Abstract
Acute humoral rejection (AHR) is uncommon after ABO-compatible liver transplantation. Herein, we report two cases of AHR treated with plasmapheresis and rituximab in two ABO-compatible liver-transplant patients with preformed anti-human leukocyte antigen donor-specific antibodies. Patient 1 experienced a biopsy-proven AHR at day 10 post-transplant. She was treated by steroid pulses, and OKT3. Because of persisting signs of biopsy-proven AHR at day 26, she was treated by plasmapheresis and rituximab. Liver enzyme levels did not improve, and she died on day 41. Patient 2 experienced a biopsy-proven AHR on day 10 post-transplant. She was treated by steroid pulses, plasmapheresis, and rituximab. Liver enzymes returned to within normal range 18 d after diagnosis. Liver biopsies, at 3 and 9 mo post-transplant, showed complete resolution of AHR. We conclude that plasmapheresis should be started as soon as AHR is diagnosed, and be associated with a B-cell depleting agent. Rituximab may be considered as a first-line therapy.
Keywords: Acute humoral rejection, Liver transplantation, Donor-specific antibodies, Rituximab, Plasmapheresis
INTRODUCTION
Acute humoral rejection (AHR) is well described in ABO-incompatible orthotopic liver transplant (OLT) patients; however, its occurrence in ABO-compatible OLTs is still an uncommon phenomenon. Acute humoral or antibody-mediated rejection in ABO-identical transplants is usually related to the presence of preformed or acquired anti-human leukocyte antigen (HLA) donor-specific antibodies (DSA)[1]. The diagnosis of AHR relies on the presence of DSA, C4d deposition, tissue pathology, and evidence of organ dysfunction[2]. Although the liver has long been regarded as resistant to antibody-mediated rejection, and despite conflicting published data, it is now thought that preformed DSA and a positive cross-match in ABO-compatible OLTs is associated with rejection and graft loss[3–6]. Recently, using a modern multiple-bead assay, i.e. Luminex, Castillo-Rama et al[7] have shown that Luminex-detected antibodies, as well as positive complement-dependent cytotoxicity T crossmatches, were associated with shorter graft survival within the first year post-transplant. In addition, they observed a correlation between the presence of preformed Luminex-detected class II or Luminex I and II antibodies and allograft rejection[7]. The treatment of these anti-HLA-mediated acute humoral rejections is still not well established. Herein, we report on two ABO-compatible liver-transplant patients with AHR, caused by specific anti-donor HLA antibodies (Table 1), who were treated with plasmapheresis and rituximab.
Table 1.
Immunological data regarding donors and recipients
|
HLA typing |
CDC cross-match pre-OLT |
DSA |
|||
| Donor | Recipient | Pre-OLT | At the time of AR | ||
| Case 1 | A2 A3 | A3 A36 | Positive on T and B cells | Anti-A2 | Anti-A2 |
| B35 B44 | B7 B35 | Anti-DR7 | Anti-DR7 | ||
| DR7 DR11 | DR15 - | Anti-B17 | |||
| Case 2 | A2 A24 | A3 A29 | Positive on T and B cells | Anti-A2 | Anti-A2 |
| B27 B38 | B7 B60 | Anti-A24 | Anti-A24 | ||
| DR4 DR11 | DR7 DR13 | Anti-B27 | Anti-B27 | ||
| Anti-DR4 | |||||
HLA: Human leukocyte antigen; CDC: Complement-dependent cytotoxicity; OLT: Orthotopic liver transplantation; DSA: Donor-specific alloantibody; AR: Acute rejection.
CASE REPORT
Case 1
A 49-year-old woman, who was ABO compatible, underwent 4 antigen mismatch orthotopic liver transplantation in July 2005 because of end-stage liver disease related to hepatitis C virus infection with hepatopulmonary syndrome. Her Child--Pugh stage was C10. Anti-viral therapy had failed to clear HCV before transplantation; and her HCV RNA concentration was 5.9 log copies/mL at transplantation. On the day of transplantation, her panel-reactive antibody rate (PRA) was 30% and she had circulating DSA directed against class II HLA antigens (anti-DR7, detected by Luminex). At the time of transplantation, crossmatches were positive for both T and B cells. The immediate postoperative period was marked by the occurrence of acute respiratory-distress syndrome, which required mechanical ventilation, and acute renal failure, which required continuous veno-venous haemodiafiltration. The initial immunosuppressive therapy was based on induction therapy of anti-thymocyte globulins (1.25 mg/kg on days 1, 3, 5 and 6; Thymoglobulin, Genzyme), plus tacrolimus monotherapy, which was introduced on day 1 at a targeted trough level of between 10 and 15 ng/mL. Liver enzyme levels improved until day 6, but then gamma glutamyl transpeptidase (γGT), alkaline phosphate (AP), and total bilirubin levels increased again, while transaminases remained within the normal ranges (Figure 1). By day 10, γGT, AP, total bilirubin, and direct bilirubin levels were, 251 IU/L, 808 IU/L, 258 μmol/L, and 136 μmol/L, respectively. Biliary tract and vascular complications were ruled out by abdominal ultrasonography and a liver CT scan. A Doppler ultrasound confirmed good blood flow in the hepatic artery, portal vein, and hepatic veins. A liver biopsy performed on day 10 revealed acute rejection with a Banff activity index of 7, mixed inflammatory cells in the portal triad, and significant cholangitis and endothelitis. Unfortunately, immunostaining for C4d was not performed. Retrospective immunostaining of liver biopsy for the presence of T and B lymphocytes showed a high proportion of B cells, i.e. 60% of total cells. Screening for anti-HLA antibodies confirmed the presence of anti-class I (anti-A2) and anti-class II (anti-DR7) HLA antibodies directed against the donor. Because of this, the patient was treated with steroid pulses (10 mg/kg per day for 3 d, and then gradually tapered), OKT3 (10 mg/d for 10 d), plus mycophenolate mofetil was introduced at a daily dose of 2 g. In the absence of any improvement in liver enzyme levels, she underwent a second liver biopsy 16 d after the first, on day 26 post-transplant. This showed the presence of inflammatory infiltration by lymphocytes, histiocytes and plasmocytes, persistent cholangitis, venulitis, hepatocanalicular cholestasis, biliary thrombi, and hepatocyte necrosis. Retrospective immunostaining of the liver biopsy for the presence of T and B lymphocytes showed a high proportion of B cells with 30% of B cells. At that time, we decided to treat the humoral part component. She was treated with plasmapheresis (5 sessions using fresh frozen plasma or 50% fresh frozen plasma and 50% albumin) and two rituximab infusions (375 mg/m2 per week for 2 wk). Unfortunately, her liver enzyme levels did not improve. She required liver support that utilized four sessions of molecular adsorbents recirculating system (MARS). Her acute respiratory distress syndrome did not improve within this postoperative period. She experienced pulmonary infections and died on day 41, i.e. 4 d after the second rituximab infusion. Before rituximab infusion, her circulating CD4-, CD8-, and CD19-positive cell counts were, respectively, 47, 49 and 85/mm3.
Figure 1.
Postoperative clinical course of patient 1. Tac: Tacrolimus; MMF: Mycophenolate mofetil; RATG: Rabbit anti-thymocyte globulins; MARS: Molecular adsorbents recirculating system; LB: Liver biopsy; PP: Plasmapheresis; R: Rituximab; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; GGT: Gamma glutamyl transpeptidase.
Case 2
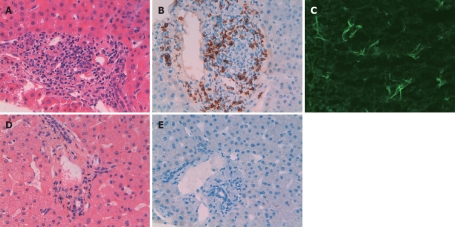
A 39-year-old woman underwent six antigen mismatch, ABO-compatible orthotopic liver transplantation in January 2008 because of end-stage liver disease related to alcohol with hepatopulmonary and hepatorenal syndromes. Her Child--Pugh stage was C10. On the day of transplantation, her PRA was 44% and she had circulating DSA directed against both class I (anti-A2, anti-A24, anti-B27) and class II (anti-DR4) HLA antigens, which were detected by Luminex. At the time of transplantation, crossmatches were positive for T and B cells. Surgery was uneventful, and the immediate postoperative course was unremarkable with a regular decrease in liver test parameters. The initial immunosuppressive therapy was based on tacrolimus (targeting a trough level of between 10 and 15 ng/mL), mycophenolate mofetil (1 g bid), and steroids (10 mg/kg before transplantation, 5 mg/kg on day 1, 2.5 mg/kg on day 2, and then 1 mg/kg). By day 4, because of significant renal function impairment (serum creatinine level rose from 130 to 280 μmol/L) caused by the high tacrolimus trough level (21 ng/mL), tacrolimus was discontinued for 2 d. The patient then received one infusion of anti-thymocyte globulins (1.25 mg/kg; Thymoglobulin, Genzyme). Liver enzyme levels improved until day 5 but, on day 6, γGT, AP, and total bilirubin levels increased significantly (Figure 2). Biliary tract complications were ruled out by abdominal ultrasonography and magnetic resonance imaging. Doppler ultrasound confirmed good blood flow in the hepatic artery, portal vein, and hepatic veins. A liver biopsy performed on day 10 revealed acute rejection, with a Banff activity index of 7, diffuse cholangitis and endothelitis, periportal edema, inflammatory infiltration by lymphocytes, histiocytes and neutrophils (Figure 3A). Immunostaining for C4d was positive (Figure 3B). Immunostaining of liver biopsy for the presence of T and B lymphocytes showed a high proportion of T cells. B cells represented 30% of total cells (Figure 3C) Consequently, she received three pulses of methylprednisolone (10 mg/kg per day), plus four infusions of rituximab (375 mg/m2 per week for 4 wk). In addition, six plasmapheresis sessions using fresh frozen plasma were realized. Her liver enzyme levels improved rapidly and were within normal range 18 d after AHR diagnosis. At 3 mo post-transplant, she underwent a second liver biopsy, which showed complete resolution of the acute rejection episode (Figure 3D). Immunostaining of liver biopsy for the presence of T and B lymphocytes showed no T and B cells (Figure 3E). All previous features of acute rejection had disappeared. At 12 mo post-transplant, her liver enzyme levels were still within the normal range, DSA directed against class I HLA antigens were still detected, while the DSA directed against the class II HLA antigen was not detected anymore. A third liver biopsy was performed and was considered normal. During the 12 mo post-transplant, she did not present with any infection episodes. Her circulating CD4-, CD8-, and CD19-positive cell counts, which were 364, 165 and 45, respectively, before the first rituximab infusion, became 980, 527 and 0/mm3 by month 3 and 673, 374 and 0/mm3 by 12 mo post-transplant.
Figure 2.
Postoperative clinical course of patient 2.
Figure 3.
Liver biopsies performed in patient 2. A: Liver biopsy performed on day 10. Acute rejection with mixed inflammatory cells in the portal triad, significant cholangitis and endothelitis. Banff activity index of 7 (HE, × 400); B: Immunostaining with L26 antibody (anti-CD20) showed moderate proportion of B cells (× 400); C: Liver biopsy performed on day 10: Immunostaining for C4d in liver biopsy (× 400); D: Liver biopsy performed at 3 mo post-transplant showed complete resolution of acute rejection (HE, × 400); E: Immunostaining with L26 antibody (anti-CD20) showed no B cell infiltration (× 400).
DISCUSSION
Anti-HLA antibody-induced acute humoral rejection is uncommon after ABO-compatible liver transplantation. Herein, we report two cases of acute humoral rejection that occurred within the first week after an ABO-compatible liver transplantation in two patients with preformed donor-specific anti-HLA antibodies. In both cases, an acute rejection episode occurred very early after transplantation, and induced significant cholestasis, while transaminases were only moderately elevated. Liver biopsies revealed acute rejection, the presence of inflammatory infiltration and, more specifically, cholangitis, endothelitis, and periportal edema. Immunostaining for C4d was found to be positive, and immunostaining of liver biopsies for the presence of T and B lymphocytes showed a relative high proportion of B cells. To the best of our knowledge, our second case report is the first to show that early treatment of AHR with plasmapheresis and rituximab without using intravenous hyperimmune globulins (IVIg) is effective in this setting, especially in a patient with four different DSAs.
Whatever the transplanted organ may be, until recently, the treatment of AHR has been based on plasmapheresis, immunoadsorption, IVIg, and tacrolimus, mycophenolate mofetil, with or without T-cell depleting agents[8–10]. Because of B-cell involvement in humoral rejection, the use of monoclonal anti-CD20 antibodies (rituximab) has been used in this setting. For ABO-incompatible kidney and liver transplantation, as well as historical and/or current positive crossmatch pre-transplantation highly sensitized patients, and in desensitization protocols in kidney transplantation, rituximab has been successfully used in association with splenectomy and plasmapheresis[11–15]. In kidney transplant patients, Becker et al[16] have shown that vascular rejection with a possible humoral component responds to a single dose of rituximab therapy when associated with plasmapheresis and steroid pulses, with or without anti-thymocyte globulins. More recently, we found that, despite a high rate of infection, the association of plasmapheresis and rituximab was efficient in treating acute humoral kidney rejection[17]. These interesting results obtained in kidney transplant patients prompted us to use the same strategy in liver transplant patients who were experiencing acute humoral rejection. Previously, Watson et al[6] treated a liver transplant patient with preformed anti-HLA antibodies and who experienced an early acute humoral rejection with IVIg, plasmapheresis, and one infusion of rituximab. In Watson et al[6] plasmapheresis and rituximab therapies were started late after AHR diagnosis, i.e. on post-transplant day 34 for rituximab, and post-transplant day 70 for plasmapheresis. This is similar to our first case report, where we treated the cellular component before the humoral component. Unfortunately, this was not effective in treating the humoral acute rejection.
In contrast, starting plasmapheresis and medications that target B cells as soon as AHR is diagnosed seems to be more effective. In our second case report, plasmapheresis and rituximab therapy were started as soon as AHR was diagnosed, i.e. on day 11 post-transplant. Similarly, Rostron et al[18] had previously reported a case of severe AHR in an ABO compatible liver transplant patient successfully treated with plasmapheresis, IVIg and conversion from azathioprine to mycophenolate mofetil. In the latter case, plasmapheresis was started at day 7 post-transplant. In another study on a combined kidney-liver transplant patient who experienced both cellular and humoral rejection, early plasmapheresis associated with steroid pulses, anti-thymocyte globulins, and IVIg effectively treated both rejections[19]. Finally, Wilson et al[20] reported a late AHR in an ABO-compatible liver transplant patient that was successfully treated with plasmapheresis, one rituximab infusion, and anti-thymocyte globulins. However, in the latter case, we wonder whether it was a late AHR or a cellular rejection that occurred in a patient with a chronic humoral rejection. Indeed, it is unknown how many anti-HLA antibodies were present in this patient. Positive immunostaining for C4d may be related to long-term silent chronic humoral rejection. In addition, in the Wilson et al case report, the acute rejection that occurred very late after transplantation, which is very uncommon, may be a steroid-resistant acute cellular rejection, especially since liver enzyme levels decreased after anti-thymocyte globulin therapy.
In summary, plasmapheresis should be started as soon as AHR is diagnosed in order to remove circulating antibodies. It should be associated with either IVIg or rituximab, both of which can be effective in this setting. However, because of rituximab’s capacity to deplete B-cells, and the good results obtained in ABO-incompatible liver transplant patients, rituximab could be the preferred first-line therapy. Further controlled studies to compare rituximab and IVIg are needed.
Peer reviewers: Hanna Gregorek, Assistant Professor, PhD, Department of Microbiology and Clinical Immunology, The Children’s Memorial Health Institute, Al. Dzieci Polskich 20, Warsaw 04-730, Poland; Yasuhiko Sugawara, MD, Artificial Organ and Transplantation Division, Department of Surgery, Graduate School of Medicine University of Tokyo, Tokyo, Japan
S- Editor Tian L L- Editor O'Neill M E- Editor Lin YP
References
- 1.Terasaki PI, Cai J. Humoral theory of transplantation: further evidence. Curr Opin Immunol. 2005;17:541–545. doi: 10.1016/j.coi.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 2.Takemoto SK, Zeevi A, Feng S, Colvin RB, Jordan S, Kobashigawa J, Kupiec-Weglinski J, Matas A, Montgomery RA, Nickerson P, et al. National conference to assess antibody-mediated rejection in solid organ transplantation. Am J Transplant. 2004;4:1033–1041. doi: 10.1111/j.1600-6143.2004.00500.x. [DOI] [PubMed] [Google Scholar]
- 3.Takaya S, Iwaki Y, Starzl TE. Liver transplantation in positive cytotoxic crossmatch cases using FK506, high-dose steroids, and prostaglandin E1. Transplantation. 1992;54:927–929. doi: 10.1097/00007890-199211000-00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ratner LE, Phelan D, Brunt EM, Mohanakumar T, Hanto DW. Probable antibody-mediated failure of two sequential ABO-compatible hepatic allografts in a single recipient. Transplantation. 1993;55:814–819. doi: 10.1097/00007890-199304000-00025. [DOI] [PubMed] [Google Scholar]
- 5.Muro M, Marin L, Miras M, Moya-Quiles R, Minguela A, Sánchez-Bueno F, Bermejo J, Robles R, Ramírez P, García-Alonso A, et al. Liver recipients harbouring anti-donor preformed lymphocytotoxic antibodies exhibit a poor allograft survival at the first year after transplantation: experience of one centre. Transpl Immunol. 2005;14:91–97. doi: 10.1016/j.trim.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 6.Watson R, Kozlowski T, Nickeleit V, Woosley JT, Schmitz JL, Zacks SL, Fair JH, Gerber DA, Andreoni KA. Isolated donor specific alloantibody-mediated rejection after ABO compatible liver transplantation. Am J Transplant. 2006;6:3022–3029. doi: 10.1111/j.1600-6143.2006.01554.x. [DOI] [PubMed] [Google Scholar]
- 7.Castillo-Rama M, Castro MJ, Bernardo I, Meneu-Diaz JC, Elola-Olaso AM, Calleja-Antolin SM, Romo E, Morales P, Moreno E, Paz-Artal E. Preformed antibodies detected by cytotoxic assay or multibead array decrease liver allograft survival: role of human leukocyte antigen compatibility. Liver Transpl. 2008;14:554–562. doi: 10.1002/lt.21408. [DOI] [PubMed] [Google Scholar]
- 8.Rocha PN, Butterly DW, Greenberg A, Reddan DN, Tuttle-Newhall J, Collins BH, Kuo PC, Reinsmoen N, Fields T, Howell DN, et al. Beneficial effect of plasmapheresis and intravenous immunoglobulin on renal allograft survival of patients with acute humoral rejection. Transplantation. 2003;75:1490–1495. doi: 10.1097/01.TP.0000060252.57111.AC. [DOI] [PubMed] [Google Scholar]
- 9.White NB, Greenstein SM, Cantafio AW, Schechner R, Glicklich D, McDonough P, Pullman J, Mohandas K, Boctor F, Uehlinger J, et al. Successful rescue therapy with plasmapheresis and intravenous immunoglobulin for acute humoral renal transplant rejection. Transplantation. 2004;78:772–774. doi: 10.1097/01.tp.0000128194.55934.48. [DOI] [PubMed] [Google Scholar]
- 10.Montgomery RA, Zachary AA, Racusen LC, Leffell MS, King KE, Burdick J, Maley WR, Ratner LE. Plasmapheresis and intravenous immune globulin provides effective rescue therapy for refractory humoral rejection and allows kidneys to be successfully transplanted into cross-match-positive recipients. Transplantation. 2000;70:887–895. doi: 10.1097/00007890-200009270-00006. [DOI] [PubMed] [Google Scholar]
- 11.Boberg KM, Foss A, Midtvedt K, Schrumpf E. ABO-incompatible deceased donor liver transplantation with the use of antigen-specific immunoadsorption and anti-CD20 monoclonal antibody. Clin Transplant. 2006;20:265–268. doi: 10.1111/j.1399-0012.2005.00470.x. [DOI] [PubMed] [Google Scholar]
- 12.Kawagishi N, Takeda I, Miyagi S, Satoh K, Akamatsu Y, Sekiguchi S, Fujimori K, Sato T, Satomi S. Management of anti-allogeneic antibody elimination by apheresis in living donor liver transplantation. Ther Apher Dial. 2007;11:319–324. doi: 10.1111/j.1744-9987.2007.00506.x. [DOI] [PubMed] [Google Scholar]
- 13.Egawa H, Ohmori K, Haga H, Tsuji H, Yurugi K, Miyagawa-Hayashino A, Oike F, Fukuda A, Yoshizawa J, Takada Y, et al. B-cell surface marker analysis for improvement of rituximab prophylaxis in ABO-incompatible adult living donor liver transplantation. Liver Transpl. 2007;13:579–588. doi: 10.1002/lt.21092. [DOI] [PubMed] [Google Scholar]
- 14.Warren DS, Zachary AA, Sonnenday CJ, King KE, Cooper M, Ratner LE, Shirey RS, Haas M, Leffell MS, Montgomery RA. Successful renal transplantation across simultaneous ABO incompatible and positive crossmatch barriers. Am J Transplant. 2004;4:561–568. doi: 10.1111/j.1600-6143.2004.00364.x. [DOI] [PubMed] [Google Scholar]
- 15.Gloor J, Cosio F, Lager DJ, Stegall MD. The spectrum of antibody-mediated renal allograft injury: implications for treatment. Am J Transplant. 2008;8:1367–1373. doi: 10.1111/j.1600-6143.2008.02262.x. [DOI] [PubMed] [Google Scholar]
- 16.Becker YT, Becker BN, Pirsch JD, Sollinger HW. Rituximab as treatment for refractory kidney transplant rejection. Am J Transplant. 2004;4:996–1001. doi: 10.1111/j.1600-6143.2004.00454.x. [DOI] [PubMed] [Google Scholar]
- 17.Faguer S, Kamar N, Guilbeaud-Frugier C, Fort M, Modesto A, Mari A, Ribes D, Cointault O, Lavayssière L, Guitard J, et al. Rituximab therapy for acute humoral rejection after kidney transplantation. Transplantation. 2007;83:1277–1280. doi: 10.1097/01.tp.0000261113.30757.d1. [DOI] [PubMed] [Google Scholar]
- 18.Rostron A, Carter V, Mutunga M, Cavanagh G, O'Suilleabhain C, Burt A, Jaques B, Talbot D, Manas D. A case of acute humoral rejection in liver transplantation: successful treatment with plasmapheresis and mycophenolate mofetil. Transpl Int. 2005;18:1298–1301. doi: 10.1111/j.1432-2277.2005.00200.x. [DOI] [PubMed] [Google Scholar]
- 19.Hadaya K, Ferrari-Lacraz S, Giostra E, Majno P, Moll S, Rubbia-Brandt L, Marangon N, Venetz JP, Bolle JF, Mentha G, et al. Humoral and cellular rejection after combined liver-kidney transplantation in low immunologic risk recipients. Transpl Int. 2009;22:242–246. doi: 10.1111/j.1432-2277.2008.00775.x. [DOI] [PubMed] [Google Scholar]
- 20.Wilson CH, Agarwal K, Carter V, Burt AD, Hübscher S, Talbot D, Jaques BC, Manas DM. Late humoral rejection in a compliant ABO-compatible liver transplant recipient. Transplantation. 2006;82:988–989. doi: 10.1097/01.tp.0000229939.85412.27. [DOI] [PubMed] [Google Scholar]