more global and academic impairment than unipolar, subsyndromal BP, and healthy teens. Biederman and colleagues (2005) reported severe functional impairment in a sample of BP youth, with adolescents more impaired than younger children. Wilens et al. (2003) reported marked global, academic, and social dysfunction among school-aged BP children. Among asymptomatic BP adolescents, Goldstein and colleagues (2006) demonstrated significant interpersonal deficits as compared with healthy controls. In BPI adolescents hospitalized for their first manic or mixed episode, Delbello and colleagues (2007) found only 39% achieved functional recovery at one-year follow-up despite high rates of syndromic and symptomatic recovery. Finally, Rademacher and colleagues (2007) reported that BPI adolescents scored below national norms in nearly all quality-of-life domains. Re-assessment following treatment revealed improvements in most domains of functioning, yet patients remained impaired in multiple functional domains as compared with norms.
Thus, the extant literature indicates that BP in youth is associated with significant psychosocial impairment. However, many questions remain about the functioning of BP youth. First, the relation between psychosocial functioning in various domains and demographic and clinical variables requires further examination. Second, given the high rates of comorbidity in pediatric BP and literature demonstrating an association between psychosocial impairment and common comorbid conditions (e.g., Attention Deficit Hyperactivity Disorder, ADHD; Faraone et al. 1998), it is not clear how comorbidity impacts functioning in pediatric BP. Finally, the extent to which psychosocial impairment continues among BP youth between mood episodes has not been examined across functional domains, nor has the relation between impairment and episode polarity. We examine these questions in a sample of BP youth recruited for longitudinal study. Based on prior literature, we hypothesized that BP youth in-episode would exhibit significant impairment in functioning across domains, with more impairment among adolescents than children. We anticipated that symptom severity would be related to functional impairment. We also expected that BP youth in remission/recovery would exhibit functional impairment, and that BP youth in-episode would be more functionally impaired than those in remission/recovery.
Method
A detailed description of the methodology employed in the Course and Outcome of Bipolar Youth (COBY) study has been described previously (Birmaher et al. 2006;Axelson et al. 2006). For the present analyses, we examined intake data for all 446 BP youth aged 7 to 17 who gave informed consent to participate in the COBY longitudinal multi-site study of pediatric BP.
Inclusionary Criteria
Subjects met the following criteria: 1) age 7 years 0 months to 17 years 11 months; 2) fulfill criteria for DSM-IV bipolar I (BPI), bipolar II (BPII), or study-operationalized criteria for bipolar disorder not otherwise specified (BPNOS; see Birmaher et al. 2006) via the Schedule for Affective Disorders and Schizophrenia for School-Aged Children, Present Episode 4th version (K-SADS-P; Kaufman et al. 1997) Depression section and Mania Rating Scale (Axelson et al. 2003); 3) determined to have a primary bipolar disorder; and 4) intellectual functioning within normal limits as determined at intake by clinical interview, child-/parent-report, and history of academic achievement. In the event that intellectual functioning inclusion criterion was questioned, the Wechsler Abbreviated Scales of Intelligence (WASI; The Psychological Corporation 1999) was administered.
Demographics/Patient Illness Characteristics
The sample was comprised of 237 (53%) males and 209 (47%) females with an average age of 12.7 years (SD=3.3). Subjects were, on average, middle class (M SES=3.4, SD=1.2; Hollingshead 1975). Eighty-one percent (n=363) identified themselves as Caucasian, 9% biracial (n=39), 8% African-American (n=34), 1% Asian (n=5), and 1% Other (n=5). Two hundred sixty participants (58%) met criteria for BPI, 32 (7%) BPII, and 154 (35%) BP NOS.
Procedures
Diagnosis
After consent and assent were obtained, COBY diagnosticians interviewed children directly, and parents about their children, for the presence of non-mood psychiatric disorders using the K-SADS-PL (Kaufman et al. 1997). The K-SADS-P depression and mania sections were used to assess each period of mood problems over the subject's lifetime (age 4 to present) to determine if DSM-IV criteria for a mood episode were met. Severity of depressive and manic symptoms for the current episode (worst week in the last month) was recorded on the K-SADS-P depression section and K-SADS-MRS.
Psychosocial Functioning
The Psychosocial Functioning Schedule of the Adolescent Longitudinal Interval Follow-Up Evaluation-Baseline (A-LIFE) was administered at study intake. Adolescents were interviewed about their own functioning, then parents were interviewed about their child. For younger subjects (<12), the child and parent were interviewed together. Summary ratings were then assigned for each item.
The A-LIFE Psychosocial Functioning Schedule has sound psychometric properties among individuals with affective disorders (Leon et al. 1999;Leon et al. 2000), and has been widely used in studies examining functional outcome in BP (Miklowitz et al. 2007) and other adolescent clinical populations (Phillips et al. 2006). The instrument examines functioning in 4 domains: 1) work (including employment, academic, and household), 2) interpersonal relations (including relatives and friends), 3) recreational activities and hobbies (e.g., reading, spectator or participant sports, listening to music, socializing, community organizations), and 4) global satisfaction. Ratings reflect the patient's functioning during the worst week of the preceding month, as follows: 1 (very good), 2 (good), 3 (fair/slightly impaired), 4 (poor/moderately impaired), and 5 (very poor/severely impaired). The total instrument score is the sum of the impairment scores in each of the 4 domains (for work and interpersonal relations, the most impaired sub-domain score is used to calculate the total), and ranges from 4 to 20.
The evaluator also rated the child's most impaired level of general functioning at intake on the Children's Global Assessment Scale (CGAS; Schaffer et al. 1983). Total scores on the A-LIFE significantly correlated with intake CGAS scores (CGAS M=54.8 ± 12.2, range=21-95; r=-.4, p<.01).
Severity of Current Mood Symptoms
Severity of depressive and manic symptoms for the current episode was assessed using the K-SADS-P depression section and the K-SADS-MRS.
Episode Status
Participants who met full DSM-IV criteria (or operationalized NOS criteria) for mania, hypomania, and/or depression via the K-SADS-P depression section and K-SADS-MRS were considered to be in-episode, consistent with definitions widely applied within the field (Frank et al. 1991;Judd et al. 2007). Partial remission was defined as less than eight consecutive weeks since the offset of the last mood episode meeting threshold criteria. Subjects were considered recovered if they had eight consecutive weeks since the offset of the last mood episode meeting threshold criteria.
Other Demographic and Clinical Information
Socioeconomic status (SES) was ascertained using the 4-factor Hollingshead scale (Hollingshead). Comorbid diagnoses and clinical characteristics were garnered from K-SADS interview summary scores. Age of BP onset was considered to be when the subject first met DSM-IV criteria for a manic, mixed, hypomanic, or major depressive episode, or when he/she first met COBY criteria for BP NOS.
In order to evaluate the differential clinical picture between BP children and adolescents, youth were divided into 3 subgroups according to age of onset and age at intake (age/age of onset) as follows: 1) childhood-onset BP (age <12; n=197, 44%); 2) adolescents with childhood onset (age ≥12 and BP onset <12; n=137, 31%); and 3) adolescents with adolescent onset (age ≥12 and BP onset ≥12; n=112, 25%).
Statistical Analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences Version 15 (SPSS). First, we used t-tests and simple regression to examine the association between the five domains of psychosocial functioning on the A-LIFE and demographic and clinical variables. These univariate analyses were considered to be hypothesis-generating, and therefore we did not apply a statistical adjustment for multiple comparisons. Next, demographic and clinical variables associated with functioning in the univariate analyses were entered into multivariate regression models conducted separately in each of the five functional domains to estimate the variance in each domain accounted for by each variable. All p-values are based on two-tailed tests, α=0.05.
Results
Psychosocial Functioning Among BP Youth
On average, the sample of BP youth had mild to moderate functional impairment across interpersonal (M=3.2 ± 1.0) and work domains (M=3.1 ± 1.2), whereas recreational functioning was good, with little to no impairment (M=2.1 ± 1.0). Subjects endorsed mild to moderate dissatisfaction with their current level of functioning (M=2.5 ± .9), yielding a mean total A-LIFE psychosocial functioning score of 10.7 (SD=3.1).
Demographic Variables
Sex
Females with BP reported more impairment in recreational functioning than males (t=2.4, p=.02, Cohen's d=.20) and were less satisfied with their current level of functioning (t=2.4, p=.02, d=.22). Females and males did not differ in interpersonal (t=1.0, p=.3, d=.09), work (t=.1, p=.9, d=.02), or total A-LIFE scores (t=1.5, p=.1, d=.19).
Age/Age of Onset
Table 1 details the relation between psychosocial impairment and current age/age of illness onset.
Table 1.
Association between A-LIFE psychosocial functioning scores and current age/age of illness onset
| A-LIFE domain of psychosocial functioning | Childhood Onset n = 197 (44%) Mean ± SD | Adolescent with Childhood Onset n = 137 (31%) Mean ± SD | Adolescent with Adolescent Onset n = 112 (25%) Mean ± SD | Child vs Adolescent with Childhood Onset | Child vs Adolescent with Adolescent Onset | Adolescent with Childhood Onset vs Adolescent with Adolescent Onset | omnibus F-value | omnibus p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| t | p | d | t | p | d | t | p | d | ||||||
| Work | 2.9 ± 1.1 | 3.2 ± 1.2 | 3.3 ± 1.2 | 2.5 | .01 | .26 | 2.8 | <.01 | .35 | .5 | .6 | .08 | F(2,415) = 5.1 | <.01 |
| Interpersonal | 3.2 ± 1.0 | 3.3 ± 1.0 | 3.1 ± 1.0 | 1.5 | .1 | .10 | .8 | .4 | .10 | 2.1 | .04 | .2 | F(2,428) = 2.2 | .1 |
| Recreation | 1.9 ± .8 | 2.1 ± 1.1 | 2.4 ± 1.1 | 1.7 | .1 | .21 | 3.7 | <.01 | .52 | 2.0 | .05 | .27 | F(2,426) = 7.4 | <.01 |
| Satisfaction | 2.3 ± .9 | 2.6 ± .9 | 2.8 ± .8 | 2.7 | <.01 | .33 | 4.5 | <.01 | .59 | 1.8 | .08 | .23 | F(2,407) = 10.1 | <.01 |
| A-LIFE Total | 10.0 ± 3.0 | 11.1 ± 3.0 | 11.4 ± 3.1 | 3.4 | <.01 | .37 | 3.9 | <.01 | .46 | .8 | .4 | .1 | F(2,430) = 9.9 | <.01 |
Race
No significant differences emerged in terms of functioning with respect to race (Caucasian versus Non-Caucasian; interpersonal t=1.2, p=.3, d=.13; work t=.9, p=.4, d=.12; recreational t=.1, p=.9, d=.01; satisfaction t=.8, p=.4, d=.10; total t=.1, p=.9, d=.01)
Socioeconomic Status
Lower SES was associated with greater impairment in interpersonal functioning (F(1,429)=6.4, p=.01, R2=.02). However, impairment in other domains of functioning did not differ by SES (p>.1, for all).
Living Situation
Subjects living with both natural parents, as opposed to those in any other type of living situation, reported significantly less impairment in interpersonal functioning (t=2.1, p=.04, d=.2), whereas impairment in other domains of functioning did not differ by living situation (p>.1 for all).
Clinical Variables
Bipolar Subtype
Participants in the sample diagnosed with BPI, II, and NOS reported similar levels of impairment in all A-LIFE domains (for all pairwise and omnibus comparisons p>.1).
Current Psychosis
BP youth who endorsed current psychosis (n=67, 15%) reported greater impairment in every domain examined (interpersonal t=3.0, p<.01, d=.48; work t=2.1, p=.04, d=.27; recreational t=2.2, p=.03, d=.27; total t = 3.5, p <.01, d=.44) and also greater dissatisfaction with their level of functioning at the trend level (t=1.8, p=.08, d=.21).
Severity of Current Mood Symptoms
Current depressive symptom severity was significantly associated with functional impairment in all domains (work F(1,406)=7.9, p<.01, R2=.02; recreational F(1,417)=35.7, p<.01, R2=.08; satisfaction F(1,398)=32.5, p<.01, R2=.08; total F(1,421)=19.8, p<.01, R2=.05) except interpersonal (F(1,419)=.02, p=.9, R2=0). Similarly, current manic symptom severity (total MRS score) significantly predicted A-LIFE scores in all domains (interpersonal (F(1,423)=8.7, p<.01, R2=.02; work F(1,410) = 15.2, p<.01, R2=.04; recreational F(1,421)=6.0, p=.02, R2=.01; satisfaction F(1,402)=6.8, p=.01, R2=.02; total F(1,425)=17.0, p<.01, R2=.04).
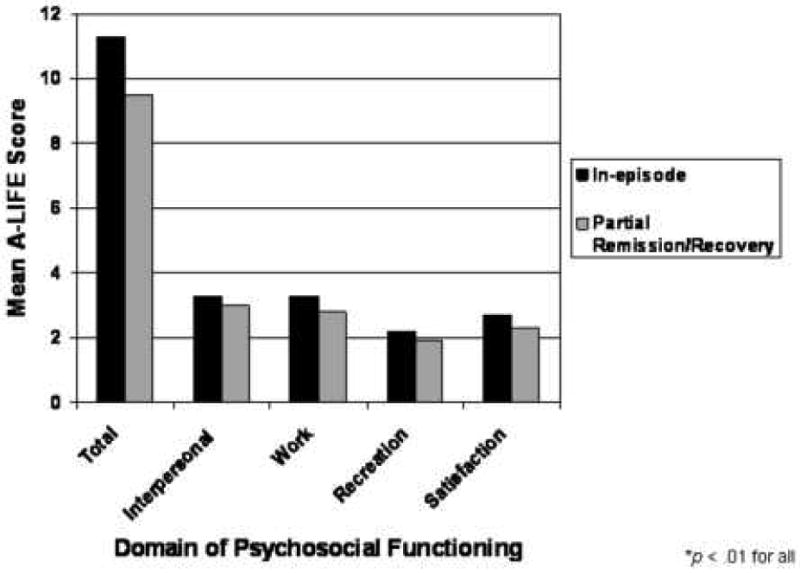
Episode Status
At intake, 64% (n=286) of subjects were in an affective episode, whereas 36% (n=160) were in partial remission or recovery. As seen in Figure 1, participants in-episode were significantly more impaired than those in partial remission/recovery in every functional domain examined (interpersonal t=2.9, p<.01, d=.3; work t=4.7, p<.01, d=.47; recreation t=4.2, p<.01, d=.4; total t=6.0, p<.01, d=.6) and were less satisfied with their functioning (t=4.1, p<.01, d=.42). However, functioning was also compromised among youth in partial remission/recovery.
Figure 1.
Mood State and Psychosocial Functioning
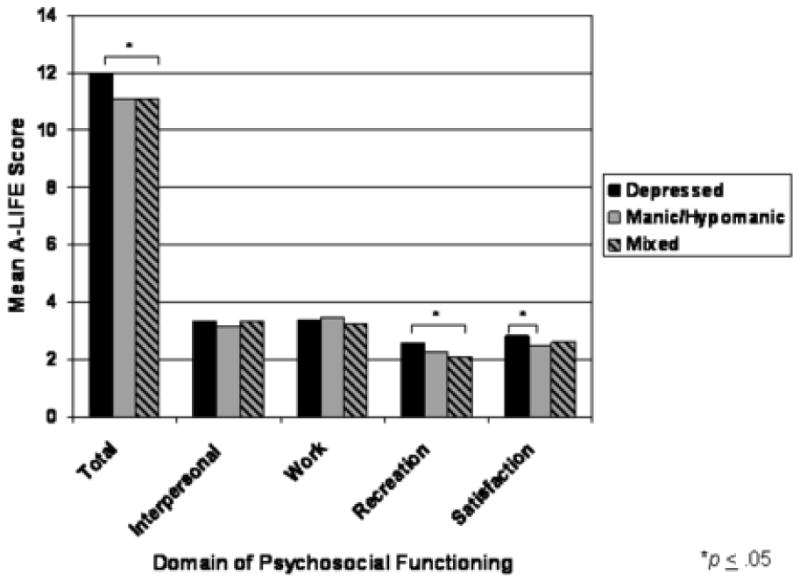
Figure 2 depicts differences in A-LIFE scores among BP youth in-episode by episode polarity. Depressed subjects had higher (i.e., more impairment) total (t=2.1, p=.04, d=.36) and recreational impairment scores (t=3.0, p<.01, d=.45) than mixed/cycling subjects, and reported greater dissatisfaction with their functioning than hypo/manic subjects (t=2.0, p=.05, d=.27). Mean interpersonal and work scores did not differ by polarity of intake mood episode.
Figure 2.
Current Comorbid Axis I Diagnoses
Table 2 summarizes findings regarding comorbid conditions and psychosocial functioning. Given that the majority of subjects in this sample met criteria for a DBD, we further examined the association between specific DBD diagnoses and functioning. Fifty-seven percent (n=252) met criteria for current ADHD. BP youth with ADHD reported greater impairment in interpersonal functioning than those without (t=2.0, p=.04, d=.2). However, comorbid ADHD was associated with less recreational impairment (t=2.5, p=.01, d=.3). Work, satisfaction, and total scores did not differ between BP youth with and without ADHD. This same pattern of functional impairment was also evident among BP youth with current Oppositional Defiant Disorder (ODD; n=147, 33%) such that current ODD was associated with greater interpersonal impairment (t=1.8, p=.08, d=.21) but less recreational impairment (t=2.1, p=.04, d=.2). There were no differences between youth with and without ODD in terms of work, satisfaction, or total scores. Fifty-one subjects (11%) met criteria for current Conduct Disorder (CD; per DSM-IV criteria, subjects who met criteria for both CD and ODD were assigned only the CD diagnosis). Those with CD were significantly more impaired than those without in all functional domains (interpersonal t=4.0, p<.01, d=.67; recreational t=1.8, p=.07, d=.29; satisfaction t=3.4, p<.01, d=.45; total t=3.6, p<.01, d=.53) with the exception of work (t=1.1, p=.3, d=.17).
Table 2.
Association between A-LIFE psychosocial functioning scores and comorbid Axis I disorders in bipolar youth
| Class of Current Comorbid Disorder | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A-LIFE Domain of Psychosocial Functioning | Current Anxiety Disorder | Current Behavioral Disorder | Current Substance Use Disorder | ||||||||||||
| Yes (n=146, 33%) M (SD) | No (n=300, 67%) M (SD) | t | p | d | Yes (n=310, 70%) M (SD) | No (n=136, 30%) M (SD) | t | p | d | Yes (n=22, 5%) M (SD) | No (n=424, 95%) M (SD) | t | p | d | |
| Work | 3.1(1.1) | 3.1(1.2) | .1 | >.1 | 0 | 3.2(1.1) | 3.0(1.2) | 1.7 | .08 | .17 | 3.6(1.3) | 3.1(1.1) | 1.6 | >.1 | .42 |
| Interpersonal | 3.2(1.0) | 3.2(1.0) | .2 | >.1 | 0 | 3.3(1.0) | 2.9(1.0) | 4.7 | <.01* | .40 | 3.1(.9) | 3.2(1.0) | .5 | >.1 | .11 |
| Recreation | 2.2(1.1) | 2.0(1.0) | 1.9 | .06 | .19 | 2.0(1.0) | 2.3(1.1) | 2.4 | .02* | .27 | 2.4(.7) | 2.1(1.0) | 2.0 | .06 | .35 |
| Satisfaction | 2.5(.9) | 2.5(.9) | .4 | >.1 | 0 | 2.5(.9) | 2.5(.9) | .4 | >.1 | 0 | 2.8(.8) | 2.5(.9) | 1.4 | >.1 | .35 |
| A-LIFE Total | 10.9(3.1) | 10.6(3.0) | 1.0 | >.1 | .10 | 10.8(3.0) | 10.4(3.3) | 1.3 | >.1 | .13 | 11.7(2.4) | 10.6(3.1) | 2.0 | .06 | .40 |
p < .05
Domain Analyses
Table 3 presents results from multiple regression analyses in each of the five functional domains entering significant demographic and clinical variables from the univariate analyses. Polarity of current mood state was not included due to high colinearity with current depressive and manic severity.
Table 3.
Multiple regression analyses by A-LIFE functional domain including significant predictors from univariate analyses
| β | Standard Error β | 95% Confidence Interval | F | p-value | |
|---|---|---|---|---|---|
| Interpersonal | |||||
| Age/Age of onset | .00 | .06 | -.12-.13 | .00 | .98 |
| SES | .06 | .04 | -.14-.02 | 1.92 | .17 |
| Lives with natural parents | -.07 | .10 | -.26-.13 | .44 | .51 |
| Currently in-episode | .19 | .11 | -.02-.39 | 3.04 | .08 |
| Current psychosis | .43 | .14 | .16-.70 | 9.96 | <.01* |
| Current manic severity score | .00 | .00 | -.01-.01 | .75 | .39 |
| Current conduct disorder | .65 | .16 | .33-.97 | 15.99 | <.01* |
| Current ADHD | .11 | .12 | -.12-.34 | .86 | .40 |
| Current ODD | .34 | .11 | .06-.53 | 6.17 | .01* |
| Number of current comorbid disorders | -.02 | .05 | -.10-.07 | .13 | .72 |
| Work | |||||
| Age/Age of onset | .23 | .07 | .09-.37 | 10.87 | <.01* |
| Currently in-episode | .41 | .13 | .16-.67 | 10.28 | <.01* |
| Current psychosis | .07 | .16 | -.25-.39 | 0.18 | .67 |
| Current depressive severity score | .00 | .00 | -.01-.02 | .37 | .54 |
| Current manic severity score | .01 | .00 | .00-.02 | 4.02 | .05* |
| Recreational | |||||
| Age/Age of onset | .13 | .07 | .00-.26 | 4.00 | .05* |
| Sex | .10 | .10 | -.10-.29 | .93 | .34 |
| Currently in-episode | .26 | .11 | .04-.48 | 5.52 | .02* |
| Current psychosis | .13 | .14 | -.14-.41 | .90 | .34 |
| Current depressive severity score | .02 | .01 | .01-.03 | 15.91 | <.01* |
| Current manic severity score | .00 | .01 | -.01-.01 | .01 | .92 |
| Current conduct disorder | .17 | .16 | -.15-.48 | 1.10 | .29 |
| Current ADHD | -.13 | .11 | -.35-.09 | 1.37 | .24 |
| Current ODD | -.01 | .11 | -.23-.20 | .00 | .95 |
| Current substance use disorder | .02 | .23 | -.43-.46 | .01 | .94 |
| Satisfaction | |||||
| Age/Age of onset | .19 | .06 | .08-.30 | 12.19 | <.01* |
| Sex | .10 | .09 | -.08-.27 | 1.24 | .27 |
| Currently in-episode | .25 | .10 | .05-.45 | 6.27 | .01* |
| Current psychosis | .11 | .13 | -.14-.35 | .71 | .40 |
| Current depressive severity score | .02 | .01 | .01-.03 | 13.48 | <.01* |
| Current manic severity score | .00 | .00 | -.01-.01 | .02 | .88 |
| Current conduct disorder | .34 | .13 | .08-.61 | 6.45 | .01* |
| A-LIFE Total | |||||
| Age/Age of onset | .70 | .18 | .35-1.06 | 15.3 | <.01* |
| Currently in-episode | 1.4 | .32 | .75-2.02 | 18.28 | <.01* |
| Current psychosis | .80 | .41 | .00-1.60 | 3.79 | .05* |
| Current depressive severity score | .03 | .02 | .00-.06 | 2.87 | .09 |
| Current manic severity score | .02 | .01 | -.01-.04 | 1.31 | .25 |
| Current conduct disorder | 1.22 | .45 | .33-2.1 | 7.27 | <.01* |
| Current substance use disorder | -.17 | .66 | -1.46-1.13 | .06 | .80 |
p ≤ .05
SES = Socioeconomic status
ODD = Oppositional defiant disorder
ADHD = Attention deficit hyperactivity disorder
Discussion
Overall, mild to moderate levels of psychosocial impairment were evident in work (includes academics) and interpersonal (includes family and friends) domains of functioning in our sample of BP youth. On average, BP youth endorsed good recreational functioning but reported moderate dissatisfaction with their overall level of functioning.
Multivariate analysis indicated that overall functional impairment among BP youth is greatest among adolescents (regardless of whether illness onset was in childhood or adolescence), those currently in a mood episode, with current psychotic symptoms, and current CD. Poorer interpersonal functioning was most strongly associated with current psychosis, CD and ODD, whereas poorer work functioning was predicted by older age, current mood episode, and greater manic severity. Impairment in recreational functioning was greatest among adolescents with late onset, those in a current mood episode, and those with greater depressive severity. Finally, dissatisfaction with functioning was most highly associated with adolescence (regardless of age of onset), current mood episode, greater depressive severity, and CD.
The level of functional impairment on the semi-structured A-LIFE scale in this sample is similar to that reported among adolescents with body dysmorphic disorder (Phillips et al. 2006). As compared with two other recent studies of functioning in BP youth, our findings indicate less functional impairment--this may be explained by two methodological differences: the type of assessment instruments used and the definition of psychosocial functioning employed. Rucklidge (2006) reported on intra-individual domains of functioning (e.g., self-esteem) using self-report methodology, whereas Esposito-Smythers et al. (2006) examined family functioning (e.g., conflict) via self- and parent-report.
Like Biederman et al. (2005), we found that BP adolescents, regardless of age of onset, reported greater functional impairment across domains than BP children. Given that psychosocial demands increase throughout development, older youth may find their illness symptoms render them less capable of meeting the mounting psychosocial challenges.
It is noteworthy that mild to moderate impairment was evident in work, interpersonal, and satisfaction domains, whereas recreational functioning remained good even while in-episode. This finding is similar to that reported by Rademacher et al. (2007) in which acutely manic/mixed adolescents exhibited impairment when compared with national norms in all domains of psychosocial functioning with the exception of “social limitations.” Our clinical experience indicates that many BP youth engage in recreational activities that remain feasible during symptomatic periods (e.g., playing computer games). It is also possible that hypomanic symptoms “buffer” against the negative impact of the illness on functioning, and even serve to enhance functioning in certain domains.
Results indicate that current psychosis is a strong predictor of impairment across functional domains in pediatric BP. Given findings from Birmaher et al. (2006) from the first 263 COBY subjects in which lifetime psychosis predicted more time with mood symptoms over follow-up, psychosis may serve as a marker for greater illness duration and severity, thereby influencing psychosocial functioning.
Functioning did not differ between BP subtypes (I, II, NOS) in the present sample of youth. These findings converge with Judd's (2007) findings in adults and suggest that BP spectrum illnesses confer similar risk for disability and impairment. Similar to findings from other samples of depressed (Seeley 2002) and BP youth (Biederman et al. 1997), we found that comorbid CD was associated with particularly poor outcomes.
In support of our hypothesis, we found BP youth in an affective episode were more impaired than those in partial remission/recovery in every functional domain examined and were less satisfied with their functioning. Similar to findings among BP adults, we found that BP youth in-episode, as compared with those in partial recovery/remission, experienced greater functional impairment in every psychosocial domain examined. Yet, functional impairment remained evident, albeit to a lesser degree, between illness episodes. Our findings converge with those of previous studies indicating significant impairment across domains among youth with BP during episodes of illness (Wilens et al. 2003;Geller et al. 2000;Lewinsohn et al. 1995) as well as during periods of syndromic and symptomatic recovery (DelBello et al. 2007;Goldstein et al. 2006). Furthermore, similar to findings by Judd and colleagues (2005) among BP adults using the LIFE, our data indicate functioning in BP youth is more highly impaired during depressive episodes versus manic/mixed/cycling episodes. Depressive symptoms appear to have a particularly deleterious impact on recreational functioning and satisfaction with functioning among BP youth, whereas manic symptoms appear to most strongly impede work functioning in this population.
The converging evidence thus supports the notion that youth with BP experience significant functional impairment both during and between mood episodes. However, the direction of causality remains to be established. It is possible that functional impairments predate illness onset. Alternatively, a third variable may account for the relationship—for example, compromised cognitive functioning. Functional impairment may emerge as a result of episodes of illness or be attributable to subsyndromal symptomatology between episodes. Per Hammen's (1991) stress generation model, episodes of illness may lead to increases in social stress and subsequent deterioration in functioning. Youth with BP may fall behind their healthy peers in terms of psychosocial development during episodes of illness and are not able to fully recover from the delay when the episode remits. Finally, Post's kindling model (Post and Weiss 1995) may not only explain course and severity of illness, but also psychosocial functioning. This argument may be particularly compelling given the critical period for brain development throughout childhood and adolescence (Dahl 2004).
Limitations
The limitations of the present study include the reliance on patient and parent retrospective report of functioning. Additionally, self- and parent-perceptions of the subjects' functioning may be differentially impacted by developmental differences—i.e., younger children may have less insight into their impairment, while their parents may have lower expectations regarding psychosocial functioning.
COBY is largely a clinical sample, and thus may not be representative of pediatric BP patients who have not sought treatment. However, results from Lewinsohn's (1995) epidemiological sample indicate similar functional impairment among BP youth. Additionally, although findings from adult studies support a relationship between cognitive deficits and functional impairment during periods of remission in BP (Martinez-Aran et al. 2004), cognitive functioning was not formally assessed at intake.
Clinical Implications
Pediatric BP is associated with significant psychosocial impairment, particularly during the adolescent years and among those with greater illness severity and comorbid DBD. The present findings highlight the importance of future work on the development of treatments focused on improving psychosocial functioning in pediatric BP, particularly in the areas of family and peer interactions. Interventions for BP youth should seek to not only reduce symptoms and prevent relapse, but also promote normalization of psychosocial functioning.
Future Directions
Forthcoming prospective data from COBY will further inform our understanding of the temporal relationship between mood symptoms, episodes of illness, comorbidities, and functioning among BP youth. Given that critical building blocks of successful psychosocial development are established throughout childhood and adolescence, further study of the impact of the illness on psychosocial development is imperative in order to decrease the deleterious impact early episodes may have on subsequent functioning.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- Axelson D, Birmaher B, Brent D, Wassick S, Hoover C, Bridge J, Ryan N. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-age Children Mania Rating Scale for Children and Adolescents. J Child Adolesc Psychopharmacol. 2003;13:463–470. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- Axelson D, Birmaher B, Strober M, Gill K, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Bridge J, Keller M. Phenomenology of children and adolescents with bipolar spectrum disorders. Arch Gen Psych. 2006;63:1139–1148. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone S, Hatch M, Mennin D. Conduct disorder with and without mania in a referred sample of ADHD children. J Affect Disord. 1997;44:177–188. doi: 10.1016/s0165-0327(97)00043-8. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone S, Wozniak J, Mick E, Kwon A, Cayton G, Clark S. Clinical correlates of bipolar disorder in a large, referred sample of children and adolescents. J Psychiat Res. 2005;39:611–622. doi: 10.1016/j.jpsychires.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Keller M. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63:175–183. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl R. Adolescent brain development: a period of vulnerabilities and opportunities. Ann NY Acad Sci. 2004;1021:1–22. doi: 10.1196/annals.1308.001. [DOI] [PubMed] [Google Scholar]
- DelBello M, Hanseman D, Adler C, Fleck D, Strakowski S. Twelve month outcome of adolescents with bipolar disorder following first-hospitalization for a manic or mixed episode. Am J Psychiatry. 2007 doi: 10.1176/ajp.2007.164.4.582. [DOI] [PubMed] [Google Scholar]
- Esposito-Smythers C, Birmaher B, Valeri S, Chiappetta L, Hunt J, Ryan N, Axelson D, Strober M, Leonard H, Sindelar H, Keller M. Child comorbidity, maternal mood disorder, and perceptions of family functioning among bipolar youth. J Am Acad Child Adolesc Psychiatry. 2006;45:955–964. doi: 10.1097/01.chi.0000222785.11359.04. [DOI] [PubMed] [Google Scholar]
- Fagiolini A, Kupfer D, Masalehdan A, Scott J, Houck P, Frank E. Functional impairment in the remission phase of bipolar disorder. Bipolar Disorders. 2005;7:281–285. doi: 10.1111/j.1399-5618.2005.00207.x. [DOI] [PubMed] [Google Scholar]
- Faraone S, Biederman J, Weber W, Russell R. Psychiatric, neuropsychological, and psychosocial features of DSM-IV subtypes of attention deficit/hyperactivity disorder: Results from a clinically referred sample. J Am Acad Child Adolesc Psychiatry. 1998;37:185–193. doi: 10.1097/00004583-199802000-00011. [DOI] [PubMed] [Google Scholar]
- Frank E, Prien R, Jarrett R, Keller M, Kupfer D, Lavori P, Rush A, Weissman M. Conceptualization and rationale for consensus definitions of terms in major depressive disorder: Remission, recovery, relapse, and recurrence. Arch Gen Psychiatry. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- Geller B, Bolhofner K, Craney J, Williams M, DelBello M, Gundersen K. Psychosocial functioning in a prepubertal and early adolescent bipolar disorder phenotype. J Am Acad Child Adolesc Psychiatry. 2000;39:1543–1548. doi: 10.1097/00004583-200012000-00018. [DOI] [PubMed] [Google Scholar]
- Goldstein T, Mullen K, Miklowitz D. Social skills knowledge and performance among adolescents with bipolar disorder. Bipolar Disorders. 2006;8:350–361. doi: 10.1111/j.1399-5618.2006.00321.x. [DOI] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. J Abnorm Psychol. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hollingshead A. Four-factor Index of Social Status. Yale University; New Haven: 1975. [Google Scholar]
- Judd L, Akiskal H, Schettler P, Endicott J. The long-term natural history of the weekly symptomatic status of bipolar disorder. Arch Gen Psychiatry. 2007;59:530–537. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- Judd L, Akiskal H, Schettler P, Endicott J, Leon A, Solomon D, Coryell W, Maser J, Keller M. Psychosocial disability in the course of bipolar I and II disorders: a prospective, comparative longitudinal study. Arch Gen Psychiatry. 2005;62:1322–1330. doi: 10.1001/archpsyc.62.12.1322. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keck P, Jr, McElroy S, Strakowski S, West S, Sax K, Hawkins J, Bourne M, Haggard P. 12-month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. Am J Psychiatry. 1998;155:646–652. doi: 10.1176/ajp.155.5.646. [DOI] [PubMed] [Google Scholar]
- Leon A, Solomon D, Mueller T, Endicott J, Posternak M, Judd L, Schettler P, Akiskal H, Keller M. A brief assessment of psychosocial functioning of subjects with bipolar I disorder. J Nerv Ment Dis. 2000;188:805–812. doi: 10.1097/00005053-200012000-00003. [DOI] [PubMed] [Google Scholar]
- Leon A, Solomon T, Turvey C, Endicott J, Keller M. The range of impaired functioning tool (LIFE-RIFT): a brief measure of functional impairment. Psychol Med. 1999;29:869–878. doi: 10.1017/s0033291799008570. [DOI] [PubMed] [Google Scholar]
- Lewinsohn P, Klein D, Seeley J. Bipolar disorders in a community sample of older adolescents: Prevalence, phenomenology, comorbidity and course. J Am Acad Child Adolesc Psychiatry. 1995;34:454–463. [PubMed] [Google Scholar]
- Martinez-Aran A, Vieta E, Reinares M, Colom F, Torrent C, Sanchez-Moreno J, Benabarre A, Goikolea J, Comes M, Salamero M. Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am J Psychiatry. 2004;161:262–270. doi: 10.1176/appi.ajp.161.2.262. [DOI] [PubMed] [Google Scholar]
- Miklowitz D, Otto M, Frank E, Reilly-Harrington N, Kogan J, Sachs G, Thase M, Calabrese J, Marangell L, Ostacher M, Patel J, Thomas M, Araga M, Gonzales J, Wisniewski S. Intensive psychosocial intervention enhances functioning in patients with bipolar depression: Results from a 9-month randomized controlled trial. Am J Psychiatry. 2007;164:1340–1347. doi: 10.1176/appi.ajp.2007.07020311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morriss R. Clincial importance of inter-episode symptoms in patients with bipolar affective disorder. J Affect Disord. 2002;72:3–13. doi: 10.1016/s0165-0327(02)00340-3. [DOI] [PubMed] [Google Scholar]
- Phillips K, Didie E, Menard W, Pagano M, Fay C, Weisberg R. Clinical features of body dysmorphic disorder in adolescents and adults. Psychiatry Res. 2006;141:305–314. doi: 10.1016/j.psychres.2005.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post R, Weiss S. The neurobiology of treatment-resistant mood disorders. In: Bloom FE, Kupfer DJ, editors. Psychopharmacology : The Fourth Generation of Progress. Raven Press; NY: 1995. pp. 1155–1170. [Google Scholar]
- Rademacher J, DelBello M, Adler C, Stanford K, Strakowski S. Health-related quality of life in adolescents with bipolar disorder. J Child Adolesc Psychopharmacol. 2007;17:97–103. doi: 10.1089/cap.2006.0049. [DOI] [PubMed] [Google Scholar]
- Rucklidge J. Psychosocial functioning of adolescents with and without paediatric bipolar disorder. J Affect Disord. 2006;91:181–188. doi: 10.1016/j.jad.2006.01.001. [DOI] [PubMed] [Google Scholar]
- Schaffer D, Gould M, Brasic J. A children's global assessment scale. Arch Gen Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Seeley J. Dissertation Abstracts International. 12A. Vol. 62. 2002. Comorbidity between conduct disorder and major depression: Phenomenology, correlates, course and familial aggregation; p. 4122. [Google Scholar]
- The Psychological Corporation. Wechsler Abbreviated Scales of Intelligence. Harcourt Brace and Company; San Antonio: 1999. [Google Scholar]
- Wilens T, Biederman J, Forkner P, Ditterline J, Morris M, Moore H, Galdo M, Spencer T, Wozniak J. Patterns of comorbidity and dysfunction in clinically referred preschool and school-age children with bipolar disorder. J Child Adolesc Psychopharmacol. 2003;13:495–505. doi: 10.1089/104454603322724887. [DOI] [PubMed] [Google Scholar]


