Dear Sir,
Induction of melanogenesis by ultraviolet radiation (UV) is a relatively slow process (Tadokoro et al., 2003; Tadokoro et al., 2005; Yamaguchi et al., 2008). UV-induces immediate pigment darkening (within minutes, remaining for hours) (Honigsmann et al., 1986; Routaboul et al., 1999), persistent pigment darkening (within hours, remaining for days) (Moyal et al., 2000; Moyal et al., 2006), and delayed pigmentation (within in days, remaining for weeks) (Ortonne, 1990; Tadokoro et al., 2003; Tadokoro et al., 2005; Young, 2006).
The majority of humans lose UV-induced pigmentation (tan) within a relatively short time, however a significant segment of the population maintains such pigmentation for many months. However, no systematic studies of long-lasting pigmentation (LLP) have been reported. Anecdotally, people know that pigmentation persists after UV exposure as “tan lines”, but the mechanism of this extended pigmentary response has not been elucidated. A literature search revealed only one study reporting pigmentation remaining 6 months after exposure to two minimal erythema doses (MED)(Suh et al., 2007).
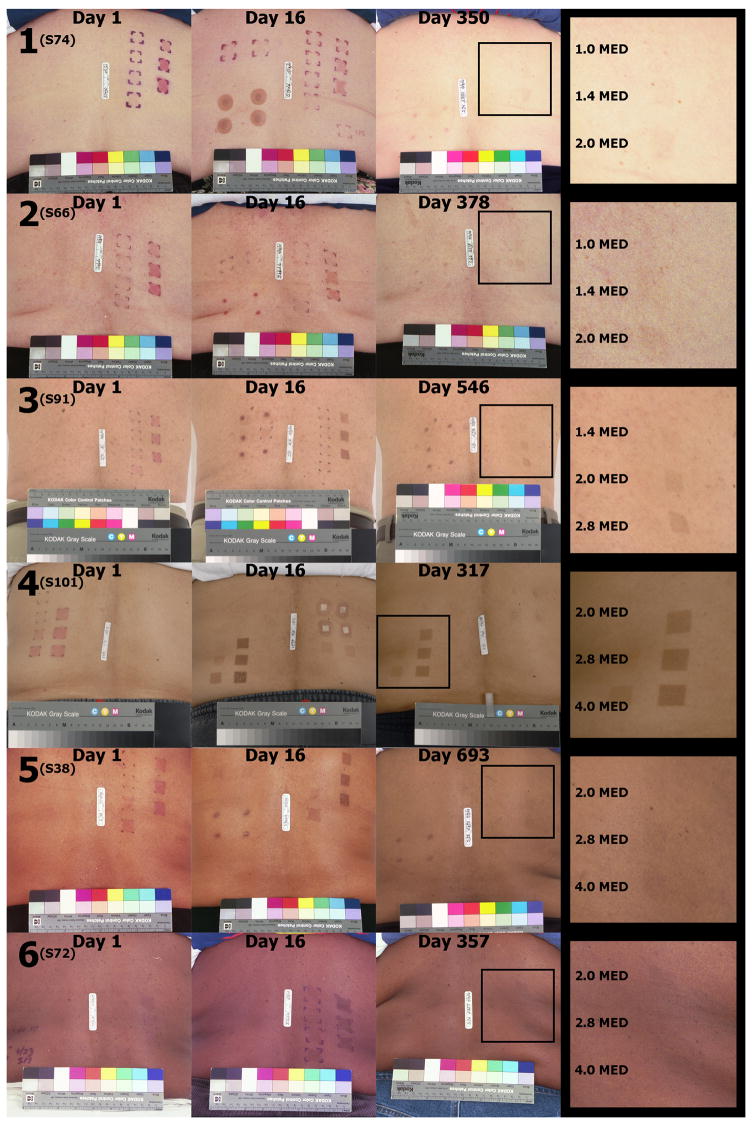
We analyzed the persistence of UV-induced pigmentation in humans of different complexion (Figure 1) and analyzed factors that may predispose to LLP. We explored parameters that included gender, age, eye color, hair color, MED, minimal melanogenic dose (MMD), phototype, race/ethnicity, and constitutive pigmentation. Figure 2 shows that virtually all subjects exposed to ≥2 MED developed early pigmentation with a grade of ≥1 on a scale 0–4 (Table S1). A proportion of these subjects showed a pigmentation grade ≥1 at ≥9 months post-exposure. LLP+ subjects typically develop a strong pigmentation within days after UV exposure. This pigmentation remains robust on post-exposure day 16 (Figure 1). Induction of LLP depends on the UV exposure level: only a few our subjects developed LLP after 1 MED, but at 2 MED the proportion of LLP+ subjects was substantial, and it increased with increasing UV dose.
Figure 1.
LLP ≥9 months after ultraviolet (UV) exposure in six phototypes (1 - Burns easily, never tans; 2 - Burns easily, tans slightly; 3 - Burns slightly, tans light brown; 4 -Burns slightly, tans moderate brown; 5 - Burns rarely, tans dark brown; 6 Never burns, tans black). The black squares show the areas with LLP, enlarged on the right side with doses in multiples of MED included. The subject numbers are given in parentheses.
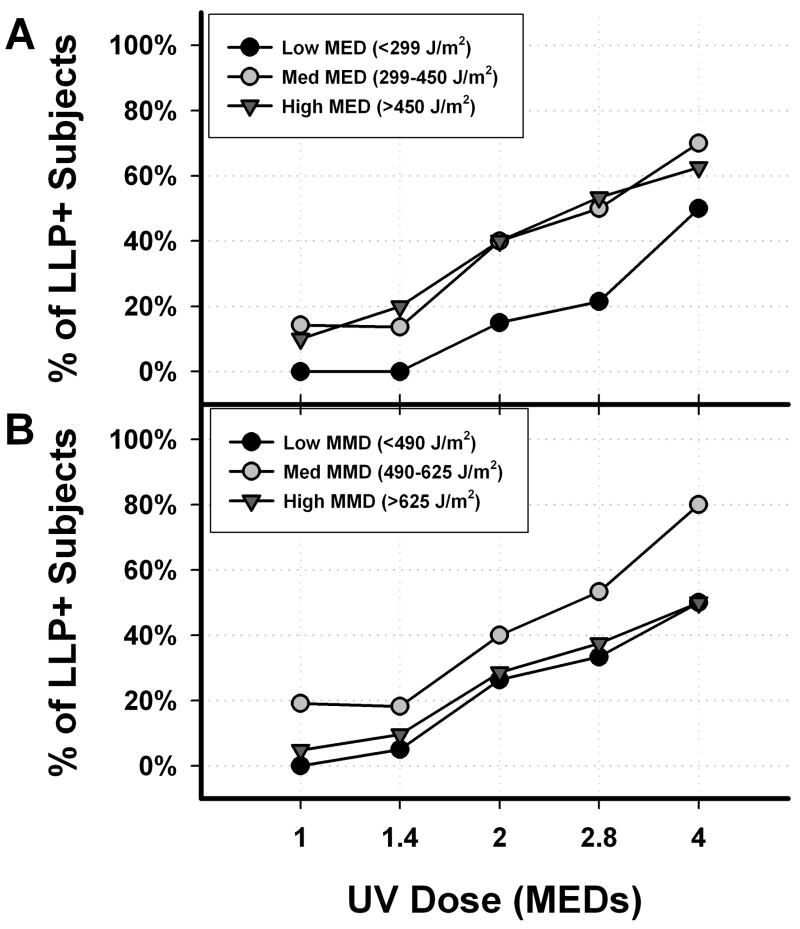
Figure 2.
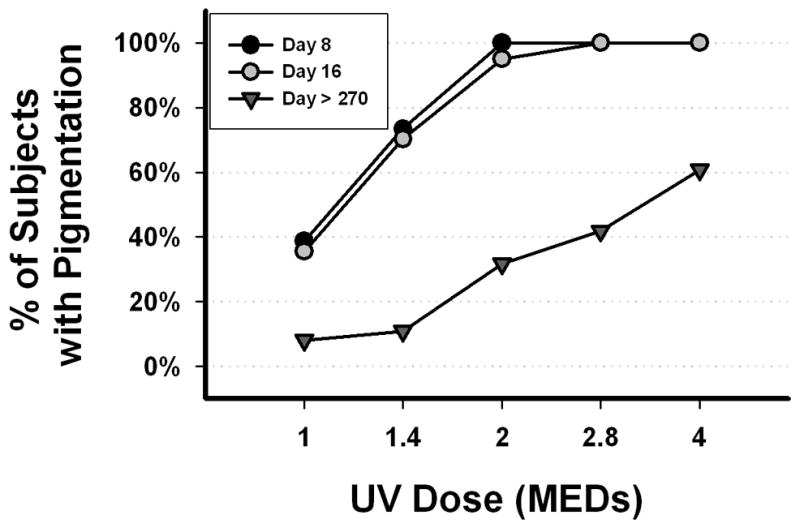
Pigmentation after 1–4 MED of UV.
Correlations between LLP+ occurrence and the three MED ranges, as defined in Appendix S1, were pronounced (Table 1 and Figure 3A). No subjects with MED <299 J/m2 showed LLP after exposure to <2 MED. Subjects in the higher MED ranges exposed to >2 MED showed LLP frequency of 40–70%. The “Unequally Spaced Repeated Measures Linear Model” (Appendix S1) demonstrated a statistically significant difference from zero, with p<0.0001, for the independent variable MED. Figure 3B shows frequency of LLP+ subjects in three MMD ranges (Appendix S1). Subjects with higher MMD values were more likely to develop LLP than those with lower MMD values, with statistically significant difference from zero and p=0.0001. The LLP+ response increased linearly with increasing age, over all ages (statistically significant difference from zero in predicting LLP, p<0.005). Hence, LLP depends more on MED or MMD than on increasing age. One might expect that propensity to LLP correlates with constitutive pigmentation, phototype, or race/ethnicity. However, we found no statistically significant effect of these parameters on the frequency of the LLP occurrence. The melanin content expressed in mg eumelanin per ml was not always higher in LLP+ than in LLP- subjects, and showed considerable variability (Table 1).
Table 1.
LLP Occurrence at Increasing Exposure Levels Sorted by Gender, MED range, MMD range, and the average constitutive melanin content (mg of eumelanin per ml).
| Multiple of MED Groups 1 | LLP | Gender | MED Range (J/m2) | MMD Range (J/m2) 2 | Constitutive Pigmentation | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low | Med | High | Low | Med | High | Eumelanin (mg/ml) | ||||
| Female | Male | < 299 | 299–450 | > 450 | < 490 | 490–625 | > 625 | Mean ± SEM | ||
|
| ||||||||||
| 1.0 MED (n=62) | − | 37 | 20 | 21 | 18 | 18 | 19 | 17 | 20 | 4.80 ± 0.71 |
| + | 3 | 2 | 0 | 3 | 2 | 0 | 4 | 1 | 6.51 ± 4.20 | |
| % | 8% | 9% | 0% | 14% | 10% | 0% | 19% | 5% | ||
|
| ||||||||||
| 1.4 MED (n=64) | − | 36 | 21 | 22 | 19 | 16 | 19 | 18 | 19 | 4.97 ± 0.78 |
| + | 5 | 2 | 0 | 3 | 4 | 1 | 4 | 2 | 4.14 ± 1.07 | |
| % | 12% | 9% | 0% | 14% | 20% | 5% | 18% | 10% | ||
|
| ||||||||||
| 2.0 MED (n=60) | − | 24 | 17 | 17 | 12 | 12 | 14 | 12 | 15 | 5.01 ± 0.92 |
| + | 16 | 3 | 3 | 8 | 8 | 5 | 8 | 6 | 5.11 ± 1.31 | |
| % | 40% | 15% | 15% | 40% | 40% | 26% | 40% | 29% | ||
|
| ||||||||||
| 2.8 MED (n=43) | − | 13 | 12 | 11 | 7 | 7 | 8 | 7 | 10 | 5.11 ± 1.14 |
| + | 14 | 4 | 3 | 7 | 8 | 4 | 8 | 6 | 6.87 ± 1.61 | |
| % | 52% | 25% | 21% | 50% | 53% | 33% | 53% | 38% | ||
|
| ||||||||||
| 4.0 MED (n=28) | − | 5 | 6 | 5 | 3 | 3 | 5 | 2 | 4 | 5.79 ± 1.83 |
| + | 12 | 5 | 5 | 7 | 5 | 5 | 8 | 4 | 5.71 ± 1.36 | |
| % | 71% | 45% | 50% | 70% | 63% | 50% | 80% | 50% | ||
- The “n” refers to the number of subjects who received the specific dose out of total of 64 subjects.
- Subject 7 was excluded here because they did not receive a dose large enough to produce a MMD value.
Figure 3.
Increasing MED, MMD, and frequency of LLP induction. (A) MED ranges, (B) MMD ranges - as defined in Appendix S1. Total number of subjects, 64; data for 62, 64, 60, 43, and 28 subjects at 1, 1.4, 2, 2.8, and 4 MED, respectively.
Photographs of the study areas on the backs of subjects representing the six phototypes are shown in Figure 1. Clearly, the LLP is more pronounced in darker phototypes but, with time, minimal perceptible pigmentation becomes harder to discern in the darker skin. Phototypes 1 and 2 showed the lowest, and phototypes 5 and 6 the highest tendency to be LLP+. LLP+ response occurred in all five racial/ethnic groups studied; however the number of subjects was too small to analyze the effects of race/ethnicity on predisposition to LLP.
Our observations indicate that after UV exposure humans can be divided into three classes: those who never develop pigmentation, those who develop pigmentation but lose it within 9 months and those who develop pigmentation that persists for at least 9 months (LLP). During that time, the pigmentation fades to varying degrees in different LLP+ subjects, nevertheless it remains visible. In our study, 32% of subjects showed LLP after ≥2 MED, while 61% had a LLP response after 4 MED. Our results are consistent with reports of LLP in Korean individuals (phototypes 3–5) up to 6 months after 2 MED (Suh et al., 2007). High MED and MMD values are the best predictors of LLP. Also, advancing age may facilitate LLP induction. The relationship of race/ethnicity to LLP needs further evaluation in a larger cohort. We found no statistically significant indication that LLP is related to gender, eye color, hair color, phototype, or constitutive pigmentation (melanin content by reflectance spectroscopy). Clear correlations between MED or MMD with LLP and lack of correlation between phototype and propensity for LLP confirm our earlier conclusions regarding the superiority of MED as a human photosensitivity criterion (Tadokoro et al., 2003).
UV-induced pigmentation could remain visible for a long time if (1) desquamation of the epidermis is retarded or (2) the activity of the melanogenic system remains elevated. It is important to determine if any or both of these mechanisms (or still another process) is involved since benefits and risks of LLP are unknown and may be significant. On one hand, increased pigmentation may be photoprotective (Yamaguchi et al., 2008; Young, 2006). However, if prolonged activation of the melanogenic system is involved, there is potential risk of uncontrolled proliferation that might lead to melanoma (Gilchrest et al., 1979). Further studies should help to define risks and benefits of LLP, and innovative approaches have been proposed (Aoki et al., 2007; Procaccini et al., 2007). Preliminary explorations in this area have just been reported (Brenner et al., 2009).
Better understanding of LLP should be sought to answer the following critical questions:
Do any changes in the desquamation rate occur in the skin with LLP?
Is the spectrum of UV-activated melanogenic factors the same in LLP+ and LLP-skin?
Is the sequence of activation of melanogenic factors altered in skin with LLP?
How persistent is the activation of different melanogenic factors?
Supplementary Material
Acknowledgments
This research was supported by the Office of Science and the Center for Devices and Radiological Health, Food and Drug Administration, and in part by the Intramural Research Program of the National Cancer Institute, National Institutes of Health. The authors wish to express their appreciation to Dr. Katalin S. Korossy and to Julia A. Kniskern, RN, for their dedication and critical contributions to this study.
References
- Aoki H, Moro O, Tagami H, Kishimoto J. Gene expression profiling analysis of solar lentigo in relation to immunohistochemical characteristics. Br J Dermatol. 2007;156:1214–1223. doi: 10.1111/j.1365-2133.2007.07830.x. [DOI] [PubMed] [Google Scholar]
- Brenner M, Coelho SG, Beer JZ, Miller SA, Wolber R, Smuda C, Hearing VJ. Long-Lasting Molecular Changes in Human Skin after Repetitive In Situ UV Irradiation. J Invest Dermatol. 2009;129:1002–11. doi: 10.1038/jid.2008.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilchrest BA, Blog FB, Szabo G. Effects of aging and chronic sun exposure on melanocytes in human skin. J Invest Dermatol. 1979;73:141–143. doi: 10.1111/1523-1747.ep12581580. [DOI] [PubMed] [Google Scholar]
- Honigsmann H, Schuler G, Aberer W, Romani N, Wolff K. Immediate pigment darkening phenomenon. A reevaluation of its mechanisms. J Invest Dermatol. 1986;87:648–652. doi: 10.1111/1523-1747.ep12456326. [DOI] [PubMed] [Google Scholar]
- Moyal D, Chardon A, Kollias N. Determination of UVA protection factors using the persistent pigment darkening (PPD) as the end point. (Part 1) Calibration of the method. Photodermatol Photoimmunol Photomed. 2000;16:245–249. doi: 10.1034/j.1600-0781.2000.160602.x. [DOI] [PubMed] [Google Scholar]
- Moyal D, Wichrowski K, Tricaud C. In vivo persistent pigment darkening method: a demonstration of the reproducibility of the UVA protection factors results at several testing laboratories. Photodermatol Photoimmunol Photomed. 2006;22:124–128. doi: 10.1111/j.1600-0781.2006.00223.x. [DOI] [PubMed] [Google Scholar]
- Ortonne JP. The effects of ultraviolet exposure on skin melanin pigmentation. J Intl Med Res. 1990;18:8C–17C. [PubMed] [Google Scholar]
- Procaccini EM, Napolitano A, Panzella L, Prizio E, Monfrecola G. Long-lasting pigmentation more than its intensity is a reliable indicator of skin sun resistance. Dermatology. 2007;215:173–179. doi: 10.1159/000106572. [DOI] [PubMed] [Google Scholar]
- Routaboul C, Denis A, Vinche A. Immediate pigment darkening: description, kinetic and biological function. Eur J Dermatol. 1999;9:95–99. [PubMed] [Google Scholar]
- Suh KS, Roh HJ, Choi SY, Jeon YS, Doh KS, Bae JH, Kim ST. Long-term evaluation of erythema and pigmentation induced by ultraviolet radiations of different wavelengths. Skin Res Technol. 2007;13:154–161. doi: 10.1111/j.1600-0846.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- Tadokoro T, Kobayashi N, Zmudzka BZ, Ito S, Wakamatsu K, Yamaguchi Y, Korossy KS, Miller SA, Beer JZ, Hearing VJ. UV-induced DNA damage and melanin content in human skin differing in racial/ethnic origin. FASEB J. 2003;17:1177–1179. doi: 10.1096/fj.02-0865fje. [DOI] [PubMed] [Google Scholar]
- Tadokoro T, Yamaguchi Y, Batzer J, Coelho SG, Zmudzka BZ, Miller SA, Wolber R, Beer JZ, Hearing VJ. Mechanisms of skin tanning in different racial/ethnic groups in response to ultraviolet radiation. J Invest Dermatol. 2005;124:1326–1332. doi: 10.1111/j.0022-202X.2005.23760.x. [DOI] [PubMed] [Google Scholar]
- Yamaguchi Y, Coelho SG, Zmudzka BZ, Takahashi K, Beer JZ, Hearing VJ, Miller SA. Cyclobutane pyrimidine dimer formation and p53 production in human skin after repeated UV irradiation. Exp Dermatol. 2008;17:916–924. doi: 10.1111/j.1600-0625.2008.00722.x. [DOI] [PubMed] [Google Scholar]
- Young AR. Acute effects of UVR on human eyes and skin. Prog Biophys Mol Biol. 2006;92:80–85. doi: 10.1016/j.pbiomolbio.2006.02.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.