Abstract
Objective
We investigated whether European American (EA) and African American (AA) women took longer to lose weight, and were less likely to maintain weight loss if they perceived others to be overweight.
Design
Overweight EA and AA women completed a Figure Rating Scale and the Three-Factor Eating Questionnaire prior to a weight loss intervention. Body composition was assessed by dual energy X-ray absorptiometry prior to and following weight loss.
Main Outcome Measures
rate of weight loss, % body fat at follow-up.
Results
For EA, but not AA women, perception of others’ body size was inversely associated with rate of weight loss and cognitive restraint, and positively associated with body fat gain following intervention. In linear regression modeling, EA, but not AA, women who perceived others as large, subsequently had greater percent body fat one year after weight loss than did those who perceived others as lean, independent of age, baseline body fat, and body size deemed “acceptable”. Inclusion of cognitive restraint in the model weakened this effect.
Conclusion
Among EA but not AA women, perception of others’ body size influenced weight loss and maintenance. This effect may have been mediated by cognitive restraint.
Keywords: Obesity, dieting, weight loss intervention, weight loss maintenance, race
Introduction
The increasing prevalence of obesity may be creating a social perception that overweight body sizes are healthy and appropriate. Indeed, recent epidemiological data suggests that despite an increase in the prevalence of overweight and obesity in recent decades, overweight people have become less likely to perceive themselves as overweight (Johnson-Taylor, Fisher, Hubbard, Starke-Reed, & Eggers, 2008). This change in body size perception may, in turn, exacerbate the obesity epidemic by inhibiting individuals’ motivation to maintain a healthy body weight or to lose excess weight. Evidence supporting this possibility was found in a recent study of a predominantly European American (EA) population, in which individuals were more likely to gain weight over three decades if their same-sex friends were obese (Christakis & Fowler, 2007). Other studies among children and adults support the tenet that peers can affect physical activity levels and caloric intake of individuals (Ball & Crawford, 2006; Keller, Allan, & Tinkle, 2006; Sallis et al., 1989; Salvy et al., 2008), potentially influencing weight status.
Despite this previous research, the extent to which weight loss and the maintenance of normal body weight are affected by one’s perception of the body size of others in general is not known. The mechanism underlying any such association is also unknown, although it may result from differences in dietary restraint. Previous research has shown that overweight people tend to overeat in the presence of another overweight person (de Luca & Spigelman, 1979; Salvy, Romero, Paluch, & Epstein, 2007), and so it is possible that those who perceive overweight body sizes as normal or acceptable, and who are susceptible to weight gain themselves, are less likely to restrict their own food intake and thus, become overweight. It is also not known whether this phenomenon might be evident across all ethnic groups. It is possible that the perception of others’ body size plays a role in weight loss and maintenance only among the EA population because EA women in particular, tend to be more dissatisfied with their body size, with increased drive to be thin, than are African American (AA) women (Roberts, Cash, Feingold, & Johnson, 2006; Wilfley et al., 1996). On the other hand, the association between perception of others’ size and weight loss or maintenance might also be present among AA women for whom larger body sizes are more accepted (Becker, Yanek, Koffman, & Bronner, 1999; DiGioacchino, Sargent, & Topping, 2001).
The purpose of this study was to investigate whether women’s perception of the body size of others was associated with weight loss, and successful maintenance of weight loss. We hypothesized that women who perceived other women their own age as overweight would experience a slower rate of weight loss during a structured weight loss program, and have more body fat one year following the intervention, than those who perceived others as less overweight. In addition, we hypothesized that these associations between the perception of others’ body size and weight loss and maintenance success would be present for both EA and AA women.
Methods
This investigation was conducted in women enrolled in a weight loss and weight loss maintenance study. At the time of enrollment, the women were moderately overweight (BMI 27-30 kg/m2), premenopausal (22-46 years), and of EA or AA ancestry. Race was self-defined, and those selected for inclusion also had parents and grandparents of the same race. Table 1 outlines the body composition and baseline psychometric characteristics of the participants. Women lost weight via diet restriction alone (investigator-provided 800 kcal/day) or diet restriction combined with structured exercise, until they obtained a BMI <25 kg/m2. During the 1-year follow-up period, participants were encouraged, but not mandated, to attend regular support group meetings and to continue with their exercise program, if applicable.
Table 1. Characteristics of study population (mean ± SEM).
| European American | African American | t | P value | |
|---|---|---|---|---|
| Baseline | ||||
| N | 60 | 60 | ||
| Age | 34.47 ± 0.84 | 35.03 ± 0.79 | -0.481 | 0.631 |
| BMI (kg/m2) | 28.20 ± 0.17 | 28.19 ± 0.15 | 0.030 | 0.977 |
| Body weight (kg) | 78.44 ± 1.07 | 78.79 ± 0.78 | 1.261 | 0.210 |
| Body fat (%) | 44.06 ± 0.48 | 42.44 ± 0.47 | 2.426 | 0.017 |
| Body fat (kg) | 34.35 ± 0.74 | 32.34 ± 0.51 | 2.231 | 0.028 |
| Perceived self body size | 5.52 ± 0.08 | 5.02 ± 0.09 | 4.127 | <0.001 |
| Ideal body size | 3.18 ± 0.08 | 3.02 ± 0.06 | 1.740 | 0.085 |
| “Acceptable” body size | 3.56 ± 0.09 | 3.28 ± 0.08 | 2.253 | 0.026 |
| Perceived size of other women | 4.07 ± 0.13 | 4.34 ± 0.13 | -1.488 | 0.140 |
| Discrepancy between size of self vs. others | 1.45 ± 0.14 | 0.68 ± 0.16 | 3.581 | <0.001 |
| Cognitive restraint | 15.52 ± 0.48 | 16.98 ± 0.41 | -2.331 | 0.021 |
| Intervention | ||||
| Weight loss (kg) | 12.33 ± 0.33 | 11.53 ± 0.27 | 1.889 | 0.061 |
| Rate of loss (kg/day) | 0.102 ± 0.006 | 0.084 ± 0.005 | 2.258 | 0.026 |
| 1-year post-intervention1 | ||||
| Weight gain (kg) | 5.06 ± 0.56 | 5.78 ± 0.57 | -0.895 | 0.373 |
| Fat mass gain (kg) | 4.12 ± 0.77 | 6.08 ± 0.46 | 1.730 | 0.026 |
| Body fat (%) gained | 4.24 ± 0.54 | 5.98 ± 0.37 | -2.730 | 0.008 |
| Body fat (%) | 38.22 ± 0.84 | 38.15 ± 0.40 | 0.060 | 0.952 |
| Body fat (kg) | 26.95 ± 0.98 | 26.99 ± 0.73 | -0.034 | 0.973 |
N = 45 EA and 53 AA.
At baseline, before weight loss, study participants were administered the Stunkard Figure Rating Scale (Stunkard, Sorenson, & Schulsinger, 1983). Women were asked to select a number from 1 (leanest) to 9 (largest), representing different body sizes, to identify their self-perceived current body size, and their ideal body size. In addition, they were asked “Which body size resembles most females your own age?” and “When you see people at school, at the mall, or on the beach, what body sizes do you think look O.K? Write down the numbers of the body sizes that you think are acceptable.” The participants also completed the 18-item revised Three-Factor Eating Questionnaire (TFEQ-R; (Karlsson, Persson, Sjöström, & Sullivan, 2000), which has been shown to be valid for the general population (de Lauzon et al., 2004). This questionnaire provides an estimate of cognitive restraint (i.e. how much individuals consciously restrict their intake), along with measures of uncontrolled and emotional eating. For the purposes of this study, data from only the cognitive restraint subscale was included because we did not hypothesize that uncontrolled and emotional eating would alter the relationship between perception of others’ body size and weight loss/regain. At baseline, immediately following weight loss, and at 1-year post-weight loss, their body composition was assessed by dual-energy X-ray absorptiometry (DXA; Prodigy, GE-Lunar, Madison, Wisconsin).
For statistical analysis, women were divided into two groups based on race (EA, AA). Race differences in body size perceptions, cognitive restraint, and body composition were assessed by t-test. Pearson correlation analysis was used to identify associations between body size perceptions and body composition. Multiple linear regression analysis was used to determine whether perception of others’ body size predicted rate of weight loss (calculated as grams of body weight lost during intervention divided by the number of days to achieve the weight loss goal) and percent body fat at 1-year following weight loss. To illustrate the differences in cognitive restraint, rate of weight loss, and percent body fat exhibited by those who perceive other women to be leaner versus larger, women were grouped into extremes according to how lean (1-3) or large (5-8; no participant reported 9 as the size of other women) they perceived others to be, and t-tests were conducted on these extreme subgroups within each race. All analyses were conducted using SPSS version 12.0.
Results
Characteristics of the study population are presented in Table 1. By study design, EA and AA women had the same BMI at baseline. AA women had less fat mass and thus, less percent body fat than the EA women. AA women perceived themselves as smaller, and reported smaller body sizes as more “acceptable” than did EA women. Although the groups did not differ on the size they perceived others to be, on average, both groups perceived others to be smaller than they perceived themselves to be. The difference between EA women’s perception of their own size and that of others was more than double that of AA women. On the TFEQ-R, AA women reported greater cognitive restraint than did EA women. During the intervention, AA women lost weight more slowly than did EA women, taking an average of 163 days to achieve a BMI < 25 mkg/m2, compared to the average 140 days taken by EA women (p=0.07). One year following the intervention, data was unavailable from 22 of the women, leaving 53 EA and 45 AA women. There were no significant differences in the key variables of interest between the women who remained in the study versus those who left the study, with the exception of rate of weight loss which was faster for AA women who remained in the study compared with those who left. Among the women who completed the study, AA women gained almost 2 kg more fat mass in the year following the weight loss intervention and thus, a greater percentage of body fat, than EA women.
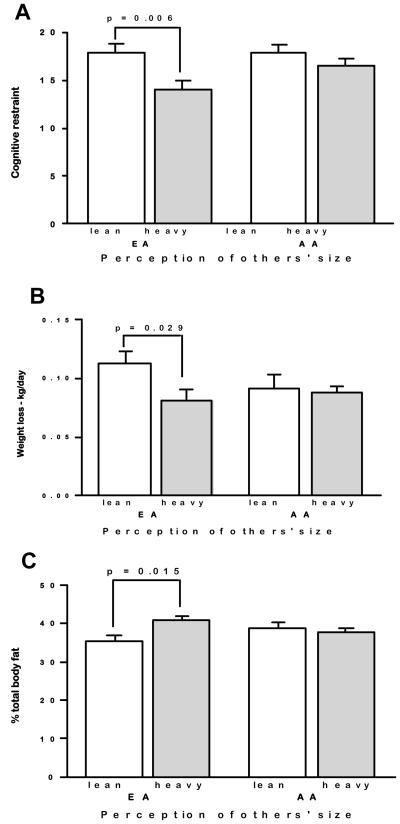
Pearson correlation analysis revealed that the perception of the body size of others was inversely associated with rate of weight loss and positively associated with percent fat gain, and total percent body fat in the year following the intervention, for EA women only. EA women who perceived others as overweight lost weight more slowly and gained more percent body fat during the year following the intervention, resulting in greater percent body fat at follow-up than EA women who perceived others to be less overweight (Table 2). In addition, EA women who perceived other women as overweight reported less cognitive restraint. When only the extreme scores of the range of figures were considered, EA women who perceived others as overweight reported less cognitive restraint, lost weight at a slower rate, and had greater percent body fat one year following weight loss (Figure 1), than did those who perceived other women as less overweight. The outcomes and characteristics did not differ by AA women’s perceptions.
Table 2. Pearson correlation coefficients for outcome variables with self-reported perception of other women’s size.
| European American | African American | ||
|---|---|---|---|
| Baseline | BMI | -0.016 | -0.116 |
| Percent total body fat | -0.165 | -0.213 | |
| Dietary restraint | -0.3821 | -0.175 | |
| Intervention | Total weight lost (kg) | -0.192 | -0.012 |
| Rate of weight loss | -0.2822 | -0.012 | |
| 1-year follow-up | Change in body weight (kg) | 0.2923 | 0.133 |
| Change in % total body fat | 0.3422 | 0.105 | |
| % total body fat | 0.2893 | -0.155 |
p< 0.01
p< 0.05
0.05>p>0.10
Figure 1.
Differences in cognitive restraint (A; EA lean n=16, EA heavy n=17; AA lean n=10, AA heavy n=24), rate of weight loss during the intervention (B; EA lean n=16, EA heavy n=17; AA lean n=10, AA heavy n=24), and one-year follow-up percent body fat (C; EA lean n=13, EA heavy n=11; AA lean n=9, AA heavy n=22) of EA and AA women who perceived others as lean (rated 1-3) or heavy (rated 5-8) at baseline.
Multiple linear regression analyses indicated that although baseline percent body fat was the strongest predictor of percent body fat one year following weight loss, after adjusting for baseline percent fat, age, and body size deemed “acceptable”, the perceived size of others remained a significant predictor of percent body fat one year following weight loss, for EA women (Table 3, Model 1). Based on a partial correlation of 0.354, results indicate that 12.5% of the variance in percent body fat at follow-up was explained by EA women’s perceptions of the body size of other women. In comparison, for AA women, only 0.2% of the variance in percent body fat at follow-up was explained by the women’s ratings of the perceived size of others. When cognitive restraint was added to the model, the perception of others’ size lost significance as a predictor of percent body fat (Table 3, Model 2). In multiple regression analysis perception of others’ body size was not associated with rate of weight loss.
Table 3. Multiple linear regression models for the dependent variable “percent total body fat at follow-up”.
| Model variables | Intercept | Slope | Model r | Standardized β | p |
|---|---|---|---|---|---|
| Model 1: | |||||
| EA women | -5.101 | 0.658 | <0.001 | ||
| Age | 0.075 | 0.086 | 0.530 | ||
| Baseline % total body fat | 0.886 | 0.507 | <0.001 | ||
| “Acceptable” body size | -1.420 | -0.190 | 0.161 | ||
| Perceived size of other women | 1.739 | 0.310 | 0.021 | ||
| AA women | -4.863 | 0.725 | <0.001 | ||
| Age | 0.106 | 0.131 | 0.255 | ||
| Baseline % total body fat | 0.936 | 0.705 | <0.001 | ||
| “Acceptable” body size | 0.125 | 0.015 | 0.880 | ||
| Perceived size of other women | -0.198 | -0.040 | 0.733 | ||
| Model 2: Includes cognitive restraint | |||||
| EA women | 3.824 | 0.674 | <0.001 | ||
| Age | 0.055 | 0.063 | 0.646 | ||
| Baseline % total body fat | 0.814 | 0.466 | 0.001 | ||
| “Acceptable” body size | -1.452 | -0.194 | 0.149 | ||
| Perceived size of other women | 1.429 | 0.255 | 0.068 | ||
| Cognitive restraint | -0.235 | -0.165 | 0.224 | ||
| AA women | -3.778 | 0.726 | <0.001 | ||
| Age | 0.111 | 0.137 | 0.244 | ||
| Baseline % total body fat | 0.938 | 0.706 | <0.001 | ||
| “Acceptable” body size | 0.081 | 0.010 | 0.924 | ||
| Perceived size of other women | -0.236 | -0.048 | 0.693 | ||
| Cognitive restraint | -0.060 | -0.037 | 0.724 | ||
Discussion
This study extends previous findings regarding the association between peer relationships and weight control (e.g. (Ball & Crawford, 2006; Christakis & Fowler, 2007)) to show that an individual’s general perception of others’ body size may influence progress and success in a structured weight loss and weight loss maintenance program. Results were specific for EA women, suggesting that cultural factors affect environmental influences on body weight regulation. These observations have important implications for both obesity research and clinical practice.
The mechanism underlying the association between the perception of others’ body size and success with weight loss may have been cognitive restraint. We observed that when cognitive restraint was added to the regression model, the association between perception of others’ body size and percent body fat one year after the intervention was weakened. This may indicate that women who perceived others as overweight may have been less willing or able to restrict their own food intake, and thus were more likely to regain body fat. Due to the correlational nature of this data, future research will be important to ascertain whether food intake patterns are indeed different for women who perceive others as being overweight versus those who perceive others as normal weight.
If differences in dietary restraint do underlie the relationship between perception of others’ size and weight gain, this may indicate an important role for social cues on appropriate meal size. For example, previous research has found that people are more likely to overeat if others sharing the meal are themselves overeating (Conger, Conger, Costanzo, Wright, & Matter, 1980; Herman, Roth, & Polivy, 2003), and studies of adults and children have found that overweight people will eat more if their meal companion is also overweight (de Luca & Spigelman, 1979; Salvy et al., 2007). It is plausible that this social facilitation effect during meals might extend to a general obesity-promoting lifestyle. In this way, women who perceive others as being overweight may view larger body sizes as the “norm”, feel less social pressure to be lean, and therefore have less dietary restraint. It is also possible that the perception of others’ body size served as a proxy measure for aspects of the environment that affect weight control, analogous to what has been observed for drug addiction (Drummond, 2000). In both cases, environmental cues may trigger deleterious behavior.
We observed a race difference in the relationship between perception of others’ body size and percent fat at one year follow-up, such that this association was observed only within EA women. This race difference may reflect cultural factors that affect behavioral regulation of body weight. Within EA women, drive for thinness is reported to affect weight loss behavior (Ard, Greene, Malpede, & Jefferson, 2007), while among AA women, ability to lose weight is limited by lack of social support (Baturka, Hornsby, & Schorling, 2000), a cultural belief in self-acceptance regardless of body size (Baturka et al., 2000), and practical issues such as food preparation and education regarding healthy diets (Ard et al., 2007). A race difference in drive for thinness is supported by the fact that in this study, EA women reported a greater discrepancy between their own body size and that of others, than did AA women. Results of the current study therefore, support the possibility that the perceived size of others may be a less important motivator for weight loss among AA women as compared to EA women.
An important strength of this study was to follow the women through both an investigator-managed weight loss program, insuring the participants achieved the goal weight, and then through the following year, when many of the women regained some weight. In doing so, we were able to investigate the effect of body size perception on both weight loss and weight maintenance. This study was also strengthened by the use of DXA to measure body fat at each time point, as opposed to simple body weight and indirect measures of body composition. Limitations of this study however, include the relatively small and homogenous sample population, inhibiting the generalizability of these results, and the fact that the primary analyses were correlational. Future studies will be important to determine who serves as a passive influence toward an individual’s weight control, and the mechanism through which this influence transpires into weight gain or maintenance.
The results of this study implicate a potential role for social perception on body weight regulation by suggesting that the mere perception of overweight as common in the general society may itself sabotage weight loss and weight maintenance success. The implication of this finding for public health is that the increasing prevalence of obesity may be facilitating weight gain amongst individuals, thereby exacerbating the obesity epidemic. A further implication for obesity researchers is to consider the importance of the social and cultural environment when designing weight loss interventions. For some populations, such as EA women, a successful intervention may need to ascertain the extent to which each individual perceives overweight body sizes as normal, and work with participants to counteract the potentially detrimental behavioral consequences of this perception.
Acknowledgements
This research was in part supported by National Institute of Health grant RO1 DK 51684-10, and General Clinical Research Center grant M01 RR-00032. No financial conflicts exist. We would like to thank Nikki Bush, Jessica Alvarez, Krista Casazza, and Pedro del Corral, for their editorial assistance; and Paul Zuckerman, Betty Darnell, and Bob Petri, for their technical assistance.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at http://www.apa.org/journals/hea/
REFERENCES
- Ard JD, Greene LC, Malpede CZ, Jefferson WK. Association between body image disparity and culturally specific factors that affect weight in Black and White women. Ethn Dis. 2007;17(suppl 2):34–39. [PubMed] [Google Scholar]
- Ball K, Crawford D. An investigation of psychological, social and environmental correlates of obesity and weight gain in young women. Int J Obes (Lond) 2006;30(8):1240–1249. doi: 10.1038/sj.ijo.0803267. [DOI] [PubMed] [Google Scholar]
- Baturka N, Hornsby PP, Schorling JB. Clinical implications of body image among rural African-American women. J Gen Intern Med. 2000;15:235–241. doi: 10.1111/j.1525-1497.2000.06479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker DM, Yanek LR, Koffman DM, Bronner YC. Body image preferences among urban African Americans and whites from low income communities. Ethn Dis. 1999;9(3):377–386. [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Conger JC, Conger AJ, Costanzo PR, Wright KL, Matter JA. The effect of social cues on the eating behavior of obese and normal subjects. J Pers. 1980;48(2):258–271. doi: 10.1111/j.1467-6494.1980.tb00832.x. [DOI] [PubMed] [Google Scholar]
- de Lauzon B, Romon M, Deschamps V, Lafay L, Borys JM, Karlsson J, et al. The Three-Factor Eating Questionnaire-R18 is able to distinguish among different eating patterns in a general population. J Nutr. 2004;134(9):3272–2380. doi: 10.1093/jn/134.9.2372. [DOI] [PubMed] [Google Scholar]
- de Luca RV, Spigelman MN. Effects of models on food intake of obese and non-obese female college students. Can J Behav Sci. 1979;11:124–129. [Google Scholar]
- DiGioacchino RF, Sargent RG, Topping M. Body dissatisfaction among White and African American male and female college students. Eat Behav. 2001;2(1):39–50. doi: 10.1016/s1471-0153(00)00022-2. [DOI] [PubMed] [Google Scholar]
- Drummond DC. What does cue-reactivity have to offer clinical research? Addiction. 2000;95(Suppl 2):S129–144. doi: 10.1080/09652140050111708. [DOI] [PubMed] [Google Scholar]
- Herman CP, Roth DA, Polivy J. Effects of the presence of others on food intake: a normative interpretation. Psychol Bull. 2003;129(6):873–886. doi: 10.1037/0033-2909.129.6.873. [DOI] [PubMed] [Google Scholar]
- Johnson-Taylor WL, Fisher RA, Hubbard VS, Starke-Reed P, Eggers PS. The change in weight perception of weight status among the overweight: comparison of NHANES III (1988-1994) and 1999-2004 NHANES. Int J Behav Nutr Phys Act. 2008;5:9. doi: 10.1186/1479-5868-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson J, Persson LO, Sjöström L, Sullivan M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. Int J Obes Relat Metab Disord. 2000;24(12):1715–1725. doi: 10.1038/sj.ijo.0801442. [DOI] [PubMed] [Google Scholar]
- Keller C, Allan J, Tinkle MB. Stages of change, processes of change, and social support for exercise and weight gain in postpartum women. J Obstet Gynecol Neonatal Nurs. 2006;35(2):232–240. doi: 10.1111/j.1552-6909.2006.00030.x. [DOI] [PubMed] [Google Scholar]
- Roberts A, Cash TF, Feingold A, Johnson BT. Are black-white differences in females’ body dissatisfaction decreasing? A meta-analytic review. J Consult Clin Psychol. 2006;74(6):1121–1131. doi: 10.1037/0022-006X.74.6.1121. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Hovell MF, Hofstetter CR, Faucher P, Elder JP, Blanchard J, et al. A multivariate study of determinants of vigorous exercise in a community sample. Prev Med. 1989;18(1):20–34. doi: 10.1016/0091-7435(89)90051-0. [DOI] [PubMed] [Google Scholar]
- Salvy SJ, Bowker JW, Roemmich JN, Romero N, Kieffer E, Paluch R, et al. Peer Influence on Children’s Physical Activity: An Experience Sampling Study. J Pediatr Psychol. 2008;33(1):39–49. doi: 10.1093/jpepsy/jsm039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvy SJ, Romero N, Paluch R, Epstein LH. Peer influence on pre-adolescent girls’ snack intake: effects of weight status. Appetite. 2007;49(1):177–182. doi: 10.1016/j.appet.2007.01.011. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Sorenson TI, Schulsinger F. Use of the Danish Adoption Register for the study of obesity and thinness. In: Kety S, Rowland LP, Sidman RL, Matthysse SW, editors. The Genetics of Neurological and Psychiatric Disorders. Raven Press; New York: 1983. pp. 115–120. [PubMed] [Google Scholar]
- Wilfley DE, Schreiber GB, Pike KM, Striegel-Moore RH, Wright DJ, Rodin J. Eating disturbance and body image: a comparison of a community sample of adult black and white women. Int J Eat Disord. 1996;20(4):377–387. doi: 10.1002/(SICI)1098-108X(199612)20:4<377::AID-EAT5>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]