Abstract
Although much has been written about transactional models in the study of parenting practices, relatively few researchers have used this approach to examine how child behavior might be related to parental well-being. This study used latent growth curve modeling to test transactional models of age 2 child noncompliance, parental depressive symptoms, and age 4 internalizing and externalizing behaviors using a subsample of families in the Early Steps Multisite Study. In unconditional models, maternal depressive symptoms showed a linear decrease from child ages 2 to 4, whereas paternal depression did not show significant change. Observed child noncompliance at age 2 showed significant associations with concurrent reports of maternal depressive symptoms and trend-level associations with paternal depressive symptoms. For both parents, higher levels of initial depressive symptoms were related to increased age 4 child internalizing behaviors. The findings provide support for reciprocal process models of parental depression and child behavior, and this study is one of the first to present empirical evidence that fathers’ depressive symptoms have bidirectional associations with their children’s behavior in early childhood.
Keywords: maternal depression, paternal depression, child effects, noncompliance, transactional model
Maternal depression is a consistent and robust correlate of children’s maladjustment (for reviews of this literature, see Cummings & Davies, 1994; Gelfand & Teti, 1990). However, the existing literature has emphasized paternal depression far less than maternal depression. When researchers have examined depression in fathers, they have found that elevated levels of paternal depression also are associated with more internalizing and externalizing symptoms in children (for reviews of this literature, see Connell & Goodman, 2002; Kane & Garber, 2004).
Child characteristics are also associated with parental behavior (Bell & Harper, 1977; Elgar, McGrath, Waschbusch, Stewart, & Curtis, 2004). Rather than consider parent effects on children and child effects on parents to be separate processes, reciprocal models of socialization regard parenting and child behaviors as recurrent, transactional exchanges over time, where both parties affect the other (Bell, 1968; Sameroff, 1995). Although there is an extensive body of research on reciprocal effects between child disruptive behavior and parenting (Bell & Harper, 1977; Danforth, Barkley, & Stokes, 1991), researchers have paid substantially less attention to potential bidirectional effects between child disruptive behavior and parental mental health, such as depressive symptoms. As both clinical depression and subclinical, elevated levels of depressive symptoms are related to child maladjustment (Cummings, Keller, & Davies, 2005), the terms parental, maternal, and paternal depression will be used to describe both criteria.
Course of Parental Depression
It is well established that women of all ages throughout the world experience higher rates of depression than men; however, less is known about possible gender differences in the course of depression (Bracke, 1998; Weissman & Klerman, 1977). When this issue has been addressed, findings have been inconsistent, with most studies concluding that women’s depression is more chronic and recurrent than men’s (Bracke, 1998; Frank, Carpenter, & Kupfer, 1988), and others finding no gender differences (Kessler, McGonagle, Swartz, Blazer, & Nelson, 1993).
The literature on the course of depression in parents is even more limited. One study found that elevated prenatal depression was a strong risk factor for both mothers and fathers who experienced postnatal depression (Matthey, Barnett, Ungerer, & Waters, 2000). Two studies used trajectory analysis to examine depression over time in mothers only. Gross, Shaw, Burwell, and Nagin (in press) analyzed depressive symptoms from child’s age 1.5 to 10 years, and Campbell, Matestic, von Stauffenberg, Mohan, and Kirchner (2007) modeled depressive symptoms from infant age 1 month until the child was 7 years old. In both studies, most mothers showed low levels of depressive symptoms. However, both studies also found a subset of women who experienced high levels of depressive symptoms throughout the study period. More research is needed to examine the course of depression for mothers and fathers with young children.
Parental Depression and Child Adjustment
Research has found consistent associations between maternal depression and disruptions in both children’s socioemotional and instrumental functioning throughout the course of children’s development (Elgar et al., 2004; Goodman & Gotlib, 1999). For example, early childhood studies have linked maternal depression to difficult child temperament (Cutrona & Troutman, 1986; Whiffen & Gotlib, 1989), insecure attachment (Campbell et al., 2004), and conduct problems (Marchand, Hock, & Widaman, 2002; Shaw, Keenan, & Vondra, 1994). Studies of school-age children and adolescents of depressed mothers have found higher rates of externalizing problems and more serious forms of antisocial behaviors (Hay, Pawlby, Angold, Harold, & Sharp, 2003; Munson, McMahon, & Spieker, 2001), increased academic and behavior problems at school (Sinclair & Murray, 1998), and elevated rates of internalizing behaviors, especially depression (Cummings et al., 2005; Hammen & Brennan, 2003).
Considerably less is known about paternal depression and child outcomes, consistent with a broader gap in the literature regarding paternal influences on children (Phares, 1992). Initial efforts to address this gap indicate that the effects of paternal psychopathology are similar to maternal psychopathology. To date, research on paternal depression and child outcomes has been primarily limited to correlational studies that examine paternal depression and child behavior (Kane & Garber, 2004) at one time point. One exception is a longitudinal study that found paternal depression at 1 month postpartum predicted higher levels of child internalizing and externalizing problems at ages 2 and 3 years (Carro, Grant, Gotlib, & Compas, 1993). In a meta-analysis (mostly correlational studies) of paternal depression and children’s adjustment, Kane and Garber (2004) found significant associations between paternal depression and all outcomes examined, including internalizing symptoms, externalizing behaviors, and parent–child conflict. However, the effects of paternal psychopathology may be smaller in magnitude than the effects of maternal psychopathology; when both are considered simultaneously, comparatively strong maternal effects may mask separate paternal effects (Connell & Goodman, 2002).
Child Effects on Parenting and Parental Well-Being
Child effects models emphasize the influence of children’s attributes and behaviors on their parents. The literature on parenting is replete with theoretical and empirical evidence of child effects on parents. In his landmark paper on the determinants of parenting, Belsky (1984) asserted that both parent and child characteristics contribute to adaptive and dysfunctional parenting. Patterson’s (1982) coercive model describes a reciprocal parenting model, in which a cycle of negative reinforcement is established when parents unwittingly reinforce child’s disruptive behavior by paying more attention to it and not responding to the child’s adaptive behavior (Eddy, Leve, & Fagot, 2001).
Just as child behaviors are thought to influence parenting, there is evidence for child effects on other adult behaviors, including marital quality (Cui, Donnellan, & Conger, 2007), alcohol consumption (Pelham et al., 1997), parenting self-efficacy (Cutrona & Trouman, 1986), and stress (Feske et al., 2001). Moreover, there is a growing body of correlational research on child effects and maternal (but not paternal) depression. Mothers report more depressive symptoms in populations where their children have been referred to clinics (R. T. Brown, Borden, Clingerman, & Jenkins, 1988; Fergusson, Lynskey, & Horwood, 1993) and have more behavioral or emotional problems (Civic & Holt, 2000). As early as infancy, high rates of child behavior problems and irritability are associated with the persistence and onset of maternal clinical depression (Ghodsian, Zajicek, & Wolkind, 1984; Murray, Stanley, Hooper, King, & Fiori-Cowley, 1996). This notion has been further supported in experimental research, in which adults who interacted with “trained” defiant boys showed more depressive symptoms than those who interacted with nondefiant children (Pelham et al., 1997). Finally, two studies tested reciprocal models of child behavior and maternal depressive symptoms in a sample of low-income boys (Gross, Shaw, Burwell, & Nagin, in press; Gross, Shaw, & Moilanen, 2008). Both studies found evidence of child effects on subsequent maternal depression (e.g., noncompliance at 18 months for Study 1; aggression at age 5 and antisocial behavior at age 11 for Study 2). In turn, higher levels of maternal depression were associated with subsequent externalizing problems, including antisocial behavior (Gross, Shaw, Burwell, & Nagin, in press) and aggression (Gross, Shaw, & Moilanen, 2008).
Although the aforementioned studies provide evidence for child effects across development, child effects may be particularly prominent during periods of developmental stress or transition. For example, toddlerhood is a period of developmental stress, as the peak of parent–child conflict occurs between ages 2 and 3 years, and often remains high until age 4 (Klimes-Dougan & Kopp, 1999). The challenging behaviors present during this time may be particularly stressful to parental well-being, as evidenced by decreases in parental satisfaction during the 2nd year of life (Fagot & Kavanagh, 1993).
There is limited research on transactional models of child behavior and paternal depression. Bidirectional effects may differ for mothers and fathers (Connell & Goodman, 2002), such that mothers may be particularly distressed by disruptive behaviors in young children, whereas fathers may be more distressed by adolescents’ irritability and acting-out behaviors. However, there is little empirical evidence about bidirectional effects with fathers during any age period.
In summary, the extant literature provides theoretical and empirical support for reciprocal models of parental well-being and child problem behavior. Reciprocal models have been tested with respect to parenting practices and child problem behavior but applied less often to parental functioning. Moreover, little is known about the longitudinal course of depression in fathers, and reciprocal models of paternal depression and child behavior have not yet been explored.
The Current Study
In the current study, we used data from the Early Steps Multisite Study, an intervention project comprising a large sample of geographically and ethnically diverse families. First, latent growth curves of parental depressive symptoms were examined over a 2-year span (child age 2 to 4 years). Then, the relations between age 2 child noncompliance, parental depressive symptoms, and age 4 child behavior problems were explored by estimating reciprocal effects models. In accordance with previous research, we hypothesized that early child noncompliance would be related to depressive symptoms for both mothers and fathers, but based on theoretical models, more strongly for mothers (Connell & Goodman, 2002). A second hypothesis was that both maternal and paternal depressive symptoms would be associated with age 4 child internalizing and externalizing symptoms. To minimize the potential for informant bias (Fergusson et al., 1993), a different caregiver reported on depressive symptoms and child problem behavior at age 4.
Method
Participants
Participants in the Early Steps Multisite Study included 731 mother–child dyads recruited between 2002 and 2003 from Women, Infants and Children programs in the metropolitan areas of Pittsburgh, Pennsylvania; Eugene, Oregon; and Charlottesville, Virginia (see Dishion, Shaw, Connell, Wilson, Gardner, & Weaver, in press). Approval was obtained from the Institutional Review Boards (IRBs) of the three institutions prior to initiating any recruitment and screening procedures. The IRBs of the three sites reviewed the study protocol, enrollment data, and consent forms on an annual basis. The study included an intervention component, with all families participating in annual assessments and approximately half of the families randomly assigned to the intervention group (367 of 731 families). Families were invited to participate if they had a 2-year-old child and met the study criteria by having socioeconomic, family, or child risk factors for future behavior problems.
The children in the sample had a mean age of 29.9 months (SD = 3.2) at the time of the age 2 assessment. Of the 731 families (49% with female children participants), 272 (37%) were recruited in Pittsburgh, 271 (37%) in Eugene, and 188 (26%) in Charlottesville. Across sites, the children belonged to the following racial groups: 27.9% African American, 50.1% European American, 13.0% biracial, and 8.9% other races (e.g. American Indian, Native Hawaiian), with 13.4% of the sample reporting being Hispanic American. From 2002 to 2003, more than two thirds of enrolled families had an annual income of less than $20,000. Forty-one percent of the population had a high school diploma or GED equivalency, and an additional 32% had 1 to 2 years of post– high school training.
Primary caregivers (PC) and target children participated in all assessments. When possible, the alternate caregiver (AC) also participated. For this subsample, maternal depression data were included if the biological mother was the PC, the PC had completed the Center for Epidemiological Studies Depression scale (CES–D; see Measures, below) at one or more time points, and there were no changes in the child’s PC. Paternal depression data were used only when the AC was the biological father and had completed the CES–D at one or more time points. This subsample consisted of 681 cases for the maternal depression model and 297 for the paternal model. All age 4 outcome data were used, regardless of the respondent’s relationship with the child (e.g., AC could have been the child’s grandmother instead of the father).
Design and Procedure
When children were ages 2, 3, and 4 years, participating PCs and ACs, if available, were scheduled for 2.5-hr assessments in their homes. After providing informed consent, PCs and ACs completed questionnaires and engaged in several videotaped tasks (totaling 43 min, including a meal preparation and lunch task). Families were paid for their participation.
As this study included an intervention component, families were randomly assigned to the intervention or control group at age 2. The intervention, the Family Check Up, included a broad assessment of the family context and parenting practices, an initial introductory meeting with the family, and a formal feedback. The intervention group families were scheduled for these meetings on a yearly basis around the time of the assessments (ages 2 to 4). More information about this intervention can be found in Dishion et al., in press. For all analyses below, intervention group status is used as a covariate and is defined by an intention to treat design.
Measures
Demographics questionnaire
PCs completed a demographics questionnaire, which included questions about family structure, parental education and income, parental criminal history, and areas of familial stress. Data from the age 2 demographics questionnaire were used for the current study.
Child noncompliance
A team of undergraduates coded the age 2 videotaped family interaction tasks using the Relationship Process Code (RPC; Jabson, Dishion, Gardner, & Burton, 2004). The RPC is a third-generation code derived from the Family Process Code (Dishion, Gardner, Patterson, Reid, & Thibodeaux, 1983). Child compliance and noncompliance behaviors were coded for all of the parent–child tasks (e.g., clean-up, delay of gratification, teaching, inhibition, and meal preparation; average team RPC percent agreement = .87, κ = .86). Compliant behavior was defined as the act of responding voluntarily to a family member’s bid for behavior change (e.g., cleaning up toys) or to positive structure (e.g., playing along with a game). Noncompliance was coded when a child clearly ignored, disagreed, or refused to cooperate. For this study, a noncompliance ratio was used as the measure of age 2 child behavior. This ratio was calculated by dividing the duration (in seconds) of noncompliance by the total duration of compliance and noncompliance.
Maternal and paternal depressive symptoms
PCs and ACs completed the 20-item CES–D (Radloff, 1977) at the age 2, 3, and 4 assessments. Participants reported how frequently they had experienced a list of depressive symptoms during the past week on a scale ranging from 0 (less than a day) to 3 (5–7 days). Item scores were summed to create an overall depressive symptoms score. In this sample, internal consistencies ranged from .67 to .78.
Child internalizing and externalizing problems
Parents also completed the Child Behavior Checklist (Achenbach & Rescorla, 2000) for ages 1.5–5 at the age 4 study visit. This questionnaire includes 99 items that assess behavioral problems in young children. Caregivers responded to each item on a 3-point response scale, ranging from 0 (not true [as far as you know]) to 3 (very true or often true). Items were summed to construct indices of internalizing and externalizing problems. The internal consistencies for age 4 externalizing behavior were .91 (PC) and .90 (AC) and for internalizing behavior, .86 (PC) and .84 (AC).
Data Preparation
Prior to analyses, data were screened for normality and patterns of missingness. Two extreme outliers were removed from the maternal depression model and three from the paternal depression model. All continuous variables were transformed to meet the assumption of multivariate normality. Descriptive statistics are presented in Table 1. Data were found to be missing completely at random in the maternal depression model and missing at random in the paternal depression model. Consequently, full information maximum likelihood was employed in model estimation procedures (Enders, 2001).
Table 1.
Descriptive Statistics for Variables in Study of Reciprocal Models of Child Behavior and Parental Depressive Symptoms
| Model | ||
|---|---|---|
| Statistic | Maternal depression–AC outcomes |
Paternal depression–PC outcomes |
| Mean (SD) noncompliance ratio | 0.21 (0.13) | 0.19 (0.12) |
| In treatment group, % | 50.3 | 48.3 |
| Male, % | 49.6 | 50.3 |
| African American, % | 27.9 | 15.3 |
| Hispanic, % | 14.0 | 13.3 |
| Biracial or other, % | 12.5 | 11.6 |
| Mothers without high school diplomas, % | 24.0 | 22.4 |
| Mothers with diplomas or GEDs, % | 41.6 | 41.2 |
| Mothers who ever attended college, % | 34.4 | 36.4 |
| Mean (SD) depression age 2 | 16.57 (10.49) | 10.06 (8.08) |
| Mean (SD) depression age 3 | 15.52 (10.95) | 10.17 (8.27) |
| Mean (SD) depression age 4 | 14.93 (10.88) | 9.35 (7.18) |
| Mean (SD) child internalizing | 8.72 (6.22) | 10.47 (6.97) |
| Mean (SD) child externalizing | 12.78 (7.78) | 15.64 (8.49) |
Note. AC = alternate caregiver; PC = primary caregiver. Descriptive statistics are presented separately by model. The first column provides descriptives for the model using maternal depression and AC-reported child internalizing and externalizing scores. The second column provides descriptives for model using paternal depression and PC-reported child outcomes.
Analysis Plan
Structural equation modeling-based latent growth curve modeling was conducted in Mplus Version 4.0 (Muthén & Muthén, 2004). A two-step procedure was employed. First, unconditional models (i.e., growth models without any predictors) were estimated to identify the shape of growth in maternal and paternal depressive symptoms. Second, conditional growth models were tested to examine the impact of the covariates on growth in parental depressive symptoms, and to examine associations between the growth parameters and later outcomes. For all models, requirements for adequate model fit included comparative fit indices (CFI) of .90 or higher, root-mean-square error of approximation (RMSEA) values of less than .05, and standardized root-mean-square residual (SRMR) values of .10 or lower (Kline, 2005). The chi-square goodness of fit statistic is also reported for all models.
Results
Characterizing Latent Growth in Parental Depressive Symptoms
For mothers, an unconditional model of linear growth showed an adequate fit to the data, χ2(3) = 7.68, p > .05; CFI = .99; RMSEA = .05; 90% confidence interval (CI) = 0.00, 0.09; SRMR = .06. On average, levels of maternal depressive symptoms (intercept = 3.99, p < .001) were moderate at age 2 and declined steadily between child’s ages 2 and 4 (slope = −.12, p < .001). Individual mothers varied in their levels of depressive symptoms at age 2 but not in patterns of growth over time , which suggests that mothers’ symptoms declined at the same rate between child’s ages 2 and 4. Intercept and slope parameters were not correlated (r = .14, p > .05).
For fathers, an unconditional model with a linear term could not be reliably estimated (i.e., slope variances could not be calculated, and the model provided a poor fit to the data). An examination of fathers’ means indicated that fathers’ depressive symptoms were at moderate levels at child’s age 2, increased slightly at age 3, and by age 4 had declined to levels lower than those at ages 2 and 3. This suggests that change in fathers’ depressive symptoms was not linear, but with only three time points, higher order growth models (e.g., quadratic, cubic) could not be fitted. Consequently, an intercept-only model of paternal depressive symptoms was examined and showed a good fit to the data, χ2(6) = 7.61, p > .05; CFI = .98; RMSEA = .03; 90% CI = 0.00, 0.09; SRMR = .06. On average, initial levels of paternal depressive symptoms (intercept = 3.11, p < .001) were in the moderate range, and individual fathers varied in their levels of depressive symptoms at age 2 . This intercept-only model was retained for conditional models; consequently, the analysis using paternal depressive symptoms explores the research questions with respect to initial (age 2) depressive symptoms.
Conditional Growth Models With Child Outcomes
In the conditional models, paths from predictors to the intercept terms and to the outcome variables were estimated, as were paths from the intercept terms to the outcome variables. Predictors included child noncompliance at age 2 and demographic variables (i.e., child gender, maternal education, child ethnicity, and intervention group status). Child outcomes were examined using cross-informant reports of age 4 child internalizing and externalizing behaviors.
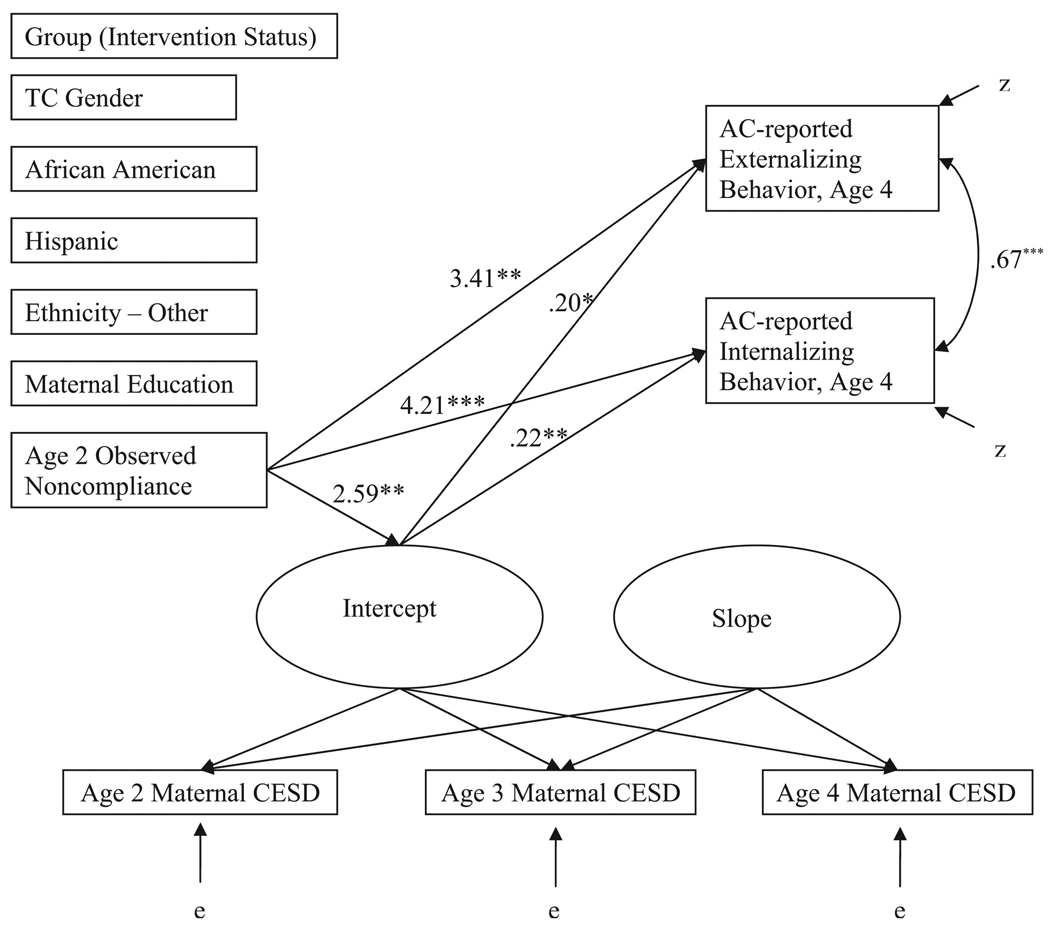
Maternal depressive symptoms and AC-reported child outcomes
The maternal depression–AC outcomes model provided good fit to the data, χ2(21) = 36.85, p < .05; CFI = .98; RMSEA = .03; 90% CI = 0.01, 0.05; SRMR = .03. There were several paths that supported transactional effects (see Figure 1). However, as there was no significant variability in the slope growth term for maternal depressive symptoms, predictors were modeled only to the intercept (age 2). As a result, associations between predictor variables (including covariates) and maternal depressive symptoms were assessed at concurrent time points. High levels of age 2 observed noncompliance were indicative of high initial (age 2) levels of maternal depressive symptoms (B = 2.59, SE = 0.89, p < .01). In terms of outcomes, high initial levels of maternal depressive symptoms were significantly related to high levels of AC-reported, age 4 child internalizing behavior (B = 0.22, SE = 0.07, p < .01) and AC-reported, age 4 externalizing problems (B = 0.20, SE = 0.08, p < .05). There were direct relations between observed noncompliance at age 2 and age 4 child behaviors (B = 4.21, SE = 1.10, p < .001, for internalizing; B = 3.41, SE = 1.22, p < .01, for externalizing). AC reports of age 4 child internalizing and externalizing behaviors were positively correlated (r = .67, p < .001). For this subsample, intervention group status was not significantly related to maternal depressive symptoms or AC-reported age 4 child outcomes.
Figure 1.
Maternal depression–alternate caregiver (AC) outcomes reciprocal effects model with significant paths. Note. All path coefficients are unstandardized. Gender was coded as 0 = male, 1 = female. Group was coded as 0 = control, 1 = intervention. Paths were also modeled between noncompliance and all covariates (e.g., group, gender, ethnicity) and the age 4 outcomes, but these are not shown. The dashed lines are used for paths that were significant at the trend level. †p < .10. * p < .05. ** p < .01. *** p < .001.
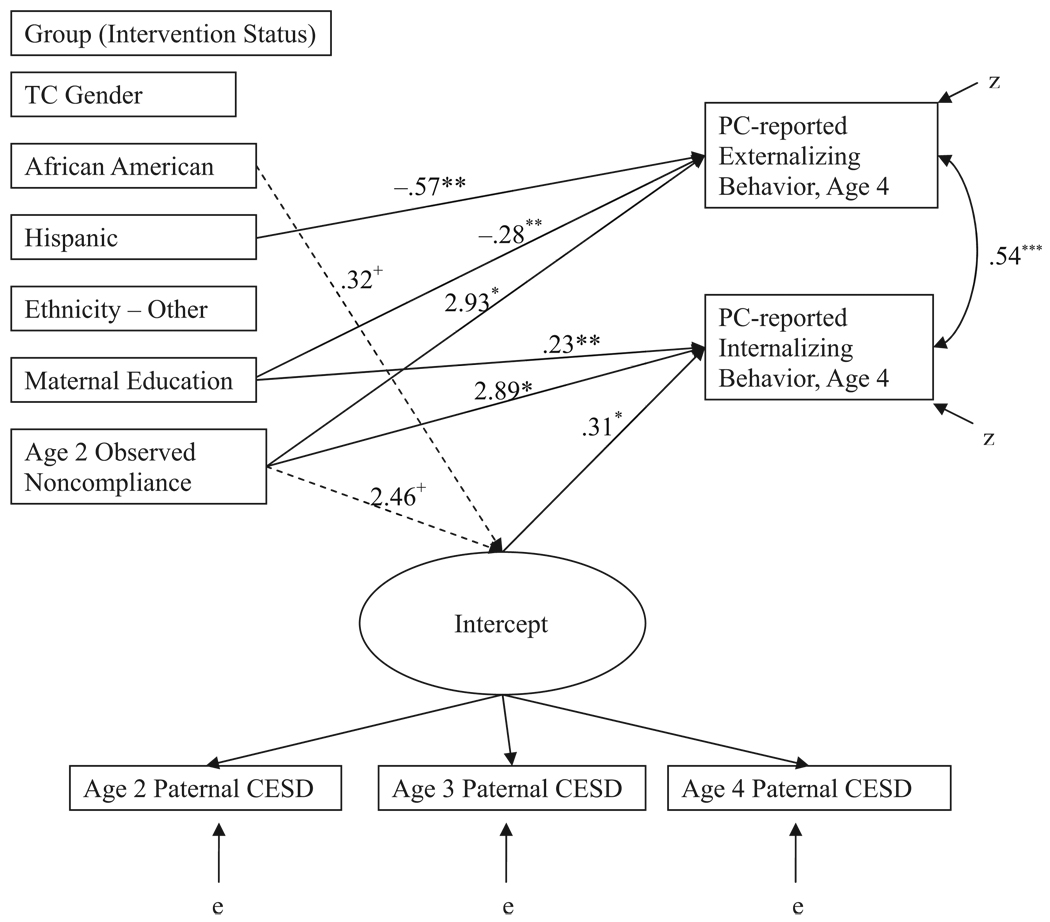
Paternal depressive symptoms and PC-reported child outcomes
The paternal depression–PC outcome model showed good model fit, χ2(24) = 24.91, p > .10; CFI = 1.00; RMSEA = .01; 90% CI = 0.00, 0.05; SRMR = .03. In this model (see Figure 2), the path between age 2 child noncompliance and intercept of paternal depressive symptoms approached significance (B = 2.47, SE = 1.32, p < .10), suggesting that high levels of child noncompliance at age 2 were marginally related to higher initial levels of paternal depressive symptoms (also at child’s age 2). There was also a trend-level association for African Americans and intercept of paternal depressive symptoms, suggesting that African American fathers had slightly higher levels of depressive symptoms at child’s age 2. There were significant associations between the intercept of paternal depressive symptoms and PC-reported age 4 internalizing behavior; higher initial levels of paternal depressive symptoms were associated with higher levels of PC-reported age 4 child internalizing problems (B = 0.31, SE = 0.10, p < .01). In addition, high levels of observed age 2 child noncompliance were directly related to high levels of PC-reported child problems at age 4 (for internalizing, B = 2.89, SE = 1.33, p < .05; for externalizing, B = 2.93, SE = 1.42, p < .05). Finally, maternal education was negatively associated with age 4 child behaviors (B = −0.23, SE = 0.08, p < .01, for internalizing; B = −0.28, SE = 0.09, p < .01, for externalizing), and children of Hispanic ethnicity were lower in age 4 externalizing symptoms than European American children (B = −0.57, SE = 0.20, p < .01). PC reports of age 4 child internalizing and externalizing behaviors were significantly correlated (r = .54, p < .001). For this subsample, intervention group status was not significantly related to paternal depressive symptoms or PC-reported age 4 child outcomes.
Figure 2.
Paternal depression–primary caregiver (PC) outcomes reciprocal effects model with significant paths. Note. All path coefficients are unstandardized. Gender was coded as 0 = male, 1 = female. Group was coded as 0 = control, 1 = intervention. Paths were also modeled between noncompliance and all covariates (e.g., group, gender, ethnicity) and the age 4 outcomes, but these are not shown. † p < .10. * p < .05. ** p < .01. *** p < .001.
Discussion
This study tested two transactional models to explore reciprocal relations among child’s age 2 noncompliance, parental (maternal and paternal) depressive symptoms from child’s age 2 to 4, and age 4 child internalizing and externalizing symptoms. Maternal depressive symptoms decreased linearly over the 2-year span, whereas symptoms in fathers showed no significant growth. Overall, the results were generally consistent with a transactional model of early child behavior and parental depressive symptoms. Model fit indices indicated that both transactional models provided good fit to the data. Higher levels of age 2 child noncompliance were significantly related to concurrent elevated depressive symptoms in mothers (p < .01) and corresponded to concurrent paternal depressive symptoms at a trend level. For both models, parental depressive symptoms were significantly associated with age 4 internalizing behavior using different informants of parental depressive symptoms and child problem behavior.
There were several significant effects found for covariates in the paternal model. At a trend level, African American fathers tended to report more depressive symptoms at child’s age 2, consistent with findings that fathers in ethnic minority groups are at higher risk for depression (Bronte-Tinkew, Moore, Matthews, & Carrano, 2007). Lower levels of maternal education were associated with increased age 4, PC-reported child behavior problems. Low maternal education is often cited as a risk factor for child behavior problems across development (Bradley & Corwyn, 2002). Finally, Hispanic children were rated as having significantly lower levels of PC-reported, age 4 externalizing problems. This finding should be confirmed in future research using diverse samples. Although an explanation for this effect could not be directly tested, at age 4 Hispanic children were less likely to be enrolled in childcare centers (28.7% of non-Hispanic children in childcare centers compared with 11.8% of Hispanic children), χ2(1, N = 581) = 9.65, p < .01. Some studies have found a link between time spent in childcare settings and higher levels of externalizing behaviors (Belsky, 1999; National Institute of Child Health and Human Development Early Child Care Research Network, 1998).
It is interesting that, in contrast to reports using the full Early Steps Multisite Study sample (Dishion et al., in press; Shaw, Dishion, Connell, Wilson, & Gardner, 2008), intervention status was not related to PC report of child behavior problems at age 4. This difference is attributable to using only a subset of 297 families that had biological fathers at the visit. Thus, the current subsample could be considered to be at lower risk than the full sample by virtue of having a second parent, which is consistent with findings from the current sample (Dishion et al., in press) and an earlier trial of the Family Check Up for toddlers (Shaw, Dishion, Supplee, Gardner, & Arnds, 2006), indicating that the intervention is more effective for higher risk families.
The finding that maternal depressive symptoms decreased slightly from child’s age 2 to 4 provides some evidence that depressive symptoms in mothers abate as young children grow older. Although existing research has found depression in women to be chronic and recurrent, levels of depressive symptoms may be elevated in mothers of infants and toddlers, which would account for the slight decline found in this sample. For fathers, growth in depressive symptoms could not be modeled in this study. The CES–D means at child’s ages 2, 3, and 4 indicate that paternal depressive symptoms may have had a quadratic pattern of growth, but this could not be tested. Future studies should model paternal depression using more than three time points.
The reciprocal models of maternal depression and child behavior extend previous research in this area (Gross, Shaw, Burwell, & Nagin, in press; Gross, Shaw, & Moilanen, 2008; Pelham et al., 1997) and provide corroborating evidence of this process in an ethnically and geographically diverse sample of boys and girls. Another strength of this study is the use of multiple informants (e.g., observed noncompliance at age 2 and cross-informant child outcome data at age 4). The current study is also one of the first to test a transactional model of child behavior and parental depression in a large sample of fathers. In this sample, the significance level of the associations between child noncompliance and depressive symptoms was stronger for mothers than fathers. This finding is consistent with the hypothesis advanced by Connell and Goodman (2002) that fathers may be less affected by their young children’s behavioral problems than mothers. However, it is notable that there were still trend-level child effects for fathers and that the magnitude of these associations was similar for mothers and fathers. Because the sample of mothers was 3 times as large as fathers, the differences in the significance of this association may, in part, be attributable to sample size.
Noncompliance as a Child Risk Factor
Although the current study examined the contribution of noncompliance to parental depressive symptoms, other child behaviors, such as aggression and negative emotionality, are likely related to parental well-being. There was some precedent for using noncompliance as the child behavior; prior research in a similar sample indicated that, compared with aggression and irritability, noncompliance had the most robust effect on maternal depression (Gross, Shaw, Burwell, & Nagin, in press). Moreover, studies of preschool and school-age hyperactive children have found that noncompliant and oppositional behaviors often create substantial distress for parents (Barkley, Karlsson, & Pollard, 1985; Fischer, 1990). Noncompliance may be a more proximal behavior for parents than other possible child behaviors; by definition, noncompliant behaviors are directed toward authority figures, such as parents. In contrast, aggression is often directed toward an object or another child, and irritability is a more general trait. Moreover, noncompliance tends to occur more frequently than other negative child behaviors, such as aggression. Parents with limited socioeconomic resources may have a particularly difficult time coping with noncompliance in children, as they generally have more stress from financial hardships and often have fewer resources on which to draw (G. W. Brown & Moran, 1997).
Limitations of Current Study and Future Directions
Although results of the growth curve models were largely consistent with child effects at age 2 and parent effects at age 4, the current results do not address the specific mechanisms by which symptoms of parental depression and child behaviors affect one another. A number of investigators have found that associations between parental depression and child adjustment are mediated by parenting, specifically tendencies for depressed mothers to be negative, critical, unresponsive, helpless, and low on positivity toward offspring (Goodman & Gotlib, 1999; Zahn-Waxler, Iannotti, Cummings, & Denham, 1990). Clearly, future research on transactional models would benefit from incorporating other measures that explore these mechanisms, such as child (e.g., inhibitory control), parent (e.g., caregiving quality), and contextual (e.g., neighborhood quality) factors. In addition, the models tested in the current study start at age 2. It is quite likely that parental factors, such as depressive symptoms, were present prior to this age and could have affected the child’s age 2 behaviors. As a result, these models should be considered a slice of a transactional process and not exhaustive. Future research should begin examining child effects as early in the postnatal period as possible.
Moreover, the path between age 2 child noncompliance and the intercept of paternal depressive symptoms was significant only at a trend level. In addition, child effects of noncompliance on parental depressive symptoms for both models were found at concurrent time points, making it difficult to interpret their directionality. Finally, the current study and much of the literature on caregiver affect have focused on depression. However, qualities such as anxiety and hostility have many features in common with depression and have been found to load onto a common negative affect factor (Clark, Beck, & Stewart, 1990; Gotlib, 1984). Further research using other facets of negative affectivity should explore how these related caregiver characteristics function in reciprocal models of parental affect and child behavior.
Implications for Clinical and Prevention Programs
The results of this study are consistent with the robust finding that higher levels of maternal depressive symptoms are associated with poor outcomes in children (Cummings & Davies, 1994; Gelfand & Teti, 1990). This finding, coupled with the relatively high stability of maternal depressive symptoms, indicates the need for early identification and preventive interventions (Olds, 2002; Shaw et al., 2006). In addition, the association between child noncompliance and concurrent depressive symptoms for both mothers and fathers suggests that mental health clinicians working with depressed parents include an assessment of child behavior and its impact on parental well-being for those with young children. The significant parent effect findings also suggest the need for clinicians working with children who have behavioral problems to focus explicitly on factors such as caregiver mood and affect.
At a broader level, the findings are consistent with an ecological approach to treat child- and parent-identified issues (Dishion & Stormshak, 2006), in that change of context can address multiple family mental health problems that tend to be etiologically linked and clustered (e.g., maternal depression, child problem behavior). In this sense, a family-centered intervention approach may be preferred for common adult mental health problems, especially when factors such as depression are embedded within a relationship or family context (Shaw et al., 2008).
In sum, this study found reciprocal associations between child behavior and parental depressive symptoms. The paternal depression models provide novel empirical evidence that in early childhood, child characteristics are associated with paternal depressive symptomatology. Other strengths of this study were the size and diversity of the sample (ethnic and geographic), the inclusion of male and female children, and the use of multiple reporters to reduce informant bias. As discussed, the findings have important implications for the intervention and prevention of depression in parents and child behavior problems.
Contributor Information
Heather E. Gross, Department of Psychology, University of Pittsburgh
Daniel S. Shaw, Department of Psychology, University of Pittsburgh
Kristin L. Moilanen, Department of Technology, Learning and Culture, University of West Virginia
Thomas J. Dishion, Department of Psychology, University of Oregon
Melvin N. Wilson, Department of Psychology, University of Virginia.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA preschool forms & profiles. Burlington: University of Vermont Department of Psychiatry; 2000. [Google Scholar]
- Barkley RA, Karlsson J, Pollard S. Effects of age on the mother–child interactions of ADD-H and normal boys. Journal of Abnormal Child Psychology. 1985;13:631–637. doi: 10.1007/BF00923146. [DOI] [PubMed] [Google Scholar]
- Bell RQ. A reinterpretation of the direction of effects in studies of socialization. Psychological Review. 1968;75:81–95. doi: 10.1037/h0025583. [DOI] [PubMed] [Google Scholar]
- Bell RQ, Harper LV. Child effects on adults. Hillsdale, NJ: Erlbaum; 1977. [Google Scholar]
- Belsky J. The determinants of parenting: A process model. Child Development. 1984;55:83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. [DOI] [PubMed] [Google Scholar]
- Belsky J. Quantity of nonmaternal care and boys’ problem behavior/adjustment at 3 and 5: Exploring the mediating role of parenting. Psychiatry: Interpersonal and Biological Processes. 1999;62:1–20. doi: 10.1080/00332747.1999.11024848. [DOI] [PubMed] [Google Scholar]
- Bracke P. Sex differences in the course of depression: Evidence from a longitudinal study of a representative sample of the Belgian population. Social Psychiatry and Psychiatric Epidemiology. 1998;33:420–429. doi: 10.1007/s001270050075. [DOI] [PubMed] [Google Scholar]
- Bradley RG, Corwyn RF. Sociodemographic status and child development. Annual Review of Psychology. 2002;53:371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- Bronte-Tinkew J, Moore KA, Matthews G, Carrano J. Symptoms of major depression in a sample of fathers of infants: Sociodemographic correlates and links to father involvement. Journal of Family Issues. 2007;28:61–99. [Google Scholar]
- Brown GW, Moran PM. Single mothers, poverty and depression. Psychological Medicine. 1997;27:21–33. doi: 10.1017/s0033291796004060. [DOI] [PubMed] [Google Scholar]
- Brown RT, Borden KA, Clingerman SR, Jenkins P. Depression in attention-deficit-disordered and normal children and their parents. Child Psychiatry and Human Development. 1988;18:119–132. doi: 10.1007/BF00709726. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Brownell CA, Hungerford A, Spieker S, Mohan R, Blessing JS. The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Development and Psychopathology. 2004;16:231–252. doi: 10.1017/s0954579404044499. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T. Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Developmental Psychology. 2007;43:1202–1215. doi: 10.1037/0012-1649.43.5.1202. [DOI] [PubMed] [Google Scholar]
- Carro MG, Grant KE, Gotlib IH, Compas BE. Postpartum depression and child development: An investigation of mothers and fathers as sources of risk and resilience. Development and Psychopathology. 1993;5:567–579. [Google Scholar]
- Civic D, Holt VL. Maternal depressive symptoms and child behavior problems in a nationally representative normal birthweight sample. Maternal and Child Health Journal. 2000;4:215–221. doi: 10.1023/a:1026667720478. [DOI] [PubMed] [Google Scholar]
- Clark DA, Beck AT, Stewart B. Cognitive specificity and positive–negative affectivity: Complementary or contradictory views on anxiety and depression? Journal of Abnormal Psychology. 1990;99:148–155. doi: 10.1037//0021-843x.99.2.148. [DOI] [PubMed] [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin. 2002;128:746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Cui M, Donnellan MB, Conger RD. Reciprocal influences between parents’ marital problems and adolescent internalizing and externalizing behavior. Developmental Psychology. 2007;43:1544–1552. doi: 10.1037/0012-1649.43.6.1544. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Maternal depression and child development. Journal of Child Psychology and Psychiatry. 1994;35:73–112. doi: 10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Keller PS, Davies PT. Towards a family process model of maternal and paternal depressive symptoms: Exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry. 2005;46:479–489. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Troutman BR. Social support, infant temperament, and parenting self-efficacy: A mediational model of postpartum depression. Child Development. 1986;57:1507–1518. [PubMed] [Google Scholar]
- Danforth JS, Barkley RA, Stokes TF. Observations of parent–child interactions with hyperactive children: Research and clinical implications. Clinical Psychology Review. 1991;11:703–727. [Google Scholar]
- Dishion TJ, Gardner K, Patterson GR, Reid JB, Thibodeaux S. The Family Process Code: A multidimensional system for observing family interaction. 1983 Unpublished coding manual. (Available from Oregon Social Learning Center, 160 East 4th Avenue, Eugene, OR 97401-2426.) [Google Scholar]
- Dishion TJ, Shaw DS, Connell A, Wilson M, Gardner F, Weaver C. The Family Check Up with high-risk indigent families: Preventing problem behavior by increasing parents’ positive behavior support in early childhood. Child Development. doi: 10.1111/j.1467-8624.2008.01195.x. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, Stormshak EA. Intervening in children’s lives: An ecological, family-centered approach to mental health care. Washington, DC: American Psychological Association; 2006. [Google Scholar]
- Eddy JM, Leve LD, Fagot BI. Coercive family processes: A replication and extension of Patterson’s coercion model. Aggressive Behavior. 2001;27:14–25. [Google Scholar]
- Elgar FJ, McGrath PJ, Waschbusch DA, Stewart SH, Curtis LJ. Mutual influences on maternal depression and child adjustment problems. Clinical Psychology Review. 2004;24:441–459. doi: 10.1016/j.cpr.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Enders CK. A primer on maximum likelihood algorithms available for use with missing data. Structural Equation Modeling. 2001;8:128–141. [Google Scholar]
- Fagot BI, Kavanagh K. Parenting during the second year: Effects of children’s age, sex, and attachment classification. Child Development. 1993;64:258–271. doi: 10.1111/j.1467-8624.1993.tb02908.x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Lynskey MT, Horwood LJ. The effect of maternal depression on maternal ratings of child behavior. Journal of Abnormal Child Psychology. 1993;21:245–269. doi: 10.1007/BF00917534. [DOI] [PubMed] [Google Scholar]
- Feske U, Shear MK, Anderson B, Cyranowski J, Strassburger M, Matty M, et al. Comparison of severe life stress in depressed mothers and non-mothers: Do children matter? Depression and Anxiety. 2001;13:109–117. doi: 10.1002/da.1026. [DOI] [PubMed] [Google Scholar]
- Fischer M. Parenting stress and the child with attention deficit hyperactivity disorder. Journal of Clinical Child Psychology. 1990;19:337–346. [Google Scholar]
- Frank E, Carpenter LL, Kupfer DJ. Sex differences in recurrent depression: Are there any that are significant? American Journal of Psychiatry. 1988;145:41–45. doi: 10.1176/ajp.145.1.41. [DOI] [PubMed] [Google Scholar]
- Gelfand DM, Teti DM. The effects of maternal depression on children. Clinical Psychology Review. 1990;10:320–354. [Google Scholar]
- Ghodsian M, Zajicek E, Wolkind S. A longitudinal study of maternal depression and child behaviour problems. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1984;25:91–109. doi: 10.1111/j.1469-7610.1984.tb01721.x. [DOI] [PubMed] [Google Scholar]
- Goodman SJ, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Gotlib IH. Depression and general psychopathology in university students. Journal of Abnormal Psychology. 1984;93:19–30. doi: 10.1037//0021-843x.93.1.19. [DOI] [PubMed] [Google Scholar]
- Gross HE, Shaw DS, Burwell RA, Nagin DS. Transactional processes in child disruptive behavior and maternal depression: A longitudinal study from early childhood to adolescence. Development and Psychopathology. doi: 10.1017/S0954579409000091. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross HE, Shaw DS, Moilanen KL. Reciprocal associations between boys’ externalizing problems and mothers’ depressive symptoms. Journal of Abnormal Child Psychology. 2008;36:693–709. doi: 10.1007/s10802-008-9224-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Archives of General Psychiatry. 2003;60:253–258. doi: 10.1001/archpsyc.60.3.253. [DOI] [PubMed] [Google Scholar]
- Hay DF, Pawlby S, Angold A, Harold GT, Sharp D. Pathways to violence in the children of mothers who were depressed postpartum. Developmental Psychology. 2003;39:1083–1094. doi: 10.1037/0012-1649.39.6.1083. [DOI] [PubMed] [Google Scholar]
- Jabson JM, Dishion TJ, Gardner FEM, Burton J. Relationship Process Code v-2.0 training manual: A system for coding relationship interactions. 2004 Unpublished coding manual. (Available from the Child and Family Center, 195 West 12th Avenue, Eugene, OR 97401-3408). [Google Scholar]
- Kane P, Garber J. The relations among depression in fathers, children’s psychopathology, and father-child conflict: A meta-analysis. Clinical Psychology Review. 2004;24:339–360. doi: 10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Co-morbidity Survey I: Lifetime prevalence, chronicity and recurrence. Journal of Affective Disorders. 1993;29:85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- Klimes-Dougan B, Kopp C. Children’s conflict tactics with mothers: A longitudinal investigation of the toddler and preschool years. Merrill Palmer Quarterly. 1999;45:226–242. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York: Guilford Press; 2005. [Google Scholar]
- Marchand JF, Hock E, Widaman K. Mutual relations between mothers’ depressive symptoms and hostile-controlling behavior and young children’s externalizing and internalizing behavior problems. Parenting: Science and Practice. 2002;2:335–353. [Google Scholar]
- Matthey S, Barnett B, Ungerer J, Waters B. Paternal and maternal depression mood during the transition to parenthood. Journal of Affective Disorders. 2000;60:75–85. doi: 10.1016/s0165-0327(99)00159-7. [DOI] [PubMed] [Google Scholar]
- Munson JA, McMahon RJ, Spieker SJ. Structure and variability in the developmental trajectory of children’s externalizing problems: Impact of infant attachment, maternal depressive sypmtomatology, and child sex. Development and Psychopathology. 2001;13:277–296. doi: 10.1017/s095457940100205x. [DOI] [PubMed] [Google Scholar]
- Murray L, Stanley C, Hooper R, King F, Fiori-Cowley A. The role of infant factors in postnatal depression and mother–infant interactions. Developmental Medicine and Child Neurology. 1996;38:109–119. doi: 10.1111/j.1469-8749.1996.tb12082.x. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 3rd ed. Los Angeles: Author; 2004. [Google Scholar]
- National Institute of Child Health and Human Development Early Child Care Research Network. Early child care and self-control, compliance, and problem behavior at 24 and 36 months. Child Development. 1998;69:1145–1170. [PubMed] [Google Scholar]
- Olds D. Prenatal and infancy home visiting by nurses: From randomized trials to community replication. Prevention Science. 2002;3:153–172. doi: 10.1023/a:1019990432161. [DOI] [PubMed] [Google Scholar]
- Patterson GR. Coercive family processes. Eugene, OR: Castalia; 1982. [Google Scholar]
- Pelham WE, Lang AR, Atkeson B, Murphy DA, Gnagy EM, Greiner AR, et al. Effects of deviant child behavior on parental distress and alcohol consumption in laboratory interactions. Journal of Abnormal Child Psychology. 1997;25:413–424. doi: 10.1023/a:1025789108958. [DOI] [PubMed] [Google Scholar]
- Phares V. Where’s poppa? The relative lack of attention to the role of fathers in child and adolescent psychopathology. American Psychologist. 1992;47:656–664. doi: 10.1037//0003-066x.47.5.656. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES–D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Sameroff A. General systems theories and developmental psychopathology. In: Cichetti D, Cohen D, editors. Developmental psychopathology: Theory and methods. Vol. 1. New York: Wiley; 1995. pp. 659–695. [Google Scholar]
- Shaw DS, Dishion TJ, Connell A, Wilson MN, Gardner F. Maternal depression as a mediator of intervention in reducing early child problem behavior. 2008 doi: 10.1017/S0954579409000236. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw DS, Dishion TJ, Supplee L, Gardner F, Arnds K. Randomized trial of a family-centered approach to the prevention of early conduct problems: 2-year effects of the family check-up in early childhood. Journal of Consulting and Clinical Psychology. 2006;74:1–9. doi: 10.1037/0022-006X.74.1.1. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Keenan K, Vondra JI. The developmental precursors of antisocial behavior: Ages 1–3. Developmental Psychology. 1994;30:355–364. [Google Scholar]
- Sinclair DA, Murray L. Effects of postnatal depression on children’s adjustment in school. British Journal of Psychiatry. 1998;172:58–63. doi: 10.1192/bjp.172.1.58. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL. Sex differences in the epidemiology of depression. Archives of General Psychiatry. 1977;34:98–111. doi: 10.1001/archpsyc.1977.01770130100011. [DOI] [PubMed] [Google Scholar]
- Whiffen VE, Gotlib IH. Infants of postpartum depressed mothers: Temperament and cognitive status. Journal of Abnormal Psychology. 1989;98:274–279. doi: 10.1037//0021-843x.98.3.274. [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Iannotti RJ, Cummings EM, Denham S. Antecedents of problem behaviors in children of depressed mothers. Development and Psychopathology. 1990;2:271–291. [Google Scholar]