Abstract
Background
The Generalized Anxiety Disorder Severity Scale (GADSS) is an interview rating scale designed specifically for assessing symptom severity of generalized anxiety disorder (GAD), which has demonstrated positive psychometric data in a sample of adult primary care patients with GAD and panic disorder. However, the psychometric properties of the GADSS have not been evaluated for older adults.
Methods
This study evaluated the psychometric properties of the GADSS, administered via telephone, with a sample of older primary care patients (n = 223) referred for treatment of worry and/or anxiety.
Results
The GADSS demonstrated adequate internal consistency, strong inter-rater reliability, adequate convergent validity, poor diagnostic accuracy, and mixed discriminant validity.
Conclusions
Results provide mixed preliminary support for use of the GADSS with older adults. Depression and Anxiety 26:E10–E15, 2009.
Keywords: Generalized Anxiety Disorder Severity Scale, generalized anxiety disorder, elderly, primary care, measurement, psychometrics
INTRODUCTION
Anxiety disorders occur commonly among the elderly, with an overall prevalence of 10.2%.[1] Generalized anxiety disorder (GAD), primarily characterized by excessive and uncontrollable worry accompanied by physical symptoms (e.g., muscle tension, irritability, sleep disturbance[2]), is one of the most common disorders among older adults, with prevalence as high as 7.3%,[1] second only to specific phobia.[3,4] Late-life GAD is also common in primary care settings, where older adults with mental health concerns are most likely to present for care, with prevalence ranging from 3.1[5] to 11.2%.[6] Anxiety in later life is associated with poor quality of life,[7,8] increased service use),[9] increased comorbidity,[10] a high degree of physical disability,[11] and sleep disturbances.[7]
Despite high prevalence and substantial impact of GAD in older adults, a dearth of instruments adequately assesses symptom severity of the disorder, especially among older adults. A well-established measure of GAD symptom severity would be useful for assessing diagnostic severity, treatment planning, case conceptualization, and tracking treatment progress. Measures used most often in recent research include the Penn State Worry Questionnaire (PSWQ)[12] and the Hamilton Rating Scale for Anxiety (HAM-A).[13] The PSWQ, however, is a self-report measure that includes an over-reliance on the “core symptom” of worry and therefore omits consideration of somatic symptoms that may be particularly significant to the evaluation of GAD in older adults.[14] Other self-report measures designed specifically for use with the elderly are the Worry Scale (WS), which assesses worry severity in three different content categories,[15] and the Geriatric Anxiety Inventory (GAI).[16] The WS, however, also omits evaluation of somatic symptoms, and the GAI assesses a broad range of anxiety symptoms not specific to GAD. The HAM-A is a clinician-rated instrument that assesses both somatic and psychological symptoms, but the measure is not specifically designed to evaluate severity of GAD symptoms according to diagnostic criteria. Thus, a more useful assessment instrument might focus on a comprehensive clinician-rated inquiry of DSM-based symptoms and severity.
One relatively new measure with particular promise for evaluation of GAD symptoms is the Generalized Anxiety Disorder Severity Scale (GADSS), an interview rating scale designed specifically for assessment of GAD symptom severity.[17] The utility of this measure was originally evaluated in the context of a randomized controlled effectiveness trial for younger primary care patients with GAD and panic disorder.[18] In this context, the telephone-administered GADSS had excellent internal consistency, construct validity, convergent validity, divergent validity and sensitivity to change, and a unifactorial structure.[17]
The utility of the GADSS, however, has not been evaluated for older adults. This measure may be particularly useful in overcoming logistic issues for older adults, as it can be easily administered via telephone and can save time and resources. It may also be valuable as an outcome measure in treatment trials with older adults as it focuses specifically on symptom severity within DSM-based criteria. No other tool like this has yet been used in the growing body of treatment outcome work with late-life anxiety.[19] However, the psychometric properties of the GADSS are unknown among older adults. The goal of this study is to examine the psychometric properties of the measure in a sample of older patients presenting for evaluation and treatment of anxiety in primary care. Consistent with prior research on validation of measures in late-life research[9,20] the GADSS was expected to have psychometric properties in older adults that are comparable to those in younger adults. Specifically, we expected comparable internal consistency, inter-rater reliability, convergent and divergent validity, factor structure, and discriminant validity.
METHODS
PARTICIPANTS
Participants were 223 older primary care patients, 140 with a principal (n = 134) or coexistent (n = 6) diagnosis of GAD and 83 without a diagnosis of GAD.1 The sample consisted of 165 women (74%) and 58 men (26%), and mean age was 67.5 years (SD = 6.09). Participants were well educated (M = 15.8 years of education [SD = 2.89]), and ethnic distribution was as follows: 165 Caucasians (74%), 48 African Americans (22%), 4 Asian Americans (2%), 3 of mixed heritage (1%), and 2 “ Other” (1%), and 1 failed to answer. With respect to occupational status, 123 were retired (55.2%), 49 employed full-time (22.0%), 32 employed part-time (14.3%), 9 homemaker (4.0%), 9 not employed (4.0%), and 1 (0.4%) missing. Physical health was average (M = 43.64, SD = 8.75).2 Participants with and without GAD did not differ with regard to gender, χ2 (1, n = 223) = 2.92, ns, age, t(221) = 1.85, ns; years of education, χ2 (10, n = 223) = 5.30, ns; ethnicity, χ2 (4, n = 223) = 3.53, ns; or physical health, t(221) = 0.47, ns. Most patients with GAD (73%) had at least one coexistent diagnosis: n = 66 (47%) mood disorder (including major depressive disorder, dysthymia, and depression not otherwise specified); n = 38 (27%) specific phobia; n = 17 (12%) social phobia; n = 5 (4%) posttraumatic stress disorder; n = 4 (3%) panic disorder without agoraphobia; n = 6 (4%) panic disorder with agoraphobia; and 1% each, agoraphobia without panic disorder, adjustment disorder, somatization disorder, and depersonalization disorder. Of the 83 patients without GAD, 49 (59%) were diagnosed with another DSM disorder: n = 28 (34%) mood disorder (including major depressive disorder, dysthymia, and depression not otherwise specified); n = 12 (15%) specific phobia; n = 11 (13%) social phobia; n = 4 (5%) panic disorder without agoraphobia; n = 2 (2%) panic disorder with agoraphobia; n = 3 (4%) posttraumatic stress disorder; n = 8 (10%) anxiety disorder not otherwise specified; n = 2 (2%) adjustment disorder; and n = 1 (1%) somatization disorder. The remaining 34 patients without GAD had no DSM disorder.
Recruitment and inclusion
Participants were evaluated in the context of an ongoing randomized trial of cognitive-behavioral therapy for late-life GAD in primary care. Patients 60 years of age or older were recruited from local primary care clinics through physician referrals, letters of invitation to patients, and/or educational brochures that advertised an ongoing study focused on worry and anxiety. Of 968 primary care patients referred to the study for evaluation of worry, 858 were able to be contacted; and 381 signed consent to participate. Of participants who signed consent, 68 individuals voluntarily withdrew from the study before the in-person diagnostic session; and 57 withdrew after the in-person diagnostic session, but before the follow-up telephone assessment, leaving 256 who completed the initial assessment.
Screening
All referred patients were screened by telephone for symptoms of GAD using two questions from the Primary Care Evaluation of Mental Disorders[23] (“ During the past month, have you often been bothered by ‘nerves’ or ‘feeling anxious or on edge?” and “During the past month, have you often been bothered by worrying about a lot of different things?”). Patients who screened positive were administered the Structured Clinical Interview for the DSM-IV Axis I (SCID-I)[24] in person by research staff, postdoctoral fellows, predoctoral interns, and advanced psychology graduate students. Twenty-five percent of diagnostic interviews were reviewed by a second clinician or project investigator to estimate reliability of diagnostic categories. Inter-rater reliability was adequate: GAD, κ = .64; depression (including major depressive disorder, dysthymia, and depression not otherwise specified), κ = .75; and anxiety diagnoses other than GAD, κ = .73.[25]
Exclusion
Participants with cognitive impairment (as defined by a Mini-Mental State Exam[26] less than 24; n = 23), current psychosis or bipolar disorder (n = 1), or active substance abuse within the past month (n = 9) were excluded, resulting in a final sample of 223.
MEASURES
Anxiety
The GADSS [17] is a six-item, clinician-rated interview rating scale designed specifically for assessment of GAD symptom severity. Each item3 is rated on a 0-to-4 scale, and total scores range from 0 to 24. Items assess frequency of worries, distress due to worrying, frequency of associated symptoms, severity and distress because of associated symptoms, impairment/interferences in work functioning, and impairment/interference in social functioning. An initial psychometric investigation indicated that the GADSS, administered via telephone, had excellent internal consistency (α = .90) and demonstrated construct validity, convergent validity (r = .79 with the HAM-A), divergent validity (r = .52 with the Panic Disorder Severity Scale), sensitivity to change, and a unifactorial structure.[17]
The Structured Interview Guide for the HAM-A (SIGH-A)[27] is a 17-item, structured, clinician-rated instrument assessing severity of anxiety symptoms, based on the widely used HAM-A.[13] The SIGH-A attempts to increase standardization and improve consistency between raters; and the measure has been validated with medical patients, ranging in age from 19 to 68, meeting DSM-IV criteria for an anxiety disorder.[27] Preliminary evidence obtained via telephone interviews with the current sample suggests excellent inter-rater reliability for the SIGH-A (intraclass correlation coefficient [ICC] = .95).[28] Cronbach’s α was .79 for the current sample.
The (PSWQ)[12] is a 16-item self-report measure designed to assess an individual’s tendency to worry and perceived control over worry, regardless of worry content. Its utility with younger adults has been extensively studied.[29,30] Data suggest that the PSWQ displays adequate psychometric properties in older adult samples, including strong internal consistency, convergent validity, and divergent validity but questionable test-retest reliability.[20,21] Cronbach’s α was .90 for the current sample.
The Beck Anxiety Inventory (BAI)[31] is a 21-item self-report questionnaire assessing cognitive and somatic anxiety symptoms. Data on its use with older adults indicate good internal consistency with older-adult community-dwelling,[32] medical patient,[33] and psychiatric outpatient[34] samples; convergent validity with older adults with GAD[33] and a stable factor structure.[32,34] Cronbach’s α for the current sample was .85.
Depressive symptoms
The Beck Depression Inventory-II (BDI-II)[35] is a widely used self-report inventory of depressive symptoms, containing 21 statements measured on a four-point Likert scale. Psychometric data are available for its use with older adults (see Reference[36]). Cronbach’s α was .86 for the current sample.
Procedures
Following the in-person diagnostic interview, a baseline assessment battery was conducted via telephone by an independent clinician who was unaware of diagnoses assigned. Instruments administered included the GADSS, SIGH-A, PSWQ, BAI, and BDI-II. Data indicate comparable psychometric properties for assessments conducted in-person and over the telephone (see Reference[37]). All baseline assessments were audiotaped, and a random 20% were rated by a second clinician, also unaware of diagnoses assigned, to assess inter-rater reliability.
Data analyses
All analyses were conducted on the full sample of patients with and without GAD (n = 223). Internal consistency of the GADSS was assessed using Cronbach’s α coefficient. Inter-rater reliability was evaluated using an ICC. The GADSS was correlated with the SIGH-A, PSWQ, and BAI to assess convergent validity and with the BDI-II to assess divergent validity. Factor structure of the GADSS was examined by principal-components extraction with varimax rotation. To assess discriminant validity, an independent-samples t-test compared GADSS scores of participants with and without a diagnosis of GAD. Additionally, a receiver operating characteristic (ROC) curve was calculated using a maximum likelihood estimate to establish the ability of GADSS scores to predict diagnostic status (i.e., GAD, no GAD). Also, a stepwise discriminant function analysis (DFA) was performed to identify any GADSS items that might reliably predict a diagnosis of GAD.
RESULTS
RELIABILITY
The internal consistency of the GADSS was acceptable (α = .79). However, interitem correlations suggested low-to-moderate correlations between individual items (r = .23–.52; see Table 1). Inter-rater reliability was excellent for both individual items (.94–.99) and total scores (.99; see Table 1).
TABLE 1.
Interitem and intraclass correlations of GADSS
| Item | 1 | 2 | 3 | 4 | 5 | 6 | ICC |
|---|---|---|---|---|---|---|---|
| 1. Freq | 1.00 | 0.96 | |||||
| 2. Dist | 0.40 | 1.00 | 0.97 | ||||
| 3. Assoc | 0.40 | 0.32 | 1.00 | 0.94 | |||
| 4. Sever | 0.28 | 0.47 | 0.58 | 1.00 | 0.97 | ||
| 5. Work | 0.29 | 0.46 | 0.40 | 0.50 | 1.00 | 0.95 | |
| 6. Social | 0.23 | 0.35 | 0.35 | 0.36 | 0.52 | 1.00 | 0.98 |
Note. GADSS = Generalized Anxiety Disorder Severity Scale; Freq = Frequency of worries; Distress = Distress due to worrying; Assoc = Frequency of associated symptoms; Severity = Severity and distress due to associated symptoms; Work = Impairment/interferences in work functioning; Social = Impairment/interferences in social functioning.
Convergent and divergent validity
The GADSS correlated moderately with the BAI (r = .45), PSWQ (r = .48), and SIGH-A (r =.67) (see Table 2). The stronger correlation with the SIGH-A suggests the role of method variance. Correlation of the GADSS and BDI-II was also moderate (r =.57), suggesting a lack of divergent validity.
TABLE 2.
Correlations between GADSS items and other measures
| Item | SIGH-A | PSWQ | BAI | BDI-II |
|---|---|---|---|---|
| Freq | 0.36 | 0.38 | 0.28 | 0.41 |
| Dist | 0.38 | 0.48 | 0.28 | 0.35 |
| Assoc | 0.54 | 0.34 | 0.34 | 0.47 |
| Sever | 0.55 | 0.38 | 0.38 | 0.42 |
| Work | 0.54 | 0.23 | 0.32 | 0.34 |
| Social | 0.45 | 0.26 | 0.30 | 0.42 |
| Total | 0.67 | 0.48 | 0.45 | 0.57 |
Note. GADSS = Generalized Anxiety Disorder Severity Scale; SIGH-A = Structured Interview Guide for the Hamilton Anxiety Scale; PSWQ = Penn State Worry Questionnaire; BAI = Beck Anxiety Inventory; BDI-II = Beck Depression Inventory-II; Freq = Frequency of worries; Distress = Distress due to worrying; Assoc = Frequency of associated symptoms; Severity = Severity and distress due to associated symptoms; Work = Impairment/interferences in work functioning; Social = Impairment/interferences in social functioning; Total = Total GADSS score.
Individual items of the GADSS were correlated with the above measures to explore whether individual items were more highly correlated to related measures than the test as a whole (see Table 2). Again, overall correlations were highest for the SIGH-A and BDI-II. Surprisingly, items assessing worry correlated only moderately with the PSWQ.
Factor structure
Principal-components extraction with varimax rotation was performed on the six GADSS items. With oblique rotation, the results were identical to the orthogonal rotation. Thus, only orthogonal results are presented. A single factor was extracted, explaining 72% of the variance. The unidimensional factor structure indicates that the GADSS measures a single construct — a cluster of symptoms of GAD (see Table 3 for communalities).
TABLE 3.
Communalities and squared multiple correlation (SMC) for GADSS items and factor
| Item | h2 | SMC |
|---|---|---|
| Freq | 0.23 | |
| Dist | 0.39 | |
| Assoc | 0.44 | |
| Sever | 0.55 | |
| Work | 0.49 | |
| Social | 0.32 | |
| Factor 1 | 0.81 |
Note. GADSS = Generalized Anxiety Disorder Severity Scale; Freq = Frequency of worries; Distress = Distress due to worrying; Assoc = Frequency of associated symptoms; Severity = Severity and distress due to associated symptoms; Work = Impairment/interferences in work functioning; Social = Impairment/interferences in social functioning.
Discriminant validity
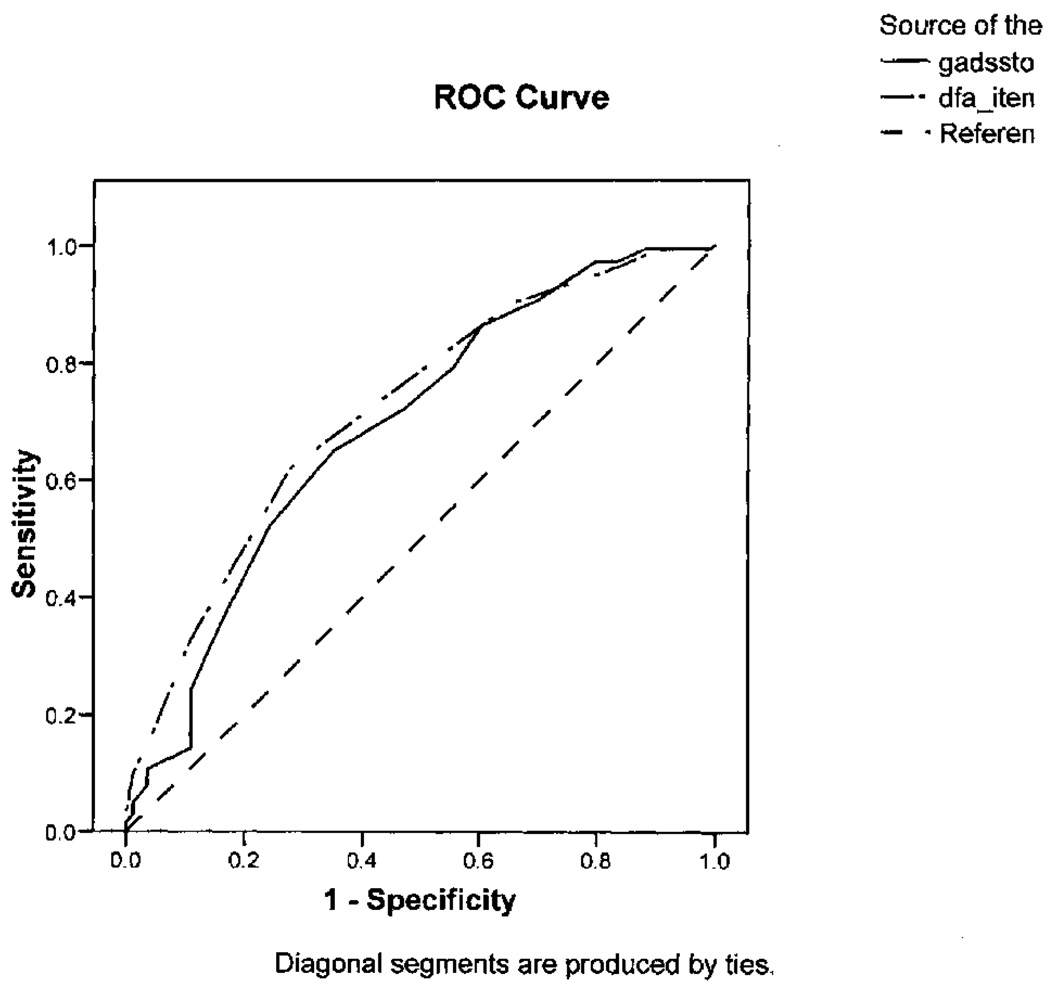
Total GADSS scores differed significantly between patients with GAD (M = 11.33, SD = 3.50) and those without GAD (M = 9.23, SD = 4.16), t(221) = 5.04, p<.0001.4 However, the GADSS exhibited poor test accuracy (area under the curve = .69, SE = .04, 95% CI = .62–.76; see Fig. 1).
Figure 1.
Receiver operating characteristic (ROC) curves for the Generalized Anxiety Disorder Severity Scale total score and the discriminant function analysis (DFA) items.
A stepwise DFA was performed where the presence/absence of clinician-diagnosed GAD was predicted using the six items of the GADSS and were entered into the DFA. Only three items (distress because of worrying; severity and distress because of associated symptoms; and impairment/interferences in work functioning) reliably predicted presence or absence of GAD. F values,Wilks’ Λ, squared canonical correlation coefficients, and partial R2 values for the significant items are presented in Table 4.
TABLE 4.
Summary of stepwise discriminant function analysis
| Step | Item | F | Wilks’ Λ | Canonical R2 | Partial R2 |
|---|---|---|---|---|---|
| 1 | Severity | 23.81** | 0.90** | 0.10** | 0.10 |
| 2 | Dist | 7.58* | 0.87** | 0.13** | 0.03 |
| 3 | Work | 3.68 | 0.86** | 0.14** | 0.02 |
Note. Severity = Severity and distress due to associated symptoms; Dist = Distress due to worrying; Work = Impairment/interferences in work functioning.
<.01
<.0001.
Post hoc analyses
To examine the ability of these three items to predict group membership, an additional ROC curve was plotted using the sum of the three GADSS items that emerged as significant in the DFA. Test accuracy for the sum of these items resulted in slightly stronger prediction of GAD than the GADSS total score (area under the curve = .72, SE = .04, 95% CI = .65–.79; see Fig. 1).
DISCUSSION
This study provides mixed preliminary support for the utility of the GADSS with older adults. The measure demonstrated adequate internal consistency and strong inter-rater reliability. Interitem correlations were low, but this might have resulted from the restricted range of possible scores on each item (0–4) and lack of sufficient variability in the study sample. The GADSS demonstrated adequate convergent validity, with highest correlations between the GADSS and SIGH-A, another clinician-rated measure of anxiety. These measures were not perfectly correlated, however, indicating that they assess different constructs within the anxiety realm. As in the original study,[17] the GADSS had a unidimensional factor structure, and scores differed significantly between patients with and without GAD. Mean scores may provide normative data against which to evaluate subsequent studies of GAD in primary care.
Despite these positive psychometric properties, diagnostic accuracy of the GADSS was poor; and results indicated a lack of divergent validity. These weaker properties may result from the nature of the study sample. All participants were self-referred for a study on GAD and screened positive for worry and/or anxiety. Thus, variability of symptoms in the study was limited, making it more difficult to differentiate the presence/absence of GAD and distinguish it from anxiety and depressive symptoms. Future studies will need to be conducted with a more heterogeneous sample. It is also possible that the poor diagnostic accuracy may be partially due to comorbidity in the GAD sample.
Although overall results are mixed for the utility of the GADSS in older adults, the sum of the three items that emerged as significant predictors of diagnostic status resulted in slightly stronger prediction of GAD. Thus, use of only these three items that assess the impact rather than frequency/duration of GAD symptoms may provide a more parsimonious measure of symptom severity, resulting in decreased burden and increased efficiency of assessment.
This study has several limitations. First, although ethnicity of the sample approximated ethnic distribution in the local community according to 2000 US census data, the sample was very well educated; and results may not generalize to a more representative sample of older adults in primary care, who may have more diverse symptoms and complaints. Further research is needed in more heterogeneous samples. Second, as noted earlier, all participants were self- or physician-referred for evaluation of worry and/or anxiety. The utility of the GADSS to identify GAD in a less selective, more randomly selected sample of primary care patients is unknown. Diagnostic accuracy may be improved in a broader sample. Third, the data here do not address the value of the GADSS as an outcome measure for clinical trials with older adults. Data addressing this question await completion of the ongoing treatment study.
Overall, results suggest that the GADSS has mixed psychometric properties among older adults presenting for evaluation and treatment of anxiety in primary care. Future studies will need to replicate the apparently strong psychometric properties (e.g., internal consistency, inter-rater reliability, convergent validity, factor structure) and examine further properties that appear to be weak in this study (e.g., divergent validity, diagnostic accuracy). It is also important to examine the measure’s sensitivity to treatment in controlled outcome studies.
Acknowledgments
This research was supported by Grant 53932 from the National Institute of Mental Health to the last author. We thank Anthony Greisinger and the staff of the Kelsey Research Foundation and Kelsey-Seybold Clinic, who provided consultation and assisted with recruitment. We also thank two anonymous reviewers for their helpful comments on an earlier version of this article. Portions of this work were presented at the 2007 convention for the Association for Behavioral and Cognitive Therapies, November, Philadelphia, PA. This work was supported in part by the Houston VA HSRVD Center of Excellence (HFP90-020).
Footnotes
This article is a US Government work and, as such, is in the public domain in the United States of America.
A coexistent diagnosis of GAD with mood disorder was assigned only if GAD symptoms were present before the mood disorder.
Physical health was assessed using the Physical Composite Score, a summary score of overall physical functioning, of the Short-Form Health Survey (SF-12). [22] Physical health also did not differ between patients under and above 65 years of age, t(221) = 0.20, ns.
Sample items include “How much distress does worrying cause you? How upset or uncomfortable do you feel when you are worrying? ” and “Over the past week, how often did you experience these symptoms? Did you have these symptoms every day? On average, during how much of each day did you have one or more of these symptoms?” For a list of all items, see Reference.[17]
Patients with and without GAD also differed significantly on the BAI, t(221) = 4.90, <.0001 (GAD = 13.53, SD = 8.73; no GAD = 8.28, SD = 5.64); PSWQ, t(221) = 6.61, p<.0001 (GAD = 55.48, SD = 10.83; no GAD = 45.28, SD = 11.67); SIGH-A, t(221) = 6.35, <.0001 (GAD = 19.56, SD = 7.64; no GAD = 13.18, SD = 6.28); and BDI-II, t(220) = 3.68, p = .0003 (GAD = 16.61, SD = 8.85; no GAD = 12.25, SD = 8.01).
REFERENCES
- 1.Beekman A, Bremmer MA, Deeg D, Van Balkom A, Smit JH, de Beurs E, Van Dyck RV, Van Tilburg W. Anxiety disorders in later life: A report from the longitudinal aging study Amsterdam. Int J Geriatr Psychiatry. 1998;13:717–726. doi: 10.1002/(sici)1099-1166(1998100)13:10<717::aid-gps857>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of mental disorders (4th ed, text revision) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 3.Krasucki C, Howard R, Mann A. Anxiety and its treatment in the elderly. Int Psychogeriatr. 1999;11:25–45. doi: 10.1017/s1041610299005566. [DOI] [PubMed] [Google Scholar]
- 4.Brenes GA, Wagener P, Stanley MA. Hand-book of Behavioral and Cognitive Therapies with Older Adults. New York, NY: Springer; 2007. Treatment of late-life generalized anxiety disorder in primary care settings. [Google Scholar]
- 5.Wittchen HU, Kessler RC, Beesdo K, Krause P, Hofler M, Hoyer J. Generalized anxiety and depression in primary care: Prevalence, recognition, and management. J Clin Psychiatry. 2002;63:24–34. [PubMed] [Google Scholar]
- 6.Tolin DF, Robison JT, Gaztambide S, Blank K. Anxiety disorders in older Puerto Rican primary care patients. Am J Geriatr Psychiatry. 2005;13:150–156. doi: 10.1176/appi.ajgp.13.2.150. [DOI] [PubMed] [Google Scholar]
- 7.Stanley MA, Hopko DR, Diefenbach GJ, Bourland SL, Rodriguez H, Wagener P. Cognitive-behavior therapy for late-life generalized anxiety disorder in primary care: Preliminary findings. Am J Geriatr Psychiatry. 2003;11:92–96. [PubMed] [Google Scholar]
- 8.Wetherell JL, Gatz M, Craske MG. Treatment of generalized anxiety disorder in older adults. J Consult Clin Psychol. 2003;71:31–40. doi: 10.1037//0022-006x.71.1.31. [DOI] [PubMed] [Google Scholar]
- 9.Stanley MA, Novy DM, Bourland SL, Beck JC, Averill PM. Assessing older adults with generalized anxiety: A replication and extension. Behav Res Ther. 2001;39:221–235. doi: 10.1016/s0005-7967(00)00030-9. [DOI] [PubMed] [Google Scholar]
- 10.Krasucki C, Howard R, Mann A. The relationship between anxiety disorders and age. Int J Geriatr Psychiatry. 1998;13:79–99. doi: 10.1002/(sici)1099-1166(199802)13:2<79::aid-gps739>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 11.Astrom M. Generalized anxiety disorder in stroke patients. A 3-year longitudinal study. Stroke. 1996;27:270–275. doi: 10.1161/01.str.27.2.270. [DOI] [PubMed] [Google Scholar]
- 12.Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validity of the Penn StateWorry Scale. Behav Res Ther. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 13.Hamilton M. The assessment of anxiety state by rating. Br J Med Psychiatry. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 14.Lenze EJ, Karp JF, Mulsant BH, et al. Somatic symptoms in late-life anxiety: Treatment issues. J Geriatr Psychiatry Neurol. 2005;18:89–96. doi: 10.1177/0891988705276251. [DOI] [PubMed] [Google Scholar]
- 15.Wisocki P, Handen B, Morse C. The Worry Scale as a measure of anxiety among homebound and community active elderly. The Behavior Therapist. 1986;9:91–95. [Google Scholar]
- 16.Pachana NA, Byrne GJ, Siddle H, Koloski N, Harley E, Arnold E. Development and evaluation of the Geriatric Anxiety Inventory. Int Psychogeriatr. 2007;19:103–114. doi: 10.1017/S1041610206003504. [DOI] [PubMed] [Google Scholar]
- 17.Shear K, Belnap BH, Mazumdar S, Houck P, Rollman BL. Generalized anxiety disorder severity scale (GADSS): A preliminary validation study. Depress Anxiety. 2006;23:77–82. doi: 10.1002/da.20149. [DOI] [PubMed] [Google Scholar]
- 18.Rollman BL, Herbeck Belnap B, Mazumdar S, et al. A randomized trial to improve the quality of treatment for panic and generalized anxiety disorders in primary care. Arch Gen Psychiatry. 2005;62:1332–1341. doi: 10.1001/archpsyc.62.12.1332. [DOI] [PubMed] [Google Scholar]
- 19.Wetherell J, Lenze E, Stanley M. Evidence-based treatment of geriatric anxiety disorders. Psychiatr Clin North Am. 2005;28:871–896. doi: 10.1016/j.psc.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 20.Beck J, Stanley M, Zebb B. Psychometric properties of the Penn State Worry Questionnaire in older adults. J Clin Geropsychol. 1995;1:33–42. [Google Scholar]
- 21.Stanley MA, Roberts RE, Bourland SL, Novy DM. Anxiety disorders among older primary care patients. J Clin Geropsychol. 2001;7:105–116. [Google Scholar]
- 22.Ware JE, Jr., Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care: The PRIME-MD 1000 study. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- 24.First MB, Spitzer RL, Miriam G, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Patient Edition with Psychotic. New York: Biometrics Research, New York State Psychiatric Institute; 1997. [Google Scholar]
- 25.Gloster AT, Senior A, Rhoades H, et al. Psychometric properties of the DASS-21 in late-life medical patients. Presented at the annual meeting for the Association for Advancement of Behavior Therapy; Chicago. 2006. [Google Scholar]
- 26.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state." A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 27.Shear MK, Vander BJ, Rucci P, Endicott J, Lydiard B, Otto MW, et al. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A) Depress Anxiety. 2001;13:166–178. [PubMed] [Google Scholar]
- 28.Skopp N, Novy D, Kunik M, et al. Investigation of cognitive behavior therapy. Am J Geriatr Psychiatry. 2006;14:292. doi: 10.1097/01.JGP.0000192505.56434.7e. [DOI] [PubMed] [Google Scholar]
- 29.Gillis M, Haaga D, Ford G. Normative values for the Beck Anxiety Inventory, Fear Questionnaire, Penn State Worry Questionnaire, and Social Phobia and Anxiety Inventory. Psychol Assess. 1995;7:450–455. [Google Scholar]
- 30.Molina S, Borkovec T. The Penn State Worry Questionnaire: Psychometric Properties and Associated Characteristics. Oxford, UK: Wiley; 1994. [Google Scholar]
- 31.Beck AT, Steer RA. Beck Anxiety Inventory manual. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- 32.Morin C, Landreville P, Colecchi C, McDonald K, Stone J, Ling W. The Beck Anxiety Inventory: Psychometric Properties with Older adults. J Clin Geropsychol. 1999;5:19–29. [Google Scholar]
- 33.Wetherell J, Gatz M. The Beck Anxiety Inventory in older adults with generalized anxiety disorder. J Psychopathol Behav Assess. 2005;27:17–24. [Google Scholar]
- 34.Kabacoff R, Segal D, Hersen M, Van Hasselt V. Psychometric properties and diagnostic utility of the Beck Anxiety Inventory and the State-Trait Anxiety Inventory with older adult psychiatric outpatients. J Anxiety Disord. 1997;11:33–47. doi: 10.1016/s0887-6185(96)00033-3. [DOI] [PubMed] [Google Scholar]
- 35.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory. 2nd ed. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 36.Snyder AG, Stanley MA, Novy DM, Averill PM, Beck JG. Measures of depression in older adults with generalized anxiety disorder: A psychometric evaluation. Depress Anxiety. 2000;11:114–120. doi: 10.1002/(sici)1520-6394(2000)11:3<114::aid-da5>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 37.Senior AC, Kunik ME, Rhoades HM, Novy DM, Wilson NL, Stanley MA. Utility of telephone assessments in an older adult population. Psychol Aging. 2007;22:392–397. doi: 10.1037/0882-7974.22.2.392. [DOI] [PubMed] [Google Scholar]