Abstract
Background
Healthy People 2010 underscores the relevance of eliminating health disparities. Thus, it is paramount to create interventions that promote health for all individuals.
Purpose
This study examined differences in rates of and reasons for ineligibility among non-Hispanic blacks and whites in a randomized controlled physical activity intervention study.
Methods
Participants (1245 adults) responded to community advertising for the research study. Eligibility at the four pre-randomization assessment sessions was determined by self-reported medical information, resting EKG, 7-Day Physical Activity Recall, fitness test, and Stage of Change. We used t-tests to examine the rates of eligibility among participant subgroups.
Results
Blacks had higher rates of overall ineligibility (86.9%) than whites (75.1%; p < .01) and were more likely to be ineligible due to lack of interest or no-show at a pre-randomization appointment (35.4% versus 24.3%; p < .01). Blacks were more likely to be ineligible for medical reasons after the telephone screen (16.3% versus 7.8%; p = .01).
Limitations
This study did not use a random sampling of potential participants from each of the racial/ethnic groups and thus, there is the potential for selection bias.
Conclusions
Blacks were more likely to choose not to enroll in the study due to a lack of interest, but had similar rates of overall medical ineligibility to whites. This highlights the importance of strategies that enhance interest among blacks who initially respond to recruitment advertising.
Keywords: Recruitment; Eligibility; Diversity; Generalizability; White, Black; African-American
Indexing Key Words: Manuscript format: research, Research purpose: descriptive, Study design: randomized trial, Outcome measure: behavioral, Setting: local community, Health focus: physical activity, Strategy: behavior change, Population age: adults, Population circumstances: race/ethnicity
INTRODUCTION
One of the U.S. health priorities outlined in Healthy People 2010 is to eliminate health disparities among individuals of different racial and ethnic backgrounds [1]). To do so, it is important to create interventions that promote health for all individuals. Developing these health promotion interventions requires that randomized clinical trials be conducted in which participants of diverse racial and ethnic backgrounds are adequately represented. In 1993, the National Institutes of Health strengthened their policies on including diverse racial/ethnic groups in clinical research to increase external validity and allow for eventual dissemination of the interventions to a larger heterogeneous population of the U.S. [2].
Research scientists must overcome numerous hurdles to recruit racial/ethnic minority groups. Barriers to recruitment of racial/ethnic minorities have been studied primarily in clinical trials that focus on the prevention and control of various cancers [3–9]. Several of these articles [3;9;10] among others [11–16] delineate the barriers and strategies to enhance recruitment of underrepresented populations (especially racial/ethnic minority samples). Within the area of health promotion interventions for non-cancer samples, there are additional studies addressing the barriers to recruiting racial/ethnic samples [12;17–20]. Barriers among racial/ethnic minority groups include mistrust, fear of exploitation, and skepticism of the medical and research fields stemming from a historical awareness of the unethical treatment of African American males in The Tuskegee Syphilis Study [11;13;21].
Other documented barriers to recruitment of racial/ethnic minorities include lack of information and access to medical and research facilities [14;18], literacy levels [18], lack of minority staff and investigators [11], lack of transportation [14], lack of childcare services [14], medical issues [18;22], co-morbid conditions [18], and burdensome procedures [11]. It has also been reported that racial/ethnic minorities, particularly African-Americans/blacks, may not perceive that they are at risk for health problems and are more likely to seek medical attention only when experiencing an acute medical problem [11;15]. Related to this, African-Americans/blacks may have varied views about preventive measures and possible side effects [11;16], which may serve as a barrier to participating in health promotion research. Even with the multiple articles addressing barriers to recruiting racial/ethnic samples, there is still a need for such studies highlighting the barriers to recruiting racial/ethnic samples in health promotion trials with multiple pre-randomization assessments.
To better understand the complexities of recruiting diverse populations into controlled clinical trials that primarily focus on health promotion, we systematically examined the reasons that potential participants who initially indicated an interest ultimately did not enroll in a health promotion efficacy trial. The overall study was designed to determine the differential effect of intervention delivery channel (Tailored Internet versus Tailored Print) on physical activity adoption and maintenance in previously sedentary adults. As an efficacy study, internal validity was a primary concern and had to be balanced with our goal to recruit a diverse sample of participants. For example, our research design consisted of 3–4 assessments prior to randomization that allowed for more fine-tuned assessment and exclusion due to various medical conditions. While strengthening the internal validity of the study, these multiple pre-randomization assessments may have led to a higher rate of exclusion among participants of racial/ethnic minority status due to increased medical issues and/or a higher rate of dropout possibly due to barriers such as multiple time demands, loss of income, and transportation concerns [17].
The primary purpose of this paper was to examine specific hypotheses related to the recruitment of racial/ethnic minorities into a randomized controlled trial with multiple pre-randomization assessments. Specifically, we hypothesized that a greater proportion of racial/ethnic minorities (e.g., non-Hispanic African-Americans/blacks) would be ineligible (defined throughout as those who did not meet inclusion/exclusion criteria and/or exhibited a lack of interest by not attending a pre-randomization screening session) compared to non-Hispanic whites. Additionally, we predicted that a greater proportion of racial/ethnic minorities, as compared to non-Hispanic whites, would be ineligible due to medical reasons.
METHOD
Participant Recruitment
Participants for the present study were individuals who responded to an advertisement for a randomized, controlled, physical activity promotion trial. The goal of the overall trial was to include 25% of the sample from individuals with a minority racial/ethnic background. This study was initially conducted in the greater Providence, Rhode Island area, where the total population consists of 76.4% White/Caucasian, 8.0% African American/Black, 0.5% Native American, 3.3% Asian, 0.8% Pacific Islander, 8.7% from other races, and 2.3% from two or more races, with 16.4% Hispanic/Latino from any of the above categories [23]. Approximately one year into the recruitment process, it was apparent that we would be unable to meet our goal of enrolling 60 participants from diverse racial/ethnic backgrounds in the Rhode Island area. Therefore, we expanded recruitment efforts to include individuals in the greater Pittsburgh, Pennsylvania area, where one of the co-investigators is employed and there is a larger racial/ethnic minority population. According to the 2004 U.S. Census, the population in Pittsburgh is 62.3% White/Caucasian, 33.0% African American/Black, 3.0% Asian, <1% from other races, and 1.2% from two or more races, with 1.2% of the population Hispanic or Latino from any of the above categories [23]. Providence has 23.6% non-White population, whereas Pittsburgh has a 37.7% non-White population. Participants at both sites were recruited through newspaper advertisements, health fairs, radio advertisements, featured newspaper stories, pay stub advertisements, and worksite website advertisements. Advertisements targeted healthy, sedentary men and women between the ages of 18 to 65. Some of the advertisements at the Rhode Island site and all of the advertisements at the Pittsburgh site were targeted specifically to potential participants from diverse racial/ethnic backgrounds.
Screening Procedures
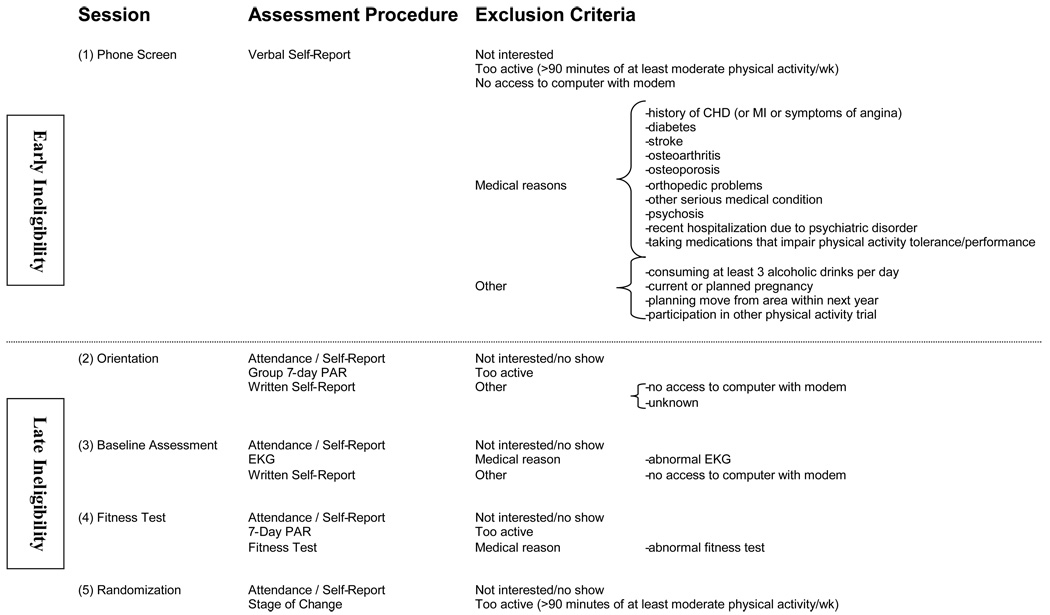
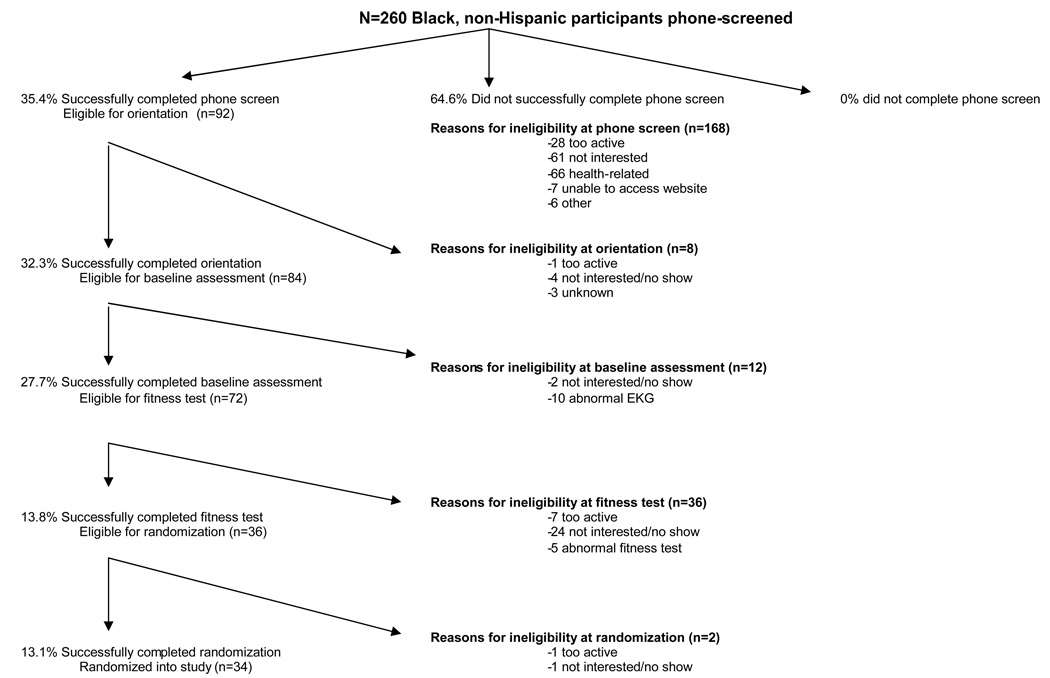
Participants were required to undergo multiple screening assessments prior to being randomized into the study, which included a (1) phone screen, (2) orientation, (3) baseline assessment, (4) fitness test, and (5) randomization (see Figure 1). The Providence site included four on-site assessments (i.e., orientation, baseline assessment, fitness test, and randomization) and the Pittsburgh site included three on-site assessments (orientation and baseline assessments were combined into one visit). Participants at both study sites responded to the recruitment advertisements by calling a dedicated line at the Providence research site staffed by a research assistant (a toll free number was provided for the Pittsburgh participants). The phone screen consisted of a brief explanation of the study and administration of a standardized screening questionnaire (see exclusion criteria). Eligible participants were scheduled to attend the group-based orientation. The orientation included 1) an overview of the study, 2) a consent form signed by interested participants that was approved by both institutional review boards, and 3) completion of a modified group-based 7-day physical activity recall (PAR) by participants, as well as a number of medical history questionnaires and various psychosocial questionnaires. In Providence, participants who remained interested and eligible were then scheduled for an individually-administered baseline assessment, while in Pittsburgh the baseline assessment occurred immediately following orientation. At the baseline assessment, each participant was given a supine EKG and anthropometric measures were taken. EKGs were read by our study cardiologist and eligible participants were scheduled for a fitness test. At the fitness test, a submaximal Balke protocol was performed and a formal 7-Day PAR was administered. The study cardiologist read fitness tests and eligible participants were scheduled for a randomization where they completed a stage-of-change questionnaire and were randomized into one of the treatment conditions.
FIGURE 1.
Screening sessions and possible reasons for ineligibility
Exclusion Criteria
Exclusion criteria were assessed by verbal self-report during the phone screen and again by written self-report during the orientation. Only sedentary and low-active participants, defined as participating in <90 minutes of moderate or vigorous physical activity per week, were eligible. Participants who did not have access to a computer with a modem through home or work were excluded. Medical exclusion criteria included history of coronary heart disease (history of myocardial infarction or symptoms of angina), diabetes, stroke, osteoarthritis, osteoporosis, orthopedic problems which would limit treadmill testing, or any other serious medical condition that would make physical activity unsafe. Other exclusion criteria included individuals who reported consuming ≥ 3 alcoholic drinks per day, current or planned pregnancy, planning to move from the area within the next year, current suicidal ideation or psychosis, hospitalization due to a psychiatric disorder in the past 3 years, taking medication that may impair physical activity tolerance or performance (e.g., beta blockers), and/or participation in one of our previous physical activity trials. Additionally, in order to complete the randomization process, participants had to attend and complete each of the pre-randomization appointments (described above). Failure to attend these sessions resulted in exclusion from the study. Missed appointments were rescheduled for participants who contacted the research staff prior to or following a cancelled appointment. If a participant did not initiate contact with the research staff concerning a missed appointment, then one attempt was made by the research staff to contact them via telephone to reschedule their appointment, after which the participant was categorized as ineligible due to lack of interest. Participants willing to participate in the study read and signed a consent form approved by both institutional review boards.
Measures
For this study, the primary outcome was randomization into the study. Intermediate outcomes were indicated by completion of each of the sessions conducted prior to randomization. The following measures were used to determine eligibility at one or more of the pre-randomization sessions (See Figure 1).
Demographic Questionnaire
This measure examines age, gender, education, race and ethnicity, SES, occupation, and marital status. We also included questions on access to the Internet via a computer at home or work.
7-Day Physical Activity Recall Interview
A modified, group form of the 7-Day Physical Activity Recall (PAR) interview was used to assess baseline physical activity at the orientation session, and the full structured interview was conducted at the baseline fitness test. Several studies have demonstrated the reliability and validity of the PAR [for a review, see [24].
Resting Electrocardiogram (EKG)
At the assessment visit, a resting EKG was performed and read by the study cardiologist, and ineligible participants were informed by our research nurse and referred to their physician for follow-up.
Fitness Test
Participants completed an exercise treadmill test that was administered following the standards and guidelines established by the American College of Sports Medicine [25]. Specifically, participants walked on a treadmill, which gradually increased in elevation until 85% of the individual’s maximum heart rate was achieved. EKGs were obtained during the last 10 seconds of every minute, at peak exercise, and throughout the recovery period (until the resting heart rate had returned to within 15% of baseline). A pre-test supine and standing blood pressure were measured during the last minute of each stage, immediately following exercise, and every two minutes until the participant was stabilized near baseline level. Participants with abnormal EKG or blood pressure responses during the fitness test were excluded.
Stage of Change
At the randomization appointment, stage of change for physical activity was assessed using the measure developed by Marcus and colleagues [26]. Moving from an early stage of change (i.e., Precontemplation, Contemplation, or Preparation stage) to Action has been shown to be significantly associated with positive changes in estimated peak VO2 [27]. Participants in the Action or Maintenance stages were excluded from the study for being too active at baseline.
Statistical Analyses
The primary purpose of this paper was to test specific hypotheses about relative rates of and reasons for ineligibility across racial/ethnic groups. To make comparisons across racial/ethnic groups, we divided participants into two categories: (1) participants who self-identified as non-Hispanic white (n=768), and (2) participants who identified as non-Hispanic black (n=260). As such, the independent variable used for the analysis was racial/ethnic category. Analysis was restricted to these two subgroups because sample sizes among the other racial/ethnic groups were too small to make statistical comparisons (Hispanic white: n=29; Hispanic black: n=18; unknown race and ethnicity: n=85; other: n=132).1
To analyze differences in recruitment rates, we computed the proportion of participants who successfully completed the randomization among participants who were telephone-screened. Additionally, to determine where in the recruitment process any differences in ineligibility rates occurred, we divided the overall recruitment rate into two mutually exclusive and exhaustive categories: (1) the proportion of participants who successfully completed the telephone screen (and were scheduled for orientation) among all participants who were telephone-screened (early ineligibility), and (2) the proportion of participants who successfully completed the randomization among those who successfully completed the phone screen and were scheduled for orientation (late ineligibility; see Figure 1). Indicators of reason for ineligibility focused on health-related reasons versus all other reasons. Specifically, we computed the proportion of participants who were ineligible due to health-related reasons among all those who were telephone-screened (overall medical ineligibility). Additionally, to further divide the overall medical ineligibility rate into two mutually exclusive and exhaustive categories, we computed (1) the proportion of participants who were ineligible for medical reasons as a result of the telephone screen among all those who were telephone-screened (early medical ineligibility), and (2) the proportion of participants who were ineligible for medical reasons after the telephone screen among all those who successfully completed the telephone screen and were scheduled for orientation (late medical ineligibility).
We conducted a series of t-tests to examine the effects of racial/ethnic group on the three dependent variables indicating rate of ineligibility (overall ineligibility, early ineligibility, and late ineligibility), and the three dependent variables indicating reason for ineligibility (overall medical ineligibility, early medical ineligibility, late medical ineligibility). A step-down Bonferroni procedure was used to adjust for multiple comparisons.
RESULTS
Site-Specific Results
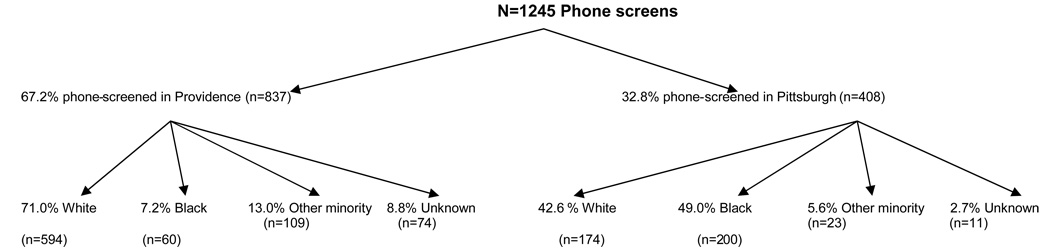
A breakdown of racial/ethnic groups by site is shown in Figure 2. As illustrated in the figure, 67% of the participants who were telephone-screened for the trial were from Providence. The Providence sample included 71% whites and 7% blacks. The more targeted approach in Pittsburgh yielded 43% whites and 49% blacks for the telephone-screening interview. The above percentages do not add to 100% due to the focus on (non-Hispanic) blacks and (non-Hispanic) whites in this manuscript.
FIGURE 2.
Racial/ethnic status of participants in the phone screen
Overall Ineligibility
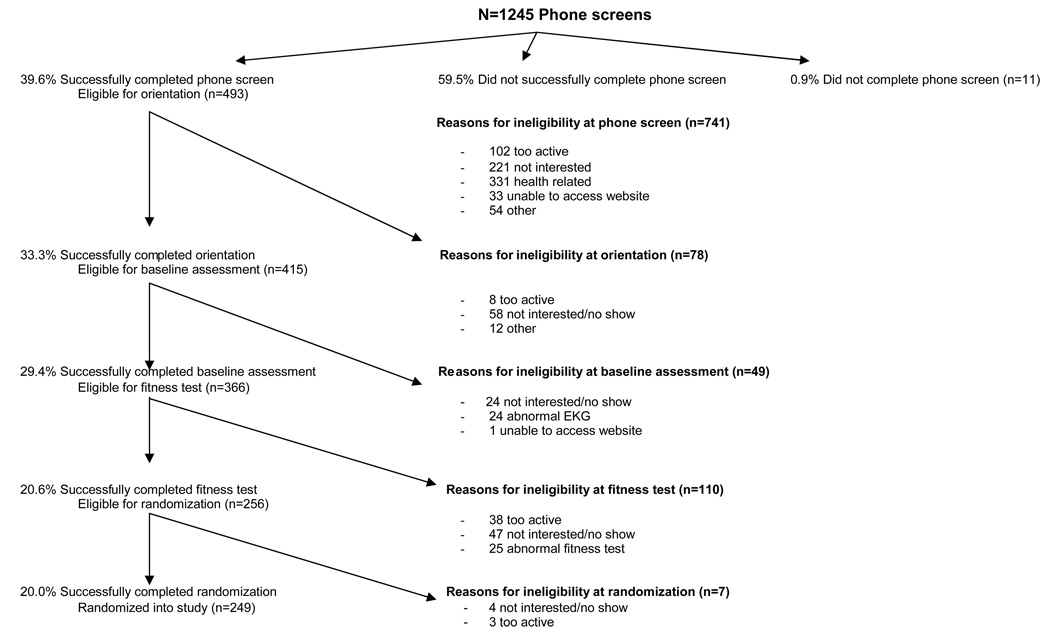
Among the 1245 participants who participated in the telephone screen 493 (39.6%) were eligible for the orientation session, 415 (33.3%) were eligible for the baseline assessment, 366 (29.4%) were eligible for a fitness test, 256 (20.6%) were eligible for randomization, and 249 (20.0%) successfully completed the randomization and enrolled in the study. Figure 3 shows the number of total participants who became ineligible at each stage of the screening process and reasons for ineligibility. Of the 741 participants who were immediately ineligible at the telephone screen, the most common reason for ineligibility was health-related (n = 331), followed by lack of interest (n = 221), being too active (n = 102), other reasons (n = 54), and unable to access the website (n = 33). After the telephone screen, the next time period where the most participants were found to be ineligible was at the fitness test (n = 110), where the reasons included not interested or did not show (n = 47), being too active (n = 38), and medical reasons (i.e., abnormal fitness test, n = 25).
FIGURE 3.
Eligibility status for all participants
Ineligibility by Racial Status
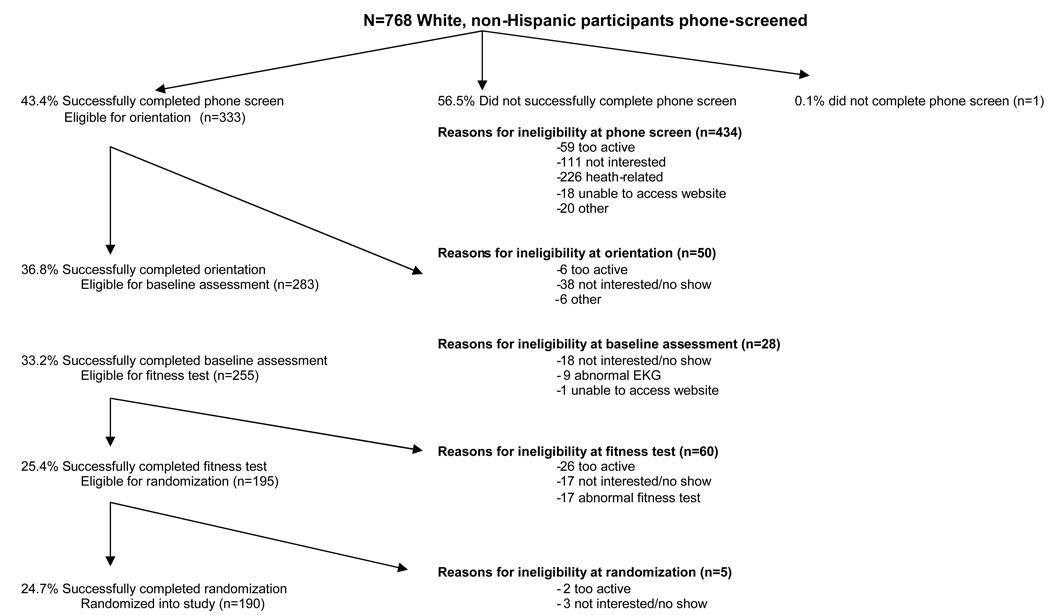
Figure 4 and Figure 5 show the pattern of participant ineligibility among whites and blacks. Analyses comparing ineligibility rates between blacks and whites (adjusted for multiple comparisons) showed blacks had higher rates of overall ineligibility (86.9% vs. 75.1%; p<.01), early ineligibility (64.6% vs. 56.5%; p =.02), and late ineligibility (63.0% vs. 42.9%; p<.01) than whites.
FIGURE 4.
Eligibility status for white participants
FIGURE 5.
Eligibility status for black participants
Medical Ineligibility
Of the 768 white participants who were telephone-screened, 252 (32.8%) were deemed ineligible to continue because of medical reasons at some point in the pre-randomization assessment process (Figure 4). Among the 260 black participants who were telephone-screened, 81 (31.2%) were deemed ineligible to continue because of medical reasons (Figure 5). While rates of overall and early medical ineligibility were not different for whites and blacks, consistent with our hypothesis, blacks had higher rates of late medical ineligibility (16.3% vs. 7.8%; p =.01) than whites. Table I shows the breakdown of specific health-related reasons regarding why these participants could no longer continue in the recruitment process. Of those ineligible at the telephone screen for medical reasons, the two most common reasons for ineligibility among black participants were cardiovascular or cerebrovascular disease, or BMI >35. Among white participants, the most common medical reasons were cardiovascular or cerebrovascular disease or musculoskeletal problems.
TABLE I.
Medical Reasons for Ineligibility at Phone Screen
| Specific Health Reasons for Ineligibility | Black (n=66) |
White (n=226) |
P |
|---|---|---|---|
| Cardiovascular or cerebrovascular disease | 28 (42.4%) | 93 (41.2%) | 0.86 |
| Chronic obstructive pulmonary disease | 3 (4.5%) | 18 (8.0%) | 0.33 |
| Acute or chronic medical problems | 4 (6.1%) | 37 (16.4%) | 0.03 |
| Musculoskeletal problems | 5 (7.6%) | 34 (15.0%) | 0.12 |
| Psychiatric conditions/medication(s) | 4 (6.1%) | 5 (2.2%) | 0.11 |
| Body mass index >35 | 21 (31.8%) | 13 (5.7%) | <0.01 |
| Prior fitness test, echocardiogram – did not obtain MD clearance | 1 (1.5%) | 26 (11.5%) | 0.01 |
| Total number ineligible for health reasons | 66 (100%) | 226 (100%) | 1.00 |
Note. Percentages represent fractions of column totals. P represents p-value for between group comparison.
Secondary Analyses
Because a large proportion of participants were ineligible due to lack of interest we also conducted secondary analyses comparing rates of disinterest between blacks and whites. In these analyses, lack of interest on the telephone screen was grouped together with no-shows for subsequent pre-randomization sessions, as the latter also indicated a lack of interest by participants. Analyses paralleled those for medical ineligibility in that we examined overall, early, and late disinterest rates. Results showed that blacks, as compared to whites, showed higher rates of overall disinterest (35.4% vs. 24.3%; p <.01), early disinterest (23.5% vs. 14.5%; p <.01), and late disinterest (33.7% vs. 22.8%; p =.03).
DISCUSSION
The goal of the present paper was to examine differences in ineligibility rates between whites and blacks. We hypothesized that a greater proportion of blacks would be excluded compared to whites. Including both sites, we successfully randomized 34 blacks (13.1% out of 260 initially interested) and 190 whites (24.7% of 768 initially interested). To be randomized, participants had to be eligible at 3–4 (depending on the recruitment site) pre-randomization assessments. As hypothesized, blacks were ineligible at higher rates than whites at all time points examined, including at the telephone screen, anytime after the telephone screen, and overall.
We further examined the reasons for these differences in ineligibility rates. Specifically, we hypothesized that a higher proportion of blacks would be excluded for medical reasons compared to whites. Results showed mixed support for our medical exclusion hypothesis, with roughly equal overall rates of medical ineligibility for blacks and whites. This is contrary to previous research in which racial/ethnic minorities were more likely to be excluded from randomized controlled trials due to co-morbid health conditions [7;16;22]. However, even though there were no differences between blacks and whites overall and for early medical eligibility, a greater proportion of blacks became ineligible for medical reasons sometime between orientation (first in-person visit) and randomization (last in-person visit prior to actual randomization) after successfully completing the telephone screen (i.e., late eligibility). Medical ineligibility after the initial phone screen but prior to randomization is not typically reported in studies examining minority recruitment. The present findings suggest that more stringent medical assessment criteria, such as the EKG and fitness test, may be more likely to differentially impact ineligibility among blacks than self-reported medical problems.
In that such a large proportion of participants were ineligible because they were not interested or failed to attend an assessment visit, we conducted secondary analyses to see if there were differences in disinterest between blacks and whites. The overall “not interested” rate for whites was 24% vs. 35% for blacks. Among the 221 participants who told us they were not interested at the time of the telephone screen, only 20 gave a specific reason. The most common reason was too busy or lack of time, followed by unwillingness to attend sessions at the research center, interest in a weight-loss or nutrition program, and desire for a more structured program instead of a lifestyle intervention. Unfortunately, we do not have data on why participants did not attend pre-randomization sessions following the initial telephone screen, and then failed to return our follow-up call. We assume that this was due to lack of interest; however, level of interest is relative to competing demands and interests. Thus, some participants may have not attended a session because they decided that they did not want to participate, while others may have wanted to participate, but had other competing demands/interests that had a higher priority. Additionally, the barriers experienced by racial/ethnic minorities, particularly the burden of appearing for multiple visits, not trusting or understanding research, and varied views about prevention, may have contributed to a lack of interest or even an inability to participate[11;13;21] [14;18]. Interestingly, not having a computer with a modem did not appear to be a common barrier in that only 3% of the black and 2% of the white participants were excluded for this reason.
In addition to difficulties keeping initially interested participants of racial/ethnic minority backgrounds in the screening and randomization process, we also had difficulty sparking initial interest among these groups. Despite targeting recruitment efforts to racial/ethnic minorities in Providence, and achieving a response from racial/ethnic minority callers (20.2%) that was fairly consistent with Providence demographics (23.6% racial minority [23]) we felt it necessary to extend recruitment to a more racially and ethnically diverse study site (i.e., Pittsburgh), in order to meet our study goal of 25% racial-ethnic minority enrollment. Rather than relying solely on passive recruitment methods used at the original study site [13], such as flyers and newspaper ads targeted to racial/ethnic groups, at the Pittsburgh site we also used more proactive recruitment approaches, such as contacting racial/ethnic minorities via personal letters. Even though some of these efforts to recruit racial/ethnic participants were not developed before the beginning of recruitment [9], we were able to utilize our research resources (during recruitment) by adding another site and using multiple strategies to recruit racial/ethnic participants (e.g., as suggested by [9;18;19]). As a result of our efforts, 54.6% of callers in Pittsburgh were of racial/ethnic background, which is well above the overall proportion of racial minorities in Pittsburgh (37.7% [23])
Taken together, nearly three times as many whites contacted us to learn more about the study than did blacks. We do not have data on why individuals from the community did not show initial interest in the study. However, the barriers to recruiting racial/ethnic minorities such as mistrust of research [21], lack of understanding about research [14], and lack of perceived risk of health problems [15], as well as competing demands [4], may help to explain why fewer racial/ethnic minorities responded to our advertisements and announcements. Additionally, we may have been unable to recruit a larger proportion of the Hispanic-Latino population because of language barriers and limited bilingual staff. In addition to the potential barriers listed above, it is also possible that the physical activity programs being tested do not appeal to racial/ethnic minorities. For example, previous research has shown that members of racial/ethnic minority groups are less likely to value preventive interventions for health promotion [11].
Due to the small number of participants from non-African-American minority groups (e.g., Hispanic whites, Hispanic blacks), we were not able to closely examine ineligibility among these groups. Future research should examine differences in recruitment rates among diverse groups of racial/ethnic minorities. We must continue to address the reasons why multiple racial/ethnic minority groups are less likely to participate in randomized controlled trials. For example, we plan to look more closely at barriers to initial response to our targeted ads so that we can develop and effectively test appropriate proactive recruitment strategies, such as building relationships and working with racial/ethnic communities. For example, some of the recruitment literature [8,9;14–17;19] use multiple strategies to recruit [18], and home health parities [8] for racial/ethnic minorities. This literature suggests the following strategies can increase accrual rates: 1) having culturally-sensitive staff, 2) hiring race-matched staff, 3) developing a community advisory board, 4) incorporating members from the community as part of the research assessor team, 5) advertising through culturally-relevant venues, 6) gaining “buy-in” from the community prior to the start of the study (e.g., pre-study meetings), 7) working with minority-focused organizations (e.g., National Black Initiative), and 8) developing a minority and medically underserved subcommittee. Many of these strategies are addressed in Paskett and colleagues’ [4] 8 categories of recruitment strategies for African Americans in cancer control and prevention trials (e.g., adequately characterize the target population, improve staff sensitivity, identify and remove barriers to participation, give something back to the community, and enhance credibility of study by using a community stakeholder).
One health promotion study found that a proactive recruitment approach (in-person appeals by study staff and health care providers) versus a reactive recruitment approach (advertisements and flyers asking participants to call a study hotline) was much more expensive ($159 per enrollee versus $22 per enrollee) [28]. As a result, the authors suggest a mixed approach, with reactive strategies added to some proactive strategies as a more efficient and cost-effective means of recruiting minority participants. Thus, although we would recommend the proactive strategies listed above, it may also be necessary to develop culturally-tailored reactive advertisements to supplement the more intensive efforts.
Finally, it is important to note that in the absence of random sampling of potential participants from each of the racial/ethnic groups, there is the potential for selection bias. That is, given that potential participants may have been exposed to recruitment through various media (e.g., newspaper, radio, minority targeted), by different research staff, in different cities, the differences in ineligibility among racial/ethnic groups could be a function of the various methods used to recruit these groups. Therefore, the present findings should be used to generate hypotheses for future research in this area, including more controlled experimental studies and studies using random sampling techniques in order to fully understand these important issues.
The main goal of this randomized controlled trial was to examine the differential effects of the Internet versus print materials to promote physical activity. This required a focus on maximizing internal validity. When a research team focuses their efforts on internal validity, external validity and generalizability can be diminished. Given the criticisms raised about lack of generalizability from homogenous samples [29], the National Institutes of Health’s goal of increasing minority recruitment is laudable to help improve minority participation in research. However, numerous barriers and challenges exist for reaching this recruitment goal. Our study found that a higher percentage of blacks were ineligible for our study than whites and that this was more likely to be due to a lack of interest than to medical conditions. This finding suggests that it may be most important to invest in strategies that enhance interest among blacks who initially respond to recruitment advertising. Thus, developing ways to explain the study protocol clearly and giving ample opportunities for participants to ask questions could be critical to retaining the interest and trust of racial/ethnic minorities. We recommend, like other researchers in the cancer prevention and control literature [6;7], that more researchers document and report minority recruitment efforts to better understand the barriers that exist for minorities to participate in health promotion research. The documentation and effective testing of racial/ethnic recruitment efforts are extremely important in health promotion studies with multiple pre-randomization assessments that increase internal validity but may contribute to greater recruitment barriers for underrepresented samples.
Acknowledgments
This research was supported in part through a grant from the National Heart, Lung, and Blood Institute (#HL69866). The authors acknowledge the contributions of Drs. Abby King, Deborah Tate, and Christopher Sciamanna in the design of this study. We also thank Maureen Hamel, B.S., Jaime Longval, M.S., Kenny McParlin, and Susan Recruiting Diverse Participant Samples Pinheiro, B.A., for their contributions to the conduct of this study. A special thank you to Ginny Shead and Melba Morrow for editorial assistance in preparing the manuscript.
Footnotes
Because only non-Hispanic participants were included in the statistical analysis, for the remainder of the manuscript, we use the terms “black” and “white” to refer to non-Hispanic black and non-Hispanic white, respectively.
Conflicts of Interest
None.
Contributor Information
Georita M Frierson, Southern Methodist University.
David M. Williams, Alpert Medical School of Brown University and The Miriam Hospital Centers for Behavioral and Preventive Medicine
Shira Dunsiger, Brown University, Program in Public Health
Beth A. Lewis, University of Minnesota – Twin Cities
Jessica A. Whiteley, Alpert Medical School of Brown University and The Miriam Hospital Centers for Behavioral and Preventive Medicine
Anna E. Albrecht, Alpert Medical School of Brown University and The Miriam Hospital Centers for Behavioral and Preventive Medicine
John M. Jakicic, University of Pittsburgh, Department of Health and Physical Activity
Santina M. Horowitz, The Miriam Hospital Centers for Behavioral and Preventive Medicine.
Bess H. Marcus, Brown University, Program in Public Health
Reference List
- 1.Healthy People 2010. U S Department of Health and Human Services. 2006 Available from: URL: http://www.healthypeople.gov/document/html/objectives/22-02.htm.
- 2.Hohmann AA, Parron DL. How the new NIH Guidelines on Inclusion of Women and Minorities apply: efficacy trials, effectiveness trials, and validity. J Consult Clin Psychol. 1996 Oct;64(5):851–855. doi: 10.1037//0022-006x.64.5.851. [DOI] [PubMed] [Google Scholar]
- 3.Paskett ED, DeGraffinreid C, Tatum CM, Margitic SE. The recruitment of African-Americans to cancer prevention and control studies. Prev Med. 1996 Sep;25(5):547–553. doi: 10.1006/pmed.1996.0088. [DOI] [PubMed] [Google Scholar]
- 4.Paskett ED, Katz ML, DeGraffinreid CR, Tatum CM. Participation in cancer trials: recruitment of underserved populations. Clin Adv Hematol Oncol. 2003 Oct;1(10):607–613. [PubMed] [Google Scholar]
- 5.Lai GY, Gary TL, Tilburt J, Bolen S, Baffi C, Wilson RF, et al. Effectiveness of strategies to recruit underrepresented populations into cancer clinical trials. Clin Trials. 2006;3(2):133–141. doi: 10.1191/1740774506cn143oa. [DOI] [PubMed] [Google Scholar]
- 6.Bolen S, Tilburt J, Baffi C, Gary TL, Powe N, Howerton M, et al. Defining "success" in recruitment of underrepresented populations to cancer clinical trials: moving toward a more consistent approach. Cancer. 2006 Mar 15;106(6):1197–1204. doi: 10.1002/cncr.21745. [DOI] [PubMed] [Google Scholar]
- 7.Ford JG, Howerton MW, Lai GY, Gary TL, Bolen S, Gibbons MC, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer. 2008 Jan 15;112(2):228–242. doi: 10.1002/cncr.23157. [DOI] [PubMed] [Google Scholar]
- 8.Robins SG, York C, Madlensky L, Gibson K, Wasserman L, Rosenthal E, et al. Health parties for African American study recruitment. J Cancer Educ. 2006;21(2):71–76. doi: 10.1207/s15430154jce2102_6. [DOI] [PubMed] [Google Scholar]
- 9.Cook ED, Moody-Thomas S, Anderson KB, Campbell R, Hamilton SJ, Harrington JM, et al. Minority recruitment to the Selenium and Vitamin E Cancer Prevention Trial (SELECT) Clin Trials. 2005;2(5):436–442. doi: 10.1191/1740774505cn111oa. [DOI] [PubMed] [Google Scholar]
- 10.Ford JG, Howerton MW, Bolen S, Gary TL, Lai GY, Tilburt J, et al. Knowledge and access to information on recruitment of underrepresented populations to cancer clinical trials. Evid Rep Technol Assess (Summ ) 2005 Jun;(122):1–11. doi: 10.1037/e439572005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blumenthal DS, Sung J, Coates R, Williams J, Liff J. Recruitment and retention of subjects for a longitudinal cancer prevention study in an inner-city black community. Health Serv Res. 1995 Apr;30(1 Pt 2):197–205. [PMC free article] [PubMed] [Google Scholar]
- 12.Banks-Wallace J, Enyart J, Johnson C. Recruitment and entrance of participants into a physical activity intervention for hypertensive African American women. ANS Adv Nurs Sci. 2004 Apr;27(2):102–116. doi: 10.1097/00012272-200404000-00004. [DOI] [PubMed] [Google Scholar]
- 13.White RM. Misrepresentations of the Tuskegee Study of Untreated Syphilis. J Natl Med Assoc. 2005 Apr;97(4):564–581. [PMC free article] [PubMed] [Google Scholar]
- 14.Larson E. Exclusion of certain groups from clinical research. Image J Nurs Sch. 1994;26(3):185–190. doi: 10.1111/j.1547-5069.1994.tb00311.x. [DOI] [PubMed] [Google Scholar]
- 15.O'Brien RL, Kosoko-Lasaki O, Cook CT, Kissell J, Peak F, Williams EH. Self-assessment of cultural attitudes and competence of clinical investigators to enhance recruitment and participation of minority populations in research. J Natl Med Assoc. 2006 May;98(5):674–682. [PMC free article] [PubMed] [Google Scholar]
- 16.Dunbar-Jacob J, Holmes JL, Sereika S, Kwoh CK, Burke LE, Starz TW, et al. Factors associated with attrition of African Americans during the recruitment phase of a clinical trial examining adherence among individuals with rheumatoid arthritis. Arthritis Rheum. 2004;51:422–428. doi: 10.1002/art.20411. [DOI] [PubMed] [Google Scholar]
- 17.Escobar-Chaves SL, Tortolero SR, Masse LC, Watson KB, Fulton JE. Recruiting and retaining minority women: findings from the Women on the Move study. Ethn Dis. 2002;12(2):242–251. [PubMed] [Google Scholar]
- 18.Margitic S, Sevick MA, Miller M, Albright C, Banton J, Callahan K, et al. Activity Counseling Trial Research Group. Challenges faced in recruiting patients from primary care practices into a physical activity intervention trial. Prev Med. 1999 Oct;29(4):277–286. doi: 10.1006/pmed.1999.0543. [DOI] [PubMed] [Google Scholar]
- 19.Eakin EG, Bull SS, Riley K, Reeves MM, Gutierrez S, McLaughlin P. Recruitment and retention of Latinos in a primary care-based physical activity and diet trial: The Resources for Health study. Health Educ Res. 2007 Jun;22(3):361–371. doi: 10.1093/her/cyl095. [DOI] [PubMed] [Google Scholar]
- 20.Staffileno BA, Coke LA. Recruiting and retaining young, sedentary, hypertension-prone African American women in a physical activity intervention study. J Cardiovasc Nurs. 2006 May;21(3):208–216. doi: 10.1097/00005082-200605000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Freimuth VS, Quinn SC, Thomas SB, Cole G, Zook E, Duncan T. African Americans' views on research and the Tuskegee Syphilis Study. Soc Sci Med. 2001 Mar;52(5):797–808. doi: 10.1016/s0277-9536(00)00178-7. [DOI] [PubMed] [Google Scholar]
- 22.Adams-Campbell LL, Ahaghotu C, Gaskins M, Dawkins FW, Smoot D, Polk OD, et al. Enrollment of African Americans onto clinical treatment trials: study design barriers. J Clin Oncol. 2004 Feb 15;22(4):730–734. doi: 10.1200/JCO.2004.03.160. [DOI] [PubMed] [Google Scholar]
- 23.U.S. Census Bureau, 2004 American Community Survey. 2006. [Google Scholar]
- 24.Pereira MA, FitzGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR, et al. A collection of physical activity questionnaires for health-related research. Med Sci Sports Exerc. 1997 Jun;29(6 Suppl):S1–S205. [PubMed] [Google Scholar]
- 25.American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 26.Marcus BH, Rossi JS, Selby VC, Niaura RS. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psych. 1992;11:386–395. doi: 10.1037//0278-6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- 27.Marcus BH, Simkin LR. The stages of exercise behavior. J Sports Med Phys Fitness. 1993;33:83–88. [PubMed] [Google Scholar]
- 28.Harris KJ, Ahluwalia JS, Catley D, Okuyemi KS, Mayo MS, Resnicow K. Successful recruitment of minorities into clinical trials: The Kick It at Swope project. Nicotine Tob Res. 2003 Aug;5(4):575–584. doi: 10.1080/1462220031000118540. [DOI] [PubMed] [Google Scholar]
- 29.Dzewaltowski DA, Estabrooks PA, Klesges LM, Bull S, Glasgow RE. Behavior change intervention research in community settings: how generalizable are the results? Health Promot Int. 2004 Jun;19(2):235–245. doi: 10.1093/heapro/dah211. [DOI] [PubMed] [Google Scholar]