Sir,
We recently read a paper published by Bolignano et al. who investigated the association between urinary levels of neutrophil gelatinase-associated lipocalin (Ngal) and severity of renal disease in proteinuric patients [1]. Urinary Ngal is largely and rapidly increased during courses of acute kidney injury (AKI), making it especially useful for early diagnosis of AKI [2–5], but its clinical impact on chronic kidney disease (CKD) remains elusive. They studied non-diabetic patients having >1 g/day of proteinuria at least for 6 months and also healthy subjects, and reported that urinary Ngal concentrations were significantly associated with the extent of proteinuria, and inversely with the estimated glomerular filtration rate. The group also revealed in another study that the elevated urinary Ngal level was a predictor of CKD progression [6].
Our team has also evaluated the correlation between urinary Ngal levels and clinical parameters in CKD patients and observed similar findings. Since the response of urinary Ngal levels to treatment has not been analysed well, here we carried out a prospective observational study. We chose a cohort of 26 hypertensive patients having either diabetes (n = 2), obesity (15) or both (9), and treated them with angiotensin receptor blockers (ARBs). They included 15 males and 11 females who had ages of 55.5 ± 3.0 years (mean ± SEM), body mass index of 32.8 ± 1.2 kg/m2, serum creatinine of 0.82 ± 0.06 mg/dl and estimated glomerular filtration rate of 79.1 ± 6.5 ml/min/ 1.73 m2 (calculated by a Japanese formula revised in year 2009 [7]). Ten healthy volunteers were also studied: 6 males and 4 females with a mean age of 55.7 years. Clinical parameters including urinary Ngal were examined before and 3 months after initiation of the treatment. Hypertension was defined as systolic blood pressure (BP) ≥ 140, diastolic BP ≥ 90 mmHg or taking antihypertensive reagents. Diabetes was determined as blood HbA1c level ≥6.5%. Subjects with a body mass index ≥25 kg/m2 were considered obese. Patients neither took any other inhibitors of the renin–angiotensin system, nor were given altered oral regimen during the course. ARBs were chosen from candesartan 12 mg, olmesartan 20 mg or telmisartan 40 mg by the treating physician's preference (n = 14, 7 or 5, respectively). The study was carried out in subjects followed at outpatient clinics of Kyoto University Hospital and Kyoto Medical Center, and was approved by ethical committees in those institutes. Patients gave written informed consent.
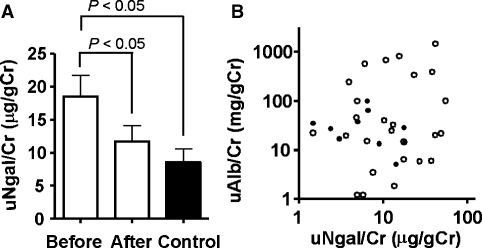
Before administration of ARBs, hypertensive patients had significantly elevated urinary Ngal levels as compared to healthy controls (Figure 1A). After 3 months of treatment, mean BP was reduced from 158 ± 3/92 ± 2 to 143 ± 2/82 ± 2 mmHg (n = 26, P < 0.001). All three ARBs similarly decreased systolic and diastolic BP by ∼10% (supplementary Table S1). At the same time, urinary excretion of both Ngal and albumin was decreased by 36% (Figure 1A) and 46%, respectively. A similar trend was observed when patients were divided into ones having normoalbuminuria, microalbuminuria or macroalbuminuria (n = 14, 6 or 6, respectively; supplementary Table S2). Of note, urinary Ngal and albumin concentrations before ARB treatment were not significantly correlated with each other (Figure 1B, P > 0.05), suggesting that these two measurements may reflect independent aspects of renal disorders, especially when the level of proteinuria is not very severe.
Fig. 1.
Urinary Ngal and albumin levels in hypertensive patients having either obesity or diabetes. (A) Mean (±SEM) urinary Ngal/urinary creatinine ratios (uNgal/Cr) in patients before and 3 months after treatment with angiotensin receptor blockers, as well as in healthy controls. Comparison was carried out by paired and unpaired t-tests. (B) No significant correlation was observed between urinary Ngal and urinary albumin excretion (uAlb/Cr) before the treatment in patients with hypertension (open circles, n = 26), when analysed with or without healthy controls (closed circles, n = 10), by linear regression analysis.
To our knowledge, this is the first report to show that short-term administration of ARBs significantly reduced urinary Ngal levels in human subjects. Consistently, we have recently observed that ARBs suppressed urinary excretion of Ngal in diabetic mice induced by streptozotocin (STZ) [8]. The concentrations of Ngal were much higher in STZ diabetic mice than human subjects investigated in this study, which may be explained by the difference in the extent of hyperglycaemia and by the species difference concerning Ngal protein metabolism. Furthermore, the treatment of nephrotic patients with steroids and other immune suppressants immediately reduced urinary Ngal excretion [8]. These findings warrant intensive research concerning usefulness of urinary Ngal as a monitoring marker of CKD.
Supplementary Material
Acknowledgments
This work was in part supported by grant from the Japan Kidney Foundation.
Conflict of interest statement. None declared.
Supplementary data
Supplementary data is available online at http://ndt.oxfordjournals.org.
References
- 1.Bolignano D, Coppolino G, Campo S, et al. Urinary neutrophil gelatinase-associated lipocalin (NGAL) is associated with severity of renal disease in proteinuric patients. Nephrol Dial Transplant. 2008;23:414–416. doi: 10.1093/ndt/gfm541. [DOI] [PubMed] [Google Scholar]
- 2.Mori K, Lee HT, Rapoport D, et al. Endocytic delivery of lipocalin-siderophore-iron complex rescues the kidney from ischemia-reperfusion injury. J Clin Invest. 2005;115:610–621. doi: 10.1172/JCI23056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mishra J, Dent C, Tarabishi R, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005;365:1231–1238. doi: 10.1016/S0140-6736(05)74811-X. [DOI] [PubMed] [Google Scholar]
- 4.Mori K, Nakao K. Neutrophil gelatinase-associated lipocalin as the real-time indicator of active kidney damage. Kidney Int. 2007;71:967–970. doi: 10.1038/sj.ki.5002165. [DOI] [PubMed] [Google Scholar]
- 5.Coca SG, Yalavarthy R, Concato J, et al. Biomarkers for the diagnosis and risk stratification of acute kidney injury: a systematic review. Kidney Int. 2008;73:1008–1016. doi: 10.1038/sj.ki.5002729. [DOI] [PubMed] [Google Scholar]
- 6.Bolignano D, Lacquaniti A, Coppolino G, et al. Neutrophil gelatinase-associated lipocalin (NGAL) and progression of chronic kidney disease. Clin J Am Soc Nephrol. 2009;4:337–344. doi: 10.2215/CJN.03530708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matsuo S, Imai E, Horio M, et al. Revised equations for estimating GFR from serum creatinine in Japan. Am J Kid Dis. doi: 10.1053/j.ajkd.2008.12.034. (2009 Epub) [DOI] [PubMed] [Google Scholar]
- 8.Kuwabara T, Mori K, Mukoyama M, et al. Urinary neutrophil gelatinase-associated lipocalin levels reflect damage to glomeruli, proximal tubules, and distal nephrons. Kidney Int. 2009;75:285–294. doi: 10.1038/ki.2008.499. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.