Abstract
OBJECTIVE
Insufficient insulin secretion is a hallmark of type 2 diabetes, and exposure of β-cells to elevated lipid levels (lipotoxicity) contributes to secretory dysfunction. Functional ablation of protein kinase C ε (PKCε) has been shown to improve glucose homeostasis in models of type 2 diabetes and, in particular, to enhance glucose-stimulated insulin secretion (GSIS) after lipid exposure. Therefore, we investigated the lipid-dependent mechanisms responsible for the enhanced GSIS after inactivation of PKCε.
RESEARCH DESIGN AND METHODS
We cultured islets isolated from PKCε knockout (PKCεKO) mice in palmitate prior to measuring GSIS, Ca2+ responses, palmitate esterification products, lipolysis, lipase activity, and gene expression.
RESULTS
The enhanced GSIS could not be explained by increased expression of another PKC isoform or by alterations in glucose-stimulated Ca2+ influx. Instead, an upregulation of the amplifying pathways of GSIS in lipid-cultured PKCεKO β-cells was revealed under conditions in which functional ATP-sensitive K+ channels were bypassed. Furthermore, we showed increased esterification of palmitate into triglyceride pools and an enhanced rate of lipolysis and triglyceride lipase activity in PKCεKO islets. Acute treatment with the lipase inhibitor orlistat blocked the enhancement of GSIS in lipid-cultured PKCεKO islets, suggesting that a lipolytic product mediates the enhancement of glucose-amplified insulin secretion after PKCε deletion.
CONCLUSIONS
Our findings demonstrate a mechanistic link between lipolysis and the amplifying pathways of GSIS in murine β-cells, and they suggest an interaction between PKCε and lipolysis. These results further highlight the therapeutic potential of PKCε inhibition to enhance GSIS from the β-cell under conditions of lipid excess.
Type 2 diabetes is characterized by hyperglycemia and dyslipidemia, and it results from insufficient insulin secretion from pancreatic β-cells to overcome the resistance of peripheral tissues to the actions of insulin. Insulin resistance is driven by genetic and environmental factors, but it is initially counteracted by an enlargement of β-cell mass and increased insulin output to maintain normal glucose homeostasis. Subsequent loss of β-cell mass and function in susceptible individuals causes impaired glucose homeostasis and progression to overt type 2 diabetes (1,2). The mechanisms underlying β-cell failure are poorly understood (3–5), although there is evidence that the β-cells of predisposed individuals are particularly compromised by exposure to high levels of circulating fatty acids, as occurs during obesity and insulin resistance (6). Moreover, model systems in which β-cells are chronically exposed to fatty acids (lipotoxicity) recapitulate both the loss of β-cell mass and many of the insulin secretory defects that are characteristic of type 2 diabetes (7,8).
Glucose-stimulated insulin secretion (GSIS) consists of triggering and amplifying pathways (9). Glucose triggers insulin secretion by generating ATP from oxidative metabolism, which closes ATP-sensitive K+ (KATP) channels, thereby inducing a membrane depolarization that stimulates Ca2+ influx via voltage-dependent Ca2+ channels. The amplifying pathways allow glucose to potentiate the secretory response to a given rise in cytosolic Ca2+ in a depolarized (triggered) β-cell (9). There is currently no consensus on the mechanism(s) coupling glucose metabolism to the amplification of insulin secretion, although several have been proposed (10–12). One candidate mechanism relates to the regulation by glucose of endogenous lipid signaling in the β-cell (11,12).
The protein kinase C (PKC) superfamily consists of conventional, novel, and atypical isoforms of serine-threonine protein kinases. The lipid-regulated subgroup of novel PKCs has been broadly implicated in the development of insulin resistance (13). This is particularly true of the PKCε isoform under conditions of nutrient oversupply (14–16) and in the livers of human type 2 diabetic subjects (17). Functional inhibition of PKCε also improves glucose homeostasis in rodent models of type 2 diabetes (18,19) and reverses acute lipid-induced hepatic insulin resistance (20). Unexpectedly, however, we recently found that enhancement of GSIS was another major means by which inhibition of PKCε function improves glucose homeostasis. This enhancement was observed in both dietary and genetic mouse models of type 2 diabetes and when using ex vivo models of β-cell dysfunction (18). Others have also reported a role for PKCε in the maturation of proinsulin to insulin (21). Because the mechanisms by which PKCε deletion improves GSIS remain unclear, our current aim was to investigate the potential role of alterations in β-cell lipid metabolism. We demonstrate that after chronic lipid exposure, PKCεKO islets show a selective increase of the amplification pathways of GSIS. This was associated with a chronic increase of palmitate tracer incorporation into triglyceride stores, and it was dependent on an increase in the subsequent glucose-stimulated hydrolysis of those stores.
RESEARCH DESIGN AND METHODS
The PKCεKO mouse has global deletion of the Prkce gene, as described previously (18). Ethical approval for mouse studies was granted by the Garvan/St. Vincent's Hospital animal ethics committee. Mice were maintained on a hybrid 129Sv/C57BL/6 background using PKCε heterozygous (Prkce+/−) breeding pairs; 12-week-old male wild-type (Prkce+/+) and PKCεKO (Prkce−/−) littermates were used for experiments. Mice had free access to water and standard mouse chow and were housed with a 12-h light/dark cycle.
Islet isolation and insulin secretion assays.
Islets were isolated as previously described (22). After pancreatic digestion, islets were purified using a Ficoll-paque (GE Healthcare, Chalfont St. Giles, U.K.) gradient before overnight culture in Dulbecco's modified Eagle's medium with 11 mmol/l glucose and 10% FCS (Invitrogen, PAISLEY, U.K.). Islets were cultured for a further 48–72 h (chronic culture) with additional 0.4 mmol/l palmitate coupled to 0.92% BSA (lipid) or BSA alone prior to study (18).
For insulin secretion assays, islets were preincubated for 1 h in Krebs-Ringer buffer containing HEPES (KRBH) containing 0.1% BSA and 2 mmol/l glucose. Batches of five islets were incubated at 37°C for 1 h in 130 μl KRBH containing 0.1% BSA and 2 mmol/l glucose (basal) supplemented with glucose (20 mmol/l) or other additions, as indicated in the text. For inhibition of lipolysis, orlistat (Sigma, St. Louis, MO), used at 200 μmol/l (unless otherwise stated), or vehicle (0.52% DMSO) was included in the KRBH throughout the insulin secretion experiment, but not during chronic culture. Insulin release was determined by radioimmunoassay (Linco/Millipore, Billerica, MA).
Western blotting.
Islet lysis and Western blotting was adapted from previous protocols (22). Islets were washed and lysed, and protein content was determined by bicinchoninic acid assay (Pierce/Thermo Scientific, Rockford, IL). Then, 25 μg protein was resolved on a 7% SDS-PAGE gel (Invitrogen) before transfer to polyvinylidene difluoride. Membranes were blocked with milk and probed with the following antibodies for 2 h at 21°C: anti-PKCα (no. 610108; BD Biosciences, San Jose, CA); anti-PKCβ (no. SC209), anti-PKCδ (no. SC213), anti-PKCζ (no. SC216), and anti–14-3-3β (no. SC1657; Santa Cruz Biotechnology, Santa Cruz, CA); anti–phospho–acetyl-CoA carboxylase (anti–phospho-ACC; no. 3661), anti-ACC (no. 3662), anti–phospho–AMP-activated protein kinase-α (anti–phospho-AMPKα) Thr172 (no. 2535), and anti-AMPKα (no. 2532; Cell Signaling Technology, Boston, MA); anti–β-actin (Sigma); and anti–hormone-sensitive lipase (anti–Hsl; Abcam, Cambridge, U.K.). Anti–adipose triglyceride lipase (anti–Atgl) was a gift from M. Watt (Monash University). After chemiluminescent detection, densitometry was performed using ImageJ1.38q (National Institutes of Health, Bethesda, MD).
Live cell imaging.
Live cell imaging was adapted from Ref. (23), as described in the methods section in the supplementary information, which is available in an online appendix at http://diabetes.diabetesjournals.org/cgi/content/full/db09-0132/DC1.
Lipid tracing, glycerol release, and lipase activity measurements.
Lipid tracing experiments were performed by adding 20 μCi/ml of [U-14C]palmitate to the culture media for 48 h with 0.4 mmol/l of unlabeled palmitate coupled to 0.92% BSA. Lipid extractions, thin-layer chromatography, and liquid scintillation spectrometry was performed as previously described (18,24). For glycerol release measurements, islets were cultured in palmitate (as above), and batches of 150 islets were incubated in 50 μl KRBH containing 20 mmol/l glucose for 3.5 h at 37°C. KRBH glycerol content was determined using free glycerol reagent (Sigma). Triglyceride lipase and cholesteryl-ester hydrolase activities were assessed using an established protocol (25). Islets were cultured with palmitate (as above) and acutely stimulated with 20 mmol/l glucose for 1 h before mechanical homogenization (100 islets/120 μl homogenization buffer).
RNA isolation and real-time quantitative RT-PCR.
RNA extraction and real-time PCR were performed using the TaqMan system (Applied Biosytems, Foster City, CA). Detailed methods and probe sets used are described in the methods section in the supplementary information.
Statistics.
All statistics were performed using GraphPad Prism5 software (Graphpad Software, La Jolla, CA) and unpaired Student's t tests and two-way ANOVA performed as appropriate. P < 0.05 was regarded as significant.
RESULTS
Effect of PKCε deletion on the expression of other PKC isoforms.
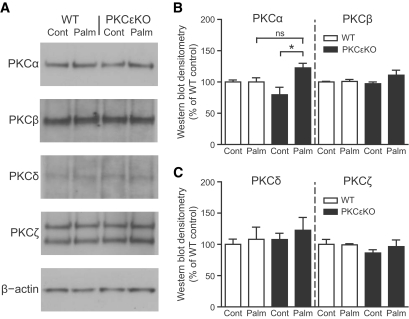
The PKC family controls multiple aspects of β-cell function (26). Therefore, one possible explanation for the increased GSIS from lipid-cultured PKCεKO islets might be enhanced expression of another PKC isoform capable of promoting secretion. We therefore compared the PKC expression profile from islets isolated from PKCεKO and wild-type mice and cultured for 48 h with palmitate (chronic lipid culture). Protein levels of PKCβ, PKCδ, and PKCζ were indistinguishable between these groups. However, we found slightly increased expression of PKCα in PKCεKO islets after lipid culture, but this is unlikely to be of functional significance because the expression was not significantly altered from the lipid-cultured wild-type group (Fig. 1A–C). Total DNA and protein contents of PKCεKO islets were not significantly altered from those of wild-type mice after lipid culture. Islet DNA content (mean ± SE) for wild-type islets was 9.1 ± 0.26 ng, versus 8.5 ± 0.25 ng for PKCεKO (not significant, n = 10). Islet protein content for wild-type islets was 320 ± 10.3 ng, versus 319 ± 9.9 ng for PKCεKO (not significant, n = 10).
FIG. 1.
Expression of PKC isoforms in PKCεKO islets. Islets isolated from 12-week-old male mice were cultured for 48 h in the presence of 0.4 mmol/l palmitate coupled to 0.92% BSA (Palm) or BSA alone (Cont) prior to lysis. A: Islet proteins were resolved by SDS-PAGE, and immunoblots for PKCα, PKCβ, PKCδ, PKCζ, and β-actin (loading control) were performed. B and C: Densitometry quantification of Western blots. Data are means ± SE from a representative experiment with n = 4 animals. The experiment was repeated twice from independent islet preparations. *P < 0.05. WT, wild type.
PKCεKO islets show enhanced glucose-amplified insulin secretion.
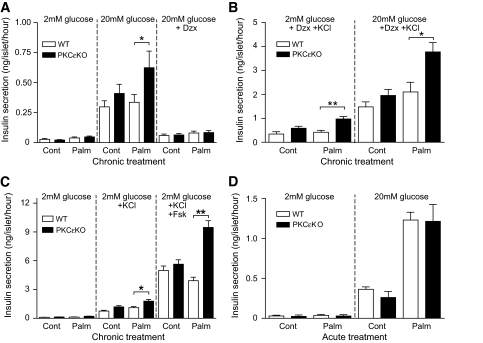
As shown previously (18), deletion of PKCε did not alter acute GSIS from islets cultured under control conditions, but it selectively enhanced this response after lipid culture (Fig. 2A). GSIS from islets under all treatment conditions was inhibited by diazoxide (Fig. 2A), which maintains KATP channels in an open conformation, preventing membrane depolarization. These results indicate that the enhanced GSIS in PKCεKO islets was dependent on normal coupling of glucose metabolism with depolarization-dependent Ca2+ influx. To measure the amplification pathways, or KATP channel–independent secretion, GSIS assays were performed in the combined presence of diazoxide and 25 mmol/l KCl (9). The latter serves as a nonmetabolic depolarizing stimulus to activate voltage-gated Ca2+ channels and trigger insulin secretion under conditions in which the glucose-dependent initiation signal is inhibited by diazoxide. The secretory response to glucose in this protocol thus represents the amplification pathway (9), which was operative in all treatment groups (Fig. 2B). Moreover, after lipid culture, glucose-amplified insulin secretion was nearly doubled from PKCεKO islets relative to wild-type islets (Fig. 2B), whereas no significant difference between the two genotypes was observed under control culture conditions. These results suggest that an augmentation of the amplifying pathways is a major contributor to the overall enhancement of GSIS observed in lipid-cultured PKCεKO islets.
FIG. 2.
The amplifying pathways of GSIS are upregulated in PKCεKO islets. A–C: Islets isolated from 12-week-old male mice were cultured for 48 h (chronic) in the presence of 0.4 mmol/l palmitate coupled to 0.92% BSA (Palm) or BSA alone (Cont). A: GSIS in response to 20 mmol/l glucose and inhibition by diazoxide (Dzx; 100 μmol/l; n = 7). B: KATP channel–independent glucose-amplified insulin secretion in the presence of 25mmol/l KCl and diazoxide (n = 5). C: Insulin secretion in response to nonnutrient secretogogues KCl (25 mmol/l) and forskolin (1 μmol/l; n = 3). D: Acute palmitate-potentiated GSIS from islets without chronic palmitate culture (n = 4). Data are the means ± SE. *P < 0.05; **P < 0.01. WT, wild type.
Although quantitatively much smaller than the effect on GSIS, secretion in response to the depolarizing stimulus KCl (at basal glucose) was also significantly elevated in PKCεKO versus wild-type islets after lipid culture, but not under control culture conditions. As expected, this response to KCl was induced irrespective of whether KATP channel closure was blocked with diazoxide (Fig. 2B) or not (Fig. 2C). When forskolin was used to activate adenylyl cyclase and increase cAMP levels, KCl-induced insulin secretion was enhanced in all treatment groups (Fig. 2C). As with the GSIS experiments, the combination of lipid culture and PKCε deletion elicited a significantly greater secretory response than the other conditions.
In addition to its chronic effects, palmitate can also acutely potentiate GSIS from β-cells (27). To test whether PKCε deletion influences this process, we examined the acute effect of palmitate on GSIS from PKCεKO islets without chronic culture. Addition of palmitate during static secretion experiments produced equivalent responses from both PKCεKO and wild-type islets (Fig. 2D), suggesting that the mechanism underlying the enhanced GSIS in PKCεKO islets is independent of the potentiation of GSIS by palmitate.
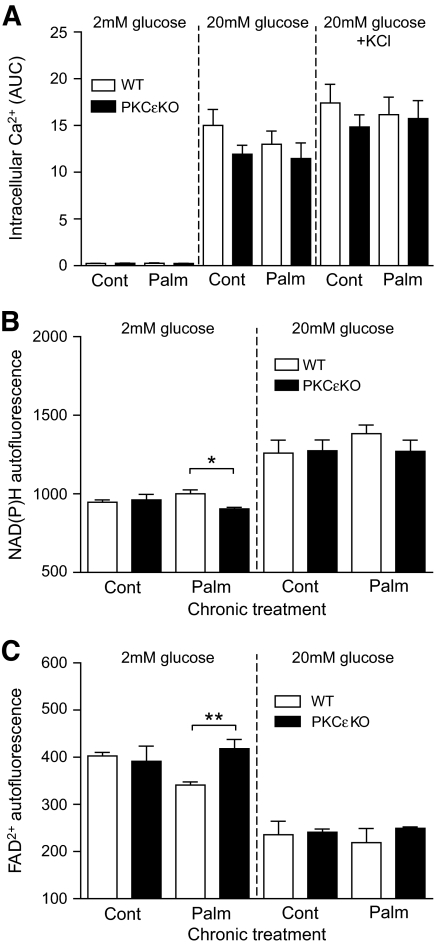
PKCεKO islets have normal intracellular free Ca2+, NAD(P)H, and flavin adenine dinucleotide levels in response to high glucose.
Although the above results point strongly to an involvement of PKCε deletion in the amplifying pathways of GSIS, they do not exclude an effect on the triggering pathway. To address this more directly, we measured the increase in intracellular free Ca2+ after glucose and KCl stimulation. Increases in intracellular free Ca2+ were equivalent in chronic lipid-cultured PKCεKO β-cells and all other groups tested (Fig. 3A and supplementary Fig. A1). This argues against alterations in the triggering pathway, upstream of Ca2+ gating, as being implicated in the enhanced GSIS we observed in lipid-cultured PKCεKO islets.
FIG. 3.
PKCεKO islets have normal intracellular free Ca2+, NAD(P)H, and FAD2+ responses to glucose. Live imaging of β-cells from 12-week-old male mice after culture for 48 h in the presence of 0.4 mmol/l palmitate coupled to 0.92% BSA (Palm) or BSA alone (Cont). A: Intracellular free Ca2+ levels measured by confocal microscopy in Furared-loaded β-cells in response to glucose and KCl, as indicated. Area under the curve (AUC) measurements were made from the complete time course trace data presented in supplementary Fig. A1. B and C: NAD(P)H and FAD2+ autofluorescence measured by microscopy in response to glucose, as indicated. Data are the means ± SE from four independent recordings from two independent cell preparations, with >20 cells monitored per recording. *P < 0.05; **P < 0.01. WT, wild type.
We next measured the redox state of the pyridine nucleotide NAD(P)H as well as flavin adenine dinucleotide (FAD2+) as a measure of glucose-stimulated metabolic flux. The autofluorescent signal captured during these redox imaging experiments is likely that of mitochondrial NADH and FAD2+ because of the abundance and concentration of the mitochondrial signal (28). Glucose stimulated both increases in NAD(P)H and decreases in the FAD2+ signal (indicating increased FADH2), but these were unaltered by PKCε deletion and/or chronic lipid culture (Fig. 3B and C). This suggests that normal metabolic flux is maintained under these conditions, and it indicates that alterations of these hydrogen carriers are unlikely to be involved in the augmentation of the amplifying pathways of GSIS described above. Under basal glucose conditions, however, lipid-cultured PKCεKO islets showed a small significant decrease in NAD(P)H levels and an increase in FAD2+ signal, indicating decreased FADH2, relative to lipid-cultured wild-type islets (Fig. 3B and C). Although this suggests that PKCε deletion might impact basal metabolic flux, we did not pursue this finding here, given our focus on GSIS.
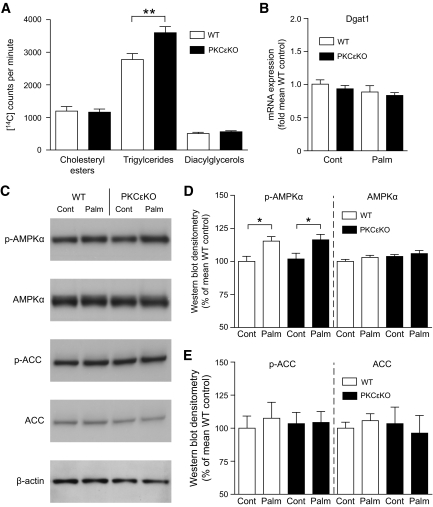
Triglyceride levels derived from exogenous palmitate are elevated in PKCεKO islets.
Acute incubation of lipid-pretreated PKCεKO islets with [U-14C]palmitate had previously revealed a switch in glucose-regulated lipid partitioning, favoring lipid esterification over oxidation (18). That approach, however, did not address whether endogenous lipid pools were chronically altered by PKCε deletion. We therefore measured incorporation of [U-14C]palmitate into neutral lipid pools over 48 h of palmitate culture, which revealed equivalent 14C labeling of diacylglycerols and cholesteryl-esters in PKCεKO and wild-type islets (Fig. 4A). However, we did observe a significant increase in triglycerides derived from exogenous [U-14C]palmitate in PKCεKO islets (Fig. 4A). Despite this, oil red O staining of lipid droplets in chronic lipid-cultured PKCεKO β-cells was indistinguishable from that of wild-type β-cells (data not shown). Expression of the enzyme diacylglycerol acyltransferase (Dgat1), responsible for the formation of triglyceride from diacylglycerol, was unaltered in islets by palmitate culture and/or PKCε deletion (Fig. 4B), excluding this as a mechanism for the enhanced triglyceride esterification in PKCεKO islets.
FIG. 4.
Enhanced incorporation of fatty acids into triglyceride stores in PKCεKO β-cells. A: Islets were cultured for 48 h with 0.4 mmol/l palmitate coupled to 0.92% BSA and 20 μCi/ml of [U-14C]palmitate. Islet lipid extracts were resolved by silica thin-layer chromatography, and incorporation of 14C-palmitate into neutral lipid pools was quantified by liquid scintillation spectrometry (n = 10–12). B: Diacylglycerol acyltransferase 1 (Dgat1) mRNA expression in islets after culture for 48 h in the presence of 0.4 mmol/l palmitate coupled to 0.92% BSA (Palm) or BSA alone (Cont). Data were expressed relative to wild-type control islets (n = 5). C–E: Islets from 12-week-old male mice, after palmitate or control culture, were lysed and proteins resolved by SDS-PAGE before immunoblots were performed for phospho-ACC Ser79 (p-ACC), ACC, phospho-AMPKα Thr172 (p-AMPKα), AMPKα, and β-actin (loading control). D and E: Densitometry quantification of Western blots; n = 4 animals from two independent islet preparations were used. Data are the means ± SE. *P < 0.05; **P < 0.01. WT, wild type.
One mechanism for the control of lipid partitioning and deposition of neutral lipid stores is the regulation of ACC activity by AMPK and the subsequent modulation of malonyl-CoA production and β-oxidation (29). Therefore, we analyzed phospho-specific markers of AMPK and ACC activity by immunoblotting. Phosphorylation of AMPKα (Thr172) was increased subtly yet significantly after chronic lipid culture of islets, but this was equivalent in both genotypes (Fig. 4C and D), suggesting that alterations in AMPK activity do not explain the increase in GSIS observed under these conditions. Chronic lipid culture has been previously shown to increase AMPKα (Thr172) phosphorylation (30), but in our hands this was not accompanied by a corresponding change in ACC (Ser79) phosphorylation (Fig. 4C–E). Although a somewhat surprising finding, this is still consistent with our overall conclusion that alterations in the AMPK/ACC axis do not account for the effects of PKCε deletion on GSIS.
Lipolysis is enhanced in PKCεKO islets and is required to mediate enhanced GSIS after lipid culture.
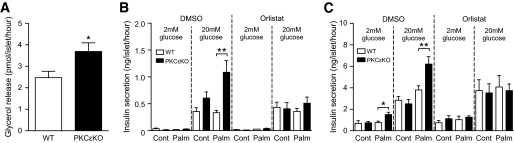
Mobilization of endogenous neutral lipid stores by lipolysis has been implicated in GSIS in rat β-cells (31,32), and these processes are glucose regulated in rat and mouse β-cells (33,34). Thus, lipolytic pathways may link the increased triglyceride formation with the enhanced lipid-dependent GSIS in PKCεKO islets. Therefore, we assayed lipolysis as glycerol generation because this metabolite is released from β-cells after lipolysis, rather than being recycled (35). Glucose-stimulated glycerol production from PKCεKO islets was significantly increased compared with wild-type islets after chronic lipid culture (Fig. 5A), suggesting that enhanced lipolysis might underlie the augmentation of GSIS observed under these conditions. To test this more directly, we assessed GSIS in the presence of the lipase inhibitor orlistat (0.2 mmol/l). Although without effect on wild-type islets, orlistat completely blocked the enhancement of GSIS and glucose-amplified insulin secretion otherwise observed using PKCεKO islets (Fig. 5B and C). This inhibition was dose dependent (supplementary Fig. A2).
FIG. 5.
Enhanced lipolysis is required for enhanced secretion in PKCεKO islets. Islets isolated from 12-week-old male mice were cultured for 48–72 h in the presence of 0.4 mmol/l palmitate coupled to 0.92% BSA (Palm) or BSA alone (Cont). A: Lipolysis was measured in islets, after palmitate culture, by detection of glycerol release in response to 20 mmol/l d-glucose (n = 7). B: GSIS in palmitate-cultured PKCεKO islets in the presence of the lipase inhibitor orlistat (0.2 mmol/l) or DMSO vehicle control (n = 9). C: Glucose-amplified insulin secretion measured under KATP channel–independent depolarizing conditions (25 mmol/l KCl and 100 μmol/l diazoxide) using palmitate-cultured PKCεKO islets in the presence of orlistat or DMSO control (n = 9). Data are the means ± SE. *P < 0.05; **P < 0.01. WT, wild type.
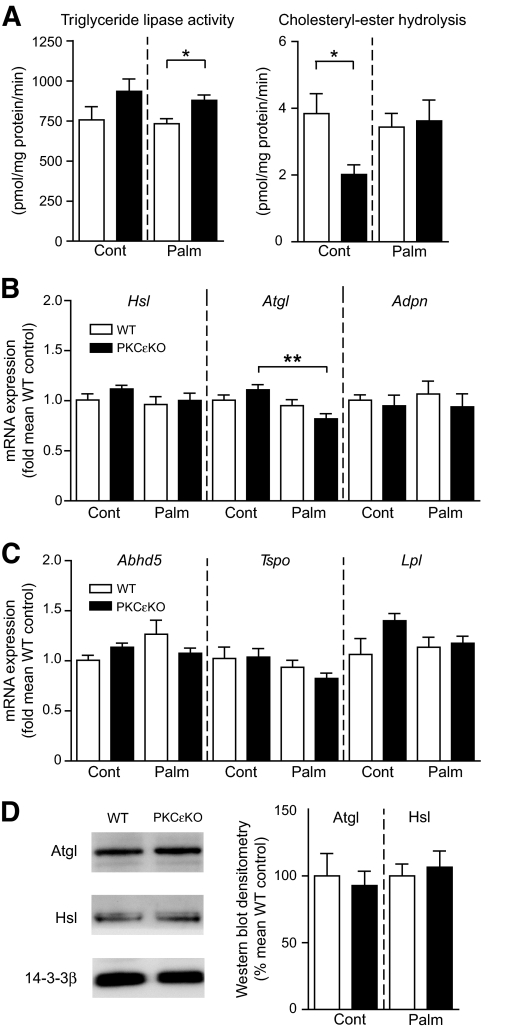
Triglyceride lipase activity is enhanced in PKCεKO islets.
We next measured glucose-stimulated lipase activities directly, using homogenates of islets derived from our different treatment groups. Triglyceride lipolysis was significantly enhanced in PKCεKO islets after palmitate culture and showed a similar, albeit nonsignificant, increase after control culture relative to wild-type islets (Fig. 6A). Cholesteryl-ester hydrolysis was 200-fold lower than that of triglyceride and was downregulated in control-cultured PKCεKO islets, relative to wild-type islets, but unaltered by genotype after palmitate culture (Fig. 6A).
FIG. 6.
Lipase activities and gene expression in PKCεKO islets. A: Lipase activities of islet homogenates after culture for 48 h in the presence of 0.4 mmol/l palmitate coupled to 0.92% BSA (Palm) or BSA alone (Cont) and subsequent stimulation with 20 mmol/l glucose for 1 h. Triglyceride or cholesteryl-ester lipid pools were provided as substrate, spiked with [3H]triolein or [14C]cholesteryl-oleate, respectively. Islets from n = 5 animals were used per genotype. B and C: mRNA expression of Hsl (Hsl), adipose triglyceride lipase (Atgl), adiponutrin (Adpn), α/β-hydrolase domain–containing protein 5 (Abhd5), translocator protein (Tspo), and lipoprotein lipase (Lpl). Islets were cultured in palmitate or control media, and data were expressed relative to wild-type control islets (n = 5). D: Western blot and quantification of Hsl and Atgl with 14-3-3β loading control; n = 3. □ = wild type, ■ = PKCεKO. Data are the means ± SE. *P < 0.05; **P < 0.01. WT, wild type.
Expression of lipases and associated factors in PKCεKO islets.
We used RT-PCR to investigate whether the enhanced PKCεKO islet triglyceride lipase activity could simply be explained by increased expression of lipases or associated genes. Expression of Hsl, Atgl, adiponutrin, and lipoprotein lipase was not increased with palmitate culture and/or deletion of PKCε (Fig. 6B–D). Atgl mRNA was slightly decreased by palmitate in PKCεKO islets (Fig. 6B), but neither mRNA nor protein levels were altered when compared with wild-type islets, indicating normal abundance of this lipase (Fig. 6B and D). We were unable to detect expression of pancreatic triglyceride lipase or the lipid droplet–associated protein perilipin (data not shown). Expression of α/β-hydrolase domain–containing protein 5—a protein known to regulate Atgl activity (36)—was unaltered by palmitate culture and/or PKCε deletion (Fig. 6C). Finally, we measured translocator protein gene (peripheral benzodiazepine receptor) mRNA levels because expression of this gene is known to be induced in some cell types by PKCε activation (37), and pharmacological activation of translocator protein causes β-cells dysfunction (38). However, expression of this gene was not altered by palmitate culture and/or PKCε deletion (Fig. 6C).
DISCUSSION
We have previously shown that functional inhibition of PKCε prevents glucose intolerance in mice fed a high-fat diet and improves glycemic control in diabetic db/db mice, in part because of an enhancement of insulin secretion (18). Enhanced GSIS from PKCεKO β-cells occurred selectively after lipid exposure, in vitro or in vivo, thereby increasing insulin output under pathophysiological conditions that confer an increased demand for insulin. Because of the potential therapeutic relevance of these findings to the treatment of type 2 diabetes, our current goal was to further characterize the molecular mechanisms underlying this phenotype. We first excluded the possible upregulation of another β-cell PKC isoform capable of promoting insulin secretion. Although we did find a small but significant increase in PKCα—a conventional PKC—in lipid-cultured PKCεKO islets, this is unlikely to be of functional relevance because we have previously shown that although conventional PKCs are activated by glucose in the β-cell, they are not required for GSIS (39).
Our current results provide two major advances in defining the mechanism whereby deletion of PKCε enhances GSIS in lipid-cultured islets. First, we have specifically identified the amplifying pathway as the major site of action. Importantly, and consistent with the specificity reported for overall GSIS (18), the augmentation of the amplification pathway in PKCεKO islets was only observed after lipid pretreatment. In addition, we have previously demonstrated an enhancement of both first- and second-phase GSIS after lipid culture of PKCεKO islets (18), which is still consistent with an enhancement of glucose-amplified insulin secretion because the amplifying pathways have been shown to be active during both phases of GSIS (40). By definition, the amplifying pathways function independently of changes in glucose-regulated intracellular Ca2+ concentrations (9). Consistent with this, we were unable to find an alteration in glucose-stimulated Ca2+ levels in PKCεKO β-cells after lipid culture. However, we do not exclude an additional effect on the triggering pathway downstream of Ca2+ influx because we did find slightly enhanced secretion in response to KCl (at basal glucose concentrations) selectively in lipid-cultured PKCεKO islets.
The molecular mechanisms underlying the amplifying pathways are poorly understood and controversial, although glucose-regulated lipid partitioning has been proposed as one coupling mechanism (11,12). Glucose-driven mitochondrial anaplerotic/cataplerotic pathways increase cytosolic levels of malonyl-CoA, which inhibits carnitine-palmitoyl transferase 1, thereby inhibiting β-oxidation and promoting the availability of long-chain acyl-CoA for esterification (41). This partitioning mechanism is a glucose-regulated signal that mediates, in part, the acute potentiation of GSIS by exogenous lipids (42). This coupling mechanism is broadly consistent with the second major finding reported here: enhanced mobilization of neutral lipid stores contributes to the increased GSIS we observe. We base this finding on several pieces of evidence, including, most directly, that orlistat selectively inhibited the augmented GSIS in lipid-cultured PKCεKO islets. In contrast to prior studies with rat islets (31,32), orlistat did not affect GSIS from wild-type mouse islets. Rat islets differ from mouse (and human) islets in that they have a more pronounced second phase of secretion (40), and it is this phase that is most sensitive to inhibition by orlistat (31). We are unaware of any previous reports of the effect of orlistat, or other lipase inhibitors, on GSIS from mouse islets.
The other pieces of evidence for a site of action in lipid partitioning relate to observed effects of PKCε deletion on the remodeling of neutral lipid stores. On the one hand, PKCεKO islets displayed increased incorporation of [14C]palmitate into triglyceride during 48-h culture with 11 mmol/l glucose. This extends our previous finding that during short-term glucose stimulation, lipid-pretreated PKCεKO islets were better able than wild-type islets to partition palmitate away from β-oxidation and toward esterification pathways (18). On the other hand, when assayed directly, glucose-stimulated triglyceride lipase activity was increased by PKCε deletion. The simplest explanation for our findings is that absence of PKCε during chronic lipid exposure results in enhanced deposition of triglyceride, which couples with enhanced lipolysis of this store during acute glucose stimulation and results in increased liberation of fatty acid in the PKCεKO β-cell. Potential inputs on both the deposition and mobilization of lipid stores would be consistent with the apparent absence on any alteration in overall lipid droplet content, and they imply that turnover of (a possibly unknown) neutral lipid contributes to the amplification of insulin secretion (31,32,43). How this fatty acid metabolite would act is unclear, but possibilities include autocrine/paracrine activation of β-cell G-protein–coupled receptors, or effects exerted intracellularly, via activation of lipid-regulated protein kinases or via acylation reactions (11,12). A final explanation for the enhanced lipolysis we observed in PKCεKO islets is that it represents an adaptive response to minimize the effects of nutrient toxicity after lipid loading (44). Further studies of the role of PKCε in lipid-cultured islets should help to resolve these possibilities, and they might shed further light on the poorly understood mechanisms underlying the amplifying pathways of GSIS.
The molecular targets of PKCε involved in regulating neutral lipid turnover remain to be identified, but our results now narrow the range of options. The finding that PKCε deletion affected triglyceride, but not diacylglycerol or cholesteryl-ester, pools suggests a mode of action independent of the broad regulation of β-oxidation versus neutral lipid synthesis that is controlled by glucose-stimulated malonyl-CoA levels. This is consistent with the observation that activation of neither the malonyl-CoA synthetic enzyme ACC, nor the upstream regulatory kinase AMPK, was altered when comparing the phosphorylation status of these proteins from wild-type or PKCεKO islets. The mechanism underlying the selectivity for deposition into triglycerides requires further investigation, but is unlikely to involve an effect of PKCε deletion on general fatty acid desaturation pathways because these impact on cholesteryl-ester as well as triglyceride formation in β-cells (24). The individual β-cell lipases responsible for coupling glucose-regulated lipolysis with the amplification of insulin secretion have not been fully established (45). Hsl is one candidate, although gene knockout studies have failed to reach a consensus on its role in β-cells (33,46,47). We have shown that the cAMP generator forskolin stimulates enhanced insulin secretion in PKCεKO islets. Because cAMP also activates lipolysis in β-cells (31,48), most probably via Hsl (49), it is possible that the activity of this enzyme may be elevated by PKCε deletion. However, the main Hsl substrates are thought to be diacylglycerols and cholesteryl-esters (45), so it is unlikely Hsl activity is responsible for the enhanced triglyceride lipolysis in PKCεKO islets. Other candidate β-cell lipases include Atgl and adiponutrin; although expression of these lipases was normal, we cannot rule in or out an upregulation of their activity in PKCεKO islets. Indeed, the GSIS phenotype in PKCεKO islets may prove a useful model for further studying the role of lipases in regulating β-cell function.
We have demonstrated that loss of PKCε function reprograms the mouse β-cell to increase GSIS after lipid exposure, via upregulation of the amplifying pathways of GSIS, which are dependent on lipolysis. Because loss of β-cell function correlates with poor prognosis during type 2 diabetes, strategies to improve GSIS remain attractive treatments for the disease. Our results here strengthen the case for further work on the inhibition of PKCε as a means of treating type 2 diabetes. Having now demonstrated a site of action in the amplifying pathways of GSIS, our work suggests PKCε inhibitors might act as a type of metabolic incretin, with the added advantage that they appear to target defective β-cells, such as those from db/db mice, or wild-type islets compromised by prior lipid exposure (18). Finally, a better understanding of the roles of PKCε in the β-cell could help elucidate the mechanisms whereby insulin secretion fails during the progression to type 2 diabetes.
Supplementary Material
Acknowledgments
This work was supported by the National Health and Medical Research Council of Australia and the Diabetes Australia Research Trust.
No potential conflicts of interest relevant to this article were reported.
We thank David Pederson and the Garvan Biological Testing Facility staff for technical assistance and Matthew Watt for provision of antibodies. We also thank Christopher Mitchell and Nigel Turner for critical evaluation of the manuscript.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Bell GI, Polonsky KS: Diabetes mellitus and genetically programmed defects in β-cell function. Nature 2001; 414: 788– 791 [DOI] [PubMed] [Google Scholar]
- 2.Kahn SE, Hull RL, Utzschneider KM: Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 2006; 444: 840– 846 [DOI] [PubMed] [Google Scholar]
- 3.Muoio DM, Newgard CB: Mechanisms of disease: molecular and metabolic mechanisms of insulin resistance and β-cell failure in type 2 diabetes. Nat Rev Mol Cell Biol 2008; 9: 193– 205 [DOI] [PubMed] [Google Scholar]
- 4.Prentki M, Nolan CJ: Islet β cell failure in type 2 diabetes. J Clin Invest 2006; 116: 1802– 1812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poitout V, Robertson RP: Glucolipotoxicity: fuel excess and β-cell dysfunction. Endocr Rev 2008; 29: 351– 366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kashyap S, Belfort R, Gastaldelli A, Pratipanawatr T, Berria R, Pratipanawatr W, Bajaj M, Mandarino L, DeFronzo R, Cusi K: A sustained increase in plasma free fatty acids impairs insulin secretion in nondiabetic subjects genetically predisposed to develop type 2 diabetes. Diabetes 2003; 52: 2461– 2474 [DOI] [PubMed] [Google Scholar]
- 7.Shimabukuro M, Zhou Y-T, Levi M, Unger RH: Fatty acid-induced β cell apoptosis: a link between obesity and diabetes. Proc Natl Acad Sci U S A 1998; 95: 2498– 2502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou YP, Grill VE: Long-term exposure of rat pancreatic islets to fatty acids inhibits glucose-induced insulin secretion and biosynthesis through a glucose fatty acid cycle. J Clin Invest 1994; 93: 870– 876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henquin JC, Ravier MA, Nenquin M, Jonas JC, Gilon P: Hierarchy of the β-cell signals controlling insulin secretion. Eur J Clin Invest 2003; 33: 742– 750 [DOI] [PubMed] [Google Scholar]
- 10.Jensen MV, Joseph JW, Ronnebaum SM, Burgess SC, Sherry AD, Newgard CB: Metabolic cycling in control of glucose-stimulated insulin secretion. Am J Physiol Endocrinol Metab 2008; 295: E1287– E1297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nolan CJ, Madiraju MS, Delghingaro-Augusto V, Peyot ML, Prentki M: Fatty acid signaling in the β-cell and insulin secretion. Diabetes 2006; 55( Suppl. 2): S16– S23 [DOI] [PubMed] [Google Scholar]
- 12.Yaney GC, Corkey BE: Fatty acid metabolism and insulin secretion in pancreatic beta cells. Diabetologia 2003; 46: 1297– 1312 [DOI] [PubMed] [Google Scholar]
- 13.Schmitz-Peiffer C, Biden TJ: Protein kinase C function in muscle, liver, and β-cells and its therapeutic implications for type 2 diabetes. Diabetes 2008; 57: 1774– 1783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schmitz-Peiffer C, Browne CL, Oakes ND, Watkinson A, Chisholm DJ, Kraegen EW, Biden TJ: Alterations in the expression and cellular localization of protein kinase C isozymes ε and θ are associated with insulin resistance in skeletal muscle of the high-fat-fed rat. Diabetes 1997; 46: 169– 178 [DOI] [PubMed] [Google Scholar]
- 15.Samuel VT, Liu ZX, Qu X, Elder BD, Bilz S, Befroy D, Romanelli AJ, Shulman GI: Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. J Biol Chem 2004; 279: 32345– 32353 [DOI] [PubMed] [Google Scholar]
- 16.Laybutt DR, Schmitz-Peiffer C, Saha AK, Ruderman NB, Biden TJ, Kraegen EW: Muscle lipid accumulation and protein kinase C activation in the insulin-resistant chronically glucose-infused rat. Am J Physiol 1999; 277: E1070– E1076 [DOI] [PubMed] [Google Scholar]
- 17.Considine RV, Nyce MR, Allen LE, Morales LM, Triester S, Serrano J, Colberg J, Lanza-Jacoby S, Caro JF: Protein kinase C is increased in the liver of humans and rats with non-insulin-dependent diabetes mellitus: an alteration not due to hyperglycemia. J Clin Invest 1995; 95: 2938– 2944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schmitz-Peiffer C, Laybutt DR, Burchfield JG, Gurisik E, Narasimhan S, Mitchell CJ, Pedersen DJ, Braun U, Cooney GJ, Leitges M, Biden TJ: Inhibition of PKCε improves glucose-stimulated insulin secretion and reduces insulin clearance. Cell Metab 2007; 6: 320– 328 [DOI] [PubMed] [Google Scholar]
- 19.Mack E, Ziv E, Reuveni H, Kalman R, Niv MY, Jorns A, Lenzen S, Shafrir E: Prevention of insulin resistance and beta-cell loss by abrogating PKCε-induced serine phosphorylation of muscle IRS-1 in Psammomys obesus. Diabetes Metab Res Rev 2008; 24: 577– 584 [DOI] [PubMed] [Google Scholar]
- 20.Samuel VT, Liu Z-X, Wang A, Beddow SA, Geisler JG, Kahn M, Zhang X-M, Monia BP, Bhanot S, Shulman GI: Inhibition of protein kinase Cε prevents hepatic insulin resistance in nonalcoholic fatty liver disease. J Clin Invest 2007; 117: 739– 745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Warwar N, Dov A, Abramovitch E, Wu R, Jmoudiak M, Haber E, Cerasi E, Nesher R: PKCepsilon mediates glucose-regulated insulin production in pancreatic beta-cells. Biochim Biophys Acta 2008; 1783: 1929– 1934 [DOI] [PubMed] [Google Scholar]
- 22.Cantley J, Choudhury AI, Asare-Anane H, Selman C, Lingard S, Heffron H, Herrera P, Persaud SJ, Withers DJ: Pancreatic deletion of insulin receptor substrate 2 reduces beta and alpha cell mass and impairs glucose homeostasis in mice. Diabetologia 2007; 50: 1248– 1256 [DOI] [PubMed] [Google Scholar]
- 23.Cantley J, Selman C, Shukla D, Abramov AY, Forstreuter F, Esteban MA, Claret M, Lingard SJ, Clements M, Harten SK, Asare-Anane H, Batterham RL, Herrera PL, Persaud SJ, Duchen MR, Maxwell PH, Withers DJ: Deletion of the von Hippel-Lindau gene in pancreatic β cells impairs glucose homeostasis in mice. J Clin Invest 2009; 119: 125– 135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Busch AK, Gurisik E, Cordery DV, Sudlow M, Denyer GS, Laybutt DR, Hughes WE, Biden TJ: Increased fatty acid desaturation and enhanced expression of stearoyl coenzyme A desaturase protects pancreatic β-cells from lipoapoptosis. Diabetes 2005; 54: 2917– 2924 [DOI] [PubMed] [Google Scholar]
- 25.Holm C, Osterlund T: Hormone-sensitive lipase and neutral cholesteryl ester lipase. Methods Mol Biol 1999; 109: 109– 121 [DOI] [PubMed] [Google Scholar]
- 26.Biden TJ, Schmitz-Peiffer C, Burchfield JG, Gurisik E, Cantley J, Mitchell CJ, Carpenter L: The diverse roles of protein kinase C in pancreatic β-cell function. Biochem Soc Trans 2008; 36: 916– 919 [DOI] [PubMed] [Google Scholar]
- 27.Stein DT, Stevenson BE, Chester MW, Basit M, Daniels MB, Turley SD, McGarry JD: The insulinotropic potency of fatty acids is influenced profoundly by their chain length and degree of saturation. J Clin Invest 1997; 100: 398– 403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duchen MR, Surin A, Jacobson J: Imaging mitochondrial function in intact cells. Methods Enzymol 2003; 361: 353– 389 [DOI] [PubMed] [Google Scholar]
- 29.Ruderman N, Prentki M: AMP kinase and malonyl-CoA: targets for therapy of the metabolic syndrome. Nat Rev Drug Discov 2004; 3: 340– 351 [DOI] [PubMed] [Google Scholar]
- 30.Wang X, Zhou L, Li G, Luo T, Gu Y, Qian L, Fu X, Li F, Li J, Luo M: Palmitate activates AMP-activated protein kinase and regulates insulin secretion from β cells. Biochem Biophys Res Commun 2007; 352: 463– 468 [DOI] [PubMed] [Google Scholar]
- 31.Mulder H, Yang S, Winzell MS, Holm C, Ahren B: Inhibition of lipase activity and lipolysis in rat islets reduces insulin secretion. Diabetes 2004; 53: 122– 128 [DOI] [PubMed] [Google Scholar]
- 32.Nolan CJ, Leahy JL, Delghingaro-Augusto V, Moibi J, Soni K, Peyot ML, Fortier M, Guay C, Lamontagne J, Barbeau A, Przybytkowski E, Joly E, Masiello P, Wang S, Mitchell GA, Prentki M: Beta cell compensation for insulin resistance in Zucker fatty rats: increased lipolysis and fatty acid signalling. Diabetologia 2006; 49: 2120– 2130 [DOI] [PubMed] [Google Scholar]
- 33.Peyot ML, Nolan CJ, Soni K, Joly E, Lussier R, Corkey BE, Wang SP, Mitchell GA, Prentki M: Hormone-sensitive lipase has a role in lipid signaling for insulin secretion but is nonessential for the incretin action of glucagon-like peptide 1. Diabetes 2004; 53: 1733– 1742 [DOI] [PubMed] [Google Scholar]
- 34.Winzell MS, Ström K, Holm C, Ahrén B: Glucose-stimulated insulin secretion correlates with β-cell lipolysis. Nutr Metab Cardiovasc Dis 2006; 16( Suppl.1): S11– S16 [DOI] [PubMed] [Google Scholar]
- 35.Noel RJ, Antinozzi PA, McGarry JD, Newgard CB: Engineering of glycerol-stimulated insulin secretion in islet beta cells: differential metabolic fates of glucose and glycerol provide insight into mechanisms of stimulus-secretion coupling. J Biol Chem 1997; 272: 18621– 18627 [DOI] [PubMed] [Google Scholar]
- 36.Lass A, Zimmermann R, Haemmerle G, Riederer M, Schoiswohl G, Schweiger M, Kienesberger P, Strauss JG, Gorkiewicz G, Zechner R: Adipose triglyceride lipase-mediated lipolysis of cellular fat stores is activated by CGI-58 and defective in Chanarin-Dorfman syndrome. Cell Metab 2006; 3: 309– 319 [DOI] [PubMed] [Google Scholar]
- 37.Batarseh A, Giatzakis C, Papadopoulos V: Phorbol-12-myristate 13-acetate acting through protein kinase Cε induces translocator protein (18-kDa) TSPO gene expression. Biochemistry 2008; 47: 12886– 12899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marselli L, Trincavelli L, Santangelo C, Lupi R, Del Guerra S, Boggi U, Falleni A, Gremigni V, Mosca F, Martini C, Dotta F, Di Mario U, Del Prato S, Marchetti P: The role of peripheralbenzodiazepine receptors on the function and survival of isolated human pancreatic islets. Eur J Endocrinol 2004; 151: 207– 214 [DOI] [PubMed] [Google Scholar]
- 39.Carpenter L, Mitchell CJ, Xu ZZ, Poronnik P, Both GW, Biden TJ: PKCα is activated but not required during glucose-induced insulin secretion from rat pancreatic islets. Diabetes 2004; 53: 53– 60 [DOI] [PubMed] [Google Scholar]
- 40.Henquin JC, Nenquin M, Stiernet P, Ahren B: In vivo and in vitro glucose-induced biphasic insulin secretion in the mouse: pattern and role of cytoplasmic Ca2+ and amplification signals in β-cells. Diabetes 2006; 55: 441– 451 [DOI] [PubMed] [Google Scholar]
- 41.Corkey BE, Glennon MC, Chen KS, Deeney JT, Matschinsky FM, Prentki M: A role for malonyl-CoA in glucose-stimulated insulin secretion from clonal pancreatic β-cells. J Biol Chem 1989; 264: 21608– 21612 [PubMed] [Google Scholar]
- 42.Roduit R, Nolan C, Alarcon C, Moore P, Barbeau A, Delghingaro-Augusto V, Przybykowski E, Morin J, Masse F, Massie B, Ruderman N, Rhodes C, Poitout V, Prentki M: A role for the malonyl-CoA/long-chain acyl-CoA pathway of lipid signaling in the regulation of insulin secretion in response to both fuel and nonfuel stimuli. Diabetes 2004; 53: 1007– 1019 [DOI] [PubMed] [Google Scholar]
- 43.Nolan CJ, Prentki M: The islet beta-cell: fuel responsive and vulnerable. Trends Endocrinol Metab 2008; 19: 285– 291 [DOI] [PubMed] [Google Scholar]
- 44.Prentki M, Madiraju SR: Glycerolipid metabolism and signaling in health and disease. Endocr Rev 2008; 29: 647– 676 [DOI] [PubMed] [Google Scholar]
- 45.Fex M, Mulder H: Lipases in the pancreatic β-cell: implications for insulin secretion. Biochem Soc Trans 2008; 36: 885– 890 [DOI] [PubMed] [Google Scholar]
- 46.Fex M, Haemmerle G, Wierup N, Dekker-Nitert M, Rehn M, Ristow M, Zechner R, Sundler F, Holm C, Eliasson L, Mulder H: A beta cell-specific knockout of hormone-sensitive lipase in mice results in hyperglycaemia and disruption of exocytosis. Diabetologia 2009; 52: 271– 280 [DOI] [PubMed] [Google Scholar]
- 47.Fex M, Olofsson CS, Fransson U, Bacos K, Lindvall H, Sorhede-Winzell M, Rorsman P, Holm C, Mulder H: Hormone-sensitive lipase deficiency in mouse islets abolishes neutral cholesterol ester hydrolase activity but leaves lipolysis, acylglycerides, fat oxidation, and insulin secretion intact. Endocrinology 2004; 145: 3746– 3753 [DOI] [PubMed] [Google Scholar]
- 48.Yaney GC, Civelek VN, Richard AM, Dillon JS, Deeney JT, Hamilton JA, Korchak HM, Tornheim K, Corkey BE, Boyd AE, 3rd: Glucagon-like peptide 1 stimulates lipolysis in clonal pancreatic β-cells (HIT). Diabetes 2001; 50: 56– 62 [DOI] [PubMed] [Google Scholar]
- 49.Holm C, Osterlund T, Laurell H, Contreras JA: Molecular mechanisms regulating hormone-sensitive lipase and lipolysis. Annu Rev Nutr 2000; 20: 365– 393 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.