Abstract
Introduction
The longitudinal ITC Scotland/U.K. survey was used to investigate adult smokers’ support for smoke-free legislation and whether this support was associated with higher quit intentions at follow-up, either directly or indirectly, via the mediation of perceived social unacceptability of smoking.
Methods
Structural equation modeling was employed to compare differences between the two samples (507 adult smokers from Scotland and 507 from the rest of the United Kingdom) across two waves (February/March 2006 and March 2007). During these two waves, a smoking ban was introduced in Scotland but not the rest of the United Kingdom.
Results
For smokers in both samples, support for smoke-free legislation at baseline significantly heightened perceived unacceptability of smoking, although perceptions of unacceptability were somewhat stronger in Scotland than the rest of the United Kingdom postban. Unlike the rest of the United Kingdom, support for a ban at baseline among smokers in Scotland was associated with higher quit intentions at follow-up. For both samples, quit intentions were significantly associated with heightened perceived unacceptability at follow-up. The overall variance explained in quit intentions was greater in Scotland than in the rest of the United Kingdom but not significantly so.
Discussion
Support for smoke-free legislation at baseline significantly increased support at follow-up for both samples. However, this did not independently increase quit intentions among smokers from both Scotland and the rest of the United Kingdom. The findings suggest that normative influences are one of the mechanisms through which comprehensive smoke-free legislation influences quit intentions.
Introduction
The recent decline in smoking prevalence in most advanced tobacco markets has been attributed to a synergism of tobacco programs and policies (Siegel, Albers, Cheng, Biener, & Rigotti, 2004; Tauras, 2005; Tauras & Chaloupka, 2001; Wilson et al., 2007). A central component to any comprehensive tobacco control program is smoke-free legislation (Levy, Chaloupka, & Gitchell, 2004), with restrictions in pubs, restaurants, and other workplaces associated with reduced smoking prevalence and increased smoking cessation, among both adults and young people (Fichtenberg & Glantz, 2002; Gallus et al., 2006; Levy, Friend, & Polishchuk, 2001; Tauras, 2005; Wakefield et al., 2000). For example, 46% of adult smokers in Ireland reported that they were more likely to consider quitting on account of the smoking ban, introduced in 2004, while 80% of quitters indicated that the ban helped them to quit and 88% to stay quit (Fong, Hyland, et al., 2006). Smoke-free legislation conveys additional benefits, including the imposition of smoke-free restrictions in the home (Hyland et al., 2007) and improved air quality in hospitality settings (Edwards et al., 2008), thus protecting workers and nonsmoking patrons from secondhand smoke (International Agency for Research on Cancer, 2004).
It is evident from the extant literature that comprehensive smoke-free legislation, covering all indoor areas, is capable of reducing smoking prevalence (Chapman et al., 1999; Eriksen & Chaloupka, 2007; Gallus et al., 2007; Levy et al., 2001; Tauras, 2005; Wilson et al., 2007). In fact, along with high tobacco taxation, comprehensive smoke-free laws may represent one of the most effective tobacco control measures available (Fichtenberg & Glantz, 2002; Levy et al., 2004). Surprisingly however, despite the direct link between smoking restrictions and reduced prevalence and intensity, the mechanisms mediating this effect, such as normative influences, are underresearched (Albers, Siegel, Cheng, Biener, & Rigotti, 2004). More than most other tobacco control measures, smoke-free legislation can denormalize tobacco use by transforming smoking norms and accelerating approval of a nonsmoking environment as the prevailing norm (Kagan & Skolnick, 1993; Opp, 2002; Ostrom, 2000). For example, research has provided evidence of changing norms about smoking concomitant with smoking restrictions in the workplace (Gilpin, Lee, & Pierce, 2004; Shopland, Gerlach, Burns, Hartman, & Gibson, 2001). As smokers conform to nonsmoking directives in workplaces, this may result in stronger antismoking norms, by reducing smoking visibility in these settings and encouraging societal disapproval of smoking (Alesci, Forster, & Blaine, 2003; Eisenberg & Forster, 2003; Siegel, Albers, Cheng, Biener, & Rigotti, 2005).
Another mechanism via which smoking restrictions can denormalize tobacco use is increased social unacceptability of smoking. Research has incorporated normative influences, such as social unacceptability, in behavioral models and found that this measure correlates with, and strongly predicts, a range of behaviors, including smoking (Armitage & Conner, 2001; Eisenberg & Forster, 2003; Hamilton, Biener, & Brennan, 2008). It has also been found to predict quit intentions and behaviors (Alamar & Glantz, 2006; Dotinga, Schrijvers, Voorham, & Mackenbach, 2005). Research that has assessed the extent to which smoking restrictions affect normative influences, such as acceptability (Albers et al., 2004; Gallus et al., 2007), is generally limited to cross-sectional data, however, thus preventing causal associations being drawn between smoke-free regulation and changes in acceptability of smoking. A notable exception is longitudinal research of Albers, Siegel, Cheng, Biener, and Rigotti (2007) assessing the effect of (weak or strong) smoking regulations in local restaurants, across 351 towns in Massachusetts, on adult smokers’ perceived acceptability of smoking and quit behaviors (quit attempts and actual cessation). For smokers who had already attempted to quit at baseline, living in a town with strong regulations increased the odds of making a quit attempt at follow-up (odds ratio = 3.1). And for smokers perceiving smoking as unacceptable at baseline, smoke-free regulations appeared to consolidate these initial beliefs, but in neither case were local regulations found to have an effect on cessation at follow-up. The fact that local smoke-free regulations were weak in the vast majority (87.5%) of towns provides a possible explanation for the failure to find increases in cessation.
In this study, we add to the tobacco control literature by assessing whether adult smokers’ quit intentions are associated with support for smoking restrictions and social unacceptability following a comprehensive smoking ban in Scotland that legitimized nonsmoking as a societal normative behavior by making smoking more unacceptable (Gruber & Zinman, 2001; Wakefield et al., 2000). Knowledge of the role of normative influences on quit intentions, if any, can contribute to the design of media campaigns, occurring alongside smoke-free legislation, aimed at promoting quitting. Specifically, we examine (a) the effect of a policy-related measure (support for smoke-free legislation) on adult smokers’ perceived social unacceptability of smoking, 1-month preban and 1-year postban, and (b) whether support for smoke-free legislation and perceived social unacceptability of smoking are associated with quit intentions postban. We extend the Albers et al. (2007) study in three ways: First, we use nationally representative samples of smokers; second, we assess comprehensive smoke-free laws that cover, without exception, an entire nation (i.e., the legislation covers all of Scotland, with no local level regulatory variations); and third, we use the rest of the United Kingdom as a control group. This enables comparisons to be drawn with these countries that have, aside from smoke-free laws, very similar tobacco control policies to Scotland at the time of the study. In terms of smoke-free laws, a comprehensive nationwide smoking ban, including restaurants and public houses (pubs), came into effect in Scotland in March 2006. For the rest of the United Kingdom, smoke-free legislation was implemented approximately 12–15 months after the Scottish ban.
Methods
Sample and procedure
The ITC Scotland/U.K. Survey was a quasi-experimental longitudinal telephone survey using nationally representative samples of both smokers and nonsmokers, aged 18 years or older, in Scotland and the rest of the United Kingdom. Participants were part of a larger cohort study conducted as part of the ITC Policy Evaluation Project (Fong, Hyland, et al., 2006). These participants were recruited by geographically stratified probability sampling with telephone numbers selected at random from the population of each country. List-assisted telephone numbers comprising a sampling frame of 100 banks (defined by area code, three-digit prefix, and first two digits of the four-digit suffix, such as the 100 consecutive numbers from 0141-936-0000 to 0141-936-0099) of residential numbers were obtained from Survey Sampling International. The next birthday method was used to select a single respondent in households with more than one eligible respondent (Binson, Canchola, & Catania, 2000). A smoker was defined as an individual who reported smoking at least once in the month prior to interview and had smoked at least 100 cigarettes in his or her lifetime.
The two samples (Scotland and the rest of the United Kingdom) were interviewed 1 month before the smoking ban came into effect in Scotland in March 2006 and 1 year later. At follow-up, smoking bans in the rest of the United Kingdom had not yet been implemented, although they were imminent. Results are weighted to be representative of the adult smoker population within each country. Smokers received a £7 shopping (Boots) voucher as an incentive to participate while nonsmokers received a £4 Boots voucher. For this study, only smokers are included in the analyses.
The total sample comprised 1,014 smokers at baseline (507 from Scotland and 507 from the rest of the United Kingdom); for age and gender classification, see Table 1. The response rate at baseline was 29% in Scotland and 30% in the rest of the United Kingdom. The retention rate for Scotland and the rest of the United Kingdom was 53% and 51%, respectively, at the follow-up survey and included 527 smokers. Analysis between responders and nonresponders on demographic information (age, gender, and socioeconomic status [SES]) found nonresponders from both countries more likely to be between the ages of 25 and 54 years, although no significant differences in gender and SES were found (see Table 2). The study protocol was approved by ethics review boards at the University of Stirling (Scotland), University of Waterloo (Canada), Roswell Park Cancer Institute (United States), and the Cancer Council Victoria (Australia).
Table 1.
Age and gender of smokers in Scotland and rest of the United Kingdom
| Scotland, N (%) |
Rest of the United Kingdom, N (%) |
|||
| Baseline | Follow-up | Baseline | Follow-up | |
| Age (years) | ||||
| 18–24 | 34 (6.7) | 11 (4.1) | 52 (10.3) | 16 (6.2) |
| 25–39 | 157 (31.0) | 77 (28.5) | 172 (33.9) | 71 (27.6) |
| 40–54 | 191 (37.7) | 108 (40.0) | 157 (31.0) | 92 (35.8) |
| 55+ | 125 (24.7) | 74 (27.4) | 126 (24.9) | 78 (30.4) |
| Gender | ||||
| Female | 297 (58.6) | 169 (62.6) | 268 (52.9) | 141 (54.9) |
| Male | 210 (41.4) | 101(37.4) | 239 (47.1) | 116 (45.1) |
Table 2.
Logistic regression for gender, age, and SES of respondents vs. nonrespondents in Scotland and rest of the United Kingdom
| Scotland |
Rest of the United Kingdom |
|||||
| OR | 95% CI | p | OR | 95% CI | p | |
| Gender | ||||||
| Female | 1.00 | 1.00 | ||||
| Male | 1.17 | 0.82–1.68 | .39 | 0.89 | 0.63–1.27 | .54 |
| Age (years) | ||||||
| 18–24 | 1.00 | 1.00 | ||||
| 25–39 | 0.32 | 0.18–0.62 | .001 | 0.26 | 0.14–0.49 | .001 |
| 40–54 | 0.39 | 0.24–0.64 | .001 | 0.40 | 0.24–0.67 | .001 |
| 55+ | 0.66 | 0.41–1.06 | .087 | 0.88 | 0.52–1.51 | .65 |
| SES | 0.83 | 0.65–1.06 | .13 | 1.14 | 0.88–1.46 | .33 |
Note. CI, confidence interval; OR, odds ratio; SES, socioeconomic status.
Measures
Policy-specific measures
Perceptions of smoking restrictions.
Two policy-related items were employed to create a single index to measure the level of support for smoking restrictions in public houses. The first item: “Do you support or oppose a total ban on smoking inside pubs” was measured on a 4-point scale ranging from “strongly support” to “strongly oppose.” The second item: “Do you think that bans on smoking in pubs are a good thing or bad thing” was measured on a 4-point scale ranging from “very bad” to “very good.” Cronbach α for this construct was .87 and .82 for Waves 1 and 2, respectively.
Psychosocial mediator
Social unacceptability of smoking.
Three items were used to create a single index to measure the social unacceptability of smoking among proximal groups (“People who are important to me believe I should not smoke”), society in general (“Society disapproves of smoking ”), and self-perception of unacceptability (“There are fewer and fewer places where I feel comfortable smoking”). Each item was assessed using a 5-point Likert scale, ranging from strongly agree to strongly disagree. Cronbach α was .62 and .60 for Waves 1 and 2, respectively.
Outcome measure
Quit intentions.
Intention to quit was assessed (at Wave 2 only) with a standard question based on the stages of change model (de Vries & Mudde, 1998; Prochaska, Redding, & Evers, 1997). The question asked how soon participants planned to quit smoking, with a 4-point scale ranging from “plan to quit smoking within the next month” to “not planning to quit,” which was collapsed into dichotomous responses “yes, intend to quit” and “no, not intending to quit.”
Analytic strategy
The hypothesized model, which tests the relations among the latent factors (independent, mediating, and dependent variables), was analyzed using structural equation modeling (SEM) with analysis of moment structures (AMOS; Arbuckle & Wothke, 2003). SEM permits simultaneous assessment of a range of relations among constructs and rigorously examines and compares similarities as well as differences between two or more groups (Hoyle, 1995). AMOS provides full maximum likelihood estimates and presents a means of controlling for the presence of measurement errors (Hoyle & Smith, 1994; Joreskog & Sorbom, 1998).
Prior to testing the structural models for both Scotland and the rest of the United Kingdom, the viability of our proposed latent factors was established using confirmatory factor analysis (CFA; Joreskog & Sorbom, 1998). CFA seeks to determine if the number of latent factors and the loadings of indicator variables on them conform to what is empirically expected (Kim & Mueller, 1978). The latent factors comprise all unobserved variables (e.g., support for smoking restrictions) which are measured by their respective observed variables (e.g., “People who are important to me believe I should not smoke ”).
Statistical tests to evaluate model fit were based on the normed fit index (NFI; Bentler & Bonett, 1980), comparative fit index (CFI; Bentler, 1990), Tucker Lewis Index (TLI; Browne & Cudeck, 1993), and root mean squared error of approximation (RMSEA; Browne & Cudeck). Values above 0.90 on the NFI, TLI, and CFI, and values less than 0.05 for RMSEA, signify good fit (Browne & Cudeck). Chi-square is reported but, as it is sensitive to sample size, it was used to evaluate the relative differences in fit among competing models (Hoyle, 1995).
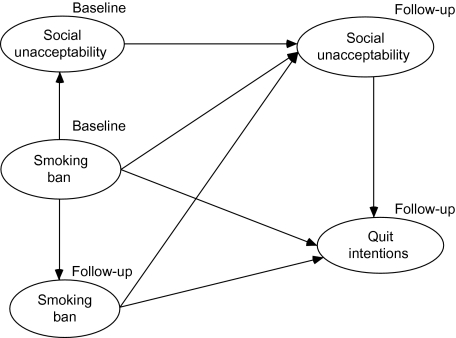
The consistency of the measurement model across group and time was established sequentially in harmony with Bollen's (1989) guidelines. Following evaluation of the measurement model, further analyses were conducted to examine the structural models that reflect hypothesized relationships among the latent variables (see Figure 1). This hypothesized model was compared against a series of alternative models using multigroup analyses to examine the consistency of the model across different groups (i.e., Scotland and the rest of the United Kingdom) along a continuum (Bollen, 1989).
Figure 1.
Hypothesized model of support for smoking ban, unacceptability, and quit intentions.
Results
Support for a smoking ban and unacceptability of smoking
To help contextualize the subsequent models for Scotland and the rest of the United Kingdom, Table 3 shows the latent variables (support for smoke-free legislation and perceived unacceptability of smoking) across Waves 1 and 2, for Scotland and the rest of the United Kingdom. The items representing unacceptability and support were initially summed and averaged before paired sample t tests and were performed to assess any difference within and between countries at Waves 1 and 2.
Table 3.
Support for a ban and unacceptability of smoking across Waves 1 and 2, within and between countries
| Scotland |
Rest of the United Kingdom |
|||||
| Within country | Wave 1 | Wave 2 | p | Wave 1 | Wave 2 | p |
| Support (1–4) | 2.44 | 2.75 | .001 | 2.34 | 2.54 | .001 |
| Unacceptability (1–5) | 2.21 | 3.27 | .001 | 2.28 | 3.21 | .001 |
| Between countries | Wave 1 | Wave 2 | ||||
| Scotland | Rest of the United Kingdom | p | Scotland | Rest of the United Kingdom | p | |
| Support (1–4) | 2.44 | 2.34 | .32 | 2.75 | 2.54 | .01 |
| Unacceptability (1–5) | 2.21 | 2.28 | .48 | 3.27 | 3.21 | .85 |
Within-country results showed a significant difference between support for a ban from Wave 1 to 2 in both Scotland and the rest of the United Kingdom. Likewise, a significant difference was found for unacceptability in both Scotland and the rest of the United Kingdom between the two waves (see Table 3). Correlational analyses also revealed significant associations (p < .01) for both Scotland and the rest of the United Kingdom for support for a ban and unacceptability. Comparing the two countries, it was found that there were no significant differences between Scotland and the rest of the United Kingdom for both unacceptability and support for a ban at Wave 1. At Wave 2, there was no significant difference between Scotland and the rest of the United Kingdom for unacceptability, although a higher increase in unacceptability was observed in Scotland. However, there was a significant difference between Scotland and the rest of the United Kingdom for support for a ban at Wave 2, with a greater increase in levels of support in Scotland.
Evaluation of measurement models
The evaluation of the multigroup models’ robustness was judged on the basis of (a) the appropriateness of the direction, strength, and significance of the parameter estimates; (b) the convergence of the maximum likelihood estimate; (c) the statistical tests and fit indices previously noted (NFI, TLI, CFI, and RMSEA); (d) a comparison of the constrained model with the unconstrained counterpart using the chi-square difference test, RMSEA, and the CFI change; and (e) the model's ability to explain the variance of quit intentions in both samples at follow-up.
Two identical measurement models, one for the Scottish sample and one for the sample from the rest of the United Kingdom, were tested separately. All variable loadings on the hypothesized latent factors were significant (p < .01). Overall fit was good for both the Scotland model (χ292 = 72.269, p < .001, CFI = 0.97, TLI = 0.95, NFI = 0.96, RMSEA = 0.04) and the model for the rest of the United Kingdom (χ292 = 105.629, p < .001, CFI = 0.95, TLI = 0.91, NFI = 0.94, RMSEA = 0.05). Following this, multigroup analysis was used to assess simultaneously the invariance across the two countries. A multigroup invariance test permits the assessment of the goodness of fit of a baseline model with all factor loadings unconstrained across the two countries compared with a constrained model. The chi-square value of the constrained model was compared with that of an unconstrained model which had no equality constraints imposed. This result indicated statistically significant group differences in the factor loadings for Scotland and the rest of the United Kingdom (Δχ132 = 23.779, p < .05).
Evaluation of structural model
Having established group difference, the hypothesized structural model, assessed separately for Scotland and the rest of the United Kingdom, was used to examine the goodness of fit (Figure 1). Good overall fit was found for both the Scottish (χ362 = 78.765, p < .001, CFI = 0.96, TLI = 0.93, NFI = 0.94, RMSEA = 0.04) and the rest of the U.K. models (χ362 = 91.910, p < .001, CFI = 0.94, TLI = 0.90, NFI = 0.91, RMSEA = 0.05). Subsequently, all path coefficients of these structural models were constrained to be identical across the two groups, which were then compared with an unconstrained model. Results of a chi-square difference test (Δχ162 = 34.53, p < .01) indicated that the unconstrained model fit the data significantly better. This shows that there are differences in the path coefficients for smokers in Scotland and the rest of the United Kingdom. Finally, the consistency of the structural model over time was tested by comparing the constrained path coefficients linking baseline and follow-up variables with an unconstrained model in which these coefficients were estimated freely. The chi-square difference test indicated that the unconstrained model fits the data better than the constrained model (Δχ82 = 16.336, p < .05). Thus, there is significant difference in the structural paths across time. A further test of invariance to pinpoint where these significant structural paths lie revealed no significant difference in structural paths from support for a ban at baseline and social unacceptability at follow-up to quit intentions between Scotland and the rest of the United Kingdom (chi-square difference values are Δχ92 = 17.0, p = .05 and Δχ82 = 15.70, p = .05, respectively). This suggests that there is no significant difference in quit intentions between Scotland and the rest of the United Kingdom. However, between the two countries, significant differences were found between the paths from support for a ban at baseline to support for a ban at follow-up (Δχ72 = 14.80, p < .05) and from social unacceptability at baseline to unacceptability at follow-up (Δχ82 = 15.91, p < .05).
Comparative evaluation of models
Table 4 shows the standardized path coefficients (i.e., standardized regression weights) among latent variables, with both the Scotland and U.K. models assessed separately. Results indicate that in Scotland support for the smoking ban significantly heightened social unacceptability of smoking at baseline (β = .19). Similarly, the path linking social unacceptability at baseline to social unacceptability at follow-up was significant (β = .75). Thus, smoking was significantly less socially acceptable at follow-up as a result of the indirect effect of support for a smoking ban. The path from unacceptability at follow-up to quit intentions at follow-up was significant (β = .20), and the path from support for a ban at baseline was significantly associated with quit intentions at follow-up (β = .21). Likewise, support for a ban at baseline also significantly increased support for a ban at follow-up (β = .68). This finding indicated that the model accounted for 19% of variance in quit intentions at follow-up. The independent paths from support for the ban at baseline and follow-up to social unacceptability at follow-up as well as support for a ban at follow-up to quit intentions were not significant in Scotland. The overall model provided good fit (χ352 = 68.152, p < .001, CFI = 0.97, TLI = 0.94, NFI = 0.94, RMSEA = 0.04).
Table 4.
Model paths of support for ban, unacceptability, and quit intentions across Scotland and rest of the United Kingdom
| Scotland |
Rest of the United Kingdom |
|||
| Paths | β | CR | β | CR |
| Unacceptability (T1) → Unacceptability (T2) | .75*** | 5.65 | .71*** | 5.39 |
| Ban (T1) → Unacceptability (T1) | .19** | 3.13 | .26*** | 4.01 |
| Ban (T1) → Ban (T2) | .68*** | 8.87 | .62*** | 7.74 |
| Ban (T1) → Unacceptability (T2) | .03 | 0.26 | −.03 | −0.23 |
| Ban (T2) → Unacceptability (T2) | .11 | 1.04 | .26 | 1.79 |
| Ban (T1) → Quit intentions (T2) | .21** | 2.91 | .16 | 1.79 |
| Ban (T2) → Quit intentions (T2) | .14 | 1.73 | .06 | 0.06 |
| Unacceptability (T2) → Quit intentions (T2) | .20** | 2.66 | .19** | 2.32 |
Note. CR, critical ratio; T1, baseline; and T2, follow-up.
*p < .05, **p < .01, ***p < .001.
In the rest of the United Kingdom, the hypothesized structural model revealed that support for a ban at baseline heightened social unacceptability at baseline (β = .26) which, in turn, significantly heightened social unacceptability at follow-up (β = .71). Support for a ban at baseline also significantly increased support for a ban at follow-up (β = .62), though this did not independently increase quit intentions at follow-up. Rather, social unacceptability at follow-up was associated with quit intentions at follow-up (β = .19). The independent paths from support for a ban at baseline and follow-up did not affect quit intentions and unacceptability at follow-up. Although the overall fit of the model was good (χ352 = 77.002, p < .001, CFI = 0.95, TLI = 0.91, NFI = 0.92, RMSEA = 0.05), the variance explained by the predictors of quit intentions (12%) was less than the variance explained in the Scottish model (19%).
Discussion
Evidence suggests that smoking restrictions are accompanied by quitting intentions and behaviors and help denormalize smoking (Albers et al., 2004; Wakefield et al., 2000;). We sought to develop a theoretical model and test the influence of smoke-free legislation on adult smokers’ quit intentions through the mediation of normative beliefs of smoking. Our findings are consistent with the Focus Theory of Normative Conduct, which predicts that individuals will conform to a relevant norm, provided it is prominent in their consciousness (Cialdini & Goldstein, 2004; Cialdini, Kallgren, & Reno, 1990, 1991). In our study, prior to the smoking ban in Scotland, support for a ban significantly heightened smokers’ perceived social unacceptability of smoking and further strengthened these perceptions postban. To the extent that the relevant norm (in this case a nonsmoking directive) is focal or salient, increased unacceptability of smoking would be expected, possibly through media portrayals and peer communication about the implementation of smoke-free laws (Cialdini & Trost, 1998; Real & Rimal, 2007). Our results provide evidence that smokers’ perceptions of nonsmoking directives at baseline can transform their smoking norms, which legislation serves to reinforce. These findings support previous research demonstrating a link between approval of bans and perceptions of smoking as less normative (Albers et al., 2007; Borland, Mullins, Trotter, & White, 1999; Trotter, Wakefield, & Borland, 2002), which are propagated in peer networks, through communication about the relevant norm (Perkins, 1997; Real & Rimal, 2007).
Similar findings were obtained for smokers in both Scotland and the rest of the United Kingdom in terms of changes in social unacceptability of smoking. However, social unacceptability of smoking among smokers in Scotland postban was slightly greater than for smokers in the rest of the United Kingdom. Thus, as the normative directive (i.e., smoke-free legislation) became evident in Scotland postban, smokers in Scotland possibly perceived smoking as more socially unacceptable than smokers from the rest of the United Kingdom, which had no ban at the time.
Comparable with the rest of the United Kingdom, in Scotland, perceived social acceptability of smoking at follow-up was associated with higher quit intentions. This finding is consistent with several studies that have found perceived social acceptability of smoking among referent groups to be independently associated with both strength of intention to quit and actual quit behavior at follow-up (de Vries, Mudde, Dijkstra, & Willemsen, 1998; Dotinga et al., 2005; Hammond, Fong, Zanna, Thrasher, & Borland, 2006). Nonetheless, as there was no significant difference in quit intentions between two countries, this association with quit intentions is perhaps indicative of the filtering effects of the Scottish ban coupled with media depictions about the enactment of smoke-free laws in the rest of the United Kingdom, which were implemented in summer 2007. To the extent that a nonsmoking directive is enacted, quit intentions and behaviors will be guided largely by normative considerations, and this will likely impact upon neighboring environments, especially on account of media campaigns and accessibility to and from both settings.
Our study also found that in the rest of the United Kingdom, support for a ban at baseline significantly increased support for a ban at follow-up, although support had no effect on quit intentions at follow-up. That support for a ban at follow-up did not affect quit intentions is perhaps suggestive of the strength of perceived unacceptability to influence quit intentions in a country preparing to introduce a ban rather than support for a ban. Likewise, among smokers in Scotland, support for a ban increased postban, but quit intentions at follow-up were associated with support for a ban at baseline rather than support for a ban at follow-up. This increase in support for a ban, and corresponding association with quit intentions, at follow-up may be partly due to the marked decreases in secondhand smoke evident in Scottish pubs (Semple, Creely, Naji, Miller, & Ayres, 2007). The variance in quit intentions at follow-up explained in Scotland was greater (19%) than that for the rest of the United Kingdom (12%), but this difference was not significant, similar in this respect to the findings of a recent Scotland/U.K. ITC study that compared smoking cessation indicators and exposure with secondhand smoke in a range of venues between Scotland and the rest of the United Kingdom (Hyland et al., 2009). These findings reflect the effectiveness of smoking bans, whether implemented or due to be implemented, in influencing quit intentions, and support the view that smoke-free laws should be a public health priority for legislators (Edwards et al., 2008).
Like all research, our study has limitations. Our model did not include moderator variables (i.e., general demographic information), which may have impacted upon the findings, although we found no significant gender differences in additional analyses (not reported). The failure to include other potential mediating variables (e.g., reduced opportunity to smoke in the workplace, dislike of smoking outside, associated mass-media campaigns and unpaid media coverage) may have similarly impacted upon the findings, and the absence of other normative constructs weakened the explanatory power of the model. Additionally, a relatively small sample size was employed as a result of the low response rate, and almost half the sample was lost to attrition at follow-up, which is slightly higher than with other research (Albers et al., 2007). Furthermore, we found significant differences between respondents and nonrespondents in terms of age, with smokers aged 25–54 years more likely to drop out. This may have impacted upon the results, although past research reporting similar response bias in terms of age suggests that this does not affect the conclusions drawn from these studies (Benfante, Reed, MacLean, & Kagan, 1989; Forthofer, 1983; Heilbrun, Nomura, & Stemmermann, 1991).
Despite these limitations, the use of a longitudinal design allowed us to assess the influence of a population-level policy measure (smoking ban) on quit intentions via a suitable general mediator (unacceptability). Longitudinal designs can overcome many of the problems associated with cross-sectional research and allow causality to be demonstrated, permitting valuable insights into the pathways involved in behavior change. Our findings shed light on how a smoking ban can increase the social unacceptability of smoking, which, in turn, is associated with quit intentions. Future research using tobacco industry perceptions as an additional normative mediator, aside from unacceptability, would be of value to examine whether smoke-free legislation influences quitting partly via the creation of less favorable industry perceptions.
Funding
Funding for this research was provided by grants from the National Cancer Institute of the United States (through the Roswell Park Trans-disciplinary Tobacco Use Research Center, P50 CA111236), the Canadian Institutes of Health Research (79551), Cancer Research UK (C312/A3726), the Flight Attendant Medical Research Institute, National Health Service Health Scotland, and the Scottish Executive.
Declaration of Interests
None declared.
Supplementary Material
References
- Alamar B, Glantz SA. Effect of increased social unacceptability of cigarette smoking on reduction in cigarette consumption. American Journal of Public Health. 2006;96:1359–1363. doi: 10.2105/AJPH.2005.069617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albers AB, Siegel M, Cheng DM, Biener L, Rigotti NA. Relation between local restaurant smoking regulations and attitudes towards the prevalence and social acceptability of smoking: A study of youths and adults who eat out predominantly at restaurants in their town. Tobacco Control. 2004;13:347–355. doi: 10.1136/tc.2003.007336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albers AB, Siegel M, Cheng DM, Biener L, Rigotti NA. Effect of smoking regulations in local restaurants on smokers’ anti-smoking attitudes and quitting behaviours. Tobacco Control. 2007;16:101–106. doi: 10.1136/tc.2006.017426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alesci NL, Forster JL, Blaine T. Smoking visibility, perceived acceptability, and frequency in various locations among youth and adults. Preventive Medicine. 2003;36:272–281. doi: 10.1016/s0091-7435(02)00029-4. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL, Wothke W. AMOS 5.0 user guide. Chicago: SPSS; 2003. [Google Scholar]
- Armitage CJ, Conner M. Efficacy of the theory of planned behavior: A meta-analytic review. British Journal of Social Psychology. 2001;40:471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- Benfante R, Reed D, MacLean C, Kagan A. Response bias in the Honolulu heart program. American Journal of Epidemiology. 1989;130:1088–1100. doi: 10.1093/oxfordjournals.aje.a115436. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- Binson D, Canchola JA, Catania JA. Random selection in a national telephone survey: A comparison of the Kish, next-birthday, and last-birthday methods. Journal of Official Statistics. 2000;16:53–60. [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- Borland R, Mullins R, Trotter L, White V. Trends in environmental tobacco smoke restrictions in the home in Victoria, Australia. Tobacco Control. 1999;8:266–271. doi: 10.1136/tc.8.3.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Chapman S, Borland R, Scollo M, Brownson RC, Dominello A, Woodward S. The impact of smoke-free workplaces on declining cigarette consumption in Australia and the United States. American Journal of Public Health. 1999;89:1018–1023. doi: 10.2105/ajph.89.7.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cialdini RB, Goldstein NJ. Social influence: Compliance and conformity. Annual Review of Psychology. 2004;55:591–622. doi: 10.1146/annurev.psych.55.090902.142015. [DOI] [PubMed] [Google Scholar]
- Cialdini RB, Kallgren CA, Reno RR. A focus theory of normative conduct: Recycling the concept of norms to reduce littering in public places. Journal of Personality and Social Psychology. 1990;58:1015–1026. [Google Scholar]
- Cialdini RB, Kallgren CA, Reno RR. A focus theory of normative conduct: A theoretical refinement and reevaluation of the role of norms in human behavior. In: Berkowitz L, editor. Advances in Experimental Social Psychology. Vol. 24. San Diego, CA: Academic Press; 1991. pp. 201–234. [Google Scholar]
- Cialdini RB, Trost MR. Social influence: Social norms, conformity, and compliance. In: Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social psychology. Boston, MA: McGraw-Hill; 1998. pp. 151–192. [Google Scholar]
- de Vries H, Mudde AN. Predicting stage transitions for smoking cessation applying the attitude social influence efficacy model. Psychology and Health. 1998;13:369–385. [Google Scholar]
- de Vries H, Mudde AN, Dijkstra A, Willemsen MC. Differential beliefs, perceived social influences, and self-efficacy expectations among smokers in various motivational phases. Preventive Medicine. 1998;27:681–689. doi: 10.1006/pmed.1998.0344. [DOI] [PubMed] [Google Scholar]
- Dotinga A, Schrijvers CTM, Voorham AJJ, Mackenbach JP. Correlates of stages of change of smoking among inhabitants of deprived neighborhoods. European Journal of Public Health. 2005;15:152–159. doi: 10.1093/eurpub/cki112. [DOI] [PubMed] [Google Scholar]
- Edwards R, Thomson G, Wilson N, Waa A, Bullen C, O’Dea D, et al. After the smoke has cleared: Evaluation of the impact of a new national smoke-free law in New Zealand. Tobacco Control. 2008;17:e2. doi: 10.1136/tc.2007.020347. [DOI] [PubMed] [Google Scholar]
- Eisenberg ME, Forster JL. Adolescent smoking behavior: Measures of social norms. American Journal of Preventive Medicine. 2003;25:122–128. doi: 10.1016/s0749-3797(03)00116-8. [DOI] [PubMed] [Google Scholar]
- Eriksen M, Chaloupka F. The economic impact of clean indoor air laws. A Cancer Journal for Clinicians. 2007;57:367–378. doi: 10.3322/CA.57.6.367. [DOI] [PubMed] [Google Scholar]
- Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behaviour: Systematic review. British Medical Journal. 2002;325:188–191. doi: 10.1136/bmj.325.7357.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong GT, Cummings KM, Borland R, Hastings G, Hyland A, Giovino GA, et al. The conceptual framework of the International Tobacco Control (ITC) Evaluation Project. Tobacco Control. 2006;15(Suppl. 3):iii3–iii11. doi: 10.1136/tc.2005.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong GT, Hyland A, Borland R, Hammond D, Hastings G, McNiell A, et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: Findings from the ITC Ireland/UK survey. Tobacco Control. 2006;15(Suppl. 3):iii51–iii58. doi: 10.1136/tc.2005.013649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forthofer RN. Investigation of nonresponse bias in NHANES 11. American Journal of Epidemiology. 1983;117:507–515. doi: 10.1093/oxfordjournals.aje.a113568. [DOI] [PubMed] [Google Scholar]
- Gallus S, Zuccaro P, Colombo P, Apolone G, Pacifici R, Garattini S, et al. Effects of new smoking regulations in Italy. Annals of Oncology. 2006;17:346–347. doi: 10.1093/annonc/mdj070. [DOI] [PubMed] [Google Scholar]
- Gallus S, Zuccaro P, Colombo P, Apolone G, Pacifici R, Garattini S, et al. Smoking in Italy 2005–2006: Effects of a comprehensive National Tobacco Regulation. Preventive Medicine. 2007;45:198–201. doi: 10.1016/j.ypmed.2007.03.009. [DOI] [PubMed] [Google Scholar]
- Gilpin EA, Lee L, Pierce JP. Changes in population attitudes about where smoking should not be allowed: California versus the rest of the USA. Tobacco Control. 2004;13:38–44. doi: 10.1136/tc.2003.004739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber J, Zinman J. In: Youth smoking in the US: Evidence and implications Risky behaviors among youths. Gruber J, editor. Chicago: University of Chicago Press; 2001. pp. 69–120. [Google Scholar]
- Hamilton WL, Biener L, Brennan RL. Do local tobacco regulations influence perceived smoking norms? Evidence from adult and youth surveys in Massachusetts. Health Education Research. 2008;23:709–722. doi: 10.1093/her/cym054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D, Fong G, Zanna M, Thrasher J, Borland R. Tobacco denormalization and industry beliefs among smokers from four countries. American Journal of Preventive Medicine. 2006;31:225–232. doi: 10.1016/j.amepre.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Heilbrun LK, Nomura A, Stemmermann GN. The effects of nonresponse in a prospective study of cancer: 15 year follow-up. International Journal of Epidemiology. 1991;20:328–338. doi: 10.1093/ije/20.2.328. [DOI] [PubMed] [Google Scholar]
- Hoyle RH. Structural equation modeling: Concepts, issues, and applications. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- Hoyle RH, Smith GT. Formulating clinical research hypotheses as structural equation models: A conceptual overview. Journal of Consulting and Clinical Psychology. 1994;62:429–440. doi: 10.1037//0022-006x.62.3.429. [DOI] [PubMed] [Google Scholar]
- Hyland A, Hassan L, Higbee C, Boudreau C, Fong GT, Borland R, et al. The impact of smokefree legislation in Scotland: Results from the Scottish ITC Scotland/UK longitudinal surveys. European Journal of Public Health. (2009);19:198–205. doi: 10.1093/eurpub/ckn141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland A, Higbee C, Hassan L, Fong GT, Borland R, Cummings M, et al. Does smoke-free Ireland have more smoking inside the home and less in pubs than the United Kingdom? Findings from the international tobacco control policy evaluation project. European Journal of Public Health. 2007;18:63–65. doi: 10.1093/eurpub/ckm054. [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer. Lyon, France: IARC; 2004. IARC monographs on the evaluation of carcinogenic risks to humans: Vol. 83. Tobacco smoking and involuntary smoking. [Google Scholar]
- Joreskog K, Sorbom D. LISREL7: A guide to the program and applications. Chicago: SPSS Inc; 1998. [Google Scholar]
- Kagan RA, Skolnick JH. Banning smoking: Compliance without enforcement. In: Rabin RL, Sugarman SD, editors. Smoking policy: Law, politics, and culture. New York: Oxford University Press; 1993. pp. 69–94. [Google Scholar]
- Kim JO, Mueller CW. Factor analysis: Statistical methods and practical issues (Quantitative applications in the social sciences, No. 14) Thousand Oaks, CA: Sage Publications; 1978. [Google Scholar]
- Levy DT, Chaloupka F, Gitchell J. The effects of tobacco control policies on smoking rates: A tobacco control scorecard. Journal of Public Health Management and Practice. 2004;10:338–353. doi: 10.1097/00124784-200407000-00011. [DOI] [PubMed] [Google Scholar]
- Levy DT, Friend K, Polishchuk E. Effect of clean indoor air laws on smokers: the clean air module of the SimSmoke computer simulation model. Tobacco Control. 2001;10:345–351. doi: 10.1136/tc.10.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opp K. When do norms emerge by human design and when by the unintended consequences of human action? The example of the no-smoking norm. Rationality and Society. 2002;14:131–158. [Google Scholar]
- Ostrom E. Collective action and the evolution of social norms. Journal of Economic Perspectives. 2000;14:137–158. [Google Scholar]
- Perkins HW. College student misperceptions of alcohol and other drug use norms among peers: Exploring causes, consequences and implications for prevention programs. In: Baker K, Maas J, McAuliffe A, Wojdyslawski S, Zweig K, editors. Designing alcohol and other drug prevention programs in higher education: Bringing theory into practice. Newton, MA: The Higher Education Center for Alcohol and Other Drug Prevention; 1997. pp. 177–206. [Google Scholar]
- Prochaska JO, Redding CA, Evers K. The transtheoretical model and stages of change. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: Theory, research, and practice. San Francisco, CA: Jossey-Bass; 1997. pp. 60–84. [Google Scholar]
- Real K, Rimal R. Friends talk to friends about drinking: Exploring the role of peer communication in the theory of normative social behaviour. Health Communication. 2007;22:169–180. doi: 10.1080/10410230701454254. [DOI] [PubMed] [Google Scholar]
- Semple S, Creely KS, Naji A, Miller BG, Ayres JG. Secondhand smoke levels in Scottish pubs: The effect of smoke-free legislation. Tobacco Control. 2007;16:127–132. doi: 10.1136/tc.2006.018119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shopland DR, Gerlach KK, Burns DM, Hartman AM, Gibson JT. State-specific trends in smoke-free workplace policy coverage: The current population survey tobacco use supplement, 1993 to 1999. Journal of Occupational and Environmental Medicine. 2001;43:680–686. doi: 10.1097/00043764-200108000-00005. [DOI] [PubMed] [Google Scholar]
- Siegel M, Albers AB, Cheng DM, Biener L, Rigotti NA. Effect of local restaurant smoking regulations on progression to established smoking among youths. Tobacco Control. 2005;14:300–306. doi: 10.1136/tc.2005.012302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel M, Albers AB, Cheng DM, Biener L, Rigotti NA. Effect of local restaurant smoking regulations on environmental tobacco smoke exposure among youths. American Journal of Public Health. 2004;94:321–325. doi: 10.2105/ajph.94.2.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tauras JA. Can public policy deter smoking escalation among young adults? Journal of Policy Analysis and Management. 2005;24:771–784. doi: 10.1002/pam.20137. [DOI] [PubMed] [Google Scholar]
- Tauras JA, Chaloupka FJ. Determinants of smoking cessation: An analysis of young adult men and women. In: Grossman M, Hsieh CR, editors. Economics of substance abuse. Northampton, MA: Edward Elgar Publishing Limited; 2001. pp. 337–364. [Google Scholar]
- Trotter L, Wakefield M, Borland R. Socially cued smoking in bars, nightclubs, and gaming venues: A case for introducing smoke-free policies. Tobacco Control. 2002;11:300–304. doi: 10.1136/tc.11.4.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakefield M, Chaloupka FJ, Kaufman NJ, Orleans CT, Barker DC, Ruel EE. Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: Cross sectional study. British Medical Journal. 2000;321:333–337. doi: 10.1136/bmj.321.7257.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson N, Sertsou G, Edwards R, Thomson G, Grigg M, Li J. A new national smokefree law increased calls to a national quitline. British Medical Journal. 2007;7:75. doi: 10.1186/1471-2458-7-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.