Abstract
Purpose Earlier research has shown that adaptation (i.e., the way in which employees cope with limitations resulting from their disease) is associated with sick leave. Our aim was to investigate signs of adequate or inadequate adaptation in employees with asthma and COPD. Methods A Q-methodological study was carried out among 34 workers with asthma or COPD. Results Four adaptation profiles were distinguished: the eager, the adjusted, the cautious, and the worried workers. The adaptation profiles provide insight into the different ways in which workers with asthma and COPD cope with their illness at work. Conclusions The adaptation profiles serve as a starting point for the design of appropriate (occupational) care. The eager workers experience little difficulties at work; the cautious workers may need assistance in learning how to accept their disease; the worried workers need reassurance, and may need reactivation; the adjusted workers deserve extra attention, and, when necessary, advice on how to live with their asthma or COPD.
Keywords: Asthma, COPD, Work, Coping, Sick leave, Q-methodology
Introduction
Employees with asthma and COPD report limitations in their ability to work [1]. Sick leave and work disability not only have financial consequences for their employers and society in general, but are also associated with a reduced quality of life for these employees [2]. Preventing sick leave is of major importance. Previous studies have shown that functional limitations, comorbidity, the severity of symptoms, and the presence of symptoms at work were associated with sick leave and work disability, whereas in a population of workers, pulmonary function measures, such as forced expiratory volume in 1 second (FEV1) were not [3, 4].
Illness perceptions play an important role in daily life functioning. In a population of pain patients, it was found that the patients who believed that they could control their pain, who avoided catastrophizing about their condition, and who believed they were not severely disabled, functioned better than those who did not [5]. In a population of patients suffering from a chronic disease, it was found that negative illness perceptions (such as finding the consequences of the illness more severe) were more prevalent in patients who were disabled from work than in patients with paid work [6].
Illness perceptions are associated with coping behaviours aimed at adaptation to health problems and limitations [7]. Previous research in patients with fibromyalgia and chronic pain has shown that when coping behaviours help to manage the demands, individuals make greater adjustments [8, 9]. However, a coping style which is emotion-focused was associated with poorer adjustment [10]. Earlier studies have also shown that people suffering from a chronic illness develop different coping strategies [11], which may be associated with different ways of adjusting to the limitations resulting from a chronic illness.
Little is known about coping strategies in relation to work and sick leave. It is important, therefore, to investigate coping and adaptation strategies that employees with a chronic illness apply in order to adjust to limitations at work and to continue working. In a previous study among workers with asthma and COPD we found indications that adaptation to functional limitations was associated with sick leave [12, 13]. However, we investigated specific aspects of adaptation only, and therefore did not obtain a complete overview of how these people adjusted their behaviour. Examples of relevant aspects of adaptation we investigated included coping with boundaries, attitude towards informing others about their disease, disease-related emotions and attitudes with regard to functioning at work.
The aim of this study was to investigate the different ways in which workers with asthma and COPD adapt to limitations at work. In addition, we aimed to investigate signs of adequate or inadequate adaptation.
Methods and Data
Q-methodology
Although Q-methodology has been applied in research on a range of health issues [14–20] it is still seen as a relatively new method. Q-methodology is a mixed qualitative–quantitative method that provides a foundation for the systematic study of subjectivity, such as people’s viewpoints, beliefs, attitudes, opinions and the like, and is a more robust technique than alternative methods for the measurement of attitudes and subjective opinion [14–22].
The aim of a Q-methodological study is to reveal the principal views with regard to a certain topic. Typically, respondents are presented with a sample of statements about the topic (in this case, adaptation to asthma and COPD in relation to functioning at work) called the Q-set. Respondents, called the P-set, are asked to rank-order the statements from their individual point of view (in this case, agreement). By ranking the statements people give their subjective meaning to the Q-set, and thus reveal their subjective viewpoint [23]. This approach is different from a questionnaire approach, since a qualitative part is included. All participants are asked to describe their arguments for the items they agreed with most and least. The individual rankings, called Q-sorts, are then correlated and factor-analyzed in order to reveal (dis)similarities in viewpoint; Stephenson [24] presented Q-methodology as an inversion of conventional factor-analysis, in the sense that Q correlates persons instead of tests (i.e., by-person-related factor-analysis). If each individual had his/her own specific likes and dislikes, their Q-sorts would not correlate. If, however, significant clusters of correlations exist, they can be factorized, and described as common viewpoints, and individuals can be mapped for a particular factor.
An important aspect is that Q-methodology typically focuses on investigating the range of viewpoints shared by specific groups of people [22]. Q-methodology can thus be used to reveal and describe a group of viewpoints and not, like with conventional factor analysis, a group of people. For this purpose, a small sample of specifically selected respondents is sufficient [17, 25]. However, a Q-methodological study will not provide any information about the number of people who adhere to any of the revealed viewpoints or how these are associated with the characteristics of the people or the context [26].
The Statements
Based on previous research and scientific literature [6, 12], we constructed a list of issues that are potentially relevant for employees with asthma or COPD, to assess their limitations in general and their limitations at work in particular:
Views about acceptance of functional limitations resulting from asthma and COPD
Insight into the disease and own role in their disease
Ways in which they cope with their own boundaries
Views about revealing their functional limitations to others
Views about openness with regard to the disease
Attitudes towards functioning at work in relation to asthma and COPD
Emotions related to the disease
Views about sick leave from work.
Two researchers formulated opinion statements with regard to adaptation, and these were discussed and adjusted by all authors. The result was a long list, which was structured to address the above-mentioned issues, stripped of double and similar statements, and condensed to form a broadly representative sample of 42 statements: the Q-set (Table 1). Finally, the statements were edited, randomly assigned a number, and printed on small yellow cards.
Table 1.
Q-statements and factor arrays
| Statements | Adaptation profiles | ||||
|---|---|---|---|---|---|
| A | B | C | D | ||
| 1 | Due to my lung disease, I cannot do as much as other people of my age | 3 | 4 | 0 | 4 |
| 2 | I find it difficult to accept that I am not completely healthy | −1 | 4 | 2 | 0 |
| 3 | I am ashamed of my lung disease | −4 | −3 | −2 | −3 |
| 4 | I feel equal to others, I just have a lung disease | 4 | 3 | 1 | 0 |
| 5 | I prefer to pretend I don’t have a lung disease | 3 | 0 | 2 | −2 |
| 6 | I am worried about my health | 0 | 2 | −1 | 3 |
| 7 | I live a healthy life | −1 | 1 | 3 | −1 |
| 8 | I feel healthy | −1 | 1 | 0 | −4 |
| 9 | I am not preoccupied with my health very much | 0 | 0 | −3 | −4 |
| 10 | I want to know everything about the consequences and the treatment of my lung disease | 1 | 1 | 1 | 0 |
| 11 | I stick to the advice of physicians and other professional helpers | 1 | 2 | 1 | 1 |
| 12 | I adjust my own medication when necessary | 1 | −1 | 3 | 0 |
| 13 | It is more important to live a pleasant life now than to be compliant with treatment | 1 | 0 | 0 | −1 |
| 14 | I always take my medication on time | 4 | 2 | 1 | 2 |
| 15 | When you have a lung disease, it is important to learn to say ‘no’ straight away | 1 | 3 | 2 | 3 |
| 16 | I slow down at work to save energy for my activities at home | −1 | −1 | −3 | −1 |
| 17 | I primarily need my holidays to recover | −4 | 0 | 1 | 0 |
| 18 | I’d rather not start an activity when I expect it to cause dyspnoea or fatigue | 1 | −1 | −1 | 0 |
| 19 | During weekends I am often exhausted | −3 | 0 | 0 | 1 |
| 20 | People often approach me differently when they know about my lung disease | 0 | −2 | −1 | −1 |
| 21 | When tobacco smoke bothers me, I say so | 0 | 3 | 1 | 0 |
| 22 | My employer knows about my lung disorder | 2 | 1 | 0 | 3 |
| 23 | I find it easy to ask for help from others when I have dyspnoea or fatigue | −1 | 1 | −4 | 0 |
| 24 | I try to take my medication without anyone seeing me | 2 | −4 | −1 | −2 |
| 25 | My colleagues do not know that I have a lung disorder | −1 | −3 | −1 | −1 |
| 26 | My colleagues understand that I cannot do as much as them because of my lung disorder | 0 | −2 | −1 | 1 |
| 27 | My employer understands that I cannot do everything because of my lung disorder | 0 | 0 | −2 | 2 |
| 28 | It is difficult to explain to others what it means to develop dyspnoea or fatigue as quickly as I do | 3 | −1 | 0 | −1 |
| 29 | I would sincerely regret it if I could not work anymore | 1 | 2 | 4 | 2 |
| 30 | It would be a solution when I did not have to work anymore | −2 | −4 | −4 | −1 |
| 31 | My employer does not take my lung disorder into account | −3 | −1 | 0 | −3 |
| 32 | My work is well adapted to my lung disorder | −1 | 0 | −2 | −2 |
| 33 | I try to arrange my work to minimize limitations resulting from my lung disorder | 0 | 1 | 1 | 1 |
| 34 | I have to slow down at work because of my lung disorder | −2 | 0 | −1 | 2 |
| 35 | My lung disorder makes me uncertain | −2 | −1 | −2 | 1 |
| 36 | I am ashamed that I do not function well because of my lung disorder | 0 | −3 | 0 | −3 |
| 37 | It is difficult that I don’t know now how I will feel tomorrow | 2 | 0 | 0 | 4 |
| 38 | I feel sad about the things I can no longer do | 0 | −1 | −3 | 0 |
| 39 | I prefer to take a day off than to take sick leave | 0 | −2 | 2 | 0 |
| 40 | I find it difficult to take sick leave | −3 | −2 | 4 | 1 |
| 41 | When I take sick leave, I increase the workload of others | −2 | 0 | 3 | −2 |
| 42 | It is better to take sick leave than to outrun yourself | 2 | 1 | 0 | 1 |
A “+4” score indicates that a typical worker with asthma or COPD in that profile would agree most with that statement, a “−4” score that (s)he would agree least (see also Fig. 1). Statements with a score of +4, +3, −3, or −4 score for a factor (or adaptation profile) are considered to characterize that factor. Values belonging to statements with a statistically different factor rank-order when compared with all other factors (P < .05; in bold type) are considered to distinguish that factor. Values belonging to statements that do not have a statistically significant rank-order for any factor are called consensus items, and are presented in italics
The Respondents
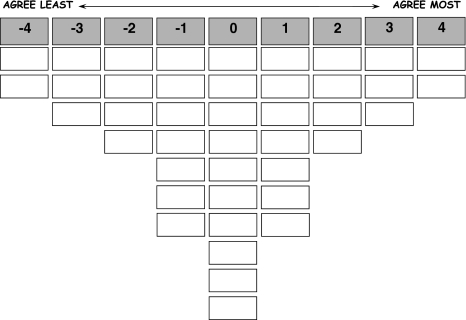
Participants were recruited in the city or direct neighbourhood of Nijmegen (The Netherlands) by personal invitation from their general practitioner or occupational physician. All Q-sorts were administered in an interview setting. The participants were asked to read the 42 cards with statements carefully and to sort them into three piles: statements with which they agreed, statements with which they disagreed, and statements which they were neutral about or did not apply to them. Next, they were asked to rank-order the statements, one pile at a time, using a quasi-normal distribution ranging from least agree to most agree (Fig. 1). Finally, they were asked to motivate their choice for the two statements they agreed with most and the two statements they agreed with least, to express any other thoughts about the statements or the experiment, and to complete a short questionnaire.
Fig. 1.
Score sheet (the scores −4 to +4 were not shown on the score sheet used by respondents)
The Questionnaire
The questionnaire consisted of 13 questions about personal characteristics (level of education, living situation), disease characteristics (time since diagnosis, functional limitations, comorbidity), lifestyle (smoking), work characteristics (number of hours of work per week, type of employment) and sick leave (frequency and duration).
Q-Analysis
The individual Q-sorts were factor-analysed. For each resulting factor, an idealized Q-sort (or composite sort) was computed. This is a weighted average ranking of the statements, computed on the basis of the Q-sorts of the respondents associated with that factor (P < .05), with the correlation coefficients as weights. This composite sort represents how a hypothetical participant with a 100% loading on the factor would have ranked the 42 statements. Table 1 represents the composite sorts of the four adaptation profiles. A rank value of “+4” indicates that the statement is positioned at the extreme right hand side of the distribution in that adaptation profile (“agree most); a “−4” at the extreme left (“agree least”; see Fig. 1).
The composite sorts are used to interpret and describe the resulting factors. A first interpretation of a factor, giving a first impression of what the adaptation profile is all about, is based on the statements characterizing that factor (those with a rank value of “+4”, “+3”, “−3”, “−4” in the composite sort; Table 1). Differences and similarities between the factors are then highlighted on the basis of the distinguishing statements (those with a statistically significantly different rank value on that factor, compared to all other factors) and the consensus statements (those that do not distinguish between any of the identified factors). Finally, the remarks that respondents loading on a factor made to explain their ranking of the statements are used for further clarification and interpretation. These remarks are also used to describe the adaptation profile.
Results
Thirty-four patients participated in this study (Table 2). Q-analysis of the 34 Q-sorts revealed four distinct factors, i.e., profiles of adaptation to functional limitations by workers with asthma and COPD. Each factor was defined by four or five variables (i.e., Q-sorts statistically significantly associated with the factor) and explained 5–19% of the variance in the Q-sorts (42% in total). In the following description of the adaptation profiles we made use of remarks from the participants, which are presented in italics and between quotation marks. The figures in between brackets correspond with the numbers of the statement (Table 1).
Table 2.
Characteristics of the study population
| Characteristics | Value |
|---|---|
| Gender (male/female) | 14/20 |
| Agea | 49.6 (9.1) |
| Diagnosis (asthma/COPD) | 20/14 |
| Years since diagnosisa | 21.8 (18.7) |
| Comorbidity (% yes) | 71 |
| Work (hours/week)a | 32.9 (10.8) |
| Sick leave (episodes per year)a | 2.1 (2.4); range: 0–10 |
| Mean duration of sick leave episode (days)a | 6.1 (16.2) |
| Episode of sick leave with longest duration (days)a | 60.2 (93.2) |
| Perceived limitations due to lung disease (score range 1–4)a | 2.2 (0.8) |
aPresented as mean (standard deviation)
Adaptation Profile A
People with this profile manage their disease well and do not need their weekends or holidays to recover (17, 19). “Especiallyinmyweekends and holidays I want to do a lot of things. By taking a break at the right time, I don’t get exhausted.” They do not find it difficult to take sick leave (40) and do not think that they increase the work load of their colleagues (41).
More than the other groups, they prefer not to start an activity if they expect it to cause dyspnoea (18). They admit that they cannot do as much as other people of the same age (1). They prefer to pretend that they are not sick (5) and try to take their medication in secrecy (24), although more than all the other profiles, they say that they always take their medication on time (14). “I don’t want myself or others to experience the consequences of my asthma. I want to function as normally as possible.” “When I exercise with people of my own age, I feel that I can’t keep up with them. I have to learn to accept this in sports.”
Although people in this profile try to take their medication in secrecy, they say not to be ashamed about having a lung disease (3) and do not feel less worthy because of this (4). “It’s true that I have asthma, but there really is nothing I can do about it.” “I didn’t ask to get this disease, but that’s the way it is, and I try to perform the best I can, and I’m not ashamed of it.”
They have informed their employer about their disease (31), but find it difficult to explain their symptoms to others (28) “People in my social environment acknowledge that there’s something wrong with me, but they immediately forget about it. Sometimes, I wish they would have asthma for a day.” “When people hear that you’ve got COPD, they think you should be wheezing and coughing all day. They don’t seem to understand that my symptoms come and go.” They find it difficult that they cannot predict how they will feel the next day (37). “Making plans is a good thing, but it is very inconvenient that my condition can change rather quickly.” This profile consisted of both asthma and COPD patients.
Adaptation Profile B
People in this profile cannot do as much as people of their own age (1), they find it difficult to accept that they are not completely healthy (2), and they worry about their health (6). “My lung disease won’t go away, it’s there to stay!”; “I would very much like to be healthy again and no longer bothered by my disease”; “There are a lot of things I would still like to do, but can’t because I’m short of breath”. Most of all profiles, they do not adjust their treatment themselves (12). In addition, when they are sick, they take sick leave, rather than just a day off (39).
Like profile A, they are not ashamed of their disease (3, 36). “Why should I be? It just happens to you…”; “Having a disease is not something to be ashamed of or to feel insecure about; it’s not something you’ve chosen, and there’s little you can do about it; “I’m not ashamed of having a disease, but I’m often gloomy when I feel ill”. They feel equal to others (4), and do not think that others approach them differently (20).
In addition, they do not attempt to take their medication in secrecy (24), and they have informed their colleagues about their disease (25). However, their colleagues do not sufficiently understand that they cannot do as much as them (26). They mention that it is important to respect their own boundaries (15) and to speak out and say that they are hindered by tobacco smoke (21). “It’s important to say ‘no’ straight away, because otherwise you suffer the consequences yourself”. It’s best to explain to your colleagues why you have to say ‘no’.”
They do not think that quitting work is a solution (30). “Working is pleasant, challenging and sociable; if I had to stop working I would miss it terribly”; “If I didn’t work anymore, I would miss a lot of things and not be able to show my talents. I want to work until I’m 65”. This profile consisted of asthma as well as COPD patients.
Adaptation Profile C
This group appears to experience the least limitations of all groups (38). They can do just as much as people of their own age (1) and, of all profiles, they have the least worries about their health (6). They are busy living a healthy life (3, 9) and adjust their medication when necessary (12).
They are highly motivated to work (29, 30). “I love my work too much to be able to live without it.” “Work plays a very important role in my life, with respect to self realization, and sense giving and satisfaction. I will always strive to find the most suitable work for my health and qualities and continue working.” “Not working is not an option for me, I need it to give purpose to my life.” They function at work without trying to save energy for activities at home (16), and find it difficult to ask others for help when they have health problems (23). “I don’t want to be seen differently.” “I find it very difficult to draw attention to my health when I experience limitations at work. It feels like asking for negative attention.” “As long as I can cope with it myself, I won’t bother others about it when I feel bad. Besides, they support me without asking; I find that difficult!”
In addition, they find it difficult to take sick leave (39, 40). “I only take sick leave when it’s the only option; I feel a lot of responsibility, and I think that I’ve set my limits very high. I’m hardly ever ill.” They also report that sick leave increases the work load of their colleagues (41). “My sick leave will cause delays for others who depend on me. Often, when I return to work I have to make up for this delay.” “The pressure on my colleagues increases. This will cause them to make mistakes, or increase the chance that they will become ill. When there’s any chance that I’ll be able to function at work, I’ll be there.” “I don’t want others to know about my disease, they might panic.”
Keeping these citations in mind, it is well imaginable that the employers of the people in this profile least understand that they cannot always perform as well as usual because of their disease (27). This profile consisted of asthma patients only.
Adaptation Profile D
This group appears to experience the most health complaints (8) and are worried about it (6). “I don’t feel healthy; I experience limitations that are unpleasant.” “I can hardly climb the stairs.” “It makes me uncertain in my work. Afraid to become dyspnoeic …. Dyspnoea is frightening.” In addition, they are very much preoccupied with their health (9). “I’m confronted with my dyspnoea all the time, so I’m also preoccupied with my health all the time.” They cannot do as much as their peers (1), and have to slow down at work (34). “All the time my condition becomes worse.” “It’s frustrating to be confronted with this.” “I’m confronted with my disease every day.” They do not pretend not to have a disease (5), and take their medication in public (24). They find it difficult that they cannot predict how they will feel the next day (37). They are not ashamed of their disease (3, 36). “I used to be ashamed. I used to be, but not any more.” They have learned that it is important to say ‘no’ straight away (15). “When I have a good day, I use all my energy. The next day, I can’t do a thing.”
Their employer knows about their disease (22), takes it into account (31) and understands that they are unable to do everything (27). However, their work is not sufficiently adapted (32). “Can’t get any worse; I work in a launderette.” This profile consisted of COPD patients only.
Discussion
The results of the present study show that within a population of employees with asthma and COPD, it is possible to distinguish different profiles in adaptation to the consequences of the disease at work. Each profile represents a different group of patients, who require a different approach from the occupational physician in the management of their diseases.
Four Profiles of Adaptation
Adaptation Profile A: Adjusted Workers
We have called this group the ‘adjusted workers’, because they have found a way in which to adapt to their limitations, by choosing a way of life in which they can slow down at work in order to reduce their limitations. These workers are limited but striving for normalcy. They pace their activity and adhere to their medications. They accept their limitations and are not overly emotionally preoccupied. At work, they do this by taking breaks regularly. Their attitude is to set strict limits to their performance at work, in order to save sufficient energy for their free time. They appear to have a strong need for control. It can be hypothesized that these workers were sufficiently assertive to make their needs known to the employer.
People within this profile prefer not to discuss why they take breaks more often, because they think that they cannot explain to others what it is like to have a pulmonary disease. They take their medication in secrecy in order to avoid questions from others. They do expect others to take their disease into account, although they don’t feel really understood by others. However, this does not seem to be an emotional issue but rather a functional and practical one.
When working is hampered due to functional limitations caused by asthma or COPD, frustrations may occur. This is well imaginable in case of severe asthma with an irregular course, or with the chronic dyspnea in COPD. When people do not achieve their goals anymore, two options are available: try harder or adjust the goals [27]. People in this profile appear to have adjusted their goals. The process of adjusting goals is called ‘adaptive self-regulation’ and occurs to avoid the negative psychological and physical consequences resulting from the experience of unattainable goals [28]. Goal adjustment consists of two processes: disengage from the unattainable goal and reengage in goal-directed effort elsewhere. This helps to maintain a sense of purpose in life and buffer the negative emotions associated with the inability to make progress towards desired goal. People who are better able to abandon unattainable goals and to reengage in other meaningful activities should experience greater subjective wellbeing and better physical health [28].
Adaptation Profile B: Cautious Workers
People in profile B are referred to as ‘cautious workers’. They worry about their health and have not (yet) accepted the fact that they are no longer able to do everything they used to do.
Acceptation of the disease and its limitations is a necessary step in the adaptation process. Acceptation of the disease and its limitations is a necessary step in the adaptation process. Patients suffering from a chronic illness have to learn to engage in meaningful activities in daily life regardless the occurrence of mild health complaints like dyspnea or fatigue, without unnecessary attempts to change their frequency or form [29]. It can be considered as an alternative to experiential avoidance [30].
These people appear to experience many negative consequences of their illness and to focus on limitations rather than on the things that they can still do. This may be explained by the fact that their limitations are more severe compared to the other profiles. Severe limitations make it difficult to focus on other things. However, the inclination to avoid dyspnea in case of asthma or COPD may lead to isolation. Accepting some dyspnea may be the solution to continue participation in meaningful activities, such as work.
They are not ashamed about their disease, and they are open about it towards colleagues. However, they feel that the people at work do not fully understand their condition. They are very cautious about their health, and take sick leave whenever they think it is necessary. They are also too worried about their health to manage their medication themselves by adjusting the dose. They will not outrun themselves, and their health worries may in fact hinder them from discovering their personal limits.
Despite of their cautiousness and perceived limitations, the people in this group are still functioning in paid work. They prefer to maintain their job instead of becoming work-disabled, because they would miss the pleasant, challenging and social aspects of work. However, it can be hypothesized that these cautious workers are more limited because of their fear of dyspnoea and further health complaints. Because of the objective severity of their lung disease, dyspnoea and health complaints cannot be avoided completely. Therefore, an additional interpretation of the behaviour in this profile is within the context of the fear-avoidance model, which hypothesizes that activities associated with health complaints (e.g., pain or dyspnoea) will be avoided. This avoidance may lead to further development or, at least, retention of the disability [27]. People in this group might function better if they would dare to try harder. The occupational physician or general practitioner may be able to assist in this process. It may be valuable to explore the applicability and effectiveness of Acceptance and Commitment Therapy (ACT) within lung patients fitting the characteristics of this profile. ACT aims to increase psychological flexibility, which is defined as the ability to contact the present moment more fully and conscious, and to change or persist in behaviour when doing so serves valued goals [31]. The applicability of such an intervention and the role of the occupational physician in (referring to) ACT needs further investigation.
Adaptation Profile C: Eager Worker
This profile appears to have the least limitations of all profiles, and these people are highly motivated to continue their work. Since they find it difficult to talk about their disease, or to take sick leave when they have health problems, the rate of sick leave will be rather low in this group. Unlike profile A, people in this group do not emphasize their illness. This may be explained by the fact that this group only experiences mild limitations. The fact that this profile consists of only asthma patients subscribes this, since the manifestation of asthma may be mild, when controlled properly. Another interpretation is that these workers reflect the early stage of illness and adaptation, including a relatively mild disease severity. It might be hypothesized then that this group eventually enters the other profiles when their limitations increase. Especially in progressive disease such as COPD, limitations will become more prevalent in time. The more limitations, the higher the need will become to face them and change the behaviour accordingly.
This group functions well at work and does not face many problems. However, when our hypothesis is true that this is the first stage in the process of adaptation, this group deserves attention from a prevention point of view. It should be kept in mind that this group is difficult to identify, because they do not take sick leave, or only seldom, and their employer may not know that they have asthma or COPD.
Adaptation Profile D: Worried Workers
These workers report the greatest functional impacts and emotional preoccupation with a progressive and troubling illness, which is following expectations, since this profile consists of COPD patients only. The relatively larger health problems in this profile may be related to longer duration of the disease. This may have helped people in this group to find a way to adapt to the limitations they experience. They feel adequately supported and do not feel stigmatized. People in this group resemble the cautious workers, but it is hypothesized that they face their limitations everyday, whereas the cautious workers do their utmost to prevent limitations. This difference may be due to a difference in illness severity, but it may also be due to differences in health perception or personality between the two groups.
Occupational physicians can help this group to accept the deterioration of their health status, and may play a role in optimizing the working environment or workload to prevent unnecessary complaints caused by sub-optimal work conditions. In addition, the margin of manoeuvre could be increased. This can be achieved by modifying organisational or work practices, such as modification of work pace or work schedule [32]. The supervisor and/or the employer play an important role in the modification process. Early contact between the employee and the supervisor, and an advice of the occupational physician in order to create goodwill and trust are important determinants of return to work, as is shown in studies on return to work following musculoskeletal disorders [33, 34]. Reference for psychotherapy might be useful to redress the consequences of anxiety for or emotional preoccupation with dyspnoea, fatigue and further limitations. In addition, it has to be kept in mind that these workers might be ‘worried’ due to comorbidity, since depression and anxiety disorders frequently occur among patients with COPD [35].
Methodological Considerations
Asthma and COPD are distinct diseases, but from the perspective of this study they are considered as one disease. The health complaints are comparable, but the course of the two diseases is rather different. Asthma has a course of intervals with ups and downs, whereas COPD is slowly progressive. This may have had consequences for the profiles. The eager group consists of asthma patients only, and all workers in the worried profile reported that they had COPD. The other two profiles consisted of both asthma and COPD patients.
We have no information about the disease severity, but previous research has shown that within a population of workers this is not a main determinant of their functioning at work [11]. However, it is well imaginable that the differences between our profiles can, at least, be partially explained by differences in perceived limitations, resulting from differences in disease severity as has been stressed above.
Unfortunately, we did not include specific items about the work context in our Q-set and we do not have information about job titles. Therefore, it cannot be ruled out that differences in the work context of the participants may partly have accounted for the differences found between the profiles.
The Q-methodological approach requires a heterogeneous group of participants with a variety of viewpoints and opinions regarding the topics under study. Ideally, the variety of viewpoints in the sample that participates in the study agrees with that in the population at large, in this case all workers with asthma and COPD. In qualitative studies representativeness refers to the variety of viewpoints, rather than to the prevalence of it. We have used different strategies to recruit patients to obtain this heterogeneity. However, it cannot be ruled out that with other recruitment strategies a sample of workers with asthma or COPD would have been included with a different set of viewpoints, leading to differences in the profiles found.
It can be suggested that the differences that were found between the adaptation profiles are partly the result of the socially accepted and reported behaviour of workers with asthtma or COPD. Some information bias might be possible due to the reporting of socially accepted behaviour and attitudes.
Implications for Research and Practice
In this paper four different adaptation profiles are presented. It becomes clear that it is possible to distinguish different ways in which people suffering from asthma or COPD cope with their limitations at work. Patients develop different coping strategies [10], and each profile requires a different approach from the professional. Some profiles may lead to avoidance of sick leave despite serious complaints, whereas others may need some encouragement to continue working or return to work, and to increase their activities. The eager workers form a difficult subgroup in this respect, because they either experience fewer health complaints, or seem to be inclined to mask being ill. Future research should focus on how to assist this specific group in accepting their asthma or COPD.
When considering these profiles, it can be hypothesized that they are also applicable to other chronic illnesses, or maybe even to populations without a chronic illness, which is in agreement with the findings of previous studies on determinants of working and sick-leave [6, 36]. Further research is needed to investigate this Q-set in other patients with chronic diseases, such as diabetes or rheumatoid arthritis.
Another focus of research would be to investigate the process of adaptation in a longitudinal study. When workers with asthma or COPD become older, many others in their age-group will experience limitations due to chronic illness. This may contribute positively to the process of acceptation and adaptation. Based on the present findings, personality, work satisfaction, motivation to continue working, and the role of work context are also aspects that need to be investigated.
Acknowledgments
We would like to thank Ms. Marian Vermeulen for performing the Q-interviews, and the anonymous referee for the very constructive comments.
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Contributor Information
C. R. L. Boot, Phone: +31-20-4449680, FAX: +31-20-4448387, Email: crl.boot@vumc.nl
N. J. A. van Exel, Email: n.vanexel@erasmusmc.nl
J. W. J. van der Gulden, Email: j.vandergulden@elg.umcn.nl
References
- 1.Eisner MD, Yelin EH, Trupin L, Blanc PD. The influence of chronic respiratory conditions on health status and work disability. Am J Public Health. 2002;92:1506–13. [DOI] [PMC free article] [PubMed]
- 2.Orbon KH, Schermer TR, van der Gulden JW, Chavannes NH, Akkermans RP, Schayck OP, et al. Employment status and quality of life in patients with chronic obstructive pulmonary disease. Int Arch Occup Environ Health. 2005;78:467–74. [DOI] [PubMed]
- 3.Balder B, Lindholm NB, Lowhagen O, Palmqvist M, Plaschke P, Tunsater A, et al. Predictors of self-assessed work ability among subjects with recent-onset asthma. Respir Med. 1998;92:729–34. [DOI] [PubMed]
- 4.Blanc PD, Jones M, Besson C, Katz P, Yelin E. Work disability among adults with asthma. Chest. 1993;104:1371–7. [DOI] [PubMed]
- 5.Jensen MP, Turner JA, Romano JM, Karoly P. Coping with chronic pain: a critical review of the literature. Pain. 1991;47:249–83. [DOI] [PubMed]
- 6.Boot CR, Heijmans M, van der Gulden JW, Rijken M. The role of illness perceptions in labor participation of the chronically ill. Int Arch Occup Environ Health. 2008;82:13–20. [DOI] [PMC free article] [PubMed]
- 7.van der Hulst M, Vollenbroek-Hutten MM, Ijzerman MJ. A systematic review of sociodemographic, physical, and psychological predictors of multidisciplinary rehabilitation-or, back school treatment outcome in patients with chronic low back pain. Spine. 2005;30:813–25. [DOI] [PubMed]
- 8.Jensen MP, Karoly P. Control beliefs, coping efforts, and adjustment to chronic pain. J Consult Clin Psychol. 1991;59:431–8. [DOI] [PubMed]
- 9.Johnson LM, Zautra AJ, Davis MC. The role of illness uncertainty on coping with fibromyalgia symptoms. Health Psychol. 2006;25:696–703. [DOI] [PMC free article] [PubMed]
- 10.Quiles Marcos Y, Terol Cantero MC, Romero Escobar C, Pagan Acosta G. Illness perception in eating disorders and psychosocial adaptation. Eur Eat Disord Rev. 2007;15:373–84. [DOI] [PubMed]
- 11.Larun L, Malterud K. Identity and coping experiences in chronic fatigue syndrome: a synthesis of qualitative studies. Patient Educ Couns. 2007;69:20–8. [DOI] [PubMed]
- 12.Boot CR, van der Gulden JW, Orbon KH, Vercoulen JH, Akkermans R, van Weel C, et al. Asthma and chronic obstructive pulmonary disease: differences between workers with and without sick leave. Int Arch Occup Environ Health. 2004;77:357–62. [DOI] [PubMed]
- 13.Boot CR, Vercoulen JH, van der Gulden JW, Orbon KH, Rooijackers JM, van Weel C, et al. Predictors of changes in sick leave in workers with asthma: a follow-up study. Int Arch Occup Environ Health. 2005;78:633–40. [DOI] [PubMed]
- 14.Bryant LD, Green JM, Hewison J. Understandings of down’s syndrome: a Q methodological investigation. Soc Sci Med. 2006;63:1188–200. [DOI] [PubMed]
- 15.Bullington P, Pawola L, Walker R, Valenta A, Briars L, John E. Identification of medication non-adherence factors in adolescent transplant patients: the patient’s viewpoint. Pediatr Transplant. 2007;11:914–21. [DOI] [PubMed]
- 16.Kreuger L, van Exel J, Nieboer A. Needs of persons with severe intellectual disabilities: a Q-methodological study of clients with severe behavioural disorders and severe intellectual disabilities. J Appl Res Intellect Disabil. 2008;21:466–76. [DOI]
- 17.Risdon A, Eccleston C, Crombez G, McCracken L. How can we learn to live with pain? A Q-methodological analysis of the diverse understandings of acceptance of chronic pain. Soc Sci Med. 2003;56:375–86. [DOI] [PubMed]
- 18.Stenner PH, Dancey CP, Watts S. The understanding of their illness amongst people with irritable bowel syndrome: a Q methodological study. Soc Sci Med. 2000;51:439–52. [DOI] [PubMed]
- 19.Tielen M, van Staa AL, Jedeloo S, van Exel NJ, Weimar W. Q-methodology to identify young adult renal transplant recipients at risk for nonadherence. Transplantation. 2008;85:700–6. [DOI] [PubMed]
- 20.van Exel J, De Graaf G, Brouwer W. Care for a break? An investigation of informal caregivers’ attitudes toward respite care using Q-methodology. Health Policy. 2007;83:332–42. [DOI] [PubMed]
- 21.van Exel NJ, De Graaf G, Brouwer WB. “Everyone dies, so you might as well have fun!” Attitudes of Dutch youths about their health lifestyle. Soc Sci Med. 2006;63:2628–39. [DOI] [PubMed]
- 22.Smith NW. Current systems in psychology: history, theory, research, and applications. Belmont, CA: Wadsworth; 2001.
- 23.Stephenson W. Correlating persons instead of tests. Charact Pers. 1935;4:17–24.
- 24.Watts S, Stenner P. Doing Q-methodology: theory, method and interpretation. Qual Res Psychol. 2005;2:67–91. [DOI]
- 25.Brown SR. Political subjectivity: applications of Q methodology in political science. New Haven/London: Yale University Press; 1980.
- 26.Oyeflaten I, Hysing M, Eriksen HR. Prognostic factors associated with return to work following multidisciplinary vocational rehabilitation. J Rehabil Med. 2008;40:548–54. [DOI] [PubMed]
- 27.Coutu MF, Baril R, Durand MJ, Cote D, Rouleau A. Representations: an important key to understanding workers’ coping behaviors during rehabilitation and the return-to-work process. J Occup Rehabil. 2007;17:522–44. [DOI] [PubMed]
- 28.Rasmussen HN, Wrosch C, Scheier MF, Carver CS. Self-regulation processes and health: the importance of optimism and goal adjustment. J Pers. 2006;74:1721–47. [DOI] [PubMed]
- 29.McCracken LM, Carson JW, Eccleston C, Keefe FJ. Acceptance and change in the context of chronic pain. Pain. 2004;109:4–7. [DOI] [PubMed]
- 30.Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44:1–25. [DOI] [PubMed]
- 31.Powers MB, Zum Vörde Sive Vörding MB, Emmelkamp PM. Acceptance and commitment therapy: a meta-analytic review. Psychother Psychosom. 2009;78:73–80. [DOI] [PubMed]
- 32.Durand MJ, Vezina N, Baril R, Loisel P, Richard MC, Ngomo S. Margin of manoeuvre indicators in the workplace during the rehabilitation process: a qualitative analysis. J Occup Rehabil. 2009;19:194–202. [DOI] [PubMed]
- 33.Franche RL, Baril R, Shaw W, Nicholas M, Loisel P. Workplace-based return-to-work interventions: optimizing the role of stakeholders in implementation and research. J Occup Rehabil. 2005;15:525–42. [DOI] [PubMed]
- 34.MacEachen E, Clarke J, Franche RL, Irvin E. Systematic review of the qualitative literature on return to work after injury. Scand J Work Environ Health. 2006;32:257–69. [PubMed]
- 35.van den Bemt L, Schermer T, Bor H, Smink R, van Weel-Baumgarten E, Lucassen P, et al. The risk for depression comorbidity in patients with COPD. Chest. 2009;135:108–14. [DOI] [PubMed]
- 36.Baanders AN, Rijken PM, Peters L. Labour participation of the chronically ill. A profile sketch. Eur J Public Health. 2002;12:124–30. [DOI] [PubMed]