Abstract
This paper reports relationships between methamphetamine use and behaviors and social influences using data from a population-based survey of 8th- and 11th-grade students in Oregon for the 2001–2003 school years. We analyze methamphetamine use within a general problem behavior framework to identify malleable correlates of behavior for future prevention interventions. We specifically test two models of methamphetamine use employing logistic regression analysis: one comprised of behaviors and traits of the individual students and another focusing on peer and parental influences. This study finds adolescent methamphetamine use related to several problem behaviors. However, the specific problems vary by grade and are moderated by gender. Findings indicate the need for tailored interventions targeting gender/grade-specific behaviors or problems such as antisocial activities, risky sex, and depression, as well as social influences such as peers engaging in antisocial behaviors or using drugs and parents favoring drug use or poorly monitoring or setting limits for their children.
Keywords: Methamphetamine use, adolescents, behavioral and social correlates, logistic regression analysis, comorbidities, tailored interventions
1. Introduction
About five million Americans have tried methamphetamine (Anglin, Burke, Perrochet, Stamper, & Dawud-Noursi, 2000). Some states or parts of states—particularly rural areas—report epidemics of methamphetamine use, especially on the West Coast, in the Midwest and in the South (Booth, Leukefeld, Falck, Wang, & Carlson, 2006; Butterfield, Malliarakis, & Dotson, 2002; Colnar, Rawson, Marinelli-Casey, Gallagher, & Herrell, 1999; Glittenberg & Anderson, 1999; Haight et al., 2005; Lineberry & Bostwick, 2006; Rawson, Anglin, & Ling, 2002; Sexton et al., 2005). Methamphetamine use is now spreading across the United States although overall national prevalence may be leveling off (Office of National Drug Control Policy, 2006).
According to the National Survey of Drug Use and Health, lifetime use of methamphetamine by those 12 and older has ranged from 4.3% in 1999 to a peak of 5.3% in 2002 before falling to 4.9% in 2004 (Substance Abuse and Mental Health Services Administration, 2005). In terms of youth, The Monitoring the Future Study shows past year methamphetamine prevalence for high school seniors at 1.5% in 2001 with a slight decline to 1.1% in 2006 (Interuniversity Consortium for Political and Social Research, 2007). The Youth Risk Behavior Survey of 9th–12th graders shows lifetime prevalence declining from 9.8% in 2001 to 4.4% in 2007 (Centers for Disease Control and Prevention, 2008).
The Oregon Healthy Teen (OHT) survey indicated that lifetime use of methamphetamine by 8th and 11th graders was 5.1% for the 2000–2001 school year and 3.0% for the 2006–2007 school year. While Oregon once had an abundance of methamphetamine labs, the number of methamphetamine labs reported by Oregon law enforcement declined by 96% during a recent four-year period (from 473 in 2003 to just 17 in 2007). The decline was due mostly to tougher enforcement and stricter control of pseudoephedrine—an over-the-counter cold remedy that is a key ingredient for methamphetamine—under recent laws passed by the Oregon Legislature and Congress (National Drug Intelligence Center, 2007).
The proximal impact of methamphetamine use is disproportionate to its prevalence and typically has immediate adverse health effects, with some groups suffering more than others the consequences of its use and abuse. These include Native Americans (Freese, Obert, Dickow, Cohen, & Lord, 2000; Glittenberg & Anderson, 1999) and adolescent and young women of childbearing years (Freese et al., 2000; Haight et al., 2005; Morgan & Joe, 1996; Paschane, Fisher, Cagle, & Fenaughty, 1998). Other populations disparately affected include gay and bisexual men (Centers for Disease Control and Prevention, 2006; Freese et al., 2000; Halkitis, Parsons, & Stirratt, 2001; Sanello, 2005) and criminal justice populations (Freese et al., 2000; McCarthy & Waters, 2003; Stoops, Tindall, Mateyoke-Scrivner, & Leukefeld, 2005).
Methamphetamine addiction has major health and safety consequences in the U.S. and other countries (Banken, 2004; Kraus et al., 2003; Sattah et al., 2002; Suwanwela & Poshyachinda, 1986; Wada, Greberman, Konuma, & Hirai, 1999; Wilkins, Pledger, Bhatta, & Casswell, 2004). Serious cardiovascular problems are common among male users (Brecht, O’Brien, Mayrhauser, & Anglin, 2004; Chan, Chen, Lee, & Deng, 1994; Hong, Matsuyama, & Nur, 1991; Perez, Jr., Arsura, & Strategos, 1999; Richards, Johnson, Stark, & Derlet, 1999; Wijetunga, Bhan, Lindsay, & Karch, 2004; Wolkoff, 1997; Yu, Larson, & Watson, 2003), putting a strain on the budgets of local governments. Serious psychiatric disorders emerge or worsen due to its use (Brecht et al., 2004; Liebowitz, McGrath, & Bush, 1980; Meredith, Jaffe, Ang-Lee, & Saxon, 2005; Roberts, Yeager, & Siegel, 2003; Shoptaw, Peck, Reback, & Rotheram-Fuller, 2003; Zweben et al., 2004), including increased risk of suicidality (Yen & Shieh, 2005). Emergency care and first responders bear a considerable burden related to meth use (Centers for Disease Control and Prevention, 2000; Lineberry & Bostwick, 2006).
Early sexual behavior and frequent unprotected sex among heterosexual and homosexual users of methamphetamine result in higher rates of Hepatitis and HIV infection rates (Davis, Kalousek, & Rubenstein, 1970; Gorman, 2003; Greenwell & Brecht, 2003; Harkess, Gildon, & Istre, 1989; Hutin et al., 2000; Koester, Glanz, & Barón, 2005; Meyer, 2003; Molitor, Truax, Ruiz, & Sun, 1998; Urbina & Jones, 2004; Vogt et al., 2006). Methamphetamine use interferes with the efficacy of HIV medications and treatment (Anonymous, 2004; Boddiger, 2005; Jernigan et al., 2005). In many jurisdictions, the consequences of methamphetamine use overwhelm trauma systems (Embry, Lopez, & Minugh, 2005; Rockett, Putnam, Jia, & Smith, 2006; Schermer & Wisner, 1999; Tominaga, Garcia, Dzierba, & Wong, 2004).
Many newborns and infants are exposed to methamphetamine directly (toxic exposure) or indirectly (through abusive or neglectful parenting), with significant impact on child-protective services and healthcare in some jurisdictions (Buchi, Zone, Langheinrich, & Varner, 2003; Plessinger, 1998; Smith et al., 2003; Thadani, 1995; Won, Bubula, McCoy, & Heller, 2001). While research indicates that treatment outcomes for methamphetamine users are similar to those of other drug users (Luchansky, 2003; Otero, Boles, Young, & Dennis, 2006; Rawson et al., 2000), the lack of treatment opportunities leaves many users underserved.
Public safety issues loom large with methamphetamine use. Children of meth users are more likely to suffer abuse, neglect, and exposure to toxins besides methamphetamine (Cohen et al., 2003; Grella, Hser, & Huang, 2006). Child and adult homicides or other acts of violence attributable to methamphetamine are serious concerns in localities with high rates of the drug’s use (Bailey & Shaw, 1989; Schermer & Wisner, 1999; Slade, Daniel, & Heisler, 1991; Tominaga et al., 2004; Zhu et al., 2000). Its manufacture and sale also create substantial risk of environmental toxin exposure for multiple parties (Allcott, Barnhart, & Mooney, 1987; Anonymous, 2003).
The political and economic impact of methamphetamine use is another concern. Some industries (e.g., trucking, mining, and mineral extraction) have high rates of methamphetamine use, which contributes to accidents and other losses (as demonstrated in Brazilian research by (Silva, Greve, Yonamine, & Leyton, 2003). Forensic studies have shown the lifetime costs of methamphetamine exposure to adults and their children to exceed $1.5 million per user, when examining costs across special education, child-protective services, criminal justice, mental health, healthcare, and other domains (McDaniel & Embry, 2001)
Thus, the prevention of early use of methamphetamine could have many health, public safety, and political benefits (Greenwell & Brecht, 2003). Epidemiological analysis of methamphetamine initiation among adolescents could contribute to the development of prevention efforts. Researchers have published two such studies of youth thus far. Herman-Stahl, Krebs, Kroutil, & Heller (2006) used data from the 2002 National Survey of Drug Use and Health (Substance Abuse and Mental Health Services Administration, 2003) to examine the demographic, psychosocial, and behavioral correlates of illicit stimulant use among adolescents aged 12 through 17. They found mental health treatment utilization correlated with use of marijuana and other illegal drugs as well as nonmedical use of amphetamine. Females reporting low religiosity, binge drinking, and selling drugs were more likely to use methamphetamine than were males or individuals who did not report these attitudes or behaviors.
Springer, Peters, Shegog, White, and Kelder (2007) analyzed methamphetamine use among a nationally representative sample of high school students who completed the Youth Risk Behavior Survey. They found the prevalence of ever having used methamphetamine was comparable to that for cocaine, but double the rate for heroin. Males reported slightly higher use than females and the rates were higher among white and Hispanic students than among black students. Those who had used the drug more than four times were significantly more likely to report having engaged in risky sexual behavior. Springer et al. (2007) did not examine the relationship of methamphetamine use to other behaviors or other risk factors.
In the present study, we examined methamphetamine use in a population-based sample of 8th- and 11th-grade adolescents in the State of Oregon. In addition to analyzing the prevalence of use, we examined the relationship between methamphetamine use and a broad range of other problem behaviors, as well as several well-established risk factors for the use of other drugs. Based on extensive evidence of the relationship among diverse adolescent problem behaviors (Biglan et al., 2004), we expected that methamphetamine use would be related to engaging in other problem behaviors.
We also examined social factors one could relate to methamphetamine use, since they would point to malleable influences on use that prevention interventions could target. We selected both family and peer correlates for our analyses based on prior social ecological research on general environmental factors, especially family dynamics, associated with drug use (Dishion, Kavanagh, Schneiger, Nelson, & Kaufman, 2002) and on social developmental research focusing upon a specific array of risk factors related to a variety of problem behaviors (Hawkins et al., 1992; Hawkins, Van Horn, & Arthur, 2004). Specifically, we included peer antisocial behavior, peer drug use, parent attitudes favorable to antisocial behavior and drug use, family conflict, and inadequate parental rule setting, rule enforcement, and monitoring.
2. Methods
2.1. Design
This paper examines the variability of self-reported methamphetamine use by Oregon teenagers using data collected from population-based samples of 8th- and 11th-grade anonymous respondents. This and other information on adolescent wellbeing came from three consecutive years of assessments from the Oregon Healthy Teens survey (2001–2003).
We attempted to survey all of the 8th- and 11th-grade students in selected schools (see below) annually over the three-year period from 2001 to 2003. We assessed the same schools, but different birth cohorts, each year. Approximately four weeks before survey administration, project staff mailed parent notification letters to the students’ homes, with instructions to notify the school if they wished their child not to participate. Research staff administered anonymous student questionnaires in classrooms during regular school periods, and students learned their participation was voluntary. Parents of 5% of the students wished their children not to participate, and an additional 2% of the students chose not to participate. In addition, another 14% of the students listed on class rosters were absent the day of the survey, bringing the student participation rate to 79%. This participation rate did not vary systematically across communities.
2.2. Participants
We used a cluster-sampling frame compatible with existing state and federal surveillance systems to identify a set of Primary Sampling Units (PSUs) consisting of high schools and the middle, junior, or elementary schools feeding into them. For the 11th-grade surveys, school and PSU are equivalent, as the high school defined the PSU. However, in some cases, two or more middle schools fed into a single high school. For this reason, we modeled individual students within schools, not in PSUs, and we chose to analyze the overall dataset as well as to conduct separate analyses for the 8th and 11th grades.
In Table 1, we report the overall number of schools in the sample for 2001–2003. Also included are breakdowns for each grade (8th and 11th) and community type. There were more middle schools than high schools since all feeder schools to a given high school were included. There were also a greater number of urban than rural schools in the sample.
Table 1.
Sample characteristics: schools—Oregon Health Teen Survey: 2001–2003
| Total population | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | 8th grade | 11th grade | |||||||||
| Number | Percent | Number | Percent | Number | Percent | ||||||
| 211 | 100 | 123 | 58.3 | 88 | 41.7 | ||||||
|
| |||||||||||
| Community type | |||||||||||
| Overall | 8th grade | 11th grade | |||||||||
| Urban | Rural | Urban | Rural | Urban | Rural | ||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % |
| 127 | 60.2 | 84 | 39.8 | 80 | 65.0 | 43 | 35.0 | 47 | 53.4 | 41 | 46.6 |
In Table 2, we report the overall number of individual respondents in the sample (each broken down by grade, gender, and if the student was white or nonwhite). As shown, whites, females, and eighth graders made up the greater numbers in our sample than nonwhite, males, and 11th graders.
Table 2.
Sample Characteristics: Individual Respondents—Oregon Health Teen Survey: 2001–2003
| Total population | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | 8th Grade | 11th Grade | |||||||||
| Count | Percent | Count | Percent | Count | Percent | ||||||
| 5,298 | 100.0 | 2,929 | 55.3 | 2,369 | 44.7 | ||||||
|
| |||||||||||
| Gender | |||||||||||
| Overall | 8th Grade | 11th Grade | |||||||||
| Male | Female | Male | Female | Male | Female | ||||||
| Count | % | Count | % | Count | % | Count | % | Count | % | Count | % |
| 2,435 | 47.5 | 2,691 | 52.5 | 1,326 | 46.3 | 1,535 | 53.7 | 1,109 | 49.0 | 1,156 | 51.0 |
|
| |||||||||||
| Race | |||||||||||
| Overall | 8th Grade | 11th Grade | |||||||||
| White | Nonwhite | White | Nonwhite | White | Nonwhite | ||||||
| Count | % | Count | % | Count | % | Count | % | Count | % | Count | % |
| 4,139 | 83.2 | 833 | 16.8 | 2,240 | 82.7 | 468 | 17.3 | 1,899 | 83.9 | 365 | 16.1 |
The effective sample size for this analysis was a subset of the total sample, due to the modular approach taken for survey administration. The survey included a demographics section and six modules; each student received one of the 20 different versions of the survey, with each version including the demographics section and three modules. Research assistants varied module order so that missing values due to failure to reach the end would follow a random pattern. With this construction, about half of the students received any given item. Of those receiving an item, about 1.8 to 3.6% did not answer it. Since the number of students who failed to respond to individual items was very low, we did not attempt any methods to recover the missing data, such as imputation. We analyzed cases with complete data only.
2.3. Measures
Both theoretical and empirical considerations drove our model identification and specification. Theoretically, social ecological models of adolescent problem behaviors (Dishion, 1990; Dishion & Andrews, 1995; Dishion & McMahon, 1997; Dishion, Patterson, & Kavanagh, 1992; Dishion, Patterson, Stoolmiller, & Skinner, 1991), social developmental perspectives focused on risk and protective factors (Arthur, Hawkins, Pollard, Catalano, & Baglioni, 2002; Hawkins et al., 1992; Hawkins et al., 2004), and the functional contextualism approach (Biglan, Duncan, Ary, & Smolkowski, 1995; Biglan, Ary, Smolkowski, Duncan, & Black, 2000; Biglan et al., 2004; Metzler, Biglan, Ary, & Li, 1998) informed this analysis. We used inferential statistics including correlation and confirmatory factor analyses to identify distinct models containing sets of mutually exclusive independent variables that were deemed statistically and theoretically relevant.
2.3.1. Student behavior
The first model focuses on the behaviors and characteristics of the teenager as an individual. The dependent variable is lifetime use of methamphetamine and the independent variables include correlates reflecting use of other substances (tobacco, alcohol, and marijuana), adolescent problem behaviors (antisocial activities and, initially, sensation seeking), academics (grades and truancy), and child traits/experiences (depression, suicide). We considered these intra-individual correlates statistically and theoretically distinct from the inter-individual variables we discuss in Model #2 (see below).
Items on drug use included cigarette smoking, alcohol (with a separate item for binge drinking), and marijuana use. Items came from the Youth Risk Behavior Survey (Kann et al., 2000), the Communities That Care assessment (Arthur et al., 2002), and surveys developed at the Oregon Research Institute in previous studies of tobacco (Biglan et al., 2000) and other substance use (Metzler et al., 1998). The substance use measures included as independent variables in this analysis assess use within the past month. Our dependent variable, use of methamphetamine, is a lifetime rather than 30-day measure.
We based the antisocial behavior measure on multiple items first used by Elliott, Busse, and Gresham (1993). Students answered questions about school suspensions, stealing something worth over $10, stealing a motor vehicle, attacking someone, having the police stop or arrest them, and fighting with a weapon. This measure reflects a self-reported number of these events in the past three months. We based sensation seeking on multiple items also. Students answered questions about how often they had done small dangerous things, how often they had done things because of a dare, and how often they had done things just because it felt good to do them.
After multiple analyses, we decided to replace the sensation-seeking correlate with a measure of risky sexual behavior. We did this for two reasons. There was a high correlation between sensation seeking and a number of other variables in the model. Second, risky sexual behavior was associated with larger odds ratios than sensation seeking was, especially for 11th graders. The risky sexual behavior measure consisted of multiple items: students reported if they had engaged in sex during the past three months, if they had used a condom or other form of birth control, and if they had made someone pregnant or had become pregnant themselves.
Students’ self-reported grades consisted of responses to single items asking them to indicate how they would describe their grades in the past 12 months. Choices included “mostly As” through “mostly Fs” plus “none of these” and “not sure.” Students’ self-reports of grades have been shown to provide a reasonably valid estimate of objectively measured grades (Crockett, Schulenberg, & Petersen, 1987). Truancy has its basis in a single item: teenagers reported how many times they had skipped school the past four weeks.
Our depression measure had four items from the Center for Epidemiological Studies, Depression (CES-D) scale, shown to predict a depression diagnosis among adolescents (Seeley, Rohde, Lewinsohn, & Clarke, 2002). Teenagers responded if, during the past week, they had a poor appetite, felt depressed, felt sad, or had low energy. The suicide measure consisted of one item: if students had made an actual suicide attempt in the past year.
2.3.2. Parent and peer influences
The second model focuses on the familial and peer environment of the teens. The dependent variable again is use of methamphetamine, and the independent variables include contextual correlates reflecting the teens’ families (poor management, high conflict, and favorable attitudes to drug use or to antisocial behavior) and peers (antisocial activities, drug use). We considered these inter-individual correlates statistically and theoretically distinct from the intra-individual variables included in Model #1.
The family domain included six measures: high family conflict, parental attitudes favorable to drug use, parental attitudes favorable to antisocial behavior, and, initially, a measure of poor family management. The high family conflict measure included three items: if the teen’s family members frequently insulted each other, had serious arguments, or argued about the same things repeatedly. The parental attitudes favorable to drug use measure consisted of two items: if the parent/parents thought it was wrong to drink alcohol or to smoke marijuana. Parental attitudes favorable to antisocial behavior included three items: whether their parent(s) thought it was wrong to steal, to draw graffiti, or to pick a fight with someone.
After multiple analyses, we decided the poor family management index was simply too complex to yield useful findings. We split this index into three separate parental measures: unclear rule setting, inconsistent rule enforcement, and poor monitoring. The unclear parental rule setting measure consisted of one item regarding the clarity of rules in the teen’s family. We measured parental rule enforcement based on student report of the parents’ response to breaking a rule using a 7-item scale: (1) noticed but did nothing in response, (2) raised their voice (scolded, yelled), (3) made the teen correct the problem, (4) threatened to punish the teen (but did nothing), (5) spanked the teen, (6) slapped or hit the teen (other than spanking), and/or (7) discussed the problem with the teen and asked questions. The poor parental monitoring measure consisted of three items: if parents asked if the teen completed his/her homework, if parents knew if the teen came home late, and/or if parents knew where the teen was when not at home.
The peer domain included two measures: interaction with antisocial peers and friends’ use of drugs. The measure assessing interaction with antisocial peers consisted of six items. Students were asked how many of their four best friends during the past year had (1) been suspended, (2) carried a handgun, (3) sold illegal drugs, (4) stolen a car, (5) dropped out of school, or (6) been arrested. The friends’ use of drugs measure included four items. Teenagers indicated if, during the past year, their best friend(s) had smoked tobacco, tried alcohol, smoked marijuana, or used LSD.
3. Results
3.1. Prevalence of Methamphetamine Use
To describe trends in methamphetamine use among Oregon teens during 2001–2003, we report prevalence rates for the overall sample and for grade and gender subsamples. Table 3 shows that prevalence declined very slightly over the three years for both grades and both genders. Note that females have self-reported prevalence rates slightly higher than those for males, something uncommon for many of the other substance use measures we track (though at p = .088, gender differences were marginally significant statistically).
Table 3.
Use of Methamphetamine—Oregon Health Teen Survey: 2001–2003
| Prevalence (%) |
|||
|---|---|---|---|
| Total Population | Overall | 8th Grade | 11th Grade |
| 2001 | 5.1 | 3.9 | 6.7 |
| 2002 | 4.2 | 3.1 | 5.6 |
| 2003 | 4.6 | 3.9 | 5.5 |
| 2001–2003 | 4.6 | 3.6 | 5.9 |
|
| |||
| Males | Overall | 8th Grade | 11th Grade |
| 2001 | 4.7 | 3.6 | 6.1 |
| 2002 | 4.1 | 2.8 | 5.7 |
| 2003 | 4.3 | 3.7 | 5.1 |
| 2001–2003 | 4.3 | 3.3 | 5.6 |
|
| |||
| Females | Overall | 8th Grade | 11th Grade |
| 2001 | 5.3 | 4.1 | 6.8 |
| 2002 | 4.3 | 3.4 | 5.5 |
| 2003 | 4.8 | 4.0 | 6.0 |
| 2001–2003 | 4.8 | 3.8 | 6.0 |
3.2. Methamphetamine use in relation to other problem behaviors and risk factors
Table 4 shows prevalence rates for numerous problem behaviors and risk factors categorized by whether or not respondents reported using methamphetamine. As shown, prevalence is often four to five times higher for those who report using methamphetamine than for those reporting no use. Of particular interest is that nearly half (45.1%) of those reporting methamphetamine use also report using other hard drugs (cocaine, heroin, ecstasy, or LSD).
Table 4.
Problem Behaviors by Methamphetamine Use—Oregon Health Teen Survey: 2001–2003
| Methamphetamine use—prevalence |
||||
|---|---|---|---|---|
| Problem behaviors | Yes | No | Significance | |
| Antisocial behavior | 8.8% | 2 | 3.9% | p < .001 |
| Risky sex | 7.4% | 6 | 18.6% | p < .001 |
| Depression | 5.6% | 4 | 20.9% | p < .001 |
| Suicide attempt | 5.4% | 2 | 5.6% | p < .001 |
| Tobacco use | 2.9% | 6 | 11.9% | p < .001 |
| Alcohol use | 0.5% | 8 | 30.0% | p < .001 |
| Binge drinking | 0.8% | 6 | 14.0% | p < .001 |
| Marijuana use | 0.7% | 7 | 14.0% | p < .001 |
| Interaction with antisocial peers | 5.7% | 8 | 40.1% | p < .001 |
| Peers’ use of drugs | 5.1% | 8 | 33.8% | p < .001 |
| Parents favor antisocial behavior | 9.1% | 6 | 47.4% | p < .001 |
| Parents favor drug use | 6.9% | 6 | 36.2% | p < .001 |
| High family conflict | 6.1% | 5 | 36.9% | p < .001 |
| Rule setting | 4.0% | 3 | 15.2% | p < .001 |
| Rule enforcement | 9.0% | 5 | 40.1% | p < .001 |
| Parental monitoring | 0.7% | 6 | 33.8% | p < .001 |
In addition to the relationship of methamphetamine use to specific problem behaviors, we were interested in the association between methamphetamine use and the total number of distinct problem behaviors.
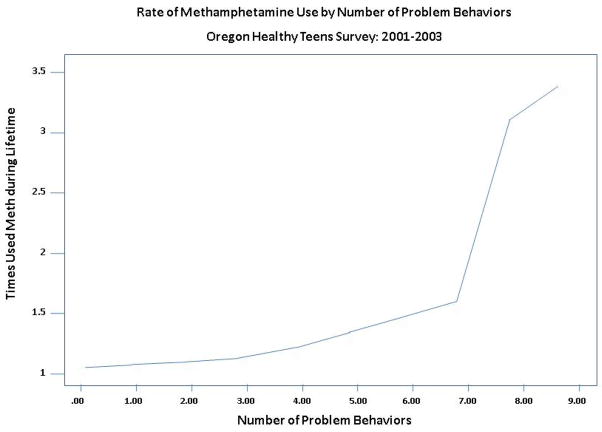
Figure 1 shows the relationship of methamphetamine use to the total number of other problem behaviors. As shown, the probability of methamphetamine use increases dramatically for young people with six or more other problems.
3.3. Analysis of models
We used two models in an attempt to explain the variance at the individual level in methamphetamine use: one that focuses on behaviors and characteristics of the teenager as an individual and another that focuses on familial and peer influences that may be manipulable. We began our analysis initially using a multilevel modeling approach to determine if there was significant variation in methamphetamine use between schools. However, we abandoned school-level analysis once multilevel analysis revealed that we could attribute more than 98% of the variance in methamphetamine use to individual-level variation (Smolkowski, Biglan, Dent, & Seeley, 2006) and less than 2% occurred at the school level. For this reason, we determined that a more traditional statistical approach, logistic regression, was appropriate for the individual-level analysis (Cox & Snell, 1989; DeMaris, 1992; Forrester, Biglan, Severson, & Smolkowski, 2007; Hosmer & Lemeshow, 1989; Jaccard, 2001; McKelvey & Zavoina, 1994; Menard, 2002; Pampel, 2000). For this set of analyses, we used the Statistical Package for the Social Sciences, Windows Version 15.0, Release 15.0.0.249 (SPSS, 2006).
3.4. Model 1: Relationship of other problem behaviors to methamphetamine use
Table 5 presents the results of logistic regression analyses relating methamphetamine use to other problem behaviors. Inspection of the results indicates that correlates of methamphetamine use differed according to both gender and grade. We therefore present results separately for each grade using gender as a factor in the analyses.
Table 5.
Logistic Regression Analysis (Y = Methamphetamine), Model #1
| Eighth Grade | Eleventh Grade | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Model Fit |
Model Fit |
||||||||
| Cases | 1,400 | Cases | 1,213 | ||||||
| AIC | 260.508 | AIC | 422.994 | ||||||
| Chi-square | 160.333 | Chi-square | 124.767 | ||||||
| Significance | 0.000 | Significance | 0.000 | ||||||
| Pseudo R2 | 0.108 | Pseudo R2 | 0.098 | ||||||
|
| |||||||||
| Independent variables | Odds Ratio: Exp(B) | Statistical Significance |
C.I. |
Independent variables | Odds Ratio: Exp(B) | Statistical Significance |
C.I. |
||
| Lower | Upper | Lower | Upper | ||||||
|
| |||||||||
| Antisocial behavior | 3.62 | 0.000 | 1.87 | 7.02 | Antisocial Behavior | 1.76 | 0.074 | 0.95 | 3.29 |
| Risky sex | 1.45 | 0.112 | 0.92 | 2.29 | Risky Sex | 2.41 | 0.000 | 1.68 | 3.47 |
| Depression | 1.28 | 0.300 | 0.80 | 2.06 | Depression | 1.36 | 0.086 | 0.96 | 1.93 |
| Suicide | 1.35 | 0.119 | 0.93 | 1.96 | Suicide | 0.70 | 0.239 | 0.39 | 1.27 |
| Smoked, last 30 days | 2.11 | 0.081 | 0.91 | 4.90 | Smoked, last 30 Days | 2.52 | 0.002 | 1.39 | 4.56 |
| Drank alcohol, last 30 days | 3.11 | 0.022 | 1.18 | 8.20 | Drank alcohol, last 30 days | 0.69 | 0.369 | 0.31 | 1.54 |
| Binge drinking, last 30 days | 0.58 | 0.259 | 0.23 | 1.49 | Binge drinking, last 30days | 1.23 | 0.584 | 0.59 | 2.54 |
| Smoked marijuana last 30 days | 3.14 | 0.012 | 1.29 | 7.64 | Smoked marijuana last 30 days | 2.44 | 0.007 | 1.28 | 4.66 |
| Gender: 0=female, 1=male | 1.63 | 0.231 | 0.73 | 3.64 | Gender: 0=female, 1=male | 1.13 | 0.663 | 0.64 | 2.00 |
| Female *antisocial behavior | 7.43 | 0.001 | 2.22 | 14.81 | Female * antisocial behavior | 5.70 | 0.017 | 1.36 | 13.84 |
|
| |||||||||
| Male *antisocial behavior | 2.60 | 0.024 | 1.13 | 5.98 | Male * antisocial behavior | 1.38 | 0.387 | 0.66 | 2.87 |
| Female * risky sex | 1.89 | 0.061 | 0.97 | 3.68 | Female * risky sex | 3.43 | 0.000 | 1.90 | 6.18 |
| Male * risky sex | 1.13 | 0.733 | 0.56 | 2.29 | Male * risky sex | 2.32 | 0.000 | 1.45 | 3.70 |
| Female * depression | 1.35 | 0.355 | 0.72 | 2.53 | Female * depression | 0.97 | 0.901 | 0.60 | 1.56 |
| Male * depression | 1.44 | 0.285 | 0.74 | 2.83 | Male * depression | 2.20 | 0.003 | 1.31 | 3.72 |
| Female * suicide | 1.01 | 0.974 | 0.60 | 1.70 | Female * suicide | 0.83 | 0.641 | 0.39 | 1.79 |
| Male * suicide | 1.86 | 0.027 | 1.07 | 3.23 | Male * suicide | 0.67 | 0.344 | 0.29 | 1.54 |
| Female * tobacco | 2.09 | 0.218 | 0.65 | 6.73 | Female * tobacco | 2.55 | 0.034 | 1.07 | 6.08 |
| Male * tobacco | 2.32 | 0.200 | 0.64 | 8.44 | Male * tobacco | 2.68 | 0.022 | 1.15 | 6.26 |
| Female * alcohol | 1.86 | 0.344 | 0.51 | 6.78 | Female * alcohol | 0.79 | 0.634 | 0.29 | 2.11 |
| Male * alcohol | 7.92 | 0.010 | 1.65 | 17.95 | Male * alcohol | 0.51 | 0.341 | 0.13 | 2.02 |
| Female * binge drinking | 0.70 | 0.571 | 0.20 | 2.43 | Female * binge drinking | 0.78 | 0.609 | 0.30 | 2.04 |
| Male * binge drinking | 0.42 | 0.238 | 0.10 | 1.76 | Male * binge drinking | 2.27 | 0.180 | 0.69 | 7.52 |
| Female * marijuana | 3.39 | 0.073 | 0.89 | 12.84 | Female * marijuana | 1.27 | 0.619 | 0.49 | 3.27 |
| Male * marijuana | 2.75 | 0.120 | 0.77 | 9.85 | Male * marijuana | 4.86 | 0.001 | 1.84 | 12.84 |
Model #1 focusing on individual-level problem behaviors and characteristics provided a better fit for the 8th-grade data as opposed to the 11th-grade data. In terms of the main effects, antisocial behavior was an important covariate for methamphetamine use in both grades (though marginally significant in the 11th grade at p = .074). Use of alcohol and use of marijuana were also critical correlates in the 8th grade, with marijuana significant for 11th graders as well. Variables that were significant for 11th graders, but not for eighth graders, included risky sex and use of tobacco, two behaviors considerably more prevalent among older students. Alcohol use, which had been an important correlate for eighth graders, was not a significant covariate for 11th graders.
Also shown in Table 5 are effects for each gender, based on analysis of the interaction between gender and each variable in predicting methamphetamine use. Interaction effects for the most part exhibited similar patterns as the main effects for eighth graders, with both females and males more likely to use methamphetamine if they also engaged in antisocial behavior (though this relationship was much stronger for females). Alcohol use was a significant covariate for methamphetamine use for males, but not for females. Suicide attempts showed a significant correlation to meth use for males, but not for females.
Interaction effects for 11th graders differed somewhat from the pattern for eighth graders, with both genders more likely to use methamphetamine if they engaged in risky sexual behaviors or used tobacco. Although antisocial behavior had been a major correlate of methamphetamine use for 8th-grade females and males, it remained a key covariate only for females in the 11th grade. In addition, although suicide attempts and alcohol were important covariates for 8th-grade males, depression and marijuana use were significant for 11th-grade males.
3.5. Model 2: Relationship of social risk factors to methamphetamine use
Table 6 presents results for relationships between methamphetamine use and peer and parent variables. Here too, we present results separately for each grade with gender as a factor in the analyses.
Table 6.
Logistic Regression Analysis (Y = Methamphetamine), Model #2
| Eighth Grade | Eleventh Grade | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Model Fit |
Model Fit |
||||||||
| Cases | 1,462 | Cases | 1,051 | ||||||
| AIC | 209.890 | AIC | 338.392 | ||||||
| Chi-square | 214.123 | Chi-square | 81.565 | ||||||
| Significance | 0.000 | Significance | 0.000 | ||||||
| Pseudo R2 | 0.136 | Pseudo R2 | 0.075 | ||||||
|
| |||||||||
| Independent variables | Odds Ratio: Exp(B) | Statistical Significance |
C.I. |
Independent variables | Odds Ratio: Exp(B) | Statistical Significance |
C.I. |
||
| Lower | Upper | Lower | Upper | ||||||
|
| |||||||||
| Interaction with antisocial peers | 1.91 | 0.004 | 1.23 | 2.96 | Interaction with antisocial peers | 1.65 | 0.048 | 1.00 | 2.70 |
| Peers use of drugs | 2.47 | 0.000 | 1.74 | 3.51 | Peers use of drugs | 2.15 | 0.000 | 1.48 | 3.13 |
| Parents favor antisocial behavior | 1.39 | 0.237 | 0.80 | 2.41 | Parents favor antisocial behavior | 0.79 | 0.548 | 0.37 | 1.69 |
| Parents favor drug use | 1.92 | 0.005 | 1.22 | 3.02 | Parents favor drug use | 1.40 | 0.155 | 0.88 | 2.24 |
| High family conflict | 1.12 | 0.608 | 0.73 | 1.71 | High family conflict | 0.84 | 0.429 | 0.55 | 1.29 |
| Rule setting | 1.06 | 0.778 | 0.70 | 1.60 | Rule setting | 1.51 | 0.070 | 0.97 | 2.35 |
| Rule enforcement | 1.18 | 0.606 | 0.63 | 2.20 | Rule enforcement | 0.60 | 0.133 | 0.31 | 1.17 |
| Parental monitoring | 1.20 | 0.499 | 0.71 | 2.05 | Parental monitoring | 1.75 | 0.054 | 0.99 | 3.10 |
| Gender (0=female, 1 = male) | 1.38 | 0.365 | 0.69 | 2.78 | Gender (0=female, 1 = male) | 2.08 | 0.029 | 1.08 | 4.03 |
| ♀* interact w/antisocial peers | 2.77 | 0.005 | 1.36 | 5.65 | ♀* interact w/antisocial peers | 1.74 | 0.106 | 0.89 | 3.39 |
| ♂* interact w/antisocial peers | 1.63 | 0.126 | 0.87 | 3.03 | ♂* interact with antisocial peers | 1.53 | 0.261 | 0.73 | 3.20 |
| ♀*peers use of drugs | 2.43 | 0.000 | 1.52 | 3.90 | ♀* peers use of drugs | 1.71 | 0.026 | 1.07 | 2.75 |
| ♂* peers use of drugs | 2.45 | 0.001 | 1.42 | 4.24 | ♂* peers use of drugs | 3.17 | 0.000 | 1.71 | 5.86 |
| ♀*parents favor antisocial beh. | 2.18 | 0.056 | 0.98 | 4.84 | ♀* parents favor antisocial beh. | 1.52 | 0.401 | 0.57 | 4.06 |
| ♂*parents favor antisocial beh. | 0.96 | 0.928 | 0.44 | 2.11 | ♂*parents favor antisocial beh. | 0.35 | 0.090 | 0.10 | 1.18 |
| ♀* parents favor drug use | 1.63 | 0.120 | 0.88 | 3.01 | ♀* parents favor drug use | 1.23 | 0.514 | 0.66 | 2.30 |
| ♂ parents favor drug use | 3.29 | 0.002 | 1.57 | 6.89 | ♂ parents favor drug use | 1.61 | 0.218 | 0.76 | 3.42 |
| Female * parents favor drug use | 0.84 | 0.574 | 0.45 | 1.55 | Female * parents favor drug use | 0.92 | 0.764 | 0.53 | 1.60 |
| Male * parents favor drug use | 1.38 | 0.310 | 0.74 | 2.55 | Male * parents favor drug use | 0.83 | 0.593 | 0.41 | 1.66 |
| Female * rule setting | 0.97 | 0.909 | 0.53 | 1.75 | Female * rule setting | 1.75 | 0.071 | 0.95 | 3.21 |
| Male * rule setting | 1.40 | 0.296 | 0.75 | 2.61 | Male * rule setting | 1.32 | 0.423 | 0.67 | 2.60 |
| Female * rule enforcement | 2.17 | 0.051 | 1.00 | 4.72 | Female * rule enforcement | 0.62 | 0.261 | 0.27 | 1.42 |
| Male * rule enforcement | 0.48 | 0.131 | 0.19 | 1.25 | Male * rule enforcement | 0.40 | 0.133 | 0.12 | 1.32 |
| Female * parental monitoring | 0.71 | 0.425 | 0.31 | 1.64 | Female * parental monitoring | 1.36 | 0.415 | 0.65 | 2.83 |
| Male * parental monitoring | 1.86 | 0.096 | 0.89 | 3.87 | Male * parental monitoring | 2.66 | 0.043 | 1.03 | 6.86 |
Model #2’s collection of contextual or environmental variables provided a better fit for the data than did Model #1, with Model #2’s fit for 8th graders better than for 11th graders. In terms of the main effects across genders, peers’ antisocial behavior and drug use were significant correlates of methamphetamine use for both grades. Having parents with favorable attitudes toward drug use was important for eighth graders, while parental monitoring was modestly associated with use for 11th graders.
Though gender was not a significant direct factor for eighth graders, there were gender differences in some of the relationships between methamphetamine use and these social influences. Females who had friends who engaged in antisocial behavior were more likely to use meth, but that was not true for males. Males who had parents with favorable attitudes toward drugs had higher rates of methamphetamine use, but this was not true for females. One measure without a significant main effect did have an important gender-based interaction effect for eighth graders: females were more likely to use methamphetamine if their parents did not enforce family rules or if enforcement was inconsistent, but that was not true for males.
For 11th graders, gender had a significant main effect with females nearly twice as likely as males to use methamphetamine. Peers’ use of drugs was a better predictor of methamphetamine use among males (OR = 3.17, p < .001) than among females (OR = 1.71, p = .026). Parental monitoring had a significant relationship to male, but not to female, use of meth.
4. Discussion
We are aware of only a handful of published studies of adolescent methamphetamine use. Regarding the prevalence of methamphetamine use, only one study has reported on the prevalence of adolescent use in a population-based sample. Springer et al. (2007) used nationwide data from the 2003 Youth Risk Behavior Survey, which assesses 9th- through 12th-grade students anonymously (Centers for Disease Control and Prevention, 2004). They reported national rates of lifetime use of methamphetamine of 8.3% for boys and 6.8% for girls (overall, national prevalence in 2003 was 7.6%, a decline from 9.8% in 2001). Using the OHT survey for 2001–2003, our rates for 11th grade were 5.6% for boys and 6.0% for girls.
The finding of higher use among girls is consistent with other research reporting gender differences in methamphetamine use. In a review of publications on methamphetamine over the past 30 years, Dluzen & Liu (2008) found that women tend to begin methamphetamine use at earlier ages, appear more dependent on it, but also respond better to treatment than do men. Methamphetamine use appears to be associated with depression in women, and women seem more committed to the drug, whereas men are more likely to use other drugs in the absence of access to methamphetamine. There is also evidence that methamphetamine use on the part of females is due in part to the desire to lose weight. In a study focusing on gender differences in drug use history among a broad cross-section (N = 350) of former clients from a large publicly funded treatment system, Brecht et al. (2004) found that five times the percentage of females than males attributed initial methamphetamine use to a desire to lose weight (36% vs. 7%).
Lack of significant diversity in Oregon (and therefore our sample) prevents any broad generalizations regarding racial/ethnic variation in the prevalence of methamphetamine use.
There are distinct limitations to what one can infer from concurrent relationships. However, the analyses show that, as expected, methamphetamine use relates to other problem behaviors. Perhaps the strongest evidence comes from the fact that not a single adolescent reported methamphetamine use and no other problem. The amount of use rises significantly as the number of adolescents’ other problem behaviors increase.
The specific problems related to methamphetamine use differed according to grade and were moderated by gender. Consistent correlates of methamphetamine use included antisocial behavior and substance use (both self-reported behavior and use and peer-reported behavior and use), although there were distinct gender differences. Though antisocial behavior was important for each gender, females in both grades were much more likely than males to use methamphetamine if they also engaged in these types of activities. Having friends who engaged in deviant behaviors was a significant influence, but was not as important as engaging in these behaviors themselves. Females in the 8th grade were more likely to use methamphetamine if they also reported using marijuana. For males, antisocial behavior of their own (or on the part of friends) was an important correlate of methamphetamine use in both grades. However, it was their substance use (or that of their friends) that had a more important influence, with self-reported alcohol use especially playing a role for 8th-grade males and self-reported marijuana use for 11th-grade males. (Peers’ use of drugs was a significant covariate for males in both grades.)
Risky sex was associated with methamphetamine use for females in the 8th grade and for both females and males in the 11th grade. Springer et al. (2007) also found a relationship between risky sexual behavior and methamphetamine use. Depression was a correlate of use for 11th-grade males, but not for other subgroups. Sussman, Dent, and Stacy (1999) found a strong relationship between methamphetamine use and alcohol use, depression, and having friends who use drugs, which is consistent with our findings regarding the importance of alcohol for 8th-grade males and depression for 11th-grade males. Herman-Stahl et al. (2006) also found that alcohol use, especially binge drinking, was an important correlate. This was contrary to our findings where alcohol was a significant correlate for 8th graders in general and 8th-grade males in particular, but not for 11th graders of either gender. Binge drinking seemed to play no important role for either grade or either gender.
The results are generally consistent with the oft-reported finding that adolescent problem behaviors are inter-related (Biglan et al., 2004; Boles, Biglan, & Smolkowski, 2006). They suggest that we may prevent some methamphetamine use if we prevent antisocial behavior, depression, and risky sexual behavior. However, more specifically, the diversity of correlates across subgroups points to the value of preventing the entire range of problems experienced by youth. That, in turn, requires that we focus on how we can change adolescents’ environments.
In terms of environmental correlates, it was not surprising to find that adolescents are more likely to use methamphetamine if their peers engage in antisocial behavior or use drugs. As mentioned above, 8th-grade females in particular were more likely to use methamphetamine if they had antisocial or drug-using peers. Based on other studies (Biglan, 1996; Hankins & Biglan, under review), we suspect these early adolescent females are involved with older antisocial males. Preventing such associations may be particularly valuable for preventing other problems.
Parental influences did not have especially strong relationships to self-reported methamphetamine use. There was a significant overall relationship between parents’ favorable attitudes toward drug use and methamphetamine use for eighth graders, especially for males. We could relate poor family rule setting and parental monitoring to methamphetamine use among 11th graders, with poor rule setting a correlate for females and inadequate parental monitoring a correlate for males. These findings may indicate that parents cannot have much influence on methamphetamine use. However, the evidence that parental monitoring and limit setting affect multiple problems of adolescents is so overwhelming (e.g., Biglan et al., 2004; Dishion et al., 2002) that this conclusion is hardly credible. Since we can correlate the use of methamphetamine with many problems that parental monitoring and setting limits do prevent, it seems premature to conclude that these parental practices will not reduce methamphetamine use.
In conclusion, this study shows that adolescent methamphetamine use is related to other problem behaviors, but that the specific problems to which it is related vary by grade and are moderated by gender. The results suggest that efforts to prevent antisocial behavior, risky sex, and depression may be of particular value. However, more generally, since methamphetamine use co-occurs with a host of other problems and in the context of peer drug use, any efforts to prevent youth problems will probably be productive. We cannot account for the relatively moderate relationships between parenting practices and methamphetamine use, but given the benefits of parenting interventions for other problems (related to methamphetamine use), we should still encourage efforts to promote better monitoring and limit setting.
Fig 1.
Acknowledgments
The National Cancer Institute (CA38273 and CA 086169) and the National Institute on Drug Abuse (DA018760) provided financial support for the completion of the work on this manuscript. The authors wish to thank Yvonne Kuo for her help with data analysis, Christine Cody for editorial and reference assistance, and Sylvia Gillings for additional help preparing this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dennis Embry, Paxis Institute.
Martin Hankins, Oregon Research Institute.
Anthony Biglan, Oregon Research Institute.
Shawn Boles, Oregon Research Institute.
Reference List
- Allcott JV, Barnhart RA, Mooney LA. Acute lead poisoning in two users of illicit methamphetamine. Journal of the American Medical Association. 1987;285:510–511. doi: 10.1001/jama.1987.03400040108032. [DOI] [PubMed] [Google Scholar]
- Anglin MD, Burke C, Perrochet B, Stamper E, Dawud-Noursi S. History of the methamphetamine problem. Journal of Psychoactive Drugs. 2000;32:137–141. doi: 10.1080/02791072.2000.10400221. [DOI] [PubMed] [Google Scholar]
- Anonymous. Illegal meth labs: Cleanup raises health and environmental concerns. Journal of Environmental Health. 2003;65:50. [PubMed] [Google Scholar]
- Anonymous. Increased HIV loads in active methamphetamine users explained by reduced effectiveness of antiretroviral therapy. AIDS Reader. 2004;4:70. [PubMed] [Google Scholar]
- Arthur MW, Hawkins JD, Pollard JA, Catalano RF, Baglioni AJ., Jr Measuring risk and protective factors for substance use, delinquency, and other adolescent problem behaviors: The Communities that Care youth survey. Evaluation Review. 2002;26:355–381. doi: 10.1177/0193841X0202600601. [DOI] [PubMed] [Google Scholar]
- Bailey DN, Shaw RF. Cocaine- and methamphetamine-related deaths in San Diego County, 1987: Homicides and accidental overdoses. Journal of Forensic Sciences. 1989;34:407–422. [PubMed] [Google Scholar]
- Banken JA. Drug abuse trends among youth in the United States. Annals of the New York Academy of Sciences. 2004;1025:465–471. doi: 10.1196/annals.1316.057. [DOI] [PubMed] [Google Scholar]
- Biglan A. Sexual coercion. In: Mattaini MA, Thyer BA, editors. Finding solutions to social problems: Behavioral strategies for change. Washington, DC: American Psychological Association; 1996. pp. 289–316. [Google Scholar]
- Biglan A, Ary DV, Smolkowski K, Duncan TE, Black C. A randomized control trial of a community intervention to prevent adolescent tobacco use. Tobacco Control. 2000;9:24–32. doi: 10.1136/tc.9.1.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biglan A, Brennan PA, Foster SL, Holder HD, Miller TL, Cunningham PB, et al. Helping adolescents at risk: Prevention of multiple problem behaviors. New York: Guilford; 2004. [Google Scholar]
- Biglan A, Duncan TE, Ary DV, Smolkowski K. Peer and parental influences on adolescent tobacco use. Journal of Behavioral Medicine. 1995;18:315–330. doi: 10.1007/BF01857657. [DOI] [PubMed] [Google Scholar]
- Boddiger D. Methamphetamine use linked to rising HIV transmission. Lancet. 2005;365:1217–1218. doi: 10.1016/S0140-6736(05)74794-2. [DOI] [PubMed] [Google Scholar]
- Boles S, Biglan A, Smolkowski K. Relationships among negative and positive behaviours in adolescence. Journal of Adolescence. 2006;29:33–52. doi: 10.1016/j.adolescence.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Booth BM, Leukefeld C, Falck R, Wang J, Carlson R. Correlates of rural methamphetamine and cocaine users: Results from a multistate community study. Journal of Studies on Alcohol. 2006;67:493–501. doi: 10.15288/jsa.2006.67.493. [DOI] [PubMed] [Google Scholar]
- Brecht ML, O’Brien A, Mayrhauser CV, Anglin MD. Methamphetamine use behaviors and gender differences. Addictive Behaviors. 2004;29:89–106. doi: 10.1016/s0306-4603(03)00082-0. [DOI] [PubMed] [Google Scholar]
- Buchi KF, Zone S, Langheinrich K, Varner MW. Changing prevalence of prenatal substance abuse in Utah. Obstetrics and Gynecology. 2003;102:27–30. doi: 10.1016/s0029-7844(03)00367-3. [DOI] [PubMed] [Google Scholar]
- Butterfield P, Malliarakis K, Dotson JAW. Billings’ methamphetamine epidemic: Nursing leaders frame a public health and environmental health problem. Nursing Leadership Forum. 2002;70:8–11. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Public health consequences among first responders to emergency events associated with illicit methamphetamine laboratories -- selected states, 1996–1999. Morbidity and Mortality Weekly Report. 2000;49:1021–1024. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth Risk Behavior Survey, 2003. Atlanta, GA: U.S. Department of Health and Human Services; 2004. [Google Scholar]
- Centers for Disease Control and Prevention. Methamphetamine use and HIV risk behaviors among heterosexual men--preliminary results from five northern California counties, December 2001–November 2003. Morbidity and Mortality Weekly Report. 2006;55:273–277. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth Risk Behavior Survey (1991–2007) Atlanta, GA: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- Chan P, Chen JH, Lee MH, Deng JF. Fatal and nonfatal methamphetamine intoxication in the intensive care unit. Journal of Toxicology-Clinical Toxicology. 1994;32:147–155. doi: 10.3109/15563659409000444. [DOI] [PubMed] [Google Scholar]
- Cohen JB, Dickow A, Horner K, Zweben JE, Balabis J, Vandersloot D, et al. Abuse and violence history of men and women in treatment for methamphetamine dependence. The American Journal on Addictions. 2003;12:377–385. [PubMed] [Google Scholar]
- Colnar R, Rawson R, Marinelli-Casey P, Gallagher C, Herrell J. Methamphetamine affects individuals and communities: Regional variations in methamphetamine route of administration in the SCAT methamphetamine treatment project, significance for public health considerations. Nebraska Nurse. 1999;32:31. [PubMed] [Google Scholar]
- Cox DR, Snell EJ. Analysis of binary data. 2. London: Chapman & Hall; 1989. [Google Scholar]
- Crockett LJ, Schulenberg JE, Petersen AC. Congruence between objective and self-report data in a sample of young adolescents. Journal of Adolescent Research. 1987;2:383–392. [Google Scholar]
- Davis LE, Kalousek G, Rubenstein E. Hepatitis associated with illicit use of intravenous methamphetamine. Public Health Reports. 1970;85:809–813. [PMC free article] [PubMed] [Google Scholar]
- DeMaris A. Logit modeling: Practical applications. Thousand Oaks, CA: Sage; 1992. [Google Scholar]
- Dishion TJ. The family ecology of boys’ peer relations in middle childhood. Child Development. 1990;61:874–892. doi: 10.1111/j.1467-8624.1990.tb02829.x. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Andrews DW. Preventing escalation in problem behaviors with high-risk young adolescents: Immediate and 1-year outcomes. Journal of Consulting and Clinical Psychology. 1995;63:538–548. doi: 10.1037//0022-006x.63.4.538. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Kavanagh K, Schneiger A, Nelson S, Kaufman NK. Preventing early adolescent substance use: a family-centered strategy for the public middle school. In R.L. Spoth, K. Kavanagh, & T.J. Dishion (Guest Eds.). Universal family-centered prevention strategies: Current findings and critical issues for public health impact . Prevention Science. 2002;3:191–201. doi: 10.1023/a:1019994500301. [Special Issue] [DOI] [PubMed] [Google Scholar]
- Dishion TJ, McMahon RJ. Parental monitoring and the prevention of child and adolescent problem behavior: a conceptual and empirical foundation. Clinical Child and Family Psychology Review. 1997;1:61–75. doi: 10.1023/a:1021800432380. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Patterson GR, Kavanagh KA. An experimental test of the coercion model: Linking theory, measurement, and intervention. In: McCord J, Tremblay RE, editors. Preventing antisocial behavior: Interventions from birth through adolescence. New York: Guilford Press; 1992. pp. 253–282. [Google Scholar]
- Dishion TJ, Patterson GR, Stoolmiller M, Skinner ML. Family, school, and behavioral antecedents to early adolescent involvement with antisocial peers. Developmental Psychology. 1991;27:172–180. [Google Scholar]
- Dluzen DE, Liu B. Gender differences in methamphetamine use and responses: A review. Gender Medicine. 2008;5:24–35. doi: 10.1016/s1550-8579(08)80005-8. [DOI] [PubMed] [Google Scholar]
- Elliott SN, Busse RT, Gresham FM. Behavior rating scales: Issues of use and development. School Psychology Review. 1993;22:313–321. [Google Scholar]
- Embry DD, Lopez D, Minugh PA. Stop the methamphetamine epidemic. Arizona Medical Association Journal. 2005;16:30–34. [Google Scholar]
- Forrester K, Biglan A, Severson HH, Smolkowski K. Predictors of smoking onset over two years. Nicotine & Tobacco Research. 2007;9:1259–1267. doi: 10.1080/14622200701705357. [DOI] [PubMed] [Google Scholar]
- Freese TE, Obert J, Dickow A, Cohen J, Lord RH. Methamphetamine abuse: Issues for special populations. Journal of Psychoactive Drugs. 2000;32:177–182. doi: 10.1080/02791072.2000.10400226. [DOI] [PubMed] [Google Scholar]
- Glittenberg J, Anderson C. Methamphetamines: Use and trafficking in the Tucson-Nogales area. Substance Use & Misuse. 1999;34:1977–1989. doi: 10.3109/10826089909039435. [DOI] [PubMed] [Google Scholar]
- Gorman EM. Research with gay drugs users and the interface with HIV: Current methodological issues for social work research. Journal of Gay & Lesbian Social Services: Issues in Practice, Policy & Research. 2003;15:79–94. [Google Scholar]
- Greenwell L, Brecht ML. Self-reported health status among treated methamphetamine users. American Journal of Drug and Alcohol Abuse. 2003;29:75–104. doi: 10.1081/ada-120018840. [DOI] [PubMed] [Google Scholar]
- Grella CE, Hser YI, Huang YC. Mothers in substance abuse treatment: Differences in characteristics based on involvement with child welfare services. Child Abuse & Neglect. 2006;30:55–73. doi: 10.1016/j.chiabu.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Haight W, Jacobsen T, Black J, Kingery L, Sheridan K, Mulder C. ‘In these bleak days’: Parent methamphetamine abuse and child welfare in the rural Midwest. Children and Youth Services Review. 2005;27:949–971. [Google Scholar]
- Halkitis PN, Parsons JT, Stirratt MJ. A double epidemic: Crystal methamphetamine drug use in relation to HIV transmission among gay men. Journal of Homosexuality. 2001;41:17–35. doi: 10.1300/J082v41n02_02. [DOI] [PubMed] [Google Scholar]
- Hankins M, Biglan A. Behavioral and social correlates of high-risk sexual behavior in a population-based sample of early and later adolescents. 2008 doi: 10.1016/j.addbeh.2008.11.019. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkess J, Gildon B, Istre GR. Outbreaks of hepatitis A among illicit drug users, Oklahoma, 1984–98 [comment] American Journal of Public Health. 1989;79:463–466. doi: 10.2105/ajph.79.4.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Morrison DM, O’Donnell J, Abbott RD, Day LE. The Seattle Social Development Project: Effects of the first four years on protective factors and problem behaviors. In: McCord J, Tremblay RE, editors. Preventing antisocial behavior: Interventions from birth through adolescence. New York, NY: Guilford; 1992. pp. 139–161. [Google Scholar]
- Hawkins JD, Van Horn ML, Arthur MW. Community variation in risk and protective factors and substance use outcomes. Prevention Science. 2004;5:213–220. doi: 10.1023/b:prev.0000045355.53137.45. [DOI] [PubMed] [Google Scholar]
- Herman-Stahl MA, Krebs CP, Kroutil LA, Heller DC. Risk and protective factors for nonmedical use of prescription stimulants and methamphetamine among adolescents. Journal of Adolescent Health. 2006;39:374–380. doi: 10.1016/j.jadohealth.2006.01.006. [DOI] [PubMed] [Google Scholar]
- Hong R, Matsuyama E, Nur K. Cardiomyopathy associated with the smoking of crystal methamphetamine. Journal of the American Medical Association. 1991;265:1152–1154. [PubMed] [Google Scholar]
- Hosmer D, Lemeshow S. Applied logistic regression. New York: Wiley & Sons; 1989. [Google Scholar]
- Hutin YJ, Sabin KM, Hutwagner LC, Schaben L, Shipp GM, Lord DM, et al. Multiple modes of hepatitis A virus transmission among methamphetamine users. American Journal of Epidemiology. 2000;152:186–192. doi: 10.1093/aje/152.2.186. [DOI] [PubMed] [Google Scholar]
- Interuniversity Consortium for Political and Social Research. The Monitoring the Future Study (1989–2006) Ann Arbor, MI: University of Michigan; 2007. [Google Scholar]
- Jaccard J. Interaction effects in logistic regression. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- Jernigan TL, Gamst AC, Archibald SL, Fennema-Notestine C, Mindt MR, Marcotte TD, et al. Effects of methamphetamine dependence and HIV infection on cerebral morphology. American Journal of Psychiatry. 2005;162:1461–1472. doi: 10.1176/appi.ajp.162.8.1461. [DOI] [PubMed] [Google Scholar]
- Kann L, Kinchen SA, Williams BI, Ross JG, Lowry R, Grunbaum JA, et al. Youth Risk Behavior Surveillance - United States, 1999. Morbidity and Mortality Weekly Report. 2000;49:1–94. [PubMed] [Google Scholar]
- Koester S, Glanz J, Barón A. Drug sharing among heroin networks: Implications for HIV and Hepatitis B and C prevention. AIDS and Behavior. 2005;9:27–39. doi: 10.1007/s10461-005-1679-y. [DOI] [PubMed] [Google Scholar]
- Kraus L, Augustin R, Frischer M, Kummler P, Uhl A, Wiessing L. Estimating prevalence of problem drug use at national level in countries of the European Union and Norway. Addiction. 2003;98:471–485. doi: 10.1046/j.1360-0443.2003.00326.x. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR, McGrath PJ, Bush SC. Mania occurring during treatment for depersonalization: A report of two cases. Journal of Clinical Psychiatry. 1980;41:33–34. [PubMed] [Google Scholar]
- Lineberry TW, Bostwick JM. Methamphetamine abuse: A perfect storm of complications. Mayo Clinic Proceedings. 2006;81:77–84. doi: 10.4065/81.1.77. [DOI] [PubMed] [Google Scholar]
- Luchansky B. Treatment for methamphetamine dependency is as effective as treatment for any other drug. Olympia, WA: Looking Glass Analytics; 2003. [Google Scholar]
- McCarthy S, Waters TF. Treating substance abuse offenders in the Southwestern United States: A report evaluating the long-term effectiveness of the Yuma County Adult Drug Court. Journal of Offender Rehabilitation. 2003;37:163–177. [Google Scholar]
- McDaniel R, Embry DD. Reclaiming Wyoming: A comprehensive Blueprint for prevention, early intervention, and treatment of substance abuse. Cheyenne, WY: Wyoming Department of Health; 2001. [Google Scholar]
- McKelvey R, Zavoina W. A statistical model for the analysis of ordinal level dependent variables. Journal of Mathematical Psychology. 1994;4:103–120. [Google Scholar]
- Menard S. Applied logistic regression analysis. 2. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Meredith CW, Jaffe C, Ang-Lee K, Saxon AJ. Implications of chronic methamphetamine use: A literature review. Harvard Review of Psychiatry. 2005;13:141–154. doi: 10.1080/10673220591003605. [DOI] [PubMed] [Google Scholar]
- Metzler CW, Biglan A, Ary DV, Li F. The stability and validity of early adolescents’ reports of parenting constructs. Journal of Family Psychology. 1998;12:600–619. [Google Scholar]
- Meyer JM. Prevalence of hepatitis A, hepatitis B, and HIV among hepatitis C-seropositive state hospital patients: Results from Oregon State Hospital. Journal of Clinical Psychiatry. 2003;64:540–545. doi: 10.4088/jcp.v64n0507. [DOI] [PubMed] [Google Scholar]
- Molitor F, Truax SR, Ruiz JD, Sun RK. Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. Western Journal of Medicine. 1998;168:93–97. [PMC free article] [PubMed] [Google Scholar]
- Morgan P, Joe KA. Citizens and outlaws: The private lives and public lifestyles of women in the illicit drug economy. Journal of Drug Issues. 1996;26:125–142. [Google Scholar]
- National Drug Intelligence Center. National drug threat assessment 2008. Washington, DC: US Department of Justice National Drug Intelligence Center; 2007. [Google Scholar]
- Office of National Drug Control Policy (ONDCP) Synthetic drug control strategy: a focus on methamphetamine and prescription drug abuse (Annual ONDCP Report) Washington, DC: Office of National Drug Control Policy (ONDCP); 2006. [Google Scholar]
- Otero C, Boles S, Young N, Dennis K. Methamphetamine addiction, treatment, and outcomes: Implications for child welfare workers. Washington, DC: Substance Abuse and Mental Health Services Administration (SAMSHA), Center for Substance Abuse Treatment; 2006. [Google Scholar]
- Pampel FC. Logistic regression: A primer. Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- Paschane DM, Fisher DG, Cagle HH, Fenaughty AM. Gonorrhea among drug users: An Alaskan versus a national sample. American Journal of Drug and Alcohol Abuse. 1998;24:285–297. doi: 10.3109/00952999809001713. [DOI] [PubMed] [Google Scholar]
- Perez JA, Jr, Arsura EL, Strategos S. Methamphetamine-related stroke: Four cases. Journal of Emergency Medicine. 1999;17:469–471. doi: 10.1016/s0736-4679(99)00009-8. [DOI] [PubMed] [Google Scholar]
- Plessinger MA. Prenatal exposure to amphetamines. Risks and adverse outcomes in pregnancy. Obstetrics and Gynecology Clinics of North America. 1998;25:119–138. doi: 10.1016/s0889-8545(05)70361-2. [DOI] [PubMed] [Google Scholar]
- Rawson RA, Anglin MD, Ling W. Will the methamphetamine problem go away? Journal of Addictive Diseases. 2002;21:5–19. doi: 10.1300/j069v21n01_02. [DOI] [PubMed] [Google Scholar]
- Rawson R, Huber A, Brethen P, Obert J, Gulati V, Shoptaw S, et al. Methamphetamine and cocaine users: Differences in characteristics and treatment retention. Journal of Psychoactive Drugs. 2000;32:233–238. doi: 10.1080/02791072.2000.10400234. [DOI] [PubMed] [Google Scholar]
- Richards JR, Johnson EB, Stark RW, Derlet RW. Methamphetamine abuse and rhabdomyolysis in the ED: A 5-year study. American Journal of Emergency Medicine. 1999;17:681–685. doi: 10.1016/s0735-6757(99)90159-6. [DOI] [PubMed] [Google Scholar]
- Roberts AR, Yeager K, Siegel A. Obsessive-compulsive disorder, comorbid depression, substance abuse, and suicide attempts: Clinical presentations, assessments, and treatment. Brief Treatment and Crisis Intervention. 2003;3:145–167. [Google Scholar]
- Rockett IRH, Putnam SL, Jia H, Smith GS. Declared and undeclared substance use among emergency department patients: A population-based study. Addiction. 2006;101:706–712. doi: 10.1111/j.1360-0443.2006.01397.x. [DOI] [PubMed] [Google Scholar]
- Sanello F. Tweakers: How crystal meth is ravaging gay America. Los Angeles, CA: Alyson; 2005. [Google Scholar]
- Sattah MV, Supawitkul S, Dondero TJ, Kilmarx PH, Young NL, Mastro TD, et al. Prevalence of and risk factors for methamphetamine use in northern Thai youth: Results of an audio-computer-assisted self-interviewing survey with urine testing. Addiction. 2002;97:801–808. doi: 10.1046/j.1360-0443.2002.00131.x. [DOI] [PubMed] [Google Scholar]
- Schermer CR, Wisner DH. Methamphetamine use in trauma patients: A population-based study. Journal of the American College of Surgeons. 1999;189:442–449. doi: 10.1016/s1072-7515(99)00188-x. [DOI] [PubMed] [Google Scholar]
- Seeley JR, Rohde P, Lewinsohn PM, Clarke GN. Depression in youth: Epidemiology, identification, and intervention. In: Shinn M, Walker H, editors. Interventions for academic and behavior problems II: Preventive and remedial approaches. Silver Spring, MD: National Association of School Psychologists; 2002. [Google Scholar]
- Sexton RL, Carlson RG, Siegal HA, Falck RS, Leukefeld C, Booth B. Barriers and pathways to diffusion of methamphetamine use among African Americans in the rural South: Preliminary ethnographic findings. Journal of Ethnicity in Substance Abuse. 2005;4:77–103. doi: 10.1300/J233v04n01_06. [DOI] [PubMed] [Google Scholar]
- Shoptaw S, Peck J, Reback CJ, Rotheram-Fuller E. Psychiatric and substance dependence comorbidities, sexually transmitted diseases, and risk behaviors among methamphetamine-dependent gay and bisexual men seeking outpatient drug abuse treatment. Journal of Psychoactive Drugs. 2003;35:161–168. doi: 10.1080/02791072.2003.10400511. [DOI] [PubMed] [Google Scholar]
- Silva OA, Greve JMD, Yonamine MC, Leyton V. Drug use by truck drivers in Brazil. Drugs: Education, Prevention & Policy. 2003;10:135–139. [Google Scholar]
- Slade M, Daniel LJ, Heisler CJ. Application of forensic toxicology to the problem of domestic violence. Journal of Forensic Sciences. 1991;36:708–713. [PubMed] [Google Scholar]
- Smith L, Yonekura ML, Wallace T, Berman N, Kuo J, Berkowitz C. Effects of prenatal methamphetamine exposure on fetal growth and drug withdrawal symptoms in infants born at term. Journal of Developmental & Behavioral Pediatrics. 2003;24:17–23. doi: 10.1097/00004703-200302000-00006. [DOI] [PubMed] [Google Scholar]
- Smolkowski K, Biglan A, Dent C, Seeley J. The multilevel structure of four adolescent problems. Prevention Science. 2006;7:239–256. doi: 10.1007/s11121-006-0034-5. [DOI] [PubMed] [Google Scholar]
- Springer AE, Peters RJ, Shegog R, White DL, Kelder SH. Methamphetamine use and sexual risk behaviors in U.S. High school students: Findings from a National Risk Behavior Survey. Prevention Science. 2007;8:103–113. doi: 10.1007/s11121-007-0065-6. [DOI] [PubMed] [Google Scholar]
- SPSS. Statistical Package for the Social Services, Windows Version 15.0. Chicago, IL: SPSS Inc; 2006. [Google Scholar]
- Stoops WW, Tindall MS, Mateyoke-Scrivner A, Leukefeld C. Methamphetamine use in nonurban and urban drug court clients. International Journal of Offender Therapy and Comparative Criminology. 2005;49:260–276. doi: 10.1177/0306624X04273438. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2002 National Survey on Drug Use and Health: National findings (DHHS No. SMA 03-3836, NSDUH Series H-22) Rockville, MD: SAMHSA Office of Applied Studies; 2003. Also available online http://www.oas.samhsa.gov. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health (1994–2004) Rockville, MD: SAMHSA, Office of Applied Studies; 2005. [Google Scholar]
- Sussman S, Dent CW, Stacy AW. The association of current stimulant use with demographic substance use, violence-related, social and intrapersonal variables among high-risk youth. Addictive Behaviors. 1999;24:741–748. doi: 10.1016/s0306-4603(98)00134-8. [DOI] [PubMed] [Google Scholar]
- Suwanwela C, Poshyachinda V. Drug abuse in Asia. Bulletin on Narcotics. 1986;38:41–53. [PubMed] [Google Scholar]
- Thadani PV. Biological mechanisms and perinatal exposure to abused drugs. Synapse. 1995;19:228–232. doi: 10.1002/syn.890190310. [DOI] [PubMed] [Google Scholar]
- Tominaga GT, Garcia G, Dzierba A, Wong J. Toll of methamphetamine on the trauma system. Archives of Surgery. 2004;139:844–847. doi: 10.1001/archsurg.139.8.844. [DOI] [PubMed] [Google Scholar]
- Urbina A, Jones K. Crystal methamphetamine, its analogues, and HIV infection: Medical and psychiatric aspects of a new epidemic. Clinical Infectious Diseases. 2004;38:890–894. doi: 10.1086/381975. [DOI] [PubMed] [Google Scholar]
- Vogt TM, Perz JF, Van Houten CKJ, Harrington R, Hansuld T, Bialek SR, et al. An outbreak of hepatitis B virus infection among methamphetamine injectors: The role of sharing injection drug equipment. Addiction. 2006;101:726–730. doi: 10.1111/j.1360-0443.2006.01407.x. [DOI] [PubMed] [Google Scholar]
- Wada K, Greberman SB, Konuma K, Hirai S. HIV and HCV infection among drug users in Japan. Addiction. 1999;94:1063–1069. doi: 10.1046/j.1360-0443.1999.947106311.x. [DOI] [PubMed] [Google Scholar]
- Wijetunga M, Bhan R, Lindsay J, Karch S. Acute coronary syndrome and crystal methamphetamine use: A case series. Hawaii Medical Journal. 2004;63:8–13. [PubMed] [Google Scholar]
- Wilkins C, Pledger M, Bhatta K, Casswell S. Patterns of amphetamine use in New Zealand: Findings from the 2001 National Drug Survey. New Zealand Medical Journal. 2004;117:U796. [PubMed] [Google Scholar]
- Wolkoff DA. Methamphetamine abuse: An overview for health care professionals. Hawaii Medical Journal. 1997;56:34–36. 44. [PubMed] [Google Scholar]
- Won L, Bubula N, McCoy H, Heller A. Methamphetamine concentrations in fetal and maternal brain following prenatal exposure. Neurotoxicology and Teratology. 2001;23:349–354. doi: 10.1016/s0892-0362(01)00151-9. [DOI] [PubMed] [Google Scholar]
- Yen CF, Shieh BL. Suicidal ideation and correlates in Taiwanese adolescent methamphetamine users. Journal of Nervous and Mental Disease. 2005;193:444–449. doi: 10.1097/01.nmd.0000168243.59956.dd. [DOI] [PubMed] [Google Scholar]
- Yu Q, Larson DF, Watson RR. Heart disease, methamphetamine, and AIDS. Life Sciences. 2003;73:129–140. doi: 10.1016/s0024-3205(03)00260-1. [DOI] [PubMed] [Google Scholar]
- Zhu BL, Oritani S, Shimotouge K, Ishida K, Quan L, Fujita MQ, et al. Methamphetamine-related fatalities in forensic autopsy during 5 years in the southern half of Osaka city and surrounding areas. Forensic Science International. 2000;113:443–447. doi: 10.1016/s0379-0738(00)00281-4. [DOI] [PubMed] [Google Scholar]
- Zweben JE, Cohen JB, Christian D, Galloway GP, Salinardi M, Parent D, et al. Psychiatric symptoms in methamphetamine users. The American Journal on Addictions. 2004;13:181–190. doi: 10.1080/10550490490436055. [DOI] [PubMed] [Google Scholar]