Abstract
Objective
The purpose of this study was to analyze the clinical outcome of 75 consecutive patients with cervical carotid artery stenosis and who were treated by carotid artery stenting (CAS) only.
Methods
From February 2003 to June 2008, there were 78 stents placed in 75 symptomatic patients (mean age : 67.3 years); 69 patients had carotid stenosis ≥70%, and 6 patients had asymptomatic stenosis ≥80%. No carotid endarterectomy (CEA) was performed during the same period. The patients were clinically followed-up for a mean of 20.1 months.
Results
The procedures were technically successful in all cases. Three (3.8%) patients had procedure-related complications. During the 30-day postprocedural period, there were no restenosis or major stroke. Minor stroke was noticed in 3 (3.8%) patients and 1 (1.3%) of the 75 patients suddenly expired 2 days after discharge. There were no new neurological symptoms that developed during the clinical follow-up period. The results of our series were not inferior to those the previously published in CAS studies, and in fact they were better.
Conclusion
Our results suggest that CAS may be safe and useful for the treatment of cervical carotid artery stenosis when it is used as the first line treatment in those institutions that lack enough experience with CEA.
Keywords: Carotid artery stenosis, Carotid artery stenting, Carotid endarterectomy, Stroke
INTRODUCTION
Carotid occlusive disease is responsible for 20-25% of all cerebral strokes2,3). Carotid endarterectomy (CEA) has been used to treat extracranial carotid occlusive disease ever since the NASCET showed that the risk of stroke is significantly reduced by CEA as compared to the medical treatment9).
The Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS)2) and the Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy trial (SAPPHIRE)13) suggested that carotid artery stenting (CAS) may have a better outcome than CEA in selected patients. Since the time of these trials, CAS has become a kind of "trend" for treating carotid stenosis. Yet, the recent SPACE trial12) failed to prove the non-inferiority of CAS as compared with CEA, and the EVA-3S trial7) showed that the rates of death and stroke were lower for CEA than for CAS. These results have overturned the current trend for performing CAS so that CEA has again come to the forefront.
Therefore, CEA has been regarded as the treatment of choice for the carotid stenosis while CAS is currently acceptable when it is offered to those patients who have the medical, angiographic and neurological risk factors to undergo CEA.
The guideline11) of American Heart Association/American Stroke Association (AHA/ASA) in 2006 indicates that CAS is a reasonable treatment option when performed by experienced and skilled operators, with established periprocedural morbidity and mortality rates of 4% to 6%. Since we did not have much experience with CEA at our institution, we offered only CAS to all the symptomatic patients or asymptomatic patients (6 patients) with arteriographically defined carotid stenosis ≥70%.
The purpose of this study was to analyze the clinical outcome of 75 consecutive patients with cervical carotid artery stenosis and who were treated by CAS only.
MATERIALS AND METHODS
Patient population
Among the 79 patients (82 arteries) who were treated by CAS between February 2003 and June 2008, the patients who had traumatic dissection (n=4) were excluded. We treated 75 patients (78 arteries) who had carotid artery stenosis by CAS. All the patients displayed symptomatic severe carotid artery stenosis of more than 70% except 6 patients with asymptomatic carotid artery stenosis of more than 80%. No CEA was performed during the same period.
We retrospectively reviewed the 75 patients for their medical conditions, the initial presentation, the angiographic characteristics of carotid artery stenosis with the stenosis ratio, the technical success rate, the procedure-related complications and the clinical outcomes, as assessed by the 30-day morbidity and mortality. Any new neurologic deficits were scored with using the National Institutes of Health Stroke Scale (NIHSS)1). Those patients who had a new neurological event lasting longer than 24 hours with an increase in the NIHSS less than 3 and this resolved completely within 30 days were classified as having a minor stroke. A major stroke was defined as a new neurological event that lasted longer than 24 hours, with an increase in the NIHSS greater than 310). The patients were clinically followed-up for a mean of 20.1 months (range : 2 to 52 months).
Clinical Manifestations
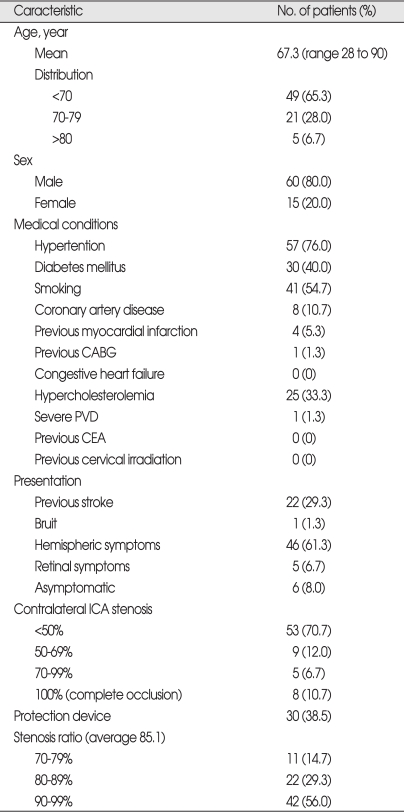
Table 1 summarizes the clinical and radiological characteristics of the 75 patients with severe carotid artery stenosis. Sixty (80.0%) patients were male and their mean age was 67.3 years (age range : 28 to 90 years). Twenty-two (29.3%) patients had a previous stroke and 46 (61.3%) patients initially had hemispheric symptoms, while only 5 (6.7%) had retinal symptoms. The percent ICA stenosis at the lesion side was a mean of 85.1%.
Table 1.
Deomographic characteristics, medical conditions, risk factors, and presenting symptoms of the patients
CABG : coronary artery bypass graft, PVD : perpheral vascular disease, CEA : carotid endarterectomy, ICA
Carotid artery stenting
The patients received clopidogrel (75 mg/day) and aspirin (100 mg/day) for at least 2 weeks before CAS. The procedures were performed under local anesthesia with strict monitoring of the blood pressure. Among the 78 cases, we used an embolic protection device in the 30 more recent cases.
RESULTS
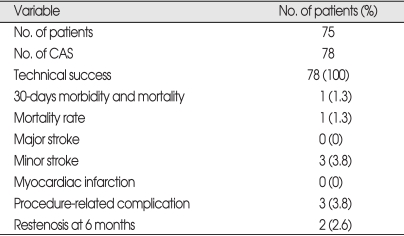
The results of our series are summarized in Table 2. The rate of technical success was 100%. There were 3 (3.8%) procedure-related complications. One patient had asymptomatic multiple small infarctions on MRI, and two patients had distal embolus that were completely recanalized by intraarterial Reopro (Abxicimab) and Urokinase.
Table 2.
Clinical results of carotid artery stenting
CAS : carotid artery stenting
While there was no major stroke and myocardial infarction in our series, minor stroke occurred in 3 (3.8%) patients, and their neurological deficit recovered completely after a few weeks. We had one (1.3%) mortality within 30 days after the procedure. Two days after discharge, the patient suddenly passed away right after complaining of dizziness and the cause of death was uncertain. Restenosis were found in 2 (2.6%) patients at the 6-month follow-up and they were treated by continuing their medications. The patients were symptom free at the time their restenosis were found. At the 12-month follow-up, the restenoses were maintained without aggravation. However, we had one patient who had an in-stent stenosis 23 months after the first CAS. He underwent re-stenting and was discharged without any deficit.
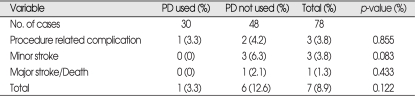
The 30 cases treated with an embolic protection device had a better outcome than did the cases without the protection device (Table 3), even though there was no statistical significance (p=0.122, Student t-test). All the 30-days morbidity and mortality (minor stroke, major stroke and death) occurred in the cases that were treated without the protection device. Also, 2 of the 3 procedure-related complications mentioned above occurred in the patients who didn't have the protection device used in them.
Table 3.
Outcomes according to the use of protection devices
p-value : evaluated by Student t-test. PD : proection device
DISCUSSION
CEA has been used to successfully treat extracranial carotid occlusive disease since the NASCET proved its efficacy in 19919). Although the CAVATAS trial2) and the SAPPHIRE13) trial have helped CAS become a proper treatment option for extracranial carotid artery stenosis, recent studies7,12) have overturned the trend of CAS so that CEA has again come to the forefront. CEA is now regarded as the treatment of choice for carotid stenosis, but many studies have tried to prove that CAS is not inferior to CEA.
Despite of the worldwide trend for performing CEA, our hospital has provided only CAS. Due to the small number of patients with carotid stenosis and our limited exper-ience with CEA, we could not guar-antee a reasonable outcome for CEA with periprocedural morbidity and mortality rates of 4% to 6%11). In such a situation, we have offered CAS to all the symptomatic patients with carotid artery stenosis (≥70%) and to all the asymptomatic patients with carotid artery stenosis ≥80% at our institution no matter what their risk factors are, even though CAS is usually acceptable when it is offered to the patients who have the medical, angiographic, technical and neurological risk factors to perform CEA. We then compared the result of our CAS series to the results from the worldwide published studies of CAS and CEA.
CAVATAS2) is a large, prospective, randomized, multicenter trial that compared CEA to CAS. There was no significant difference in the risk of stroke or death related to the procedure between CEA and CAS. The rate of any stroke lasting more than 7 days or death within 30 days of the first treatment was about 10% in the CEA or CAS groups. The rate of disabling stroke or death within 30 days of the first treatment was 6% in both groups. The SAPPHIRE13) trial randomized 307 high-risk patients to CEA or CAS with using a distal protection device. The perioperative stroke (major stroke and minor stroke) and death rates were 7.3% for CEA versus 4.4% for CAS. The rates of myocardial infarction were 7.3% for surgery versus 2.6% for stenting. In 2001, Roubin et al.10) reported on the results of 604 CAS procedures in 528 patients. The reported rate of technical success was 98%; the procedure related mortality rate (including cardiac death) was 1.6%, the major stroke rate was 1%, the minor stroke rates was 4.8% and the 6-month restenosis rate was 3%. In 2004, Yadav et al.14) reported on the result of CAS in 159 patients. The mortality rate was 0.6% with a minor stroke rate of 3.1%, a major stroke rate of 3.1% and a 12-month restenosis rate of 0.7%.
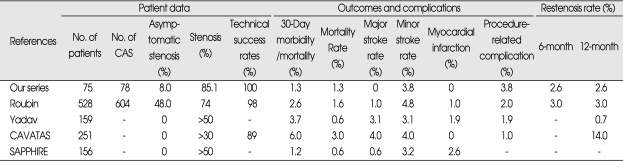
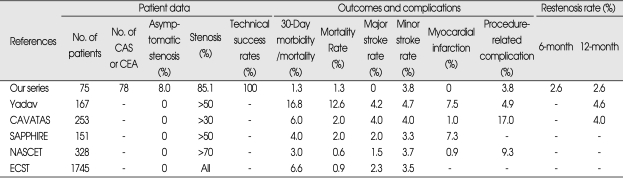
Our results cannot be directly compared with the previously published results because of the non-randomized, single-center, retrospective nature of our study. However, our study does provide evidence that CAS was safely performed at our institution. The morbidity/mortality rate (1.3%) of our series is much better than that of the AHA/ASA guideline's recommendation11), which described that 'CAS is a reasonable treatment option when performed by operators with established periprocedural morbidity and mortality rates of 4% to 6%.' The thirty-day morbidity/mortality rate (1.3%), the restenosis rate (2.6%), the procedure-related complications (3.8%) and myocardial infarction (0%) were similar or quite better in our series as compared to the published results (Table 4). From the comparative analysis, we carefully suggest that CAS may be regarded as a proper treatment option at our institution even though comparative analysis of these reports is made difficult by the inconsistencies in the sample populations, the lesion characteristics, the surgical or endovascular techniques and the outcome data.
Table 4.
Comparison of our series of carotid artery stenting to previously published studies
The result of our CAS series were also compared to the results of the worldwide published studie of CEA2,4,9,13,14) (Table 5). In 1991, NASCET9) performed 328 CEAs in patients with carotid artery stenosis more than 70%. The mortality rate within 30 days was 0.6%, with a major stroke rate of 1.5%. The ECST4) reported favorable results with 1745 symptomatic carotid stenosis patients. The reported rate of 30-day morbidity and mortality was 6.6%. Yadav et al.14) in 2004 reported on the results of 167 CEA procedures in patients with carotid artery stenosis more than 50%. The mortality rate was 12.6% with a minor stroke rate of 4.7%, a major stroke rate of 4.2% and a 12-month restenosis rate of 4.6%.
Table 5.
Comparison of our series of carotid artery stenting to representative series of carotid endarterectomy
The result of our CAS series is better for the 30-day morbidity and mortality rates, the restenosis rate and the procedure-related complications, as compared with the previously reported results of CEA (Table 5), which emphasizes the suitability of CAS as a good treatment option for carotid artery stenosis.
In 2000, Adel et al.6) suggested that CAS may be useful for the treatment of symptomatic cervical carotid stenosis in high-risk patients with severe medical, angiographic and neurological risk factors. Yet, without being deterred by the high-risk factors for CEA or the indications for CAS, we obtained quite good result for treating all the patients with symptomatic carotid artery stenosis with offering CAS only. It would be better to find a proper treatment option for each institution rather than performing unpracticed or unskilled CEA. Thus, CAS could be an adequate treatment option for carotid artery stenosis at our institution. Having had its safety and efficacy proven (reasonable morbidity and mortality) with the operator's increased experience, CAS may become a good option for treating carotid stenosis in high volume medical institutions.
The outcomes for treating carotid stenosis have become better according to the development of new techniques, tools and the operator's accumulated experience. As for the embolic protection device, it helped reduce the periprocedural complications, morbidity and mortality in our series while there are some reported pros5) and cons8) about its efficacy. We obtained better outcomes when the protection device was used (Table 3), but this was not statistically significant. One (4%) of the 25 patients for whom we used the embolic protection device had asymptomatic procedure-related complications, while 6 (14.6%) of the 41 patients who didn't have the device used had procedure-related complications (4.9%), minor stroke (7.3%) and death (2.4%).
CONCLUSION
If CEA doesn't show adequate treatment outcomes due to the lack of experience, then CAS could be the first line treatment for carotid stenosis with reasonable outcomes.
References
- 1.Brott T, Adams HP, Jr, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurement of acute cerebral infarction : a clinical examination scale. Stroke. 1989;20:864–870. doi: 10.1161/01.str.20.7.864. [DOI] [PubMed] [Google Scholar]
- 2.CAVATAS Investigators. Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS) : a randomised trial. Lancet. 2001;357:1729–1737. [PubMed] [Google Scholar]
- 3.Dyken M. In: Stroke Risk Factors in Prevention of Stork. Norris JW, Hachinski VC, editors. New York: Springer-Verlag; 1991. pp. 83–102. [Google Scholar]
- 4.European Carotid Surgery Trialists' Collaborative Group. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST) Lancet. 1998;351:1379–1387. [PubMed] [Google Scholar]
- 5.Katzen BT, Criado FJ, Ramee SR, Massop DW, Hopkins LN, Donohoe D, et al. Carotid artery stenting with emboli protection surveillance study : thirty-day results of the CASES-PMS study. Catheter Cardiovasc Interv. 2007;70:316–323. doi: 10.1002/ccd.21222. [DOI] [PubMed] [Google Scholar]
- 6.Malek AM, Higashida RT, Phatouros CC, Lempert TE, Meyers PM, Smith WS, et al. Stent angioplasty for cervical carotid artery stenosis in high-risk symptomatic NASCET-Ineligible Patients. Stroke. 2000;31:3029–3033. doi: 10.1161/01.str.31.12.3029. [DOI] [PubMed] [Google Scholar]
- 7.Mas JL, Chatellier G, Beyssen B, Branchereau A, Moulin T, Becquemin JP, et al. Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. N Engl J Med. 2006;355:1660–1671. doi: 10.1056/NEJMoa061752. [DOI] [PubMed] [Google Scholar]
- 8.Maynar M, Baldi S, Rostagno R, Zander T, Rabellino M, Llorens R, et al. Carotid stenting without use of balloon angioplasty and distal protection devices : preliminary experience in 100 cases. AJNR Am J Neuroradiol. 2007;28:1378–1383. doi: 10.3174/ajnr.A0543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.North American Symptomatic Carotid Endarterectomy Trial Collborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade stenosis. N Engl J Med. 1991;325:445–453. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 10.Roubin GS, New G, Iyer SS, Vitek JJ, Al-Mubarak N, Liu MW, et al. Immediate and late clinical outcomes of carotid artery stenting in patients with symptomatic and asymptomatic carotid artery stenosis : a 5-year prospective analysis. Circulation. 2001;103:532–537. doi: 10.1161/01.cir.103.4.532. [DOI] [PubMed] [Google Scholar]
- 11.Sacco RL, Adams R, Albers G, Alberts MJ, Benavente O, Furie K, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack : a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke : co-sponsored by the Council on Cardiovascular Radiology and Intervention : the American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37:577–617. doi: 10.1161/01.STR.0000199147.30016.74. [DOI] [PubMed] [Google Scholar]
- 12.SPACE Collaborative Group. Ringleb PA, Allenberg J, Brückmann H, Eckstein HH, Fraedrich G, et al. 30 day results from the SPACE trial of stnet-protected angioplasty versus carotid endarterectomy in symptomatic patients : a randomised non-inferiority trial. Lancet. 2006;368:1239–1247. doi: 10.1016/S0140-6736(06)69122-8. [DOI] [PubMed] [Google Scholar]
- 13.Yadav J. Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy (SAPPHIRE) Chicago, Ill: American Heart Association; 2002. [Google Scholar]
- 14.Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004;351:1493–1501. doi: 10.1056/NEJMoa040127. [DOI] [PubMed] [Google Scholar]