Abstract
The prevalence of childhood sexual and physical abuse among persons with severe mental illness (SMI) is disproportionately high. Adults with SMI also engage in high rates of HIV risk behaviors. This study examined the association between childhood abuse and adult victimization, substance abuse, and lifetime HIV sexual risk in a sample of 152 adults with SMI receiving community mental health services. Structured interviews assessed psychiatric, psychosocial, and behavioral risk factors. Seventy percent reported childhood physical and/or sexual abuse, and 32% reported both types of abuse. Participants with childhood abuse were more likely to report adult victimization and greater HIV risk. A structural equation model found that childhood abuse was directly and indirectly associated with HIV risk through drug abuse and adult vicitimization. Integrated treatment approaches that address interpersonal violence and substance abuse may be necessary for HIV risk reduction in this population.
Keywords: severe mental illness, HIV risk behavior, childhood abuse, substance abuse, revictimization
INTRODUCTION
The prevalence of childhood sexual and physical abuse among persons with severe mental illness (SMI) is disturbingly high. Among women with SMI, 43-52% report a history of childhood sexual abuse and 33-52% report a history of childhood physical abuse (e.g., Cloitre et al., 1996; Muenzenmaier et al., 1993; Mueser et al., 1998; Rosenberg et al., 2007), compared to 13-32% and 20-21%, respectively, among women in the general population (Briere and Elliot, 2003; Chartier et al., 2007; Edwards et al., 2003; Finkelhor et al., 1990). Many fewer studies have examined the prevalence of childhood abuse among men. Two studies reported that 29-36% of men with SMI reported childhood sexual abuse and 38-59% reported childhood physical abuse (Mueser et al., 1998; Rosenberg et al., 2007), compared to 4-18% and 15-31%, respectively, among men in the general population (Briere and Elliot, 2003; Chartier et al., 2007; Edwards et al., 2003; Finkelhor et al., 1990). Overall, women are more likely than men to report childhood sexual abuse, but there is no gender difference in the prevalence of childhood physical abuse (Briere and Elliot, 2003; Finkelhor et al., 1990; Goodman et al., 2001). Childhood sexual and physical abuse often co-occur, making it difficult to tease apart the long-term sequelae of each type of abuse (Briere and Elliot, 2003; Dévieux et al., 2007; Rosenberg et al., 2007).
Adults with severe mental illness (SMI) are disproportionately affected by HIV/AIDS. A large multi-city study reported HIV seroprevalence rates ranging from 2% to 5% in rural and metropolitan sites, respectively (Rosenberg et al., 2001), compared to 0.8% in the United States population (UNAIDS, 2006). Prior research has also documented that adults with SMI engage in high rates of sexual risk behaviors associated with HIV transmission, including multiple partners and sex trading (Meade and Sikkema, 2005a). Yet, few studies have examined the relationship between childhood abuse and HIV sexual risk behavior in this population. These studies have linked sexual and/or physical abuse, typically occurring in childhood, with sex trading (Goodman and Fallot, 1998; van Dorn et al., 2005), inconsistent condom use (Brown et al., 2000; Meade and Sikkema, 2007; van Dorn et al., 2005), more sex acts and sex partners (Malow et al., in press), higher sexual risk (Dévieux et al., 2007), and sexually transmitted infections (Brown et al., 2000). However, the complex associations between childhood abuse and HIV risk have been inadequately examined, particularly among men, and studies have not systematically examined factors that may mediate this relationship (e.g. substance abuse, adult victimization).
Theoretical models linking childhood abuse to HIV risk
Theoretical models have been proposed to explain the relationship between childhood abuse and HIV risk behavior in the general population, with the long-term sequelae of childhood abuse mediating this relationship. In perhaps the most comprehensive model, Malow and colleagues (2006) proposed that childhood sexual abuse is directly related to HIV risk behavior, with substance use, adult revictimization, and psychopathology acting as mediators. Similarly, Miller (1999) proposed a model in which the relationship between sexual abuse and HIV risk in women is mediated by drug use, sexual adjustment, and psychopathology. These authors urged that the causal and mediating pathways be empirically evaluated using modeling approaches. The primary purpose of the current study was to examine the relationship between childhood abuse and HIV risk behavior among adults with SMI using structural equation modeling (SEM). Figure I represents the hypothesized model in which childhood abuse is directly associated with lifetime HIV risk, and indirectly associated with HIV risk through substance abuse and adult victimization. Because childhood sexual and physical abuse frequently co-occur, especially in high risk samples, it can be difficult to tease apart the unique effects of each type of abuse. Therefore, as in prior studies (e.g., Kimerling et al., 2007; Sachs-Ericsson et al., 2007), we examined childhood abuse as a single variable encompassing both sexual and physical abuse. Literature related to each of these pathways is described below.
Figure I.
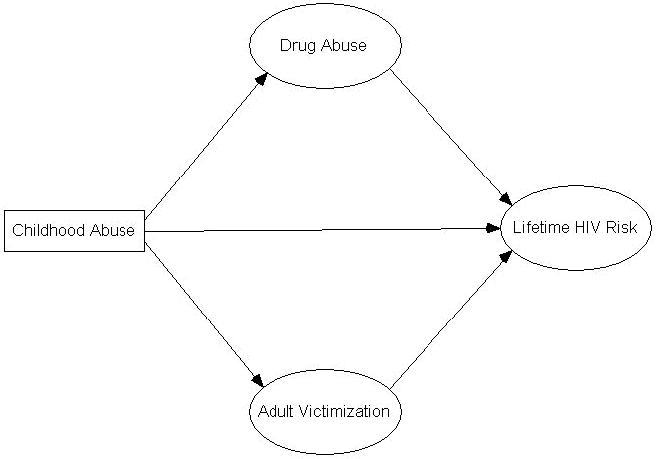
Hypothesized relationships between childhood abuse, drug abuse, adult victimization, and lifetime HIV risk
Childhood sexual and physical abuse are associated with mental health problems and psychiatric disorders in adulthood (MacMillian et al., 2001; Molnar et al., 2001). Among adults with SMI, childhood abuse is associated with greater psychiatric symptoms, including depression, psychosis, dissociation, and posttraumatic stress (Craine et al., 1988; Malow et al., in press). In non-SMI samples, childhood abuse is related to HIV risk behaviors, including earlier sexual debut, multiple sex partners, unprotected intercourse, sex trading, and sexually transmitted infections (e.g., Arriola et al., 2005; Cohen et al., 2000; Parillo et al., 2001). As discussed above, emerging evidence suggests that this may also be the case among adults with SMI. Thus, it was hypothesized that childhood abuse would be directly associated with HIV risk.
Approximately half of adults with SMI have co-occurring substance use disorders (Regier et al., 1990). Childhood physical and sexual abuse are risk factors for substance abuse in the general (Simpson and Miller, 2002) and SMI (Craine et al., 1988; Goodman et al., 1997) populations. In turn, substance abuse, particularly cocaine (Vaddiparti et al., 2006), is a strong predictor of HIV risk behavior in non-SMI populations (Chesney et al., 1998; Weinhardt and Carey, 2000). Thus, it was hypothesized that substance abuse would be directly associated with HIV risk and would mediate the relationship between childhood abuse and HIV risk.
Individuals who are abused in childhood are more likely to be sexually and physically abused again in adulthood, often repeatedly (Arriola et al., 2005; Cloitre et al., 1996; Goodman et al., 2001), and SMI is a risk factor for revictimization (Classen et al., 2005). In a recent review, childhood physical and sexual abuse each predicted sexual revictimization in adulthood, which in turn predicted greater substance abuse and HIV risk behavior, including more sex partners, sex trading, and sexually transmitted infections (Classen et al., 2005). Thus, it was hypothesized that adult victimization would be directly associated with HIV risk and would mediate the relationship between childhood abuse on HIV risk.
Study aims
The purpose of this study was to examine the association between childhood abuse and adult victimization, substance abuse, and lifetime HIV risk. First, we compared participants with sexual abuse only, physical abuse only, both sexual and physical abuse, and no abuse to determine whether childhood physical and sexual abuse yield differential outcomes. We hypothesized that participants with any childhood abuse would report higher rates of substance abuse, adult victimization, and HIV risk compared to participants with no childhood abuse. Second, we tested a model of HIV risk among adults with SMI using SEM (see Figure I). We hypothesized that childhood abuse would be both directly and indirectly associated with HIV risk through substance abuse and adult victimization. Third, we examined gender differences in the prevalence and long-term correlates of childhood abuse. We expected that women would experience higher rates of both childhood abuse and adult victimization, but that childhood abuse would be predictive of lifetime HIV risk in both genders.
METHODS
Participants and procedure
Data for this study came from a research project examining HIV risk among adults with SMI (see also Meade, 2006; Meade and Sikkema, 2005b, 2007). Participants were recruited between March 2003 and March 2004 from multiple sites serving adults with SMI in a small, Northeastern city. These included a community mental health center (25%), an intensive outpatient program (14%), a crisis/respite center (25%), and four supportive housing programs (36%). The vast majority of participants received their primary psychiatric treatment from the community mental health center and adjunctive services through affiliated agencies (e.g., intensive outpatient, vocational counseling, residential treatment). Based on data compiled by the clinical information department at the community mental health center, study participants were similar to the greater population of patients served at this center in terms of gender, age, marital status, and educational attainment, but they were less likely to be Black (27% vs. 38%, p < .05).
Recruitment strategies included flyers, presentations, and clinician referral. Eligibility criteria were: diagnosis of SMI (e.g., schizophrenia, major depression, or bipolar disorder, persisting over time and causing extensive disability in social, occupational, and other important areas of functioning), 18-65 years of age, English proficiency, and no major cognitive impairments precluding an interview. A face-to-face, structured, 90-minute interview assessed psychiatric, psychosocial, behavioral, and demographic factors. All participants provided informed consent, completed the full interview, and received $20 compensation. Study procedures were approved by an institutional review board.
Measures
Childhood abuse and adult victimization
The Trauma History Questionnaire (THQ) was used to identify physical and sexual abuse occurring in childhood (≤17 years) and adulthood (≥18 years) (Green, 1996). Physical abuse was defined as any type of physical harm caused by another person (e.g., hitting, slapping, chocking, burning, or beating). Sexual abuse was defined as any unwanted sexual touching, oral sex, or vaginal/anal intercourse that was forced or coerced, and any type of sexual contact with someone at least 5 years older before 13 years of age. Participants also reported how often each type of abuse happened and its duration. The THQ has high inter-rater reliability and test-retest reliability and has been used extensively with adults with SMI (Mueser et al., 2001). A prior analysis of the current data found that childhood sexual abuse was associated with inconsistent condom use in the past year (Meade and Sikkema, 2007).
Lifetime substance abuse
Clinicians provided DSM-IV-TR Axis I diagnoses, including lifetime alcohol and drug use disorders (APA, 2000). Participants reported whether or not they had ever had a “substance abuse problem”. They also reported their lifetime use of specific substances, including cocaine and crack.
Lifetime HIV sexual risk
Items were derived from prior risk behavior assessments that the have been used successfully with adults with SMI and have high test-retest reliability (McKinnon et al., 1993; Sohler et al., 2000). Participants reported the total number of lifetime sex partners, history of lifetime sex trading for money, alcohol/drugs, or other goods, and history of sexually transmitted infection. Prior research has established that adults with SMI can reliably report lifetime HIV risk behaviors (Rosenberg et al., 2003) and that they are predictive of HIV infection (Essock et al., 2003).
Demographic information
Participants reported their age, gender, race/ethnicity, sexual orientation, marital status, employment status, and monthly income.
Data analytic strategy
The prevalence of childhood sexual and physical abuse were computed, and gender differences were examined using chi-square tests. These childhood abuse experiences were then described, including prevalence of repeated abuse, mean duration of abuse, and relationship to perpetrator(s). Participants were categorized by their childhood abuse status: sexual abuse only, physical abuse only, both sexual and physical abuse, and no abuse. Chi-square tests were used to compare these groups on the following dichotomous variables: lifetime substance abuse (drug use disorder diagnosis, alcohol use disorder diagnosis, self-reported substance abuse problem, and cocaine/crack use), adult victimization (sexual abuse, physical abuse), and lifetime HIV risk (≥20 sex partners, sex trading, sexually transmitted infection). As planned contrasts are more appropriate than omnibus tests for focused questions of multiple groups and allow greater statistical power and clarity of interpretation (Rosnow and Rosenthal, 2002), two planned contrasts were conducted: (1) sexual abuse only versus physical abuse only (to determine whether participants with either type of childhood abuse were equally likely to report negative outcomes), and (2) sexual and/or physical abuse versus no abuse (to determine whether participants with any type of childhood abuse were more likely to have negative outcomes compared to those with no childhood abuse history). These analyses were conducted in SPSS 13.0 (SPSS, Chicago, IL).
SEM was used to assess the hypothesized model. Multiple indicator latent variables were created as follows: lifetime drug abuse (drug use disorder diagnosis, cocaine/crack use, self-reported substance abuse problem), adult victimization (sexual abuse, physical abuse), and lifetime HIV sexual risk (number of sex partners, sex trading, sexually transmitted infection). Number of partners was winsorized to minimize skew and reduce the influence of extreme scores. All of the other indicator variables were dichotomous. A polychoric correlation matrix using weighted least squares estimation and an asymptotic covariance matrix was used (Joreskog, 2004). The advantage of this analysis is that it does not make distributional assumptions and is therefore appropriate for ordinal and non-normally distributed variables.
Five things were assessed: (1) overall fit of the model, (2) amount of variability (R2) of the latent mediators and outcome accounted for by the variables in the model, (3) significance of the individual structural paths, (4) direct and indirect effects of childhood abuse on lifetime HIV risk (test for mediation) and (5) whether the model and individual paths differed significantly between men and women. For the overall fit, the closeness of the hypothetical model to the empirical data was evaluated through goodness-of-fit indices. A chi-square value of no more than twice the degrees of freedom in the model is generally indicative of a plausible, well-fitting model (Bollen, 1989; Jaccard and Wan, 1996). However, as the chi-square value is influenced by sample size and even good fitting models may have significant chi-square values, it is recommended that multiple fit indices be used to assess model fit. The root mean square error of approximation (RMSEA) assesses absolute fit but penalizes for less parsimonious models. The RMSEA is a badness-of-fit index, with values less than 0.06 being desirable (Hu and Bentler, 1999). The comparative fit index (CFI) and the non-normed fit index (NNFI) compare the absolute fit with an independence model that assumes no relationships among variables, and values greater than .95 indicate good fit (Hu and Bentler, 1999). We used the chi-square, the RMSEA, the CFI, and the NNFI to evaluate the overall fit of the model. Mediation was tested by first assessing whether there was a direct and overall indirect relationship between the predictors and HIV risk, and then testing the indirect effect of each predictor on HIV risk using Sobel tests. This method has been shown to be a valid and reliable method of assessing mediation (Preacher and Hayes, 2004). Finally, multiple-group comparisons were used to determine whether the overall model or individual paths differed among men and women (Bollen, 1989; Jaccard and Wan, 1996). This was done by running two models: In one model the parameter of interest was allowed to vary across groups, and in the other model the structural path was constrained to be equal across the two groups. The difference between the two chi-square fit indices for each model yielded a chi-square test indicating whether or not the path differed significantly across the groups. A significant differential chi-square would indicate that gender moderates the path. All SEM analyses were performed using LISREL 8.5 (SSI, Lincolnwood, IL).
RESULTS
Participant characteristics
The sample was comprised of 70 women and 82 men with SMI. Participants ranged in age from 20 to 63 years (M = 38.61 ± 9.28) and were racially diverse (58% White, 27% Black, 11% Hispanic, 4% mixed/other). Most identified as heterosexual (85%) and had a high school education (80%). Reflecting their SMI status, the majority was single (66% never married, 28% divorced/separated, 1% widowed), was currently unemployed (82%), had a monthly income under $1000 (89%), and had a history of homelessness (80%). Primary psychiatric diagnoses were: 40% psychotic disorder (20% schizoaffective, 18% schizophrenia, 2% other) and 60% non-psychotic disorder (29% major depressive, 26% bipolar, 5% posttraumatic stress). Two thirds had a lifetime history of substance use disorder, and 47% met criteria within the past year. Ninety percent had one or more inpatient psychiatric hospitalizations (M = 7.03 ± 8.35), and 54% were hospitalized in the past year. All were currently receiving treatment for their SMI.
Almost all participants (93%) had at least one lifetime sex partner. The mean number of sex partners was 22.82 (SD = 36.37, range = 0–300); 37% of participants had 20 or more sex partners. One third (33%) had ever engaged in sex trading, and 36% had a history of sexually transmitted infection. Two participants reported that they were HIV-positive.
Prevalence, description, and correlates of childhood abuse
The prevalence of childhood sexual and physical abuse was 47% and 58%, respectively. The majority (70%) reported at least one type of abuse, and 32% reported both types of abuse. Women were more likely than men to have been sexually abused (63% vs. 33%, χ2(1) = 13.59, p < .001), but there was no gender difference for physical abuse (61% vs. 50%, χ2(1) = 2.00, p = 0.16). Men were more likely to report no childhood abuse (40% vs. 19%, χ2(1) = 8.40, p = .004). Whites were more likely to report a history of physical abuse (65% vs. 42%, χ2(1) = 7.65, p = .006), but there was no race difference for sexual abuse (51% vs. 41%, χ2(1) = 1.65, p = .20). There were no group differences on age, educational attainment, sexual orientation, or marital status (all p > .10).
There were also gender and race differences on adult victimization. Women were more likely to report adult sexual abuse (46% vs. 9%, χ2(1) = 27.36, p < .001) and adult physical abuse (43% vs. 24%, χ2(1) = 10.96, p = .001). Whites were more likely to report adult sexual abuse (33% vs. 16%, χ2(1) = 5.83, p = .016) but not adult physical abuse (49% vs. 35%, χ2(1) = 3.18, p = .08)
Table I describes participants’ childhood abuse experiences. Among participants who reported childhood sexual abuse, 61% experienced repeated abuse occurring over a mean of 5.13 years (SD = 3.92). Women were more likely than men to have been repeatedly sexually abused, abused for longer duration, and abused by a family member. Among participants who reported childhood physical abuse, 68% reported repeated abuse occurring over a mean of 7.57 years (SD = 6.29). There were no gender differences in the frequency and duration of physical abuse, but women were more likely to have been physically abused by a partner.
Table I.
Description of childhood abuse experiences among adults with SMI
| Women | Men | Statistic | p-value | |
|---|---|---|---|---|
| Sexual abuse | n = 44 | n = 27 | ||
| Repeated abuse | 73% | 44% | χ2(1)=5.34 | .021 |
| Duration of abuse (yrs) | M = 6.02 ± 4.22 | M = 3.28 ± 2.41 | t(34)=2.50 | .017 |
| Perpetrator | ||||
| Family member | 73% | 37% | χ2(1)=8.27 | .004 |
| Other adult | 22% | 33% | χ2(1)=1.10 | .295 |
| Partner | 7% | 0% | χ2(1)=1.51 | .220 |
| Stranger | 16% | 19% | χ2(1)=0.06 | .809 |
| Peer | 8% | 26% | χ2(1)=3.76 | .053 |
| Multiple | 24% | 15% | χ2(1)=0.87 | .350 |
| Physical abuse | n = 43 | n = 41 | ||
| Repeated abuse | 79% | 59% | χ2(1)=3.72 | .054 |
| Duration of abuse (yrs) | M = 6.41 ± 5.26 | M = 8.93 ± 7.19 | t(50)=1.46 | .152 |
| Perpetrator | ||||
| Family member | 73% | 63% | χ2(1)=0.72 | .395 |
| Other adult | 0% | 5% | χ2(1)=1.65 | .198 |
| Partner | 15% | 0% | χ2(1)=6.66 | .010 |
| Stranger | 3% | 15% | χ2(1)=2.87 | .090 |
| Peer | 12% | 24% | χ2(1)=1.79 | .180 |
| Multiple | 26% | 30% | χ2(1)=0.72 | .788 |
Table II compares participants with physical abuse only, sexual abuse only, physical and sexual abuse, and no abuse on lifetime substance abuse, adult victimization, and HIV sexual risk. There were overall group differences on all variables except substance abuse problem and cocaine use. When comparing participants with sexual abuse only versus physical abuse only, those with sexual abuse only were significantly more likely to have a lifetime drug use disorder (68% vs. 29%); otherwise there were no significant differences between these groups. In contrast, when comparing participants with any abuse versus no abuse, those with any abuse were significantly more likely to report adult physical abuse (48% vs. 30%), adult sexual abuse (33% vs. 9%), sex trading (40% vs. 24%), sexually transmitted infection (44% vs. 17%), and 20 or more sex partners (43% vs. 24%); however, there were no differences in substance abuse variables. These findings suggest that childhood sexual abuse may be a unique predictor of drug use disorder, but any childhood abuse (sexual and/or physical abuse) is a risk factor for adult victimization and lifetime HIV risk.
Table II.
Effect of childhood abuse on lifetime substance abuse, adult victimization, and HIV sexual risk
| Planned contrasts |
|||||||
|---|---|---|---|---|---|---|---|
| Physical abuse only n = 35 | Sexual abuse only n = 22 | Physical and sexual abuse n = 49 | No abuse n = 46 | Overall differences | Physical only vs. sexual only | Any abuse vs. no abuse | |
| Substance abuse | |||||||
| Drug use disorder | 29% | 68% | 57% | 46% | χ2 = 10.59* | χ2 = 8.61** | χ2 = 0.24 |
| Alcohol use disorder | 40% | 27% | 39% | 44% | χ2 = 1.68 | χ2 = 0.96 | χ2 = 0.60 |
| Substance use problem | 71% | 82% | 74% | 70% | χ2 = 1.19 | χ2 = 0.79 | χ2 = 0.40 |
| Cocaine use | 54% | 73% | 59% | 52% | χ2 = 2.82 | χ2 = 1.94 | χ2 = 0.89 |
| Adult victimization | |||||||
| Physical | 46% | 27% | 59% | 30% | χ2 = 10.54* | χ2 = 1.94 | χ2 = 4.10* |
| Sexual | 29% | 18% | 43% | 9% | χ2 = 15.34** | χ2 = 0.79 | χ2 = 9.95** |
| Lifetime HIV risk | |||||||
| Sex trading | 26% | 46% | 47% | 17% | χ2 = 11.78** | χ2 = 2.37 | χ2 = 7.18** |
| ≥20 sex partners | 37% | 46% | 47% | 24% | χ2 = 6.08* | χ2 = 0.39 | χ2 = 5.20* |
| Sexually transmitted infections | 40% | 50% | 45% | 17% | χ2 = 10.69* | χ2 = 0.55 | χ2 = 10.09** |
p < .05,
p < .01
Model testing
We then tested the hypothetical model. All indicator loadings on the latent factors were greater than .50 (p < .001). Because race and gender were associated with both childhood and adult abuse, they were added as covariates. The model had adequate fit (χ2(37) = 50.22, p > .05; RMSEA = 0.049; CFI = 0.92; NNFI = 0.95). Inspection of modification indices suggested that controlling for the effects of race on drug abuse and HIV risk improved model fit. Figure II depicts this final structural model with path coefficients. This model had excellent fit (χ2(35) = 35.53, p > .05; RMSEA < 0.01; CFI = 1.00; NNFI = 1.00).
Figure II.
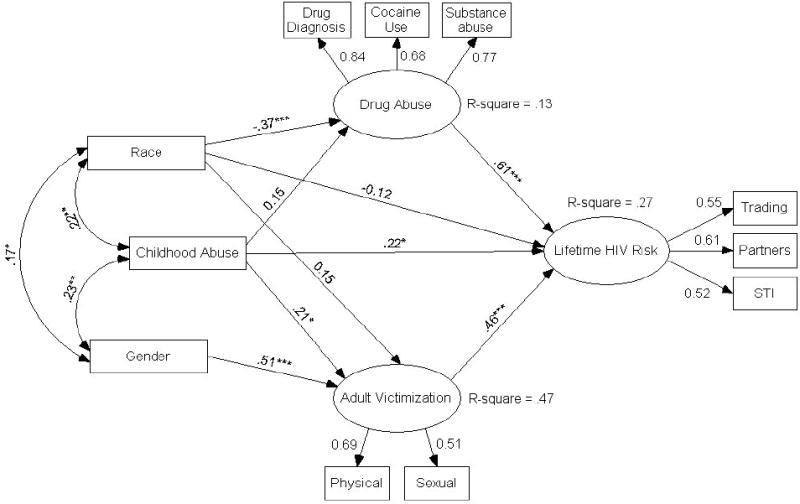
Structural equation model depicting paths and standardized estimates among childhood abuse, drug abuse, adult victimization, and HIV risk behavior (measurement error terms not shown).
χ2(35) = 35.53, p = .44; RMSEA = 0.00 (0.00 - .06); CFI = 1.00; NNFI = 1.00
*p < .05, **p < .01, ***p < .001
Table III shows the direct and indirect effects of all variables in the final model. Childhood abuse was directly (z = 2.03, p < .05) and indirectly (z = 2.28, p < .05) associated with HIV risk. Childhood abuse was directly associated with adult victimization (z = 2.04, p < .05), and adult victimization was directly associated with HIV risk (z = 2.89, p < .01). Childhood abuse was not directly associated with drug abuse (z = 1.72, p > .05), but drug abuse was directly and strongly associated with HIV risk (z = 4.44, p < .01). While the overall indirect effect of childhood abuse on HIV risk was significant, Sobel tests for mediation found that the individual indirect effects of drug abuse and adult victimization on HIV risk were not significant (t = 1.64, p = .10 and t = 1.71, p = .09, respectively), though the effects were in the expected direction.
Table III.
Direct and indirect effects of childhood abuse on drug abuse, adult victimization, and HIV sexual risk
| Childhood Abuse | Drug abuse | Adult victimization | Female gender | White race | ||||
|---|---|---|---|---|---|---|---|---|
| Direct | Indirect | Direct | Direct | Direct | Indirect | Direct | Indirect | |
| Drug abuse | .15 | -- | -- | -- | -- | -- | -.37*** | -- |
| Adult victimization | .21* | -- | -- | -- | .51*** | -- | .15 | -- |
| Lifetime HIV risk | .22* | .19* | .61*** | .46*** | -- | .24* | .12 | .15 |
p < .05,
p < .01,
p < .001
Multiple group comparisons indicated no significant difference in the models by gender (χ2(8) = 6.44, p > .05), indicating that the model did not differ significantly between men and women. There were also no differences between men and women for individual paths in the model (data not shown).
DISCUSSION
Consistent with our hypothesis, childhood abuse was directly and indirectly associated with increased HIV sexual risk. This finding is notable due to the disproportionately high rate of childhood abuse in adults with SMI. In this sample, 81% of women and 60% of men reported sexual and/or physical abuse in childhood, and 32% reported both types of abuse. Persons with SMI may be at high risk for HIV due to associated cognitive, emotional, and social impairments resulting from childhood abuse experiences. For example, poor judgment and impulsivity may impair accurate risk assessment and promote sexual involvement with multiple risky partners. Individuals with histories of childhood abuse may be at especially high risk for revictimization and sexual risk behavior. Mueser and colleagues (2002) proposed that trauma and SMI interact in complex ways, leading to poorer outcomes, including more severe psychiatric symptoms, higher risk of relapse, and revictimization. Indeed, a recent study found that adverse childhood events, including sexual and physical abuse, predicted HIV infection in adults with schizophrenia (Rosenberg et al., 2007).
Results suggest that participants who were abused in childhood were more likely to be abused in adulthood, and this in turn was associated with greater HIV risk. Childhood is a critical developmental period, and abuse perpetrated during this period may distort an individual’s construction of relational schemas (Briere, 2002; Wenninger and Ehlers, 1998), setting the stage for future victimization and HIV risk behavior (Parillo et al., 2001; Senn et al., 2006; van Dorn et al., 2005; Wyatt et al., 2002). Although the relationship between childhood abuse and HIV risk behavior was similar for male and female participants, women were more likely to report childhood abuse and adult victimization. Results also suggest potential racial differences. In this sample, white participants were more likely to report childhood abuse but less likely to abuse drugs. Prior studies examining the effects of race on these outcomes have yielded conflicting results (Buka, 2002; Kenny and McEachern, 2000), suggesting complex relationships. Further studies with larger, well-matched samples are needed to ascertain how race may moderate the effects of childhood abuse.
Contrary to our hypothesis, childhood abuse was not predictive of drug abuse. The association between childhood abuse and substance abuse may be weaker among high risk samples, particularly in the context of multiple risk factors (e.g., poverty, mental illness) (Brown et al., 2000; Kang et al., Morrill et al., 2001). Nevertheless, drug abuse was a strong predictor of lifetime HIV risk. Among substance abusers in general, drug abuse is more strongly related to HIV risk behavior than alcohol abuse (Morrill et al., 2001; Newman et al., 2004; Windle, 1997). Drug abusers may also be more likely to have high risk partners (e.g., injection drug users) and be part of a social network in which sexual risk behaviors are more normative (Latkin et al., 2003). The current findings suggest that individuals with SMI who have a history of childhood abuse and co-occurring drug abuse may be at particularly high risk for HIV.
Several limitations should be noted. First, this study was based primarily on self-report, which may be complicated by psychosis, medication side-effects, or substance abuse. However, prior research conducted among persons with SMI has established reasonable test-retest reliability and predictive validity of self-report measures of trauma exposure, substance abuse, and sexual behaviors (Goodman et al., 1999; McKinnon et al., 1993; Weiss et al., 1998). Second, due to the cross-sectional design of the study, causality could not be determined. However, childhood abuse must have predated any adult victimization and likely also predated drug abuse and HIV risk behaviors. Research using longitudinal designs is needed to adequately assess the temporal relationships between trauma symptoms, revictimization, drug abuse, and HIV risk behavior. Third, the sample size was relatively small for an SEM analysis, though within the guidelines to yield stable parameter estimates (Jaccard and Wan, 1996). However, low power may have contributed to the lack of differences between participants who experienced physical versus sexual abuse only. This supports our rationale for examining a combined variable of childhood abuse in the final model. Replication studies with larger samples are needed. Finally, use of a convenience sample raises the possibility of selection bias, though the current sample reflects the SMI population in terms of diagnoses, chronicity, and severity of functional impairments. Nevertheless, results may not generalize to adults with SMI who are not in psychiatric treatment, are less socioeconomically disadvantaged, and/or live in non-urban areas or other regions of the United States.
In sum, the results of this study suggest that childhood sexual and physical abuse may play an important role in HIV risk behavior among adults with SMI. It has been suggested that this population is at “triple jeopardy” for HIV infection due to the combination of psychiatric disabilities, substance abuse, and interpersonal trauma (Dévieux et al., 2007). Integrated treatment approaches that address interpersonal violence and substance abuse may be necessary for HIV prevention in this population. Unfortunately, among the few such interventions available, there is a lack of empirical support for efficacy in general and application to SMI populations in particular (Briere, 2003; Hansen et al., 2006; Wyatt et al., 2004). Although much more work is needed to develop effective HIV risk reduction interventions, mental health providers should be aware of the high prevalence of childhood abuse and sexual risk behaviors and should address these issues with SMI clients.
Acknowledgments
This study was supported by grants F31-MH067370 and T32-DA01536 from the National Institutes of Health.
References
- APA. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Arriola KRJ, Louden T, Doldren MA, Fortenberry RM. A meta-analysis of the relationship of child sexual abuse to HIV risk behavior among women. Child Abuse and Neglect. 2005;29:725–746. doi: 10.1016/j.chiabu.2004.10.014. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural Equations with Latent Variables. New York: Wiley; 1989. [Google Scholar]
- Briere J. Treating Adult Survivors of Severe Childhood Abuse and Neglect: Further Development of an Integrative Model. In: B L, Myers JEB, Briere J, Hendrix CT, Jenny C, Reid T, editors. The APSAC Handbook on Child Maltreatment. 2. Newbury Park, CA: Sage Publications; 2002. p. 26. [Google Scholar]
- Briere J. Integrating HIV/AIDS prevention activities into psychotherapy for sexual abuse survivors. In: Koenig LJ, Doll LS, O’Leary A, Pequegnat W, editors. From Child Sexual Abuse to Adult Sexual Risk: Trauma, Revictimization, and Intervention. Washington, DC: American Psychological Association; 2003. [Google Scholar]
- Briere J, Elliot DM. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse and Neglect. 2003;27:1205–1222. doi: 10.1016/j.chiabu.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Brown LK, Lourie KJ, Zlotnick C, Cohn J. Impact of sexual abuse on the HIV-risk-related behavior of adolescents in intensive psychiatric treatment. American Journal of Psychiatry. 2000;157:1413–1415. doi: 10.1176/appi.ajp.157.9.1413. [DOI] [PubMed] [Google Scholar]
- Buka SL. Disparities in health status and substance use: ethnicity and socioeconomic factors. Public Health Reports. 2002;117:S118–S125. [PMC free article] [PubMed] [Google Scholar]
- Chartier MJ, Walker JR, Naimark B. Childhood abuse, adult health, and health care utilization: Results from a representative community sample. American Journal of Epidemiology. 2007;165:1031–1038. doi: 10.1093/aje/kwk113. [DOI] [PubMed] [Google Scholar]
- Chesney MA, Barrett DC, Stall R. Histories of substance abuse and risk behavior: Precursors to HIV seroconversion in homosexual men. American Journal of Public Health. 1998;88:113–116. doi: 10.2105/ajph.88.1.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Classen CC, Palesh OG, Aggarwal R. Sexual revictimization: A review of the empirical literature. Trauma, Violence, and Abuse. 2005;6:103–129. doi: 10.1177/1524838005275087. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Tardiff K, Marzuk PM, Leon AC, Potera L. Childhood abuse and subsequent sexual assault among female inpatients. Journal of Traumatic Stress. 1996;9:473–482. doi: 10.1007/BF02103659. [DOI] [PubMed] [Google Scholar]
- Cohen M, Deamant C, Barkan S, Richardson J, Young M, Holman S, et al. Domestic violence and childhood sexual abuse in HIV-infected women and women at risk for HIV. American Journal of Public Health. 2000;90:560–565. doi: 10.2105/ajph.90.4.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craine LS, Henson CE, Colliver JA, MacLean DG. Prevalence of a history of sexual abuse among female psychiatric patients in a state hospital system. Hospital and Community Psychiatry. 1988;39:300–304. doi: 10.1176/ps.39.3.300. [DOI] [PubMed] [Google Scholar]
- Devieux JG, Malow RM, Lerner BG, Dyer JG, Baptista L, Lucenko B, et al. Triple jeopardy for HIV substance using severely mentally ill adults. Journal of Prevention and Intervention in the Community. 2007;33:5–18. doi: 10.1300/J005v33n01_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. American Journal of Psychiatry. 2003;160:1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Essock SM, Dowden S, Constantine NT, Katz L, Swartz MS, Meador KG, et al. Risk factors for HIV, Hepatitis B, and Hepatitis C among persons with severe mental illness. Psychiatric Services. 2003;54:836–841. doi: 10.1176/appi.ps.54.6.836. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Hotaling G, Lewis IA, Smith C. Sexual abuse in a national survey of adult men and women: Prevalence, characteristics, and risk factors. Child Abuse and Neglect. 1990;14:19–28. doi: 10.1016/0145-2134(90)90077-7. [DOI] [PubMed] [Google Scholar]
- Goodman LA, Fallot RD. HIV risk-behavior in poor urban women with serious mental illness: Association with childhood physical and sexual abuse. American Journal of Orthopsychiatry. 1998;68:73–83. doi: 10.1037/h0080272. [DOI] [PubMed] [Google Scholar]
- Goodman LA, Rosenberg SD, Mueser KT, Drake RE. Physical and sexual assault history in women with severe mental illness: Prevalence, correlates, treatment, and future research directions. Schizophrenia Bulletin. 1997;23:685–696. doi: 10.1093/schbul/23.4.685. [DOI] [PubMed] [Google Scholar]
- Goodman LA, Salyers MP, Mueser KT, Rosenberg SD, Swartz M, Essock SM, et al. Recent victimization in women and men with severe mental illness: Prevalence and correlates. Journal of Traumatic Stress. 2001;14:615–632. doi: 10.1023/A:1013026318450. [DOI] [PubMed] [Google Scholar]
- Goodman LA, Thompson KM, Weinfurt K, Corl S, Acker P, Mueser KT, et al. Reliability of reports of violent victimization and PTSD among men and women with SMI. Journal of Traumatic Stress. 1999;12:587–599. doi: 10.1023/A:1024708916143. [DOI] [PubMed] [Google Scholar]
- Green BL. Trauma History Questionnaire. In: Stamm BH, editor. Measurement of Stress, Trauma, and Adaptation. Lutherville, MD: Sidran; 1996. pp. 366–368. [Google Scholar]
- Hansen NB, Sikkema KJ, Tarakeshwar N, Kochman A, Briere J, Fox AM, et al. Group Intervention For Sexually Abused, HIV Positive Adults: Resiliency, Process And Outcome. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies; Hollywood, CA. 2006. Nov, [Google Scholar]
- Hu L, Bentler PM. Cutoff criterion for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jaccard J, Wan CK. LISREL Approaches to Interaction Effects in Multiple Regression. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- Joreskog KG. Structural Equation Modeling with Ordinal Variables using LISREL. 2004 Retrieved 12/06/2006, 2006, from http://www.ssicentral.com/lisrel/techdocs/ordinal.pdf.
- Kang SY, Deren S, Goldstein MF. Relationships between childhood abuse and neglect experience and HIV risk behaviors among methadone treatment drop-outs. Child Abuse and Neglect. 2002;26:1275–1289. doi: 10.1016/s0145-2134(02)00412-x. [DOI] [PubMed] [Google Scholar]
- Kenny MC, McEachern AG. Racial, ethnic, and cultural factors of childhood sexual abuse: A selected review of the literature. Clinical Psychology Review. 2000;20:905–922. doi: 10.1016/s0272-7358(99)00022-7. [DOI] [PubMed] [Google Scholar]
- Kimerling R, Alvarez J, Pavao J, Kaminski A, Baumrind N. Epidemiology and consequences of women’s revictimization. Women’s Health Issues. 2007;17:101–106. doi: 10.1016/j.whi.2006.12.002. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Forman V, Knowlton A, Sherman S. Norms, social norms, and HIV-related risk behaviors among urban disadvantaged drug users. Social Science and Medicine. 2003;56:465–476. doi: 10.1016/s0277-9536(02)00047-3. [DOI] [PubMed] [Google Scholar]
- MacMillian HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, et al. Childhood abuse and lifetime psychopathology in a community sample. American Journal of Psychiatry. 2001;158:1878–1883. doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- Malow RM, Devieux J, Lucenko BA. History of childhood sexual abuse as a risk factor for HIV risk behavior. Journal of Trauma Practice. 2006;5:13–32. [Google Scholar]
- Malow RM, Devieux JG, Martinez L, Peipman F, Lucenko BA, Kalichman SC. History of traumatic abuse and HIV risk behaviors in severely mentally ill substance abusing adults. Journal of Family Violence in press. [Google Scholar]
- McKinnon K, Cournos F, Meyer-Bahlburg HF, Guido JR, Caraballo LR, Margoshes ES, et al. Reliability of sexual risk behavior interviews with psychiatric patients. American Journal of Psychiatry. 1993;150:972–974. doi: 10.1176/ajp.150.6.972. [DOI] [PubMed] [Google Scholar]
- Meade CS. Sexual risk behavior among persons dually diagnosed with severe mental illness and substance use disorder. Journal of Substance Abuse Treatment. 2006;30:147–157. doi: 10.1016/j.jsat.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Meade CS, Sikkema KJ. HIV risk behavior among persons with severe mental illness: A systematic review. Clinical Psychology Review. 2005a;25:433–457. doi: 10.1016/j.cpr.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Meade CS, Sikkema KJ. Voluntary HIV testing among adults with severe mental illness: frequency and associated factors. AIDS and Behavior. 2005b;9:465–473. doi: 10.1007/s10461-005-9033-y. [DOI] [PubMed] [Google Scholar]
- Meade CS, Sikkema KJ. Psychiatric and psychosocial correlates of sexual risk behavior among adults with severe mental illness. Community Mental Health Journal. 2007;43:153–169. doi: 10.1007/s10597-006-9071-6. [DOI] [PubMed] [Google Scholar]
- Miller M. A model to explain the relationship between sexual abuse and HIV risk among women. AIDS Care. 1999;11:3–20. doi: 10.1080/09540129948162. [DOI] [PubMed] [Google Scholar]
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: Results from the National Comorbidity Survey. American Journal of Public Health. 2001;91:753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrill AC, Kasten L, Urato M, Larson MJ. Abuse, addiction, and depression as pathways to sexual risk in women and men with a history of substance abuse. Journal of Substance Abuse. 2001;13:169–184. doi: 10.1016/s0899-3289(01)00065-7. [DOI] [PubMed] [Google Scholar]
- Muenzenmaier K, Meyer I, Struening E, Ferber J. Childhood abuse and neglect among women outpatients with chronic mental illness. Hospital and Community Psychiatry. 1993;44:666–670. doi: 10.1176/ps.44.7.666. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Goodman LA, Trumbetta SL, Rosenberg SD, Osher FC, Vidaver R, et al. Trauma and posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology. 1998;66:493–499. doi: 10.1037//0022-006x.66.3.493. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Salyers MP, Rosenberg SD, Ford JD, Fox L, Carty P. Psychometric evaluation of trauma and posttraumatic stress disorder assessments in persons with severe mental illness. Psychological Assessments. 2001;13:110–117. doi: 10.1037//1040-3590.13.1.110. [DOI] [PubMed] [Google Scholar]
- Newman PA, Rhodes F, Weiss RE. Correlates of sex trading among drug-using men who have sex with men. American Journal of Public Health. 2004;94:1998–2003. doi: 10.2105/ajph.94.11.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parillo KM, Freeman RC, Collier K, Young P. Associations between early sexual abuse and adult HIV-risky sexual behaviors among community-recruited women. Child Abuse and Neglect. 2001;25:335–346. doi: 10.1016/s0145-2134(00)00253-2. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavioral Research Methods, Instruments, and Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiological Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Rosenberg SD, Goodman LA, Osher FC, Swartz MS, Essock SM, Butterfield MI, et al. Prevalence of HIV, Hepatitis B, and Hepatitis C in people with severe mental illness. American Journal of Public Health. 2001;91:31–37. doi: 10.2105/ajph.91.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg SD, Lu W, Mueser KT, Jankowski MK, Cournos F. Correlates of adverse childhood events among adults with schizophrenia spectrum disorders. Psychiatric Services. 2007;58:245–253. doi: 10.1176/ps.2007.58.2.245. [DOI] [PubMed] [Google Scholar]
- Rosenberg SD, Swanson JW, Wolford GI, Swartz MS, Essock SM, Butterfield M, et al. The Five-Site Health and Risk Study of blood-borne infections among persons with severe mental illness. Psychiatric Services. 2003;54:827–835. doi: 10.1176/appi.ps.54.6.827. [DOI] [PubMed] [Google Scholar]
- Rosnow RL, Rosenthal R. Contrasts and correlations in theory assessment. Journal of Pediatric Psychology. 2002;27:59–66. doi: 10.1093/jpepsy/27.1.59. [DOI] [PubMed] [Google Scholar]
- Sachs-Ericsson N, Kendall-Tackett K, Hernandez A. Childhood abuse, chronic pain, and depression in the National Comorbidity Study. Child Abuse and Neglect. 2007;31:531–547. doi: 10.1016/j.chiabu.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA, Coury-Doniger P, Urban MA. Childhood sexual abuse and sexual risk behavior among men and women attending sexually transmitted disease clinic. Journal of Consulting and Clinical Psychology. 2006;74:720–731. doi: 10.1037/0022-006X.74.4.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson TL, Miller WR. Concomitance between childhood sexual and physical abuse and substance use problems: A review. Clinical Psychology Review. 2002;22:27–77. doi: 10.1016/s0272-7358(00)00088-x. [DOI] [PubMed] [Google Scholar]
- Sohler N, Colson PW, Meyer-Bahlburg HF, Susser E. Reliability of self-reports about sexual risk behavior for HIV among homeless men with severe mental illness. Psychiatric Services. 2000;51:814–816. doi: 10.1176/appi.ps.51.6.814. [DOI] [PubMed] [Google Scholar]
- UNAIDS. Report on the Global AIDS Epidemic. Geneva: UNAIDS; 2006. [Google Scholar]
- Vaddiparti K, Bogetto J, Cullahan C, Abdallah AB, Spitznagel EL, Cottler LB. The effects of childhood trauma on sex trading in substance using women. Archives of Sexual Behavior. 2006;35:451–459. doi: 10.1007/s10508-006-9044-4. [DOI] [PubMed] [Google Scholar]
- van Dorn RA, Mustillo S, Elbogen EB, Dorsey S, Swanson JW, Swartz MS. The effects of early sexual abuse on adult risky sexual behaviors among persons with severe mental illness. Child Abuse and Neglect. 2005;29:1265–1279. doi: 10.1016/j.chiabu.2005.06.004. [DOI] [PubMed] [Google Scholar]
- Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annual Review of Sex Research. 2000;11:125–157. [PMC free article] [PubMed] [Google Scholar]
- Weiss RD, Najavits LM, Greenfield SF, Soto JA, Shaw SR, Wyner D. Validity of substance use self-reports in dually diagnosed outpatients. American Journal of Psychiatry. 1998;155:127–128. doi: 10.1176/ajp.155.1.127. [DOI] [PubMed] [Google Scholar]
- Wenninger K, Ehlers A. Dysfunctional cognitions and adult psychological functioning in child sexual abuse survivors. Journal of Traumatic Stress. 1998;11:231–300. doi: 10.1023/A:1024451103931. [DOI] [PubMed] [Google Scholar]
- Windle M. The trading of sex for money or drugs, sexually transmitted diseases (STDs), and HIV-related risk behaviors among multisubstance using alcoholic inpatients. Drug and Alcohol Dependence. 1997;49:33–38. doi: 10.1016/s0376-8716(97)00136-1. [DOI] [PubMed] [Google Scholar]
- Wyatt GE, Longshore D, Chin D, Carmona JV, Loeb T, Myers HF, et al. The efficacy of an integrated risk reduction intervention for HIV-positive women with child sexual abuse histories. AIDS and Behavior. 2004;8:453–462. doi: 10.1007/s10461-004-7329-y. [DOI] [PubMed] [Google Scholar]
- Wyatt GE, Myers HF, Williams JK, Kitchen CR, Loeb T, Carmone JV, et al. Does a history of trauma contribute to HIV risk for women of color? Implications for prevention and policy. American Journal of Public Health. 2002;92:660–665. doi: 10.2105/ajph.92.4.660. [DOI] [PMC free article] [PubMed] [Google Scholar]


