Abstract
The immune system is subject to destruction and dysfunction as a result of attacks by pathogenic and environmental agents. In addition, many clinical situations exist in which it is desirable to stimulate or suppress the immune system. The present study evaluated the screening efficacy of flow cytometric lymphocyte subset typing in peripheral blood mononuclear cells from healthy individuals (HI) and from patients with non-Hodgkin lymphoma (NHL) treated with different concentrations of FR-91, a standardized lysate of microbial cells belonging to the Bacillus genus, and in vitro cytokine production. Increased expression of subset markers (CD3, CD4, CD8) in NHL and CD3 in HI suggests an immunomodulating effect of FR-91. In addition the results of cytokine production also demonstrated a clear effect of FR-91 on both populations. A significant increase of IL-6, IL-12, IFN-γ and TNF-α was observed in the HI group after treatment with FR-91. In a similar manner an increase of IL-2, IL-6, IL-12, IFN-γ and TNF-α was also observed in the NHL group. In conclusion FR-91 seems to affect lymphocyte subpopulations, in vitro cytokine production, as well as mitogen-induced lymphocyte activation in a dose-dependent manner in both healthy individuals and NHL patients.
1. Introduction
The immune system is a highly complex, intricately regulated group of cells whose integrated function is crucial to health. Cells belonging to the immune system usually interact in a cell-cell manner and may also respond to intercellular signals including hormones, cytokines, short peptides, and other small costimulator molecules as histamine, kinins, leukotrienes, prostaglandins, and serotonin that are capable of turning the immune system on or off and in the process profoundly affecting human health. The immune system can be modified by diet, pharmacological compounds, environmental pollutants, and naturally occurring food constituents, such as vitamins, antioxidant, and free radical scavengers. Over 4000 structurally unique chemical compounds have been identified in plant sources and they are prominent components of citrus fruits and other food sources and are consumed regularly with the human diet [1–3]. These low molecular weight substances, found in all vascular plants, are phenylbenzo-pyrones with an assortment of structures based on a common three-ring nucleus and they are usually subdivided according to their substituents into flavanols, anthocyanidins, and flavones [4]. Some effects of natural occurring compounds on the function of T lymphocytes, B lymphocytes, macrophages, natural killer cells (NK), basophils, neutrophils, eosinophils, and platelets have been described [5–7], and it seems evident that the majority of them display, to a variable extent, a remarkable array of biochemical and pharmacological actions which suggest that certain members of this group of compounds significantly affect the function of the immune system and inflammatory cells.
In the last three decades the use of nonspecific immunomodulators has been suggested for clinical use in all those situations characterized by enhanced susceptibility to infections in the nonimmunocompromised host, and a good cost/benefit ratio seems to be offered by immunobiotherapeutics such as bacterial extracts (BEs), which are the strongest natural exogenous immunomodulating agents [8–10]. A number of immunostimulating agents of bacterial origin are available in the European market for the prevention and treatment of recurrent infections and food allergies [11, 12]. Since the early 1970s, oral lyophilized (active) extracts of bacteria species, which are frequently responsible for lower respiratory tract infections in patients with chronic obstructive pulmonary disease (COPD), have been used. These remedies are thought to enhance specific and nonspecific immune responses through humoral and cellular immunomodulating activities [13–16]. One large randomized placebo-controlled trial performed in 1997 (the Prevention of Acute Respiratory Infection by an Immunostimulant Study) found that treatment with oral purified bacterial extracts reduced the severity of exacerbations and the rate of hospitalizations in COPD patients [17].
In in vitro conditions, BEs are able to stimulate functional activities of macrophages and lymphocytes, to activate NK cells and the release of cytokines from human peripheral blood mononuclear cells [18, 19]. In animals treated in vivo with BEs, bacterial killing is enhanced and immunoglobulin production and secretion can be augmented in definite conditions [20–22].
The aim of the present study was to evaluate the effects of FR-91, a standardized lysate of microbial cells belonging to the Bacillus genus, on cells of the immune system from healthy individuals and from patients with non-Hodgkin lymphoma to provide a possible rational for the use of FR-91as an immunostimulant agent in clinical trials for the prevention of associated recurrent infections.
2. Subjects and Methods
2.1. Materials
Fluorescein isothiocyanate-labeled mouse antihuman CD3, CDCD25 and CD69, and R-phycoerythrin-labeled mouse antihuman CD4, CD8, and HLA-DR were purchased from Becton Dickinson Biosciences (Erembodegem, Belgium). HEPES-buffered RPMI 1640 medium was obtained from PAA (Pasching, Austria). Glutamine and antibiotics (penicillin and streptomycin) were purchased from Sigma-Aldrich (Madrid, Spain). Kits for measurements of cytokines in culture supernatants were purchased from LINCO Research Inc. (St. Charles, USA). All other reagents, including Con A and LPS were purchased from Sigma-Aldrich (Madrid, Spain).
2.2. Subjects and Study Design
The study was conducted at Euroespes Biotechnology Centre in La Coruña (Spain). Fifteen healthy subjects aged 25–52 years were selected after confirming that they were healthy; had a body mass index (BMI: in kg/m2) >20 and <27; had no diagnosis of cardiovascular disease, diabetes, liver or endocrine dysfunction, or chronic inflammatory disease; were not taking any medication; were not vegetarians or vegans; were not heavy smokers (>10 cigarettes/d); were not heavy consumers of alcohol (<10 units/wk); were not consuming any supplements (e.g., vitamins, fish oils). Subjects fitting these criteria were then screened for fasting plasma concentrations of cholesterol (3.0–5.2 mmol/L), triacylglycerol (0.45–1.81 mmol/L), and glucose (3.9–5.8 mmol/L) and for markers of liver dysfunction (total bilirubin, alanine aminotransferase, and aspartate aminotransferase). All volunteers gave informed consent and completed a health and lifestyle questionnaire before entering the study. Ten patients aged 65–77 diagnosed with non-Hodgkin lymphoma at stage 1 (according to the Ann Arbor Staging System, NHL is limited to one lymph node group, above or below the diaphragm, or NHL is in an organ or site other than the lymph nodes, but has not spread to other organs or lymph nodes) gave informed consent and were included in the study.
2.3. Analysis of PMBC Subsets
For the determination of PBMC subsets, whole blood (100 μL) was incubated with various combinations of fluorescently labelled monoclonal antibodies (10 μL of each antibody) for 30 minutes at 4°C. The monoclonal antibody combinations used were anti-CD3/anti-HLA-DR (to distinguish T lymphocytes as CD3+, B lymphocytes as CD3−/HLA-DR+, and activated T lymphocytes as CD3+/HLA-DR+), anti-CD4/anti-CD8 (to distinguish T helper lymphocytes as CD4+ and cytotoxic T lymphocytes as CD8+), and anti-CD25/antiCD69 (to distinguish early activated lymphocytes as CD69+ and activated T lymphocytes that express IL-2 receptor as CD25+ cells). After incubation, erythrocytes were lysed with the use of 2 mL lysing solution (3.75 mL formaldehyde, 4.5 mL diethylene glycol, and 1.75 mL of 0.2 mol/L Tris made up to 1 L with distilled water) and the leukocytes were washed and then fixed with 0.2 mL fixing solution (phosphate-buffered solution containing 2 mL/100 mL formaldehyde). Fixed leukocytes were analyzed with a FACScan flow cytometer (Becton Dickinson). Fluorescence data were collected on 1 × 104 cells and analyzed with Cellquest software. All flow cytometry experiments were validated by internal controls.
2.4. Measurement of Mitogen-Induced Activation in Whole Blood
Mitogen and FR-91 induced lymphocyte activation was determined by measuring the expression of CD69, a cell surface marker whose expression is upregulated in response to stimulation. Blood was diluted 1 : 1 with culture complete RPMI 1640 medium and then cultured for 24 hours with Con A (positive control) at final concentrations of 0, 6.25, 12.5, or 25 μg/mL and with FR-91 at final concentrations of 10 and 25 μg/mL. For the determination of CD69 expression on lymphocytes, 200 μL of samples were incubated with fluorescently labelled monoclonal antibody for 30 minutes at 4°C. The monoclonal antibodies used were anti-CD69 with anti-CD4. At the end of incubation, the erythrocytes were lysed and the leukocytes were washed, centrifuged, and fixed. The cell preparations were then analyzed by flow cytometry in a Becton Dickinson FACScan flow cytometer. Fluorescence data were collected on 2 × 104 cells and analyzed with Cellquest software. The proportions of all activated T lymphocytes expressing CD69 on their surface were determined.
2.5. Preparation of PBMCs
Blood samples were collected into heparin-treated evacuated tubes between 08:00 and 10:00 after the subjects fasted for around 10 hours. The blood was layered onto Histopaque (density: 1.077 g/L; ratio of blood to Histopaque: 1 : 1), and centrifuged for 15 minutes at 800 × g at 20°C. PBMCs were collected from the interface and washed once with RPMI culture medium containing 0.75 mmol/L glutamine and antibiotics (penicillin and streptomycin), and 10% fetal bovine serum (FBS). After resuspension in 4 mL culture medium, the cells were layered onto 4 mL Histopaque and then centrifuged once more (15 minutes, 800 × g, 20°C) to achieve a lower degree of erythrocyte contamination, washed with culture medium, and finally resuspended and counted with a Coulter ZI Cell Counter (Beckman Coulter Ltd, Luton, UK).
2.6. Measurement of the Production of Cytokines by PBMC Cultures
PBMCs (2 × 106) were cultured for 48 hours in culture medium, supplemented with 50 μL autologous plasma, and either unstimulated or stimulated with 12.5 μg/mL Con A or 5 μg/mL LPS and with three different concentrations of FR-91 (10 and 25 μg/mL). The final culture volume was 2 mL. At the end of the incubation, the plates were centrifuged (800 × g, 10 minutes, room temperature) and the culture supernatants were collected and frozen in aliquots. The concentrations of cytokines were measured by flow cytometry with the use of the multiplex bead array assays (Luminex system, a combination of three core xMAP technologies). Tumour necrosis factor α (TNF-α), interferon γ (IFN-γ), interleukin (IL) 1-β, IL-2, IL-6, IL-8, IL-10 p70, and IL-12 were measured in the supernatant fractions of cells stimulated with ConA, LPS (positive controls) and FR-91. The limits of detection for the LPS assays, supplied by the manufacturer of the kits, were 3.7 pg/mL (TNF-α), 3.3 pg/mL (IL1-β), 6.8 pg/mL (IFN-γ), 2.8 pg/mL (IL-2), 3.1 pg/mL (IL-6), 3.3 pg/ml (IL-8), 4.2 pg/mL (IL-10 p70), and 3.5 pg/mL (IL-12); those for the Con A assays were 3.5 pg/mL (TNF-α), 3.1 pg/mL (IL1-β), 5.8 pg/mL (IFN-γ), 3.0 pg/mL (IL-2), 3.4 pg/mL (IL-6), 3.0 pg/ml (IL-8), 3.2 pg/mL (IL-10 p70), and 2.5 pg/mL (IL-12). Fluorescence data were collected and analyzed with the use of the IS 2.3 software. The interassay and intraassay CVs were <10% for all cytokine bead arrays.
2.7. Statistical Analysis
All statistical tests were performed with the use of SPSS (version 11.0; SPSS Inc, Chicago, Ill, USA) and a P-value <.05 indicated statistical significance. Data were analyzed by using a two-factor repeated-measures analysis of variance (ANOVA) followed by a post-hoc analysis where relevant (one-factor repeated-measures ANOVA, followed by Tukey's tests for a significant effect of dose and paired t tests for a significant effect of FR-91 treatment).
3. Results
3.1. Effects of FR-91 on PBMC Subsets
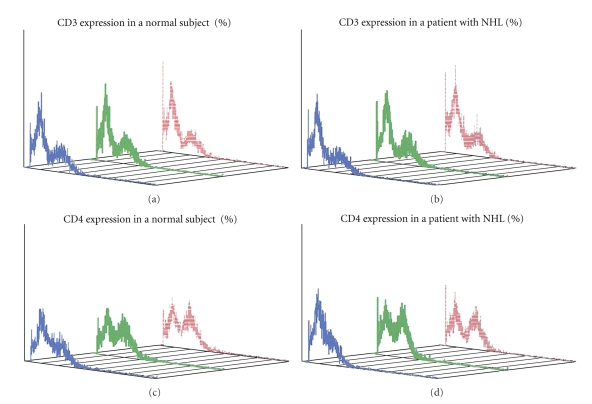
In the healthy group, there were no consistent effects of FR-91 on the percentage of CD4+ lymphocytes, CD25+ T cells, CD69+ T cells, and HLA-DR+ lymphocytes, although there were significant effects of FR-91 at both 10 and 25 μg/mL concentrations on CD3+ and CD8+ T lymphocytes. The percentage of CD3+ T lymphocytes treated with 10 μg/mL of FR-91 was 73.48, the percentage of CD3+ T lymphocytes treated with 25 μg/mL was 75.26, while the control group showed a mean of 65.59%. The significant difference in CD3+ cells in the group treated with 10 μg/mL of FR-91 was of P = .024, and P = .022 in the group treated with 25 μg/mL of FR-91 with respect to the control. Significant decreases were observed with respect to CD8+ T lymphocytes (FR-91 10 μg/mL: 25.04%, P = .029 vs/controls, 29.46%; FR-91 25 μg/mL: 25.72%, P = .05 vs/controls, 29.46%). Table 1 shows the mean, SD, CV, and P-value obtained in the healthy group. The expression of CD3 and CD4 in the NHL group was highly significant with respect to controls. Lymphocytes treated with 10 μg/mL of FR-91 showed a CD3 mean of 71.09%, while lymphocytes treated with 25 μg/mL of FR-91 showed a CD3 mean of 69.45%. Both mean values were significant different with respect to controls (58.73%), P < .001 and P < .002, respectively. CD4+ lymphocytes also showed a significant increase with respect to controls. Lymphocytes treated with 10 μg/mL of FR-91 showed a CD4 mean of 48.39%, while lymphocytes treated with 25 μg/mL of FR-91 showed a CD4 mean of 47.41%. Both mean values were significantly different with respect to controls (36.28%), P < .001 and P < .002, respectively. In addition to CD3 and CD4, a significant reduction in expression of HLA-DR and CD69 was observed. Lymphocytes treated with 10 μg/mL of FR-91 showed an HLA-DR mean of 5.66%, while lymphocytes treated with 25 μg/mL of FR-91 showed a HLA-DR mean of 6.36%. Both mean values were significantly different with respect to controls (8.5%), P < .001 and P < .002, respectively. The mean percentage of CD69 expression was 12.83 (group treated with 10 μg/mL of FR-91), and 13.33 (group treated with 25 μg/mL of FR-91) and both mean values were significantly different with respect to controls (22.37%), P < .001 and P < .008, respectively. Data of lymphocyte subset percentages in the NHL group are shown in Table 2. Flow cytometry results of CD3 and CD4 expressions in a normal subject (a) and (c) and in a patient with NHL (b) and (d) are shown in Figure 1.
Table 1.
Effect of FR-91 on peripheral blood mononuclear cell (PBMC) subsets from healthy subjects.
| CD3/control | CD3/FR-91 10 μg/mL | CD3/FR-91 25 μg/mL | |
| X* | 65.59 | 73.48 | 75.26 |
| SD** | 10.92 | 5.87 | 8.43 |
| CV*** | 0.16 | 0.08 | 0.11 |
| P**** | .024 | .022 | |
| HLA-DR/control | HLA-DR/FR-91 10 μg/mL | HLA-DR/FR-91 25 μg/mL | |
| X | 4.48 | 3.26 | 3.65 |
| SD | 3.54 | 1.49 | 1.66 |
| CV | 0.79 | 0.45 | 0.45 |
| P | .27 | .84 | |
| CD4/control | CD4/FR-91 10 μg/mL | CD4/FR-91 25 μg/mL | |
| X | 43.81 | 47.24 | 46.21 |
| SD | 11.8 | 7.9 | 9.6 |
| CV | 0.27 | 0.17 | 0.2 |
| P | .15 | .35 | |
| CD25/control | CD25/FR-91 10 μg/mL | CD25/FR-91 25 μg/mL | |
| X | 5.5 | 5.47 | 6 |
| SD | 3.7 | 3.47 | 3.83 |
| CV | 0.67 | 0.63 | 0.64 |
| P | .9 | .42 | |
| CD8/control | CD8/FR-91 10 μg/mL | CD8/FR-91 25 μg/mL | |
| X | 29.46 | 25.04 | 25.72 |
| SD | 8.91 | 4.41 | 5.37 |
| CV | 0.3 | 0.17 | 0.21 |
| P | .029 | .05 | |
| CD69/control | CD69/FR-91 10 μg/mL | CD69/FR-91 25 μg/mL | |
| X | 13.76 | 10.04 | 11.1 |
| SD | 10.87 | 4.57 | 5.67 |
| CV | 0.79 | 0.46 | 0.51 |
| P | .14 | .26 | |
n = 15; *mean; **standard deviation; ***coefficient of variation; **** <.05: significant values.
Table 2.
Effect of FR-91 on peripheral blood mononuclear cell (PBMC) subsets from NHL patients.
| CD3/control | CD3/FR-91 10 μg/mL | CD3/FR-91 25 μg/mL | |
| X* | 57.73 | 71.09 | 69.45 |
| SD** | 3.97 | 4.67 | 6.72 |
| CV*** | 0.06 | 0.06 | 0.09 |
| P**** | .001 | .002 | |
| HLA-DR/control | HLA-DR/FR-91 10 μg/mL | HLA-DR/FR-91 25 μg/mL | |
| X | 8.5 | 5.66 | 6.36 |
| SD | 2.08 | 2.18 | 4.16 |
| CV | 0.24 | 0.38 | 0.65 |
| P | .002 | .109 | |
| CD4/control | CD4/FR-91 10 μg/mL | CD4/FR-91 25 μg/mL | |
| X | 36.28 | 48.39 | 47.41 |
| SD | 8.6 | 6.27 | 4.95 |
| CV | 0.23 | 0.13 | 0.1 |
| P | .001 | .002 | |
| CD25/control | CD25/FR-91 10 μg/mL | CD25/FR-91 25 μg/mL | |
| X | 6.12 | 5.62 | 5.47 |
| SD | 4.34 | 3.84 | 2.51 |
| CV | 0.7 | 0.68 | 0.46 |
| P | .32 | .41 | |
| CD8/control | CD8/FR-91 10 μg/mL | CD8/FR-91 25 μg/mL | |
| X | 26.96 | 23.47 | 23.96 |
| SD | 7.52 | 4.22 | 3.58 |
| CV | 0.27 | 0.17 | 0.15 |
| P | .17 | .11 | |
| CD69/control | CD69/FR-91 10 μg/mL | CD69/FR-91 25 μg/mL | |
| X | 22.37 | 12.83 | 13.33 |
| SD | 9.63 | 4.06 | 4.31 |
| CV | 0.43 | 0.31 | 0.32 |
| P | .01 | .008 | |
n = 15; *mean; **standard deviation; ***coefficient of variation; **** <.05: significant values.
Figure 1.
Flow cytometric analysis of CD3 and CD4 expressions in a normal individual and in a patient with NHL. Blue histograms represent untreated lymphocytes, green histograms represent lymphocytes treated with 10 μg/mL of FR-91, and red histograms represent lymphocytes treated with 25 μg/mL of FR-91. Flow cytometric analysis in (a) shows a reduction in CD3 antigen expression after exposure to 25 μg/mL of FR-91, while an increase in both green and red histograms can be observed in the NHL patients (b). A similar pattern of CD4 expression can be observed both in the normal patient as well as in the NHL patient, being the expression of CD4 higher after treatment with 10 μg/mL of FR-91 (d).
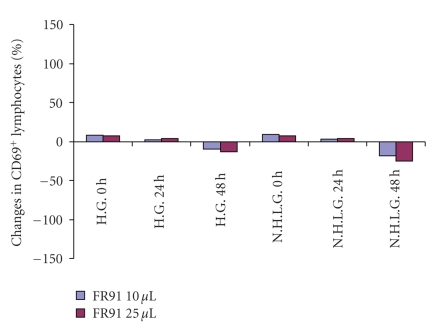
3.2. Effects of FR-91 on Mitogen-Induced T Lymphocyte Activation
Mitogen-induced activation of lymphocytes was assessed by the expression of the early activation marker CD69 on helper T lymphocytes (CD4+/CD69+). Expression of CD69 correlates strongly with lymphocyte proliferation, as assessed by the VisionBlue Quick cell proliferation assay kit, which utilizes the redox dye reasuzirin which is not fluorescent, but upon reduction by viable metabolically active cells, the dye become highly fluorescent and the intensity of fluorescence can be easily measured by an ELISA reader (data not shown). There were significant effects of Con A concentration and FR-91 concentration on CD69 expression in both healthy and NHL groups. The percentage change from baseline CD69 expression by T lymphocytes in response to FR-91, after stimulation of lymphocytes with 12.5 μg/mL Con A, is shown in Figure 2. There was a significant effect of FR-91 concentration on the change from initial CD69 expression (P < .005) and the reduction on CD69 expression was more evident in the NHL group.
Figure 2.
Mean changes in lymphocytes expressing CD69 from the healthy and NHL groups. Lymphocytes were stimulated with 10 and 25 μL of FR-91, and results were analyzed by flow cytometry. Results are expressed as percentage of change with respect to time 0.
3.3. Effects of FR-91 on Cytokine Production by PBMCs
The effects of both concentrations of FR-91 on the production of cytokines are shown in Tables 3 and 4. In the healthy group (Table 3) there were significant effects of FR-91 on the production of IL-6 (FR-91 10 microliters: 6.5 ± 2.46, P < .05; FR-91 25 microliters 9.28 ± 4.08, P < .001; control group: 4.14 ± 1.58), IL-12 (FR-91 10 microliters: 6.73 ± 2.55, P < .05; FR-91 25 microliters 10.5 ± 4.41, P < .005; control group: 3.88 ± 0.55), IFN-γ (FR-91 10 microliters: 8.48 ± 4.09, P < .001; FR-91 25 microliters 15.5 ± 7.76, P < .001; control group: 4.18 ± 0.89), and TNF-α (FR-91 10 microliters: 7.72 ± 2.43, P < .001; FR-91 25 microliters 12.5 ± 4.17, P < .001; control group: 4.08 ± 0.86). No differences between treated and untreated groups on IL-1β, IL-2, IL-8, and IL-10 production were observed. In the group of NHL patients a significant increase in cytokine production was also observed: IL-2 (FR-91 10 microliters: 7.19 ± 2.58, P < .005; FR-91 25 microliters 13.36 ± 5.98, P < .005; control group: 4.67 ± 0.95), IL-6 (FR-91 10 microliters: 6.89 ± 2.26, P < .005; FR-91 25 microliters 14.13 ± 8.04, P < .005; control group: 4.2 ± 0.96), IL-12 (FR-91 10 microliters: 5.26 ± 2.02, P < .05; FR-91 25 microliters 16 ± 7.36, P < .005; control group: 4.68 ± 0.82), IFN-γ (FR-91 10 microliters: 5.26 ± 2.02, P < .05; FR-91 25 microliters 11.84 ± 6.12, P < .005; control group: 3.86 ± 0.9), and TNF-α (FR-91 10 microliters: 15.4 ± 8.4, P < .005; FR-91 25 microliters 23.38 ± 7.83, P < .005; control group: 4.86 ± 1.69).
Table 3.
Effect of FR-91 on production of cytokines by peripheral blood mononuclear cells from healthy subjects.
| IL-1β control | IL-1β/FR-91 10 micro | IL-1β/FR-91 25 micro | |
| X | 2.18 ± 0.38 | 2.17 ± 0.34 | 2.33 ± 0.3 |
| IL-2 control | IL-2/FR-91 10 micro | IL-2/FR-91 25 micro | |
| X | 3.94 ± 0.81 | 5.85 ± 1.4 | 9.52 ± 5.66 |
| IL-6 control | IL-6/FR-91 10 micro | IL-6/FR-91 25 micro | |
| X | 4.14 ± 1.58 | 6.5 ± 2.46 | 9.28 ± 4.08* |
| IL-8 control | IL-8/FR-91 10 micro | IL-8/FR-91 25 micro | |
| X | 2.24 ± 0.36 | 2.22 ± 0.38 | 2.3 ± 0.37 |
| IL-10 control | IL-10/FR-91 10 micro | IL-10/FR-91 25 micro | |
| X | 2.3 ± 0.3 | 2.38 ± 0.34 | 2.18 ± 0.4 |
| IL-12 control | IL-12/FR-91 10 micro | IL-12/FR-91 25 micro | |
| X | 3.88 ± 0.55 | 6.73 ± 2.55** | 10.5 ± 4.41** |
| IFN-γ control | IFN-γ/FR-91 10 micro | IFN-γ/FR-91 25 micro | |
| X | 4.18 ± 0.89 | 8.48 ± 4.09* | 15.5 ± 7.76* |
| TNF-α control | TNF-α/FR-91 10 micro | TNF-α/FR-91 25 micro | |
| X | 4.08 ± 0.86 | 7.72 ± 2.43* | 12.5 ± 4.17* |
X: mean ± SD; n = 15; *P < .001; **P < .05.
Table 4.
Effect of FR-91 on production of cytokines by peripheral blood mononuclear cells from NHL patients.
| IL-1β control | IL-1β/FR-91 10 micro | IL-1β/FR-91 25 micro | |
| X | 2.52 ± 0.2 | 2.24 ± 0.45 | 2.21 ± 0.43 |
| IL-2 control | IL-2/FR-91 10 micro | IL-2/FR-91 25 micro | |
| X | 4.67 ± 0.95 | 7.19 ± 2.58* | 13.36 ± 5.98* |
| IL-6 control | IL-6/FR-91 10 micro | IL-6/FR-91 25 micro | |
| X | 4.2 ± 0.96 | 6.89 ± 2.26* | 14.13 ± 8.04* |
| IL-8 control | IL-8/FR-91 10 micro | IL-8/FR-91 25 micro | |
| X | 2.16 ± 0.34 | 2.42 ± 0.24 | 2.21 ± 0.41 |
| IL-10 control | IL-10/FR-91 10 micro | IL-10/FR-91 25 micro | |
| X | 2.18 ± 0.46 | 2.14 ± 0.48 | 2.14 ± 0.46 |
| IL-12 control | IL-12/FR-91 10 micro | IL-12/FR-91 25 micro | |
| X | 4.68 ± 0.82 | 7.61 ± 2.5* | 16 ± 7.36* |
| IFN-γ control | IFN-γ/FR-91 10 micro | IFN-γ/FR-91 25 micro | |
| X | 3.86 ± 0.9 | 5.26 ± 2.02** | 11.84 ± 6.12* |
| TNF-α control | TNF-α/FR-91 10 micro | TNF-α/FR-91 25 micro | |
| X | 4.86 ± 1.69 | 15.4 ± 8.4* | 23.38 ± 7.83* |
X: mean ± SD; n = 10; *P < .005; **P < .05.
4. Discussion
The acquired immune system is a sophisticated defense machinery. It can recognize and respond to foreign invaders and can learn from the experience so that the body responds faster and more effectively when exposed to the invader a second time. However, there is a risk associated with this, the risk of damaging normal body components. One reason the acquired immune system is so complex is that considerable effort must be put into ensuring that it will attack only foreign or abnormal tissues and will ignore normal healthy tissues, and many different mechanisms ensure that the chances of developing autoimmunity are minimized. In addition, immune responses must be regulated to ensure that they are appropriate with respect to both quality and quality.
The demonstration that the gut microflora is an important constituent in the intestine's mucosal barrier has introduced the concept of probiotic therapy. A probiotic has been defined as a live microbial feed supplement whose benefit affects the host by improving its intestinal microbial balance [23–25]. The criteria for a microorganism to be defined as a probiotic include that the strain is of human origin, is safe for human use, is stable in acid and bile, and adhere to the intestinal mucosa [26]. Probiotic bacteria are shown to promote the endogeneous host defense mechanisms. In addition to the effects of probiotics on nonimmunologic gut defense, which is characterized by stabilization of the gut microflora [27, 28], probiotic bacteria have been shown to enhance humoral immune responses and thereby promote the intestine's immunology barrier [29, 30]. Moreover, probiotic bacteria have been shown to stimulate nonspecific host resistance to microbial pathogens [31, 32], thereby to aid in immune elimination, and to modulate the host's immune responses to potentially harmful antigens with a potential to downregulate hypersensitivity reactions [33].
Immune modulators can shape the host response to challenge with innocuous antigens and protect against allergic airway inflammation in asthma and possibly other diseases affecting the immune system, including different types of tumours. Among several potential modulators, FR-91 which is a standardized lysate of microbial cells belonging to the Bacillus genus has been shown to enhance some immune system associated functions in different clinical trials and has been used in this study to demonstrate its ability in modulating the expression, in in vitro assays, of activation markers by lymphocytes and the release by PBMCs, obtained from healthy individuals and patients with NHL, of different cytokines related to the activated phase. Immunological lymphocyte subset typing is a widespread routine laboratory method to assess numbers and ratios of peripheral blood lymphocytes and various alterations of blood lymphocyte subsets in almost every conceivable physiological and pathological conditions have been described [34]. It plays a significant role in the diagnosis and monitoring of immunodeficiency syndromes, especially in the prognostic classification of HIV infection [35]. It is further an important tool to monitor lymphocyte targeted immunosuppressive therapy in patients at risk for rejection after solid organ transplantation [36]. The major diagnostic role of lymphocyte subset typing is the screening for non-Hodgkin lymphomas with peripheral blood involvement and their differentiation from reactive lymphoproliferative conditions [37].
In the present study only small differences between NHL lymphocyte subsets (increased expression of CD3, CD4, and CD69) comparing to healthy subjects (increased expression of CD3 and reduction of expression of CD8) after treatment with FR-91 were observed and this could be due to the fact that low-grade NHL that primarily involve the spleen might send only a few pathological cells into the peripheral blood, without causing evident changes in lymphocyte subsets as well as in absolute lymphocyte counts.
A homeostatic mechanism that maintains normal levels of CD3+ T cells in HIV+ patients irrespective of CD4+ or CD8+ T cell levels has been described recently, refocusing efforts to understand the homeostatic processes that maintain T cell population [38]. The mechanisms by which FR-91 modulates immune function at the cellular and molecular levels are still poorly understood. Furthermore, because the function of CD69 is not known, the implications and relevance of the effects of FR-91 on mitogen-induced lymphocyte activation are not clear. Thus, whereas a reduction in lymphocyte activation may be undesirable in terms of host defense, it may be useful in situations such as allergy and inflammatory disease.
A series of cytokine assays corroborated the speculation that FR-91 can induce lymphocyte activation and cytokine release. FR-91 effectively enhanced the production of TNF-α, IFN-γ, and IL-12 p70. These products are considered important mediators of tumour cytostasis and/or cytotoxicity. TNF-α may be able to directly cause haemorrhagic necrosis of tumours [39, 40]. IL-1β has been shown to be a mediator of tumour cytostasis [41], and IL-12 p70, the biologically active heterodimer of IL-12, may induce toxic effects indirectly by enhancing the Th1 cellular immune response [42]. Therefore, FR-91 may mediate its immune functions by stimulating immune cells to release an arsenal of tumouricidal mediators. The influence of FR-91 on the cell-mediated cytotoxicity of NK and T cells may be inferred from its suppressive effect on IL-4 production from stimulated lymphocytes as well as its stimulatory effect on IL-12 p70 production. IL4 and IL-12 generally have opposing effects on cell-mediated immunity [43]. IL-4 acts in most instances opposite to a Th1 cellular immune response, whereas IL-12 promotes a Th1 response. The contrary effects of FR-91 on IL-4 and IL-12 production may augment the Th1 response and enhance the cytotoxicity of CTL and NK cells.
The immunomodulatory effect of FR-91 on TNF-α and IFN-γ was similar to LPS. Significant differences were observed between healthy individuals and NHL patients. Both agents stimulated a comparable pattern of release, with the quantity produced by untreated cells consistently lower than LPS and FR-91. The amount of IL-12 p70 stimulated by FR-91 was approximately the same as the amount produced by LPS, but again higher in the NHL patient group.
It is important to point out the role played by FR-91 in the IL-2 production in the NHL group. IL-2 represents the most important cytokine discovered to date and appears to act as a conductor of the immunologic orchestra. Among its potential roles in cancer therapy are its ability to induce the proliferation of tumour-specific T cells and to cause normal lymphocytes to acquire an ability to lyse a variety of tumour targets in preference to normal targets. In murine models tumour-specific T lymphocytes have been generated from the peripheral blood and various organs as well as from the site of the tumour and have been reported to be immunotherapeutically effective when adoptively transferred in conjunction with cyclophosphamide and IL-2 [44–46].
It is possible that the theoretical advantages of in vitro T cells activated by FR-91 treatments include (a) target specificity, (b) ability to “home” to sites of tumour and proliferate there in response to tumour, (c) ability to persist in vivo long term, and (d) ability to maintain proliferative and cytolytic function in the presence of far lower IL-2 concentration. All these results demonstrate the presence, in the FR-91 bacterial extract, of small peptides able to actively modulate the response of peripheral immune system.
In conclusion FR-91 seems to affect lymphocyte subpopulations, in vitro cytokine production, and mitogen-induced lymphocyte activation in a dose-dependent manner in both healthy individuals and NHL patients and the use of FR-91 can be recommended in pathological situations where the immune system is immunocompromized and in those situations where immune system functioning must be restored.
References
- 1.Arulrayan N, Rangasamy S, James E, Pitchai D. A database for medicinal plants used in the treatment of diabetes and its secondary complications. Bioinformation. 2007;2:22–23. doi: 10.6026/97320630002022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kasirajan B, Maruthamuthu R, Gopalakrishnan V, et al. A database for medicinal plants used in treatment of asthma. Bioinformation. 2007;2(3):105–106. doi: 10.6026/97320630002105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mayer AMS, Rodríguez AD, Berlinck RGS, Hamann MT. Marine pharmacology in 2003-4: marine compounds with anthelmintic antibacterial, anticoagulant, antifungal, anti-inflammatory, antimalarial, antiplatelet, antiprotozoal, antituberculosis, and antiviral activities; affecting the cardiovascular, immune and nervous systems, and other miscellaneous mechanisms of action. Comparative Biochemistry and Physiology C. 2007;145:553–581. doi: 10.1016/j.cbpc.2007.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tapsell LC, Hemphill I, Cobiac L, et al. Health benefits of herbs and spices: the past, the present, the future. The Medical Journal of Australia. 2006;185(4, supplement):S4–S24. doi: 10.5694/j.1326-5377.2006.tb00548.x. [DOI] [PubMed] [Google Scholar]
- 5.Lee B-B, Cha M-R, Kim S-Y, Park E, Park H-R, Lee S-C. Antioxidative and anticancer activity of extracts of cherry (Prunus serrulata var. spontanea) blossoms. Plant Foods for Human Nutrition. 2007;62(2):79–84. doi: 10.1007/s11130-007-0045-9. [DOI] [PubMed] [Google Scholar]
- 6.Ko H-C, Wang Y-H, Liou K-T, et al. Anti-inflammatory effects and mechanisms of the ethanol extract of Evodia rutaecarpa and its bioactive components on neutrophils and microglial cells. European Journal of Pharmacology. 2007;555(2-3):211–217. doi: 10.1016/j.ejphar.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 7.Härtel C, Iblher P, Puzik A, et al. Immunosuppressive activity of the immunophilin-binding drug sanglifehrin A in human whole blood: potent inhibition of interleukin-6 produced by lymphocytes and monocytes. Scandinavian Journal of Immunology. 2006;63(1):26–34. doi: 10.1111/j.1365-3083.2006.01702.x. [DOI] [PubMed] [Google Scholar]
- 8.Lara-Villoslada F, Olivares M, Sierra S, Rodríguez JM, Boza J, Xaus J. Beneficial effects of probiotic bacteria isolated from breast milk. British Journal of Nutrition. 2007;98(supplement 1):S96–S100. doi: 10.1017/S0007114507832910. [DOI] [PubMed] [Google Scholar]
- 9.Bengmark S, Gil A. Bioecological and nutritional control of disease: prebiotics, probiotics and synbiotics. Nutricion Hospitalaria. 2006;21(supplement 2):73–86. [PubMed] [Google Scholar]
- 10.Jordan JL, Sullivan AM, Lee TDG. Immune activation by a sterile aqueous extract of Cordyceps sinensis: mechanism of action. Immunopharmacology and Immunotoxicology. 2008;30(1):53–70. doi: 10.1080/08923970701812332. [DOI] [PubMed] [Google Scholar]
- 11.Savilahti E, Kuitunen M, Vaarala O. Pre and probiotics in the prevention and treatment of food allergy. Current Opinion in Allergy and Clinical Immunology. 2008;8(3):243–248. doi: 10.1097/ACI.0b013e3282ffb134. [DOI] [PubMed] [Google Scholar]
- 12.Hatakka K, Saxelin M. Probiotics in intestinal and non-intestinal infectious diseases—clinical evidence. Current Pharmaceutical Design. 2008;14(14):1351–1367. doi: 10.2174/138161208784480162. [DOI] [PubMed] [Google Scholar]
- 13.Steurer-Stey C, Bachmann LM, Steurer J, Tramèr MR. Oral purified bacterial extracts in chronic brochitis and COPD: systematic review. Chest. 2004;126(5):1645–1655. doi: 10.1378/chest.126.5.1645. [DOI] [PubMed] [Google Scholar]
- 14.Braido F, Tarantini F, Ghiglione V, Melioli G, Canonica GW. Bacterial lysate in the prevention of acute exacerbation of COPD and in respiratory recurrent infections. International Journal of COPD. 2007;2(3):335–345. [PMC free article] [PubMed] [Google Scholar]
- 15.Cazzola M, Rogliani P, Curradi G. Bacterial extracts for the prevention of acute exacerbations in chronic obstructive pulmonary disease: a point of view. Respiratory Medicine. 2008;102(3):321–327. doi: 10.1016/j.rmed.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Arandjus C, Black PN, Poole PJ, Wood Baker R, Steurer-Stey C. Oral bacterial vaccines for the prevention of acute exacerbations in chronic obstructive pulmonary disease and chronic bronchitis. Respiratory Medicine. 2006;100(10):1671–1681. doi: 10.1016/j.rmed.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 17.Collet JP, Shapiro S, Ernst P, et al. Effects of an immunostimulating agent on acute exacerbations and hospitalizations in patients with chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine. 1997;156(6):1719–1724. doi: 10.1164/ajrccm.156.6.9612096. [DOI] [PubMed] [Google Scholar]
- 18.Lanzilli G, Falchetti R, Tricarico M, Ungheri D, Fuggetta MP. In vitro effects of an immunostimulating bacterial lysate on human lymphocyte function. International Journal of Immunopathology and Pharmacology. 2005;18(2):245–254. doi: 10.1177/039463200501800207. [DOI] [PubMed] [Google Scholar]
- 19.Lanzilli G, Falchetti R, Cottarelli A, Macchi A, Ungheri D, Fuggetta MP. In vivo effect of an immunostimulating bacterial lysate on human B lymphocytes. International Journal of Immunopathology and Pharmacology. 2006;19(3):551–559. doi: 10.1177/039463200601900311. [DOI] [PubMed] [Google Scholar]
- 20.Park J-H, Um J-I, Lee B-J, et al. Encapsulated Bifidobacterium bifidum potentiates intestinal IgA production. Cellular Immunology. 2002;219(1):22–27. doi: 10.1016/s0008-8749(02)00579-8. [DOI] [PubMed] [Google Scholar]
- 21.de Moreno de LeBlanc A, Chaves S, Carmuega E, Weill R, Antóine J, Perdigón G. Effect of long-term continuous consumption of fermented milk containing probiotic bacteria on mucosal immunity and the activity of peritoneal macrophages. Immunobiology. 2008;213(2):97–108. doi: 10.1016/j.imbio.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 22.Díaz-Ropero MP, Martín R, Sierra S, et al. Two Lactobacillus strains, isolated from breast milk, differently modulate the immune response. Journal of Applied Microbiology. 2007;102(2):337–343. doi: 10.1111/j.1365-2672.2006.03102.x. [DOI] [PubMed] [Google Scholar]
- 23.Penna FJ, Péret LA, Vieira LQ, Nicoli JR. Probiotics and mucosal barrier in children. Current Opinion in Clinical Nutrition and Metabolic Care. 2008;11(5):640–644. doi: 10.1097/MCO.0b013e32830a70ab. [DOI] [PubMed] [Google Scholar]
- 24.Khan SH, Ansari FA. Probiotics—the friendly bacteria with market potential in global market. Pakistan Journal of Pharmaceutical Sciences. 2007;20(1):76–82. [PubMed] [Google Scholar]
- 25.Macfarlane S, Macfarlane GT, Cummings JH. Review article: prebiotics in the gastrointestinal tract. Alimentary Pharmacology and Therapeutics. 2006;24(5):701–714. doi: 10.1111/j.1365-2036.2006.03042.x. [DOI] [PubMed] [Google Scholar]
- 26.Blandino G, Fazio D, Di Marco R. Probiotics: overview of microbiological and immunological characteristics. Expert Review of Anti-Infective Therapy. 2008;6(4):497–508. doi: 10.1586/14787210.6.4.497. [DOI] [PubMed] [Google Scholar]
- 27.de Vrese M, Schrezenmeir J. Probiotics, prebiotics, and synbiotics. Advances in Biochemical Engineering/Biotechnology. 2008;111:1–66. doi: 10.1007/10_2008_097. [DOI] [PubMed] [Google Scholar]
- 28.Gibson GR. Prebiotics as gut microflora management tools. Journal of Clinical Gastroenterology. 2008;42(supplement 2):S75–S79. doi: 10.1097/MCG.0b013e31815ed097. [DOI] [PubMed] [Google Scholar]
- 29.Madsen K. Probiotics and the immune response. Journal of Clinical Gastroenterology. 2006;40(3):232–234. doi: 10.1097/00004836-200603000-00014. [DOI] [PubMed] [Google Scholar]
- 30.Lutgendorff F, Akkermans LMA, Söderholm JD. The role of microbiota and probiotics in stress-induced gastrointestinal damage. Current Molecular Medicine. 2008;8(4):282–298. doi: 10.2174/156652408784533779. [DOI] [PubMed] [Google Scholar]
- 31.Kim Y, Kim S-H, Whang K-Y, Kim Y-J, Oh S. Inhibition of Escherichia coli O157:H7 attachment by interactions between lactic acid bacteria and intestinal epithelial cells. Journal of Microbiology and Biotechnology. 2008;18(7):1278–1285. [PubMed] [Google Scholar]
- 32.Spinler JK, Taweechotipatr M, Rognerud CL, Ou CN, Tumwasorn S, Versalovic J. Human-derived probiotic Lactobacillus reuteri demonstrate antimicrobial activities targeting diverse enteric bacterial pathogens. Anaerobe. 2008;14(3):166–171. doi: 10.1016/j.anaerobe.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Isolauri E, Salminen S. Probiotics: use in allergic disorders: a Nutrition, Allergy, Mucosal Immunology, and Intestinal Microbiota (NAMI) Research Group Report. Journal of Clinical Gastroenterology. 2008;42(supplement 2):S91–S96. doi: 10.1097/MCG.0b013e3181639a98. [DOI] [PubMed] [Google Scholar]
- 34.Armitage J, Vose J, Weisenburger D. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes international T-cell lymphoma project. Journal of Clinical Oncology. 2008;26(25):4124–4130. doi: 10.1200/JCO.2008.16.4558. [DOI] [PubMed] [Google Scholar]
- 35.Barnett D, Walker B, Landay A, Denny TN. CD4 immunophenotyping in HIV infection. Nature Reviews Microbiology. 2008;6(supplement 11):S7–S15. doi: 10.1038/nrmicro1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cady FM, Morice WG. Flow cytometric assessment of T-cell chronic lymphoproliferative disorders. Clinics in Laboratory Medicine. 2007;27(3):513–532. doi: 10.1016/j.cll.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 37.Lindsey WB, Lowdell MW, Marti GE, et al. CD69 expression as an index of T-cell function: assay standardization, validation and use in monitoring immune recovery. Cytotherapy. 2007;9(2):123–132. doi: 10.1080/14653240601182838. [DOI] [PubMed] [Google Scholar]
- 38.Kingkeow D, Heilig CM, Costello C, et al. Lymphocyte homeostasis in HIV-infected northern Thais. AIDS Research and Human Retroviruses. 2004;20(6):636–641. doi: 10.1089/0889222041217491. [DOI] [PubMed] [Google Scholar]
- 39.Wang S. The promise of cancer therapeutics targeting the TNF-related apoptosis-inducing ligand and TRAIL receptor pathway. Oncogene. 2008;27(48):6207–6215. doi: 10.1038/onc.2008.298. [DOI] [PubMed] [Google Scholar]
- 40.Johnstone RW, Frew AJ, Smyth MJ. The TRAIL apoptotic pathway in cancer onset, progression and therapy. Nature Reviews Cancer. 2008;8(10):782–798. doi: 10.1038/nrc2465. [DOI] [PubMed] [Google Scholar]
- 41.Thorns V, Walter GF, Licastro F. Effects of IL6 and IL1β on aFGF expression and excitotoxicity in NT2N cells. Journal of Neuroimmunology. 2002;127(1-2):22–29. doi: 10.1016/s0165-5728(02)00072-3. [DOI] [PubMed] [Google Scholar]
- 42.Wang M, Xie Z, Shi M, et al. A new strategy to induce effective antitumour response in vitro and in vivo. Scandinavian Journal of Immunology. 2008;68(3):287–296. doi: 10.1111/j.1365-3083.2008.02140.x. [DOI] [PubMed] [Google Scholar]
- 43.Ghadimi D, Fölster-Holst R, de Vrese M, Winkler P, Heller KJ, Schrezenmeir J. Effects of probiotic bacteria and their genomic DNA on TH1/TH2-cytokine production by peripheral blood mononuclear cells (PBMCs) of healthy and allergic subjects. Immunobiology. 2008;213(8):677–692. doi: 10.1016/j.imbio.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 44.Cheadle EJ, Gilham DE, Hawkins RE. The combination of cyclophosphamide and human T cells genetically engineered to target CD19 can eradicate established B-cell lymphoma. British Journal of Haematology. 2008;142(1):65–68. doi: 10.1111/j.1365-2141.2008.07145.x. [DOI] [PubMed] [Google Scholar]
- 45.Quan WDY, Jr., Quan FM, King LA, Walker PR. Low-dose cyclophosphamide and continuous-infusion interleukin-2 with famotidine in previously treated metastatic melanoma or kidney cancer. Cancer Biotherapy and Radiopharmaceuticals. 2008;23(1):108–113. doi: 10.1089/cbr.2007.0420. [DOI] [PubMed] [Google Scholar]
- 46.Bracci L, Moschella F, Sestili P, et al. Cyclophosphamide enhances the antitumor efficacy of adoptively transferred immune cells through the induction of cytokine expression, B-cell and T-cell homeostatic proliferation, and specific tumor infiltration. Clinical Cancer Research. 2007;13(2):644–653. doi: 10.1158/1078-0432.CCR-06-1209. [DOI] [PubMed] [Google Scholar]