Abstract
Pneumatosis cystoides intestinalis (PCI) is a relatively rare condition characterized by intraluminal gas in the gastrointestinal tract. Several chemotherapeutic agents have been reported to be associated with PCI, although fluorouracil-related PCI is extremely rare. We report a case of a 76-year old man who received adjuvant chemotherapy for rectal cancer with fluorouracil (FU) and leucovorin (LV). After 1 cycle of the treatment, he presented with diarrhea and abdominal pain. Abdominal radiogram revealed the presence of free air under the diaphragm and intramural gas in the intestine. Laparotomy was performed, showing a suspected diagnosis of perforation in the gastrointestinal tract. Intraoperative findings revealed pneumatosis of the intestine without evidence of perforation. He was treated supportively and his symptoms improved. In conclusion, we should consider the possibility of PCI occurring in patients with malignancies during chemotherapy treatment.
Keywords: Pneumatosis cystoides intestinalis, Chemotherapy, Fluorouracil, Colorectal cancer
INTRODUCTION
Fluorouracil (FU) is one of the most commonly used chemotherapeutic agents in clinical oncology regimens. With regard to colorectal cancer, treatment involving FU with leucovorin (LV) can improve the survival, tumor response and quality of life[1] of patients. We report a case of pneumatosis cystoides intestinalis (PCI) in a patient who received adjuvant chemotherapy with 5-FU and l-LV[2]. To our knowledge, FU-related or FU-induced PCI has not been reported previously. This case will add to the reported series of patients with FU-induced small bowel toxicity[3,4] and chemotherapy-related PCI[5–9].
CASE REPORT
A 76-year-old male underwent anterior resection for stage III rectal cancer. He received an adjuvant chemotherapy protocol comprising intravenous bolus injection of 600 mg/m2 5-FU at 1 h after the initiation of 2 h-long 250 mg/m2 l-LV infusion, once a week for 6 wk, followed by 2 wk of rest[2]. After 1 cycle of this treatment, the patient presented with diarrhea and abdominal pain. Although his abdomen was distended, he did not exhibit any peritoneal signs. He was afebrile and had no neutropenia. His stool culture was negative. An abdominal radiogram revealed the presence of free air under the diaphragm and intramural gas in the entire intestine (Figure 1). Abdominal computed tomography (CT) revealed the presence of free air in the intestinal wall, retroperitoneal space (Figure 2A), and falciform ligament (Figure 2B). Since bowel perforation was strongly suspected, an emergency operation was performed. Laparotomy revealed pneumatosis of the intestine (Figure 3) and colon, and pneumoretroperitoneum without evidence of perforation. Therefore, gastrostomy was performed to reduce the pressure in the bowel. PCI was disappeared within 2 wk after parenteral nutrition, antibiotic treatment and oxygen therapy. Enema showed no incidence of anastomotic stenosis and he administered oral uracil-ftorafur, and no recurrence of PCI was observed during the 1-year follow-up.
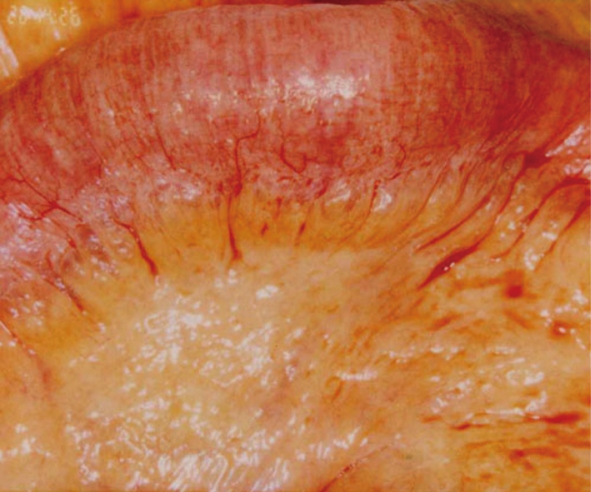
Figure 1.
Abdominal radiogram showing intraluminal gases in the entire small intestine and free air under the diaphragm.
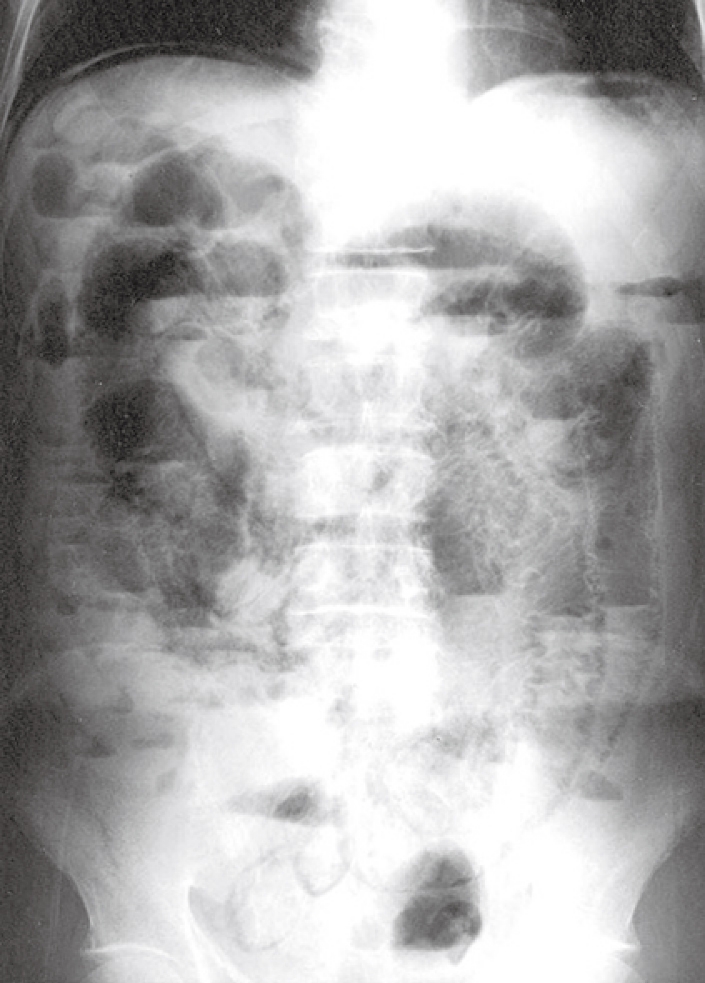
Figure 2.
Abdominal CT scan showing excessive intraluminal gases in the entire small intestine and free air in the retroperitoneal space (A), and free air in the falciform ligament (B).
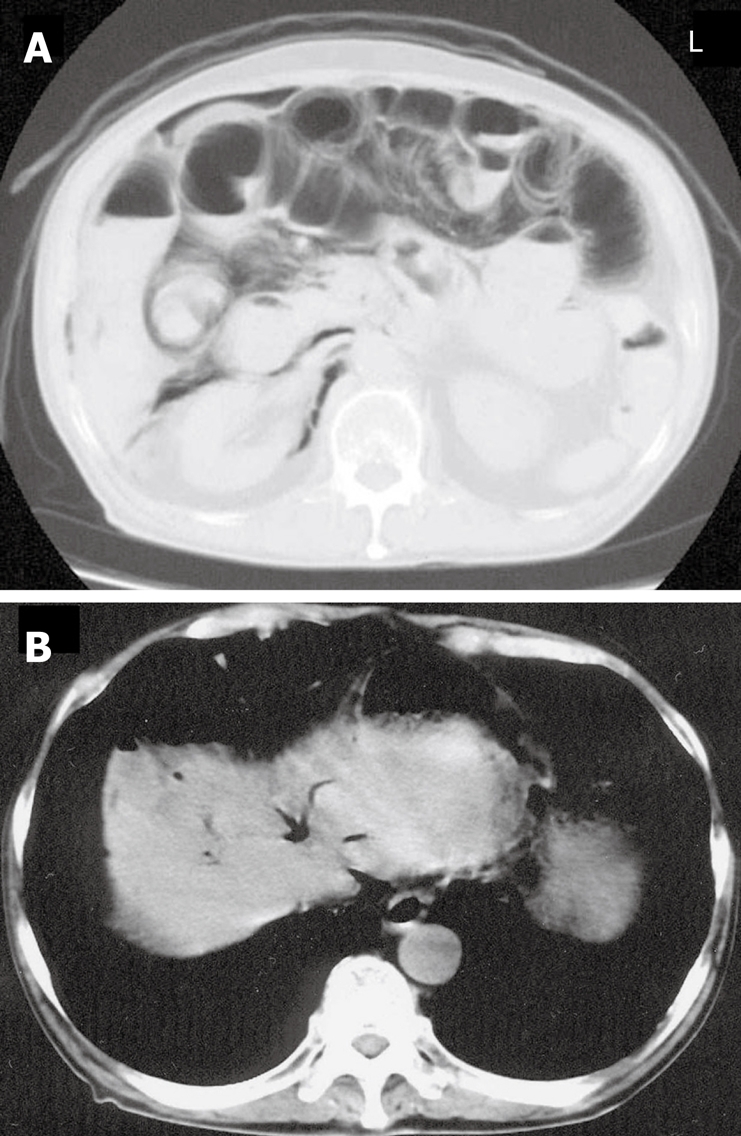
Figure 3.
Expanded intraluminal air spaces in the small intestine and mesenterium during intra-operation.
DISCUSSION
PCI is relatively rare condition characterized by multiple intraluminal gases existing in any part of the gastrointestinal tract. The mechanism and etiology of PCI are not fully understood. According to most hypotheses, mechanical and bacterial factors are the predominant causes for PCI[10–12]. However, in this present case, no mechanical or bacterial factors, including bowel ischemia, bowel obstruction[13,14], inflammatory bowel disease and infectious colitis, for the gas production in the intestinal wall were observed.
Several chemotherapeutic agents have been reported to be associated with PCI, including cyclophosphamide, cytarabine, vincristine, doxorubicin, daunorubicin, etoposide, docetaxel, irinotecan and cisplatin[5–9]. Although fluorouracil-related PCI has not been previously described, the cytotoxic effect of chemotherapy on the epithelial bowel can also play a role in the pathogenesis of PCI[7]. Because the intestinal mucosa is highly proliferative, mucosal damage occurs easily during chemotherapy[6]. Moreover, the chemotherapeutic agent might interfere with the mucosal integrity of the intestinal tract, resulting in extensive intramural air[8]. Tamura et al[15] reported that PCI following chemotherapy might be due to depletion of submucosal lymphoid tissue or leukemic infiltrates, such as denuded Peyer’s patches producing mucosal defects, thereby permitting entry of gas into the bowel wall. It was reported that chemotherapy-related PCI occurs due to immunosuppressive treatment for hematological malignancies[5,6]. Neutropenia is an important factor for the development of PCI[5–9]. However, the current patient did not suffer from neutropenia before or when PCI was diagnosed.
Several studies have reported severe erosion and superficial ulceration in the ileum after chemotherapy comprising 5-FU and LV in colon cancer patients[3,4]. The mechanisms are thought to be multifactorial, including alteration in the local mucosal blood flow and thrombogenic and vasospastic effects of 5-FU on the vascular epithelium[5]. The mechanism underlying 5-FU-induced PCI is thought to be multifactorial, including bowel toxicity caused by 5-FU itself.
In conclusion, although PCI is a rare complication of chemotherapy, the possibility of PCI occurring in patients undergoing chemotherapy should be kept in mind.
Acknowledgments
The written consent was obtained from the patient for publication of this case report.
Peer reviewer: Damian Casadesus Rodriguez, MD, PhD, Calixto Garcia University Hospital, J and University, Vedado, Havana City, Cuba
S- Editor Li DL L- Editor Wang XL E- Editor Liu Y
References
- 1.Poon MA, O'Connell MJ, Wieand HS, Krook JE, Gerstner JB, Tschetter LK, Levitt R, Kardinal CG, Mailliard JA. Biochemical modulation of fluorouracil with leucovorin: confirmatory evidence of improved therapeutic efficacy in advanced colorectal cancer. J Clin Oncol. 1991;9:1967–1972. doi: 10.1200/JCO.1991.9.11.1967. [DOI] [PubMed] [Google Scholar]
- 2.Yoshino M, Ota K, Kurihara M, Akazawa S, Tominaga T, Sasaki T, Konishi T, Kodaira S, Kumai K, Sugano K. [Late phase II trial of high-dose l-leucovorin and 5-fluorouracil in advanced colorectal carcinoma. l-Leucovorin and 5-FU Study Group (Japan Eastern Group)] Gan To Kagaku Ryoho. 1995;22:785–792. [PubMed] [Google Scholar]
- 3.Fata F, Ron IG, Kemeny N, O'Reilly E, Klimstra D, Kelsen DP. 5-fluorouracil-induced small bowel toxicity in patients with colorectal carcinoma. Cancer. 1999;86:1129–1134. doi: 10.1002/(sici)1097-0142(19991001)86:7<1129::aid-cncr5>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 4.Bucaloiu ID, Dubagunta S, Pachipala KK, Kamal N, Fata F. Small-cell cancers, and an unusual reaction to chemotherapy: Case 4. Fluorouracil-related small bowel vasculitis. J Clin Oncol. 2003;21:2442–2443. doi: 10.1200/JCO.2003.11.055. [DOI] [PubMed] [Google Scholar]
- 5.Galm O, Fabry U, Adam G, Osieka R. Pneumatosis intestinalis following cytotoxic or immunosuppressive treatment. Digestion. 2001;64:128–132. doi: 10.1159/000048852. [DOI] [PubMed] [Google Scholar]
- 6.Hashimoto S, Saitoh H, Wada K, Kobayashi T, Furushima H, Kawai H, Shinbo T, Funakoshi K, Takahashi H, Shibata A. Pneumatosis cystoides intestinalis after chemotherapy for hematological malignancies: report of 4 cases. Intern Med. 1995;34:212–215. doi: 10.2169/internalmedicine.34.212. [DOI] [PubMed] [Google Scholar]
- 7.Candelaria M, Bourlon-Cuellar R, Zubieta JL, Noel-Ettiene LM, Sanchez-Sanchez JM. Gastrointestinal pneumatosis after docetaxel chemotherapy. J Clin Gastroenterol. 2002;34:444–445. doi: 10.1097/00004836-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Shih IL, Lu YS, Wang HP, Liu KL. Pneumatosis coli after etoposide chemotherapy for breast cancer. J Clin Oncol. 2007;25:1623–1625. doi: 10.1200/JCO.2006.10.5742. [DOI] [PubMed] [Google Scholar]
- 9.Kung D, Ruan DT, Chan RK, Ericsson ML, Saund MS. Pneumatosis intestinalis and portal venous gas without bowel ischemia in a patient treated with irinotecan and cisplatin. Dig Dis Sci. 2008;53:217–219. doi: 10.1007/s10620-007-9846-9. [DOI] [PubMed] [Google Scholar]
- 10.Heng Y, Schuffler MD, Haggitt RC, Rohrmann CA. Pneumatosis intestinalis: a review. Am J Gastroenterol. 1995;90:1747–1758. [PubMed] [Google Scholar]
- 11.Shindelman LE, Geller SA, Wisch N, Bauer JJ. Pneumatosis cystoides intestinalis: a complication of systemic chemotherapy. Am J Gastroenterol. 1981;75:270–274. [PubMed] [Google Scholar]
- 12.Rogy MA, Mirza DF, Kovats E, Rauhs R. Pneumatosis cystoides intestinalis (PCI) Int J Colorectal Dis. 1990;5:120–124. doi: 10.1007/BF00298485. [DOI] [PubMed] [Google Scholar]
- 13.Horiuchi A, Akamatsu T, Mukawa K, Ochi Y, Arakura N, Kiyosawa K. Case report: Pneumatosis cystoides intestinalis associated with post-surgical bowel anastomosis: a report of three cases and review of the Japanese literature. J Gastroenterol Hepatol. 1998;13:534–537. doi: 10.1111/j.1440-1746.1998.tb00682.x. [DOI] [PubMed] [Google Scholar]
- 14.Knechtle SJ, Davidoff AM, Rice RP. Pneumatosis intestinalis. Surgical management and clinical outcome. Ann Surg. 1990;212:160–165. doi: 10.1097/00000658-199008000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tamura N, Kojo H, Miyoshi Y, Fukumoto S, Hirayama C. Pneumatosis cystoides intestinalis: Report of 3 cases with special reference to its non-surgical treatment. Z Gastroenterol. 1980;18:617–624. [PubMed] [Google Scholar]