Abstract
In spite of the serious and costly problems presented by juvenile sexual offenders, rigorous tests of promising interventions have rarely been conducted. This study presents a community-based effectiveness trial comparing multisystemic therapy (MST) adapted for juvenile sexual offenders with services that are typical of those provided to juvenile sexual offenders in the U.S. Youth were randomized to MST (n = 67) or treatment as usual for juvenile sexual offenders (TAU-JSO; n = 60). Outcomes through 12 months post recruitment were assessed for problem sexual behavior, delinquency, substance use, mental health functioning, and out-of-home placements. Relative to youth who received TAU-JSO, youth in the MST condition evidenced significant reductions in sexual behavior problems, delinquency, substance use, externalizing symptoms, and out-of-home placements. The findings suggest that family- and community-based interventions, especially those with an established evidence-base in treating adolescent antisocial behavior, hold considerable promise in meeting the clinical needs of juvenile sexual offenders.
Keywords: juvenile sexual offender, multisystemic therapy, cognitive-behavior therapy, randomized clinical trial, effectiveness research
Policy discussions regarding the legal and treatment dispositions of adolescents arrested for sexual offenses have been contentious, with some policy makers and treatment professionals arguing for lifelong placement on sexual offender registries and extended residential treatment (e.g., J. Ring, quoted in Michels, 8/16/2007), and others emphasizing the generally low recidivism rates of such youth and their need for strength-focused, community-based services (e.g., Chaffin, 2008). Regardless of these different perspectives, however, virtually all stakeholders agree that the scope of sexual offending by juveniles is substantial and warrants the development of effective interventions.
Regarding the scope and consequences of adolescent sexual offending, official records indicate that minors account for about 20% of all serious sexual crimes (Pastore & Maguire, 2007), and victim reports indicate that the proportion of juvenile (vs. adult) offenders increases as the age of victims decreases (Snyder & Sickmund, 2006). Importantly, sexual assault victims are at relatively high risk for numerous negative sequelae (see Chapman, Dube, & Anda, 2007; Letourneau, Resnick, Kilpatrick, Saunders, & Best, 1996), and estimates of the annual U.S. cost for sexual assault place the sum in the billions of dollars (e.g., Post, Mezey, Maxwell, & Wibert, 2002). Moreover, though engendering little public sympathy, significant social and fiscal costs also are borne by juvenile sexual offenders. Many are removed from their families for years and are required to register publicly for life, processes that likely limit the development of their social, academic, and vocational competencies (Chaffin, 2008; Letourneau & Miner, 2005). In consideration of these circumstances, the validation of effective interventions could reduce the significant social and fiscal costs to victims, offenders, and society by reducing future sexual victimizations and increasing the likelihood that juvenile sexual offenders become law-abiding and productive citizens.
In developing effective treatments for juvenile sexual offenders, it seems reasonable to draw on the knowledge base regarding the risk factors for sexual offending by adolescents as well as the literature on the types of interventions that have been effective in treating other types of serious antisocial behavior in adolescents such as criminal activity and substance abuse. Interestingly, research shows that the risk factors for adolescent sexual offending are very similar to those observed for these other types of serious antisocial behavior. For example, in a longitudinal study examining 66 correlates of juvenile sexual and violent offending, van Wijk et al. (2005) found that violent sexual offenders were similar to violent nonsexual offenders with respect to nearly all family (e.g., poor supervision and communication) and peer (e.g., involvement with delinquent and substance-abusing peers) risk factors. Similarly, Ronis and Borduin (2007) found that juvenile sexual offenders, like other serious juvenile offenders, had lower bonding to family and school and higher involvement with deviant peers than did nondelinquent youth.
Regarding interventions that have been identified as effective in treating other types of antisocial behavior in adolescents, the Surgeon General’s report on youth violence (U.S. Public Health Service, 2001) identified three treatments for juvenile criminal behavior with established effectiveness (i.e., functional family therapy, multidimensional treatment foster care, multisystemic therapy). Significantly, these interventions share a family-based focus as well as the capacity to address a comprehensive array of risk factors in the youth and family’s natural environment. Likewise, based on Waldron and Turner’s (2008) recent review of the adolescent substance abuse treatment literature, several relatively comprehensive family-based interventions (e.g., brief strategic family therapy, functional family therapy, multidimensional family therapy, multisystemic therapy) have shown considerable promise or success in attenuating this type of antisocial behavior. Together, these findings suggest that a family-based approach with the capacity to address a comprehensive array of risk factors might provide an effective treatment for adolescent sexual offenders. Indeed, the small efficacy research literature on juvenile sexual offenders supports this possibility.
Recent reviews of the juvenile sexual offender outcome literature (Hanson et al., 2002; Reitzel & Carbonell, 2006) have noted that two efficacy trials of multisystemic therapy (MST; Henggeler, Schoenwald, Borduin, Rowland, & Cunningham, 1998) are the only randomized trials conducted in this area of research; both produced promising results. As suggested previously, the comprehensive nature and family- and community-based emphases of MST are consistent with the types of interventions that have been successful in treating other types of antisocial behavior in adolescents. In the first small efficacy trial with juvenile sexual offenders (n = 16), Borduin and colleagues (Borduin, Henggeler, Blaske, & Stein, 1990) reported that significantly fewer youth in the MST condition (12.5%) than in the outpatient “usual services” condition (75%) were rearrested for sexual crimes over a 3-year follow-up. A second, larger efficacy study (Borduin, Schaeffer, & Heiblum, in press) included 48 juvenile sexual offenders randomized to MST or usual services (a combination of cognitive-behavioral group and individual treatment administered in a juvenile court setting) conditions. At 8.9 years post-treatment, MST participants were significantly less likely than their usual services counterparts to be rearrested for sexual (8% vs. 46%) and nonsexual (29% vs. 58%) offenses. Thus, the results from these two relatively small-scale efficacy studies support the potential of MST as an effective community-based treatment for juvenile sexual offenders.
The purpose of the present study was to provide a rigorous effectiveness trial of MST with juvenile sexual offenders that included a comparison condition that is generally typical of the community based services provided to such offenders in the U.S. Although a precise definition of an effectiveness does not exist, as the efficacy-effectiveness distinction can vary on many dimensions (e.g., characteristics of the intervention, practitioners, clients, service delivery, provider organization and service sytem; Schoenwald & Hoagwood, 2001), the general distinction between efficacy and effectiveness trials is important for the emerging field of implementation science (Fixsen, Naoom, Blase, Friedman, & Wallace; 2005). Weisz and his colleagues (e.g., Weisz, Donenberg, Han, & Weiss, 1995) have shown that the average effect size in child mental health efficacy studies (i.e., often university based, using graduate students as therapists) is considerably greater than the average effect size of effectiveness trials conducted in community practice settings using real world practitioners. A recent meta-analysis of MST randomized trials (Curtis, Ronan, & Borduin, 2004) drew a similar conclusion, with MST efficacy trials having larger effect sizes than MST effectiveness trials. Pertaining to MST with juvenile sexual offenders, the two aforementioned trials conducted by Borduin and his colleagues were primarily efficacy studies. Although participants had a wide variety of co-occurring problems, the therapists were clinical psychology doctoral students, and the principle investigator provided the clinical training and supervision. In contrast, in the present study, community-based MST services were provided by an existing private provider agency. Thus, the present study represents an important step in bridging the gap between science and practice (National Institute of Mental Health, 1999) for this clinical population.
In conducting this effectiveness trial, a primary goal was to include a comparison intervention that represented the types of services typically provided for juvenile sexual offenders. Treatment as usual for juvenile sexual offenders (TAU-JSO) includes interventions that have a cognitive-behavioral orientation, focus on individual (youth-level) behavioral drivers, and are delivered in weekly group treatment sessions for a year or longer (Letourneau, 2004; Letourneau & Borduin, 2008; McGrath, Cumming, & Burchard; 2003; Walker, McGovern, Poey, & Otis, 2004). The individual treatment focus and the group-oriented delivery of TAU-JSO contrast well with the family-based and ecological emphases of MST.
In sum, within the context of community-based treatment programs, the relative effectiveness of a promising family-based approach (i.e., MST) was contrasted with a set of interventions that generally reflect treatment as usual for juvenile sexual offenders. As described subsequently, 1-year post-recruitment outcomes were examined for deviant sexual interest/risk behaviors, delinquency, substance use, mental health symptoms, and out-of-home placements.
Method
Design and Procedures
A 2 (treatment type: MST versus TAU-JSO) × 3 (time: pretreatment, 6 months, 12 months) factorial design with random assignment of youth to treatment conditions was used. Research assessments were conducted with each youth and his or her caregiver at three points in time: within 72 hours of recruitment into the study (pretreatment; T1), 6 months post recruitment (T2), and 12 months post recruitment (T3). Research assistants administered the assessment battery at a time and place that was convenient to families, which was almost always in their homes. During the assessment interview, caregivers and youth jointly completed a comprehensive survey of demographic characteristics and then completed individual assessment protocols separately. Additionally, research assistants contacted caregivers once per month to obtain information on possible youth out-of-home placement. During this monthly contact, caregivers in the MST condition also completed a treatment adherence measure. Although research and clinical staff were housed separately, it was difficult for researcher assistants to be blind to the treatment conditions, as some participated in the randomization that immediately followed recruitment and families sometimes gave clues regarding the nature of the services they received during later assessments. Caregivers were compensated for their time for each of the completed research assessments and monthly interviews.
Participants
Participants were 127 youth referred by the county State’s Attorney after having been charged with a sexual offense. Inclusion criteria were (a) judicial order for outpatient sexual offender treatment either as part of post-adjudication probation or pre-adjudication diversion, (b) presence of a local (i.e., in the study county) caregiver with whom the youth resided, (c) youth age between 11 and 17 years inclusive (one youth was 17 at referral and 18 at recruitment), (d) fluency in either English or Spanish (all forms and measures were available in English and Spanish), and (e) absence of current psychotic symptoms or serious mental retardation. To maximize generalizability of results, youth with other co-morbid psychiatric disorders (e.g., depression, anxiety) or co-occurring conduct problems (e.g., school truancy, nonsexual offenses, substance abuse) were included in the study.
Recruitment
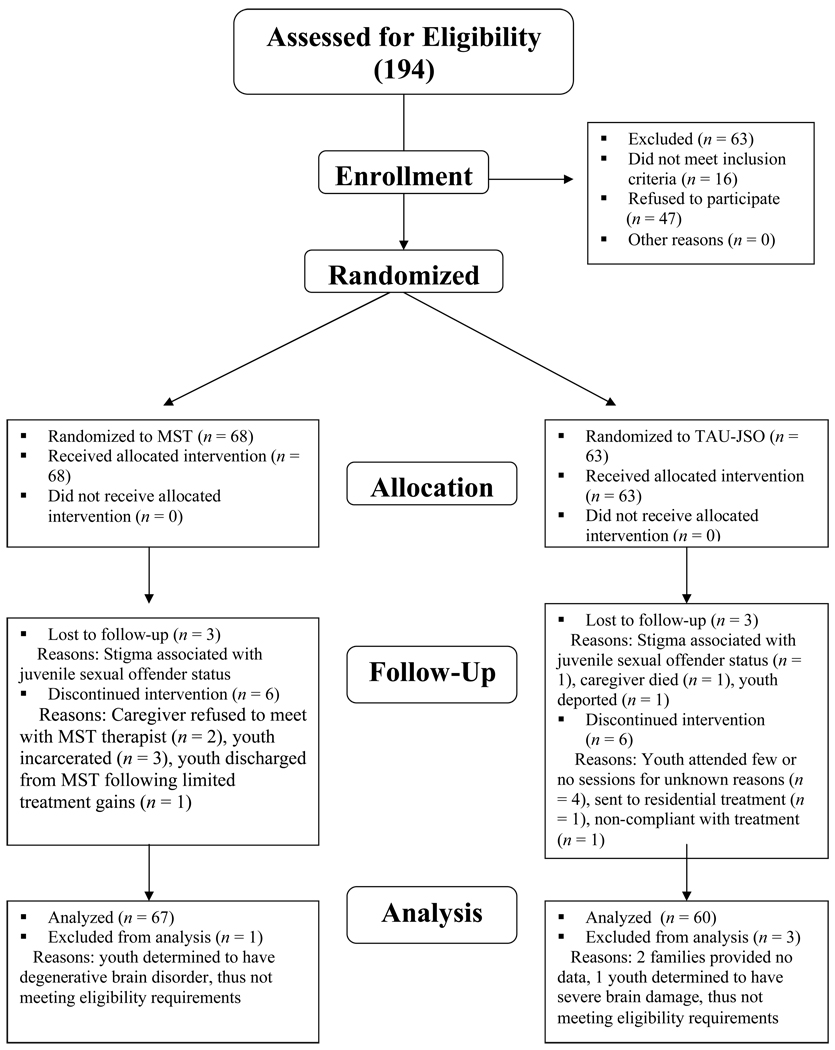
Families were recruited by a researcher who obtained informed consent and assent, with all forms and procedures approved by the institutional review boards of the participating universities. Figure 1 depicts the study flow from referral through data analyses. As can be seen, 178 eligible youth were referred to the study, and 131 consented to participate (74%). This recruitment rate was below that achieved in other MST trials with juvenile offenders (e.g., Henggeler et al., 2006) and likely reflects the considerable stigma associated with sexual offending. Immediately following recruitment, a sealed envelope was opened, and the family was informed of the treatment condition to which they were assigned. Two families immediately withdrew from the study (both in TAU-JSO) upon learning that they were not randomized to their desired intervention, and two others (one in MST, one in TAU-JSO) were subsequently excluded due to degenerative brain disorders in the youth – leaving a final sample of 127 participants.
Figure 1.
Study enrollment flow chart.
Even with randomization, chance imbalances across important prognostic factors can occur (Kernan, Viscoli, Makuch, Brass, & Horwitz, 1999). The risk of chance imbalances is magnified for prognostic variables that are not equally distributed within the sample pool. In the subject population accessed for the present study, a higher percentage of offenders had younger versus peer (or older) victims. Thus, a “stratified permuted blocks randomization” (McEntegart, 2003, p. 297) process was used, with separate randomization categories based on index victim age. In practice, all participants were randomly assigned to treatment groups, but separate randomization lists were used for treatment group assignments of youth with child versus peer/older victims.
Research and Treatment Retention
Of the 127 study participants who provided data, 6 families dropped out after completing one or more assessments, resulting in a 95% research retention rate. Additionally, some families who remained in the study were unable to complete one or more research assessments for various reasons. Overall, 127 assessments were completed at T1, 124 (98%) at T2, and 120 (94%) at T3. Regarding treatment retention, few youth failed to complete MST (n = 6) or TAU-JSO (n = 5), and these failures were typically due to youth placement in secure settings. Recruitment was conducted from January 2004 through June 2006 with follow-up continuing through November 2007. Analysis was by intent-to-treat.
Intervention Conditions
At the outset of study involvement, youth had been referred for sexual offender-specific treatment either as part of probation requirements (immediately following either adjudication or return from residential placement) or as part of a diversion program through the State’s Attorney Office. Youth on probation (n = 71) were typically required to comply with numerous conditions, including regular meetings with probation officers, home and school probation visits, mandatory curfews, community service, and completing treatment. Youth who had received diversion from the State’s Attorney (n = 56) were required to comply with a more limited set of conditions, but one of those conditions included the completion of treatment. Random assignment resulted in 36 (54%) probation and 31 (46%) diverted youth in the MST condition, and 35 (58%) probation and 25 (42%) diverted youth in the TAU-JSO condition.
MST
The MST therapists worked on a team with individual caseloads of four to six families per therapist. As is standard with MST, the practitioners used a home-based model of service delivery in which treatment was delivered in home and community (e.g., school) settings at times convenient to families. In addition, rotating members of the team were available to respond to crises 24 hours per day, 7 days per week.
MST interventions for adolescent antisocial behavior are specified in a treatment manual (Henggeler et al., 1998) that describes the empirical, conceptual, and philosophical bases of MST and delineates the processes by which youth and family problems are prioritized and targeted for change. Rather than providing session-by-session breakdowns of recommended clinical procedures, nine treatment principles are used to guide therapists' case conceptualizations, prioritization of interventions, and implementation of intervention strategies. The overriding goals of MST are to empower parents with the skills and resources needed to independently address the inevitable difficulties that arise in raising adolescents and to empower adolescents to cope with familial and extrafamilial problems. Using well-validated treatment strategies derived from pragmatic family therapies, behavioral parent training, and cognitive-behavioral therapy, MST directly addresses intrapersonal (e.g., cognitive problem solving), familial (e.g., inconsistent discipline, low monitoring, family conflict), and extrafamilial (e.g., association with deviant peers, school difficulties) factors that are associated with youth serious antisocial behavior, including sexual offending. Because different contributing factors are relevant for different youth and families, MST interventions are individualized and flexible.
To more fully account for clinical issues relevant to juveniles who have sexually offended and their families, the investigators adapted MST to the special needs of this clinical population. Importantly, MST for juvenile sexual offenders is identical to standard MST in its broad and individualized focus on the risk factors associated with juvenile offending generally, but enhances standard MST by addressing aspects of the social ecology that are functionally related to the youth’s sexual delinquency. The three main adaptations to MST are specified in a supplemental therapist training manual (Borduin, Letourneau, Henggeler, Saldana, & Swenson, 2005). (1) Protocols addressed youth and caregiver denial about the offense. Therapists were trained to assess the primary drivers of an individual’s denial (e.g., shame, fear of additional social or legal consequences) and the extent to which denial interfered with treatment goals (e.g., whether, despite denying the extent of the offense, caregivers remained willing to make changes to reduce the likelihood of future offending). In several cases, youths’ defense attorneys (from whom some families obtained the impression they should not admit to the offense) were contacted and successfully engaged in efforts to reduce caregiver or youth denial. Youth denial was considered relatively normative, given the general propensity of adolescents to lie to stay out of trouble. Provided caregivers and youth made relevant behavioral changes, they were retained in treatment despite denial, rather than discharged from treatment as often occurs in usual services settings. (2) Protocols also addressed safety planning to minimize the youth’s access to potential victims. Safety planning was based on the functional analysis of the index offense, in which the behavioral drivers and other factors leading up to the offense were targeted for change. For example, if easy access to younger children (e.g., via frequent unmonitored babysitting or sharing bedrooms) was a driver of the youth’s offending behavior, that access would be eliminated. (3) And, protocols addressed promotion of age-appropriate and normative social experiences with peers. Interventions could include strategies for identifying prosocial peers among a youth’s acquaintances and assisting parents to make their homes attractive places for these prosocial youth to congregate. After-school and community activities also were identified and caregivers given strategies to assist youth involvement in such activities.
TAU-JSO
All youth in the TAU-JSO condition (n = 60) were referred for sexual offender-specific treatment and the vast majority received services provided by the juvenile sexual offender unit (JSO Unit) of the juvenile probation department. The youth on probation were directly under the supervision of probation officers and met for sexual offender treatment in groups of approximately 8 to 10 youth for weekly 60-minute sessions. The sexual offender treatment groups included components that addressed deviant arousal, victim empathy, cognitive distortions, relapse prevention, and family counseling. Youth with other specific needs (e.g., substance abuse) could be referred for additional services. Key treatment objectives included youth acceptance of responsibility for the offense(s), breaking the sexual offense cycle by increasing youth’s awareness of triggers, identification and exercise of internal and external behavioral controls, and development of a relapse prevention protocol to reduce the risk of recidivism. As discussed previously, these clinical emphases and the group-based model of service delivery are consistent with the types of services typically provided to juvenile sexual offenders in community settings (McGrath et al., 2003). Diverted youth participated in the same group treatment sessions with the youth on probation, but the former received no direct probation supervision (i.e., no field officer initiated home or school visits).
Families had the option of paying for private treatment rather than participating in the juvenile sexual offender groups offered by probation, and five families chose to do so. Two of the youth attended a private treatment facility that specialized in juvenile sexual offenders and whose treatment procedures and goals overlapped considerably with those of the JSO Unit. Information on the treatment foci for the remaining three youth who received private treatment could not be obtained. However, the participating state has legislated minimum standards for sexual offender treatment providers, who must be approved by the state’s sex offender management board. These standards require adherence to sexual offender assessment and treatment interventions similar to those provided by the JSO Unit. Thus, the youth who received private therapy were retained in the TAU-JSO condition.
Therapist Characteristics
MST
MST was provided by one pre-doctoral, three masters-level, and one bachelor-level clinicians employed by a private community-based provider agency. Two of the therapists had prior MST experience. All MST clinicians complete a standard 5-day MST training curriculum, and the therapists in this study also completed a 1.5-day training specific to working with juvenile sexual offenders and their families within the context of MST (Borduin et al., 2005). One therapist was bilingual and treated Spanish-speaking families. Consistent with standard MST quality assurance procedures (Schoenwald, 2008), weekly supervision sessions were held with an on-site MST supervisor, and weekly consultation sessions were held via conference calls with MST expert consultants. These meetings focused on promoting treatment fidelity and identifying and overcoming barriers to achieving treatment goals. As part of the standard MST training model, quarterly booster sessions also were provided to address special challenges experienced by the MST team. The only compromise to conducting a pure effectiveness trial was that the first and third authors served in the role of MST expert consultant during the weekly conference calls and quarterly booster trainings.
TAU-JSO
The sexual offender treatment groups were led by seven specially trained “treatment probation officers,” of whom three held bachelor’s degrees and four held master’s degrees. Three master’s level treatment probation officers also held clinical licenses, and all treatment probation officers completed a certification course for treating juvenile sexual offenders. At least one probation officer was bilingual and treated Spanish-speaking youth. The treatment probation officers received group supervision approximately twice per month from their supervisor, who was licensed and experienced. All treatment probation officers received ongoing training resulting in a minimum of 20 annual continuing education units.
Treatment Fidelity
MST
Four aspects of intervention fidelity are relevant. First, as noted previously, MST has a well-specified quality assurance protocol aimed at promoting therapist adherence, and this protocol was fully implemented in the present study. Second, the MST quality assurance protocol includes a standard measure of therapist adherence to the nine MST treatment principles, and several studies have demonstrated significant associations between adherence scores on this measure and short- and long-term youth outcomes in MST clinical trials and dissemination sites (Schoenwald, 2008). For present purposes, the MST Therapist Adherence Measure (TAM; Henggeler & Borduin, 1992) was completed monthly by caregivers in the MST condition to assess treatment adherence. Although mean adherence scores of 3.99 (SD = .68) in the present study were below those of MST therapists a 45-site transportability study (M = 4.41, SD = .49; Schoenwald, Sheidow, Letourneau, & Liao, 2003), scores were well above those of community-based therapists who were not delivering MST in a recently completed clinical trial (Henggeler et al., 2006). Third, the 91% treatment completion rate met or exceeded MST program standards. Fourth, the average duration was 7.1 months (SD = 2.8 months), which is similar to that of Borduin et al. (in press) efficacy study and other studies examining adaptations of MST (e.g., Ellis, Naar-King, Cunningham, & Secord, 2006). This average length, however, is considerably longer than the typical 4-month duration of standard MST in community programs. The extended treatment length is likely due to a combination of factors, including intense community safety concerns presented by this clinical population and more general factors associated with adapting evidence-based interventions for new populations.
TAU-JSO
Formal measures of treatment fidelity were not collected for the TAU-JSO condition because such measures have not been validated for this intervention. The group-based intervention was standardized, however, with particular therapeutic activities and workbooks used by all clinicians. Moreover, the clinical emphases were consistent, and the same supervisor provided guidance to the group therapists throughout the project. Although treatment adherence, per se, was not assessed, caregivers completed a client satisfaction questionnaire (CSQ; Attkinsson et al., 2000) at the T2 assessment. Mean scores on this survey indicated a reasonable degree of satisfaction with services. For example, caregivers gave a mean score of 1.8 (1 = excellent, 4 = poor) on the item “how would you rate the quality of service you received?” (Ratings by caregivers in the MST condition were similar; e.g., M = 1.6 for the same item). Treatment length was also examined as a gross indicator of fidelity. The average length of treatment was expected to last approximately 1 year for youth placed on probation and 6 months for diverted youth. The observed average treatment durations of 14.6 months (SD = 11.0 months) and 8.2 months (SD = 5.5 months) for the probation and diverted youth, respectively, were slightly longer than expected. Nevertheless, these treatment lengths are typical of U.S. juvenile sexual offender treatment programs (McGrath et al., 2003).
Criminal Records
Criminal records from city, state, and national sources were accessed to determine index sexual offenses (i.e., those charges that triggered study eligibility and for which youth were referred to treatment) and prior sexual and non-sexual offense charges. Data on 433 charges were entered separately by two “blind” raters who had 98.6% agreement regarding individual charges (i.e., both raters coded 427 of the 433 records the same, but differed on whether they considered the remaining entries to be independent charges vs. modifiers of previously entered charges) and dates of charges. In addition, police investigative reports were reviewed for descriptive information on index sexual offenses pertaining to victim gender, age at offense, and relationship to offender as well as whether an offense included penetration, multiple victims, multiple offenders, or excessive force. Interrater reliability computed across two reviewers for all 127 cases on each of these items was excellent for some of these variables (e.g., whether the index offense involved one or more victims), but unacceptable for others (e.g., whether the index offense involved excessive force). Thus, information on index offenses is provided subsequently for descriptive purposes only, and was not used in subsequent analyses.
Outcome Measures
This report focuses on the key outcomes of interest for these juveniles. These outcomes pertain to the youth’s sexual behaviors, delinquency, substance use, and mental health symptoms assessed at T1, T2, and T3; and to possible out-of-home placements assessed during the monthly phone interviews. Before describing these measures, it is important to explain why sexual reoffending was not examined in this report. Juvenile sexual recidivism is a low base rate event (Caldwell, 2002; Fortune & Lambie, 2006), and a 12-month follow-up does not provide enough time to identify the number of recidivism events needed to support statistical analyses. Indeed, only one instance of officially recorded sexual recidivism was identified with the present sample throughout the 12-month follow-up period.
Problem sexual behavior
Two subscales of the Adolescent Sexual Behavior Inventory (ASBI; Friedrich, Lysne, Sims, & Shamos, 2004) were used to assess inappropriate adolescent sexual behaviors from both youth and caregiver perspectives. Derived through factor analyses, the 5-item (youth version) and 9-item (parent version) deviant sexual interests subscale taps youth behaviors such as owning pornography, use of phone sex lines, and voyeurism. The 10-item (youth version) and 8-item (parent version) sexual risk/misuse subscale assesses overt sexual behaviors such as having unprotected sex, being sexually used by others, and pushing others into having sex. The ASBI has demonstrated adequate reliability (coefficient alphas ranging from .65 to .81) and validity with non-abused youth and with sexually abused youth, of whom a significant percentage reported engaging in sexually abusive acts (Friedrich et al., 2004). In the present sample, mean alpha coefficients across the three time points were .67 and .73 for caregiver reported deviant sexual interests and sexual risk/misuse subscales, respectively. Mean alpha coefficients were .50 for both youth reported versions of these scales, likely due to low item endorsement rates by youth.
Delinquency
Youth criminal behavior was measured by the self-report delinquency scale (SRD), which was designed for the National Youth Survey (NYS; Elliott, Huizinga, & Ageton, 1985) to assess self-reported criminal and delinquent acts during the past 90 days. The present study focused on the 35-item General Delinquency subscale, which includes a wide variety of criminal and delinquent behaviors. The SRD is regarded as one of the best validated measures of self-reported delinquency (e.g., Thornberry & Krohn, 2000), and the mean coefficient alpha across assessment points was .67 in the present sample
Substance use
Youth substance use was assessed with a subscale of the Personal Experience Inventory (PEI; Winters & Henly, 1989). This subscale combines two items assessing the frequency of adolescent alcohol and marijuana use for the previous 90 days. The PEI is a reliable and well-validated instrument (Stinchfield & Winters, 1997).
Mental health symptoms
Youth mental health symptoms were assessed with the Externalizing and Internalizing scales of the parent-reported Child Behavior Checklist (CBCL; Achenbach, 1995) and the corresponding Youth Self Report (YRS; Achenbach; 2001). These measures are well-validated and considered among the best for assessing youth mental health functioning (e.g., Rescorla & Achenbach, 2004).
Out-of-home placements
The caregiver-reported monthly Services Utilization Tracking form (Henggeler, Pickrel, Brondino, Ward, & Rowland, 1997) was used to collect youth placement data. This instrument has been used in previous MST studies (e.g., Henggeler et al., 2006; Schoenwald, Ward, Henggeler, Pickrel, & Patel, 1996). Caregivers were asked whether the youth resided outside the home since the last assessment. If a change in residence was noted, the nature of the change was recorded (e.g., detention, foster care, residential sexual offender treatment).
Data Analyses
Data for the current study are comprised of three repeated measurements (level-1) nested within 127 youth/caregivers (level-2), yielding a two-level Mixed-Effects Regression Model (MRM). The outcomes were modeled according to a linear polynomial term with values of 0, 1, and 2 corresponding to the three evenly spaced measurement occasions; and treatment condition was coded such that MST = 0 and TAU-JSO = 1. Due to a preponderance of 0 responses, scores on the ASBI scales, SRD, and PEI were dichotomized to reflect any report of sexual behavior problems, delinquent behavior, or substance use at each assessment occasion. Of note, the out-of-home placement outcome was based on 12 (monthly) repeated measurements (level-1) nested within youth/caregivers (level-2), with the linear polynomial term coded with values of 0 to 11.
MRMs were performed using HLM software (version 6.04; Raudenbush, Bryk, Cheong, Congdon, & du Toit, 2004), with restricted maximum likelihood estimation for continuous outcomes and a Bernoulli model with a logit link function and Laplace approximation of maximum likelihood function for dichotomous outcomes. The dichotomous out-of-home placement outcome was modeled according to a Binomial Trial that adjusted for the number of days covered by each report. Specification of random effects was based on the likelihood ratio test when possible and otherwise was based on the Wald test for variance components (Singer & Willett, 2003). Robust SEs were used to compute the Wald (i.e., T-ratio) test statistic for the fixed effects (Maas & Hox, 2005), and population-average results were interpreted for the dichotomous outcomes (Raundenbush & Bryk, 2002).
Covariates entered into each model included age at recruitment, race (white or other), and number of prior nonsexual offenses. Hispanic ethnicity was initially included but dropped due to high colinearity with race. Due to the small number of girls, some models (i.e., involving ASBI scales and out-of-home placement) would not converge until the gender covariate was removed.
Results
Participant Characteristics
Youth demographics and index sexual offenses
The mean age of youth at pretreatment was 14.6 years (SD = 1.7 years, range = 11 to 18 years). Only three (2.4%) participants were female. Most youth were Black (54%) or White (44%), and 31% of youth indicated Hispanic ethnicity. This sample reflected the demographic makeup of the surrounding urban county. Thirty-five percent of youth had nonsexual offenses in addition to sexual offenses, ranging from ordinance violations to serious person-related offenses. In the 3 months prior to baseline, 11% of the youth had received mental health services, and 4% had received substance abuse services.
Index sexual offense charges included aggravated criminal sexual assault (31%), criminal sexual assault (18%), aggravated criminal sexual abuse (15%), criminal sexual abuse (24%), other sexual offenses (5%), and sexual offenses that were pled down to nonsexual offenses (7%). Police investigative reports indicated that most youth acted alone at the time of their offense (84%) and offended against a single victim (80%). Victim ages ranged from 1 year through adulthood, with most victims falling between 4 and 15 years of age. Most youth (74%) had female victims, 20% had male victims and 6% had male and female victims. Youth offended against relatives (36%), friends (including classmates and neighbors, 37%), acquaintances (21%), and/or strangers (6%). Offense descriptions indicated that, in general, “assault” offenses were more serious than “abuse” offenses and “aggravated” offenses more serious than offenses not so designated. Offenses leading to charges of aggravated criminal sexual assault were more likely to involve excessive force in combination with sexual penetration than were offenses leading to other charges. For example, one youth charged with this offense collaborated with two other offenders to kidnap and physically and sexually assault a woman. Offenses leading to criminal sexual assault charges usually involved some form of penetration but were not often characterized by excessive force. For example, one case involved a youth raping but not otherwise physically assaulting his victim. Offenses leading to charges of aggravated criminal sexual abuse typically involved sexual penetration. For example, one such charge involved an offender who forced three victims to perform oral sex on him and on one another. Offenses leading to criminal sexual abuse charges were more likely to involve fondling than penetration. For example, a youth charged with criminal sexual abuse touched and licked a much younger victim’s vagina. The remaining charges (e.g., sexual exploitation of a child, pleas resulting in non-sexual offense charges) tended to result from less serious offenses. For example, one youth charged with sexual exploitation of a child coaxed a much younger child to remove her clothing.
Caregiver and family-level demographics
Youth’s primary caregivers were mothers (64%), fathers (15%), other female relatives (19%), foster parents (2%), and a male relative (1%). Primary caregivers were partly or fully employed outside the home (52%), unemployed (24%), or homemakers (19%). Many caregivers (41%) had not completed high school, while 27% were high school graduates, and 32% had completed one or more years of college. At T1, primary caregivers were married (48%), divorced (20%), separated (8%), never married (21%), or widowed (3%). Family economic status varied, with 33% of families earning less than $10,000/year, 38% earning $10,000 to $30,000/year, and 28.5% earning $30,000 or more. These data indicate that the participating families were generally socio-economically deprived.
Baseline comparisons
Independent samples t-tests and chi-square analyses were used to examine baseline differences between treatment conditions on the index offense, presence of prior non-sexual offenses, and demographic variables. In no case did a statistically significant between-groups difference emerge, supporting the effectiveness of the randomization process.
Outcomes
Table 1 provides descriptive statistics for each of the outcome measures by treatment condition and assessment occasion. The results from the MRMs are presented in Table 2. All analyses were conducted with and without the five TAU-JSO youth treated by private practitioners, and the results did not differ. Hence, the findings for the full sample are presented.
Table 1.
Pretreatment (T1), 6-Month (T2), and 12-Month (T3) Scores for Dichotomous (Percentage Responding Positive) and Continuous (Mean and Standard Deviation) Outcomes.
| MST | TAU-JSO | |||||
|---|---|---|---|---|---|---|
| Outcome Instrument | T1 | T2 | T3 | T1 | T2 | T3 |
| Problem Sexual Behavior | ||||||
| ASBI Deviant Sexual Interests youth-report | 26.9% | 16.9% | 10.9% | 20.0% | 24.1% | 15.4% |
| ASBI Sexual Risk/Misuse youth-report | 58.2% | 43.1% | 29.7% | 53.3% | 53.4% | 48.1% |
| ASBI Deviant Sexual Interests caregiver-report | 78.8% | 45.3% | 36.5% | 68.3% | 56.1% | 52.9% |
| ASBI Sexual Risk/Misuse caregiver-report | 34.3% | 17.2% | 7.9% | 20.0% | 19.3% | 19.2% |
| Antisocial Behavior | ||||||
| SRD Delinquent Behavior | 74.6% | 41.5% | 29.7% | 51.7% | 53.4% | 42.3% |
| PEI Substance Use Index | 35.8% | 24.6% | 17.2% | 23.3% | 32.8% | 38.5% |
| Mental Health Symptoms | ||||||
| YSR Externalizing T-score | 47.5 (12.8) | 41.9 (11.1) | 40.8 (10.0) | 47.1 (9.7) | 48.2 (10.3) | 44.9 (9.7) |
| YSR Internalizing T-score | 47.2 (12.6) | 42.1 (10.8) | 39.37 (9.8) | 47.1 (10.6) | 45.8 (9.4) | 41.7 (9.4) |
| CBCL Externalizing T-score | 52.5 (13.2) | 47.1 (12.9) | 45.4 (12.7) | 54.9 (11.4) | 53.4 (11.3) | 48.5 (10.3) |
| CBCL Internalizing T-score | 53.4 (11.4) | 46.2 (12.1) | 42.8 (11.4) | 54.4 (11.8) | 52.0 (12.6) | 46.2 (11.0) |
Note. ASBI = Adolescent Sexual Behavior Inventory; SRD = Self-Report Delinquency Scale; PEI = Personal Experiences Inventory; YSR = Youth Self-Report; CBCL = Child Behavior Checklist.
Table 2.
Mixed-Effect Regression Models for Treatment Outcome Measures
| Initial Status | Rate of Change | ||||
|---|---|---|---|---|---|
| Outcome Instrument | Parameter | Intercept (π0i) | Condition × Intercept (β01) | Linear (π1i) | Condition × Linear (β11) |
| Dichotomous Models | |||||
| ASBI Deviant Sexual Interests youth-report |
β | −0.71 | −0.20 | −0.62*** | 0.51* |
| SE | 0.34 | 0.39 | 0.16 | 0.26 | |
| df | 122 | 122 | 359 | 359 | |
| OR | 0.49 | 0.82 | 0.54 | 1.66 | |
| 95% CI | 0.25 – 0.96 | 0.38 – 1.78 | 0.39 – 0.73 | 1.00 – 2.75 | |
| ASBI Sexual Risk/Misuse youth-report |
β | −0.58 | −0.11 | −0.75*** | 0.65* |
| SE | 0.28 | 0.36 | 0.19 | 0.28 | |
| df | 122 | 122 | 359 | 359 | |
| OR | 0.56 | 0.90 | 0.47 | 1.92 | |
| 95% CI | 0.32 – 0.98 | 0.44 – 1.81 | 0.33 – 0.68 | 1.16 – 3.29 | |
| ASBI Deviant Sexual Interests caregiver-report |
β | 0.45 | −0.38 | −0.99*** | 0.65* |
| SE | 0.27 | 0.35 | 0.17 | 0.26 | |
| df | 122 | 122 | 354 | 354 | |
| OR | 1.56 | 0.68 | 0.37 | 1.92 | |
| 95% CI | .91 – 2.69 | 0.34 – 1.37 | 0.27 – 0.52 | 1.16 – 3.19 | |
| ASBI Sexual Risk/Misuse caregiver-report |
β | −1.75 | −0.74 | −1.02*** | 1.02** |
| SE | 0.33 | 0.42 | 0.24 | 0.31 | |
| df | 122 | 122 | 356 | 356 | |
| OR | 0.17 | 0.48 | 0.36 | 2.78 | |
| 95% CI | 0.09 – 0.33 | 0.21 – 1.10 | 0.23 – 0.58 | 1.51 – 5.13 | |
| SRD Delinquent Behavior |
β | 0.32 | −0.82 | −1.09*** | 0.92** |
| SE | 0.29 | 0.32 | 0.19 | 0.27 | |
| df | 121 | 121 | 358 | 358 | |
| OR | 1.38 | 0.44 | 0.34 | 2.50 | |
| 95% CI | 0.78 – 2.43 | 0.23 – 0.84 | 0.23 – 0.49 | 1.47 – 4.25 | |
| PEI Substance Use Index |
β | −1.49 | −0.54 | −0.70** | 1.20*** |
| SE | 0.45 | 0.48 | 0.20 | 0.29 | |
| df | 121 | 121 | 358 | 358 | |
| OR | 0.22 | 0.58 | 0.50 | 3.33 | |
| 95% CI | 0.09 – 0.55 | 0.23 – 1.50 | 0.34 – 0.73 | 1.90 – 5.85 | |
| Out-of-home placements |
β | −6.83 | 0.15 | −0.01 | 0.07*** |
| SE | 0.16 | 0.20 | 0.01 | 0.02 | |
| df | 122 | 122 | 1155 | 1155 | |
| OR | .001 | 1.16 | 0.99 | 1.07 | |
| 95% CI | .001 – .001 | 0.78 – 1.73 | 0.97 – 1.01 | 1.04 – 1.12 | |
| Continuous Models | |||||
| YSR Externalizing T-score |
β | 44.41 | 0.79 | −3.10** | 2.49* |
| SE | 1.81 | 1.88 | 0.87 | 1.08 | |
| df | 121 | 121 | 333 | 333 | |
| YSR Internalizing T-score |
β | 45.05 | 0.72 | −3.72*** | 1.33 |
| SE | 1.66 | 1.94 | 0.95 | 1.22 | |
| df | 121 | 121 | 125 | 125 | |
| CBCL Externalizing T-score |
β | 47.17 | 3.36 | −3.79*** | 0.76 |
| SE | 1.80 | 2.01 | 0.75 | 1.08 | |
| df | 121 | 121 | 331 | 331 | |
| CBCL Internalizing T-score |
β | 50.57 | 2.41 | −5.20*** | 1.21 |
| SE | 1.71 | 2.10 | 0.71 | 1.18 | |
| df | 121 | 121 | 331 | 331 | |
Note. The T ratio test statistic for each parameter (omitted) was computed as βtij/SE; Condition was coded as 0 = MST, 1 = TAU-JSO. Youth age, gender, race (coded as 0 = white, 1 = non-white), and history of prior offenses (coded as 0 = no priors, 1 = one or more priors) were included as covariates in each model. ASBI = Adolescent Sexual Behavior Inventory; SRD = Self-Report Delinquency Scale; PEI = Personal Experiences Inventory; YSR = Youth Self-Report; CBCL = Child Behavior Checklist.
p < .05.
p < .01.
p <.001.
Problem sexual behavior
Bernoulli MRMs revealed significant negative linear effects on all four ASBI scales (ps < .001), indicating that the scores on these scales for youth in the MST condition decreased from pretreatment to 12 months post recruitment (see Table 2). The condition × linear effects were positive and significant for each ASBI scale (ps < .05). This indicates that the MST youth evidenced significantly greater reduction in problem sexual behavior over time, relative to their TAU-JSO counterparts. For example, as seen in Table 1, caregiver reports of youth sexual risk/misuse declined from T1 to T3 by about 77% for youth in the MST condition, in comparison with minimal decline for youth in the TAU-JSO condition.
Delinquency and substance use
Bernoulli MRMs revealed significant negative linear effects on the SRD (p < .001) and PEI (p < .01), indicating reduced self-reported delinquent behavior and substance use over time for youth in the MST condition (see Table 2). The condition × linear effects were positive and significant in both models (ps < .01). These results indicate that, in contrast to TAU-JSO youth, participants in the MST condition reported significantly greater reduction in delinquent behavior and decreased substance use from T1 to T3. As shown in Table 1, the percentage of youth reporting delinquent behavior decreased by about 60% from T1 to T3, whereas the corresponding decrease for youth in the TAU-JSO condition was 18%. Similarly, although the percentage of MST youth who reported substance use decreased by about 50% from T1 to T3, the percentages of substance using youth in the TAU-JSO condition almost doubled during this same time.
Mental health symptoms
MRM analyses yielded a significant negative linear effect (p < .01) and a significant positive condition × linear effect (p < .05) on the YSR externalizing scale (see Table 2). This indicates that the MST youth evidenced significantly greater reduction in self-reported externalizing symptoms over time compared to their TAU-JSO counterparts (see Table 1). Results revealed significant negative linear effects (ps < .01) but no condition × linear effects (ps > .05) on the remaining outcome variables, suggesting that the MST and TAU-JSO groups evidenced similar reductions in caregiver-reported externalizing and youth- and caregiver-reported internalizing symptoms over time. Baseline mean scores for all four mental health symptom scales were in the normal range, suggesting that statistically significant reductions might not translate to clinically relevant improvement over time. Clinical significance for youth whose baseline YSR externalizing T scores were at or above 60 (i.e., sub-clinical to clinical range), however, was assessed. Seventy-three percent (8 of 11) of youth in the MST condition demonstrated clinically significant improvements at T3 (i.e., T scores declined to below 60) in comparison with 20% (1 of 5) of youth in the TAU-JSO condition. Although limited by the small sample of clinically distressed youth, this finding supports a clinically meaningful treatment effect regarding youth reports of externalizing symptoms.
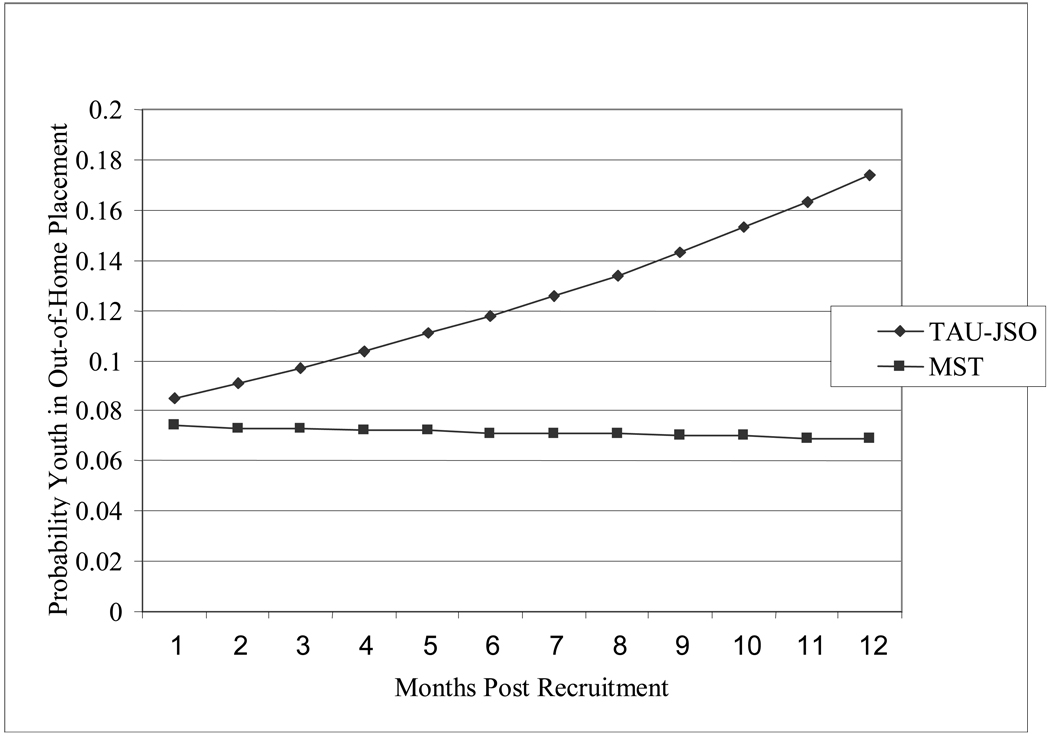
Out-of-home placements
The Binomial Trial MRM, adjusting for the number of days covered by each report, indicated a significant condition × linear effect (p < .001) for the percentages of youth in out-of-home placements throughout the monthly assessments (see Table 2). As depicted in Figure 2, the probability that an MST youth was in an out-of-home placement (i.e., detention, residential treatment, foster care) during the past 30 days remained approximately 7% through 12 months post recruitment. For youth in the TAU-JSO condition, the probability of being placed increased from 8% to 17% during the course of the follow-up.
Figure 2.
Out-of-home placements as a function of treatment condition and assessment time point.
Moderator Analyses
Moderator analyses were conducted to determine whether treatment effects varied by perpetrator-victim age differential (Kemper & Kistner, 2007) and level of aggression in the sexual offense (Butler & Seto, 2002). For age differential, youth were classified as having “child” victims if one or more victims was at least 5 years younger than the offender (n = 70) or “peer/older” victims if all victims were within 4 years of age or older than the offender at the time of the offense (n = 57). For level of aggression, adjudication was used as a proxy variable, where youth who were diverted prior to adjudication (n = 56) were considered to have perpetrated less aggressive sexual offenses than youth who were formally prosecuted and placed on probation (n = 71). Bernoulli MRMs were conducted to determine whether MST treatment effects for each of the outcome variables were moderated by either of these offender subtypes. In no case did a significant interaction effect emerge, thereby indicating that treatment effects did not vary by the nature of the juveniles’ offenses.
Discussion
The primary aim of this study was to conduct a rigorous community-based effectiveness trial in which MST adapted for juvenile sexual offenders was compared with the type of group-based services that are typically provided to such offenders in the U.S. The implementation of the study was successful, with strong and consistent collaboration from juvenile justice authorities, sustained clinical efforts from the private agency providing the adapted MST treatment, and high rates of participant clinical and research retention. Regarding the conceptual aims of the study, intent-to-treat analyses consistently supported the ability of MST to achieve desired outcomes through 1-year post recruitment. Indeed, MST was more effective than TAU-JSO in decreasing deviant sexual interest/risk behaviors, delinquent and substance use behaviors, externalizing problems, and costly out-of-home placements. Although officially documented sexual recidivism was not examined in the present study due to low rates of short-term re-offending (as noted previously), the favorable 1-year findings for MST are consistent with the long-term reductions in sexual reoffending observed in two prior MST efficacy studies with juvenile sexual offenders (Borduin et al., 1990; Borduin et al., in press).
The findings from the present study have important clinical and policy implications. The generally favorable outcomes for the MST condition support the viability of community-based and family-focused interventions that address the known risk factors of serious antisocial behavior, including sexual offending behaviors, across multiple ecological systems in which youth are embedded. As noted previously, the evidence-based practices that have emerged in the treatment of other types of serious antisocial behavior in adolescents have usually been family-based and comprehensive in nature. As such, the present findings are congruent with the growing consensus that family-focused interventions targeting multiple ecological systems are among the most supported interventions for serious behavior problems, including child sexual behavior problems (St. Amand, Bard, & Silovsky, 2008), serious juvenile delinquency (Elliott, 1998; U.S. Public Health Service, 2001), and adolescent substance abuse and dependence (Waldron & Turner, 2008). In addition, the finding that MST was more effective than TAU-JSO at maintaining youth in their homes is consistent with system of care principles (Stroul & Friedman, 1996), supports the value of addressing youth needs in the least restrictive judicial and clinical settings (Federal Advisory Committee on Juvenile Justice, 2007), and might result in cost savings.
In addition, current results supporting MST bring into question the public health/safety effects of the increasingly severe legal consequences (e.g., lifetime public registration, prolonged residential treatment) placed on juveniles who sexually offend (Chaffin, 2008). Clinical findings such as those presented here and the favorable reductions in recidivism achieved in the aforementioned MST efficacy trials (Borduin et al., 1990; Borduin et al., in press), in conjunction with emerging findings that deterrent-oriented sexual offender registries for juveniles do not influence sexual recidivism rates (Letourneau & Armstrong, in press), can be used to promote a more strength-focused and rehabilitative approach to addressing the needs of juvenile sexual offenders.
Limitations
Several types of limitations should be noted. The first set concerns challenges in measurement methods for juvenile sexual offender outcome research. A longer follow-up is clearly needed to determine whether the observed 1-year outcomes will translate to reduced sexual offending, and such a follow-up is in progress. In addition, self-report measures of inappropriate or criminal sexual behaviors for adolescents have not yet been fully validated, particularly with respect to predictive validity. The ASBI was used in this study to assess youth sexual behaviors because it is one of few measures that is developmentally sensitive and not based on an adult measure, provides a multi-informant strategy that increased confidence in results (as caregiver and youth reports converged in this study), and has been tested on non-offending groups. Finally, a review of score means (e.g., SRD, PEI, and ASBI scores had to be dichotomized, CBCL means were within the normal range) indicates that, similar to findings from studies of other juvenile sexual offenders (e.g., Butler & Seto, 2002; Ronis & Borduin, 2007), youth in the present study did not evidence high rates of psychopathology. Such could be an accurate reflection of youth functioning or indicate self-presentational bias due to the serious stigma and legal sanctions associated with sexual offending (Zimring, 2004). Although care was taken to reduce self-presentational bias (e.g., extensive training of research assistants; emphasis on confidentiality of data, including a Federal Certificate of Confidentiality; use of well validated assessment instruments), the effectiveness of such efforts is difficult to ascertain.
A second limitation of this study pertains to the external validity of the sample. A small portion (5%) of otherwise eligible youth was excluded from the study because they were initially sent to restrictive placements (e.g., residential treatment, incarceration). Although such youth became eligible when they returned from placement, the findings do not necessarily generalize to the most serious juvenile sexual offenders.
Third, the research assistants were often not blind to the families’ treatment conditions. Although the research assistants were housed in different offices than the clinicians to promote clinical/research boundaries, some researchers were involved in the consenting and randomization process and it was not possible to prevent families from providing clues as to the nature of their intervention condition – especially in light of the considerable distinctions between the family- and home-based MST condition versus the group- and office-based TAU-JSO condition. To attenuate possible bias in the present case, research assistants were rigorously trained and supervised on the implementation of the research protocol by a non-MST affiliated co-investigator.
A final limitation pertains to the external validity of the MST interventions and quality assurance protocol. In contrast with other recent MST effectiveness trials (Ogden & Hagen, 2006; Stambaugh et al., 2007; Timmons-Mitchell, Bender, Kishna, & Mitchell, 2006), developers of the MST adaptations for juvenile sexual offenders provided clinical oversight and training in the role of expert consultants. The MST expert consultant role is well defined in the quality assurance system used by MST programs worldwide (Schoenwald, 2008), but this role is not filled by MST developers in dissemination sites. Thus, it remains to be seen through replication studies whether MST teams can achieve the same results when other expert consultants are used. As noted previously, however, the present study is an important step in the dissemination process.
Future Directions
Several directions for future research seem pertinent. First, as reviewers have noted (Chaffin, 2006; Letourneau & Borduin, 2008), few rigorous evaluations have been conducted with juvenile sexual offenders. In light of the wide spread use of group-based, cognitive- behavioral, and relapse prevention approaches, it seems critical that the best specified and most promising of these interventions be evaluated in randomized clinical trials. Continued support for favored interventions should be based on their established effectiveness. Similarly, other comprehensive family-based interventions should be tested to determine their utility with this clinical population.
Second, although the present results and those of other family-based treatments of antisocial behavior have been promising, little is known about the mechanisms by which their favorable outcomes have been achieved (Kazdin, 2007). To address this issue, mediational analyses (Henggeler et al., in press) were recently conducted on the outcomes described in this article. These analyses revealed that changes in caregiver discipline and concern about the youth’s deviant peers were the key mediators of the outcomes. Replication of such findings will be important for determining the most critical factors in reducing antisocial and sexual risk behaviors in adolescents.
Third, program cost is a crucial factor in the decision of fiscal stakeholders to support the adoption of an evidence-based practice. Intensive family- and community-based programs such as MST are likely more costly to implement than community-based group treatment models. However, as described in the Surgeon General’s report on youth violence (U.S. Public Health Service, 2001), family-based approaches can be highly cost effective if they prevent crime and reduce out-of-home placements. The escalating out-of-home placement rates for youth in the TAU-JSO condition and the decreased antisocial behavior of youth in the MST condition suggest possible long-term cost savings, and formal cost analyses currently are being conducted.
In summary, this study presents the first randomized effectiveness trial with juvenile sexual offenders, and, consistent with previous MST efficacy research with this clinical population, the results support the capacity of MST to achieve favorable outcomes pertaining to problem sexual behavior and antisocial behavior. The findings support the viability of comprehensive family-based approaches to treating juvenile sexual offenders and suggest that prevailing group-based approaches warrant closer evaluation.
Acknowledgments
This manuscript was supported by grant R01MH65414 from the National Institute of Mental Health.
We sincerely thank the many families that participated in this project as well as the clinical and research teams including Jessica Jankowski, David Camacho, Carlos Corado, Tresa Taylor, Jennifer Smith Powell, Timothy Snowden, Charles Alexander, Michael Selders, Gaby Adisho, Laura Oddi, Donyetta Jones, and Amy Cullen. The success of this study depended upon close collaboration with the Cook County State’s Attorneys Office, especially Sister Katherine Ryan, Kathleen Bankhead, James McCarter, Margaret Cunningham, Mary Jennings, Lynda Peters, and Joan Pernecke. Finally, we are indebted to professionals at the Circuit Court of Cook County and Juvenile Probation and Court Services. Judge Curtis Heaston permitted the random assignment of youth to treatment conditions. Director Michael J. Rohan, Simon Dmukauskas, Irvin Ashford, and Amanda Halawa-Mahdi provided access to essential treatment information.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at http://www.apa.org/journals/fam/.
Contributor Information
Elizabeth J. Letourneau, Family Services Research Center, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina
Scott W. Henggeler, Family Services Research Center, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina
Charles M. Borduin, Department of Psychological Sciences, University of Missouri
Paul A. Schewe, Department of Criminology, Law, and Justice, University of Illinois at Chicago
Michael R. McCart, Family Services Research Center, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina
Jason E. Chapman, Family Services Research Center, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina
Lisa Saldana, Center for Research to Practice.
References
- Achenbach TM. Youth Self-Report. Burlington: University of Vermont, Research Center for Children, Youth, and Families; 1995. [Google Scholar]
- Achenbach TM. Child Behavior Checklist for ages 6 to 18. Burlington: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Attkinsson CC, Larsen DL, Hargreaves WA, LeVios M, Nguyen TD, Roberts RE, Stegner B. Client Satisfaction Questionnaire—8 (CSQ) In: Rush AJ Jr, Pincus HA, First MB, Blacker D, Endicott J, Keith SJ, Phillips KA, Ryan ND, Smith GR Jr, Tsuang MT, Widiger TA, Zarin DA, editors. Handbook of psychiatric measures. Washington, DC: American Psychiatric Association; 2000. pp. 186–188. [Google Scholar]
- Borduin CM, Henggeler SW, Blaske DM, Stein R. Multisystemic treatment of adolescent sexual offenders. International Journal of Offender Therapy and Comparative Criminology. 1990;34:105–113. [Google Scholar]
- Borduin CM, Letourneau EJ, Henggeler SW, Saldana L, Swenson CC. Treatment manual for Multisystemic Therapy with juvenile sexual offenders and their families. Charleston, SC: Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina; 2005. Unpublished manual. [Google Scholar]
- Borduin CM, Schaeffer CM, Heiblum N. A randomized clinical trial of multisystemic therapy with juvenile sexual offenders: Effects on youth social ecology and criminal activity. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0013035. in press. [DOI] [PubMed] [Google Scholar]
- Butler SM, Seto MC. Distinguishing two types of adolescent sex offenders. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:83–90. doi: 10.1097/00004583-200201000-00015. [DOI] [PubMed] [Google Scholar]
- Caldwell MF. What we do not know about juvenile sexual reoffense risk. Child Maltreatment. 2002;7(4):291–302. doi: 10.1177/107755902237260. [DOI] [PubMed] [Google Scholar]
- Chaffin M. Can we develop evidence-based practice with adolescent sex offenders? In: Longo RE, Prescott DS, editors. Current perspectives: Working with sexually aggressive youth and youth with sexual behavior problems. Holyoke, MA: NEARI Press; 2006. pp. 661–682. [Google Scholar]
- Chaffin M. Our minds are made up: Don’t confuse us with the facts. Child Maltreatment [Special Issue: Children with Sexual Behavior Problems.] 2008;13:110–121. doi: 10.1177/1077559508314510. [DOI] [PubMed] [Google Scholar]
- Chapman DP, Dube SR, Anda RF. Adverse childhood events as risk factors for negative mental health outcomes. Psychiatric Annals. 2007;37:359–364. [Google Scholar]
- Curtis NM, Ronan KR, Borduin CM. Multisystemic treatment: A meta-analysis of outcome studies. Journal of Family Psychology. 2004;18:411–419. doi: 10.1037/0893-3200.18.3.411. [DOI] [PubMed] [Google Scholar]
- Elliott DS (Series Ed.), editor. Blueprints for violence prevention (University of Colorado, Center for the Study and Prevention of Violence) Boulder, CO: Blueprints Publications; 1998. [Google Scholar]
- Elliott DS, Huizinga D, Ageton SS. Explaining delinquency and drug use. Beverly Hills, CA: Sage; 1985. [Google Scholar]
- Ellis DA, Naar-King S, Cunningham PB, Secord E. Use of multisystemic therapy to improve antiretroviral adherence and health outcomes in HIV-infected pediatric patients: Evaluation of a pilot program. AIDS, Patient Care, and STD’s. 2006;20:112–121. doi: 10.1089/apc.2006.20.112. [DOI] [PubMed] [Google Scholar]
- Federal Advisory Committee on Juvenile Justice. Annual report 2007. 2007 Accessed on June 27, 2008 at < http://www.facjj.org/annualreport/ccFACJJ%20Report%20508.pdf>.
- Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation research: A synthesis of the literature. Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute, The National Implementation Research Network (FMHI Publication #231); 2005. [Google Scholar]
- Friedrich WN, Lysne M, Sim L, Shamos S. Assessing sexual behavior in high-risk adolescents with the Adolescent Clinical Sexual Behavior Inventory (ACSBI) Child Maltreatment. 2004;9:239–250. doi: 10.1177/1077559504266907. [DOI] [PubMed] [Google Scholar]
- Fortune C, Lambie I. Sexually abusive youth: A review of recidivism studies and methodological issues for future research. Clinical Psychology Review. 2006;26:1078–1095. doi: 10.1016/j.cpr.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Hanson RK, Gordon A, Harris AJR, Marques JK, Murphy W, Quinsey VL, Seto MC. First report of the collaborative outcome data project on the effectiveness of psychological treatment for sex offenders. Sexual Abuse: A Journal of Research and Treatment. 2002;14:169–194. doi: 10.1177/107906320201400207. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Borduin CM. Multisystemic Therapy Adherence Scales. Charleston, SC: Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina; 1992. Unpublished instrument. [Google Scholar]
- Henggeler SW, Halliday-Boykins CA, Cunningham PB, Randall J, Shapiro SB, Chapman JE. Juvenile drug court: Enhancing outcomes by integrating evidence-based treatments. Journal of Consulting and Clinical Psychology. 2006;74:42–54. doi: 10.1037/0022-006X.74.1.42. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Letourneau EJ, Chapman JE, Borduin CM, Schewe PA, McCart MR. Mediators of change for multisystemic therapy with juvenile sexual offenders. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0013971. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henggeler SW, Pickrel SG, Brondino MJ, Ward D, Rowland MR. Service Utilization Tracking Form II. Charleston, SC: Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina; 1997. [Google Scholar]
- Henggeler SW, Schoenwald SK, Borduin CM, Rowland MD, Cunningham PB. Multisystemic treatment of antisocial behavior in children and adolescents. New York: Guilford Press; 1998. [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kemper TS, Kistner JA. Offense history and recidivism in three victim-age-based groups of juvenile sex offenders. Sexual Abuse: A Journal of Research and Treatment. 2007;19:409–424. doi: 10.1177/107906320701900406. [DOI] [PubMed] [Google Scholar]
- Kernan WN, Viscoli CM, Makuch RW, Brass LM, Horwitz RI. Stratified randomization for clinical trials. Journal of Clinical Epidemiology. 1999;52:19–26. doi: 10.1016/s0895-4356(98)00138-3. [DOI] [PubMed] [Google Scholar]
- Letourneau EJ. A Comment on the First Report. Sexual Abuse: A Journal of Research and Treatment. 2004;16:77–81. doi: 10.1177/107906320401600106. [DOI] [PubMed] [Google Scholar]
- Letourneau EJ, Armstrong K. Recidivism rates for registered and non-registered juvenile sexual offenders. Sexual Abuse: A Journal of Research and Treatment. doi: 10.1177/1079063208324661. in press. [DOI] [PubMed] [Google Scholar]
- Letourneau EJ, Borduin CM. The effective treatment of juveniles who sexually offend: An ethical imperative. Ethics and Behavior [Special Issue: Ethics of Treatment and Intervention Research with Children and Adolescents with Behavioral and Mental Disorders] 2008;18:286–306. doi: 10.1080/10508420802066940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letourneau EJ, Borduin CM, Schaeffer CM. Multisystemic therapy for youth with problem sexual behaviors. In: Beech A, Craig L, Browne K, editors. Assessment and treatment of sexual offenders: A handbook. London: Wiley; in press. [Google Scholar]
- Letourneau EJ, Miner MH. Juvenile sex offenders: A case against the legal and clinical status quo. Sexual Abuse: A Journal of Research and Treatment. 2005;17:313–331. doi: 10.1177/107906320501700304. [DOI] [PubMed] [Google Scholar]
- Letourneau EJ, Resnick HS, Kilpatrick DG, Saunders BE, Best CL. Comorbidity of sexual problems and posttraumatic stress disorder in female crime victims. Behavior Therapy. 1996;27:321–336. [Google Scholar]
- Maas CJM, Hox JJ. Sufficient sample sizes for multilevel modeling. Methodology. 2005;1:86–92. [Google Scholar]
- McEntegart DJ. The pursuit of balance using stratified and dynamic randomization techniques: An overview. Drug Information Journal. 2003;37:293–308. [Google Scholar]
- McGrath RJ, Cumming GF, Burchard BL. Current practices and trends in sexual abuser management: The Safer Society 2002 nationwide survey. Brandon, VT: Safer Society Press; 2003. [Google Scholar]
- Michels S. Should 14-year-olds have to register as sex offenders? 2007 Aug 16; ABC News. Downloaded 12/17/2007 from http://abcnews.go.com/TheLaw/Story?id=3483364&page=1.
- National Institute of Mental Health. Bridging science and service. Author; 1999. NIH Publication No. 99–4353. [Google Scholar]
- Ogden T, Hagen KA. Multisystemic therapy of serious behaviour problems in youth: Sustainability of therapy effectiveness two years after intake. Journal of Child and Adolescent Mental Health. 2006;11:142–149. doi: 10.1111/j.1475-3588.2006.00396.x. [DOI] [PubMed] [Google Scholar]
- Pastore AL, Maguire K, editors. Sourcebook of criminal justice statistics: 31st Edition. 2007. [Online]. Available: http://www.albany.edu/sourcebook/ [August 23, 2007]. [Google Scholar]
- Post LA, Mezey NJ, Maxwell C, Wibert WN. The rape tax: Tangible and intangible costs of sexual violence. Journal of Interpersonal Violence. 2002;17:773–782. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon R, du Toit M. HLM 6: Hierarchical linear and nonlinear modeling [computer software and manual] Lincolnwood, IL: Scientific Software International; 2004. [Google Scholar]
- Reitzel LR, Carbonell JL. The effectiveness of sexual offender treatment for juveniles as measured by recidivism: A meta-analysis. Sexual Abuse: A Journal of Research and Treatment. 2006;18:401–422. doi: 10.1177/107906320601800407. [DOI] [PubMed] [Google Scholar]
- Rescorla LA, Achenbach TM. The Achenbach system of empirically based assessment (ASEBA) for ages 18 to 90 years. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment: Volume 3: Instruments for adults. (3rd ed) Mahwah, NJ: Lawrence Erlbaum Associates; 2004. pp. 115–152. [Google Scholar]
- Ronis ST, Borduin CM. Individual, family, peer, and academic characteristics of male juvenile sexual offenders. Journal of Abnormal Child Psychology. 2007;35:153–163. doi: 10.1007/s10802-006-9058-3. [DOI] [PubMed] [Google Scholar]
- Schoenwald SK. Toward evidence-based transport of evidence-based treatments: MST as an example. Journal of Child and Adolescent Substance Abuse. 2008;17:69–91. [Google Scholar]
- Schoenwald SK, Hoagwood K. Effectiveness, transportability, and dissemination of interventions: What matters when? Psychiatric Services. 2001;52:1190–1197. doi: 10.1176/appi.ps.52.9.1190. [DOI] [PubMed] [Google Scholar]
- Schoenwald SK, Sheidow AJ, Letourneau EJ, Liao JG. Transportability of multisystemic therapy: Evidence for multi-level influences. Mental Health Services Research. 2003;4:223–239. doi: 10.1023/a:1026229102151. [DOI] [PubMed] [Google Scholar]
- Schoenwald SK, Ward DM, Henggeler SW, Pickrel SG, Patel H. MST treatment of substance abusing or dependent adolescent offenders: Costs of reducing incarceration, inpatient, and residential placement. Journal of Child and Family Studies. 1996;5:431–444. [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford: Oxford University Press; 2003. [Google Scholar]
- Snyder HN, Sickmund M. Juvenile offenders and victims: 2006 national report. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Office of Juvenile Justice and Delinquency Prevention; 2006. [Google Scholar]
- St. Amand A, Bard D, Silovsky JF. Treatment of child sexual behavior problems: Practice elements and outcomes. Child Maltreatment [Special Issue: Children with Sexual Behavior Problems.] 2008;13:145–166. doi: 10.1177/1077559508315353. [DOI] [PubMed] [Google Scholar]
- Stambaugh LF, Mustillo SA, Burns BJ, Stephens RL, Baxter B, Edwards D, DeKraai M. Outcomes from wraparound and multisystemic therapy in a center for mental health services system-of-care demonstration site. Journal of Emotional and Behavioral Disorders. 2007;15:143–155. [Google Scholar]
- Stinchfield R, Winters KC. Measuring change in adolescent drug misuse with the Personal Experience Inventory (PEI) Substance Use and Misuse. 1997;32:63–76. doi: 10.3109/10826089709027297. [DOI] [PubMed] [Google Scholar]
- Stroul BA, Friedman RM. A system of care for children and adolescents with severe emotional disturbance. (Rev. ed.) Washington, DC: National Technical Assistance Center for Child Mental Health, Georgetown University Child Development Center; 1996. [Google Scholar]
- Thornberry TP, Krohn MD. The self-report method for measuring delinquency and crime. Criminal Justice. 2000;4:33–83. [Google Scholar]
- Timmons-Mitchell J, Bender MB, Kishna MA, Mitchell CC. An independent effectiveness trial of multisystemic therapy with juvenile justice youth. Journal of Clinical Child and Adolescent Psychology. 2006;35:227–236. doi: 10.1207/s15374424jccp3502_6. [DOI] [PubMed] [Google Scholar]
- U.S. Public Health Service. Youth Violence: A report of the Surgeon General. Washington, DC: Author; 2001. [PubMed] [Google Scholar]
- van Wijk A, Loeber R, Vermeiren R, Pardini D, Bullens R, Doreleijers T. Violent juvenile sex offenders compared with violent juvenile nonsex offenders: Explorative findings from the Pittsburgh Youth Study. Sexual Abuse: A Journal of Research and Treatment. 2005;17:333–352. doi: 10.1177/107906320501700306. [DOI] [PubMed] [Google Scholar]
- Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical and Adolescent Psychology. 2008;37:238–261. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- Walker DF, McGovern SK, Poey EL, Otis KE. Treatment effectiveness for male adolescent sexual offenders: A meta-analysis and review. Journal of Child Sexual Abuse. 2004;13:281–293. doi: 10.1300/j070v13n03_14. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Donenberg GR, Han SS, Weiss B. Bridging the gap between laboratory and clinic in child and adolescent psychotherapy. Journal of Consulting and Clinical Psychology. 1995;63:688–701. doi: 10.1037//0022-006x.63.5.688. [DOI] [PubMed] [Google Scholar]
- Winters KC, Henly G. The Personal Experiences Inventory. Los Angeles: Western Psychological Services; 1989. [Google Scholar]
- Zimring FE. An American travesty: Legal responses to adolescent sexual offending. Chicago, IL: University of Chicago Press; 2004. [Google Scholar]