Abstract
We used a large medical insurance claims database to identify three groups: chronic opioid (>180 therapeutic days, N=3726); acute opioid use (<10 therapeutic days, N=37,108); and a non-opioid group (N=337,366) who filled at least one insurance claim but none for opioids. Our results showed that, although chronic opioid users represented only 0.65% of the total population, they filed 4.56% of all insurance claims, used 45% of all opioid analgesics and had much more physical and psychiatric co-morbidity than the acute opioid or non-opioid samples. Women were substantially over-represented (>63%) in the chronic pain group and used a much greater share of all medical services than males especially as they grew older. Although our data suggest that chronic pain is optimally managed in a multidisciplinary patient- and gender-specific treatment plan, this was rarely the case with internists being the primary, and often only, physician seen. Moreover, our data suggest that opioids were often used for conditions in which they are generally not indicated (e.g. arthritis and headaches) or contraindicated by co-existing physical ailments (COPD). Finally, we conclude that adherence to the WHO analgesic ladder and other pain treatment guidelines was relatively infrequent: first, opioid extended release preparations which are ideally suited for chronic pain were used only in 1 in 4 patients; and, second, the selection of a weak (propoxyphene, codeine, tramadol) or strong opioid (e.g. morphine, oxycodone, etc.) seemed to be driven by numerous factors not necessarily related to the intensity or duration of pain.
Introduction
Individuals experiencing chronic pain often have numerous co-morbid mental and physical illnesses, and, as such, represent a huge burden on the United States’ health care system. [13,19,20,23] However, the latter conclusion is based on estimates and extrapolations from national surveys and, consequently, is at best an approximation. With respect to addressing the scope and magnitude of co-morbidity, especially in a quantifiable sense, most studies to date [8,12,24,26,27] have used retrospective surveys which collect self-reports of illness, often in relatively small samples drawn from a few select treatment clinics. Accordingly, the results inadequately generalize to the total population, since those in treatment programs represent only a fraction of all patients receiving opioid pain medications. An additional limitation of existing studies is that they have largely relied on self-reported opioid drug use, and precise information on dosage and type of analgesic drug is typically limited.
To overcome these problems, we reasoned that a large medical insurance claims database would provide a more objective and quantifiable index of the use of opioid analgesics by those in chronic pain, their utilization of medical services, drugs prescribed and the prevalence of diagnosed physical and mental disorders. Accordingly all medical and drug claims were extracted from a database provided by a Midwest subsidiary of a national managed care company for the calendar year January 1, 2004 – December 31, 2004. One year was used so that measures of co-morbidity would refer to concurrent disease rather than life time prevalence which could be determined in a longitudinal study.
Most importantly, in this study we had such a large population base that we were able to draw very clear distinctions between chronic and acute opioid use. Because of the low incidence of chronic opioid use in the general population, most prior studies have been forced to use relatively broad criteria to distinguish acute and chronic opioid use such that the distinction between the two was often blurred, leading to ambiguous findings. Likewise, it is also difficult to distinguish between acute and chronic pain which leads to even more ambiguity.
Our aims were four fold: first, to describe the prevalence of chronic and acute prescription opioid use for pain in a large sample (611,801) of an insured population; second, to determine the extent of concurrent health service utilization; third, to examine the prevalence of opioid abuse/dependence in individuals receiving acute and chronic opioid analgesics; and finally, to describe the types of opioid drugs being prescribed to those in acute and chronic pain.
Methods and Materials
Database and General Methods
The entire database contained all medical and drug benefit claims for 611,801 privately (i.e. no Medicare of Medicaid) insured people who were continually insured for all 12 months of 2004 in a Mid-west state with a mixed urban/rural population of nearly 6 million people. The database contains information on health care contacts, the ICD-9 coded medical conditions, [11] prescriptions written and filled, primary physicians and all specialists seen by patients each of whom have unique IDs. The data were made available to Washington University, whose Institutional Review Board (IRB) approved the study, by a collaborative agreement between the University and the managed care company. All patient and physician names were encrypted to Washington University researchers. Since our intent was to examine concurrent utilization of medical services and co-morbidity, not life-time prevalence, claims were limited to one year- 2004.
All medical and pharmacy claims for these patients were extracted. Physician specialties were self-declared. All medical and psychiatric disorders were classified by their respective ICD-9 codes. Supplementary Table 1 lists all of the ICD-9 codes that were used to define the major categories of physical and mental diseases used in this paper.
Classification of Patients
This is a private insurance database in the United States (US). To give some perspectives to non-US readers, who live in countries for the most part in which the health delivery system is government provided or heavily subsidized, in 2008, 67.5% of all US residents carried privately financed insurance, often in part subsidized by their employer. Government subsidized programs – Medicare and Medicaid – for the poor, elderly or disabled covers an additional 28.5%, whereas 15.3% of the US population have no medical insurance at all (there is some overlap between Medicare and private insurance as the wealthier elderly population often have both). Thus, two-thirds of the population in the database are employed, or retired with insurance benefits and all earn income well above the poverty line in the US.
Definition of Terms
Days of Supply (DOS) was defined as the number of “therapy days” provided in a single prescription. That is, a drug with a label indication to be taken 1, 2 or 4 times per day for 10 days equals 10 DOS, no matter that the number of tablets in the prescriptions ranges from 10 – 40 tablets. Thus, DOS provides a standardized index to compare all opioid drugs with large differences in bioavailability and pharmacokinetics which require specific dosing regimens. We have also used the empirical terms, acute opioid, chronic opioid or non-opioid use, as a descriptor of the groups we studied, rather than acute or chronic pain, since we could not measure pain which is presumably an over-arching construct which may or may not have required opioid analgesics to provide relief.
In some of these analyses, we also used the distinction between the use of “weak opioids” (propoxyphene, codeine, and tramadol) and “strong opioids” (e.g. hydrocodone, oxycodone, fentanyl, morphine and other more potent opioids) in accordance with the WHO analgesic ladder [28] and the British and American Pain Society Guidelines.
Definition of Groups
The database Washington University used was a “claims database” which contained no information on those insured individuals who were fully covered by insurance but did not file a claim for either a drug or medical services in the 12 month study period (N=174,842, 28.6% of the total insured population of 611,801). This left 436,959 (71.4%) individuals from which we excluded “cancer pain” leaving an N of 408,190 persons who filed at least one non-cancer related insurance claim in 12 months. This population of 408,190 people was divided into three groups: acute opioid use, individuals who received 1 prescription for less than 10 DOS of opioid analgesics in the calendar year (N=37,108, 9.1% of the insured population); chronic opioid use, those who received 180 DOS or more per year (N = 3,726, 0.65% of the total); and the non-opioid group, individuals who filed 1 or more non-opioid insurance claim in the calendar year (N=337,336, 83%). The remaining individuals received opioids at levels which were intermediate between the defined acute and chronic groups and this group was excluded from the study. It should be noted that our definition of acute and chronic opioid use was arbitrary (e.g. <5 DOS could have been used to define acute opioid use and anything more than 5 days chronic as has been done in most prior studies). However, our goal was to avoid shades of grey in the distinction between the two groups, by selecting two completely non-overlapping groups which would be presumably more homogeneous.
Statistical Analysis
The raw data were stored in a database management system that supports Structured Query Language (SQL). SQL is a standard interactive and programming language for querying and modifying data, and managing databases. SQL is powerful in retrieving, inserting, updating, and deleting data, and performing management and administrative functions. Based on the raw insurance claim data, we created a table that included all 408,190 patients’ historical information on health service utilization and diagnosis during the year. The initial results generated from SQL were then used to do statistical tests. For data related to health service utilization in tables 1 and 2, SAS-GLM procedure was used to see whether there were significant relationships between the listed health service utilization and groups by gender. For data related to the ICD-9, SAS was used to run multiple logistic regression models. The independent variables were the same as the GLM models (“Groups” and “Female”).
Table 1.
Health service utilization by chronic opioid, acute opioid and non-opioid Groups.
| Average Number of | Chronic Opioid | Acute Opioid | Non-Opioid | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Male | Female | All | Male | Female | All | Male | Female | ||||||||||
| N=3726 | N=1370 37% | N=2356 63% | N=37108 | N=16654 45% | N=20454 55% | N=337366 | N=164596 49% | N=172770 51% | ||||||||||
| # | S.E. | # | S.E. | # | S.E. | # | S.E. | # | S.E. | # | S.E. | # | S.E. | # | S.E. | # | S.E. | |
| # of Insurance Claims | 169.29 | 2.25 | 145.52 | 3.31 | 183.12 | 2.97 | 57.12 | 0.34 | 47.16 | 0.50 | 65.23 | 0.46 | 28.54 | 0.08 | 23.23 | 0.10 | 33.60 | 0.12 |
| Mean of Distinct Diagnosed ICD9s | 20.66 | 0.23 | 17.70 | 0.35 | 22.38 | 0.29 | 11.61 | 0.04 | 9.74 | 0.06 | 13.06 | 0.06 | 7.79 | 0.01 | 6.64 | 0.01 | 8.76 | 0.02 |
| Doctors/Providers Seen by Patient* | 9.81 | 0.12 | 8.57 | 0.19 | 10.52 | 0.15 | 6.34 | 0.02 | 5.46 | 0.03 | 7.02 | 0.03 | 3.39 | 0.01 | 2.68 | 0.01 | 4.06 | 0.01 |
| Office Visits | 16.91 | 0.25 | 14.80 | 0.38 | 18.14 | 0.33 | 8.67 | 0.05 | 7.46 | 0.07 | 9.58 | 0.07 | 5.06 | 0.01 | 4.20 | 0.02 | 5.89 | 0.02 |
| ER Visits | 0.62 | 0.03 | 0.53 | 0.04 | 0.67 | 0.04 | 0.31 | 0.00 | 0.32 | 0.01 | 0.30 | 0.00 | 0.11 | 0.00 | 0.10 | 0.00 | 0.11 | 0.00 |
| Hospital Days | 1.66 | 0.09 | 1.42 | 0.14 | 1.80 | 0.12 | 0.56 | 0.02 | 0.45 | 0.03 | 0.64 | 0.02 | 0.22 | 0.01 | 0.18 | 0.01 | 0.26 | 0.02 |
Excluding Radiologists and Pathologists; SAS multiple GLM (General linear models) procedures were used to specify statistically significant differences (independent variables: Groups and Female). All esitimated parameters were significant at p<0.01. Post hoc test of group differences were all significant at p<0.01; Post hoc tests of gender differences were all significant at p<0.05.
Table 2.
Selected Physical and Mental Health Diagnosis in chronic opioid, acute opioid and non-opioid groups.
| Chronic Opioid | Acute Opioid | Non-Opioid | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Diagnosis in 2004 | All N=3726 |
Male N=1370 37% |
Female N=2356 63% |
All N=37108 |
Male N=16654 45% |
Female N=20454 55% |
All N=337366 |
Male N=164596 49% |
Female N=172770 51% |
|
| Pain | Muscle, Joint, and Limb Pain | 52.9% | 46.7% | 56.5% | 25.3% | 24.8% | 25.6% | 11.5% | 10.2% | 12.9% |
| Back Pain | 51.0% | 54.1% | 49.2% | 13.7% | 12.7% | 14.5% | 5.8% | 5.2% | 6.5% | |
| Arthritis | 33.3% | 26.9% | 37.1% | 7.0% | 6.2% | 7.6% | 3.6% | 2.7% | 4.6% | |
| Abdominal Pain | 21.2% | 16.8% | 23.7% | 14.3% | 11.0% | 17.1% | 5.6% | 4.2% | 6.9% | |
| Neck Pain | 20.0% | 18.5% | 20.8% | 6.2% | 5.1% | 7.2% | 2.7% | 2.1% | 3.2% | |
| Headache | 18.8% | 13.7% | 21.8% | 8.0% | 5.1% | 10.3% | 3.9% | 2.6% | 5.1% | |
| Other Physical Health | Hypertension (high blood pressure) | 43.1% | 40.5% | 44.6% | 18.5% | 18.8% | 18.3% | 13.7% | 13.1% | 14.2% |
| Endocrinological disorders (Diabetes mellitus or Hypothyroidism) | 23.5% | 19.4% | 25.9% | 10.4% | 7.7% | 12.5% | 7.7% | 5.9% | 9.4% | |
| Hyperlipidemia | 21.4% | 24.3% | 19.7% | 11.2% | 12.7% | 10.1% | 8.7% | 9.4% | 8.0% | |
| COPD | 12.7% | 9.0% | 14.9% | 5.5% | 4.9% | 6.0% | 4.3% | 4.1% | 4.4% | |
| Mental Health | Any Mental Health Diagnosis | 35.4% | 29.7% | 38.7% | 15.4% | 13.5% | 17.1% | 11.0% | 10.0% | 12.0% |
| Depression or Mood Disorders | 22.0% | 16.4% | 25.3% | 8.0% | 5.6% | 9.9% | 5.0% | 3.5% | 6.5% | |
| Anxiety Disorders | 11.0% | 9.2% | 12.0% | 4.2% | 3.1% | 5.0% | 2.7% | 2.0% | 3.4% | |
| Sbustance Abuse | Opioid Abuse/Dependence | 1.29% | 1.31% | 1.27% | 0.04% | 0.07% | 0.02% | 0.01% | 0.02% | 0.01% |
| Alcohol Related Psychiatric Disorder | 1.23% | 2.26% | 0.64% | 0.52% | 0.79% | 0.30% | 0.28% | 0.41% | 0.15% | |
SAS multiple logistic regression models (independent variables: Groups and Female) results: all estimated parameters were significant at p<0.01 except for “Alcohol Related Psychiatric Disorder” (p=0.16) between Acute Group and Non-Opioid Group; Post hoc test of group differences were all significant at p<0.01; Post hoc test showed gender differences were signicant in chronic group at p<0.05 except for Neck Pain (P=0.1), and Opioid abuse/dependence (p=0.91); Post hoc test of gender differences were significant in both Acute and non-opioid groups on all diagnosis (p<0.05) except for Muscle, Joint, and Limb Pain in Acute Group (P=0.09).
Results
Incidence of Acute and Chronic Pain and Use of Opioid Analgesics
Chronic opioid users received 1.42 (±0.01) prescriptions for an opioid each month, which provided an average of 29.83 (±0.23) DOS. By definition, the acute opioid group received 1 prescription in a year for <10 DOS and the non-opioid group none. While the vast majority of the chronic opioid group got their prescriptions from 1 doctor, 3.2% received opioid prescriptions from 2 or more doctors in one month for 6 or more months in the calendar year and 0.9% got the same opioid prescription from 2 or more doctors. In both instances, 70–75% of those individuals receiving redundant prescriptions were female. In terms of state-wide utilization of opioid analgesics, 2,933,275 DOS were prescribed and, although they represented less than 1% of the insured population, the chronic opioid group used 45% of the total.
Age & Gender of the Non-opioid, Acute opioid use and Chronic opioid use Groups
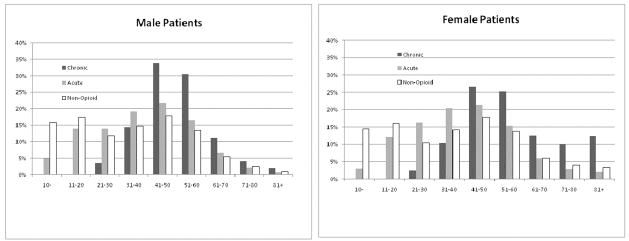
The average age of females in the non-opioid group was 36.51 (± 0.1) which was significantly older than males 33.57 (± 0.1). Females made up 51% of the non-opioid population. In sharp contrast, the chronic opioid group was on average about 20 years older than the non-opioid group with females substantially older on average (57.31 ± 0.3) than males (50.56 ± 0.3); the acute opioid use group was also significantly older than the non-opioid group, but not to the extent seen in the chronic group. These group averages obscure an important age × gender interaction which is shown in Figure 1. The age × gender frequency distribution in the chronic opioid use group was markedly skewed to the right (older) when compared to the acute opioid use group and the non-opioid insured population. This was true for both sexes but especially so in females. In terms of the acute opioid use group, the average age and frequency distribution were more like the population norms than the chronic opioid use group, but this group was none-the-less significantly older than the non-opioid group (Figure 1).
Figure 1.
The percent of the total males (left panel) and females (right panel) in the chronic opioid, acute opioid, and non-opioid control as a function of the age brackets shown.
Utilization of Medical Services and Incidence of Pain in Non-opioid, Acute opioid use and Chronic opioid use Groups
Table 1 shows the utilization of medical services for the three groups expressed as the mean (±SEM) per year. Clearly, chronic pain patients, in all respects, utilized more health services than either the acute opioid use group or the non-opioid insured group. In a broad sense, the three groups filed over 12 million medical claims during the year, but the chronic opioid group, representing only 0.65% of the total population, was responsible for over 5%. There was also a very large gender difference in all 3 groups with females filing significantly more insurance claims than males (table 1). With regard to all other indices of medical services utilization, the chronic opioid use group had many more ICD-9 coded physical and mental diseases, saw more doctors more often, and had significantly more emergency room visits, and days in the hospital. In all cases females utilized a much greater share of medical services than males. The acute opioid group fell between the chronic opioid but more closely compared to the non-opioid insured group.
Physical and Mental Health
Table 2 shows the pain diagnosis and other co-morbid physical, mental health and substance abuse disorders in the three groups. Muscle, joint and limb pain were the most frequent pain diagnoses in all 3 groups, but was diagnosed in more than 50% of the chronic opioid group. Back pain (51%), arthritis (33.3%), abdominal pain (21%), neck pain (20%) and headaches (19%) were the next most frequent diagnoses. Men and women within the chronic opioid use group also had a significantly greater burden of physical ailments (e.g. hypertension, endocrine disorders, hyperlidemia, chronic pulmonary obstructive disease [COPD]) than either the acute or non-opioid groups. Mental health disorders were found in 35% of all chronic opioid users which was significantly greater than that found in individuals in either the acute opioid or non-opioid population. Although there were some significant gender differences in pain and other physical disorders (table 2), this difference was considerably more prominent in psychopathology with women having many more psychiatric diagnoses than men.
Substance Abuse and Dependence
A diagnosis of opioid abuse and dependence was rare in all groups (table 2). However, the rates, at 1.31% in males and 1.27% in females in the chronic sample, were 31 and 128 times greater, respectively, than the rates observed in the non-opioid group. Pain patients were also several times more likely to have a diagnosis of an alcohol-related disorder (alcoholism and its complications) than the acute opioid group and non-opioid group. However, females had many fewer alcohol related problems that men in all groups but particularly so in the chronic pain group in which they were 4 times less common than in males. Moreover, the incidence of alcohol-related problems was 10–20 times greater than opioid abuse in the acute opioid and non-opioid samples, but they occurred with equal frequency in the chronic opioid group. However, there were clear gender differences in this respect. Males in the chronic opioid group had twice as many alcohol-related problems as opioid problems, but the opposite was true in females: opioid abuse was 2 times greater than alcohol abuse.
Specialties of Doctors Prescribing Opioids
Internists and family practitioners were the doctors seen most often by all three groups, but particularly for the chronic pain patients, 77% of whom were treated by internists. Less than a third of the chronic pain patients were managed by a pain management specialist. Moreover, despite the high incidence of muscle skeletal pain in the chronic opioid use group, only 3% saw a rheumatologist. Finally, although the prevalence of psychiatric disorders and substance abuse in this population was very high, only 9% received care from a psychiatrist.
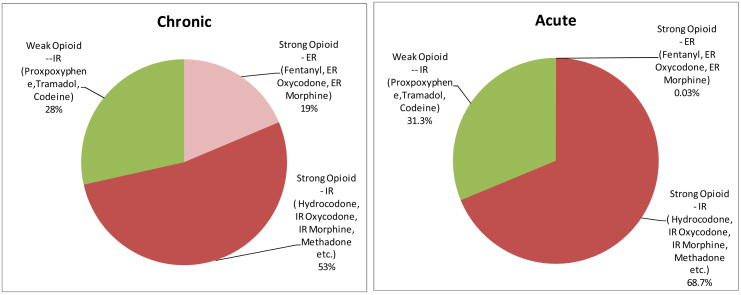
Types of Opioids Used
Figure 2 summarizes the different types of opioids prescribed in the chronic and acute opioid use groups. Extended release (ER) preparations of strong opioids were used much more frequently in the chronic opioid use group than in the acute group, although their use was still limited to only 19% of the group. The use of immediate release (IR) compounds (most often containing acetaminophen or ibuprophen), taken multiple times per day, still seemed to be the preferred choice of physicians in the chronic opioid use group (>80% utilized IR).
Figure 2.
The distribution, by percent, of the immediate release (IR) and extended release (ER) weak and strong opioids used by those in chronic pain (left panel) and acute pain (right panel)
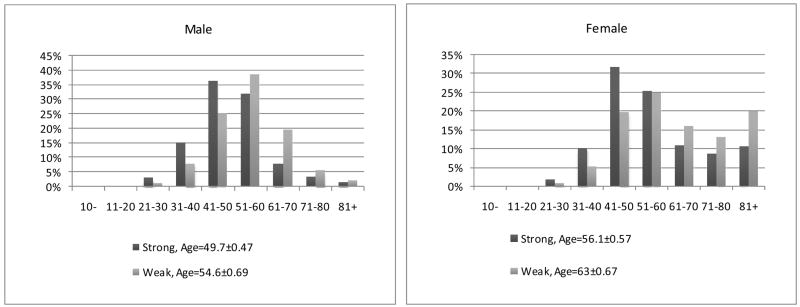
Health Status in Those Prescribed Weak or Strong Opioids
Figure 2 shows the distribution of weak versus strong opioids in the treatment of acute and chronic pain. Although a substantial majority of patients in chronic pain were treated with strong opioids, 28% were treated with weak opioids generally given many times a day. Figure 3 demonstrates a marked gender × age difference in the use of weak and strong opioids. The frequency distribution indicates two things: First, the use of all opioids in older females is markedly higher than in males; and, second, the older female opioid users were much more likely to be prescribed a weak opioid than a strong one. The health status of those prescribed weak and strong opioids are shown in Tables 3 and 4. Table 3 shows the health services utilization of those chronic pain patients treated with strong opioids, weak opioids and both, whereas table 4 shows the pain diagnosis, physical health problems and mental health status of the 4 groups. There was significant but rather small differences between those prescribed strong versus weak opioids, but those who used both were by far both physically and mentally more ill. It should be noted that no matter the opioid used, those in chronic pain were much more ill than the non-opioid insured group.
Figure 3.
The percent of the total females males (left panel) and males females (right panel) in the chronic opioid, stratified by the use of weak opioids, strong opioids, or both acute opioid, and non-opioid control as a function of the age brackets shown.
Table 3.
Health Service Utilization by the Chronic Opioid Group divided into those receiving weak opioids, strong opioids or both.
| Average Number of | Chronic Opioid-100% Strong | Chronic Opioid -both Weak and Strong | Chronic Opioid -100% Weak | Non-Opioid | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Male | Female | All | Male | Female | All | Male | Female | All | Male | Female | |||||||||||||
| N= 1400 | N= 610 44% | N= 790 56% | N=1460 | N= 490 34% | N= 970 66% | N= 866 | N= 270 31% | N= 596 69% | N=337366 | N=164596 49% | N=172770 51% | |||||||||||||
| # | S.E. | # | S.E. | # | S.E. | |||||||||||||||||||
| # of Insurance Claims | 156.18 | 3.41 | 132.42 | 4.55 | 174.53 | 4.81 | 201.19 | 3.99 | 182.26 | 6.40 | 210.75 | 5.03 | 136.72 | 3.89 | 108.43 | 5.17 | 149.54 | 5.07 | 28.54 | 0.08 | 23.23 | 0.10 | 33.60 | 0.12 |
| Mean of Distinct Diagnosed ICD9s | 18.91 | 0.35 | 16.40 | 0.51 | 20.84 | 0.47 | 24.40 | 0.39 | 21.34 | 0.65 | 25.96 | 0.47 | 17.11 | 0.41 | 13.84 | 0.58 | 18.55 | 0.52 | 7.79 | 0.01 | 6.64 | 0.01 | 8.76 | 0.02 |
| Doctors/Providers Seen by Patient* | 8.83 | 0.18 | 7.50 | 0.25 | 9.85 | 0.25 | 11.64 | 0.20 | 10.88 | 0.37 | 12.02 | 0.24 | 8.09 | 0.21 | 6.42 | 0.32 | 8.84 | 0.27 | 3.39 | 0.01 | 2.68 | 0.01 | 4.06 | 0.01 |
| Office Visits | 15.70 | 0.41 | 13.43 | 0.52 | 17.48 | 0.60 | 19.70 | 0.70 | 17.90 | 0.70 | 20.63 | 0.54 | 13.52 | 0.46 | 11.53 | 0.79 | 14.43 | 0.57 | 5.06 | 0.01 | 4.20 | 0.02 | 5.89 | 0.02 |
| ER Visits | 0.49 | 0.03 | 0.44 | 0.05 | 0.53 | 0.04 | 0.92 | 0.06 | 0.83 | 0.08 | 0.97 | 0.08 | 0.30 | 0.03 | 0.17 | 0.03 | 0.36 | 0.03 | 0.11 | 0.00 | 0.10 | 0.00 | 0.11 | 0.00 |
| Hospital Days | 1.53 | 0.15 | 1.12 | 0.18 | 1.85 | 0.23 | 2.27 | 0.16 | 2.30 | 0.29 | 2.26 | 0.19 | 0.85 | 0.12 | 0.50 | 0.12 | 1.00 | 0.17 | 0.22 | 0.01 | 0.18 | 0.01 | 0.26 | 0.02 |
SAS multiple GLM procedures of group and Gender differences are all significant (p<0.01). Post Hoc test of within group gender difference are all significant (p<0.01) except for Hospital Days in group strong, both and weak, and ER visit in group strong and both. Post Hoc test on group differences are all significant (p<0.01)
Table 4.
Selected Physical and Mental Health Diagnosis in chronic opioid users stratified by the use of weak opioids, strong opioids, or both.
| Diagnosis in 2004 | ChronicOpioid-100% Strong Only |
Chronic Opioid -both Weak and Strong |
Chronic Opioid -100% Weak Only |
Non-Opioid | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All N=1400 |
Male N=610 44% |
Female N=790 56% |
All N=1460 |
Male N=490 34% |
Female N=970 66% |
All N=866 |
Male N=270 31% |
Female N=596 69% |
All N=337366 |
Male N=164596 49% |
Female N=172770 51% |
||
| pain | Back Pain | 58.6% | 62.5% | 55.6% | 58.2% | 58.6% | 57.9% | 26.8% | 27.0% | 26.7% | 11.5% | 10.2% | 12.9% |
| Muscle, Joint and Limb Pain | 50.8% | 46.6% | 54.1% | 61.2% | 53.3% | 65.3% | 42.3% | 35.2% | 45.5% | 5.8% | 5.2% | 6.5% | |
| Arthritis | 30.4% | 23.9% | 35.3% | 35.8% | 29.8% | 38.9% | 33.8% | 28.1% | 36.4% | 3.6% | 2.7% | 4.6% | |
| Neck Pain | 21.1% | 19.5% | 22.3% | 25.1% | 23.5% | 25.9% | 9.6% | 7.4% | 10.6% | 5.6% | 4.2% | 6.9% | |
| Abdominal Pain | 19.6% | 14.8% | 23.4% | 27.6% | 24.1% | 29.4% | 12.8% | 8.1% | 14.9% | 2.7% | 2.1% | 3.2% | |
| Headache | 17.1% | 12.0% | 21.0% | 24.5% | 18.8% | 27.3% | 12.2% | 8.5% | 13.9% | 3.9% | 2.6% | 5.1% | |
| Other Physical Health | Hypertension (high blood pressure) | 38.7% | 38.5% | 38.9% | 43.0% | 41.0% | 44.0% | 50.2% | 44.1% | 53.0% | 13.7% | 13.1% | 14.2% |
| Endocrinological disorders (Diabetes mellitus or Hypothyroidism) | 21.7% | 18.9% | 23.9% | 23.2% | 18.0% | 25.9% | 27.0% | 23.3% | 28.7% | 7.7% | 5.9% | 9.4% | |
| Hyperlipidemia | 18.9% | 22.1% | 16.5% | 21.2% | 23.5% | 20.0% | 25.9% | 30.7% | 23.7% | 8.7% | 9.4% | 8.0% | |
| COPD | 12.9% | 9.2% | 15.7% | 13.9% | 9.2% | 16.3% | 10.4% | 8.1% | 11.4% | 4.3% | 4.1% | 4.4% | |
| Mental Health | Any Mental Health Diagnosis | 34.5% | 29.5% | 38.4% | 41.2% | 35.3% | 44.2% | 26.9% | 20.0% | 30.0% | 11.0% | 10.0% | 12.0% |
| Depression or Mood Disorders | 22% | 17% | 26% | 25.4% | 18.6% | 28.9% | 16.1% | 11.5% | 18.1% | 5.0% | 3.5% | 6.5% | |
| Anxiety Disorders | 11.4% | 10.3% | 12.3% | 13.4% | 10.8% | 14.6% | 6.1% | 3.7% | 7.2% | 2.7% | 2.0% | 3.4% | |
| Sbustance Abuse | Opioid Abuse/Dependence * | 0.93% | 1.48% | 0.51% | 2.33% | 1.63% | 2.68% | 0.12% | 0.37% | 0.00% | 0.01% | 0.02% | 0.01% |
| Alcohol Related Psychiatric Disorder | 1.43% | 2.46% | 0.63% | 1.23% | 2.04% | 0.82% | 0.92% | 2.22% | 0.34% | 0.28% | 0.41% | 0.15% | |
Please see the discussion for appropriate reservations about diagnosing abuse/dependence in those on chronic opioids
Substance abuse diagnosis in those prescribed strong and weak opioids
A diagnosis of opioid abuse was very low in the non- opioid insured population and was somewhat but significantly elevated in those in chronic pain treated with weak opioids. In contrast, the rate of an abuse diagnosis in those exposed to strong opioids, and particularly both strong and weak opioids, was much higher (10 to several hundred times greater) than in the weak opioid group and the non-opioid insured population.
Discussion
Although only 0.65% of the total insured population, those patients prescribed chronic opioids were much heavier consumers of all medical services than either the acute opioid or non-opioid groups. Collectively, these patients filed over 5% of all medical insurance claims, received 45% of all opioids prescribed in the state, had many more non-pain related physical disorders, more psychiatric co-morbidity, saw significantly more doctors, had more office and E.R. visits, and days in the hospital. As such, these data provide quantitative data to support prior extrapolations [8,12,13,19,20,23,24,26,27] that indicated that chronic pain patients have significant rates of co-morbid physical and mental health related problems and represent a disproportionately high percentage of those utilizing medical services. As a result, it seems clear, as stressed previously, [9,11] that any comprehensive pain management program should treat not only pain and the underlying physical disease state causing the pain, but other co-morbid physical and psychiatric conditions as well. Moreover, given the pharmacological complexity of managing pain with opioids, including breakthrough pain, the involvement of pain management specialists in the treatment plan for most of those in chronic pain seems appropriate to provide optimal treatment.
Our data suggest that at present such comprehensive pain management approaches may be relatively rare in actual practice: first, only a third of those receiving chronic opioid prescriptions were seen by a pain management specialist; second, a very high percentage (>80%) of the chronic pain patients had musculo-skeletal and joint pain but less than 4% were referred to the logical specialist, a rheumatologist; and, third, although 35% of those in chronic pain had a formal psychiatric diagnosis, less than 10% received psychiatric care. Moreover, while each physician must use his own clinical judgment about which opioid to use in each patient and for what condition, there were some puzzling findings which raise questions about some of the clinical judgments. For example, despite many systematic studies [1,21] over the past two decades, demonstrating that propoxyphene lacks efficacy any greater than over-the-counter drugs and may have safety issues, physicians still prescribed formulations containing this drug to 13 to 18% of patients in acute and chronic pain, respectively. In addition, despite the recommendation of all pain guidelines, only 19% of those in chronic pain were prescribed ER opioids far below what one would expect.
Our distinction between weak and strong opioids was, of course, arbitrary as was the decision to use the WHO analgesic ladder. Certainly, more contemporary sets of guidelines, such as those of the British and American Pain Society, emphasize the need for more clinical flexibility, but it seems to be acknowledged that the definition of weak versus strong opioids in the WHO analgesic ladder remains a common standard on an international level, particularly in third world countries which have not, or cannot, adopt their own set of guidelines.
An implicit assumption made in these studies is that the level of pain, its chronicity, the decision to use opioids and which ones – strong or weak – can be inferred from prescription data in an insurance database. While this may be true to a greater or lesser extent, there are many factors which are part of the decision to use opioids, including concerns about abuse potential, fear of side effects, cultural, socioeconomic concerns and so forth. Moreover, a physician seeing a patient in pain may have a number of reasons for using a particular opioid in a specific individual which may or may not comport with commonly accepted guidelines. For example, a physician may well decide to use a relatively weak opioid when a stronger one might be indicated because of patient intolerance to the side effects associated with very powerful opioids. Thus, in some cases, what would appear to be a questionable decision may in fact be the medically appropriate one. However, given that the vast majority of physicians are not pain management specialists, it seems doubtful that clinical judgment alone can explain the differences we observed (e.g., the use of propoxyphene, weak opioids in chronic pain, and so forth).
Although females constituted 51% of the non-opioid group, as the intensity and persistence of pain increased so did the percentage of females: 55% in the acute opioid use group and 63% of those in chronic pain. Moreover, there was a clear age × gender interaction. With increasing age, females became progressively more dominant, such that over 80% of the chronic pain sample age 61 or older was female. As important, females utilized all medical services to a much greater extent than males and the difference grew as a function of the degree of opioid use (chronic > acute > none). Moreover, as indicated above, there were striking gender × age differences in the use of strong and weak opioid with older females much more likely to receive a weak opioid than a strong one, in direct opposition to the pattern seen in males. To the extent that pain reflects the choice of which opioids to use – by no means a certainty – these data suggest one of two interpretations: First, older women have more pain than males, but it can be treated optimally with weaker opioids; or, second, physicians are more reluctant to use strong opioids in older females for any one of a number of reasons (e.g. fear of addiction, more severe adverse events, mental clouding, etc.). A final gender difference needs to be emphasized: a diagnosis of opioid abuse, while very high in both males and females in the chronic opioid group, was lower in females treated with either weak or strong opioids than males. However, it was very much higher in women prescribed both weak and chronic opioids. These data suggest that gender considerations need to be an integral part of any comprehensive pain management program [14,17].
There is a significant confound in our studies which cannot be easily addressed. Specifically, we cannot state with certainty whether any or all of the associations and correlations we have found in chronic pain patients on chronic opioids are due to the extensive use of opioids or the pain condition itself. However, given that those in chronic pain prescribed weak opioids had nearly the same co-morbid conditions as those prescribed strong opioids, it seems reasonable to infer that the use of strong opioids does not cause the co-morbidity chronic pain patients [6,7,11,12,18,19,22].
Our findings suggest that a diagnosis of opioid abuse is a relatively rare phenomenon in the chronic opioid use group but none-the-less was diagnosed more than 31 and 128 times greater in males and females respectively in the chronic pain patient administered strong opioid and several hundred times greater in those treated with both strong and weak opioids. These data are significant from two perspectives: first, females receiving chronic opioid therapy appear to be much more prone to be diagnosed with an opioid abuse problem than males; and, second, the incidence of dependence/abuse seems to be quite low at less than 2% of all patients in the chronic opioid group. The last conclusion – abuse being very low in the chronic opioid group – needs to be very carefully interpreted for a number of reasons: First, physicians are very hesitant to attach a label of substance abuse to their patients which could lead to a significant level of underreporting of substance abuse/dependence; second, we are not sure ICD-9 codes, used by physicians, can appropriately be used as an index of abuse defined by more appropriate criteria (e.g. DSM-IV or similar); and, finally, it is extraordinarily difficult to diagnose abuse or dependence using any diagnostic criteria in those maintained on chronic opioid administration. The latter is probably the most important point, since most patients on a chronic opioid regimen will develop tolerance and experience a withdrawal syndrome if the drug dosage is reduced, or the drug stopped abruptly. As a result, chronic pain patients on opioids easily meet two or more DSM-IV criteria for abuse or dependence (i.e. “pseudo-addiction”).
Despite the obvious strengths of using an insurance database to accurately and objectively determine co-morbidity in chronic pain patients, there are limitations in the use of such data. Most importantly, we have no way of knowing the motivation of physicians in using certain drugs, the factors which influence their diagnoses or their referral to specialists. Moreover, the physician who prescribed the opioid is not always known with a 100% certainty in the database. That is, although each prescription claim contains the Drug Enforcement Agency (DEA) number of the prescribing physician, it is often difficult to link this number back to the treating physician since many clinics, especially academic medical centers, have institutional DEA numbers shared by multiple physicians. One other limitation is also worth emphasizing: our data reflect only patients who were continually insured by a private insurance company in 2004 in the state of Missouri in the US. Thus, our data cannot be generalized to the entire population of pain patients in the US and elsewhere, because we have no information on those with no medical insurance at all or those covered by government programs such as Medicare or Medicaid in the United States.
Supplementary Material
Table 1. ICD-9 Codes for all diagnosed physical and psychiatric disorders.
Acknowledgments
This research was institutionally supported by unrestricted funds from the Department of Psychiatry, Washington University School of Medicine. No pharmaceutical company, or the insurance company providing the database, sponsored the research in any way. Theodore J. Cicero receives consulting fees from several pharmaceutical companies, none of which would have any particular interest in the outcome of these studies which were funded by an unrestricted grant from Washington University. Theodore J. Cicero had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Keith Isenberg and Gordon Wong provided the database and preliminary reports. Michael Lynskey, Alexandre Todorov, Yuhong Tian and Theodore Cicero designed the studies and prepared the reports. All of the above mentioned authors had full access to the data and assisted in the preparation of the datasets and this manuscript.
Supported in part by NIH grant DA 020791.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Barkin RL, Barkin SJ, Barkin DS. Propoxyphene (dextropropoxyphene): a critical review of a weak opioid analgesic that should remain in antiquity. Am J Ther. 2006 Nov-Dec;13(6):534–42. doi: 10.1097/01.mjt.0000253850.86480.fb. [DOI] [PubMed] [Google Scholar]
- 2.Blondell RD, Dodds HN, Blondell MN, Droz DC. Is the Kentucky prescription reporting system useful in the care of hospitalized patients? J Ky Med Assoc. 2004 Jan;102(1):15–9. [PubMed] [Google Scholar]
- 3.Cicero TJ, Nock B, Meyer E. Gender-linked difference in the expression of physical dependence in the rat. Pharmacol Biochem Behav. 2002;72:691–697. doi: 10.1016/s0091-3057(02)00740-2. [DOI] [PubMed] [Google Scholar]
- 4.Cicero TJ, Shores CN, Paradis AG, Ellis MS. Source of Drugs for Prescription Opioid Analgesic Abusers: A Role for the Internet? Pain Med. doi: 10.1111/j.1526–4637.2007.00323.x. Epub 20 August 2007. [DOI] [PubMed] [Google Scholar]
- 5.Cicero TJ, Surratt H, Inciardi JA. Relationship Between Therapeutic Use and Abuse of Opioid Analgesics in Rural, Suburban and Urban Locations in the United States. Pharmacoepidemiol Drug Saf. 2007;16(8):827–40. doi: 10.1002/pds.1452. [DOI] [PubMed] [Google Scholar]
- 6.Cicero TJ, Surratt HL, Inciardi J. Use and misuse of buprenorphine in the management of opioid addiction. J Opioid Manag. 2007 Nov–Dec;3(6):302–8. doi: 10.5055/jom.2007.0018. [DOI] [PubMed] [Google Scholar]
- 7.Cruciani R. Treatment of pain with opioids and the risk of opioid dependence: the search for a balance. Advances in Pain Management. 2008;2(1):2–3. [Google Scholar]
- 8.Edlund MJ, Sullivan M, Steffick D, Harris KM, Wells KB. Do users of regularly prescribed opioids have higher rates of substance use problems than nonusers? Pain Med. 2007 Nov–Dec;8(8):647–56. doi: 10.1111/j.1526-4637.2006.00200.x. [DOI] [PubMed] [Google Scholar]
- 9.Flor H, Fydrich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: a meta-analytic review. Pain. 1992 May;49(2):221–30. doi: 10.1016/0304-3959(92)90145-2. [DOI] [PubMed] [Google Scholar]
- 10.Fontana JS. The social and political forces affecting prescribing practices for chronic pain. J Prof Nurs. 2008 Jan–Feb;24(1):30–5. doi: 10.1016/j.profnurs.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Gatchel RJ, Okifuji A. Evidence-based scientific data documenting the treatment and cost-effectiveness of comprehensive pain programs for chronic nonmalignant pain. J Pain. 2006 Nov;7(11):779–93. doi: 10.1016/j.jpain.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Saplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004 Aug;61(8):807–16. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 13.Green CR, Wheeler JR, LaPorte F, Marchant B, Guerrero E. How well is chronic pain managed? Who does it well? Pain Med. 2002 Mar;3(1):56–65. doi: 10.1046/j.1526-4637.2002.02003.x. [DOI] [PubMed] [Google Scholar]
- 14.Greenspan JD, Craft RM, LeResche L, Arendt-Nielsen L, Berkley KJ, Fillingim RB, Gold MS, Holdcroft A, Lautenbacher S, Mayer EA, Mogil JS, Murphy AZ, Traub RJ. Consensus Working Group of the Sex, Gender, and Pain SIG of the IASP. Studying sex and gender differences in pain and analgesia: a consensus report. Pain. 2007 Nov;132(Suppl 1):S26–45. doi: 10.1016/j.pain.2007.10.014. Epub 2007 Oct 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Griswold KS, Aronoff H, Kernan JB, Kahn LS. Adolescent substance use and abuse: recognition and management. Am Fam Physician. 2008 Feb 1;77(3):331–6. [PubMed] [Google Scholar]
- 16.Ives TJ, Chelminski PR, Hammett-Stabler CA, Malone RM, Perhac JS, Potisek NM, Shilliday BB, DeWalt DA, Pignone MP. Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Serv Res. 2006 Apr 4;6:46. doi: 10.1186/1472-6963-6-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keogh E, McCracken LM, Eccleston C. Do men and women differ in their response to interdisciplinary chronic pain management? Pain. 2005 Mar;114(1–2):37–46. doi: 10.1016/j.pain.2004.12.009. Epub 2005 Jan 22. [DOI] [PubMed] [Google Scholar]
- 18.Loyd DR, Morgan MM, Murphy AZ. Sexually dimorphic activation of the periaqueductal gray-rostral ventromedial medullary circuit during the development of tolerance to morphine in the rat. Eur J Neurosci. 2008 Mar;27(6):1517–24. doi: 10.1111/j.1460-9568.2008.06100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mata M, Hao S, Fink DJ. Applications of gene therapy to the treatment of chronic pain. Curr Gene Ther. 2008 Feb;8(1):42–8. doi: 10.2174/156652308783688527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meisler JD. Toward Optimal Health: The Experts Discuss Chronic Pain. J Womens Health Gend Based Med. 2002 May;11(4):341–5. doi: 10.1089/152460902317585976. [DOI] [PubMed] [Google Scholar]
- 21.Miller RR. Propoxyphene: a review. Am J Hosp Pharm. 1977 Apr;34(4):413–23. [PubMed] [Google Scholar]
- 22.Passik SD, Kirsh KL. Appropriate Prescribing of Opioids and Associated Risk Minimization. Advances in Pain Management. 2008;2(1):9–16. [Google Scholar]
- 23.Portenoy RK. Current pharmacotherapy of chronic pain. J Pain Symptom Manage. 2000 Jan;19(1 Suppl):S16–20. doi: 10.1016/s0885-3924(99)00124-4. [DOI] [PubMed] [Google Scholar]
- 24.Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990 Nov 21;264(19):2511–8. [PubMed] [Google Scholar]
- 25.Spandorfer JM, Israel Y, Turner BJ. Primary care physicians’ views on screening and management of alcohol abuse: inconsistencies with national guidelines. J Fam Pract. 1999 Nov;48(11):899–902. [PubMed] [Google Scholar]
- 26.Sullivan MD, Edlund MJ, Steffick D, Unützer J. Regular use of prescribed opioids: association with common psychiatric disorders. Pain. 2005 Dec 15;119(1–3):95–103. doi: 10.1016/j.pain.2005.09.020. Epub 2005 Nov 17. [DOI] [PubMed] [Google Scholar]
- 27.Sullivan MD, Edlund MJ, Zhang L, Unützer J, Wells KB. Association between mental health disorders, problem drug use, and regular prescription opioid use. Arch Intern Med. 2006 Oct 23;166(19):2087–93. doi: 10.1001/archinte.166.19.2087. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. [Accessed on 9/24/2008]; http://www.who.int/cancer/palliative/painladder/en/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table 1. ICD-9 Codes for all diagnosed physical and psychiatric disorders.