Abstract
Dual-energy X-ray absorptiometry (DXA) has become a common measurement of human body composition. However, obese subjects have been understudied largely due to weight and scan area restrictions. Newer DXA instruments allow for heavier subjects to be supported by the DXA scanner, but the imaging area is still smaller than the body size of some obese subjects. In this study, we determined the validity of an automated half-scan methodology by comparing to the standard whole-body scans in a cohort of obese volunteers. Fifty-two subjects whose BMI >30 kg/m2 completed whole-body iDXA (GE Lunar) scans. The resulting scans were analyzed in three ways: the standard whole-body scan, total body estimated from the left side, and from the right side. Fat mass, nonbone lean mass, bone mineral content (BMC), and percent fat derived from each half scan were compared to the whole-body scans. Total fat mass, nonbone lean mass, or percent fat was comparable for the whole-body scans, left, and right side scans (>97% within individuals and >99.9% for the group). The BMC estimate using the right side scan was slightly but statistically higher than the whole-body BMC (∼30 g or 1%, P < 0.001), while the left side scan BMC estimate was lower than the whole-body BMC by the same magnitude. No significant magnitude bias was found for any of the composition variables. We conclude that the new iDXA half-body analysis in obese subjects appears to be closely comparable to whole-body analysis for fat mass, nonbone lean mass, and percent fat.
INTRODUCTION
The determination of body composition is important to clinicians, researchers, patients, and the general public. The study of body composition changes in health and disease have lead to a greater understanding of growth, aging, malnutrition, and obesity as well as the impact of medical interventions (1). Among several methods for studying in vivo human body composition, dual-energy X-ray absorptiometry (DXA) has emerged as one of the most commonly used clinical standards (2). Typically the energy source produces photons at two different energy levels, 40 and 70 keV, which pass through tissues and attenuate at rates related to its elemental composition. Bone is rich in highly attenuating minerals, calcium and phosphorous, and is readily distinguished from soft tissues. The unique elemental profiles of bone, fat, and nonbone lean tissue allow for visualization and separate analysis of each tissue type. Most currently marketed DXA instruments use standardized calibrations (3), have quick scans (5–20 min), and use standard software for analyses. The ability to study body composition in the whole body and individual body segments is also helpful for determining body fat distribution and regional bone mineral density.
Two unfortunate limitations of DXA scanners have been the weight limitation of the scanning bed (typically 300 lb) and the width of the scanning area (usually ∼60 cm). When an individual's body dimensions exceed these limits, the accuracy of the measurement is typically compromised. This limitation has lead to the development of a technique to estimate total-body composition from a half-body scan.
To our knowledge, there is only one study that compared half-body scan to total-body composition (4). However, the subject population included in this study was restricted due to the stringent body weight and size limitation of the particular instrument used (DPX-1; Lunar Radiation, Madison, WI). With the recent introduction of iDXA (GE Lunar Medical Systems, Madison, WI), the weight limit has been raised to 400 lb, scanning width increased to 66 cm, and scanning arm height, which constrains the maximal torso thickness, increased to 46 cm. Furthermore, one side of the scanning table has been extended an additional 10 cm beyond the scan area to allow half-body scans of larger individuals.
The purpose of this study was to validate the half-scan analysis by comparing to the standard whole-body scans in a sample of obese adults. Simulated half-body scans were compared to each subject's total-body scan in terms of percent body fat, nonbone lean body mass, fat mass, and bone mineral content (BMC).
METHODS AND PROCEDURES
Subjects
A sample of 53 obese subjects (BMI > 30 kg/m2) recruited to participate in the obesity-related clinical research protocols at the National Institutes of Health were included in this study. Participants were admitted to the Metabolic Clinical Research Unit of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) in Bethesda, Maryland for clinical metabolic assessment including a DXA scan. All subjects had body dimensions that could be contained within the imaging field of the GE iDXA scanner. Subjects were generally healthy, and weight stable at the time of measurement. No female subjects were pregnant as verified by urine pregnancy tests obtained <48 h before the study. Further details of the study subjects are displayed in Table 1. The protocol was approved by the institutional review board of the National Institute of Diabetes and Digestive and Kidney Diseases. Informed consent was obtained from all subjects before the scans.
Table 1.
Characteristics of study subjects presented as mean ± s.d. and minimum–maximum
| All subjects (n = 52) | Women (n = 37) | Men (n =15) | |
|---|---|---|---|
| Age (years) | 43.1 ± 8.8 (19–63) | 43.0 ± 9.1 (19–63) | 43.2 ± 8.2 (27–58) |
| Height (cm) | 165.9 ± 10.0 (147.5–196.0) | 161.1 ± 5.2 (147.5–169.6) | 177.8 ± 9.2 (164.9–196.0) |
| Body mass (kg) | 95.6 ± 11.7 (75.2–126.0) | 90.7 ± 8.5 (75.2–111.8) | 107.8 ± 9.5 (93.8–126.0) |
| BMI (kg/m2) | 34.7 ± 3.0 (30.4–41.0) | 34.9 ± 3.2 (30.4–41.0) | 34.2 ± 2.6 (30.9–38.9) |
Instrumentation
DXA measurements were made using a total-body scanner (Lunar iDXA; GE Healthcare, Madison, WI). The iDXA is a narrow fan-beam DXA instrument with a high weight limit (400 lb limit) and a relatively wide scanning space (66 cm) designed to accommodate obese subjects. The instrument has three scan modes that adjust the X-ray attenuation for the thickness of each patient: thin (<13 cm), standard (13–25 cm), and thick (>25 cm). For this experiment, all scans were conducted in thick mode, which requires ∼13 min of scan time with an effective radiation dose of 3 μGy per scan (from manufacturer's technical data).
Scan analysis was performed using GE Encore 11.10 software. This software allows for adjustment of regions of interest including the sagittal line, which controls the left–right body distribution of tissue. In addition, the software uses an automatic detection routine to determine whether the subject is within the scan space. This determination is corroborated by a trained operator. If the subject's body is not contained within the scan space, a half-scan analysis is automatically performed by assuming symmetry of the body.
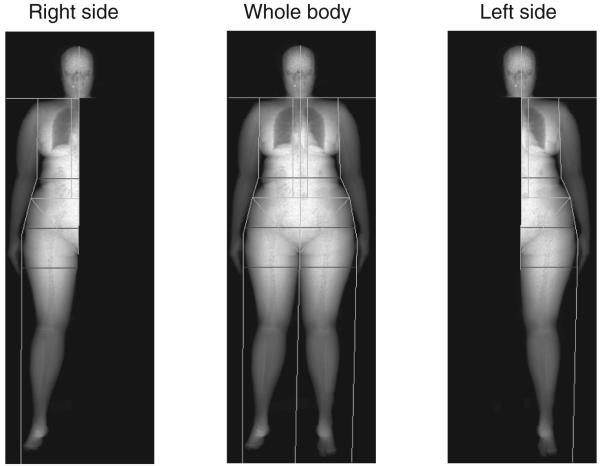
In this study, we took advantage of the automated half-scan analysis by simulating half scans on a cohort of obese patients. Each whole-body image was analyzed, including the manual placement of an appropriate sagittal line. Following this analysis, we chose to re-analyze each scan as a right side scan and a left side scan (Figure 1). By using each side of the body to simulate the whole body, we were able to determine the validity of the half-scan analysis routine in comparison to the whole-body values measured by our iDXA scanner, while only exposing the subjects to one scan.
Figure 1.
Example of iDXA total-body composition image and a representation of the portions of the total-body image used to generate the right side and left side images.
Statistical analysis
All values are expressed as mean ± s.d. and (range) unless otherwise indicated. Mean values for percent body fat, fat mass, lean body mass, BMC, and total tissue were compared between the whole body and right side, and separately between the whole-body and left side scans. We used nonparametric paired t-tests with Bonferroni adjustment for making 10 multiple comparisons, thus the P value for statistical significance used was 0.005 (P = 0.05/10). Correlation plots between whole body and each side were presented across individuals. Bland–Altman analysis (5) was performed to test for magnitude bias in all composition parameters. Statistical analysis was performed using SPSS version 16.0. Due to a small sample of men (n = 15) in our study, and no observable differences between men and women, we pooled the data for the analyses.
RESULTS
In our study, the group differences between the two half-scan simulations and the total-body DXA scan were not significantly different in percent fat, fat mass, nonbone lean mass, or total tissue mass (Table 2). In absolute terms, the fat mass and percent body fat were slightly lower using left side scan (−0.10 ± 0.51 kg and −0.06 ± 0.28%, respectively), and the nonbone lean mass is slightly lower than the whole body using both the right (−0.04 ± 0.54 kg) and left scans (−0.04 ± 0.51 kg). The BMC was significantly different (P < 0.001) between each of the half-body scan estimates and the whole body, with the right side slightly overestimating BMC (23 ± 31 g) and the left side slightly underestimating whole-body BMC (−27 ± 32 g). The differences between men and women were similar.
Table 2.
Comparison of the mean values for the two simulated half scans, and the total-body DXA scan
| Whole body | Right | Left | |
|---|---|---|---|
| Percent fat (%) | 42.2 ± 5.8 (28.9–54.5) | 42.2 ± 5.8 (28.6–55.0) | 42.1 ± 5.8 (29.2–54) |
| Fat (kg) | 39.9 ± 6.0 (28.5–52.2) | 39.9 ± 6.0 (27.7–53.1) | 39.8 ± 6.0 (29.2–52.7) |
| Nonbone lean (kg) | 52.4 ± 9.9 (34.2–76.0) | 52.4 ± 9.8 (33.6–76.5) | 52.4 ± 9.9 (34.8–75.6) |
| BMC (kg) | 2.85 ± 0.48 (1.81–4.24) | 2.88 ± 0.48* (1.84–4.26) | 2.83 ± 0.50* (1.78–4.22) |
| Total tissue mass (kg) | 95.2 ± 11.6 (75.2–124.8) | 95.2 ± 11.5 (74.5–125.3) | 95.1 ± 11.8 (75.9–124.3) |
Mean ± s.d. and minimum–maximum are presented (n = 52).
P < 0.001 vs. whole body.
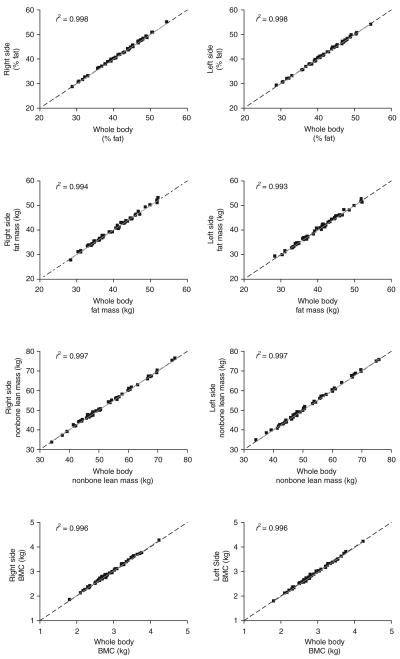
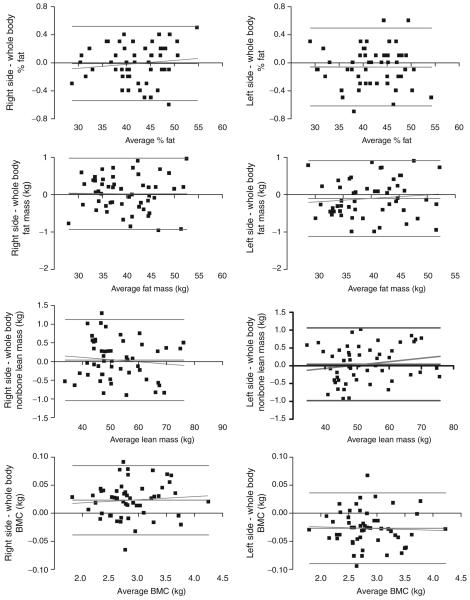
The between-individual measures of percent body fat, fat mass, nonbone lean mass, and BMC estimated from right and left sides were highly correlated with (R2 > 0.99) and closely comparable to the respective measurements from the whole body (Figure 2). Furthermore, Bland–Altman analysis revealed no significant magnitude bias in prediction of percent fat, fat mass, lean mass, or BMC. The 95% confidence intervals were similar between the right and left side methods (Figure 3).
Figure 2.
Correlation plots between right side, left side, and whole-body scans (n = 52). Dashed lines represent line of identity.
Figure 3.
Bland–Altman plots comparing the right side, left side, and whole-body scans. No significant magnitude bias was detected for any of the composition parameters. All r2 < 0.033 (not significant, n = 52).
DISCUSSION
In this study, we used the new iDXA scanner to test the accuracy of body composition estimations from half-body analysis in a group of obese study volunteers. Our results showed that half-body scans can accurately predict whole-body percent body fat, fat mass, and nonbone lean mass in the thick total-body scanning mode. Small but significant differences in BMC were found when the differences between the half-body and whole-body scans were compared.
Although the DXA was created and continues to be used widely as a clinical tool to assess bone mineral density and BMC, it has been applied as a useful technique to measure total and regional body composition during the past 20 years (6-8). It is a direct measure of fat, nonbone lean, and bone tissue compositions. Several previous studies have shown its validity by comparing DXA-derived body composition measurements with values determined by criterion methods (2,4,9-14). Excellent precision of the DXA has also been reported as within-subject test–retest reproducibility (4,15). It is a short duration and technically simple test to perform in most subjects, thus it has been used in large multicenter studies including the National Health and Nutrition Examination Survey (16,17).
However, DXA does have some limitations. The radiation dosage, although small, limits its wide usage in certain populations (children and pregnancy). Systematic variations between devices and software versions have been reported previously (11,17). Moreover, before the introduction of the iDXA, most DXA scanners support a maximum body mass of 300 lbs only and have limited scanning areas (∼190 × 60 cm2), making the study of body composition in obese individuals using DXA difficult.
To our knowledge, Tataranni and Ravussin were the first to report that whole-body composition can be accurately predicted from the results from half-body DXA scans in obese subjects who did not fit entirely in the scanning area (4). In an elegant study of 183 subjects (27 obese individuals were scanned twice, once each on left and right side), the overall symmetry between the left and right sides: 0.03 ± 0.08 kg for bone mineral (r2 = 0.89), −0.04 ± 0.62 kg for fat mass (r2 = 0.99), and −0.04 ± 0.86 kg for nonbone lean mass (r2 =0.97). However, in the obese individuals (n = 21) who completed two scans, the group differences between the two sides were slightly larger for fat mass (0.72 ± 0.11 kg) and nonbone lean mass (0.30 ± 0.11 kg). In comparison, the group differences between half-body and whole-body scans were considerably smaller in our study. This could be a result of body shifts that occur during the multiple scans in the previous study (3) or processing errors in the identified regions of interest.
Recognizing an emerging need to measure body composition in obese individuals, iDXA was introduced to the market recently. It has expanded its capacity to support subjects' body weight up to 400 lb and 66 cm of scanning width. However, this width still does not cover some subjects, even those with a body mass <400 lb. The iDXA scanner table has allowed an extra 10 cm outside of the scanning area on opposite side of the moving arm to permit an off-center shift of the subject for a half scan of his/her right side. The software version 11.0 will automatically detect this change and analyze only the right side of the image and yield the half-body scan results. To our knowledge, the validity of the iDXA half-body scan as compared to whole-body scans has not been reported in obese subjects.
For this purpose, we re-analyzed the images of a group of obese healthy volunteers (BMI > 30 kg/m2) who were able to fit in the iDXA scanning area. Each of the simulated half-body scans was compared to the whole-body scan, made on the same iDXA machine, and used to develop the half-body estimations. This was done to eliminate the need of repositioning and rescanning different sides which could introduce estimation errors such as seen in the previous study (4). Results from our study indicate that there are no significant differences between the estimated percent fat, fat mass, and nonbone lean mass from half-scan parameters and the whole-body scan parameters. However, the slight differences between right and left-scan BMC did reach statistical significance. Although the group difference was small, ∼30 g or 1%, the individual variation ranged from −66 to 95 g (−3.5 to 3.38%) compared to the whole-body BMC values. This is likely due to lateral BMC differences in right- vs. left-handed subjects. Although this has been shown in athletes in sports such as tennis (18), Akar et al. also found significant higher forearm BMC in dominant compared to nondominant arms (19). In our subjects, we did not assess their handedness; but since ∼90% of the general populations are right-handed, the difference in BMC between right and left scans makes sense. We further examined BMC differences in arms and legs separately between the right vs. left sides, and found the differences were more pronounced for arms (right-left : 5.9 ± 9.17 g) than for legs (2.99 ± 16.1 g). We postulate that as our legs are used more for ambulatory functions, such as walking, the difference in BMC would be smaller than in arms which would be used more preferentially in sports or daily living.
Although the minor differences between the studies could be attributed to the hardware (Lunar DPX-1 vs. iDXA), thickness mode (various modes vs. single mode >25 cm), and software (1.3z vs. 11.0), our main conclusion in obese individuals thus confirms that of Tataranni and Ravussin (4). We further explored the ranges of individual variability by Bland and Altman approach, showing no significant trend in the differences between half-body and total-body scan and measured percent fat or tissue masses. The 95% confidence intervals for all these measurements were also comparable to the test–retest reproducibility for total-body scan parameters within a subset of the subjects (n = 16) who completed two scans (data not shown). Thus, the small differences observed in this study suggest that there is a low risk of introducing systematic bias into a data set by utilizing both whole-body and half-body scans within a single study. Although we did not include subjects who could not fit into the scanning area of the iDXA in this study, there were no significant trends in between-individual magnitude bias in the differences between half-body and whole-body scans. This persistent symmetry suggests that the half-body DXA scan results could be comparable to whole-body scans even for larger subjects.
Diverging slightly from the previous work (4), we did not compare right and left body scans to one another. We determined that since each half scan could be compared to a total-body scan, which should be the gold standard reference for our estimation routine, comparisons between left and right sides are unlikely to be significantly different. Similarly, rather than comparing our half scans to whole-body analysis using a different assessment modality, such as hydrodensitometry, we were able to narrowly focus our analysis on half-body vs. whole-body DXA body composition thereby eliminating differences in composition resulting from differences in instrumentation.
We conclude that measurements of nonbone lean and fat masses, and percent fat in obese healthy adults can be assessed by half-body scan which is closely comparable to whole-body scans using the new iDXA scanner. The increased scanning area and additional table width of iDXA further enhance its ability to measure body composition in obese individuals. If the BMC is the desired outcome parameter, a whole-body scan or scanning both sides separately may be required. Future studies should address whether the iDXA measurements of body composition, half-body or whole-body scans, are accurate as compared to other reference measures of total-body composition in lean and obese individuals.
ACKNOWLEDGMENT
This work was supported by the Intramural Research Program of the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Clinical Endocrinology Branch.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1.Lee S, Gallagher D. Assessment methods in human body composition. Curr Opin Clin Nutr Metab Care. 2008;11:566–572. doi: 10.1097/MCO.0b013e32830b5f23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ellis KJ. Human body composition: in vivo methods. Physiol Rev. 2000;80:649–680. doi: 10.1152/physrev.2000.80.2.649. [DOI] [PubMed] [Google Scholar]
- 3.Goodsitt MM. Evaluation of a new set of calibration standards for the measurement of fat content via DPA and DXA. Med Phys. 1992;19:35–44. doi: 10.1118/1.596890. [DOI] [PubMed] [Google Scholar]
- 4.Tataranni PA, Ravussin E. Use of dual-energy X-ray absorptiometry in obese individuals. Am J Clin Nutr. 1995;62:730–734. doi: 10.1093/ajcn/62.4.730. [DOI] [PubMed] [Google Scholar]
- 5.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 6.Laskey MA. Dual-energy X-ray absorptiometry and body composition. Nutrition. 1996;12:45–51. doi: 10.1016/0899-9007(95)00017-8. [DOI] [PubMed] [Google Scholar]
- 7.Mazess RB, Barden HS, Bisek JP, Hanson J. Dual-energy x-ray absorptiometry for total-body and regional bone-mineral and soft-tissue composition. Am J Clin Nutr. 1990;51:1106–1112. doi: 10.1093/ajcn/51.6.1106. [DOI] [PubMed] [Google Scholar]
- 8.Roubenoff R, Kehayias JJ, Dawson-Hughes B, Heymsfield SB. Use of dual-energy x-ray absorptiometry in body-composition studies: not yet a “gold standard”. Am J Clin Nutr. 1993;58:589–591. doi: 10.1093/ajcn/58.5.589. [DOI] [PubMed] [Google Scholar]
- 9.Goran MI, Toth MJ, Poehlman ET. Assessment of research-based body composition techniques in healthy elderly men and women using the 4-compartment model as a criterion method. Int J Obes Relat Metab Disord. 1998;22:135–142. doi: 10.1038/sj.ijo.0800555. [DOI] [PubMed] [Google Scholar]
- 10.Kistorp CN, Svendsen OL. Body composition analysis by dual energy X-ray absorptiometry in female diabetics differ between manufacturers. Eur J Clin Nutr. 1997;51:449–454. doi: 10.1038/sj.ejcn.1600424. [DOI] [PubMed] [Google Scholar]
- 11.Lohman T. Dual X-ray absorptiometry. In: Roche AF, Heymsfield SB, Lohman TG, editors. Human Body Composition. Human Kinetics; Champaign, IL: 1996. pp. 63–78. [Google Scholar]
- 12.Visser M, Fuerst T, Lang T, Salamone L, Harris TB. Validity of fan-beam dual-energy X-ray absorptiometry for measuring fat-free mass and leg muscle mass. Health, Aging, and Body Composition Study—Dual-Energy X-ray Absorptiometry and Body Composition Working Group. J Appl Physiol. 1999;87:1513–1520. doi: 10.1152/jappl.1999.87.4.1513. [DOI] [PubMed] [Google Scholar]
- 13.Wang J, Thornton JC, Horlick M, et al. Dual X-Ray absorptiometry in pediatric studies: changing scan modes alters bone and body composition measurements. J Clin Densitom. 1999;2:135–141. doi: 10.1385/jcd:2:2:135. [DOI] [PubMed] [Google Scholar]
- 14.Chen Z, Wang Z, Lohman T, et al. Dual-energy X-ray absorptiometry is a valid tool for assessing skeletal muscle mass in older women. J Nutr. 2007;137:2775–2780. doi: 10.1093/jn/137.12.2775. [DOI] [PubMed] [Google Scholar]
- 15.Buchholz AC, Majchrzak KM, Chen KY, Shankar SM, Buchowski MS. Use of air displacement plethysmography in the determination of percentage of fat mass in African American children. Pediatr Res. 2004;56:47–54. doi: 10.1203/01.PDR.0000130477.05324.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention NHANES 1999–2000 Public Data Release File Documentation. 1999 < http://www.cdc.gov/nchs/data/nhanes/gendoc.pdf>.
- 17.Schoeller DA, Tylavsky FA, Baer DJ, et al. QDR 4500A dual-energy X-ray absorptiometer underestimates fat mass in comparison with criterion methods in adults. Am J Clin Nutr. 2005;81:1018–1025. doi: 10.1093/ajcn/81.5.1018. [DOI] [PubMed] [Google Scholar]
- 18.Kontulainen S, Kannus P, Haapasalo H, et al. Changes in bone mineral content with decreased training in competitive young adult tennis players and controls: a prospective 4-yr follow-up. Med Sci Sports Exerc. 1999;31:646–652. doi: 10.1097/00005768-199905000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Akar S, Sivrikaya H, Canikli A, Varoglu E. Lateralized mineral content and density in distal forearm bones in right-handed men and women: relation of structure to function. Int J Neurosci. 2002;112:301–311. doi: 10.1080/00207450212034. [DOI] [PubMed] [Google Scholar]