Abstract
Context
Prescription drug costs are a major component of health care expenditures, yet resources to support evidence-based prescribing are not widely available.
Objective
To evaluate the effectiveness of computerized prescribing alerts, with or without physician-led group educational sessions, to reduce the prescribing of heavily marketed hypnotic medications.
Design
Cluster-randomized controlled trial.
Setting
We randomly allocated 14 internal medicine practice sites to receive usual care, computerized prescribing alerts alone, or alerts plus group educational sessions.
Measurements
Proportion of heavily marketed hypnotics prescribed before and after the implementation of computerized alerts and educational sessions.
Main Results
The activation of computerized alerts held the prescribing of heavily marketed hypnotic medications at pre-intervention levels in both the alert-only group (adjusted risk ratio [RR] 0.97; 95% CI 0.82–1.14) and the alert-plus-education group (RR 0.98; 95% CI 0.83–1.17) while the usual-care group experienced an increase in prescribing (RR 1.31; 95% CI 1.08–1.60). Compared to the usual-care group, the relative risk of prescribing heavily marketed medications was less in both the alert-group (Ratio of risk ratios [RRR] 0.74; 95% CI 0.57–0.96) and the alert-plus-education group (RRR 0.74; 95% CI 0.58–0.97). The prescribing of heavily marketed medications was similar in the alert-group and alert-plus-education group (RRR 1.02; 95% CI 0.80–1.29). Most clinicians reported that the alerts provided useful prescribing information (88%) and did not interfere with daily workflow (70%).
Conclusions
Computerized decision support is an effective tool to reduce the prescribing of heavily marketed hypnotic medications in ambulatory care settings.
Trial Registration
clinicaltrials.gov Identifier: NCT00788346.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-009-1013-x) contains supplementary material, which is available to authorized users.
KEY WORDS: prescription drugs, effectiveness, marketed medications, prescribing, decision support, computerized alerts
BACKGROUND
Total heath care expenditures in the United States grew to $2.1 trillion in 2006, costing $7,026 per person and accounting for 16% of the U.S. gross domestic product.1,2 Prescription drug costs remain a key component of health care expenses, totaling over $216 billion per year.2 Concurrently, the U.S. pharmaceutical industry spent over $29 billion to promote medications to consumers and health care professionals.3–6 While the merits of pharmaceutical advertising have been intensely debated, concerns remain that advertising may lead to clinically unnecessary and overly expensive treatments.4,7–9
Despite rising pharmaceutical costs, resources to support evidence-based prescribing and to offset the pharmaceutical industry’s consumer and prescriber marketing efforts are not widely available. Computerized prescribing alerts and decision-support tools have been shown to improve the safety of prescribing in numerous settings10–15 and promote the use of formulary medications in the inpatient setting,16 but their ability to support prescribing around heavily marketed medications in the ambulatory setting has not been evaluated.
In 2004, the pharmaceutical manufacturer Warner-Lambert, now a subsidiary of Pfizer Inc., plead guilty to allegations of illegally marketing the drug Neurontin® (gabapentin).17,18 The settlement provided for the establishment of the Consumer and Prescriber Education Grant Program with the goal of developing programs to provide information to health care professionals and consumers about prescription drugs.18 This study is one of the Program’s early initiatives.
We evaluated the use of computerized prescribing alerts, with and without physician-led educational sessions, to reduce the prescribing of heavily marketed hypnotic medications in the ambulatory setting. The intervention targeted these agents because they were the most heavily marketed medication class in 2006.1,4,19 We hypothesized that computerized decision support would decrease the prescribing of heavily marketed hypnotic medications and that group educational sessions would enhance that effect.
METHODS
Setting and Study Design
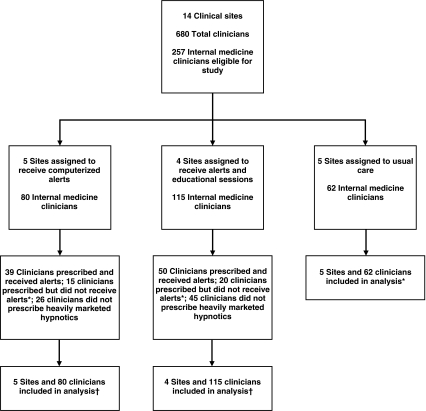
We carried out a cluster-randomized controlled trial at 14 internal medicine practice sites within Harvard Vanguard Medical Associates (HVMA), a large multi-specialty group practice. We assessed the effectiveness of prescribing alerts, with and without physician-led educational sessions, to reduce the prescribing of heavily marketed hypnotic medications. We randomized practice sites to receive computerized alerts alone, alerts plus educational sessions, or usual care (Fig. 1). Usual care consisted of an alert stating only the copayment tier of the medication (1, 2, or 3 – corresponding to the out-of-pocket cost of the medication incurred by the patient). The statistician (FZ) used a random number generator in SAS to assign clinical sites to study groups while accounting for the total number of physicians at each site. Once the random assignments were made, the other investigators were informed of assignments to allow for planning of the educational sessions and activation of the alerts.
Figure 1.
Study Flow Diagram * Clinicians did not receive prescribing alerts for refills for medications begun prior to the initiation of the study or if they joined HMVA after the initiation of the study † Analyses performed on group level data; Actual number of clinicians in each group may vary during the study period based on newly hired clinicians or clinicians leaving the practice.
We targeted Ambien CR® (zolpidem tartrate extended release), Lunesta® (eszopiclone), Sonata® (zaleplon), and Rozerem® (ramelteon) due to the high intensity of direct-to-consumer and direct-to-prescriber marketing of these medications in 2006 and the availability of lower cost efficacious alternatives. Ambien CR® became available in October 2005, Lunesta® in April 2005, Rozerem® in August 2005, and Sonata® was FDA approved in 1999 and available shortly thereafter. Based on the HVMA Pharmaceutical and Therapeutics Committee guidelines,20 the alerts recommended generic zolpidem or trazodone for the initial pharmacologic treatment of insomnia after sleep hygiene correction. We collected prescribing data directly from the electronic health record between (3/11/2005 - 3/10/2008). Data collected from 3/11/2005–3/10/2006 was intended to establish the initial rise in prescribing of these new hypnotics and was not included in the analysis. We limited our pre-specified analyses to the one-year baseline period (3/11/2006–3/10/2007) and throughout the intervention period (3/11/2007–3/10/2008).
We included all clinicians practicing in internal medicine, including physicians and advanced practice clinicians (nurse practitioners or physician assistants). Within internal medicine clinical sites, we included both primary care and urgent care providers.
This study was approved by the Human Studies Committee of HVMA and Harvard Pilgrim Health Care and was supported by a grant from the Attorneys General Consumer and Prescriber Education Grant Program.
Prescribing Alerts
HVMA has used an electronic health record, Epic® (Epic Systems Corporation, Verona, Wisconsin), for all ambulatory patient encounters since 1997. When Epic® was installed, use of its integrated electronic prescribing functionality was mandated and paper prescriptions were eliminated. As such, handwritten prescriptions have constituted far less than 1% of all prescriptions written over the past decade. Clinicians can still telephone prescriptions to non-HVMA pharmacies without generating an electronic prescription in Epic®; however, these prescriptions are rare—accounting for less than 1% of prescriptions in internal medicine at HVMA over the past 5 years.
We developed a novel decision support system that was based on the Best Practice® and SmartSet® platforms available in Epic®. Any new prescription for a study medication (Ambien CR®, Lunesta®, Sonata®, or Rozerem®) triggered an alert. We considered a new prescription to be one which was not previously prescribed within Epic®. To prevent clinicians from repeatedly receiving alerts for the same patient, we did not activate alerts for subsequent refills of study medications. The alert began by recommending an alternative medication, prompting the prescribing clinician to continue to an Epic® SmartSet, i.e., an order set with decision-support options (Online Appendix Fig. 1). The decision support provided recommendations for alternative medications (zolpidem, trazodone), links to graphical summaries of current evidence from the literature, specific co-payment information, prescribing information, and patient educational materials about insomnia and sleep hygiene. The alerts also offered the ability to assign an appropriate diagnostic code and level of service to the encounter.
Group Educational Sessions
Between June and July 2007, we scheduled a group educational session at each of the four practice sites allocated to this study arm. A total of 58 internal medicine clinicians (71% of eligible clinicians; Site 1, = 12; Site , N = 13; Site N = 23; Site 4, = 10) participated in the 45-minute interactive group discussions, which were led by an experienced internist (either FXC or SRS). These group educational sessions, incorporating principles of academic detailing,21 focused on medications for insomnia, including the barriers to prescribing the agents recommended in the HVMA guidelines. The sessions also emphasized nonpharmacologic therapies, including sleep hygiene correction. Urgent care medicine providers did not attend the educational sessions due to scheduling constraints. We subsequently sent a single educational information packet via interoffice mail to each internal medicine clinician at the group educational sites; the packet included educational information on insomnia and hypnotic medications.
Survey
We performed a post-intervention survey to assess clinicians’ attitudes regarding the new computerized prescribing alerts. The post-intervention survey was part of a larger survey conducted at HVMA. A total of 89 internal medicine clinicians received at least one new hypnotic alert and were eligible to respond to the questions regarding the new alerts.
Prescribing Data Collection
We obtained prescribing data through a direct query of the HVMA Epic® electronic health record. Members of the information technology team at HVMA, independent of the research team, performed the query of the electronic health record based on National Drug Codes (NDC) for all generic and trade names and all strengths of the study medications.
Outcomes and Statistical Analysis
Our primary outcome was the proportion of prescriptions for hypnotic medications that were for heavily marketed medications (i.e. study medications/study medications plus zolpidem and trazodone). We used binomial regression with generalized estimating equations to compare the proportion of heavily marketed medications prescribed before and after the activation of alerts in each study group and the usual care group. We used binomial regression models to calculate risk ratios (RR) rather than odds ratios (OR) based on previously validated methods.22 The models corrected for clustering within practice sites and for repeated pre- and post-intervention measurements for each provider. In addition the models controlled for clinician age, gender, full-time status (≥ 0.75 full-time equivalent [FTE]), years in practice, role (advanced practice clinician [nurse practitioner, physician assistant] or physician), and whether the prescribing clinician was a primary care or urgent care physician. We used an interaction term (ratio of adjusted risk ratios) to compare the differences in prescribing before and after the intervention between the study groups and the usual care group.
We also analyzed data directly from the activation of alerts and performed stratified analyses of factors correlated with alert-induced prescribing change. The proportion of prescriptions changed in response to the alerts was calculated directly and stratified analyses evaluated with χ2 test statistics and analysis of variance (ANOVA).
We dichotomized survey responses (agree vs. disagree) and present descriptive statistics with 95% confidence intervals.
We performed all analysis based on the original intention to treat (Fig. 1). All tests were two-tailed, with < 0.05 used to determine statistical significance, and performed using SAS version 9.1.
RESULTS
Study Groups
Of the 257 internal medicine clinicians included in this study, 179 providers prescribed one or more heavily market hypnotic medication during the study period from 3/11/2007 to 3/10/2008. Eighty-nine internal medicine providers received at least one alert, with a total of 245 alerts activated during the study period. Characteristics of the study groups are listed in Table 1. There were more internal medicine clinicians in the alert plus education group compared to the alert-only or control groups, and the alert-only group had a higher percentage of full-time providers. Other group characteristics were balanced.
Table 1.
Characteristics of Study Groups
| Characteristic | Alerts ( = 5 Sites) | Alerts + Education* ( = 4 Sites) | Control ( = 5 Sites) | P† |
|---|---|---|---|---|
| Number of clinicians‡ | 80 | 115 | 62 | |
| Role | ||||
| Physician | 58 (73%) | 83 (72%) | 40 (65%) | 0.5 |
| NP/PA§ | 22 (28%) | 32 (28%) | 22 (35%) | |
| Average clinician age (years) | 48.8 | 47.8 | 50.6 | 0.2 |
| Female | 53 (66%) | 72 (63%) | 44 (71%) | 0.5 |
| Full Time ‖ | 61 (76%) | 59 (51%) | 33 (53%) | 0.001 |
| Primary care provider | 52 (65%) | 60 (52%) | 36 (58%) | 0.2 |
| Average panel size, | 1545 | 1573 | 1713 | 0.6 |
| Average years in practice | 12.0 | 11.5 | 11.7 | 0.9 |
* Education indicates group educational sessions with follow-up mailings
† ANOVA or χ2
‡ Includes both primary care and urgent care clinicians in internal medicine
§ NP/PA indicates nurse practitioner or physician assistant
‖ ≥ 0.75 full-time equivalent (FTE)
Computerized Alerts and Group Educational Sessions
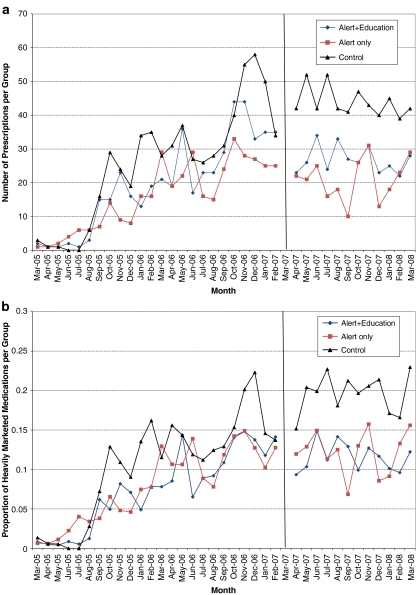
The numbers of prescriptions for Ambien CR®, Lunesta®, Rozerem®, and Sonata® increased sharply in mid-2005 as these medications became increasingly available. There were 1,111 prescriptions for heavily marketed hypnotics during the baseline period (3/11/2006–3/10/2007) and 1,107 prescriptions after the prescribing alerts were activated (3/11/2007–3/10/2008). The activation of computerized prescribing alerts held the proportion of heavily marketed medications prescribed at pre-intervention levels in the alert-only and alert-plus-education groups (Fig. 2 a and b). At the same time, the usual-care sites experienced an increase in the proportion of heavily marketed hypnotic medications prescribed (Fig. 2a and b).
Figure 2.
a. Monthly Prescriptions for Heavily Marketed Hypnotic Medications. The figure shows the reduction of heavily marketed hypnotic medications attributable to the implementation of alerts (vertical lint) in both the alert-only and alert-plus-education groups. The initial increase in prescribing corresponds to the increasing availability of Ambien CR®, Lunesta®, and Rozerem® in mid-2005. b. After the implementation of alerts (vertical line), the proportion of heavily marketed hypnotics [study medications/study medications plus generic zolpidem and trazodone] remained stable in the alert-only and alert-plus-education groups while the proportion increased in the usual-care group.
Table 2 shows the results of the binomial regression analysis with generalized estimating equations to control for clustering at the level of the physician as well as physician-level covariates. Compared to the baseline period, the usual-care group experienced an increase in the total proportion of heavily marketed hypnotic medications prescribed. Over the same time period, the proportion of heavily marketed hypnotic medications prescribed in the intervention groups remained stable (Table 2). Comparing the adjusted risk ratios between study groups, the relative risk of prescribing heavily marketed medications in the alert-group during the intervention period was less than in the usual-care group (Ratio of risk ratios (RRR) 0.74; 95% CI 0.57–0.96; P = 0.02). Similarly, the relative risk of prescribing heavily marketed hypnotics in the alert-plus-education group was less than in the usual-care group (RRR 0.74; 95% CI 0.58–0.97, P = 0.03). The prescribing of heavily marketed medications was similar in the alert-only group and the alert-plus-education group (RRR 1.02; 95% CI 0.80 - 1.29; P = 0.90).
Table 2.
Changes in the Proportion of Prescriptions for Heavily Marketed Medications after the Implementation of Computerized Prescribing Alerts
| Study Arms | Baseline Period | Intervention Period RR (95%CI) | Intervention Period Adjusted RR * (95%CI) | Ratio of RR † (95%CI) |
|---|---|---|---|---|
| Control | 1.0 | 1.27 (1.05, 1.54) | 1.31 (1.08, 1.60) | 1.0 |
| Alert | 1.0 | 0.99 (0.84, 1.17) | 0.97 (0.82, 1.14) | 0.74 (0.57, 0.96) |
| Alert + Education | 1.0 | 1.03 (0.89, 1.21) | 0.98 (0.83, 1.17) | 0.74 (0.58, 0.97) |
* Adjusted for physician age, gender, full time status (0/1, ≥ 0.75 FTE), years in practice, degree, PCP (yes/no)
† A ratio of the risk ratios was used to compare the adjusted risk ratios between the intervention groups and the control group
Overall, 23.3% (57/245) of prescriptions for heavily marketed hypnotics that activated an electronic alert were changed to a generic equivalent. The efficacy of the alerts did not vary by type of encounter (office visit, urgent care, telephone), clinician age, gender, full-time status, role (MD/DO or NP/PA), practice location (inside vs. outside Boston), or whether the site received group educational sessions (data not shown).
Survey
Among 89 internal medicine clinicians who received the new hypnotic alerts, a total of 51 (57.3%) responded to questions regarding the new prescribing alerts (Table 3).
Table 3.
Clinician Attitudes Regarding New Prescribing Alerts
| Question* | % Agree | 95% CI |
|---|---|---|
| Alerts prompted me to spend more time discussing alternative treatments with my patient(s) ( = 51) | 24 (47%) | 33–62% |
| Alerts provide useful evidence to support prescribing decisions ( = 49) | 43 (88%) | 75–95% |
| Alerts provide useful patient educational materials regarding insomnia ( = 48) | 40 (83%) | 70–93% |
| Alerts increased my awareness of hypnotic medication costs ( = 49) | 35 (71%) | 57–83% |
| Alerts changed my prescribing decision(s) ( = 49) | 11 (23%) | 12–37% |
| Alerts did not interfere with workflow ( = 50) | 35 (70%) | 55–82% |
* A total of 89 internal medicine clinicians received hypnotic prescribing alerts and were eligible to respond to questions regarding the new prescribing alerts. Fifty-one clinicians (57.3%) responded to some or all of the questions
DISCUSSION
In the setting of rising medication costs and influential marketing from the pharmaceutical industry, clinicians increasingly need real-time access to evidence-based information to support prescribing decisions. This study demonstrates that computerized decision support can limit the prescribing of heavily marketed medications in a community-based ambulatory care setting.
Prior studies have demonstrated that computerized prescribing alerts prevent medication errors, reduce the prescribing of inappropriate medications in the elderly, guide dosing in patients with renal insufficiency, limit hypnotic and anticholinergics in hospitalized elderly, and promote the use of formulary medications in the inpatient setting.10–16,23 The present study extends this work by demonstrating the effectiveness of computerized alerts to support prescribing decisions surrounding heavily marketed medications in the ambulatory setting. In a system where physicians are frequently unaware of patients’ out-of-pocket medication expenses24,25 and infrequently discuss costs with patients,26 the novel use of computerized alerts to prompt discussions regarding alternative treatment options offers a potential solution to limit unnecessarily expensive treatments.
Overall, the computerized alerts were well received by the clinicians surveyed. The majority reported that the alerts provided useful evidence to support prescribing decisions and relevant patient educational materials. Many clinicians also indicated that the alerts prompted them to spend more time discussing alternative treatments with patients. Following principles of effective decision support,27–29 the alerts were designed to limit disruptions in workflow by allowing the clinician to prescribe the original or alternative medications, quickly access references, and document the level of service and diagnosis codes for the visit. Furthermore, refills for medications were not subject to the alert, preventing clinicians from repeatedly receiving the same alert for the same patient. Selectively implementing streamlined computerized alerts with diverse functionality is essential to maximizing the alerts’ effectiveness and clinician acceptance.28–30
We did not find an additional effect of educational sessions and educational mailings beyond the effect of the alerts alone. The group educational sessions were focused on providing current prescribing information and facilitating discussions around the use of heavily marketed medications and less costly alternatives. While traditional academic detailing has been effective in improving health care quality in several settings, 31–34 its use in combination with computerized alerts has not demonstrated additive benefit in two prior studies.11,12,31Nevertheless, group educational sessions remain an enticing option to change physician behavior. While we did not detect an additive effect of a single group-based educational session, we are unable to determine if more intensive sessions–for example, multiple sessions over time, or individual (one-on-one) detailing – would have been more effective.
In the setting of escalating medication costs, the use of computerized alerts to support prescribing offers the potential for significant cost savings. In 2007, total sales of Lunesta® exceeded $600 million dollars35 while sales of Ambien CR® surpassed $751 million dollars.36 Substituting generic agents for even a small fraction of prescriptions for heavily marketed hypnotics would translate into considerable savings to the health care system.
This study has several limitations. First, this study evaluated a single class of medications. There are, however, numerous classes of medications with comparably effective generic equivalents that would be potentially amenable to similar interventions. Second, the alerts were not activated for physicians joining HVMA after the initiation of the study. This may have led to an underestimation of the effect of the alerts. Furthermore, encounters for medication refills were not subject to the alert, preventing clinicians from repeatedly receiving the same alert for the same patient, but further dampening the potential effect of the alerts. Third, the group educational sessions were limited to a single meeting and did not include urgent care providers, limiting the potential efficacy of this educational intervention. Fourth, our data collection was limited to one year after the activation of alerts. Although there was no apparent increasing trend in the number of heavily marketed hypnotics prescribed in the intervention groups during the one year intervention period, we are unable to determine if the effects of the alerts will diminish over time. Lastly, the generalizability of computerized prescribing alerts is limited to clinical settings with electronic prescribing linked to the capability of real-time clinical decision-support. Although a minority of practices have these capabilities at present,37 recent studies have shown encouraging trends of increasing adoption of electronic health records in ambulatory settings.38,39 Moreover, American Recovery and Reinvestment Act of 2009 includes more than $19 billion in financial incentives to speed EHR adoption in the coming years.
In summary, we found that computerized decision support is an effective tool to reduce the prescribing of heavily marketed medications in ambulatory care settings. The alerts held the prescribing of heavily marketed hypnotic medications at pre-intervention levels while the control group experienced an increase in the proportion prescribed. The addition of group educational sessions, however, yielded similar results to the alerts alone. In the setting of escalating medication costs, clinicians increasingly need tools to provide current prescribing information and facilitate discussions surrounding alternative treatment options. Computerized alerts offer an adaptable platform to support evidence-based prescribing and limit the external influences of pharmaceutical marketing.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOC 285 Kb)
Acknowledgements
This work was supported by a grant from the State Attorney General Consumer and Prescriber Education Grant Program, which is funded through the multi-state settlement from the unlawful marketing of the prescription drug Neurontin®. Dr. Fortuna was supported by an Institutional National Research Service Award, #5 T32 HP11001–18.
Conflict of Interest None disclosed.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-009-1013-x) contains supplementary material, which is available to authorized users.
References
- 1.Catlin A, Cowan C, Hartman M, Heffler S. National health spending in 2006: a year of change for prescription drugs. Health Aff (Millwood). 2008;27:14–29. [DOI] [PubMed]
- 2.Center for Medicare & Medicaid Services. National Health Expenditure Accounts 2006 Highlights. http://www.cms.hhs.gov/NationalHealthExpendData/downloads/highlights.pdf. 2006. Accessed April 21, 2009.
- 3.US Government Accountability Office. Prescription Drugs: Improvements Needed in FDA's Oversight of Direct-to-Consumer Advertising (GAO-07–54). 11–16–0008.
- 4.Kessler DA, Levy DA. Direct-to-consumer advertising: is it too late to manage the risks? Ann Fam Med. 2007;5:4–5. [DOI] [PMC free article] [PubMed]
- 5.Donohue JM, Cevasco M, Rosenthal MB. A decade of direct-to-consumer advertising of prescription drugs. N Engl J Med. 2007;357:673–81. [DOI] [PubMed]
- 6.Rosenthal MB, Berndt ER, Donohue JM, Frank RG, Epstein AM. Promotion of prescription drugs to consumers. N Engl J Med. 2002;346:498–505. [DOI] [PubMed]
- 7.Kravitz RL, Epstein RM, Feldman MD, Franz CE, Azari R, Wilkes MS, et al. Influence of patients’ requests for direct-to-consumer advertised antidepressants: a randomized controlled trial. JAMA. 2005;29:1995–2002. [DOI] [PMC free article] [PubMed]
- 8.Mintzes B, Barer ML, Kravitz RL, Bassett K, Lexchin J, Kazanjian A, et al. How does direct-to-consumer advertising (DTCA) affect prescribing? A survey in primary care environments with and without legal DTCA. CMAJ. 2003;169:405–12. [PMC free article] [PubMed]
- 9.Mintzes B, Barer ML, Kravitz RL, Kazanjian A, Bassett K, Lexchin J, et al. Influence of direct to consumer pharmaceutical advertising and patients’ requests on prescribing decisions: two site cross sectional survey. BMJ. 2002;324:278–9. [DOI] [PMC free article] [PubMed]
- 10.Chertow GM, Lee J, Kuperman GJ, Burdick E, Horsky J, Seger DL, et al. Guided medication dosing for inpatients with renal insufficiency. JAMA. 2001;286:2839–44. [DOI] [PubMed]
- 11.Feldstein AC, Smith DH, Perrin N, Yang X, Simon SR, Krall M, et al. Reducing warfarin medication interactions: an interrupted time series evaluation. Arch Intern Med. 2006;166:1009–115. [DOI] [PubMed]
- 12.Simon SR, Smith DH, Feldstein AC, Perrin N, Yang X, Zhou Y, et al. Computerized prescribing alerts and group academic detailing to reduce the use of potentially inappropriate medications in older people. J Am Geriatr Soc. 2006;54:963–8. [DOI] [PubMed]
- 13.Smith DH, Perrin N, Feldstein A, Yang X, Kuang D, Simon SR, et al. The impact of prescribing safety alerts for elderly persons in an electronic medical record: an interrupted time series evaluation. Arch Intern Med. 2006;166:1098–104. [DOI] [PubMed]
- 14.Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280:1311–6. [DOI] [PubMed]
- 15.Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma'Luf N, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999;6:313–21. [DOI] [PMC free article] [PubMed]
- 16.Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. Effects of computerized physician order entry on prescribing practices. Arch Intern Med. 2000;160:2741–7. [DOI] [PubMed]
- 17.The Department of Justice. Warner-Lambert to Pay $430 Million to Resolve Criminal & Civil Health Care Liability Relating to Off-Label Promotion. The Department of Justice. http://www.usdoj.gov/opa/pr/2004/May/04_civ_322.htm. Accessed April 21, 2009.
- 18.Oregon Health & Science University. Attorney General Consumer and Prescriber Grant Program. State Attorney Generals. http://www.ohsu.edu/cpgp. Accessed April 21, 2009.
- 19.Express Scripts. 2006 Drug Trend Report. http://www.express-scripts.com/industryresearch/industryreports/drugtrendreport/2006. Accessed April 21, 2009.
- 20.Atrius Health Pharmacy & Therapeutics Committee. Fact Sheet Hypnotics for Insomnia. 2–27–2008.
- 21.Soumerai SB, Avorn J. Principles of educational outreach (‘academic detailing’) to improve clinical decision making. JAMA. 1990;263:549–56. [DOI] [PubMed]
- 22.Robbins AS, Chao SY, Fonseca VP. What's the relative risk? A method to directly estimate risk ratios in cohort studies of common outcomes. Ann Epidemiol. 2002;12:452–4. [DOI] [PubMed]
- 23.Agostini JV, Zhang Y, Inouye SK. Use of a computer-based reminder to improve sedative-hypnotic prescribing in older hospitalized patients. J Am Geriatr Soc. 2007;55:43–8. [DOI] [PubMed]
- 24.Shrank WH, Joseph GJ, Choudhry NK, Young HN, Ettner SL, Glassman P, et al. Physicians’ perceptions of relevant prescription drug costs: do costs to the individual patient or to the population matter most. Am J Manag Care. 2006;12:545–54. [PubMed]
- 25.Reichert S, Simon T, Halm EA. Physicians’ attitudes about prescribing and knowledge of the costs of common medications. Arch Intern Med. 2000;160:2799–803. [DOI] [PubMed]
- 26.Tarn DM, Paterniti DA, Heritage J, Hays RD, Kravitz RL, Wenger NS. Physician communication about the cost and acquisition of newly prescribed medications. Am J Manag Care. 2006;12:657–64. [PubMed]
- 27.Bates DW, Kuperman GJ, Wang S, Shah NR, Seger AC, Seger DL, Fiskio JM, Kuperman GJ, Blumenfeld B, et al. Improving acceptance of computerized prescribing alerts in ambulatory care. J Am Med Inform Assoc. 2006;13:5–11. [DOI] [PMC free article] [PubMed]
- 28.Shah NR, Seger AC, Seger DL, Fiskio JM, Kuperman GJ, Blumenfeld B, et al. Improving acceptance of computerized prescribing alerts in ambulatory care. J Am Med Inform Assoc. 2006;13:5–11. [DOI] [PMC free article] [PubMed]
- 29.Feldstein A, Simon SR, Schneider J, Krall M, Laferriere D, Smith DH, et al. How to design computerized alerts to safe prescribing practices. Jt Comm J Qual Saf. 2004;30:602–13. [DOI] [PubMed]
- 30.Isaac T, Weissman JS, Davis RB, Massagli M, Cyrulik A, Sands DZ, et al. Overrides of medication alerts in ambulatory care. Arch Intern Med. 2009;169:305–11. [DOI] [PubMed]
- 31.Lu CY, Ross-Degnan D, Soumerai SB, Pearson SA. Interventions designed to improve the quality and efficiency of medication use in managed care: a critical review of the literature - 2001–2007. BMC Health Serv Res. 2008;8:75. [DOI] [PMC free article] [PubMed]
- 32.O'Brien MA, Rogers S, Jamtvedt G, Oxman AD, Odgaard-Jensen J, Kristoffersen DT, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2007;CD000409. [DOI] [PMC free article] [PubMed]
- 33.Simon SR, Majumdar SR, Prosser LA, Salem-Schatz S, Warner C, Kleinman K, et al. Group versus individual academic detailing to improve the use of antihypertensive medications in primary care: a cluster-randomized controlled trial. Am J Med. 2005;118:521–8. [DOI] [PubMed]
- 34.Fosnight SM, Holder CM, Allen KR, Hazelett S. A strategy to decrease the use of risky drugs in the elderly. Cleve.Clin J Med. 2004;71:561–8. [DOI] [PubMed]
- 35.Peter Loftus. PHARMA MARKET: Glow Of Sepracor Sleep Drug Gets Dimmer. Dow Jones Newswires. http://www.istockanalyst.com/article/viewiStockNews/articleid/2342109. Accessed April 21, 2009.
- 36.Sanofi-Aventis. United States Securities and Exchange Commission Form 20-F. United States Securities and Exchange Commission, 83. http://en.sanofi-aventis.com/binaries/20-F_2007_EN_tcm28–1519.pdf. Accessed April 21, 2009.s
- 37.DesRoches CM, Campbell EG, Rao SR, Donelan K, Ferris TG, Jha A, et al. Electronic health records in ambulatory care–a national survey of physicians. N.Engl.J Med. 2008;359:50–60. [DOI] [PubMed]
- 38.Simon SR, Kaushal R, Cleary PD, Jenter CA, Volk LA, Orav EJ, et al. Physicians and electronic health records: a statewide survey. Arch Intern Med. 2007;167:507–12. [DOI] [PubMed]
- 39.Simon SR, Soran CS, Kaushal R, Jenter CA, Volk LA, Burdick E, Cleary PD, Orav EJ, Poon EG, and Bates DW. Physicians’ Usage of Key Functions in Electronic Health Records from 2005 to 2007: A Statewide Survey. J Am Med Inform Assoc 2009; In press. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.
(DOC 285 Kb)