Abstract
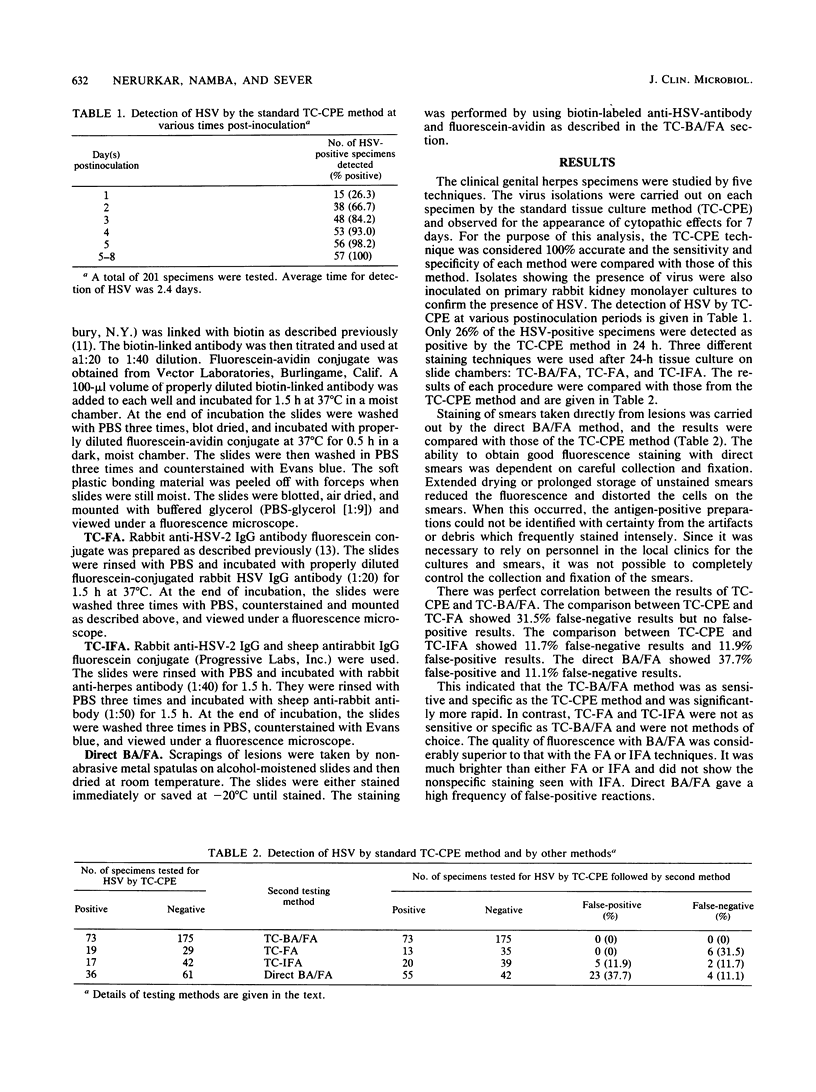
Genital herpes simplex virus infection in women was studied by using conventional tissue culture (TC) virus isolation compared with short-term (24-h) TC on Lab-Tek chamber slides followed by fluorescent-antibody (FA) staining. Three different staining techniques were used after TC: (i) staining with biotin-avidin (TC-BA/FA), (ii) direct FA (TC-FA), and (iii) indirect FA. The TC-BA/FA method showed complete correlation with the TC method. The TC-FA method showed no false-positive results but 31.5% false-negative results compared with the TC method. In contrast, the TC-indirect FA method showed 11.9% false-positive results and 11.7% false-negative results. The direct staining of specimens by the biotin-avidin technique (direct BA/FA) without prior tissue culture showed 37.7% false-positive results and 11.1% false-negative results. The TC-BA/FA technique thus was as sensitive as, but more rapid than, the TC method. The quality of fluorescence was far superior in TC-BA/FA staining as compared with TC-FA or TC-indirect FA procedures. The TC-BA/FA appears to be a valuable technique in laboratory diagnosis of genital herpes infections, especially in clinical situations requiring rapid detection of the virus.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brown S. T., Jaffe H. W., Zaidi A., Filker R., Herrmann K. L., Lylerla H. C., Jove D. F., Budell J. W. Sensitivity and specificity of diagnostic tests for genital infection with herpesvirus hominis. Sex Transm Dis. 1979 Jan-Mar;6(1):10–13. doi: 10.1097/00007435-197901000-00003. [DOI] [PubMed] [Google Scholar]
- Cho C. T., Feng K. K. Sensitivity of the virus isolation and immunofluorescent staining methods in diagnosis of infections with herpes simplex virus. J Infect Dis. 1978 Oct;138(4):536–540. doi: 10.1093/infdis/138.4.536. [DOI] [PubMed] [Google Scholar]
- Gardner P. S., McQuillin J., Black M. M., Richardson J. Rapid diagnosis of herpesvirus hominis infections in superficial lesions by immunofluorescent antibody technics. Br Med J. 1968 Oct 12;4(5623):89–92. doi: 10.1136/bmj.4.5623.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks M. I. Method for the preparation of a herpesvirus hominis fluorescent conjugate for direct immunofluorescence. Arch Gesamte Virusforsch. 1970;32(4):373–378. doi: 10.1007/BF01250065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M. J., Howell C. L. Rapid detection and identification of herpes simplex virus in cell culture by a direct immunoperoxidase staining procedure. J Clin Microbiol. 1983 Sep;18(3):550–553. doi: 10.1128/jcm.18.3.550-553.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller S. E., Lang D. J. Rapid diagnosis of herpes simplex infection: amplification for electron-microscopy by short-term in vitro replication. J Infect. 1982 Jan;4(1):37–41. doi: 10.1016/s0163-4453(82)90959-8. [DOI] [PubMed] [Google Scholar]
- Moseley R. C., Corey L., Benjamin D., Winter C., Remington M. L. Comparison of viral isolation, direct immunofluorescence, and indirect immunoperoxidase techniques for detection of genital herpes simplex virus infection. J Clin Microbiol. 1981 May;13(5):913–918. doi: 10.1128/jcm.13.5.913-918.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nerurkar L. S., Jacob A. J., Madden D. L., Sever J. L. Detection of genital herpes simplex infections by a tissue culture-fluorescent-antibody technique with biotin-avidin. J Clin Microbiol. 1983 Jan;17(1):149–154. doi: 10.1128/jcm.17.1.149-154.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RINDERKNECHT H. Ultra-rapid fluorescent labelling of proteins. Nature. 1962 Jan 13;193:167–168. doi: 10.1038/193167b0. [DOI] [PubMed] [Google Scholar]
- Schmidt N. J., Dennis J., Devlin V., Gallo D., Mills J. Comparison of direct immunofluorescence and direct immunoperoxidase procedures for detection of herpes simplex virus antigen in lesion specimens. J Clin Microbiol. 1983 Aug;18(2):445–448. doi: 10.1128/jcm.18.2.445-448.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt N. J., Gallo D., Devlin V., Woodie J. D., Emmons R. W. Direct immunofluorescence staining for detection of herpes simplex and varicella-zoster virus antigens in vesicular lesions and certain tissue specimens. J Clin Microbiol. 1980 Nov;12(5):651–655. doi: 10.1128/jcm.12.5.651-655.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt N. J., Ho H. H., Chin J. Application of immunoperoxidase staining to more rapid detection and identification of rubella virus isolates. J Clin Microbiol. 1981 Apr;13(4):627–630. doi: 10.1128/jcm.13.4.627-630.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sever J. L., Jacob A. J. Laboratory diagnosis of herpesvirus infections. Semin Perinatol. 1983 Jan;7(1):57–63. [PubMed] [Google Scholar]
- Stagno S., Pass R. F., Reynolds D. W., Moore M. A., Nahmias A. J., Alford C. A. Comparative study of diagnostic procedures for congenital cytomegalovirus infection. Pediatrics. 1980 Feb;65(2):251–257. [PubMed] [Google Scholar]


