Abstract
Background
Excessive kyphosis may be associated with earlier mortality, but previous studies have not controlled for clinically silent vertebral fractures that are a known mortality risk factor.
Objective
To determine whether hyperkyphosis predicts increased mortality independent of vertebral fractures.
Design
Prospective cohort study.
Setting
Four clinical centers in Baltimore County, Maryland; Portland, Oregon; Minneapolis, Minnesota; and the Monongahela Valley, Pennsylvania.
Patients
610 women, aged 67-93 years, from a cohort of 9704 women recruited from community-based listings between 1986 and 1988.
Measurements
Kyphosis was measured using a flexicurve. Prevalent radiographic vertebral fractures at baseline were defined by morphometry, and mortality was assessed during an average follow-up of 13.5 years.
Results
In age-adjusted models, each SD increase in kyphosis carried a 1.14-fold increased risk of mortality (95% C.I.: 1.02-1.27, p = 0.02). After adjusting for age and other predictors of mortality including osteoporosis related factors such as low bone density, moderate and severe prevalent vertebral fractures, and number of prevalent vertebral fractures, women with greater kyphosis were at increased risk for earlier mortality (Relative hazard per SD increase: 1.15; 95% C.I.: 1.01-1.30, p = 0.03). Upon stratification by prevalent vertebral fracture status, only women with prevalent fractures were at increased mortality risk from hyperkyphosis, independent of age, self-reported health, smoking, spine bone mineral density, number of vertebral fractures, and severe vertebral fractures (Relative hazard per SD increase: 1.58; 95% CI: 1.06 - 2.35, p = 0.02).
Limitations
The study population only included Caucasian women.
Conclusions
We conclude that in older women with vertebral fractures, hyperkyphosis predicts an increased risk of mortality, independent of underlying spinal osteoporosis and the extent and severity of vertebral fractures.
Introduction
It is well known that vertebral fractures are associated with an increased risk of mortality in older persons(1-4), but the explanation for why vertebral fractures may lead to an increased mortality risk is unknown. Our previous work suggested that those with vertebral fractures were more likely to die from a pulmonary cause, in particular, and we postulated that this might be because of vertebral fracture induced changes in the thoracic kyphotic curvature that could detrimentally affect respiratory function(2). In that paper, we performed a sub-analysis that demonstrated that older women with the worst degrees of thoracic hyperkyphosis were more likely to die from a pulmonary cause; however, only one third of those with the greatest kyphotic curvatures had evidence of underlying vertebral fractures(2). While this study provided a plausible mechanism by which vertebral fractures might lead to mortality, it also suggested that non-osteoporotic kyphosis may also be associated with adverse health.
Some studies have suggested that hyperkyphosis itself may be a risk factor for mortality(5, 6). However, these studies were unable to assess whether it was the increased thoracic curvature itself or the presence of clinically undetected vertebral fractures that were the underlying explanation of the apparent association between hyperkyphosis and increased mortality risk. Therefore, to test whether hyperkyphosis is associated with an increased risk of mortality independent of vertebral fractures and low bone mineral density, we conducted a prospective cohort study of 610 older women who had measures of kyphosis, bone mineral density, and morphometric vertebral fractures, and assessed mortality rates over an average follow-up of 13.5 years.
Methods
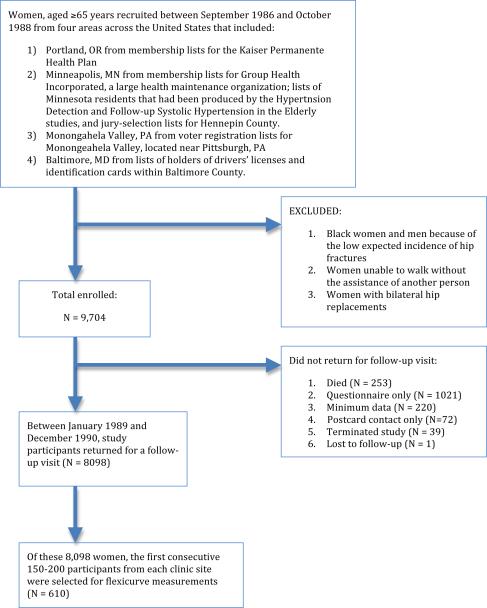
Study participants were from the Study of Osteoporotic Fractures, an ongoing prospective study of risk factors for fractures and other health outcomes. Between 1986-1988, 9,704 community-dwelling women aged 65 years or older were recruited from various population-based listings in Baltimore, MD; Minneapolis MN; Portland, OR; and the Monongahela Valley, PA(7). During the year two follow-up visit, 610 women, representing all four clinic centers, were consecutively sampled to undergo flexicurve measurements to document the degree of thoracic curvature, known as the kyphosis index. The details of the original cohort study design and the sampling of the women for the purposes of the kyphosis study are depicted in a flow diagram (Figure 1). The institutional review boards at each clinical site approved the study protocol, and written informed consent was obtained from all participants.
Figure 1.
Study Flow Diagram
Flexicurve measurement of kyphosis
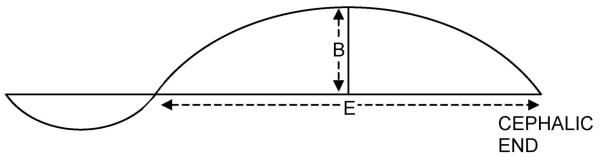
Originally developed for study in the 1970's, an architect's flexicurve was used to measure kyphosis during the second clinic examination. Examiners placed the flexible ruler against the subject's back while standing erect, with the upper end placed just below the C7 spinous process, and the lower end just at the S2 spinous process. The outline of the curve was then captured using a handheld digital scanner, and xy coordinates computed to derive: 1) a reference line between curve ends; 2) distance from origin to first intersection of the curve with the reference line defining the vertical length of the upper back curve; and 3) maximum horizontal distance from the upper back curve to the reference line (Figure 2). The kyphosis index is defined as 100 times the maximum horizontal distance divided by the vertical length of the upper back curve (8). All technicians underwent teaching of the measurement at the centralized coordinating center. To assess reproducibility, two technicians from each clinic site performed the flexicurve measurement in a separate sample comprising 75 women selected from the Study of Osteoporotic Fractures cohort. After the tracings were obtained at the four clinical centers, they were sent to the coordinating center for centralized readings. The coefficient of variation for replicate kyphosis index values was 12.6%, and the Pearson correlation coefficient between the paired measurements was 0.66 (8). In addition, as a second check of validity, 20 tracings were selected from the study sample, two from each decile of kyphosis index, and two independent observers were asked to rank the tracings visually by order of kyphosis severity. The Spearman correlation coefficient between the visual rankings of the tracings by two observers was 0.89, and the correlations between the ranking of observers and ranking of kyphosis index were 0.943 (observer 1) and 0.931 (observer 2) (8).
Figure 2.
Flexicurve measurement calculation: the index of thoracic curvature, or the kyphosis index (KI), is 100 times the maximum horizontal distance divided by the vertical length of the upper back curve (B/E X 100). Adapted from Milne and Lauder (5).
Vertebral morphometry measurements
At the baseline visit in 1986-1988, radiographs of the thoracic and lumbar spine were obtained in accordance with the 1995 National Osteoporosis Foundation guidelines(9). Using visual triage, trained technicians separated radiographs into normal, uncertain, or probably fractured groups based upon a semiquantitative grading scheme that categorized a subject by the most abnormal vertebral level(10, 11). The study radiologist further categorized those classified as uncertain as normal or probably fractured. Those classified as probably fractured were then evaluated by morphometry using six-point digitization to calculate the anterior (Ha), mid- (Hm), and posterior (Hp) heights for each vertebral body from T4 to L4. For each vertebral level, three height ratios were calculated (Ha/Hp, Hm/Hp, and Hp/Hp±1 or Ha/Ha±1), and a vertebra was classified as having a prevalent fracture if any of the three height ratios were more than 3 SDs below the study population-specific mean for that level(12). A severe prevalent fracture was defined if any of the three height ratios were more than 4 SDs below the study population-specific mean for that level.
Incident Vertebral Fracture Assessment
Incident vertebral fractures were defined if any of three vertebral height ratios decreased by more than 20% and by at least 4mm compared with the baseline films on repeat radiographs taken an average of 4.2 years after the initial assessment of prevalent vertebral fractures. The study radiologist reviewed the morphometrically defined incident vertebral fractures to exclude imaging artifacts or conditions such as Scheuermann disease, and reclassified 7% as not having an incident fracture. In a random sample of 503 women selected from the original study cohort whose radiographs were triaged and then digitized, triage missed no incident fractures according to the study definition.
Questionnaire and Examination
All study participants completed a comprehensive baseline and more limited second follow-up questionnaire that included questions about demographics (age and education), medical history, and health behaviors. Whenever possible, data obtained from the second visit were used to best correspond with the timing of the kyphosis index measurement. Baseline measures included a family history of osteoporosis, self-reported spine fractures, stroke, self-reported health status, physical activity, and detailed questions about alcohol use. Information obtained from the second visit questionnaire included data about age and cigarette use. At the baseline and second clinic examination, height and weight were measured, and weight change was calculated as the difference in weight between baseline and the 2nd follow-up visit. Body mass index was calculated as the weight in kilograms divided by the height in square meters. At the second examination, participants were tested to see if they could stand from a chair five times without using their arms and they were also asked to perform a tandem stand. Also at the second examination, total hip and spine bone mineral density were measured using dual-energy X-ray absorptiometry (QDR 1,000, Hologic, Inc., Waltham, MA). Details of bone density measurements and quality control procedures have been previously published (13).
Ascertainment of Death
Participants were contacted by mail or telephone every 4 months. The study follow-up for vital statistics was 95% complete as of August 2007. All deaths were confirmed by receipt of death certificates.
Statistical analysis
Because kyphosis is strongly associated with vertebral fractures, a known mortality risk factor, and this study aims to disentangle the ill health effect of vertebral fractures from kyphosis, we compared the characteristics of women by prevalent vertebral fracture status using chi-squared for dichotomous variables or Student's t tests for continuous measures.
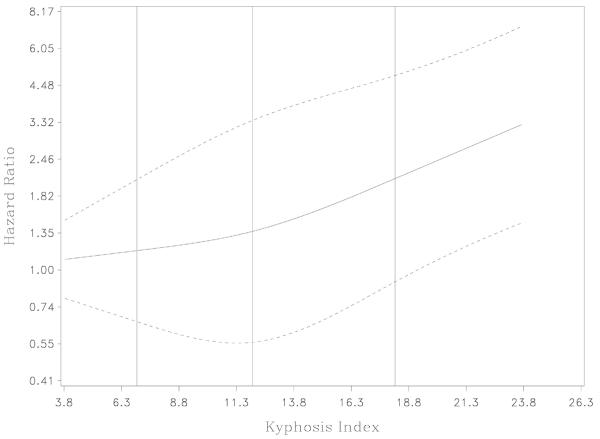
After confirming the assumption that the hazards rates were proportional, we used Cox proportional hazards models to determine the association between kyphosis index and all-cause mortality. All results are reported as relative hazards (HR) with 95 % confidence intervals (CI). We first used non-parametric regression modeling with spline transformation to assess the nature of the relation (linear versus non-linear) between kyphosis index and mortality, using Harrell's (1991) SAS Macro %Psplinet (http://biostat.mc.vanderbilt.edu/twiki/pub/Main/SasMacros/survrisk.txt)(14). Since the relationship appeared close to linear, we chose to conduct proportional hazards regression with kyphosis index as a continuous predictor.
We first performed age-adjusted proportional hazards models of kyphosis index as a continuous predictor of all-cause mortality. After adjusting for age and kyphosis, we considered each demographic, health behavior and physical performance variable in association with mortality. In building the multivariable models, we next included known mortality risk factors, adjusting for health status (self-reported health: very good or excellent versus very poor, poor, or fair), health behavior (current smoker versus past or never), and spinal osteoporosis (spinal bone mineral density, the presence of any prevalent vertebral fracture). To remove any residual confounding by spinal osteoporosis, we added number (range 0-10, assessed 2.2 (SD = 0.2) years before the kyphosis index), and severity of vertebral fractures to the model. Stroke, physical activity/performance are potential confounders of the kyphosis-mortality association but might also be in the causal pathway from kyphosis to mortality. Therefore, we added the following variables to the model at the end: stroke (self-reported yes/no), amount of weight lost between the baseline and 2nd clinic visit (per SD), and the ability to stand from a chair five times without the use of the arms (yes/no). We tested for effect modification by prevalent vertebral fracture by including an interaction term between kyphosis and prevalent vertebral fracture in an age-adjusted model. Finally, we ran the multivariable analyses stratified by baseline vertebral fracture. We used SAS software (15) to perform all analyses.
Role of the Funding Source
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the National Institute on Aging (NIA) provided funding for the study, but played no role in the data analysis, data interpretation, or manuscript preparation.
Results
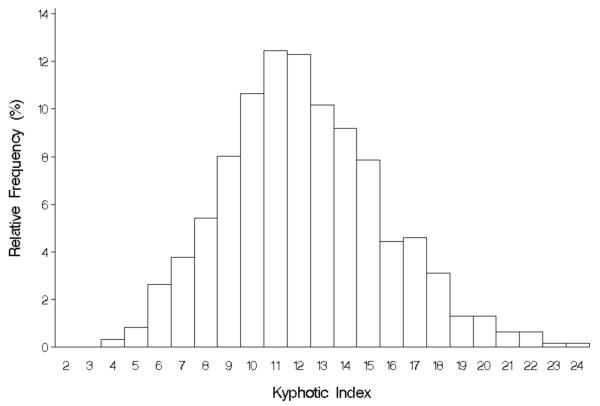
The baseline characteristics between women with and without radiographically detected prevalent vertebral fractures were similar except that women with vertebral fractures were more likely to have lower spine and hip bone density, to report a history of spine fracture, and to develop an incident vertebral fracture (Table 1). Kyphosis index was normally distributed, with a mean index of 12.3 and standard deviation 3.4 (Figure 3). Over an average follow-up of 13.5 years (median follow-up 15 years), 317 women died. The association between kyphosis and the log hazard of mortality (in non-parametric regression using spline transformation) was close to being linear (Figure 4), justifying the use of kyphosis index as a continuous predictor in proportional hazards regression.
Table 1.
Characteristics of all women, and by prevalent vertebral fracture status*
| Characteristic | All women N = 610 | Women with prevalent vertebral fracture N = 95 | Women without prevalent vertebral fracture N = 510 | P value |
|---|---|---|---|---|
| Age (years), mean ± SD | 72.8 ± 4.7 | 73.3 ± 4.7 | 72.8 ± 4.7 | 0.38 |
| Education (> 12 yrs), % | 38.0 | 45.3 | 36.7 | 0.11 |
| Body mass index (kg/m2), mean ± SD | 26.4 ± 4.8 | 26.5 ± 4.4 | 26.4 ± 4.9 | 0.90 |
| Physical activity (kcal/wk), mean ± SD | 1510 ±1402 | 1407 ± 1293 | 1547 ± 1425 | 0.37 |
| Self-reported good/excellent health status, % | 82.8 | 83.2 | 82.9 | 0.96 |
| History of stroke, % | 2.5 | 3.2 | 2.4 | 0.65 |
| Smoking (current), % | 8.9 | 12.6 | 7.9 | 0.13 |
| Alcohol use (# per week), mean ± SD | 2.0 ± 4.1 | 2.1 ± 5.0 | 2.0 ± 3.9 | 0.76 |
| Spine bone mineral density (g/cm2), mean ± SD | 0.85 ± 0.16 | 0.78 ± 0.15 | 0.86 ± 0.16 | <0.001 |
| Hip bone mineral density (g/cm2), mean ± SD | 0.76 ± 0.13 | 0.69 ± 0.12 | 0.78 ± 0.13 | <0.001 |
| Self-reported prevalent spine fracture, % | 6.5 | 19.4 | 3.9 | <0.001 |
| Morphometric incident vertebral fracture, % | 5.0 | 16.3 | 2.7 | <0.001 |
| Chair stand without arms, % | 97.6 | 95.8 | 98.0 | 0.21 |
| Weight change 2 yrs prior to study (kg), mean ± SD | -0.62 ± 3.92 | -0.41 ± 4.43 | -0.68 ± 3.83 | 0.54 |
| Death, % | 52.0 | 47.4 | 52.8 | 0.34 |
Of note, 5 of 610 participants were left out of the analyses because they did not have baseline radiographs of acceptable quality to determine whether or not a prevalent vertebral fracture was present.
Figure 3.
Distribution of kyphosis index among 610 older women (histogram)
Figure 4.
In age-adjusted proportional hazards models, each standard deviation increase in kyphosis index was associated with a 1.14-fold increased risk of all cause-mortality (95% C.I.: 1.02-1.27, p = 0.02). After considering each demographic, health behavior, and physical performance variable in conjunction with kyphosis, age, and risk of mortality, only age, self-reported health, history of stroke, physical activity, inability to rise from a chair 5 times without using the arms, and total hip bone mineral density were statistically significantly associated with an increased risk of mortality. Based upon these results and underlying biologic plausibility, we created several different multivariable models. The first considered the basic variables associated with mortality, but not factors that would be likely to be in the causal pathway between kyphosis and mortality (Table 2). In models adjusted for age, self-reported health, smoking, spine bone mineral density, and the presence of any prevalent vertebral fractures, there was a 1.17-fold increased risk of all-cause mortality with each standard deviation increase in kyphosis index (adjusting for hip instead of spine bone mineral density: relative hazard = 1.16; 95% C.I.: 1.03 - 1.30, p = 0.01). Adding related factors that might fall along the causal pathway such as stroke, physical activity, weight loss, and chair stand did not materially change the results (Table 2).
Table 2.
The multivariable association between kyphosis index and mortality, adjusted for vertebral fractures by number and severity, bone mineral density, and other factors
| Model, with relative hazards representing kyphosis, per SD | Relative Hazards (95% Confidence interval) | P value |
|---|---|---|
| Age-adjusted | 1.14 (1.02 - 1.27) | 0.02 |
| Adjusted for age, self-reported health, smoking, lumbar spine bone mineral density, any prevalent vertebral fracture | 1.17 (1.04 - 1.32) | 0.009 |
| Adjusted for age, self-reported health, smoking, lumbar bone mineral density, any prevalent vertebral fracture, physical activity, stroke, weight loss, chair stand | 1.17 (1.04 - 1.33) | 0.01 |
| Adjusted for age, self-reported health, smoking, lumbar bone mineral density, any prevalent vertebral fracture, physical activity, stroke, weight loss, chair stand, severe vertebral fracture, number of prevalent vertebral fractures | 1.15 (1.01 - 1.30) | 0.03 |
Since vertebral fractures have been previously associated with an increased risk of mortality(1-4), to better capture (and remove any residual confounding by) the overall vertebral fracture burden, we added the number of vertebral fractures as well as an indicator of more severe vertebral fractures in the same multivariable model and found no noteworthy change in the overall results (Table 2). As incident vertebral fractures have also been associated with increased mortality(16, 17), we also adjusted for incident vertebral fractures, but the results were unchanged (data not shown).
To further explore the question as to whether kyphosis itself in the absence of vertebral fractures predicts mortality, we tested for and found a strong suggestion of an interaction between kyphosis, prevalent vertebral fractures, and mortality (p = 0.06). We therefore performed further analyses stratified by prevalent vertebral fracture status. In age-adjusted analyses, hyperkyphosis in women without prevalent vertebral fractures was no longer statistically significantly associated with increased mortality (relative hazard per SD = 1.09; 95% CI: 0.97-1.22, p = 0.17). On the other hand, in women with underlying vertebral fractures, with each standard deviation increase in kyphosis index, the risk of mortality increased 1.5 fold (Table 3). Further adjustment for self-reported health, smoking, and lumbar bone mineral density, severe vertebral fractures, and number of vertebral fractures made little difference in the relative hazards (Table 3).
Table 3.
The multivariable association between kyphosis index and mortality, including only women with prevalent vertebral fractures (n = 95)
| Model, with relative hazards representing kyphosis, per SD | Relative Hazards (95% Confidence interval) | P value |
|---|---|---|
| Age-adjusted | 1.50 (1.11 - 2.03) | 0.009 |
| Adjusted for age, self-reported health, smoking, lumbar spine bone mineral density | 1.77 (1.23 - 2.55) | 0.002 |
| Adjusted for age, self-reported health, smoking, lumbar bone mineral density, severe vertebral fracture, and number of prevalent vertebral fractures | 1.58 (1.06 - 2.35) | 0.02 |
Discussion
In older women with previous vertebral fractures, increased kyphosis predicts increased risk for all-cause mortality, independent of the extent and severity of the underlying spinal osteoporosis. To date, most clinicians and patients attribute their hyperkyphotic posture to underlying osteoporosis; however, these data confirm that postural changes provide important clinical predictive ability that is not provided by markers of osteoporosis alone. Our results suggest that women with vertebral fractures and hyperkyphosis are at greater risk for mortality than women with either only vertebral fractures or only hyperkyphosis.
Other large epidemiologic studies have demonstrated that kyphotic posture may be associated with worse health including impaired pulmonary function, poor physical function, inferior quality of life, injurious falls, fractures, and mortality (6, 18-20), but none to date have been able to fully account for the possibility that undiagnosed vertebral fractures may be the underlying cause. Multiple previous studies have demonstrated that clinically apparent and silent vertebral fractures themselves are associated with worse health outcomes. Our results do indicate that underlying vertebral fractures are an important cause of kyphosis associated mortality given that among those women without vertebral fracture, there was no association between kyphosis and mortality. However, our findings substantiate the idea that it is not enough to look for vertebral fractures alone, the degree of kyphosis has additional predictive value that is not captured by the presence, severity, and number of vertebral fractures.
By what mechanisms might postural change affect mortality? Our previous work and that of others has demonstrated an association between hyperkyphosis and compromised pulmonary function and pulmonary death (2,16, 21). Certainly, muscle weakness, poor physical functional capability, and falls might be other plausible mechanisms by which kyphosis could lead to subsequent increased mortality. In our exploratory analyses, the inability to stand up five times without using one's arms and a history of stroke were associated both with kyphosis and mortality, but adjustment for these factors did not diminish the kyphosis-mortality association.
We postulate that the phenotype of hyperkyphosis is an easily assessable clinical marker of accelerated physiologic aging or frailty. While chronologic age is a strong predictor of functional decline and mortality, frailty or advanced physiologic age may be a more powerful predictor of adverse health among older persons. Hyperkyphosis may be a good marker of at least one category of a frail phenotype, and if so, it may prove to be an important clinical marker that to date has largely been ignored.
Our study had some limitations. Recent studies have demonstrated that hyperkyphosis not only affects older women, but also men (21), and only white women were included in the present study so these results are not generalizable to men or non-white women. Also, the morphometric reading of vertebral fractures is based upon vertebral height ratios only, and therefore, may lead to misclassification of other causes of decrements in height ratios (i.e. such as Scheurmann's disease). For that reason, we also included a variable of self-reported spine fractures, but found that adjustment for clinically reported vertebral fractures also did not affect the association between hyperkyphosis and increased mortality in this cohort. A third limitation is the difference in timing of the different variables, namely the timing of assessment of vertebral fractures and of kyphosis. Given that average progression of kyphosis in the overall cohort was only about 6.7 degrees over 15 years of follow-up (23), the difference of 2.2 years in the timing of measurements likely made little difference in our results. Finally, the correlation between kyphosis index and either the kyphosis angle or clinical measures of the distance from occiput-to-wall are not known so it is hard to make clinically relevant comparisons; however, each measure has been shown to have construct validity, and the flexicurve may even be superior to those that depend upon specific vertebral edges such as the more widely used Cobb angle. Our study also had several strengths. First, this was a prospective study with substantial long-term and 95 % complete follow-up over 13.5 years. Second, all women underwent standardized testing for underlying vertebral fractures so that this study did not have the limitation of previous studies that couldn't exclude underlying vertebral fractures as a mechanism of the association of hyperkyphosis and ill health.
In summary, we have demonstrated that in older women with previous vertebral fractures, independent of the number and severity of vertebral fractures, hyperkyphosis is associated with an increased risk of mortality. These study results add to a growing literature that suggests that hyperkyphosis is a clinically important finding. Because it is readily observed and is associated with ill health in older persons, hyperkyphosis should be recognized as a geriatric syndrome, i.e., a “multifactorial health condition that occurs when the accumulated effect of impairments in multiple systems renders a person vulnerable to situational challenges.”(22)
Acknowledgements
None.
Grant support: The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the National Institute on Aging (NIA) under the following grant numbers: AG05407, AR35582, AG05394, AR35584, AR35583, R01 AG005407, R01 AG027576-22, 2 R01 AG005394-22A1, 2 R01 AG027574-22A1, 1K12AG01004, and 1R01 AG024246.
Footnotes
Publisher's Disclaimer: This is the prepublication, author-produced version of a manuscript accepted for publication in Annals of Internal Medicine. This version does not include post- acceptance editing and formatting. The American College of Physicians, the publisher of Annals of Internal Medicine, is not responsible for the content or presentation of the author-produced accepted version of the manuscript or any version that a third party derives from it. Readers who wish to access the definitive published version of this manuscript and any ancillary material related to this manuscript (e.g., correspondence, corrections, editorials, linked articles) should go to www.annals.org or to the print issue in which the article appears. Those who cite this manuscript should cite the published version, as it is the official version of record.
References
- 1.Cooper C, Atkinson EJ, Jacobsen SJ, O'Fallon WM, Melton LJ., 3rd Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993;137(9):1001–5. doi: 10.1093/oxfordjournals.aje.a116756. [DOI] [PubMed] [Google Scholar]
- 2.Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159(11):1215–20. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 3.Ismail AA, O'Neill TW, Cooper C, et al. Mortality associated with vertebral deformity in men and women: results from the European Prospective Osteoporosis Study (EPOS) Osteoporos Int. 1998;8(3):291–7. doi: 10.1007/s001980050067. [DOI] [PubMed] [Google Scholar]
- 4.Ensrud KE, Thompson DE, Cauley JA, et al. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc. 2000;48(3):241–9. doi: 10.1111/j.1532-5415.2000.tb02641.x. [DOI] [PubMed] [Google Scholar]
- 5.Milne JS, Williamson J. A longitudinal study of kyphosis in older people. Age Ageing. 1983;12(3):225–33. doi: 10.1093/ageing/12.3.225. [DOI] [PubMed] [Google Scholar]
- 6.Kado DM, Huang MH, Karlamangla AS, Barrett-Connor E, Greendale GA. Hyperkyphotic posture predicts mortality in older community-dwelling men and women: a prospective study. J Am Geriatr Soc. 2004;52(10):1662–7. doi: 10.1111/j.1532-5415.2004.52458.x. [DOI] [PubMed] [Google Scholar]
- 7.Cummings SR, Black DM, Nevitt MC, et al. Appendicular bone density and age predict hip fracture in women. The Study of Osteoporotic Fractures Research Group. JAMA. 1990;263(5):665–8. [PubMed] [Google Scholar]
- 8.Ettinger B, Black DM, Palermo L, Nevitt MC, Melnikoff S, Cummings SR. Kyphosis in older women and its relation to back pain, disability and osteopenia: the study of osteoporotic fractures. Osteoporos Int. 1994;4:55–60. doi: 10.1007/BF02352262. [DOI] [PubMed] [Google Scholar]
- 9.Kiel D. Assessing vertebral fractures. National Osteoporosis Foundation Working Group on Vertebral Fractures. J Bone Miner Res. 1995;10(4):518–23. doi: 10.1002/jbmr.5650100403. [DOI] [PubMed] [Google Scholar]
- 10.Genant HK, Engelke K, Fuerst T, et al. Noninvasive assessment of bone mineral and structure: state of the art. J Bone Miner Res. 1996;11(6):707–30. doi: 10.1002/jbmr.5650110602. [DOI] [PubMed] [Google Scholar]
- 11.Genant HK, Jergas M, Palermo L, et al. Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis The Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1996;11(7):984–96. doi: 10.1002/jbmr.5650110716. [DOI] [PubMed] [Google Scholar]
- 12.Black DM, Palermo L, Nevitt MC, et al. Comparison of methods for defining prevalent vertebral deformities: the Study of Osteoporotic Fractures. J Bone Miner Res. 1995;10(6):890–902. doi: 10.1002/jbmr.5650100610. [DOI] [PubMed] [Google Scholar]
- 13.Steiger P, Cummings SR, Black DM, Spencer NE, Genant HK. Age-related decrements in bone mineral density in women over 65. J Bone Miner Res. 1992;7(6):625–32. doi: 10.1002/jbmr.5650070606. [DOI] [PubMed] [Google Scholar]
- 14.Harrell FE, Jr., Lee KL, Pollock BG. Regression models in clinical studies: determining relationships between predictors and response. J Natl Cancer Inst. 1988;80(15):1198–202. doi: 10.1093/jnci/80.15.1198. [DOI] [PubMed] [Google Scholar]
- 15.SAS/STAT® Statistical Analysis Software program] SAS Institute Inc.; [Google Scholar]
- 16.Kado DM, Duong T, Stone KL, et al. Incident vertebral fractures and mortality in older women: a prospective study. Osteoporos Int. 2003;14(7):589–94. doi: 10.1007/s00198-003-1412-5. [DOI] [PubMed] [Google Scholar]
- 17.Pongchaiyakul C, Nguyen ND, Jones G, Center JR, Eisman JA, Nguyen TV. Asymptomatic vertebral deformity as a major risk factor for subsequent fractures and mortality: a long-term prospective study. J Bone Miner Res. 2005;20(8):1349–55. doi: 10.1359/JBMR.050317. [DOI] [PubMed] [Google Scholar]
- 18.Kado DM, Huang MH, Barrett-Connor E, Greendale GA. Hyperkyphotic posture and poor physical functional ability in older community-dwelling men and women: the Rancho Bernardo study. J Gerontol A Biol Sci Med Sci. 2005;60(5):633–7. doi: 10.1093/gerona/60.5.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kado DM, Huang MH, Nguyen CB, Barrett-Connor E, Greendale GA. Hyperkyphotic posture and risk of injurious falls in older persons: the Rancho Bernardo Study. J Gerontol A Biol Sci Med Sci. 2007;62(6):652–7. doi: 10.1093/gerona/62.6.652. [DOI] [PubMed] [Google Scholar]
- 20.Huang MH, Barrett-Connor E, Greendale GA, Kado DM. Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J Bone Miner Res. 2006;21(3):419–23. doi: 10.1359/JBMR.051201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kado DM, Prenovost K, Crandall C. Narrative review: hyperkyphosis in older persons. Ann Intern Med. 2007;147(5):330–8. doi: 10.7326/0003-4819-147-5-200709040-00008. [DOI] [PubMed] [Google Scholar]
- 22.Tinetti ME, Williams CS, Gill TM. Dizziness among older adults: a possible geriatric syndrome. Ann Intern Med. 2000;132(5):337–44. doi: 10.7326/0003-4819-132-5-200003070-00002. [DOI] [PubMed] [Google Scholar]