Abstract
Glaucoma, the second leading cause of blindness, is characterized by changes in the optic disc and visual field defects. The elevated intraocular pressure was considered the prime factor responsible for the glaucomatous optic neuropathy involving death of retinal ganglion cells and their axons. Extensive investigations into the pathophysiology of glaucoma now reveal the role of multiple factors in the development of retinal ganglion cell death. A better understanding of the pathophysiological mechanisms involved in the onset and progression of glaucomatous optic neuropathy is crucial in the development of better therapeutic options. This review is an effort to summarize the current concepts in the pathophysiology of glaucoma so that newer therapeutic targets can be recognized.
The literature available in the National Medical Library and online Pubmed search engine was used for literature review.
Keywords: Glaucoma, pathophysiology, retinal ganglion cells
Glaucoma, a leading cause of irreversible visual loss, is characterized by loss of retinal ganglion cells (RGC) and their axons over a period of many years. Glaucomatous optic neuropathy is characterized by changes in the optic disc and visual field defects.[1,2] The morphologic changes in the optic disc are in the form of thinning of neuroretinal rim, pallor and progressive cupping of the optic disc. The hemorrhage-associated retinal nerve fiber layer defects precede measurable changes of the optic disc configuration.[3] The visual field defects in glaucoma are often detected only after 40% of the axons are lost.[4]
The pathophysiology of glaucomatous optic neuropathy is not well understood. Whether the site of primary damage is the ganglion cell body or their axons remains fiercely debatable. Irrespective of the initial site of neuronal injury and mechanisms involved, the terminal outcome is the death of RGCs and their axons leading to irreversible visual loss. This paper presents a review of the various mechanisms involved in the development of glaucomatous optic neuropathy. The literature published during 1984 to 2006 was reviewed except for the two research papers (Lucas and Newhouse, 1957 and Onley, 1969) which were included to show that the important role of glutamate toxicity in glaucomatous optic atrophy has been suspected for a long time. All the literature reviewed was obtained from the National Medical Library and online Pubmed search engine. All articles referenced were published in English language journals.
Multifactorial pathogenesis of glaucoma
Glaucoma is a heterogeneous group of diseases and the pathophysiology of glaucoma is believed to be multifactorial. Multiple factors acting either on cell bodies or their axons are believed to lead to RGC death. According to various theories put forth, factors like elevated intraocular pressure (IOP) and vascular dysregulation primarily contribute to the initial insult during glaucomatous atrophy in the form of obstruction to axoplasmic flow within the RGC axons at the lamina cribrosa, altered optic nerve microcirculation at the level of lamina and changes in the laminar glial and connective tissue. The factors leading to secondary insult include excitotoxic damage caused by glutamate or glycine released from injured neurons and oxidative damage caused by over-production of nitric oxide (NO) and other reactive oxygen species. Whatever may be the primary and secondary factors, the end result in glaucomatous eyes is the dysfunction and death of RGCs leading to irreversible visual loss, as a result of a complex interplay of multiple factors rather than any one of them functioning individually.[5]
Neuronal loss in glaucoma by apoptosis
The characteristic change in the optic nerve head in glaucoma is a “cupping” of the optic disc where ganglion cell axons have been lost. The death of the axons is associated with a loss of ganglion cell bodies in the retina and ganglion cell axon terminals in the dorsal lateral geniculate body. Death of RGCs in glaucomatous human eyes and experimental animal models of glaucoma takes place by apoptosis,[6,7] which is also the means of eliminating 50% of the RGCs during normal developmental organization of the visual pathway.[8] Apoptosis is a process of programmed cell death in the absence of inflammation, characterized by DNA fragmentation, chromosome clumping, cell shrinkage and membrane blebbing.[9] Nuclear damage is followed by breaking down of the cell into multiple membrane-bound vesicles which are engulfed by neighboring cells. Some researchers have suggested preferential loss of larger ganglion cells in the retina belonging to parasol and midget cell classes[4,10–12] but this issue still remains debatable.[13] Although there are compelling evidences showing apoptosis as the primary and early mechanism of ganglion cell death in glaucoma, necrosis is also a contributory mechanism in the late phase, evidence to which was observed in rats subjected to optic nerve transection.[14]
The caspases, a family of cysteine aspartyl-specific proteases have emerged as the central regulators of apoptosis. These enzymes are present as inactive zymogens and once activated initiate an ordered cascade leading to proteolysis of key cytosolic and nuclear components and eventual destruction of the cell.[15] The activation of caspases involves an extrinsic and an intrinsic pathway. The extrinsic pathway involves interaction of specific ligands such as tumor necrosis factor-alpha (TNF-A) with the proapoptotic cell surface receptors while the intrinsic pathway is regulated by proapoptotic molecules released from the mitichondrion.[16] In rats subjected to axotomy, intraocular application of various caspase inhibitors rescued up to 34% of RGCs that would otherwise have died 14 days after optic nerve transection. Involvement of caspases in RGC apoptosis suggests the possible role of additional interventional strategies using caspase inhibitors.[17]
While the evidences suggest the central role of caspases in adult RGC death, there is a growing body of evidence suggesting involvement of caspase-independent pathways in RGC death under certain conditions. Spalding et al. have reported significant RGC death within 24 h of superior colliculus ablation in neonatal rats which was not inhibited by general or specific caspase inhibitors.[18]
Elevated intraocular pressure - the prime factor?
Until recently it was believed that elevated IOP plays a major role in RGC apoptosis and it is also true that reduction of elevated IOP often helps in slowing down the progression of degenerative changes in glaucoma. However, among glaucoma patients only one-third to half of all glaucoma patients have elevated IOP at the initial stages.[1,19,20] On an average, 30-40% of patients with glaucomatous visual field defects are being diagnosed as having normal tension glaucoma (NTG) in peripheral clinics.[21] Therefore, elevated IOP is now believed to be an important but not the only factor responsible for optic nerve damage.
Elevated IOP often results from alterations in aqueous humor dynamics due to changes in trabecular meshwork leading to impaired drainage of aqueous. The trabecular meshwork has been shown to exhibit cytoskeletal changes in cells,[22] altered cellularity[23,24] and changes in extracellular matrix (ECM).[25–27] Several investigators have studied the association of RGC loss and elevated IOP. A significant positive correlation has been observed between change in IOP and RGC death in glaucomatous rats.[28–30] A positive correlation has also been observed between the level and duration of elevated IOP and RGC axon loss.[29,30] Loss of half of the ganglion cells takes place during the initial two to three months of IOP elevation.[31–33] RGC death in experimental glaucoma has been shown to occur by the process of apoptosis[7,34] and IOP elevation can directly induce RGC death by apoptosis.[32] Results of a number of experiments suggest that RGC death after exposure to elevated IOP takes place in two phases. The first phase lasts for about three weeks, with loss of approximately 12% RGCs per week. This is believed to be followed by a second slower phase of neuronal loss.[32] The primary mechanism of neuronal loss in the initial phase is apoptosis[35] while in the second phase neuronal loss is due to toxic effects of the primary degenerating neurons in addition to continuing exposure to elevated IOP.[30]
Molecular mechanisms of retinal ganglion cell apoptosis in response to elevated intraocular pressure
Cellular responses to changes in IOP, leading to apoptosis of RGCs are not well understood. A possible mechanism of RGC apoptosis seems to be related to changes in extracelluar matrix components in the retina of glaucomatous eyes in response to elevated IOP. Extensive remodeling of the ECM, including collagen I and IV, transforming growth factor-ß2 (TGF-ß2), and matrix metalloproteinase (MMP)-1 have been detected in glaucomatous eyes.[36–38] ECM is responsible for providing adherence signals thereby controlling the cell functions and cell survival.[39] Therefore, changes in specific ECM components can interrupt cell-cell and cell-ECM interactions, leading to cell death by apoptosis.
MMPs are the major matrix-degrading enzymes. In a recent study enhanced MMP-9 activity was detected in apoptotic RGCs along with decreased deposition of laminin in the RGC layer suggesting increased degradation of the ECM at the retinal site in response to exposure to elevated IOP.[40] Laminin is an important ECM component, which facilitates cell adherence and survival by interacting with cellular integrins. Disintegration and loss of laminin as a result of increased amount of proteases such as MMP-9 leads to deficient cell-ECM communication thereby favoring cell loss by apoptosis.[41] Thus the results of the above-mentioned studies indicate that upon exposure to elevated IOP there is increased secretion of MMP-9 from RGCs leading to increased degradation of laminin and apoptosis. According to another explanation elevated IOP causes mechanical damage to RGC axons in the region of optic nerve head which progresses to retrograde damage of the RGC body. Damage to RGC bodies leads to enhanced secretion of MMPs, which in turn causes ECM changes and apoptosis. Another alternative theory suggests that increased MMP expression as a result of exposure to elevated IOP could be mediated indirectly by the excitatory neurotransmitter glutamate. Upregulation of glutamate receptors in retinal cells was found to be associated with increased MMP-9 expression.[42] It has also been demonstrated that exposure to elevated IOP leads to activation of retinal astrocytes.[43] These activated astrocytes release MMPs to bring about changes in the pattern of matrix remodeling.[44]
Growth factors and their receptors are known to regulate cellular functions, cytoskeletal organizations and components of ECM in ocular tissue. Trabecular meshwork, optic nerve astrocytes as well as lamina cribrosa cells express a wide variety of growth factors such as neurotrophin factor and TGF-ß2. These growth factors may play an important role by affecting the normal development and cellular functions in the trabecular meshwork as well as retina. In the retina retrograde axoplasmic transport block, as a result of elevated IOP can deprive the RGCs of the supply of brain-derived neurotrophin factor (BDNF), important for regulating cell metabolism and cell survival. Deficiency of BDNF can further lead to progression of RGC apoptosis.[45] These effects seem to be further modulated by increased release of TGF-ß2 by activated astrocytes in response to elevated IOP.[37]
Nakazawa et al., have now demonstrated rapid upregulation of TNF-A in rats with experimentally induced elevated IOP and this was followed sequentially by microglial activation, loss of optic nerve oligodendrocytes, and delayed loss of RGCs.[46] An upregulation of TNF-A in the astrocytes was also detected in human glaucomatous optic nerve head and this expression was found to parallel the progression of neurodegeneration. TNF-A stimulation seems to contribute to neuronal damage by both a direct effect on the axons of the RGCs and by inducing nitric oxide synthase (NOS)-2 in astrocytes.[47] A summary of mechanisms involved in RGC apoptosis secondary to elevated IOP is presented in Fig. 1.
Figure 1.
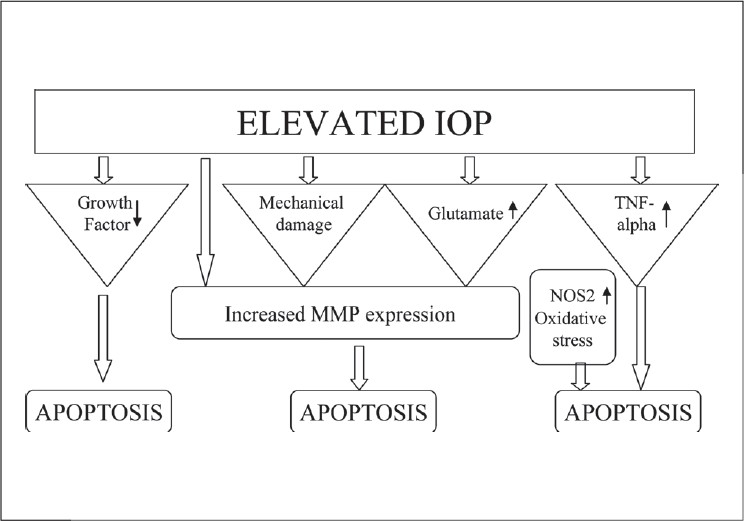
Mechanisms involved in glaucomatous RGC apoptosis secondary to elevated IOP. TNF-A - Tumor necrosis factor-alpha, MMP - Matrix metalloproteinase, NOS-2 - Nitric oxide synthase-2
Vascular insufficiency: Another important factor
Clearly, elevated IOP plays a major role in RGC damage in glaucomatous eyes but therapeutic control of IOP in many patients is not sufficient to improve the visual functions and arrest the progression of the disease process.[48,49] Besides, glaucomatous changes have been observed in individuals with normal IOP. This suggests a critical role of other factors in the initiation and progression of glaucomatous changes.
A number of circumstantial evidences point towards an association between vascular insufficiency and glaucoma. A positive association of glaucoma has been observed with migraine[50,51] and peripheral vascular abnormalities[52,53] that involve dysregulation of cerebral and peripheral vasculature respectively. Increased sensitivity to endothelin-1-mediated vasoconstriction is implicated in these vascular abnormalities. The possible role of this vasoconstrictor is also suspected in the pathogenesis of glaucoma as increased levels of endothelin-1 have been detected in the aqueous humor and plasma of glaucoma patients.[54–57] Further evidences indicating a positive association between glaucoma and vascular insufficiency were provided by magnetic resonance imaging in glaucoma patients revealing pan-cerebral ischemia[58] and increased incidence of cerebral infarcts.[59] Aging is also considered an important risk factor for glaucoma and a progressive decline in cerebral and ocular perfusion has been observed with increasing age.[60,61] Based on these observations it can be hypothesized that neuronal damage in glaucoma represents a chronic anterior ischemic optic neuropathy.
In a healthy eye, a constant flow of blood is required in the retina and optic nerve head so as to meet the high metabolic needs in these vital parts of the eye. To maintain a constant rate of blood flow an efficient autoregulatory mechanism operates in arteries, arterioles and capillaries over a wide range of day-to-day fluctuations in ocular perfusion pressure that is dependent on both the systemic blood pressure and IOP.[62] These autoregulatory mechanisms are not as robust in aging individuals as in youth. Evidence of this can be observed in a study done by Matsuura and Kawai, showing robust choroidal hyperperfusion in response to experimentally induced ocular hypertension in young rats while in older rats a similar increase in choroidal perfusion was not observed.[63] Thus, deficient autoregulatory mechanisms leading to ischemia contribute to the development of glaucomatous neuronal damage with increasing age. Primary open angle glaucoma (POAG) and NTG patients have also shown a chronically reduced optic nerve head and retinal blood flow[64,65] especially in people with low systemic blood pressure leading to reduced ocular perfusion pressure.[66] Reduced diastolic perfusion pressure is now recognized as an important risk factor for POAG.[67]
The molecular mechanisms leading to RGC death due to vascular dysregulation are not clearly understood. The vascular insufficiency can directly damage and cause RGC apoptosis. Upregulation of MMP-9 expression in circulating leucocytes has been observed in patients with vasospastic NTG.[68] The upregulation of MMP can be a direct response to ischemic injury or it can be a secondary response to increased levels of endothelin and TNF-A. The MMP produced by the circulating leukocytes of these patients might be involved in the partial barrier breakdown and RGC damage[69] [Fig. 2].
Figure 2.
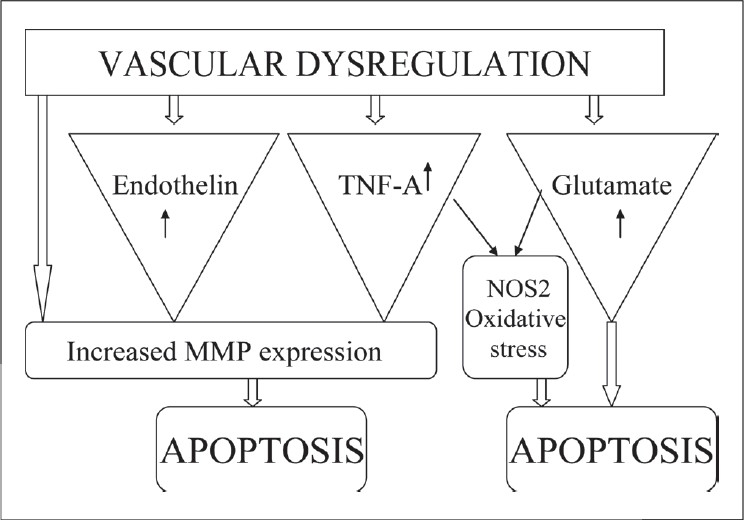
Mechanisms involved in glaucomatous RGC apoptosis secondary to vascular dysregulation. TNF-A - Tumor necrosis factor-alpha, MMP - Matrix metalloproteinase, NOS-2 - Nitric oxide synthase-2
Role of glutamate in retinal ganglion cell death
Apoptotic cell death of RGCs has also been attributed to glutamate-mediated toxicity and upon exposure to hypoxic conditions retinal cells are known to release glutamate.[70] The amino acid glutamate is an essential neurotransmitter in the central nervous system and retina. Concentrations of glutamate higher than the physiological concentration are toxic to neurons depending upon the duration and extent of increase in concentration. The toxicity following acute exposure to high levels of glutamate is well documented. This toxicity of glutamate was first described by Lucas and Newhouse in 1957 who observed severe destruction of RGCs after subcutaneous injection of glutamate in young mice.[71] A similar glutamate-induced retinal toxicity was also observed by Onley and as the lesions developed upon exposure to excess levels of excitatory neurotransmitter they were described as excitotoxic.[72] A minor but chronic elevation of glutamate was also found to be toxic to ganglion cells.[73]
Glutamate-mediated neurotransmission is via ionotropic and metabotropic receptors [Fig. 3]. The ionotropic glutamate receptors include N-methyl-D-aspartate (NMDA), kianate (KA) and alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPA) receptors. The metabotropic receptors (mGluR) are G protein-linked receptors and are divided into three groups. Glutamate-induced excitotoxicity is primarily mediated by ionotropic NMDA subtype receptors.[74,75] NMDA receptor activation leads to opening of associated ion channels and the entry of extracellular Ca++ and Na+ into the neurons. Glutamate-mediated neuronal toxicity is dependent on the influx of extracellular Ca+, which in turn acts as second messenger to activate downstream signaling pathways finally leading to cell death.[74,76,77] Experimental administration of NMDA-antagonists has been shown to prevent glutamate-induced excitotoxicity.[78] In addition, tissue plasminogen activator (tPA) present in retinal neurons has also been suggested to be an important endogenous factor facilitating NMDA-mediated excitotoxicity. Although the mechanism of action of tPA is not well understood, it seems to be unrelated to conversion of plasminogen to plasmin.[79,80] Activation of metabotropic non-NMDA receptor has been demonstrated to protect against NMDA-mediated glutamate toxicity in primary culture of cerebellar neurons.[81]
Figure 3.
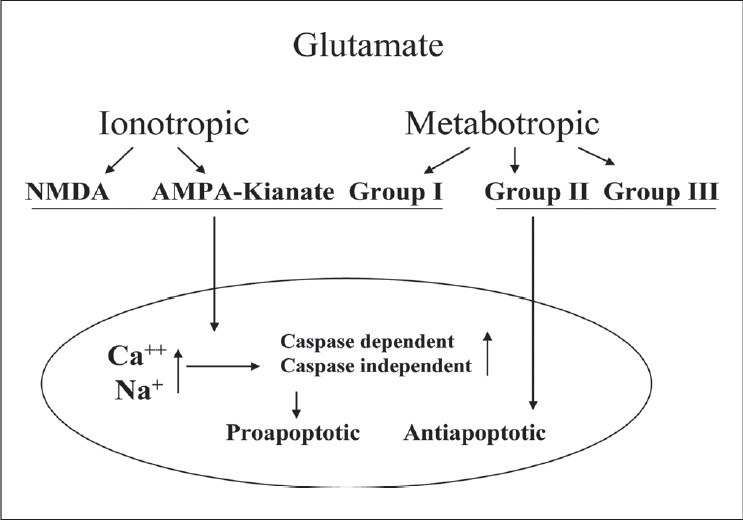
Glutamate excitotoxicity leading to RGC apoptosis
Low concentrations of glutamate were found to activate Ca++-permeable AMPA-KA receptors in cultured RGCs, leading to increases in Ca++ and decreased RGC survival.[82] The KA receptors are non-synaptic and are uniquely positioned to report non-synaptic glutamate. At low concentrations of 1–5 μM kainate internal calcium concentration rises significantly without significant depolarization. This low concentration of kainate causes ganglion cell death, which could be inhibited by specific kainate receptor antagonists. The kainate-associated toxicity which results from excess influx of calcium can also be inhibited by polyamines and calcium phosphatase which suppress the calcium influx. Thus, activation of ionotropic glutamate receptors can produce neurotoxicity uncoupled from neuroexcitation.[83]
There is evidence that among the mGluR activation of group I mGluRs increases neuronal excitation, whereas that of group II and III reduces synaptic transmission. Therefore, group I mGluR antagonists and group II and III mGluR agonists are expected to provide neuroprotective effects.[84]
To maintain the physiological concentrations and to protect ganglion cells from excitotoxic cell death, appropriate removal of synaptic glutamate is required. Glial cells, especially the Muller cells and astrocytes, present around the synapses express the glutamate transporter which helps in clearing extracellular glutamate by transporting it to the interior of glial cells.[85] Within the glial cells the glutamate gets converted to glutamine in the presence of glutamine synthetase. Glutamine is non-toxic and is released by glial cells to be taken up by neuronal cells where it again gets converted to glutamate in the presence of glutaminase and thus the neurotransmitter stores are replenished and glutamate toxicity is prevented.
Deviations from this normal retinal glutamate/glutamine cycle have been observed in experimental models of glaucoma. In a glaucoma model of rat, Moreno et al., reported significant decrease of retinal glutamate uptake, decreased activity of glutamine synthetase, significantly increased glutamine uptake and release and significantly increased glutaminase activity in oculohypertensive rats.[86] In one study immunohistochemical analysis of human glaucomatous and control eyes revealed decreased levels of both the glutamate transporter, excitatory amino acid transporter (EAAT)-1, and the NMDAR1 subtype suggesting that the loss of EAAT-1 in glaucoma may account for the elevated level of glutamate found in glaucomatous vitreous and lead to a compensatory downregulation of NMDAR-1. In the same study it was also observed that intravitreal injection of glial-derived neurotrophic factor (GDNF) in rats leads to elevated levels of both EAAT-1 and NMDAR-1.[87] A robust expression of a variant of glutamate transporter GLT-1c has been observed in RGC both in humans and rats. The GLT-1c in normal eyes is expressed only in photoreceptors. The induction of GLT-1c in RGCs in an attempt to protect themselves from toxic levels of glutamate indicates an important role of disturbed glutamate homeostasis in glaucomatous cell death.[88] Furthermore, alterations in the level of glutamate transporter m-RNA levels have been observed in both acute and chronic models of sublethal injuries in the eye and these alterations probably represent a transcriptionally regulated physiologic response.[89]
Some studies have suggested a correlation between elevated levels of glutamate in vitreous and apoptotic cell death in retina, however, others have reported no alterations in vitreous glutamate levels in glaucomatous eyes. Increased glutamate levels have been observed in mutant quail with a glaucoma-like disorder.[90] Elevated vitreous levels of glutamate were detected in an in vivo rat model of optic nerve ischemia.[91] In patients with retinal artery occlusion leading to acute retinal ischemia, the aqueous levels of glutamate were found to be elevated probably as a result of diffusion from the vitreous suggesting an important role of elevated levels of extracellular glutamate in ischemic retinal damage.[92] Dreyer et al., reported significantly elevated vitreal glutamate levels in glaucomatous monkeys as compared to normal monkeys.[93] Later, in a study involving 26 monkeys Carter-Dawson et al., reported that there were no significant differences in vitreal glutamate concentration between vitreous from normal control eyes and glaucomatous eyes, nor was there a significant difference in the results between the analyses performed in two independent laboratories.[94] Hare et al., also reported no significant changes in vitreal glutamate levels in glaucomatous monkey eyes as compared to control eyes.[95] In another study involving eight glaucoma patients no significant changes were observed in vitreal glutamate levels by Honkanen.[96] These findings were in marked contrast to the report by Dreyer et al., and even after considering all possible factors that could have influenced the measurement of glutamate levels, the exceptionally high glutamate levels reported could not be explained. The validity of results of Dreyer et al., was therefore doubtful. A probe into the charges of scientific misconduct was initiated by Harvard University officials and the author quickly admitted fabricating some of his data. A heavy punishment of a 10-year debarment from receiving federal research funds was imposed.[97]
In spite of the controversial issues mentioned earlier glutamate excitotoxicity seems to play an important role in neurodegenerative changes in glaucoma. However, it remains to be determined whether the glutamate excitotoxicity is an initial response to elevated pressure and ischemia or whether the secondary response due to release from dying ganglion cells plays the more critical role.
Role of nitric oxide in glaucoma
Nitric oxide plays an important and beneficial role in body function when secreted in physiological quantities, however, excess production of NO has been associated with a variety of non-neurological and neurological conditions including glaucoma. NOS produces NO by oxidation of L-arginine and has been detected in three isoforms.[98]
In normal human eyes the presence of NOS-1 has been detected in scattered astrocytes throughout the optic nerve head indicating that the NOS-1 is a constitutive enzyme in certain glia and NO serves functions as a physiological mediator between astrocytes or between astrocytes and axons. In patients with glaucoma a large number of cells show NOS-1 positivity on vitreal surface, in the remnant glial cells and in the cells in lamina cribrosa within glaucomatous tissue. Increased gene expression of the mRNA and presumably de novo synthesis of the NOS-1 isoform in astrocytes of the lamina cribrosa have also been observed. NOS-3 is also a constitutive enzyme present in the vascular endothelial cells in the prelaminar region of the optic nerve head in normal eyes and functions as a vasodilator. In glaucomatous eyes by causing vasodilation and increasing the blood flow NOS-3 induction can provide neuroprotective effects. The role of NOS-3 present in the astrocytes of glaucomatous optic nerve heads is not clearly known.[99]
NOS-2 is the inducible form of the enzyme (iNOS), which produces excessive quantities of NO under diverse conditions such as exposure to cytokines[100] and pressure.[101] Significant quantities of NOS-2 have been detected in the astrocytes[102] and microglia[103] at optic nerve head of glaucoma patients. Elevated NO levels have been observed in the aqueous humor of glaucoma patients[104] and a genetic association of iNOS and POAG has also been observed.[105] The animal experiments have also shown an association of elevated ocular NO levels with RGC death. Siu et al., observed significantly elevated NO levels in the retina of rats, 35 days after laser treatment.[106] At this time point, post laser treatment, the rats had significantly elevated IOP and significantly reduced number of RGCs thus establishing an association between the excess production of NO and RGC death. Abnormalities of NO-containing cells in trabecular meshwork, Schlemm's canal and ciliary body have also been detected in patients with POAG, however, it is not known whether these abnormalities are the manifestations of glaucoma and its treatment or precede the development of disease.[107]
The molecular mechanisms of NOS-2 induction and production of neurotoxic quantities of NO have been studied in human optic nerve astrocyte culture. Besides elevated pressure various cytokines appear to play a key role in NOS-2 induction. Exposure of optic nerve astrocytes to interferon gamma and interleukin-1β in culture stimulates NOS-2 production within 24 h.[102] TNF-A appears to be another more relevant cytokine and exposure of astrocytes to TNF-A in culture causes induction of NOS-2.[47] This cytokine along with the TNF receptor-1 has been detected in glaucomatous optic nerve heads. Thus the exposure to cytokines transforms the human optic nerve astrocytes into reactive astrocytes, which contain NOS-2 and have the capability to produce neurotoxic quantities of NO. Besides the important role of cytokines it has also been observed that the human optic nerve astrocytes when exposed to elevated hydrostatic pressure in culture, express elevated NOS-2 levels indicating a direct effect of elevated pressure for induction of NOS-2 in astrocytes.[106] The direct neurotoxic effects of NO on RGC in optic nerve head were further evidenced by the neuroprotective effects of aminoguanidine, a specific NOS-2 inhibitor in rats with chronically elevated IOP.[108]
Thus a large body of evidence suggests that excessive quantities of NO produced by astrocytes and microglia in optic nerve head play a crucial role in the development of optic neuropathy associated with glaucoma. The excess of NO thus produced enters freely into the cells after diffusion through the local microenvironment.[109] It is a free radical of moderate reactivity and after entering the cell leads to the production of highly reactive free radicals such as peroxynitrite after combining with superoxide (a product of mitochondrial metabolism). These highly reactive free radicals are capable of causing massive destruction of cell components and macromolecules.[110]
Oxidative stress and glaucoma
The ocular tissue is provided with a very efficient antioxidant defense mechanism, which includes reduced glutathione (GSH) and superoxide dismutase-catalase system. Ascorbic acid also has an important protective role and its high concentration has been detected in the vitreous humor,[111] cornea,[112] lacrimal film,[113] central corneal epithelium[114] and aqueous humor.[115] The excessive formation of free radicals and oxidative stress is recognized as an etiopathogenetic factor in many ocular diseases such as cataract,[116] age-related macular degeneration[117] and more recently glaucoma.[118] The glaucoma-affected patients have shown significantly depleted antioxidant potential in the aqueous humor,[119] an increase in serum antibodies against glutathione-S-transferase,[120] a decrease in plasma glutathione levels[121] and an increase in lipid peroxidation products in the plasma.[122]
Vascular dysregulation by causing ischemia and reperfusion may be the fundamental pathogenic step in inducing oxidative stress.[123] Under oxidative stress the endothelial functions are altered, especially the production of endothelian-1 and NO.[124,125] The endothelin-1 has been identified as the possible effector in POAG as it brings about changes in the cells of trabecular meshwork by causing vasoconstriction and thereby altering the IOP.[126] Significantly raised endothelin-1 levels have been detected in the aqueous humor of glaucoma patients as compared to normal controls.[57] NO, besides causing increased release of glutamate and neuronal toxicity also reacts with superoxide anion to form the peroxynitrite radical, which adds to the oxidative stress-induced damage.[127] Oxidative stress as a result of free radical accumulation either from aerobic metabolism or vascular dysregulation is known to damage the DNA of the trabecular meshwork cells.[128] As a result, altered adhesion of trabecular cells with the ECM proteins leads to cytoskeleton rearrangements and increased resistance to outflow leading to elevated IOP.[129] Human studies have revealed alterations in aqueous humor drainage following exposure to hydrogen peroxide.[130] More extensive alterations in trabecular cells have been detected in the layers of trabecular meshwork closer to the anterior chamber thus indicating that the exposure to toxic substances such as free radicals, in the anterior chamber plays a crucial role as a pathogenetic factor.
The results of some of the animal experiments have suggested possible benefits of antioxidants in glaucomatous optic neuropathy. In a rat model of glaucoma topical administration of a novel free radical scavenger with esterified ion chelator side groups on a methoxypolyethylene glycol backbone was found to lower IOP by 29.6%. In the same study the RGC loss in rats in response to intravitreal NMDA was also found to be reduced when NMDA was co-administered with the same novel free radical scavanger.[131] BDNF in combination with a nonspecific free radical scavenger was shown to rescue RGC from death in rat eyes with elevated IOP.[132] The results of these studies indicate an association of oxidative stress and development of glaucoma and possible benefits of antioxidants in glaucomatous optic neuropathy.
Current therapeutic approaches
Glaucomatous optic neuropathy is a chronic process, which progresses over many years. Until recently, modulation of elevated IOP was the only mode of therapeutic intervention. As the glaucomatous changes continue to progress despite well-controlled IOP, development of pressure-independent and preferentially neuroprotective treatment strategies is extremely important. As the understanding of pathophysiological mechanisms involved in glaucomatous optic neuropathy has advanced tremendously, an enormous amount of research has been stimulated for the development of effective neuroprotective strategies.
As a result a variety of therapeutic options have shown efficacy as neuroprotective agents in experimental studies. Besides ocular hypotensive agents the ocular blood flow enhancers such as calcium channel blockers were suggested to provide neuroprotection by improving the optic nerve head blood flow. But there were concerns as these agents reduce the systemic blood pressure and might worsen the optic nerve head ischemia by reducing the perfusion pressure. Carbonic anhydrase inhibitors are also suggested to improve the optic nerve head blood flow.
A variety of agents with antiapoptotic activity have been evaluated for neuroprotective effects in experimental animal models. Both the reversible and irreversible caspase inhibitors were found to protect RGCs in axotomised rats. Erythropoietin, which promotes proliferation and differentiation of bone marrow precursor cells by inhibiting apoptosis, when given by intravitreal injection in an episcleral vessel cautery-induced rat model of glaucoma was found to increase RGC viability.[133] However, the use of these agents, which act by preventing the apoptosis, is actually the treatment of the result rather than the degenerative process itself.
Therapeutic interventions to alter the process of RGC degeneration have also been studied extensively. A variety of neurotrophic factors (BDNF, nerve growth factor), an antioxidant (N-ace-tyl-L-cysteine), and a NOS inhibitor (L-NAME, aminoguinidine) have shown promising neuroprotective effects by modulating the process of RGC degeneration in experimental animals. The NMDA antagonists especially seem to hold promise in glaucoma neuroprotection. NMDA receptor antagonists have largely failed the clinical trials as they act by virtually blocking all the NMDA receptors, and physiological NMDA activity is essential for normal neuronal functions. Memantine, an adamantine derivative, has shown encouraging results as it selectively blocks the excessive receptor activation without affecting the normal receptor activity. Memantine is a noncompetitive, low-affinity, open channel blocker and blocks the receptor-associated ion channel when it is excessively open. As its off-rate is very high it does not accumulate substantially within the channel to interfere with the normal neuronal functions. Memantine is thus well tolerated and has been approved for use in Alzheimer's disease.[134] The results of the efficacy of oral memantine treatment in a Phase 3, randomized, multicenter, placebo-controlled, double-blind clinical trial involving POAG patients are awaited.
In spite of a large number of drugs showing efficacy in animal experiments only one has progressed to the stage of clinical trial. Clearly, the concept of neuroprotective agents playing a major role in glaucoma management is still in infancy. However, a better understanding of the pathophysiological mechanisms involved in glaucoma will undoubtedly lead us to new, safe and effective glaucoma therapy.
Summary and Conclusions
To summarize, the primary factors responsible for apoptotic cell death in glaucoma include not only elevated IOP but also vascular dysregulation, especially in people with NTG. The molecular mechanisms involved largely include glutamate excitotoxicity, increased MMP expression, TNF-alpha upregulation, increased NOS-2 expression and oxidative stress. The complex interrelationship between primary and secondary mechanisms involved in the pathophysiology of glaucoma is shown in Fig. 4. Although current therapeutic approaches, which primarily aim to lower the elevated IOP have shown great efficacy in saving the vision in glaucomatous optic neuropathy, further research to identify and develop pharmacological means with predominant neuroprotective effects is expected to provide better therapeutic options. Limited success so far in the development of effective neuroprotective therapy probably indicates the need of future research that incorporates multiple factors involved in the pathophysiology of neuronal damage in glaucoma.
Figure 4.
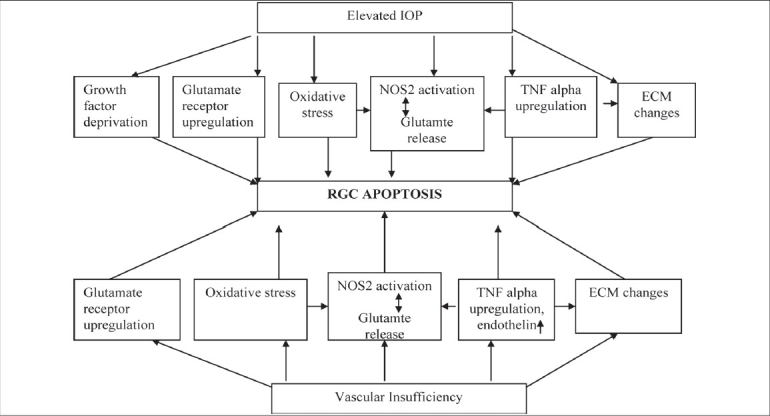
The complex interplay of primary and secondary factors leading to RGC apoptosis in glaucoma. TNF-A - Tumor necrosis factor-alpha, ECM - Extracellular matrix, NOS-2 - Nitric oxide synthase-2
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gupta N, Weinreb RN. New definitions of glaucoma. Curr Opin Ophthalmol. 1997;8:38–41. doi: 10.1097/00055735-199704000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Quigley HA. Neuronal death in glaucoma. Prog Retin Eye Res. 1999;18:39–57. doi: 10.1016/s1350-9462(98)00014-7. [DOI] [PubMed] [Google Scholar]
- 3.Airaksinen PJ, Alanko HI. Effect of retinal nerve fibre loss on the optic nerve head configuration in early glaucoma. Graefes Arch Clin Exp Ophthalmol. 1982;220:193–6. doi: 10.1007/BF02186668. [DOI] [PubMed] [Google Scholar]
- 4.Quigley HA, Dunkelbarger GR, Green WR. Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol. 1989;107:453–64. doi: 10.1016/0002-9394(89)90488-1. [DOI] [PubMed] [Google Scholar]
- 5.Kaushik S, Pandav SS, Ram J. Neuroprotection in glaucoma. J Postgrad Med. 2003;49:90–5. doi: 10.4103/0022-3859.917. [DOI] [PubMed] [Google Scholar]
- 6.Quigley HA, Nickells RW, Kerrigan LA, Pease ME, Thibault DJ, Zack DJ. Retinal ganglion cell death in experimental glaucoma and after axotomy occurs by apoptosis. Invest Ophthalmol Vis Sci. 1995;36:774–86. [PubMed] [Google Scholar]
- 7.Pease ME, McKinnon SJ, Quigley HA, Kerrigan-Baumrind LA, Zack DJ. Obstructed axonal transport of BDNF and its receptor TrkB in experimental glaucoma. Invest Ophthalmol Vis Sci. 2000;41:764–74. [PubMed] [Google Scholar]
- 8.Levin LA. Mechanisms of optic neuropathy. Curr Opin Ophthalmol. 1997;78:9–15. doi: 10.1097/00055735-199712000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Farkas RH, Grosskreutz CL. Apoptosis, neuroprotection and retinal ganglion cell death: An overview. Int Ophthalmol Clin. 2001;41:111–30. doi: 10.1097/00004397-200101000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Quigley HA, Dunkelberger G, Green W. Chronic human glaucoma causing selectively greater loss of large optic nerve fibres. Ophthalmology. 1998;95:357–63. doi: 10.1016/s0161-6420(88)33176-3. [DOI] [PubMed] [Google Scholar]
- 11.Glovinsky Y, Quigley H, Dunkelburger G. Retinal ganglion cell loss is size dependent in experimental glaucoma. Invest Ophthalmol Vis Sci. 1991;32:184–91. [PubMed] [Google Scholar]
- 12.Glovinsky Y, Quigley H, Pease M. Foveal ganglion cell loss is size dependent in experimental glaucoma. Invest Ophthalmol Vis Sci. 1993;34:395–400. [PubMed] [Google Scholar]
- 13.James EM, Hideya U, Joseph C. Retinal ganglion cell death in experimental glaucoma. Br J Ophthalmol. 2000;84:303–10. doi: 10.1136/bjo.84.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bien A, Seidenbecher CI, Bockers TM, Sabel BA, Kreutz MR. Apoptotic versus necrotic characteristics of retinal ganglion cell death after partial optic nerve injury. J Neurotrauma. 1999;16:153–63. doi: 10.1089/neu.1999.16.153. [DOI] [PubMed] [Google Scholar]
- 15.Earnshaw WC, Martins LM, Kaufmann SH. Mammalian caspases: Structure, activation, substrates and functions during apoptosis. Annu Rev Biochem. 1999;68:383–424. doi: 10.1146/annurev.biochem.68.1.383. [DOI] [PubMed] [Google Scholar]
- 16.Marc BG, Declan P M, Colm JO, Thomas GC. Retinal ganglion cells: Dying to survive. Int J Dev Biol. 2006;50:665–74. doi: 10.1387/ijdb.062159mg. [DOI] [PubMed] [Google Scholar]
- 17.Kermer P, Klöcker N, Labes M, Bähr M. Inhibition of CPP32-like proteases rescues axotomized retinal ganglion cells from secondary cell death in vivo. J Neurosci. 1998;18:4656–62. doi: 10.1523/JNEUROSCI.18-12-04656.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spalding KL, Dharmarajan AM, Harvey AR. Caspase independent retinal ganglion cell death after target ablation in the neonatal rat. Eur J Neurosci. 2005;21:33–45. doi: 10.1111/j.1460-9568.2004.03826.x. [DOI] [PubMed] [Google Scholar]
- 19.Klein BE, Klein R, Sponsel WE, Franke T, Cantor LB, Martone J, et al. Prevalence of glaucoma: The Beaver Dam Eye Study. Ophthalmology. 1992;99:1499–504. doi: 10.1016/s0161-6420(92)31774-9. [DOI] [PubMed] [Google Scholar]
- 20.Tielsch JM, Katz J, Singh K, Quigley HA, Gottsch JD, Javitt J, et al. A population-based evaluation of glaucoma screening: The Baltimore Eye Survey. Am J Epidemiol. 1991;134:1102–10. doi: 10.1093/oxfordjournals.aje.a116013. [DOI] [PubMed] [Google Scholar]
- 21.Hendrickx KH, van den Enden A, Rasker MT, Hoyng PF. Cumulative incidence of patients with disc hemorrhages in glaucoma and the effect of therapy. Ophthalmology. 1994;101:1165–72. doi: 10.1016/s0161-6420(94)31192-4. [DOI] [PubMed] [Google Scholar]
- 22.Clark AF, Miggans ST, Wilson K, Browder S, McCartney MD. Cytoskeletal changes in cultured human glaucoma trabecular meshwork cells. J Glaucoma. 1995;4:183–8. [PubMed] [Google Scholar]
- 23.Alvarado J, Murphy C, Juster R. Trabecular meshwork cellularity in primary open-angle glaucoma and nonglaucomatous normals. Ophthalmology. 1984;91:564–79. doi: 10.1016/s0161-6420(84)34248-8. [DOI] [PubMed] [Google Scholar]
- 24.Grierson I. What is open angle glaucoma? Eye. 1987;1:15–28. doi: 10.1038/eye.1987.3. [DOI] [PubMed] [Google Scholar]
- 25.Lutjen-Drecoll E, Shimizu T, Rohrbach M, Rohen JW. Quantitative analysis of 'plaque material' in the inner- and outer wall of Schlemm's canal in normal- and glaucomatous eyes. Exp Eye Res. 1986;42:443–55. doi: 10.1016/0014-4835(86)90004-7. [DOI] [PubMed] [Google Scholar]
- 26.Knepper PA, Goossens W, Hvizd M, Palmberg PF. Glycosaminoglycans of the human trabecular meshwork in primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 1986;37:1360–7. [PubMed] [Google Scholar]
- 27.Lutjen-Drecoll E, Rohen JW. Morphology of aqueous outflow pathways in normal and glaucomatous eyes. In: Ritch R, Shields MB, Krupin T, editors. The glaucomas. St. Louis: Mosby Year; 1996. pp. 89–123. [Google Scholar]
- 28.Morrison JC, Moore CG, Deppmeier LM, Gold BG, Meshul CK, Johnson EC. A rat model of chronic pressure-induced optic nerve damage. Exp Eye Res. 1997;64:85–96. doi: 10.1006/exer.1996.0184. [DOI] [PubMed] [Google Scholar]
- 29.Chauhan BC, Pan J, Archibald ML, LeVatte TL, Kelly ME, Tremblay F. Effect of intraocular pressure on optic disc topography, electroretinography, and axonal loss in a chronic pressure-induced rat model of optic nerve damage. Invest Ophthalmol Vis Sci. 2002;43:2969–76. [PubMed] [Google Scholar]
- 30.Levkovitch-Verbin H, Quigley HA, Martin KR, Valenta D, Baumrind LA, Pease ME. Translimbal laser photocoagulation to the trabecular meshwork as a model of glaucoma in rats. Invest Ophthalmol Vis Sci. 2002;43:402–10. [PubMed] [Google Scholar]
- 31.Mittag TW, Danias J, Pohorenec G, Yuan HM, Burakgazi E, Redman RC, et al. Retinal damage after 3 to 4 months of elevated intraocular pressure in a rat glaucoma model. Invest Ophthalmol Vis Sci. 2000;41:3451–9. [PubMed] [Google Scholar]
- 32.WoldeMussie E, Ruiz G, Wijono M, Wheeler LA. Neuroprotection of retinal ganglion cells by brimonidine in rats with laser-induced chronic ocular hypertension. Invest Ophthalmol Vis Sci. 2001;42:2849–55. [PubMed] [Google Scholar]
- 33.Naskar R, Wissing M, Thanos S. Detection of early neuron degeneration and accompanying microglial responses in the retina of a rat model of glaucoma. Invest Ophthalmol Vis Sci. 2002;43:2962–8. [PubMed] [Google Scholar]
- 34.Garcia-Valenzuela E, Shareef S, Walsh J, Sharma SC. Programmed cell death of retinal ganglion cells during experimental glaucoma. Exp Eye Res. 1995;61:33–44. doi: 10.1016/s0014-4835(95)80056-5. [DOI] [PubMed] [Google Scholar]
- 35.Agar A, Yip SS, Hill MA, Coroneo MT. Pressure related apoptosis in neuronal cell lines. J Neurosci Res. 2000;60:495–503. doi: 10.1002/(SICI)1097-4547(20000515)60:4<495::AID-JNR8>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 36.Johnson EC, Morrison JC, Farrell S, Deppmeier L, Moore CG, McGinty MR. The effect of chronically elevated intraocular pressure on the rat optic nerve head extracellular matrix. Exp Eye Res. 1996;62:663–74. doi: 10.1006/exer.1996.0077. [DOI] [PubMed] [Google Scholar]
- 37.Pena JD, Taylor AW, Ricard CS, Vidal I, Hernandez MR. Transforming growth factor beta isoforms in human optic nerve heads. Br J Ophthalmol. 1999;83:209–18. doi: 10.1136/bjo.83.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cordeiro MF. Beyond mitomycin: TGF-beta and wound healing. Prog Retin Eye Res. 2002;21:75–89. doi: 10.1016/s1350-9462(01)00021-0. [DOI] [PubMed] [Google Scholar]
- 39.Werb Z. ECM and cell surface proteolysis: Regulating cellular ecology. Cell. 1997;91:439–42. doi: 10.1016/s0092-8674(00)80429-8. [DOI] [PubMed] [Google Scholar]
- 40.Li G, Moss SE, Alexander RA, Ali RR, Fitzke FW, Cordeiro MF. Retinal ganglion cell apoptosis in glaucoma is related to intraocular pressure and IOP-induced effects on extracellular matrix. Invest Ophthalmol Vis Sci. 2005;46:175–82. doi: 10.1167/iovs.04-0832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grossmann J. Molecular mechanisms of “detachment-induced apoptosis-anoikis”. Apoptosis. 2002;7:247–60. doi: 10.1023/a:1015312119693. [DOI] [PubMed] [Google Scholar]
- 42.Zhang X, Cheng M, Chintala SK. Kainic acid-mediated upregulation of matrix metalloproteinase-9 promotes retinal degeneration. Invest Ophthalmol Vis Sci. 2004;45:2374–83. doi: 10.1167/iovs.03-1239. [DOI] [PubMed] [Google Scholar]
- 43.Yan X, Tezel G, Wax MB, Edward DP. Matrix metalloproteinases and tumor necrosis factor alpha in glaucomatous optic nerve head. Arch Ophthalmol. 2000;118:666–73. doi: 10.1001/archopht.118.5.666. [DOI] [PubMed] [Google Scholar]
- 44.Agapova OA, Ricard CS, Salvador-Silva M, Hernandez MR. Expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in human optic nerve head astrocytes. Glia. 2001;33:205–16. doi: 10.1002/1098-1136(200103)33:3<205::aid-glia1019>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 45.Nickells W. Retinal ganglion cell death in glaucoma: The how, the witty and the maybe. J Glaucoma. 1996;5:345–56. [PubMed] [Google Scholar]
- 46.Nakazawa T, Nakazawa C, Matsubara A, Noda K, Hisatomi T, She H, et al. Tumor necrosis factor- mediates oligodendrocyte death and delayed retinal ganglion cell loss in a mouse model of glaucoma. J Neurosci. 2006;26:12633–41. doi: 10.1523/JNEUROSCI.2801-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yuan L, Neufeld AH. Tumor necrosis factor-alpha: A potentially neurodestructive cytokine produced by glia in the human glaucomatous optic nerve head. Glia. 2000;32:42–50. [PubMed] [Google Scholar]
- 48.Rossetti L, Marchetti I, Orzalesi N, Scorpiglione N, Torri V, Liberati A. Randomized clinical trials on medical treatment of glaucoma: Are they appropriate to guide clinical practice? Arch Ophthalmol. 1993;111:96–103. doi: 10.1001/archopht.1993.01090010100034. [DOI] [PubMed] [Google Scholar]
- 49.Chauhan BC. The relationship between intraocular pressure and visual field progression in glaucoma. In: Drance SM, editor. Update to glaucoma, blood flow and drug treatment. Amsterdam: Kugler; 1995. pp. 1–6. [DOI] [PubMed] [Google Scholar]
- 50.Wang JJ, Mitchell P, Smith W. Is there an association between migraine headache and open-angle glaucoma? Findings of the Blue Mountains Study. Ophthalmol. 1997;104:1714–9. doi: 10.1016/s0161-6420(97)30075-x. [DOI] [PubMed] [Google Scholar]
- 51.Curseifen C, Wisse M, Curseifen S, Junemann A, Martus P, Korth M. Migraine and tension headache in high-pressure and normal-pressure glaucoma. Am J Ophthalmol. 2000;129:102–4. doi: 10.1016/s0002-9394(99)00289-5. [DOI] [PubMed] [Google Scholar]
- 52.Gass A, Flammer J, Linder L, Romerio SC, Gasser P, Haefeli WE. Inverse correlation between endothelin-1-induced peripheral microvascular vasoconstriction and blood pressure in glaucoma patients. Graefes Arch Clin Exp Ophthalmol. 1997;235:634–8. doi: 10.1007/BF00946939. [DOI] [PubMed] [Google Scholar]
- 53.O'Brien C, Butt Z. Blood flow velocity in the peripheral circulation of glaucoma patients. Ophthalmologica. 1999;213:150–3. doi: 10.1159/000027410. [DOI] [PubMed] [Google Scholar]
- 54.Cellini M, Possati GL, Profazio V, Sbrocca M, Caramazza N, Caramazza R. Color Doppler imaging and plasma levels of endothelin-1 in low-tension glaucoma. Acta Ophthalmol Scand. 1997;224:11–3. doi: 10.1111/j.1600-0420.1997.tb00448.x. [DOI] [PubMed] [Google Scholar]
- 55.Noske W, Hensen J, Wiederholt M. Endothelin-like immunoreactivity in aqueous humor of patients with primary open-angle glaucoma and cataract. Graefes Arch Clin Exp Ophthalmol. 1997;235:551–2. doi: 10.1007/BF00947082. [DOI] [PubMed] [Google Scholar]
- 56.Tezel G, Kass MA, Kolker AE, Becker B, Wax MB. Plasma and aqueous humor endothelin levels in primary open-angle glaucoma. J Glaucoma. 1997;6:83–9. [PubMed] [Google Scholar]
- 57.Hollo G, Lakatos P, Farkas K. Cold pressor test and plasma endothelin-1 concentration in primary open-angle and capsular glaucoma. J Glaucoma. 1998;7:105–10. [PubMed] [Google Scholar]
- 58.Stroman GA, Stewart WC, Golnik KC, Cure JK, Olinger RE. Magnetic resonance imaging in patients with low-tension glaucoma. Arch Ophthalmol. 1995;113:168–72. doi: 10.1001/archopht.1995.01100020050027. [DOI] [PubMed] [Google Scholar]
- 59.Ong K, Farinelli A, Billson F, Houang M, Stern M. Comparative study of brain magnetic resonance imaging findings in patients with low-tension glaucoma and control subjects. Ophthalmol. 1995;102:1632–8. doi: 10.1016/s0161-6420(95)30816-0. [DOI] [PubMed] [Google Scholar]
- 60.Nomura H, Shimokata H, Ando F, Miyake Y, Kuzuya F. Age-related changes in intraocular pressure in a large Japanese population: A cross-sectional and longitudinal study. Ophthalmology. 1999;106:2016–22. doi: 10.1016/S0161-6420(99)90417-7. [DOI] [PubMed] [Google Scholar]
- 61.Harris A, Arend O, Chung HS, Kagemann L, Cantor L, Martin B. A comparative study of betaxolol and dorzolamide on the ocular circulation in normal-tension glaucoma patients. Ophthalmology. 2000;107:430–4. doi: 10.1016/s0161-6420(99)00093-7. [DOI] [PubMed] [Google Scholar]
- 62.Bill A, Sperber GO. Control of retinal and choroidal blood flow. Eye. 1990;4:319–25. doi: 10.1038/eye.1990.43. [DOI] [PubMed] [Google Scholar]
- 63.Matsuura K, Kawai Y. Effects of hypothermia and aging on postischemic reperfusion in rat eyes. Jpn J Physiol. 1998;48:9–15. doi: 10.2170/jjphysiol.48.9. [DOI] [PubMed] [Google Scholar]
- 64.Michelson G, Langhans M J, Harazny J, Dichtl A. Visual field defect and perfusion of the juxtapapillary retina and the neuroretinal rim area in primary open-angle glaucoma. Graefe's Arch Clin Exp Ophthalmol. 1998;236:80–5. doi: 10.1007/s004170050046. [DOI] [PubMed] [Google Scholar]
- 65.Chung HS, Harris A, Kagemann L, Martin B. Peripapillary retinal blood flow in normal-tension glaucoma. Br J Ophthalmol. 1999;83:466–9. doi: 10.1136/bjo.83.4.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Grunwald JE, Piltz J, Hariprasad SM, Dupont J, Maguire MG. Optic nerve blood flow in glaucoma: Effect of systemic hypertension. Am J Ophthalmol. 1999;127:516–22. doi: 10.1016/s0002-9394(99)00028-8. [DOI] [PubMed] [Google Scholar]
- 67.Bonomi L, Marchini G, Marraffa M, Bernardi P, Morbio R, Varotto A. Vascular risk factors for primary open angle glaucoma: The Egna-Neumarkt Study. Ophthalmology. 2000;107:1287–93. doi: 10.1016/s0161-6420(00)00138-x. [DOI] [PubMed] [Google Scholar]
- 68.Golubnitschaja-Labudova O, Liu R, Decker C, Zhu P, Haeflinger IO, Flammer J. Altered gene expression in lymphocytes of patients with normal-tension glaucoma. Curr Eye Res. 2000;21:867–76. doi: 10.1076/ceyr.21.5.867.5534. [DOI] [PubMed] [Google Scholar]
- 69.Golubnitschaja O, Yeghiazaryan, Kristina RN, Liu R, Mönkemann H, Leppert D, et al. Increased expression of matrix metalloproteinases in mononuclear blood cells of normal-tension glaucoma patients. J Glaucoma. 2004;13:66–72. doi: 10.1097/00061198-200402000-00013. [DOI] [PubMed] [Google Scholar]
- 70.Neal MJ, Cunningham JR, Hutson PH, Hogg J. Effects of ischaemia on neurotransmitter release from the isolated retina. J Neurochem. 1994;62:1025–33. doi: 10.1046/j.1471-4159.1994.62031025.x. [DOI] [PubMed] [Google Scholar]
- 71.Lucas DR, Newhouse JP. The toxic effect of sodium L-glutamate on the inner layers of the retina. Am Med Assoc Arch Ophthalmol. 1957;58:193–201. doi: 10.1001/archopht.1957.00940010205006. [DOI] [PubMed] [Google Scholar]
- 72.Olney JW. Glutamate-induced retinal degeneration in neonatal mice: Electron microscopy of the acutely evolving lesion. J Neuropathol Exp Neurol. 1969;28:455–74. doi: 10.1097/00005072-196907000-00007. [DOI] [PubMed] [Google Scholar]
- 73.Vorwerk CK, Lipton SA, Zurakowski D, Hyman BT, Sabel BA, Dreyer EB. Chronic low-dose glutamate is toxic to retinal ganglion cells: Toxicity blocked by memantine. Invest Ophthalmol Vis Sci. 1996;37:1618–24. [PubMed] [Google Scholar]
- 74.Choi DW. Ionic dependence of glutamate neurotoxicity. J Neurosci. 1987;7:369–79. doi: 10.1523/JNEUROSCI.07-02-00369.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Novelli A, Reilly JA, Lysko PG, Henneberry RC. Glutamate becomes neurotoxic via the N-methyl-D-aspartate receptor when intracellular energy levels are reduced. Brain Res. 1988;451:205–12. doi: 10.1016/0006-8993(88)90765-2. [DOI] [PubMed] [Google Scholar]
- 76.Manev H, Favaron M, Guidotti A, Costa E. Delayed increase of Ca++ influx elicited by glutamate: Role in neuronal death. Mol Pharmacol. 1989;36:106–12. [PubMed] [Google Scholar]
- 77.Sucher NJ, Lipton SA, Dreyer EB. Molecular basis of glutamate toxicity in retinal ganglion cells. Vis Res. 1997;27:3483–93. doi: 10.1016/S0042-6989(97)00047-3. [DOI] [PubMed] [Google Scholar]
- 78.Li Guo, Salt TE, Maass A, Luong VY, Moss SE, Fred WF, Cordeiro MF. Assessment of neuroprotective effects of glutamate modulation on glaucoma-related retinal ganglion cell apoptosis in vivo. Invest Ophthalmol Vis Sci. 2006;47:626–33. doi: 10.1167/iovs.05-0754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kumada M, Niwa M, Hara A, Matsuno H, Mori H, Ueshima S, et al. Tissue type plasminogen activator facilitates NMDA-receptor-mediated retinal apoptosis through an independent fibrinolytic cascade. Invest Ophthalmol Vis Sci. 2005;46:1504–7. doi: 10.1167/iovs.04-0595. [DOI] [PubMed] [Google Scholar]
- 80.Mali RS, Mali, Cheng M, Chintala SK. Plasminogen activators promote excitotoxicity-induced retinal damage. FASEB J. 2005;19:1280–9. doi: 10.1096/fj.04-3403com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Montoliu C, Llansola M, Cucarella C, Grisolía S, Felipo V. Activation of the metabotropic glutamate receptor mglur5 prevents glutamate toxicity in primary cultures of cerebellar neurons. Pharmacol Exp Ther. 1997;281:643–7. [PubMed] [Google Scholar]
- 82.Otori Y, Wei JY, Barnstable CJ. Neurotoxic effects of low doses of glutamate on purified rat retinal ganglion cells. Invest Ophthalmol Vis Sci. 1998;39:972–81. [PubMed] [Google Scholar]
- 83.Nicholls D, Attwell D. The release and uptake of excitatory amino acids. Trends Pharmacol Sci. 1990;11:462–8. doi: 10.1016/0165-6147(90)90129-v. [DOI] [PubMed] [Google Scholar]
- 84.Nicoletti F, Bruno V, Copani A, Casabona G, Knopfel T. Metabotropic glutamate receptors: A new target for the therapy of neurodegenerative disorders? Trends Neurosci. 1996;19:267–71. doi: 10.1016/S0166-2236(96)20019-0. [DOI] [PubMed] [Google Scholar]
- 85.Moreno MC, Moreno, Sande P, Aldana H, Marcos, Zavalía N de, et al. Effect of glaucoma on the retinal glutamate/glutamine cycle activity. FASEB J. 2005;19:1161–2. doi: 10.1096/fj.04-3313fje. [DOI] [PubMed] [Google Scholar]
- 86.Naskar R, Vorwerk CK, Dreyer EB. Concurrent downregulation of a glutamate transporter and receptor in glaucoma. Invest Ophthalmol Vis sci. 2000;41:1940–4. [PubMed] [Google Scholar]
- 87.Robert KP, Sullivan, Elizabeth WM, Lauren M, Guadalupe R, David VP. Evoked expression of the glutamate transporter GLT-1c in retinal ganglion cells in human glaucoma and in a rat model. Invest Ophthalmol Vis Sci. 2006;47:3853–9. doi: 10.1167/iovs.06-0231. [DOI] [PubMed] [Google Scholar]
- 88.Christian M, Thomas P, Martina P, Knut D, Wolfgang BB, Christian KV. Changes of retinal glutamate transporter GLT-1 mRNA levels following optic nerve damage. Mol Vis. 2003;9:10–13. [PubMed] [Google Scholar]
- 89.Shen W, Slaugter MM. A non excitatory paradigm of glutamate toxicity. J Neurophysiol. 2002;87:1629–34. doi: 10.1152/jn.00532.2000. [DOI] [PubMed] [Google Scholar]
- 90.Dkhissi O, Chanut E, Wasowicz M, Savoldelli M, Nguyen-Legros J, Minvielle F, et al. Retinal TUNEL-positive cells and high glutamate levels in vitreous humor of mutant quail with a glaucoma-like disorder. Invest Ophthalmol Vis Sci. 1999;40:990–5. [PubMed] [Google Scholar]
- 91.Kim TW, Kang KB, Choung HK, Park KH, Kim DM. Elevated glutamate levels in the vitreous body of an in vivo model of optic nerve ischemia. Arch Ophthalmol. 2000;118:533–6. doi: 10.1001/archopht.118.4.533. [DOI] [PubMed] [Google Scholar]
- 92.Wakabayashi Y, Yagihashi T, Kezuka J, Muramatsu D, Usui M, Iwasaki T. Glutamate levels in aqueous humor of patients with retinal artery occlusion. Retina. 2006;26:432–6. doi: 10.1097/00006982-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 93.Dreyer EB, Zurakowski D, Schumer RA, Podos SM, Lipton SA. Elevated glutamate levels in the vitreous body of humans and monkeys with glaucoma. Arch ophthalmol. 1996;114:299–305. doi: 10.1001/archopht.1996.01100130295012. [DOI] [PubMed] [Google Scholar]
- 94.Carter-Dawson L, Crawford ML, Harwerth RS, Smith EL, 3rd, Feldman R, Shen FF, et al. Vitreal glutamate concentration in monkeys with experimental glaucoma. Invest Ophthalmol Vis Sci. 2002;43:2633–7. [PubMed] [Google Scholar]
- 95.Hare WA, WoldeMussie E, Lai RK, Ton H, Ruiz G, Chun T, et al. Efficacy and safety of memantine treatment for reduction of changes associated with experimental glaucoma in monkey, I: Functional measures. Invest Ophthalmol Vis Sci. 2004;45:2625–39. doi: 10.1167/iovs.03-0566. [DOI] [PubMed] [Google Scholar]
- 96.Honkanen RA, Baruah S, Zimmerman MB, Khanna CL, Weaver YK, Narkiewicz J, et al. Vitreous amino acid concentrations in patients with glaucoma undergoing vitrectomy. Arch Ophthalmol. 2003;121:183–8. doi: 10.1001/archopht.121.2.183. [DOI] [PubMed] [Google Scholar]
- 97.Dalton R. Private investigations. Nature. 2001;411:129–30. doi: 10.1038/35075752. [DOI] [PubMed] [Google Scholar]
- 98.Moncada S, Higgs A. The L-arginine-nitric oxide pathway. N Engl J Med. 1993;329:2002–12. doi: 10.1056/NEJM199312303292706. [DOI] [PubMed] [Google Scholar]
- 99.Neufeld AH. Nitric oxide a potential mediator of retinal ganglion cell damage in glaucoma. Surv Ophthalmol. 1999;43:S129–35. doi: 10.1016/s0039-6257(99)00010-7. [DOI] [PubMed] [Google Scholar]
- 100.Liu J, Zhao ML, Brosnan CF, Lee SC. Expression of type II nitric oxide synthase in primary human astrocytes and microglia: Role of IL-1beta and IL-1 receptor antagonist. J Immunol. 1996;157:3569–76. [PubMed] [Google Scholar]
- 101.Liu B, Neufeld AH. Nitric oxide synthase-2 in human optic nerve head astrocytes induced by elevated pressure in vitro. Arch Ophthalmol. 2001;119:240–5. [PubMed] [Google Scholar]
- 102.Liu B, Neufeld AH. Expression of nitric oxide synthase-2 (NOS-2) in reactive astrocytes of the human glaucomatous optic nerve head. Glia. 2000;30:178–86. doi: 10.1002/(sici)1098-1136(200004)30:2<178::aid-glia7>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 103.Yuan L, Neufeld AH. Activated microglia in the human glaucomatous optic nerve head. J Neurosci Res. 2001;64:523–32. doi: 10.1002/jnr.1104. [DOI] [PubMed] [Google Scholar]
- 104.Tsai DC, Hsu WM, Chou CK, Chen SJ, Peng CH, Chi CW, et al. Significant variation of the elevated nitric oxide levels in aqueous humor from patients with different types of glaucoma. Ophthalmologica. 2003;216:346–50. doi: 10.1159/000066187. [DOI] [PubMed] [Google Scholar]
- 105.Motallebipaur M, Rada-Iqlesias A, Jansson, Wadelius C. The promoter of inducible nitric oxide synthase implicated in glaucoma based on genetic analysis and nuclear factor binding. Mol Vis. 2005;11:950–7. [PubMed] [Google Scholar]
- 106.Siu AW, Leung MC, Ho TC, Siu FK, Ji JZ, Fai SK. Total retinal nitric oxide production is increased in intraocular pressure-elevated rats. Exp Eye Res. 2002;75:401–6. [PubMed] [Google Scholar]
- 107.Nathanson JA, Mckee M. Alterations of ocular nitric oxide synthase in human glaucoma. Invest Ophthalmol Vis Sci. 1995;36:1774–84. [PubMed] [Google Scholar]
- 108.Neufeld AH. Pharmacologic neuroprotection with an inhibitor of nitric oxide synthase for the treatment of glaucoma. Brain Res Bull. 2004;62:455–9. doi: 10.1016/j.brainresbull.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 109.Garthwaite J, Boulton CL. Nitric oxide signaling in the central nervous system. Ann Rev Physiol. 1995;57:683–706. doi: 10.1146/annurev.ph.57.030195.003343. [DOI] [PubMed] [Google Scholar]
- 110.Lipton SA, Choi YB, Pan ZH, Lei SZ, Chen HS, Sucher NJ, et al. A redox-based mechanism for the neuroprotective and neurodestructive effects of nitric oxide and related nitroso-compounds. Nature. 1993;364:626–32. doi: 10.1038/364626a0. [DOI] [PubMed] [Google Scholar]
- 111.Hanashima, Namiki H. Reduced viability of vascular endothelial cells by high concentration of ascorbic acid in vitreous humor. Cell Biol Int. 1999;23:287–98. doi: 10.1006/cbir.1999.0347. [DOI] [PubMed] [Google Scholar]
- 112.Brubaker RF, Bourne WM, Bachman LA, McLaren JW. Ascorbic acid content of human corneal epithelium. Invest Ophthalmol Vis Sci. 2000;41:1681–3. [PubMed] [Google Scholar]
- 113.Dreyer R, Rose RC. Lachrymal gland uptake and metabolism of ascorbic acid. Proc Soc Exp Biol Med. 1993;202:212–6. doi: 10.3181/00379727-202-43529. [DOI] [PubMed] [Google Scholar]
- 114.Ringvold A, Anderssen E, Kjonniksen I. Distribution of ascorbate in the anterior bovine eye. Invest Ophthalmol Vis Sci. 2000;41:20–3. [PubMed] [Google Scholar]
- 115.Giblin FJ, McCready JP, Kodama T, Reddy VN. A direct correlation between the levels of ascorbic acid and H2O2 in aqueous humor. Exp Eye Res. 1984;38:87–93. doi: 10.1016/0014-4835(84)90142-8. [DOI] [PubMed] [Google Scholar]
- 116.Truscott RJ. Age-related nuclear cataract oxidation is the key. Exp Eye Res. 2005;80:709–25. doi: 10.1016/j.exer.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 117.Yildirim O, Ates, Tamer L, Muslu N, Ercan B, Atik U, et al. Changes in antioxidant enzyme activity and malondialdehyde level in patients with age-related macular degeneration. Ophthalmologica. 2004;218:202–6. doi: 10.1159/000076845. [DOI] [PubMed] [Google Scholar]
- 118.Chen JZ, Kadlubar FF. A new clue to glaucoma pathogenesis. Am J Med. 2003;114:697–8. doi: 10.1016/s0002-9343(03)00199-2. [DOI] [PubMed] [Google Scholar]
- 119.Ferreira SM, Lerner SF, Brunzini R, Evelson PA, Llesuy SF. Oxidative stress markers in aqueous humor of glaucoma patients. Am J Ophthalmol. 2004;137:62–9. doi: 10.1016/s0002-9394(03)00788-8. [DOI] [PubMed] [Google Scholar]
- 120.Yang J, Tezel G, Patil RV, Romno C, Wax MB. Serum autoantibody against glutathione-S-transferase in patients with glaucoma. Invest Ophthalmol Vis Sci. 2001;42:1273–6. [PubMed] [Google Scholar]
- 121.Gherghel D, Griffiths HR, Hilton EJ, Cunliffe IA, Hosking SL. Systemic reduction in glutathione levels occurs in patients with primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 2005;46:877–83. doi: 10.1167/iovs.04-0777. [DOI] [PubMed] [Google Scholar]
- 122.Yildirim O, Ates NA, Ercan B, Muslu N, Unlu A, Tamer L, Atik U, Kanik A. Role of oxidative stress enzymes in open angle glaucoma. Eye. 2005;19:580–3. doi: 10.1038/sj.eye.6701565. [DOI] [PubMed] [Google Scholar]
- 123.Flammer J, Haefliger IO, Orgul S, Resink T. Vascular dysregulation: A principal risk factor for glaucoma damage? J Glaucoma. 1999;8:21–9. [PubMed] [Google Scholar]
- 124.Tamm ER, Russell P, Johnson DH, Piatigorsky J. Human and monkey trabecular meshwork accumulate alpha B-crystallin in response to heat shock and oxidative stress. Invest Ophthalmol Vis Sci. 1996;37:2402–13. [PubMed] [Google Scholar]
- 125.Wiederholt M. Nitric Oxide and endothelin in aqueous humor outflow regulation. In: Haefliger IO, Flammer J, editors. Nitric Oxide and Endothelin in the Pathogenesis of Glaucoma. New York: Lippincott-Raven; 1998. pp. 168–77. [Google Scholar]
- 126.Orgul S, Gugleta K, Flammer J. Physiology of perfusion as it relates to the optic nerve head. Surv Ophthalmol. 1999;43:17–26. doi: 10.1016/s0039-6257(99)00009-0. [DOI] [PubMed] [Google Scholar]
- 127.Lipton SA. Neuronal protection and destruction by NO. Cell Death Diff. 1999;6:943–51. doi: 10.1038/sj.cdd.4400580. [DOI] [PubMed] [Google Scholar]
- 128.Izzotti A, Sacca SC, Cartiglia C, De Flora S. Oxidative deoxyribonucleic acid damage in the eyes of glaucoma patients. Am J Med. 2003;114:638–46. doi: 10.1016/s0002-9343(03)00114-1. [DOI] [PubMed] [Google Scholar]
- 129.Zhou L, Li Y, Yue BY. Oxidative stress affects cytoskeletal structure and cell-matrix interactions in cells from an ocular tissue: The trabecular meshwork. J Cell Physiol. 1999;180:182–9. doi: 10.1002/(SICI)1097-4652(199908)180:2<182::AID-JCP6>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 130.Saccà SC, Pascotto A, Camicione P, Capris P, Izzotti A. Oxidative DNA damage in human trabecular meshwork and its correlation with intraocular pressure and visual field in primary open angle glaucoma. Arch Ophthalmol. 2005;123:458–63. doi: 10.1001/archopht.123.4.458. [DOI] [PubMed] [Google Scholar]
- 131.Hosseini A, Lattanzio FA, Schellenberg K, Shaeffer J, Samudre SS, Williams PB. Effects of novel free radical scavengers on intraocular pressure and electroretinograms in rat glaucoma models. FASEB J. 2006;20:689. [Google Scholar]
- 132.Ko ML, Hu DN, Ritch R, Sharma SC. The combined effect of brain-derived neurotrophic factor and a free radical scavenger in experimental glaucoma. Invest Ophthalmol Vis Sci. 2000;41:2967–71. [PubMed] [Google Scholar]
- 133.Koseki Y, Kitano S, Podos SM. A nitric oxide synthase inhibitor protects against anoxia in cultured rat retinal ganglion cells. Invest Ophthalmol Vis Sci. 1994;35:1968. [Google Scholar]
- 134.Lipton SA. Paradigm shift in NMDA receptor antagonist drug development: Molecular mechanism of uncompetitive inhibition by memantine in the treatment of Alzheimer's disease and other neurologic disorders. J Alzheimers Dis. 2004;6:S61–74. doi: 10.3233/jad-2004-6s610. [DOI] [PubMed] [Google Scholar]


