ABSTRACT
BACKGROUND
A difficult to manage comorbid condition, like chronic pain, could adversely affect the delivery of recommended care for other serious health problems, such as hypertension.
OBJECTIVE
We examined whether addressing pain at a primary care visit acts as a competing demand in decisions to intensify blood pressure (BP) medications for diabetic patients with an elevated BP.
DESIGN
Prospective cohort study. Participants: 1,169 diabetic patients with a BP ≥140/90 prior to a primary care provider (PCP) visit were enrolled.
MEASUREMENTS
After the visit, PCPs provided information about the top three issues discussed and whether hypertension medications were intensified or reasons for not intensifying. We used multi-level logistic regression to assess whether discussing pain during the visit decreased the likelihood of BP medication intensification. We calculated predicted probabilities of medication intensification by whether pain was discussed.
RESULTS
PCPs discussed pain during 222 (20%) of the visits. Visit BP did not differ between patients with whom pain was and was not discussed. BP medications were intensified during 44% of the visits. The predicted probability of BP medication intensification when pain was discussed was significantly lower than when pain was not discussed (35% vs. 46%, p = 0.02).
CONCLUSIONS
Discussing pain at a primary care visit competed with the intensification of BP medication. This finding is concerning given that controlling blood pressure may be the most important factor in decreasing long-term complications for patients with diabetes. Better care management models for complex patients are needed to ensure that both pain and other chronic conditions are adequately addressed.
KEY WORDS: chronic pain, comorbidity, hypertension management
INTRODUCTION
Increasingly, health-care providers and systems are faced with the challenging task of providing care for patients with multiple chronic health conditions. In fact, over 50% of older adults have two or more chronic health conditions.1 How comorbidity affects the management of common chronic conditions, such as diabetes or hypertension, however, is not well understood.2
To date, research in this area has produced conflicting results. Some studies suggest that care quality may improve as the number of conditions increases,3 or at least remain comparable for patients with and without another significant comorbid condition.4 In contrast, other studies show that having more conditions, particularly unrelated conditions, is associated with poorer quality.5–9 Research also suggests that the types of conditions (e.g., related vs. unrelated) and the saliency or severity of a condition at a particular point in time are likely to be important factors in understanding both the potential consequences and management challenges of patients with multiple chronic conditions.2,5,6,9–11
Chronic pain is a prevalent comorbid condition among patients with other significant chronic illnesses, including those with diabetes or chronic heart failure.12 Chronic pain has many serious psychosocial consequences, is often difficult to manage and has also been shown to interfere with patients’ self-management of their other conditions.12–18 Given the prominence of pain as a symptom and the challenges associated with its management, dealing with chronic pain at an encounter could directly compete with the delivery of other recommended care for serious medical problems. Therefore, in this study we examined whether discussing pain during a primary care visit acts as a competing demand in decisions to intensify blood pressure (BP) medications for diabetes patients presenting with an elevated blood pressure.
METHODS
This research is part of a larger project, the Addressing Barriers to Treatment for Hypertension (ABATe) study, which was designed to better understand factors, such as competing demands, underlying apparent clinical inertia for hypertension.6 Specifically, ABATe examined treatment decisions for primary care patients with diabetes and an elevated blood pressure. The ABATe conceptual model focused on four domains hypothesized to affect treatment decisions at a visit: (1) clinical uncertainty, (2) competing demands and prioritization, (3) medication-related factors, and (4) care organization. Additional details about the conceptual model and study methods are described elsewhere.6
Study Design and Setting
ABATe was a prospective cohort study of patients with scheduled primary care visits at nine Department of Veterans Affairs (VA) facilities located in three midwestern states. These facilities included three large academic-affiliated medical centers, one large non-academic medical center, and one large and four small community-based outpatient clinics. IRB approval for the study was obtained at all participating facilities, and written, informed consent was obtained from both patients and providers prior to their participation.
All non-resident primary care providers with patient care responsibilities at least 2 half-days per week were invited to participate. Of the 126 eligible providers approached, 104 consented to participate, for an overall recruitment rate of 83%. However, 12 providers stopped working at their facility or changed their patient care responsibilities by the time recruitment started, resulting in 92 participating primary care providers.
During study enrollment, over 33,000 patients with diabetes visited primary care providers (including residents) at the study facilities. Potentially eligible patients were referred to study staff by triage personnel. Study staff then screened all referred patients who presented for a scheduled visit to a participating primary care provider and whose lowest triage systolic blood pressure was ≥140 mmHg or whose lowest triage diastolic blood pressure was ≥90 mmHg. In each facility, the triage blood pressures were routinely obtained using an electronic cuff.
In addition to triage blood pressure, patients were screened using the following inclusion criteria: the subject confirmed a diagnosis of diabetes, the participating provider was the primary provider of diabetes care for the subject and the subject was an English-speaker. Patients with impaired decision-making ability (e.g., dementia, traumatic brain injury), terminal disease and residents of nursing homes were excluded. Of the 1,556 patients approached by study staff, 213 were not eligible, and 1,169 provided written informed consent to participate in the study (87% of those approached and eligible). The pre-specified sample size for the study main analysis was 880, although slightly more were enrolled to ensure there were enough patients per participating provider to assess provider level effects.
Data Sources
Data were obtained from five sources: (1) a baseline provider survey, (2) a brief post-visit survey completed by providers for each patient after the clinic visit (completion rate 99%), (3) a patient enrollment survey (completion rate 91%), (4) a review of patients’ electronic medical records and (5) the Veterans Health Administration automated data sources.
Variables
Dependent Variable: Blood Pressure Medication Intensification
The main dependent variable for this analysis was whether or not the blood pressure medication was intensified by the primary care provider at the visit in response to the elevated triage blood pressure, defined as a blood pressure of 140/90 mmHg or greater, immediately prior to the primary care visit. The VA/DoD hypertension guideline (revised in 2005) recommends a target value of <140/80 mmHg for patients with diabetes. Intensification was considered to have occurred if the provider indicated on the post-visit survey (or in the medical record if a post-visit survey was not completed) that s/he added a blood pressure medication or increased the dose of an existing medication.
Independent Variable: Pain Discussed
Given our focus on the extent to which pain may serve as a competing demand, the primary independent variable was whether or not pain was discussed during the visit. As part of the post-visit survey, providers were asked to list the three areas on which they spent the most time during the visit. Examples were provided as part of the question (e.g., back pain, depression, glycemic control, preventive care), but the responses were elicited as free-text and not by providing a fixed set of items from which the provider could choose. We considered any discussion of a pain condition, except for chest pain, among the top three issues as evidence of pain discussed. Chest pain, which was mentioned in only one encounter, was considered an acute problem necessitating a different type of workup, and our main interest was the effect of chronic pain.
Covariates
While pain discussed was our primary variable of interest, we also included other variables in our analysis that might be expected to influence the medication intensification decision. Specifically, we included visit systolic and diastolic blood pressures and mean systolic blood pressure in the prior year (calculated as the mean of all prior year systolic blood pressures stored in the automated data) as continuous variables. We also took into account whether the provider reported discussing other non-pain comorbid conditions during the visit. Two variables were constructed by classifying these conditions as either related (concordant) or unrelated (discordant) with diabetes and hypertension.2 Concordant conditions included hyperlipidemia, obesity, heart failure, ischemic heart disease, peripheral vascular disease, renal disease and cerebrovascular disease. All other conditions, such as cancer or mental health conditions (with pain excluded), were considered discordant. Other potentially important factors included the average number of minutes the provider had available for a follow-up visit, which was ascertained from the provider baseline survey, and, based on automated data, the number of classes of blood pressure medications the patients was already on at the enrollment visit. Finally, we also adjusted for patient age, race (as identified by the patient) and gender.
Statistical Analysis
We examined the association between blood pressure medication intensification and whether pain was discussed using a three-level logistic regression model, with the first level consisting of patient-specific variables, the second level the primary care provider and the third level the site where the provider practiced. Multi-level models allow one to appropriately account for the clustering of patients within providers and sites. For clarity of presentation, we present the estimated model parameters as odds ratios. However, based on the model parameters, we also calculated the probability of intensification when pain was discussed and when it was not, for a hypothetical patient, with all covariates set at the mean level and the random effect set to zero, representing a visit with a physician whose intensification rate was at the modal or most common level for the population of physicians.
The missing data rates were quite low for variables not collected by survey ranging from 0–1.6%. The total number of patients with any missing data was only 64 out of 1,169. Thirty-three observations were eliminated from the analysis due to missing information for our primary independent variable, and our final multivariate results were derived with a sample of 1,105. Those excluded from the multivariate analysis had higher visit diastolic blood pressures and were on fewer classes of blood pressure medications than those in the final sample, but were similar with respect to age, race and gender. The results presented in the text are from the final multivariate model with the predicted probability expressed as a percent. All analyses were conducted using Stata 10.0. (StataCorp 2007, Stata Statistical Software: Release 10. College Station, TX; StataCorp LP.)
To further our understanding of the potential impact of pain on the medication intensification decision, we used data from the post-visit survey and medical record review to: (1) examine the reasons given for not intensifying blood pressure medications and (2) ascertain whether for those not intensified at the visit if there was evidence of subsequent intensification or a follow-up visit during the next 4 weeks. We hypothesized that if pain did interfere during a given encounter, then providers might schedule another visit soon after to address outstanding issues.
RESULTS
Pain was one of the top three issues primary care providers discussed with their patients at 20% (222/1,136) of the visits (Table 1). Patients with whom pain was discussed were slightly younger than those with whom pain was not discussed (64 years vs. 66 years), but there were no significant differences in blood pressure levels between groups. There were also no differences in gender, race or number of current blood pressure medications between those with whom pain was or was not discussed at the visit. However, among patients with whom pain was not discussed at the visit, providers were more likely to discuss at least one condition concordant with diabetes and hypertension (54%) or at least one non-pain discordant condition (45%) compared to those with whom pain was discussed (21% and 28% respectively, p < 0.001).
Table 1.
Patient Characteristics among Those with and without Pain Discussed During the Visit
| Pain discussed at visit | |||
|---|---|---|---|
| No (n = 914) | Yes (n = 222) | P value | |
| Age, mean, (SD), years | 66.3 (10.8) | 63.7 (10.4) | 0.001 |
| Female, no. (%) | 27 (3) | 11 (5) | 0.14 |
| Black, no. (%) | 184 (20) | 48 (22) | 0.65 |
| Visit systolic BP, mean (SD), mmHg | 154.0 (13.8) | 152.2 (12.7) | 0.09 |
| Visit diastolic BP, mean (SD), mmHg | 78.0 (12.1) | 77.9 (11.7) | 0.89 |
| Prior year systolic BP, mean (SD), mmHg | 145.2 (15.5) | 143.2 (13.8) | 0.07 |
| Number of blood pressure medication classes, mean (SD) | 2.1 (1.3) | 2.1 (1.4) | 0.98 |
| PCP average minutes for follow-up visit 30 or more min, no. (%) | 545 (60) | 134 (60) | 0.84 |
| At least one concordant condition * discussed, no. (%) | 493 (54) | 47 (21) | <0.001 |
| At least one non-pain discordant condition † discussed, no. (%) | 415 (45) | 62 (28) | <0.001 |
*Conditions concordant with diabetes and hypertension, such as hyperlipidemia, obesity, heart failure, ischemic heart disease, peripheral vascular disease, renal disease and cerebrovascular disease
†Conditions not concordant with diabetes and hypertension, such as cancer or mental health conditions (with pain conditions excluded)
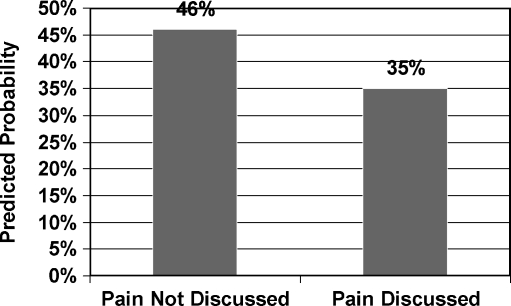
Primary care providers intensified hypertension medications during 44% (497/1,136) of visits overall. Blood pressure medication intensification was significantly less likely, however, during visits at which pain was discussed (p = 0.02) (Table 2). After adjusting for other important factors, including blood pressure levels, the predicted probability of intensifying blood pressure medication was 35% when pain was discussed compared to 46% when pain was not discussed (Fig. 1). As expected, the odds of blood pressure medication intensification were also significantly associated with higher blood pressure levels; however, there were no observed associations between intensification and whether other conditions (either concordant or non-pain discordant) were discussed during the visit.
Table 2.
Multi-level Regression Results: Adjusted Odds Ratio of Blood Pressure Medication Intensification at Visit
| AOR* | 95% Confidence interval | |
|---|---|---|
| Pain discussed at visit | 0.63 | 0.44–0.92 |
| Visit systolic BP (10 mmHg) | 1.25 | 1.11–1.40 |
| Visit diastolic BP (10 mmHg) | 1.14 | 1.00–1.29 |
| Mean prior year systolic BP (10 mmHg) | 1.27 | 1.15–1.41 |
| At least one concordant condition discussed at visit | 1.04 | 0.75–1.44 |
| At least one non-pain discordant condition discussed at visit | 0.82 | 0.60–1.13 |
| Black race | 0.86 | 0.60–1.22 |
| Age 56–75 (vs. <56) | 0.82 | 0.55–1.22 |
| Age 76+ (vs. <56) | 0.80 | 0.49–1.30 |
| At least 30 min for follow-up visit | 1.26 | 0.86–1.87 |
| Female gender | 1.22 | 0.52–2.84 |
| Number of BP medication classes | 0.99 | 0.89–1.10 |
*Includes adjustment for covariates as well as clustering of observations by provider (n = 92) and by site (n = 9)
Figure 1.
Predicted probability of blood pressure medication intensification for those with whom pain was and was not discussed derived from the logistic regression model shown in Table 2 with values for all other variables in the model set to the sample mean.
When asked in the post-visit survey why they did not change hypertension treatment, the most common reason given by a provider (regardless of whether pain was or was not discussed) was that the patient’s blood pressure was in good control or close enough to good control (42% pain discussed vs. 37% pain not discussed, p = 0.24). This assessment often occurred after the provider had rechecked the blood pressure. Other frequently cited reasons were that the blood pressure was “usually in good control, even though today it is high” and that the patient did not take their medications before the visit. However, of all the reasons noted the only one that differed significantly between those with whom pain was and was not discussed was the patient reported having lower blood pressure readings at home (11% when pain was discussed vs. 20% when pain was not discussed, p = 0.01) (Table 3). At only 5 of the 222 visits in which pain was discussed did the primary care provider explicitly indicate that they did not intensify blood pressure medications because they suspected that pain was causing the blood pressure elevation. Removing these observations from the analysis did not significantly change the model results.
Table 3.
Reasons for not Intensifying Hypertension Medication in Response to Elevated Visit Blood Pressure
| Pain discussed at visit | |||
|---|---|---|---|
| No (n = 492) | Yes (n = 142) | P value | |
| BP is in good control or is close enough to being in good control today, no. (%) | 181 (36.5) | 60 (42.0) | 0.24 |
| BP is usually in good control, even though today it is high, no. (%) | 86 (17.3) | 28 (19.6) | 0.54 |
| Patient reports having lower blood pressure readings at home, no. (%) | 98 (19.8) | 15 (10.5) | 0.01 |
| Patient did not take medications before visit today, no. (%) | 109 (22.0) | 21 (14.7) | 0.06 |
| Patient was not willing to change or add medications, no. (%) | 30 (6.1) | 8 (5.6) | 0.84 |
| Patient’s compliance with current regimen can be improved, no. (%) | 79 (15.9) | 20 (14.0) | 0.57 |
| Intensifying treatment would have created side effects, no. (%) | 17 (3.4) | 6 (4.2) | 0.66 |
| There were other more pressing issues to address today, no. (%) | 49 (9.9) | 16 (11.2) | 0.65 |
| Other *no. (%) | 82 (16.5) | 25 (17.5) | 0.79 |
BP = blood pressure
*Other includes recent medication change, repeat or recheck within 1 month, patient has a doctor outside the VA, referred to BP class or gave BP home monitor
We found that among the 639 patients who did not have their medications intensified at the index visit, 72 (11%) had medications intensified and/or a follow-up visit within 4 weeks of the initial visit. However, we did not find any evidence that those with whom pain was discussed were more likely to have their medications intensified or a close follow-up visit. Specifically, 17 of the 143 patients (12%) with whom pain was discussed at the initial visit had intensification or a follow-up visit compared to 55 of the 496 patients (11%) with whom pain was not discussed (p = 0.79).
DISCUSSION
Discussing pain during a primary care visit reduced the odds of medication intensification by 40% for a diabetes patient who presented with an elevated triage blood pressure. This finding suggests that having to address chronic pain does indeed serve as a competing demand in providing recommended care during a clinical encounter for patients with diabetes. The fact that discussing pain specifically influenced treatment decisions related to blood pressure management is of particular concern when considering that controlling blood pressure may be the most important factor in reducing microvascular and macrovascular complications for patients with diabetes.19
These results are consistent with other research, which found that the number of patient concerns discussed during a primary care encounter decreased the likelihood of a diabetes medication change7 and that having more unrelated comorbid conditions was negatively associated with antihypertensive treatment intensification.5 However, our study also demonstrates that chronic pain, which tends to be prominently symptomatic and difficult to manage, may be especially problematic since we found no association between medication intensification and the discussion of either concordant or other, non-pain, discordant conditions.
While our results show that pain disrupted the decision to intensify hypertension medication at a given visit, this could reflect appropriate prioritization by the clinician. However, we also found that among patients whose hypertension medication was not intensified, those with whom pain was discussed were no more likely to have a follow-up visit or intensification soon after the visit. Additional longitudinal analyses are needed to fully investigate the potential long-term implications of pain as a competing demand. But, if this pattern persists, it suggests that pain could lead to a net reduction in attention paid to key conditions, such as hypertension, over time. These findings also indicate that patients with pain may be a specific subgroup of complex patients that would be a good target for care management or other types of enhanced care programs to ensure that they receive all needed pain and non-pain-related services.
One possible reason for not intensifying hypertension medications is the belief that pain is causing the higher blood pressure. However, in only five instances did providers explicitly indicate they did not intensify medications because they believed that pain was causing the elevated reading. Furthermore, while some acute pain situations may elevate blood pressure, there is little empirical evidence to support an association between chronic pain and a transient increase in blood pressure. In fact, studies of patients in the emergency department (ED) have found that those that present with an abnormal blood pressure often continue to have abnormal blood pressure readings without any apparent relationship to pain.20,21 On the other hand, there is some evidence that the functional interaction between the cardiovascular and pain regulatory systems may be altered in chronic pain sufferers,22 and at least one study that suggests that chronic pain may be associated with an increased risk of hypertension.23
To our knowledge this is the first large multi-site study to investigate whether discussing pain at a primary care visit acts as a competing demand in decisions to intensify blood pressure medications for patients with diabetes and an elevated blood pressure reading. One limitation of this study is that the sample is predominately male. While we know of no prior literature that would suggest an interaction between gender and pain management with regard to the effect on blood pressure treatment, it is not known whether similar results would be found in settings with a higher proportion of female patients. A second limitation of this study is that we are not able to fully characterize the nature of the pain discussed during the visits. Among patients with whom pain was discussed, 73% either reported on an independent baseline survey that they had chronic/persistent pain or, according to automated VA data, had a fill for an opiod medication in the past 3 months (39%). In addition, the specific pain conditions discussed, as noted on the post-visit survey, appear to be mostly chronic in nature, such as back pain (n = 62) and arthritis, joint pain (most commonly shoulder, hip, knee, leg and foot) or degenerative joint disease (n = 102). In several cases these conditions were qualified with the word chronic. Among the other conditions listed were headaches or migraines, abdominal pain, “chronic pain,” carpal tunnel syndrome and “pain issues.” Nonetheless, for some patients with whom pain was discussed, the conversation during the visit may have been related to another acute pain-related problem or an acute exacerbation of their chronic pain condition.
In conclusion, discussing pain at a primary care visit was a competing demand in the decision to intensify antihypertensive medications for diabetes patients with an elevated blood pressure. This finding is of concern considering the role that blood pressure control plays in reducing long-term complications for patients with diabetes. Additional research is required to fully understand how chronic pain affects care over the long term. Nevertheless, given the prevalence of chronic pain and the importance of controlling clinical factors that increase patient risk for poor outcomes, we need to develop care models to ensure that both pain and other chronic conditions are adequately addressed.
Acknowledgement
This study was supported through grants IIR 02–225 and DIB 98–001 from the Department of Veterans Affairs (VA), Health Services Research and Development Service. John Piette is a VA Career Scientist. This work was also supported in part by the Michigan Diabetes Research and Training Center grant P60DK-20572 from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the University of Michigan or the NIH. The authors are indebted to our recruitment coordinator and research assistants who worked tirelessly to recruit patients for this study; to our data manager; to our site principal investigators, without whom this study could not have taken place; and to the many providers and patients who participated in the study. The authors would also like to thank Dr. Connie Standiford for her comments on earlier drafts of this manuscript.
Conflict of Interest None disclosed.
References
- 1.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162(20):2269–76. [DOI] [PubMed]
- 2.Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29(3):725–31. [DOI] [PubMed]
- 3.Higashi T, Wenger NS, Adams JL, et al. Relationship between number of medical conditions and quality of care. N Engl J Med. 14 2007; 356(24):2496–504. [DOI] [PubMed]
- 4.Krein SL, Bingham CR, McCarthy JF, Mitchinson A, Payes J, Valenstein M. Diabetes treatment among VA patients with comorbid serious mental illness. Psychiatr Serv. 2006;57(7):1016–21. [DOI] [PubMed]
- 5.Turner BJ, Hollenbeak CS, Weiner M, Ten Have T, Tang SS. Effect of unrelated comorbid conditions on hypertension management. Ann Intern Med. 2008;148(8):578–86. [DOI] [PubMed]
- 6.Kerr EA, Zikmund-Fisher BJ, Klamerus ML, Subramanian U, Hogan MM, Hofer TP. The role of clinical uncertainty in treatment decisions for diabetic patients with uncontrolled blood pressure. Ann Intern Med. 2008;148(10):717–27. [DOI] [PubMed]
- 7.Parchman ML, Pugh JA, Romero RL, Bowers KW. Competing demands or clinical inertia: the case of elevated glycosylated hemoglobin. Ann Fam Med. 2007;5(3):196–201. [DOI] [PMC free article] [PubMed]
- 8.Frayne SM, Halanych JH, Miller DR, et al. Disparities in diabetes care: impact of mental illness. Arch Intern Med. 2005;165(22):2631–8. [DOI] [PubMed]
- 9.Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases. N Engl J Med. 1998;338(21):1516–20. [DOI] [PubMed]
- 10.Parchman ML, Romero RL, Pugh JA. Encounters by patients with type 2 diabetes–complex and demanding: an observational study. Ann Fam Med. 2006;4(1):40–5. [DOI] [PMC free article] [PubMed]
- 11.Kerr EA, Heisler M, Krein SL, et al. Beyond comorbidity counts: how do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? J Gen Intern Med. 2007;22(12):1635–40. [DOI] [PMC free article] [PubMed]
- 12.Krein SL, Heisler M, Piette JD, Butchart A, Kerr EA. Overcoming the influence of chronic pain on older patients’ difficulty with recommended self-management activities. Gerontologist. 2007;47(1):61–8. [DOI] [PubMed]
- 13.Brooks PM. The burden of musculoskeletal disease–a global perspective. Clin Rheumatol. 2006;25(6):778–81. [DOI] [PubMed]
- 14.Smith BH, Elliott AM, Chambers WA, Smith WC, Hannaford PC, Penny K. The impact of chronic pain in the community. Fam Pract. 2001;18(3):292–9. [DOI] [PubMed]
- 15.Crosby FE, Colestro J, Ventura MR, Graham K. Survey of pain among veterans in Western New York. Pain Manag Nurs. 2006;7(1):12–22. [DOI] [PubMed]
- 16.Mitchinson AR, Kerr EA, Krein SL. Management of chronic noncancer pain by VA primary care providers: when is pain control a priority? Am J Manag Care. 2008;14(2):77–84. [PubMed]
- 17.Green CR, Wheeler JR, Marchant B, LaPorte F, Guerrero E. Analysis of the physician variable in pain management. Pain Med. 2001;2(4):317–27. [DOI] [PubMed]
- 18.Krein SL, Heisler M, Piette JD, Makki F, Kerr EA. The effect of chronic pain on diabetes patients’ self-management. Diabetes Care. 2005;28(1):65–70. [DOI] [PubMed]
- 19.Vijan S, Hayward RA. Treatment of hypertension in type 2 diabetes mellitus: blood pressure goals, choice of agents, and setting priorities in diabetes care. Ann Intern Med. 2003;138(7):593–602. [DOI] [PubMed]
- 20.Tanabe P, Persell SD, Adams JG, McCormick JC, Martinovich Z, Baker DW. Increased blood pressure in the emergency department: pain, anxiety, or undiagnosed hypertension? Ann Emerg Med. 2008;51(3):221–9. [DOI] [PubMed]
- 21.Backer HD, Decker L, Ackerson L. Reproducibility of increased blood pressure during an emergency department or urgent care visit. Ann Emerg Med. 2003;41(4):507–12. [DOI] [PubMed]
- 22.Bruehl S, Chung OY. Interactions between the cardiovascular and pain regulatory systems: an updated review of mechanisms and possible alterations in chronic pain. Neurosci Biobehav Rev. 2004;28(4):395–414. [DOI] [PubMed]
- 23.Bruehl S, Chung OY, Jirjis JN, Biridepalli S. Prevalence of clinical hypertension in patients with chronic pain compared to nonpain general medical patients. Clin J Pain. 2005;21(2):147–53. [DOI] [PubMed]