Abstract
Though split-liver and living-related transplantation are routinely performed, they are done almost exclusively for primary liver transplantation because of potential surgical difficulties. These difficulties are generally related to arterial revascularization, particularly if there is hepatic artery thrombosis. According to UNOS data, of the hepatic retransplantations performed between 1996 and 2007, only 8.7% were done using right or extended right grafts from deceased donors, and 14.3% using right grafts from live donors. Here we report our experience with 5 hepatic retransplantations in which right partial grafts resulting from conventional in situ splits, and one right lobe resulting from an adult-to-adult living-related transplant, were successfully used with different modalities of graft arterialization.
Keywords: Hepatic artery, Liver transplantation, Split liver, Living related transplantation, Hepatic retransplantation
TO THE EDITOR
Hepatic retransplantation (HR) is a major challenge due to inferior results when compared to primary transplantation, ethical questions related to the use of a limited resource, major economic costs, and more demanding surgical techniques[1,2]. Arterial revascularization of a graft can be challenging, especially if hepatic artery thrombosis or vascular abnormalities are present[3,4].
The chronic shortage of cadaveric livers has led surgeons to alternative approaches, namely split-liver[5] and living-related transplantation[6], which are now routinely performed, but almost exclusively for primary liver transplantation.
According to UNOS data, of the HRs performed between 1996 and 2007, only 8.7% were done using right or extended right grafts from deceased donors, and 14.3% using right grafts from live donors[7].
In our institute, as well as in most European centers, both the right lobe from a living donor and the right extended graft from the deceased donor are procured with only the right branch of the hepatic artery for arterial supply. When a right partial graft is transplanted, the need to use the right branch of the hepatic artery instead of the entire hepatic artery, or the celiac trunk, or the aortic patch, can discourage surgeons from considering the possibility of an interposition graft.
Here we report our experience with 5 HRs in which right partial grafts resulting from conventional in situ extended right graft split livers (ERSL), and one right lobe resulting from an adult-to-adult living-related transplant (LRLT) were used.
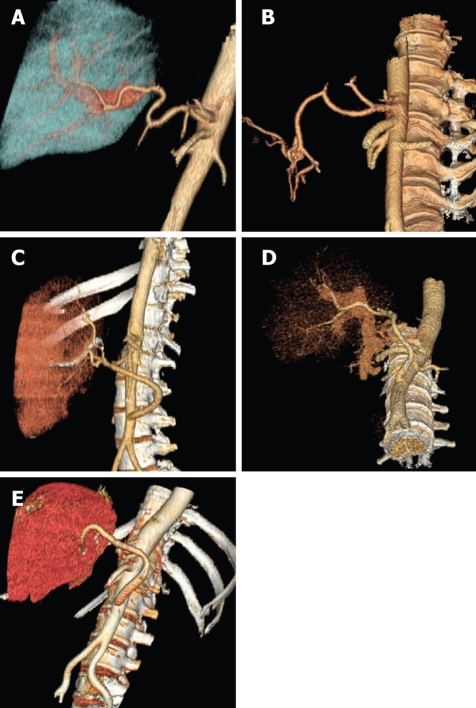
For arterial reconstruction, we used, in the first case, an end-to-end anastomosis between the right branch of the ERSL and the recipient proper hepatic artery in a patient who needed retransplantation after LRLT (Figure 1A). In the second case, we performed an end-to-end anastomosis between the right branch of the ERSL and the recipient splenic artery in a patient transplanted because of hepatic artery thrombosis after LRLT (Figure 1B). In the third case, a living-related transplant involving a patient who had hepatic artery thrombosis after the standard primary transplant, the arterial reconstruction was obtained using a cadaveric donor iliac interposition graft between the infra renal aorta and the right branch of the right lobe (Figure 1C). In the fourth case, an ERSL was used to re-transplant a patient having undergone a standard primary liver transplant. In this case, arterial revascularization was obtained using a cadaveric donor iliac interposition graft between the infra renal aorta and the right branch of the ERSL (Figure 1D). In the last case, after the failure of an LRLT, an ERSL was used, with the need again for a cadaveric donor iliac interposition graft between the infra renal aorta and the right branch of the ERSL (Figure 1E). All the patients here reported received a mean follow-up of 28 mo (3-42) and are alive and free of biliary complications, or required relaparotomy due to graft loss.
Figure 1.
Arterial Reconstruction. A: End-to-end anastomosis between the right branch of the extended right graft split livers (ERSL) and the recipient proper hepatic artery in a patient who needed retransplantation after living-related transplant (LRLT); B: End-to-end anastomosis between the right branch of the ERSL and recipient splenic artery in a patient transplanted because of hepatic artery thrombosis after LRLT; C: Cadaveric donor iliac interposition graft between the infra renal aorta and the right branch of the LRLT in a patient who had hepatic artery thrombosis after the standard primary transplant; D: Arterial revascularization using a cadaveric donor iliac interposition graft between the infra renal aorta and the right branch of the ERSL; E: Cadaveric donor iliac interposition graft between the infra renal aorta and the right branch of the ERSL.
The HR rate in our center is 8.6% out of a total of 580 liver transplants performed since 1999. Recipients are considered candidates for HR if they fit our listing criteria for primary transplantation. During HR, from a technical stand point, we always perform the standard technique with the use of veno-venous bypass. Portal vein and hepatic artery reconstruction are realized according to the vascular anatomy of each single patient. Vessel mismatch is not problematic when a wider iliac graft, which does not require spatulating or modifying in any way the larger artery, is used.
In regions like ours, with a rate of 9.3 cadaveric donor pmp, the chance of using right partial graft gave us the possibility to re-transplant patients that otherwise could not be cured. Although the surgical technique of arterial reconstruction here described is not a novelty, it should be emphasized that right partial grafting for HR achieves good results and allows optimization of a limited resource.
Acknowledgments
The authors thank Warren Blumberg for his help in editing this letter.
Footnotes
Peer reviewer: Mitsuo Shimada, Professor, Department of Digestive and Pediatric Surgery, Tokushima University, Kuramoto 3-18-15, Tokushima 770-8503, Japan; Kazuhiro Hanazaki, MD, Professor and Chairman, Department of Surgery, Kochi Medical School, Kochi University, Kohasu, Okohcho, Nankoku, Kochi 783-8505, Japan
S- Editor Tian L L- Editor Wang XL E- Editor Yin DH
References
- 1.Pfitzmann R, Benscheidt B, Langrehr JM, Schumacher G, Neuhaus R, Neuhaus P. Trends and experiences in liver retransplantation over 15 years. Liver Transpl. 2007;13:248–257. doi: 10.1002/lt.20904. [DOI] [PubMed] [Google Scholar]
- 2.Chen GH, Fu BS, Cai CJ, Lu MQ, Yang Y, Yi SH, Xu C, Li H, Wang GS, Zhang T. A single-center experience of retransplantation for liver transplant recipients with a failing graft. Transplant Proc. 2008;40:1485–1487. doi: 10.1016/j.transproceed.2008.01.076. [DOI] [PubMed] [Google Scholar]
- 3.Nikeghbalian S, Kazemi K, Davari HR, Salahi H, Bahador A, Jalaeian H, Khosravi MB, Ghaffari S, Lahsaee M, Alizadeh M, et al. Early hepatic artery thrombosis after liver transplantation: diagnosis and treatment. Transplant Proc. 2007;39:1195–1196. doi: 10.1016/j.transproceed.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 4.Wang K, Hu S, Jiang X, Zhu M, Jin B. Liver transplantation for patient with variant hepatic artery arising from right renal artery: a case report. Transplant Proc. 2007;39:1716–1717. doi: 10.1016/j.transproceed.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 5.Colledan M, Andorno E, Valente U, Gridelli B. A new splitting technique for liver grafts. Lancet. 1999;353:1763. doi: 10.1016/S0140-6736(99)00661-3. [DOI] [PubMed] [Google Scholar]
- 6.Gruttadauria S, Marsh JW, Cintorino D, Biondo D, Luca A, Arcadipane A, Vizzini G, Volpes R, Marcos A, Gridelli B. Adult to adult living-related liver transplant: report on an initial experience in Italy. Dig Liver Dis. 2007;39:342–350. doi: 10.1016/j.dld.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 7.OPTN data. Available from: URL: http://www.unos.org/data/about/viewDataReports.asp.