Abstract
The overall goal of tissue engineering is to create functional tissue grafts that can regenerate or replace our defective or worn out tissues and organs. Examples of grafts that are now in pre/clinical studies or clinical use include engineered skin, cartilage, bone, blood vessels, skeletal muscle, bladder, trachea, and myocardium. Engineered tissues are also finding applications as platforms for pharmacological and physiological studies in vitro. To fully mobilize the cell’s biological potential, a new generation of tissue engineering systems is now being developed to more closely recapitulate the native developmental milieu, and mimic the physiologic mechanisms of transport and signaling. We discuss the interactions between regenerative biology and engineering, in the context of (i) creation of functional tissue grafts for regenerative medicine (where biological input is critical), and (ii) studies of stem cells, development and disease (where engineered tissues can serve as advanced 3D models).
Keywords: Stem cells, scaffoldl, bioreactor, electrical signals, perfusion
1 “BIOMIMETIC” APPROACH TO TISSUE ENGINEERING
Tissue development and remodeling in living organisms is orchestrated by cascades of regulatory factors interacting at multiple levels, in space and time. Whole animal models certainly provide biologic fidelity (at least within given species), but offer limited control over the local environment, and limited real-time insight. In contrast, traditional cell culture provides significant control over cellular environment along with precise insight into cellular processes, but at the expense of a largely oversimplified 2D experimental context.
In tissue engineering, directing the cells to differentiate at the right time, in the right place, and into the right phenotype, also requires an environment providing the same factors that govern cellular processes in vivo. The field is moving away from “flat biology” of cell monolayers in favor of more realistic yet controllable 3D culture environments. We are now getting closer to a new generation of tissue engineering systems that would authentically represent the cell’s environment in a living organism while enabling tight control over the cell environment and real-time insight into cellular and morphogenic events. Along these lines, a “biomimetic” approach to the formation of engineered tissues (Figure 1) directs the assembly of functional tissues using biologically derived design requirements.
Figure 1. Developmental biology and tissue engineering.
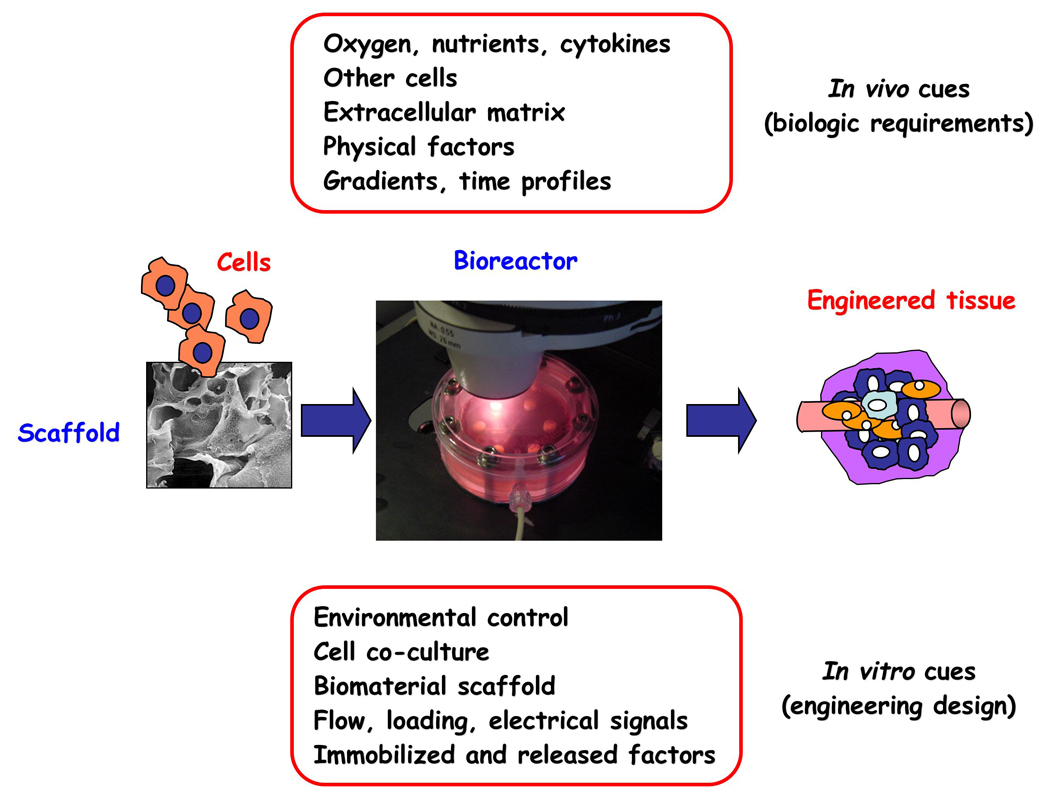
In vivo, the progression of tissue development and remodeling depends on the interaction of time and space gradients of multiple factors that are not entirely known. The “biomimetic” approach to tissue engineering aims to utilize these same factors through the design of biomaterial scaffolds (providing structural, mechanical and logistic templates for cell attachment and tissue formation) and bioreactors (providing environmental control, exchange of nutrients and metabolites, and the molecular and physical regulatory signals). This way, the biological requirements inspire the design of tissue engineering systems, whereas tissue engineering provides controllable models of high fidelity for regenerative biology studies.
2 BIOMATERIAL SCAFFOLDS FOR GUIDING TISSUE ORGANIZATION
Scaffold materials – native or synthetic, permanent or biodegradable – are processed into 3D architectures suitable for cell seeding and cultivation. Material choices are guided by the need to restore cell signaling and to match the mechanical behavior of the tissue being engineered. Scaffolds also serve as “informational templates” to the cells, by implementing patterning, binding of ligands, and sustained release of cytokines [1]. Each tissue poses its own challenges to scaffold design, and we will use cardiac muscle and bone as examples of tissues with distinctly different scaffold requirements (Figure 2).
Figure 2. Biomaterial scaffolds as templates for cell attachment and tissue formation.
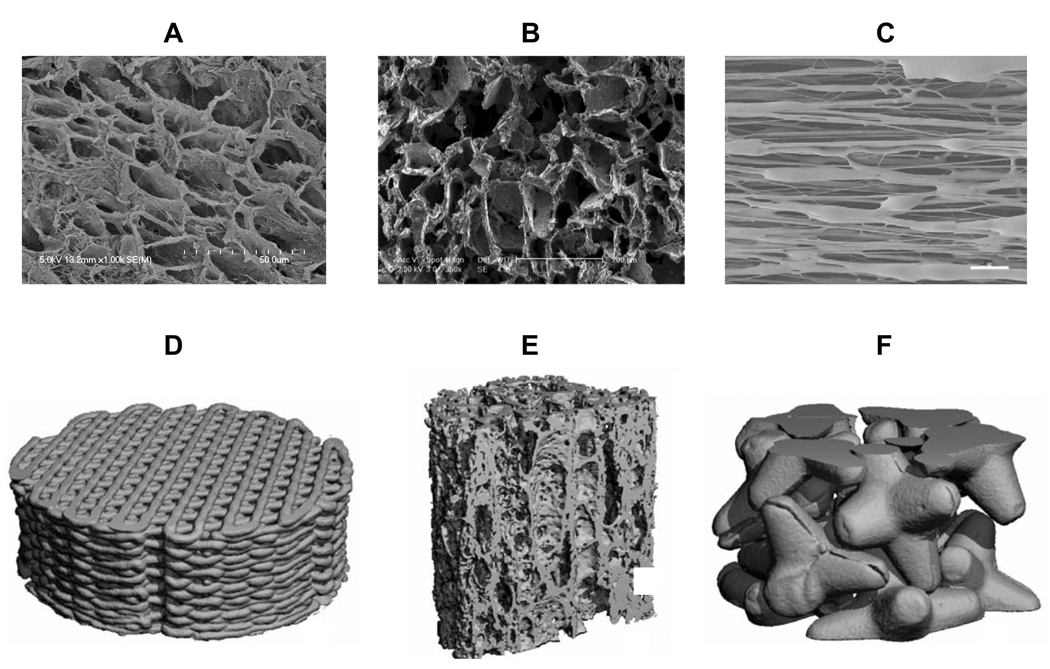
Examples of native and synthetic scaffolds for cardiac tissue engineering (shown as scanning electron micrographs) include A decellularized human cardiac tissue and B synthetic poly(glycerol sebacate) scaffold, with great similarities in structure and pore distribution, and C aligned electrospun, biodegradable polyurethane [4]. Scaffolds for bone tissue engineering (shown as microcomputer tomography images include D composite PCL/TCP scaffold produced using fused deposition modeling, E poly(L-lactide-co-DL-lactide) scaffold with anisotropic pore structure designed to encourage tissue ingrowth, and F jacks-shaped ceramic particles intended to fill bone defects while providing pores for cell and vascular ingrowth [37].
Cardiac muscle, a dense synctium of electromechanically coupled cells that transmit force and deformations in multiple directions, requires soft and elastic scaffolds. Examples include hydrogels that enhanced the expression of Nkx2.5, elastomer scaffolds seeded sequentially with cardiac fibroblasts and myocytes that provided an environment for cell differentiation and coupling [2, 3]. Also, alignment of scaffold fibers lowered the levels of atrial natriuretic peptide (ANP), indicating a shift towards a more mature cell phenotype [4].
Bone, a tissue containing dense mineralized matrix that can withstand significant compressive loads, requires scaffolds that can provide a framework for mechanical stability along with interconnected large pores for cell infiltration. In one study, silk fibroin scaffold was designed to guide differentiation of human mesenchymal stem cells (hMSCs) into trabecular- or cortical-like mineralized networks [5]. In another study, fully decellularized bone provided "biomimetic" topography, composition, and mechanical properties for osteogenic differentiation of hMSCs [6].
Custom-designed scaffolds also find utility in developing tissue models for drug screening and studies of disease. One partcular 3D model of tumor biology was shown to more closely predict cell responses to chemotherapeutic agents than traditional 2D culture [7]. Pioneering work by the Taylor lab [8] has shown that decellularization of intact hearts can produce an ECM-based template which permits perfusion, vascularization, and seeding of myocytes leading to ex vivo pumping function. Cell culture on scaffolds may thus provide new insights into the cellular responses to their environment and the regeneration of tissues, and thereby facilitate application of biological paradigms in tissue engineering.
3 BIOREACTORS FOR ENVIRONMENTAL CONTROL AND PHYSICAL SIGNALLING
3.1 Environmental control of nutrients and metabolites
The critical parameter for cell survival in native and engineered tissues is oxygen (due to its low solubility in plasma and culture medium). In native tissues, oxygen is supplied by vascular network, over short diffusional transport distances and with the utilization of hemoglobin that increases the total oxygen content of blood. In conventional tissue engineering approaches, tissue constructs are just immersed in culture medium. Diffusional transport of oxygen under these conditions can support cell viability within only a ~100 µm thick outer layer, while the construct interior remains hypoxic (Figure 3A,B). To solve this problem, the entire construct can be perfused with culture medium, to supply oxygen to the cells occurs via both diffusion and convection, as in native tissues [9–11].
Figure 3. Environmental control of cells in bioreactors via medium perfusion .
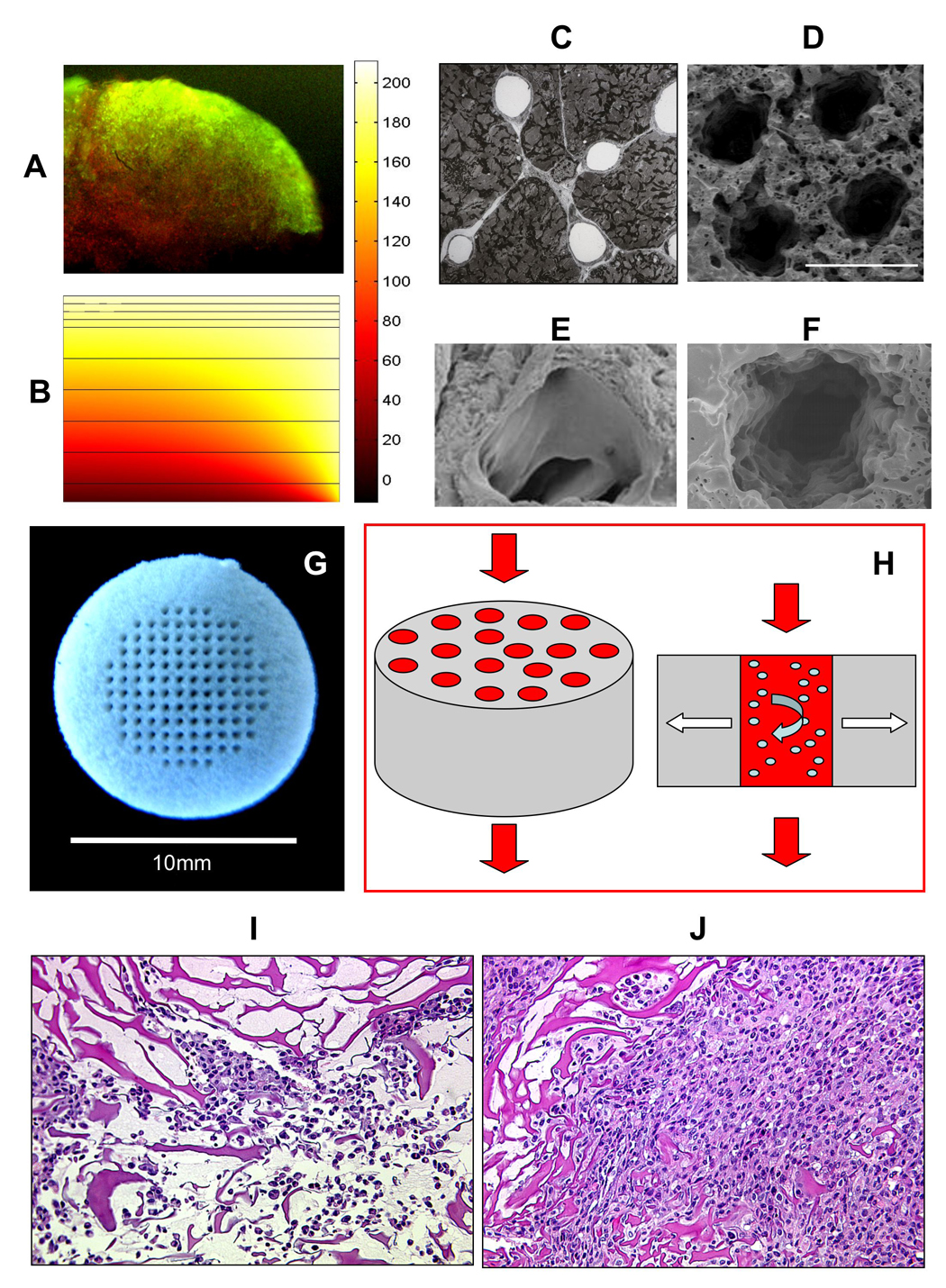
A) Live (green) and dead (red) staining of engineered cardiac tissue cultivated under static conditions B) Mathematical model of oxygen concentration in an engineered cardiac tissue. The model indicates that when oxygen is supplied by diffusion alone the interior of the construct remains hypoxic (one half of construct cross-section shown) C) Capillary network in the native myocardium D) Poly (glycerol sebacate) (PGS) scaffold with a channel array E) One capillary in the native myocardium F) One channel in the PGS scaffold G) Channel array in the PGS scaffold for perfusion cultivation H) Oxygen supply in a channeled engineered tissue using culture medium with PFC oxygen carriers. H&E staining of a collagen scaffold seeded with C2C12 myoblasts under I) static conditions or J) interstitial culture medium flow [9–11].
Our group has utilized gel-cell inoculation and an immediate establishment of the interstitial flow of culture medium through the seeded scaffolds to support physiologically high densities of cultured cells (Figure 3I,J) [9]. In this system, cells are “locked” into the scaffold during a short (10 min) gelation period, and supplied with oxygen at all times during culture. As the culture medium flow rate increases, so does the rate of oxygen supply. At the same time, the flow shear increases as well, creating a non-physiologic situation that can be detrimental to the cells. Recent studies with neonatal cardiomyocytes indicate that the application of interstitial flow at shear stresses higher than 2.4 dyn/cm2 resulted in p38 activation and initiation of apoptosis [12].
In native heart, cardiomyocytes are shielded from direct contact with blood by endothelial cells. To mimic the capillary network, cells were cultured on highly porous elastic polymer scaffold [13] with a parallel array of channels (Figure 3C–H). To mimic oxygen supply by hemoglobin, the culture medium was supplemented with a perfluorocarbon (PFC) emulsion (Figure 3H). Since PFC particles are immiscible with the aqueous phase of culture medium, they serve as rechargeable oxygen reservoirs, a mechanism of oxygen supply analogous to that provided by hemoglobin in blood. The combination of medium perfusion through channeled scaffolds and medium supplementation with PFC enabled the cultivation of millimeters thick cardiac constructs with physiologic density of viable cells expressing the molecular and functional cardiac markers [10, 11].
3.2 Providing mechanical forces to habitually loaded cells/tissues
In vivo, the changing 3D morphology gives rise to distinct mechanical stimuli that act synergistically with biological factors to regulate tissue development, maturation and remodeling. The iterative interaction between mechanical signals and organizational structure of the tissue results in specific structure-function relationships. For example, the anisotropic mechanical properties of long bones - result of the microscopic lamellar structure - are designed for structural load bearing along the long axis.
From a tissue-engineering perspective, subjecting immature tissues to physiological loading could be a way to acquire the necessary structural and functional characteristics. In most cases, much remains to be learned about the exact nature, levels and regime of application of mechanical signals. Mechanical stimulation also enhances the transport of nutrients to cells within the constructs by inducing convection. Shear stress was shown to have anabolic effect on osteoblasts and to stimulated the expression of bone-specific genes [14], a finding that enabled improved bioreactor designs [15, 16]. Similar insights have led to the development of advanced bioreactors with compressive loading of chondrocytes embedded in agarose to form cartilage [17] and cyclic tension to cardiomyoctes in collagen to engineer heart tissue [18]. Notably, the combined use of growth factors and mechanical stimulation synergistically improved the functional properties of engineered cartilage [19].
For bone, it is rather difficult to isolate the effects of shear from those of convective mass transfer. One important study used dextran molecules to obtain medium with different viscosities and thereby vary the shear levels without changing mass transport rates [20]. This approach enabled correlation between matrix deposition and shear stress, without affecting cell proliferation rates and the alkaline phosphatase (AP) activity of the cells.
For cardiac muscle, a classical study performed by Zimmermann and Eschenhagen lab explored the role of mechanical stress on maturation of engineered cardiac tissue [18]. The application of dynamic stretch to neonatal rat cardiomyocytes in ring-shaped collagen gels for just 7 days resulted in mature muscle bundles, well established ultra-structural organization, cell coupling, and force generation.
3.3 Providing electrical signals to excitable cells/tissues
The control of heart contractions is almost entirely self-contained. The propagation of electrical signals across specialized intracellular junctions produces mechanical contractions that pump blood forward. Orderly coupling between electrical pacing signals and macroscopic contractions is therefore crucial for the heart development and function.
The provision of electrical signals was thus expected to also enhance the assembly of engineered cardiac tissues. Cardiac constructs were subjected to supra-threshold electrical signals designed to mimic those in native heart [21]. Over only 8 days in vitro, electrical stimulation induced cell alignment and coupling, increased the amplitude of synchronous contractions by 7-fold, and resulted in remarkable ultrastructural organization. Development of conductive and contractile properties of cardiac constructs was concurrent, with strong dependence on the initiation and duration of the applied electrical stimulation (Figure 3).
There are two possible mechanisms of electrical stimulation: via electrical gradients or via electrically inducted contraction, and our data [21] as well as data from 2D studies suggest the latter. Interestingly, tissues engineered with the application of electrical field stimulation resemble in many aspects those engineered with mechanical stimulation [18]. Electrical stimulation induced hyperpolarization at the anode end of the cell and depolarization at the cathode end of the cell [22], such that the cells aligned with the electrical field lines were subjected to the largest voltage difference and were likely the first ones to generate action potentials, contract, and couple with other cells via processes at the cells’ ends.
The enhanced organization of contractile apparatus by electrical stimulation in vitro may parallel some aspects of embryonic development. There is a positive feedback between the electrical stimulation and the progressive development of contractile behavior and tissue ultrastructure. Induction and sensing of stretch appears to be crucial for the development and assembly of sarcomeres. In our experience [23] non-stimulated constructs had thick, diffuse Z-lines (Fig. 3C) similar to those found in the mice knockout for muscle LIM protein, a key Z-line protein involved in the sensing of stretch and signal propagation. It appears that the induction of synchronous contractions by electrical stimulation ensured unaltered calcium handling and maintained the capacity and density of L type Ca2+ channels [24].
3.4 Microarray platforms utilizing engineered tissues
Microtechnologies based on tissue engineering are becoming powerful tools to manipulate the cellular microenvironment and study cellular responses in real time and in quantitative fashion [25]. Small scale allows high-throughput studies designed to evaluate a large experimental space while utilizing small amounts of cells and materials [26]. One example of this approach is a microarray bioreactor with twelve culture wells on a standard microscope slide format (Figure 6 A,B) [27], designed to accommodate two culture settings: cells attached to a 2D substrate, and cells encapsulated in 3D hydrogel. Both formats allow for controlled perfusion of fluid to the cells, providing strict control of medium composition and hydrodynamic shear that the cells are exposed to. Human embryonic stem cells were cultivated in this system, and assessed for their cardiovascular differentiation potential. Cell viability of cells was greatly enhanced by perfusion (Figure 6E). Another attractive feature of this technology is its compliance with standard imaging formats. Since twelve culture wells were created on a glass slide, light, fluorescence and confocal microscopy can all be used and combined with numerous image analysis options [27].
Figure 6. Microarray bioreactors.
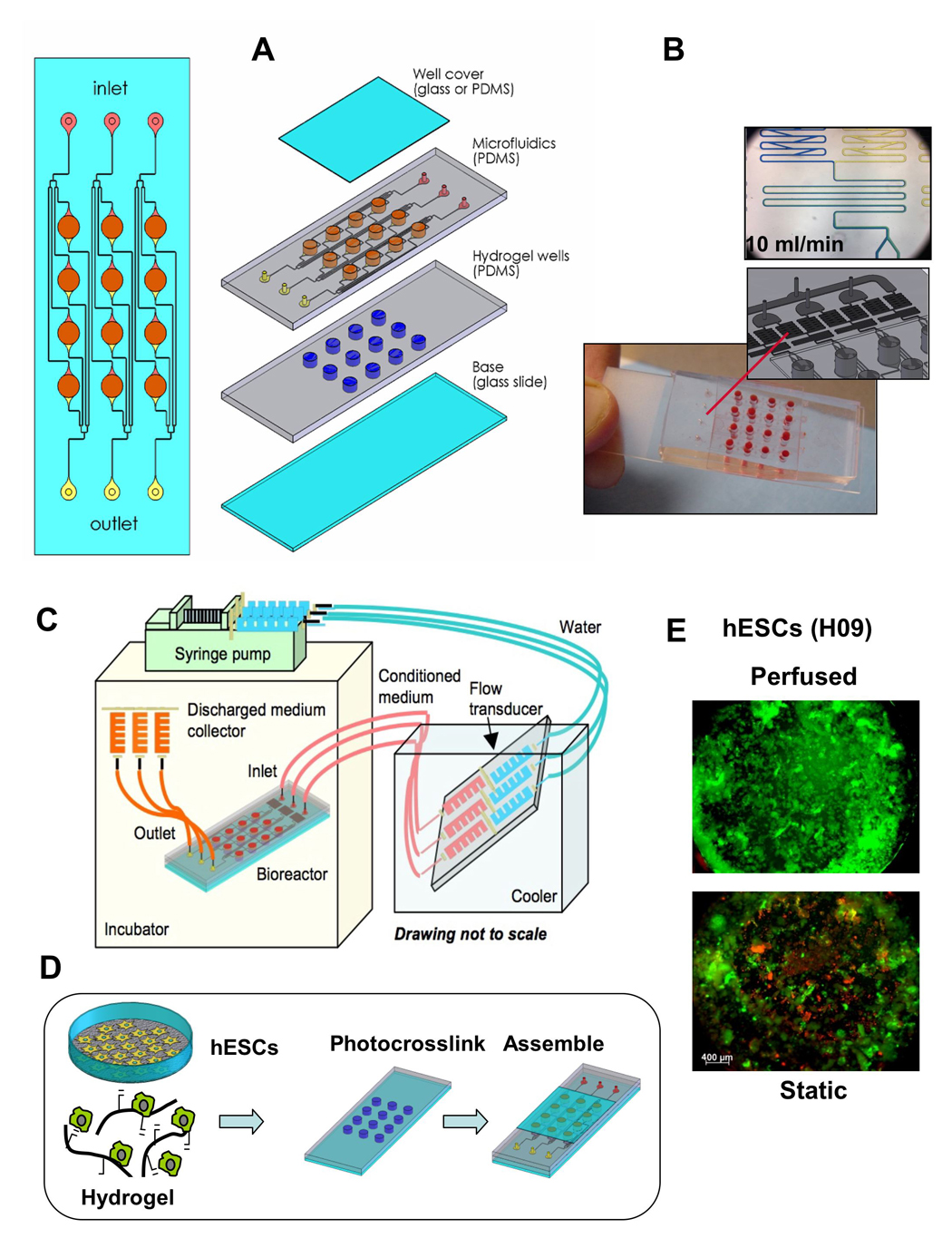
A An array of 3×4 independent culture wells (3.5 mm in diameter) that are independently perfused with culture medium and can be used for either 2D or 3D cell culture. This microbioreactor has a size of a microscope slide, and is assembled from layers of poly(dimethylsiloxane) (PDMS) and glass attached via plasma treatment. B Microfluidic “mixers” are used to supplement medium with a desired concentration of molecular factors. C Bioreactor setup in the incubator. D Assembly process for photoencapsulation of hESC. E Perfusion enhanced hESC viability [27].
Microtechnologies can also be utilized to generate small but functional tissue “organoids” for a variety of applications. Form example, cardiomyocytes were patterned on a substrate to produce synchronously contractile organoids that mimic the highly specific organization of cardiomyocytes in vivo (Figure 7 A,B). Over time, the cells functionally couple to each other to create strands of synchronously beating cardiac tissue, with progressively developing contractile function (Figure 7H) and expression of the cardiac differentiation markers (Figure 7 E,F) [28]. Such organoids can find utility in drug screening, electrophysiological studies and fundamental biological research.
Figure 7. Small tissue organoids for high-throughput research.
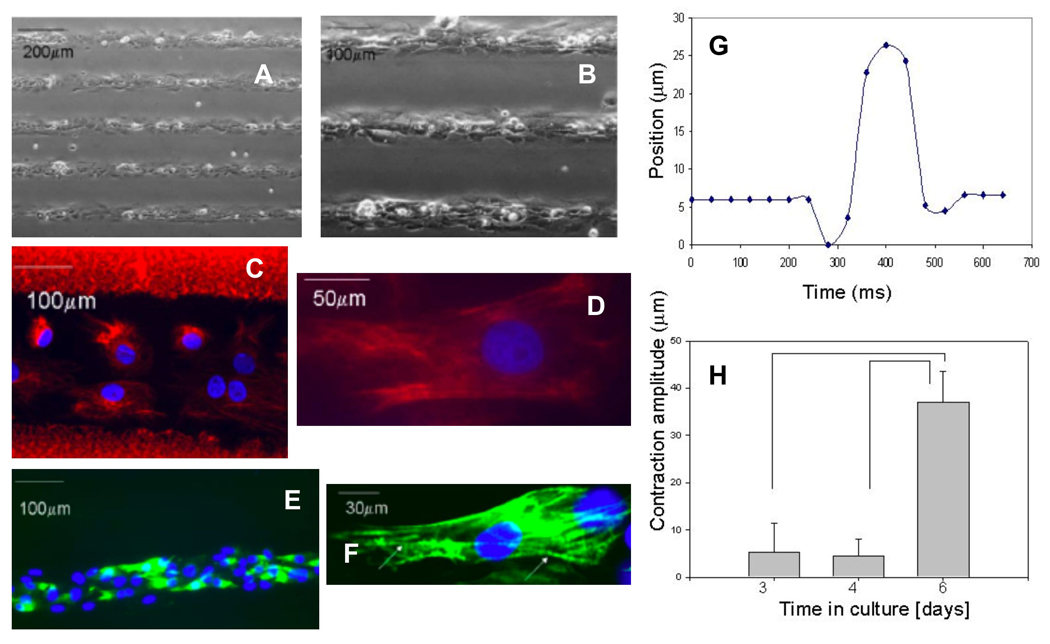
A,B Patterned surfaces were used to form contractile cardiac organoids over 8 days of culture, starting from isolated cardiac myosytes. C,D Immunofluorescent stain for intermediate filament vimentin (red). E,F Cardiac troponin I (green) and contractile apparatus (arrows). Nuclei are counterstained with DAPI (blue). G Contraction profile of a single organoid determined by on-line imaging. H Contraction amplitude of organoids increased with time of culture [28, 38].
4 COMPLEX TISSUES
Tissue engineering has largely utilized “minimalistic” approaches based on homogenous populations of cells provided with suitable environmental conditions to give rise to specific practical outcomes (e.g., mineralized scaffolds or contractile tissues). However, only a few tissue types are derived from single-cell populations. Bone, for example, is in a constant state of flux, based on interactions of osteocytes, osteoblasts and osteoclasts. Both the bone and cardiac tissues are highly vascularized such that the primary cell types are in close contact with other cell phenotypes. Creating complex tissues poses new requirements to the design of in vitro model systems, regarding the provision of multiple regulatory signals, mediation of cell-cell interactions and decision-making processes, and the spatial control of cell differentiation and tissue formation. This is the area where inputs from developmental biology are most valuable and most needed. The challenges faced by biologists and engineers are not trivial, and the field may need new tools for regulating micro-environmental conditions towards the formation of complex tissues.
4.1 Engineering osteochondral grafts
Cartilage and bone arise from a common progenitor, the mesenchymal stem cell, and exist in apposition at articular surfaces of synovial joints as well as in the epiphyseal growth plate. Initially, the differences in regulatory factors for chondrogenesis and osteogenesis were addressed by separate cultivation of cartilage an bone constructs, and subsequent joining of the two tissues to stimulate integration [29, 30]. In one of the most successful in vitro studies, hMSC pellets were press-fit into scaffolds and cultured in chondrogenic medium, followed by the seeding of hMSCs grown in osteogenic medium into the bone portion of the scaffolds. Cartilage-bone integration would likely be facilitated if the two tissues could be formed concurrently, in bioreactors that provide separate supply of bulk medium into the cartilage and bone regions, and separate mechanical loading. Many technical challenges to this truly “biomimetic” approach still need to be overcome, and the biological basis has not been fully established either.
4.2 Engineering vascularized grafts
Tissue engineering has a long-standing focus on the creation of stable vascular networks [31–33], and the vascularization of tissues including muscle [34] and bone [35, 36]. Studies investigated co-culture between osteoblasts or osteoprogenitors and endothelial cells resulted in contradictory findings regarding the ability of endothelial cells to induce or inhibit the expression of osteogenic genes. However, even in cases where the endothelial cells have had an inductive effect, concomitant in vitro formation of calcium deposition – the hallmark of bone – and blood vessel formation has not been achieved. Angiogenesis and osteogenesis are closely connected and tightly-regulated processes in vivo and much needs to be learned about the combinations and timing of the signals – molecular, structural, physical - needed to stimulate the two processes simultaneously in vitro.
5 SUMMARY
By faithfully recapitulating the tissue context in vitro, we would create realistic experimental models that can be used to better understand developmental and regenerative processes. Because of the complex and dynamic nature of cell responses to regulatory signals, non-invasive (longitudinal) imaging of engineered constructs during cultivation would greatly advance our ability to study cellular responses to micro-environmental parameters with spatial and temporal specificity. The selection of functional readouts and the creation of appropriate molecular markers, through insights from developmental biology, are critical for developing bioreactor-imaging technologies. On-line imaging would enable us to learn about the combinations and timing of biophysical stimuli that are necessary to direct the fate-making decisions of stem-progenitor cells and guide the formation of tissues with multiple cellular phenotypes. It is rare that the effects of different stimuli – molecular, structural and physical - are additive, and it is necessary to study the biophysical stimulation from a systemic point, and to focus on the entire context. We seem to be getting closer to this goal, through interactions between biology and engineering at multiple levels. While biology provides the fundamental design requirements for tissue engineering, engineered tissues can serve as models for studies of development and disease and thereby foster biological research.
Figure 4. Perfusion and loading for engineering of osteochondral tissues.
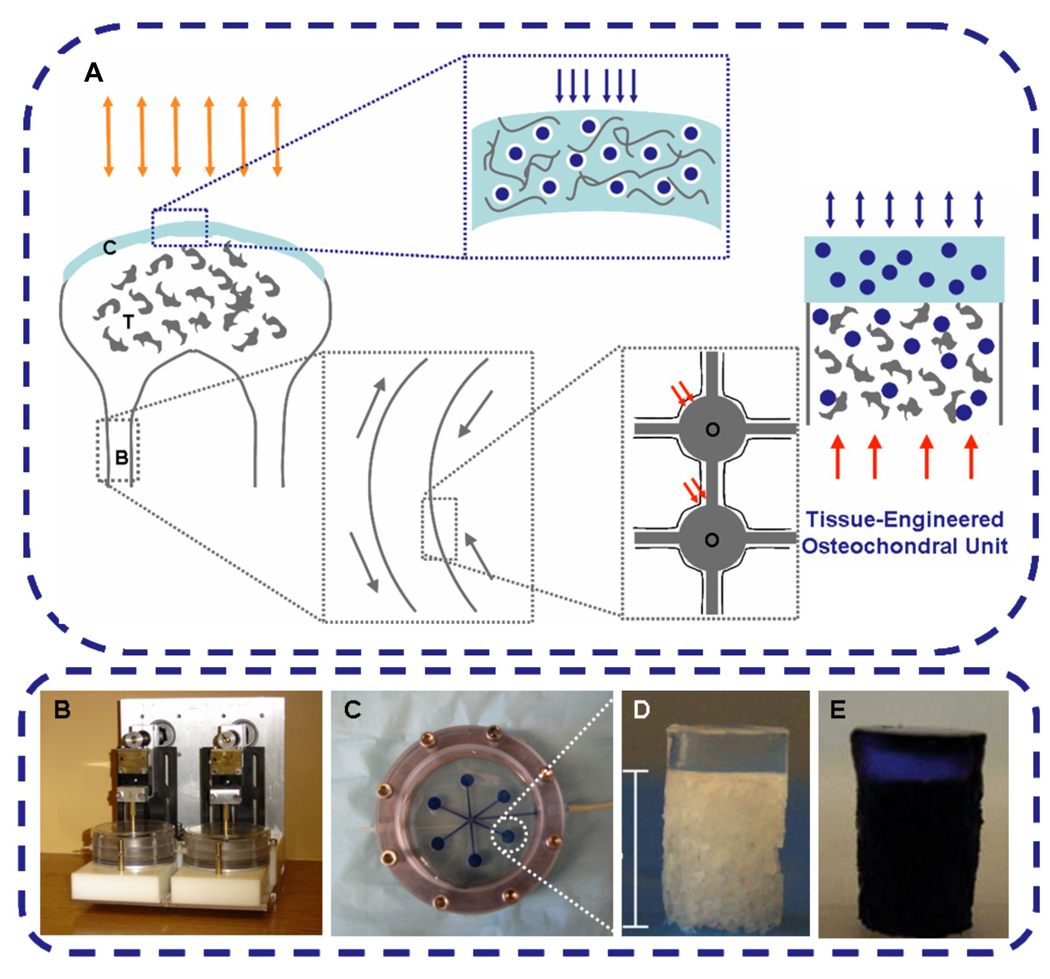
A Translation of mechanical forces in an articular joint involves compressive loading (orange arrows) of cartilage C) and bone (B). In the cartilage region (blue box), the loads (blue arrows) are transferred to chondrocytes through compression of the ECM resulting in mechanical straining of cells (blue circles). In the bone region (grey box), the compressive loads cause bending (grey arrows) and oscillatory fluid flow around the osteocytes (O) trapped in lacunae (red arrows). B–E Tissue engineering bioreactors can be designed to provide these same mechanical stimuli – dynamic compression of the cartilage region (blue arrows), and perfusion of the bone region (red arrows). Bioreactors used to impart dynamic compression (via steel platens) to cartilage regions (B) and interstitial fluid flow through the bone regions (six osteochondral plugs are shown), C). D In both cases, osteochondral plugs are made from decellularized bovine trabecular bone (bone scaffold) interfaced with hydrogel (cartilage scaffold). E Blue dye traces flow patterns in the constructs.
Figure 5. Electrical and mechanical stimulation for engineering of cardiac tissues.
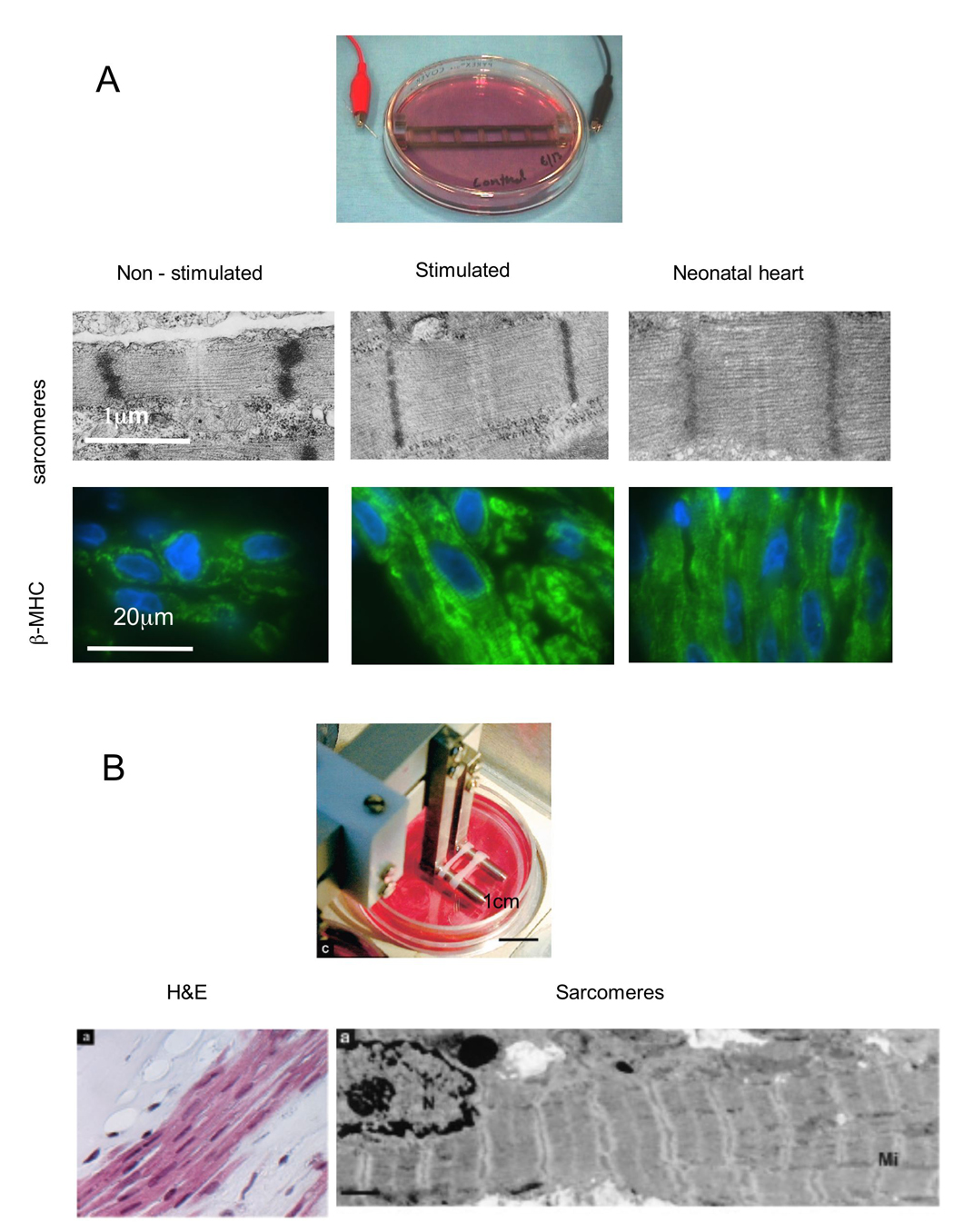
A Cardiac-like electrical field stimulation applied to cardiac cells inoculated via hydrogel into collagen sponges [21]. B Cyclic mechanical stretch was applied to cardiac cells inoculated incollagen gel [18]. In both cases, stimulation enhanced cell differentiation, alignment and coupling, and resulted in a remarkably well-developed contractile apparatus.
ACKNOWLEDGMENT
The authors gratefully acknowledge research support by the National Institutes of Health (HL076485, DE16525 and EB002520 to G.V.-N.) and Canada Foundation for Innovation (Leaders Opportunity Fund to M.R.).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Ferreira LS, Gerecht S, Fuller J, Shieh HF, Vunjak-Novakovic G, Langer R. Bioactive hydrogel scaffolds for controllable vascular differentiation of human embryonic stem cells. Biomaterials. 2007;28:2706–2717. doi: 10.1016/j.biomaterials.2007.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kraehenbuehl TP, Zammaretti P, Van der Vlies AJ, Schoenmakers RG, Lutolf MP, Jaconi ME, et al. Three-dimensional extracellular matrix-directed cardioprogenitor differentiation: Systematic modulation of a synthetic cell-responsive PEG-hydrogel. Biomaterials. 2008;29:2757–2766. doi: 10.1016/j.biomaterials.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 3.Radisic M, Park H, Martens TP, Salazar-Lazaro JE, Geng WL, Wang YD, et al. Pre-treatment of synthetic elastomeric scaffolds by cardiac fibroblasts improves engineered heart tissue. Journal of Biomedical Materials Research Part A. 2008;86A:713–724. doi: 10.1002/jbm.a.31578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rockwood DN, Akins RE, Jr, Parrag IC, Woodhouse KA, Rabolt JF. Culture on electrospun polyurethane scaffolds decreases atrial natriuretic peptide expression by cardiomyocytes in vitro. Biomaterials. 2008;29:4783–4791. doi: 10.1016/j.biomaterials.2008.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uebersax L, Hagenmueller H, Hofmann S, Gruenblatt E, Mueller R, Vunjak-Novakovic G, et al. Effect of scaffold design on bone morphology in vitro. Tissue Engineering. 2006;12:3417–3429. doi: 10.1089/ten.2006.12.3417. [DOI] [PubMed] [Google Scholar]
- 6.Grayson WL, Bhumiratana S, Cannizzaro C, Chao GP, Lennon D, Caplan AI, Vunjak-Novakovic G. Effects of initial seeding density and fluid perfusion rate on formation of tissue-engineered bone. Tissue Eng A. 2008;14:1809–1820. doi: 10.1089/ten.tea.2007.0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fischbach C, Chen R, Matsumoto T, Schmelzle T, Brugge JS, Polverini PJ, et al. Engineering tumors with 3D scaffolds. Nature Methods. 2007;4:855–860. doi: 10.1038/nmeth1085. [DOI] [PubMed] [Google Scholar]
- 8.Ott HC, Matthiesen TS, Goh SK, Black LD, Kren SM, Netoff TI, et al. Perfusion-decellularized matrix: using nature's platform to engineer a bioartificial heart. Nature Medicine. 2008;14:213–221. doi: 10.1038/nm1684. [DOI] [PubMed] [Google Scholar]
- 9.Radisic M, Euloth M, Yang L, Langer R, Freed LE, Vunjak-Novakovic G. High-density seeding of myocyte cells for cardiac tissue engineering. Biotechnol Bioeng. 2003;82:403–414. doi: 10.1002/bit.10594. [DOI] [PubMed] [Google Scholar]
- 10.Radisic M, Park H, Chen F, Salazar-Lazzaro JE, Wang Y, Dennis R, et al. Biomimetic approach to cardiac tissue engineering: oxygen carriers and channeled scaffolds. Tissue Eng. 2006;12:2077–2091. doi: 10.1089/ten.2006.12.2077. [DOI] [PubMed] [Google Scholar]
- 11.Radisic M, Yang L, Boublik J, Cohen RJ, Langer R, Freed LE, et al. Medium perfusion enables engineering of compact and contractile cardiac tissue. Am J Physiol Heart Circ Physiol. 2004;286:H507–H516. doi: 10.1152/ajpheart.00171.2003. [DOI] [PubMed] [Google Scholar]
- 12.Dvir T, Levy O, Shachar M, Granot Y, Cohen S. Activation of the ERK1/2 cascade via pulsatile interstitial fluid flow promotes cardiac tissue assembly. Tissue Eng. 2007;13:2185–2193. doi: 10.1089/ten.2006.0364. [DOI] [PubMed] [Google Scholar]
- 13.Wang Y, Ameer GA, Sheppard BJ, Langer R. A tough biodegradable elastomer. Nature Biotechnology. 2002;20:602–606. doi: 10.1038/nbt0602-602. [DOI] [PubMed] [Google Scholar]
- 14.Owan I, Burr DB, Turner CH, Qiu JY, Tu Y, Onyia JE, et al. Mechanotransduction in bone: Osteoblasts are more responsive to fluid forces than mechanical strain. American Journal of Physiology-Cell Physiology. 1997;42 doi: 10.1152/ajpcell.1997.273.3.C810. C810-C5. [DOI] [PubMed] [Google Scholar]
- 15.Bancroft GN, Sikavitsas VI, Mikos AG. Design of a flow perfusion bioreactor system for bone tissue-engineering applications. Tissue Engineering. 2003;9:549–554. doi: 10.1089/107632703322066723. [DOI] [PubMed] [Google Scholar]
- 16.Grayson WL, Bhumiratana S, Cannizzaro C, Chao GP, Lennon D, Caplan AI, Vunjak-Novakovic G. Effects of initial seeding density and fluid perfusion rate on formation of tissue-engineered bone. Tissue Eng. doi: 10.1089/ten.tea.2007.0255. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mauck RL, Soltz MA, Wang CC, Wong DD, Chao P-HG, Valhmu WB, et al. Functional tissue engineering of articular cartilage through dynamic loading of chondrocyte-seeded agarose gels. J. Biomech. Eng. 2000;122:252–260. doi: 10.1115/1.429656. [DOI] [PubMed] [Google Scholar]
- 18.Zimmermann WH, Schneiderbanger K, Schubert P, Didie M, Munzel F, Heubach JF, et al. Tissue engineering of a differentiated cardiac muscle construct. Circulation Research. 2002;90:223–230. doi: 10.1161/hh0202.103644. [DOI] [PubMed] [Google Scholar]
- 19.Mauck RL, Nicoll SB, Seyhan SL, Ateshian GA, Hung CT. Synergistic action of growth factors and dynamic loading for articular cartilage tissue engineering. Tissue Engineering. 2003;9:597–611. doi: 10.1089/107632703768247304. [DOI] [PubMed] [Google Scholar]
- 20.Sikavitsas VI, Bancroft GN, Holtorf HL, Jansen JA, Mikos AG. Mineralized matrix deposition by marrow stromal osteoblasts in 3D perfusion culture increases with increasing fluid shear forces. Proceedings of the National Academy of Sciences of the United States of America. 2003;100:14683–14688. doi: 10.1073/pnas.2434367100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Radisic M, Park H, Shing H, Consi T, Schoen FJ, Langer R, et al. Functional assembly of engineered myocardium by electrical stimulation of cardiac myocytes cultured on scaffolds. Proceedings of the National Academy of Sciences of the United States of America. 2004;101:18129–18134. doi: 10.1073/pnas.0407817101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tung L, Sliz N, Mulligan MR. Influence of electrical axis of stimulation on excitation of cardiac muscle cells. Circulation Research. 1991;69:722–730. doi: 10.1161/01.res.69.3.722. [DOI] [PubMed] [Google Scholar]
- 23.Radisic M, Park H, Shing H, Consi T, Schoen FJ, Langer R, et al. Functional assembly of engineered myocardium by electrical stimulation of cardiac myocytes cultured on scaffolds. Proc Natl Acad Sci U S A. 2004;101:18129–18134. doi: 10.1073/pnas.0407817101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berger HJ, Prasad SK, Davidoff AJ, Pimental D, Ellingsen O, Marsh JD, et al. Continual electric field stimulation preserves contractile function of adult ventricular myocytes in primary culture. American Journal of Physiology: Heart and Circulatory Physiology. 1994;266:H341–H349. doi: 10.1152/ajpheart.1994.266.1.H341. [DOI] [PubMed] [Google Scholar]
- 25.Li N, Tourovskaia A, Folch A. Biology on a chip: microfabrication for studying the behavior of cultured cells. Critical Reviews in Biomedical Engineering. 2003;31:423–488. doi: 10.1615/critrevbiomedeng.v31.i56.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sia SK, Whitesides GM. Microfluidic devices fabricated in poly(dimethylsiloxane) for biological studies. Electrophoresis. 2003;24:3563–3576. doi: 10.1002/elps.200305584. [DOI] [PubMed] [Google Scholar]
- 27.Figallo E, Cannizzaro C, Gerecht-Nir S, Burdick J, Langer R, Elvassore N, Vunjak-Novakovic G. Microbioreactor for controlled differentiation of human embryonic stem cells. Lab on a Chip. 2007;7:710–719. doi: 10.1039/b700063d. [DOI] [PubMed] [Google Scholar]
- 28.Khademhosseini A, Eng G, Yeh J, Kucharczyk PA, Langer R, Vunjak-Novakovic G, et al. Microfluidic patterning for fabrication of contractile cardiac organoids. Biomedical Microdevices. 2007;9:149–157. doi: 10.1007/s10544-006-9013-7. [DOI] [PubMed] [Google Scholar]
- 29.Alhadlaq A, Elisseeff JH, Hong L, Williams CG, Caplan AI, Sharma B, et al. Adult stem cell driven genesis of human-shaped articular condyle. Annals of Biomedical Engineering. 2004;32:911–923. doi: 10.1023/b:abme.0000032454.53116.ee. [DOI] [PubMed] [Google Scholar]
- 30.Augst A, Marolt D, Freed LE, Vepari C, Meinel L, Farley M, et al. Effects of chondrogenic and osteogenic regulatory factors on composite constructs grown using human mesenchymal stem cells, silk scaffolds and bioreactors. Journal of the Royal Society Interface. 2008;5:929–939. doi: 10.1098/rsif.2007.1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Au P, Tam J, Fukumura D, Jain RK. Bone marrow-derived mesenchymal stem cells facilitate engineering of long-lasting functional vasculature. Blood. 2008;111:4551–4558. doi: 10.1182/blood-2007-10-118273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Koike N, Fukumura D, Gralla O, Au P, Schechner JS, Jain RK. Creation of long-lasting blood vessels. Nature. 2004;428:138–139. doi: 10.1038/428138a. [DOI] [PubMed] [Google Scholar]
- 33.Peters MC, Polverini PJ, Mooney DJ. Engineering vascular networks in porous polymer matrices. Journal of Biomedical Materials Research. 2002;60:668–678. doi: 10.1002/jbm.10134. [DOI] [PubMed] [Google Scholar]
- 34.Levenberg S, Rouwkema J, Macdonald M, Garfein ES, Kohane DS, Darland DC, et al. Engineering vascularized skeletal muscle tissue. Nature Biotechnology. 2005;23:879–884. doi: 10.1038/nbt1109. [DOI] [PubMed] [Google Scholar]
- 35.Rouwkema J, Rivron NC, Bettahalli NMS, Stamatialis D, Wessling M, van Blitterswijk CA. Mesenchymal stem cells differentiate towards endothelial cells in a prevascularized bone tissue engineering setting. Tissue Engineering Part A. 2008;14:OP188. [Google Scholar]
- 36.Kneser U, Schaefer DJ, Polykandriotis E, Horch RE. Tissue engineering of bone: the reconstructive surgeon' point of view. Journal of Cellular and Molecular Medicine. 2006;10:7–19. doi: 10.1111/j.1582-4934.2006.tb00287.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guldberg RE, Boerckel JD, Dosier CR, Dupont KM, Johnson MR, Lin ASP, Oest ME, Peister A, O'keefe RJ. Transational approaches to bone repair. In: Mao JJ, Vunjak-Novakovic G, Mikos A, Atala A, editors. Translational Approaches in Tissue Engineering. Artech House: 2007. [Google Scholar]
- 38.Karp JM, Yeo Y, Geng WL, Cannizarro C, Yan K, Kohane DS, et al. A photolithographic method to create cellular micropatterns. Biomaterials. 2006;27:4755–4764. doi: 10.1016/j.biomaterials.2006.04.028. [DOI] [PubMed] [Google Scholar]


