Abstract
The objectives of this multisite study were to: (i) examine differences by gender and race on generic and weight- specific health-related quality of life (HRQOL) in adolescents with extreme obesity (BMI ≥ 40 kg/m2) and (ii) explore HRQOL differences based on treatment pursued (behavioral vs. bariatric surgery). Study participants included 145 obese adolescents (mean age = 15.3 years; 68% female; 46% black; mean BMI = 50.6) referred to pediatric weight management programs. Participants completed generic (PedsQL) and weight-specific (Impact of Weight on Quality of Life-Kids (IWQOL-Kids)) HRQOL measures. Generic and weight-specific measures indicated global (e.g., all domains) HRQOL impairment and significant differences by race. Physical, emotional, and social scores of the PedsQL (Ps < 0.01) and the physical comfort and body esteem scores of the IWQOL-Kids (Ps < 0.001) were significantly higher for black compared to white adolescents with extreme obesity. Extremely obese adolescents pursuing bariatric surgery reported similar HRQOL to adolescents pursuing behavioral treatment (n = 30 matched pairs). HRQOL did not differ for extremely obese adolescents based on type of treatment sought, but race/ethnicity should be considered when characterizing these youth. Although racial differences in adolescent body image/esteem have been reported, it is unknown why black adolescents with extreme obesity would report less impact of weight on their physical functioning. Overall, these data suggest that HRQOL is not homogenous in adolescents with extreme obesity.
INTRODUCTION
With the epidemic of pediatric obesity now well documented, there is an increased focus on identifying subgroups at particular risk. Grave concerns have been raised about the increase in degree of pediatric overweight (1,2), with an estimated 4% of children and adolescents meeting criteria for extreme obesity (BMI ≥ 40 kg/m2) (1). Racial disparities exist for both sexes, with the most recent obesity prevalence rates notably higher for black youth compared to whites beginning in early adolescence (3). In recent decades, the rate and prevalence of extreme obesity in pediatric populations have increased dramatically, with a fourfold increase in the number of youth with BMI levels above the 99th percentile (1). For example, the highest prevalence of extreme obesity between 1999 and 2002 was seen in Mexican-American boys (7%) and black girls (6%) (1). Unfortunately, there are few empirically supported treatments for youth with extreme obesity and as such, obese adolescents have an inordinate risk of carrying the burden of obesity into adulthood. Modest treatment improvements have been reported for behavioral weight management programs (4,5) and medications (6). However, bariatric surgery is currently being evaluated as a viable option for the extremely obese adolescent (7).
The effect of extreme obesity in adolescence is multifold, affecting individuals during both adolescence and adulthood, their families, and the larger health-care system. For example, adolescents with extreme obesity experience increased morbidity (8–14) and global impairments in daily functioning (15). The development of effective prevention and intervention models targeting youth has thus become a public health priority.
Health-related quality of life (HRQOL) has become a well-established patient-reported outcome for clinical trials in the past decade and is defined as a multidimensional construct, which encompasses an individual’s subjective evaluation of his/her physical, emotional, and social well-being (16). There is considerable literature documenting a strong and consistent relationship between pediatric obesity and impaired HRQOL across all domains of functioning (e.g., physical, social, and emotional) (15,17–22). Furthermore, there is evidence that youth experience lower HRQOL with increasing BMI (19,22). In particular, we recently reported that adolescents with extreme obesity (e.g., BMI > 40 kg/m2) may suffer from the poorest HRQOL relative to both healthy youth and youth with lesser degrees of obesity (15). Similar to adult obese populations (23,24), it is also important to note preliminary evidence suggesting that HRQOL may vary by race with black adolescents reporting better HRQOL compared to white adolescents (25, 26). Similarly, gender differences have been reported in overweight and obese children/adolescents (26) and adults with extreme obesity (24). However, little is known about HRQOL in extremely obese adolescents and whether this varies by gender and race.
Our knowledge of HRQOL in obese youth is based on studies which have used generic measures, such as the PedsQL (20) and Children’s Health Questionnaire (CHQ) (27), which are not as sensitive to the physical and psychosocial aspects of obesity. Thus, what remains poorly characterized is the impact of obesity on aspects of child and adolescent daily functioning most pertinent to the condition, such as physical limitations, peer-related teasing, and body esteem. Recently, a weight-specific HRQOL measure, the Impact of Weight on Quality of Life-Kids (IWQOL-Kids), was developed for adolescents that measures condition-specific domains of functioning, including physical comfort, body esteem, social life, and family life (26). Initial evidence suggests that the IWQOL-Kids has shown greater responsiveness to weight loss compared to the PedsQL (26). Research in adult populations suggests that weight-specific HRQOL becomes more impaired as BMI increases and as patients seek more intensive treatment options (e.g., bariatric surgery) (23,28). The objectives of this multisite study were to: (i) examine race and gender differences in generic and weight-specific HRQOL in treatment-seeking obese adolescents with extreme obesity and (ii) explore HRQOL differences based on treatment pursued (behavioral vs. bariatric surgery).
METHODS AND PROCEDURES
Participants
Participants included 145 adolescents with extreme obesity (BMI ≥ 40 kg/m2) from two pediatric centers in the Midwest and Southeast United States, each with both behavioral weight management and adolescent bariatric surgery programs. No significant differences were noted between the two sites regarding child/adolescent age (t (143) = −0.26, P = n.s.), race (χ2 (3, N = 145) = 2.6, P = n.s.), gender (χ2 (1, N = 145) = 0.66, P = n.s.), or BMI (t (143) = −0.79, P = n.s.). Participants included in this analyses were previously recruited for two larger studies of obese youth, which examined psychosocial functioning of children prior to initiation of weight management interventions. These studies had 95% (Cincinnati Children’s Hospital Medical Center) and 84% (University of Alabama at Birmingham) recruitment for patients pursuing behavioral weight management and bariatric surgery at each respective site. The behavioral weight management programs require a BMI ≥ 95th percentile for age/sex and exclude youth with genetic syndromes associated with obesity and developmental disabilities whereas the adolescent bariatric surgery programs adhere to adolescent patient selection guidelines as previously described (7). Inclusion criteria for these analyses included (i) patients 11–18 years of age (behavioral treatment) or 13–18 years of age (bariatric surgery), (ii) having no developmental disability, (iii) BMI ≥ 40 kg/m2, and (iv) willingness to comply with study procedures and provide written informed consent/assent.
Procedures
Eligible families were approached during their initial evaluation at the comprehensive pediatric weight management programs. During this clinic appointment, participants completed several questionnaires. Weight and height data, which were collected by trained health-care professionals, were used to calculate BMI (in kg/m2). Given that BMI increases with age as children mature, standardized zBMI was calculated using age- (to the nearest month) and sex-specific median, s.d., and power of the Box–Cox transformation (LMS method) based on national norms from the Centers for Disease Control (29). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. The protocol and consent forms were approved by the appropriate Institutional Review Board.
Measures
Demographic background questionnaire
Primary caregivers completed a basic background questionnaire documenting the child’s race/ethnicity, age, and gender.
PedsQL
The PedsQL is a 23-item generic HRQOL measure designed for parents of children between 2 and 18 years of age and children aged 5–18 years. For this study, the PedsQL parent report of children (aged 8–12 years) and PedsQL parent report of adolescents (aged 13–18 years) were used. Children and adolescents completed the child self-report (aged 8–12 years) and adolescent self-report (aged 13–18 years) forms, respectively. The PedsQL assesses several domains of functioning: physical (eight items), emotional (five items), social (five items), and school (five items). In addition, a psychosocial functioning scale (emotional, social, and school) and total score (physical, emotional, social, and school) were calculated. The measure uses a 5-point Likert scale (0 = never a problem to 4 = almost always a problem). The PedsQL has been found to have excellent reliability for self-reported (α = 0.68 (school subscale) – 0.88 (total score)) and parent-proxy versions (α = 0.76 (school subscale) – 0.90 (total score)). Validity has been demonstrated through known-group comparisons (e.g., chronically ill vs. healthy samples) and correlations between morbidity and PedsQL scales (20). Scores range from 0 to 100, with higher scores representing better HRQOL.
IWQOL-Kids
The IWQOL-Kids is a weight-specific HRQOL measure for adolescents, aged ≥11 years. It comprised four subscales (physical comfort, body esteem, social life, and family life), and a total score. The physical comfort scale (six items) examines the impact of weight on an individual’s physical mobility and comfort. The body esteem scale (nine items) assesses how an individual feels about themselves and their body in context of their weight. The social life scale (six items) reflects the impact of weight on how an individual is treated in their social environment and peer relations. The family life scale (six items) examines the individual’s perception of what family members may think and feel about them and their weight. The IWQOL-Kids was validated on 642 adolescents, with 362 categorized as obese based on BMI > 95th percentile). The IWQOL-Kids has been shown to have excellent internal consistency coefficients (α = 0.88 (family relations) to 0.95 (body esteem)). In addition, IWQOL-Kids scales demonstrated convergence with the PedsQL (r = 0.76) and significant differences across BMI groups (26).
Statistical and data analyses
Descriptive analyses, including means and s.d., were calculated for self-reported and parent-proxy generic HRQOL and self-report of weight-specific HRQOL. z-Tests were conducted to compare HRQOL scores between the instrument normative data of a healthy sample and youth with extreme obesity. Separate multivariate ANOVA (MANOVAs) were conducted to compare HRQOL scores between (1) males and females and (2) white and black youth, controlling for BMI (similar results were obtained when using zBMI instead of BMI). In addition, the race and gender interaction term was tested in the MANOVA examining both generic and weight-specific HRQOL. To examine differences in HRQOL by type of treatment being pursued, the bariatric sample was matched based on age, gender, and race to individuals in the behavioral treatment sample. MANOVAs were conducted to examine differences in HRQOL scores between adolescents pursuing behavioral treatment compared to those pursuing bariatric surgery, controlling for BMI (similar results were obtained when using zBMI instead of BMI) as we expected significant group differences in degree of overweight. Similar to other multivariate F values (e.g., Wilks’ Lambda, Pillai’s criterion), Hotelling’s trace was used for these analyses and is based on a comparison of the pooled ratio of effect variance to error variance. When the omnibus test (MANOVA) was significant, post hoc analyses were conducted. Significance was defined as P < 0.05. Analyses were performed using SPSS statistical software (SPSS, Chicago, IL).
RESULTS
Descriptive data and normative values
Demographic data for the multisite sample are presented in Table 1. Both parent-proxy and self-reported PedsQL scores for youth with extreme obesity were significantly impaired compared to published data on nontreatment seeking obese youth (see Table 2). Compared to another sample of treatment-seeking obese youth, self-reported physical functioning and a majority of parent-proxy scales, with the exception of school functioning were significantly elevated for youth with extreme obesity.
Table 1.
Demographic information of youth with extreme obesity (n = 145)
| N | Mean (s.d.) | % | Range | |
|---|---|---|---|---|
| Age | 15.3 (1.7) | 11–18 | ||
| Sex | ||||
| Girls | 99 | 68 | ||
| Boys | 46 | 32 | ||
| Race | ||||
| White | 76 | 52 | ||
| Black | 66 | 45 | ||
| Hispanic | 1 | 1 | ||
| Other | 2 | 1 | ||
| Anthropometrics | ||||
| BMI | 50.6 (9.6) | 40–89 | ||
| zBMI | 2.8 (.24) | 2.3–3.7 | ||
Table 2.
Generic HRQOL scale for youth with extreme obesity and comparison groups
| Youth with extreme obesity (n = 145) |
Nontreatment seeking obese youth (n = 63)a |
Treatment-seeking obese youth (n = 106)b |
||||||
|---|---|---|---|---|---|---|---|---|
| PedsQL | Mean (s.d.) | Mean (s.d.) | df | z | Mean (s.d.) | df | z | |
| Youth self-report | ||||||||
| Physical functioning | 63.4 (21.0) | 77.5 (17.9) | 206 | −4.94*** | 71.0 (18.8) | 249 | −3.00** | |
| Emotional functioning | 62.4 (23.9) | 68.6 (18.5) | 206 | −2.02* | 63.2 (20.1) | 249 | −0.29 | |
| Social functioning | 64.6 (25.8) | 72.6 (18.2) | 206 | −2.55** | 67.5 (25.0) | 248 | −0.89 | |
| School functioning | 64.3 (20.9) | 75.0 (14.5) | 204 | −4.23*** | 64.1 (20.4) | 247 | 0.08 | |
| Psychosocial functioning | 63.6 (19.3) | 72.1 (14.1) | 206 | −3.56*** | 64.9 (17.7) | 249 | −0.55 | |
| Total score | 63.6 (18.6) | 74.0 (14.2) | 206 | −4.39*** | 67.0 (16.3) | 249 | −1.53 | |
| Parent-proxy report | ||||||||
| Physical functioning | 49.0 (19.6) | 76.3 (17.6) | 205 | −9.90*** | 63.6 (24.0) | 247 | −5.11*** | |
| Emotional functioning | 55.3 (21.4) | 72.6 (17.8) | 205 | −6.03*** | 60.9 (21.7) | 247 | −2.02* | |
| Social functioning | 52.6 (22.4) | 73.5 (17.3) | 206 | −7.27*** | 67.2 (26.1) | 248 | −4.62*** | |
| School functioning | 59.3 (20.7) | 76.6 (17.0) | 203 | −6.26*** | 61.4 (21.4) | 245 | −0.77 | |
| Psychosocial functioning | 55.9 (17.4) | 73.9 (15.3) | 202 | −7.42*** | 63.1 (18.6) | 244 | −3.08*** | |
| Total score | 53.5 (16.3) | 75.0 (14.5) | 201 | −9.38*** | 63.3 (19.2) | 243 | −4.21*** | |
HRQOL, health-related quality of life.
Adapted from published data for nontreatment seeking obese youth (M age total sample= 10.4 (1.1) years; 44% male; race not reported (22)).
Adapted from published data for obese youth seeking treatment (Mage = 12.1 (3.0) years; 57% male; 26% white non-Hispanic (19)).
z-Values are significant *P < 0.05, **P < 0.01, ***P < 0.001
Differences in HRQOL by gender
No significant differences were found between males and females for age (t (143) = −0.48, P = n.s.) or race (χ2 (3, N = 145) = 2.8, P = n.s.). MANOVAs indicated significant differences between males and females with extreme obesity on the self-report PedsQL, after controlling for BMI (Hotelling’s T = 0.13, F (4, 136) = 4.4, P < 0.01). Post hoc analyses indicated that males reported higher scores on the emotional scale compared to females (t (142) = 2.2, P < 0.05; Mmales = 70.4 vs. Mfemales = 59.1). No significant differences were found between males and females on parent-proxy PedsQL scores.
Significant differences were also found between males and females on the IWQOL-Kids, after controlling for BMI (Hotelling’s T = 0.11, F (4, 138) = 3.9, P < 0.01). Specifically, males reported higher scores for the body esteem (Mmales = 64.8 vs. Mfemales = 52.1; t (143) = 2.2, P < 0.05) and family life scales (Mmales = 95.7 vs. Mfemales = 90.0; t (142) = 2.4, P < 0.05). Gender by race interactions were tested in all the HRQOL models with no significant findings.
Differences in HRQOL by race
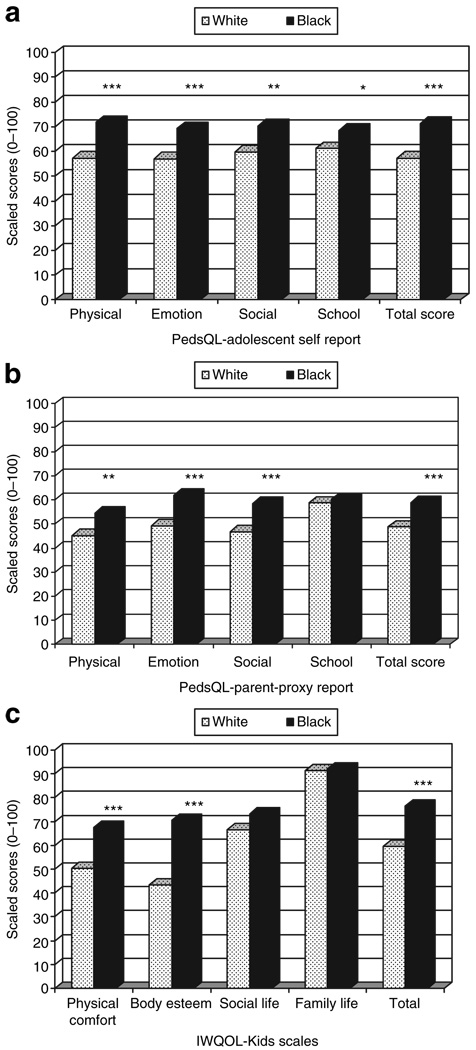
No significant differences were found between white and black youth for age (t (140) = −1.9, P = n.s.) or gender (χ2 (3, N = 145) = 2.8, P = n.s.). Controlling for BMI, MANOVAs indicated significant differences between white and black youth with extreme obesity on both the self-report (Hotelling’s T = 0.16, F (4, 133) = 5.2, P < 0.001) and parent-proxy generic PedsQL (Hotelling’s T = 0.15, F (4, 131) = 4.8, P < 0.001). Post hoc analyses revealed black youth self-reported significantly higher HRQOL scores compared to white youth on the physical (t (139) = 5.3, P < 0.0001), emotional (t (139) = 3.9, P < 0.0001), social (t (139) = 3.1, P < 0.01), school (t (137) = 2.4, P < 0.05), and total score scales (t (139) = 4.8, P < 0.0001). Similarly, with the exception of the school scale, post hoc analyses indicated that parents reported higher physical (t (139) = 3.0, P < 0.01), emotional (t (139) = 3.6, P < 0.0001), social (t (140) = 3.7, P < 0.0001), and total score scales (t (135) = 3.7, P < 0.0001) for black youth compared to white youth (see Figure 1).
Figure 1.
Differences by race on health-related quality of life: (a) self-reported PedsQL scores, (b) parent-proxy PedsQL scores, (c) Impact of Weight on Quality of Life-Kids (IWQOL-Kids) scores, *P < 0.05, **P < 0.01, and ***P < 0.001.
Similarly, MANOVAs indicated significant differences between white and black youth with extreme obesity on the IWQOL-Kids, after controlling for BMI (Hotelling’s T = 0.41, F (4, 135) = 13.8, P < 0.0001). Post hoc analyses indicated that black youth reported better weight-specific HRQOL on the physical comfort (t (140) = 5.4, P < 0.0001), body esteem (t (140) = 6.5, P < 0.0001), and total score scales (t (139) = 5.3, P < 0.0001). No significant differences were noted for the social and family life scales (see Figure 1).
Weight management treatment and HRQOL
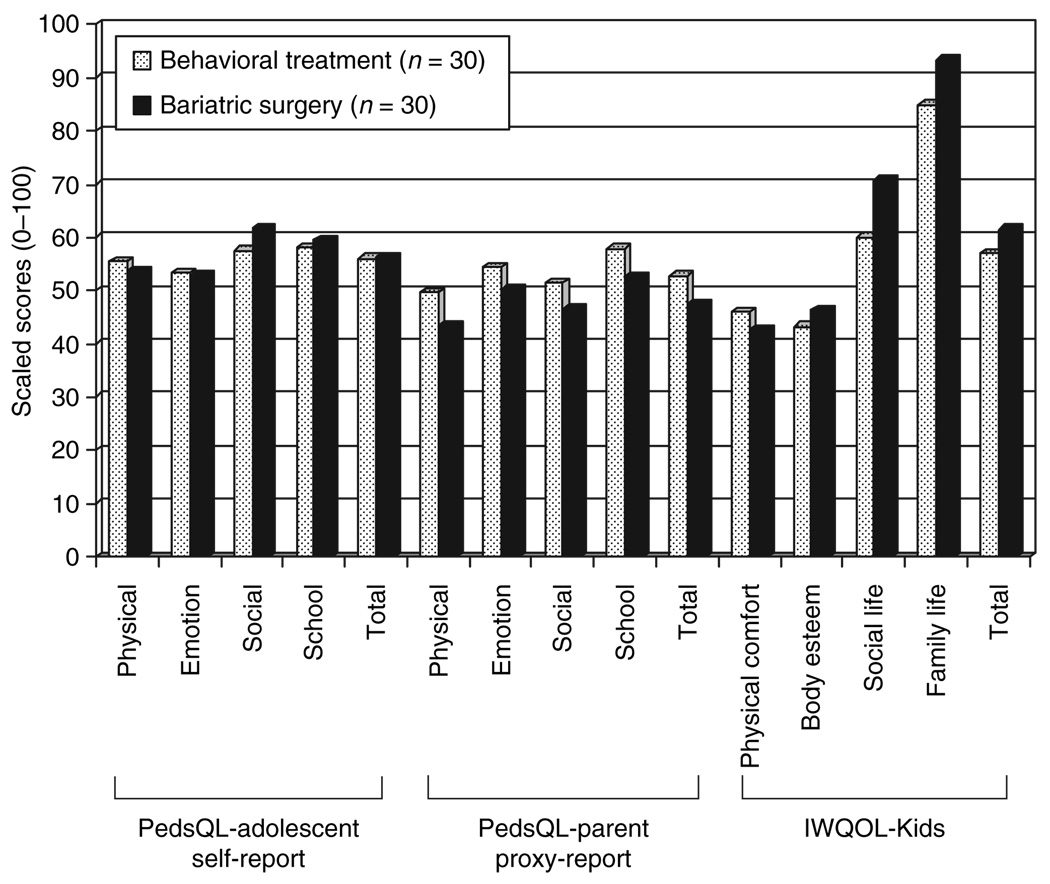
No significant differences were found between bariatric and behavioral samples (age: t (58) = −1.46, P = n.s.; gender: χ2 (1, N = 60) = 0, P = n.s.; race: χ2 (1, N = 60) = 0, P = n.s.). As expected, BMI significantly differed between the groups (Mbariatric sample (s.d.) = 61.8 (8.8) vs. Mbehavioral sample (s.d.) = 51.3 (6.0); t (58) = −5.4, P < 0.0001). After controlling for BMI between youth with extreme obesity pursuing behavioral weight management compared to bariatric surgery, no significant differences were found on PedsQL self (Hotelling’s T = 0.04, F (4, 52) = 0.47, P = n.s.) and parent-proxy reports (Hotelling’s T = 0.04, F (4, 51) = 0.55, P = n.s.) or IWQOL-Kids (Hotelling’s T = 0.12, F (4, 54) = 1.5, P = n.s.) (see Figure 2).
Figure 2.
Differences on health-related quality of life based on treatment type, controlling for BMI. All comparisons were nonsignificant. IWQOL-Kids, Impact of Weight on Quality of Life-Kids.
DISCUSSION
Our study is the first to document global HRQOL impairment across both generic and weight-related domains in a multisite, diverse sample of extremely obese youth. As expected, children and adolescents with extreme obesity suffer from the worst HRQOL compared to other treatment-seeking (19) and nontreatment seeking obese youth (22). One could speculate that the severity of HRQOL impairments seen in the extremely obese adolescent are due to the blatantly visible nature of extreme obesity, the social stigma attached to obesity in youth (30), and the limits it places on day-to-day activities, including physical comfort and capabilities.
Consistent with the broader pediatric and adult HRQOL literature (18,23), obese females report lower HRQOL compared to obese males. Furthermore, it is widely accepted that females, in general, report poorer body esteem/image (31–34) and poorer emotional functioning (35,36) compared to males. However, it is important to note that regardless of gender, adolescents with extreme obesity report significant impairments in these areas of functioning.
These data indicated that black youth demonstrated better HRQOL compared to white adolescents across several weight-specific and generic domains of functioning. Although generic HRQOL impairments are informative when adolescents have psychosocial stressors that impact quality of life that are not weight-related (e.g., divorce, academic difficulties), the findings of greatest interest are related to the weight-specific domains of HRQOL: body esteem and physical comfort. There are multiple reasons for these differences, which are consistent with the broader adolescent and adult literature. For example, studies characterizing black children (37), and black adolescent girls specifically (38–40) indicate that black youth prefer a significantly heavier ideal body size, are less likely to perceive themselves as overweight (41–43) and report better body satisfaction (40,44) compared to whites. The current data are the first to document that black youth, including males, have better body image and are more comfortable with being at extreme levels of overweight than whites. Interestingly, our data also indicate that black youth report better weight-related physical comfort compared to whites of similar extreme weight. However, this is consistent with the adult literature (23,24). It may be that black youth are less likely to endorse discomfort with their physical body when they have better body esteem. Indeed post hoc probing suggests high correlations between these two scales in our sample (r = 0.72; P < 0.0001).
To date, no studies in pediatric obesity have examined differences in HRQOL for adolescents pursuing behavioral treatment compared to bariatric surgery. It could be assumed that extremely obese adolescents with poorer HRQOL may pursue a more aggressive and invasive medical intervention. Certainly the adult obesity literature supports this assumption (23,28). However, this study contradicts such findings and suggests that adolescents with extreme obesity presenting for bariatric surgery do not significantly differ in HRQOL impairment compared to a demographically matched sample of adolescents with extreme obesity presenting for behavioral weight management. Replication of these data with a larger matched sample will prove informative. Similarly, HRQOL measures, specifically weight-specific instruments will be valuable in determining the outcomes of different treatment approaches. In fact, although minimal clinically important differences have not been determined for the IWQOL-Kids, statistically significant differences ranged from 9 to 18 points depending on the subscale when evaluating a weight-loss camp intervention (26).
This study makes important empirical contributions to the pediatric obesity literature, but it is not without limitations. First, this represents a select group of youth who, along with their caregivers and referring physician, have recognized the need for weight management intervention, had access (e.g., location, insurance, and/or Medicaid) to comprehensive hospital-based pediatric weight management programs, and successfully initiated treatment. It is vital to better understand whether these HRQOL characteristics are unique to extremely obese adolescents who seek behavioral or surgical treatment or whether this is typical of adolescents in the broader community who are not accessing care. Second, the sample was limited to adolescents. Future research should focus on the growing number of younger, school-aged children whose BMIs are greater than the 99th percentile (1). In addition, our analyses focused on examining differences between only white and black youth. Although few studies have described the psychosocial adjustment of black youth (21,25,45–47), there are even more limited psychosocial data regarding Hispanic (19,46,48), Asian (49), or Native American youth, known to be at considerable obesity risk. Finally, this study was cross-sectional in nature. The pediatric obesity literature is severely lacking in prospective longitudinal psychosocial studies in general, and specifically studies that characterize adolescents with extreme obesity. With these types of studies, prevention and intervention strategies targeting pediatric obesity can be tailored and/or personalized based on the needs of the family within its cultural context. Overall, research is critically needed to examine factors that contribute to the development and progression of obesity to extreme levels.
ACKNOWLEDGMENTS
Investigator’s efforts for this research were funded by the National Institutes of Health (NIH), including a postdoctoral training grant from the NIH (T32 DK063929) awarded to A.C.M. and a career development award (K23 DK60031) awarded to M.H.Z. Additional funds (CReFF award) were provided to M.H.Z. by the Cincinnati Children’s Hospital Medical Center–General Clinical Research Center, which is supported in part by United States Public Health Service Grant #M01 RR 08084 from the General Clinical Research Centers Program, National Center for Research Resources/NIH.
We extend our deepest appreciation to children and adolescents and their families who participated in this study. We thank the research assistants and summer students who were instrumental in recruiting participants and collecting data, including Christina Ramey, Lindsay Wilson, Stephanie Ridel, Kate Grampp, Ambica Tumkur, and Rachel Jordan from Cincinnati Children’s Hospital Medical Center. We also thank Beverly Haynes and the staff at the Birmingham Children’s Center for Weight Management for their support.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1.Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity (Silver Spring) 2006;14:301–308. doi: 10.1038/oby.2006.39. [DOI] [PubMed] [Google Scholar]
- 2.Jolliffe D. Extent of overweight among US children and adolescents from 1971 to 2000. Int J Obes Relat Metab Disord. 2004;28:4–9. doi: 10.1038/sj.ijo.0802421. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 4.Kirk S, Zeller MH, Claytor R, et al. The relationship of health outcomes to improvement in BMI in children and adolescents. Obes Res. 2005;13:876–882. doi: 10.1038/oby.2005.101. [DOI] [PubMed] [Google Scholar]
- 5.Levine MD, Ringham RM, Kalarchian MA, Wisniewski L, Marcus MD. Is family-based behavioral weight control appropriate for severe pediatric obesity? Int J Eat Disord. 2001;30:318–328. doi: 10.1002/eat.1091. [DOI] [PubMed] [Google Scholar]
- 6.Berkowitz RI, Fujioka K, Daniels SR, et al. Effects of sibutramine treatment in obese adolescents: a randomized trial. Ann Intern Med. 2006;145:81–90. doi: 10.7326/0003-4819-145-2-200607180-00005. [DOI] [PubMed] [Google Scholar]
- 7.Inge TH, Krebs NF, Garcia VF, et al. Bariatric surgery for severely overweight adolescents: concerns and recommendations. Pediatrics. 2004;114:217–223. doi: 10.1542/peds.114.1.217. [DOI] [PubMed] [Google Scholar]
- 8.Pinhas-Hamiel O, Dolan LM, Daniels SR, et al. Increased incidence of non-insulin-dependent diabetes mellitus among adolescents. J Pediatr. 1996;128:608–615. doi: 10.1016/s0022-3476(96)80124-7. [DOI] [PubMed] [Google Scholar]
- 9.Schwimmer JB, Deutsch R, Rauch JB, et al. Obesity, insulin resistance, and other clinicopathological correlates of pediatric nonalcoholic fatty liver disease. J Pediatr. 2003;143:500–505. doi: 10.1067/S0022-3476(03)00325-1. [DOI] [PubMed] [Google Scholar]
- 10.Amin R, Daniels S. Relationship between obesity and sleep-disordered breathing in children: is it a closed loop? J Pediatr. 2002;140:641–643. doi: 10.1067/mpd.2002.125255. [DOI] [PubMed] [Google Scholar]
- 11.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108:712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 12.Balcer LJ, Liu GT, Forman S, et al. Idiopathic intracranial hypertension: relation of age and obesity in children. Neurology. 1999;52:870–872. doi: 10.1212/wnl.52.4.870. [DOI] [PubMed] [Google Scholar]
- 13.Dean H. Natural history of type 2 diabetes diagnosed in childhood: longterm follow up in young adult years. Diabetes. 2002;51(Suppl 2):A24–A25. [Google Scholar]
- 14.Karlson EW, Mandl LA, Aweh GN, et al. Total hip replacement due to osteoarthritis: the importance of age, obesity, and other modifiable risk factors. Am J Med. 2003;114:93–98. doi: 10.1016/s0002-9343(02)01447-x. [DOI] [PubMed] [Google Scholar]
- 15.Zeller MH, Roehrig HR, Modi AC, Daniels SR, Inge TH. Health-related quality of life and depressive symptoms in adolescents with extreme obesity presenting for bariatric surgery. Pediatrics. 2006;117:1155–1161. doi: 10.1542/peds.2005-1141. [DOI] [PubMed] [Google Scholar]
- 16.Schipper H, Clinch JL, Olweny LM. Quality of life studies: definitions and conceptual issues. In: Spilker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials. 2nd edn. Philadelphia, PA: Lippincott-Raven; 1996. pp. 11–24. [Google Scholar]
- 17.Friedlander SL, Larkin EK, Rosen CL, Palermo TM, Redline S. Decreased quality of life associated with obesity in school-aged children. Arch Pediatr Adolesc Med. 2003;157:1206–1211. doi: 10.1001/archpedi.157.12.1206. [DOI] [PubMed] [Google Scholar]
- 18.Ravens-Sieberer U, Redegeld M, Bullinger M. Quality of life after in-patient rehabilitation in children with obesity. Int J Obes Relat Metab Disord. 2001;25(Suppl 1):S63–S65. doi: 10.1038/sj.ijo.0801702. [DOI] [PubMed] [Google Scholar]
- 19.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289:1813–1819. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 20.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Zeller MH, Modi AC. Predictors of health-related quality of life in obese youth. Obesity (Silver Spring) 2006;14:122–130. doi: 10.1038/oby.2006.15. [DOI] [PubMed] [Google Scholar]
- 22.Williams J, Wake M, Hesketh K, Maher E, Waters E. Health-related quality of life of overweight and obese children. JAMA. 2005;293:70–76. doi: 10.1001/jama.293.1.70. [DOI] [PubMed] [Google Scholar]
- 23.Kolotkin RL, Crosby RD, Williams GR. Health-related quality of life varies among obese subgroups. Obes Res. 2002;10:748–756. doi: 10.1038/oby.2002.102. [DOI] [PubMed] [Google Scholar]
- 24.White MA, O’Neil PM, Kolotkin RL, Byrne TK. Gender, race, and obesity-related quality of life at extreme levels of obesity. Obes Res. 2004;12:949–955. doi: 10.1038/oby.2004.116. [DOI] [PubMed] [Google Scholar]
- 25.Fallon EM, Tanofsky-Kraff M, Norman AC, et al. Health-related quality of life in overweight and nonoverweight black and white adolescents. J Pediatr. 2005;147:443–450. doi: 10.1016/j.jpeds.2005.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kolotkin RL, Zeller M, Modi AC, et al. Assessing weight-related quality of life in adolescents. Obesity (Silver Spring) 2006;14:448–457. doi: 10.1038/oby.2006.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Landgraf J, Abetz L, Ware JE. Child Health Questionnaire (CHQ): A User's Manual. Boston, MA: The Health Institute, New England Medical Center; 1996. [Google Scholar]
- 28.de Zwaan M, Lancaster KL, Mitchell JE, et al. Health-related quality of life in morbidly obese patients: effect of gastric bypass surgery. Obes Surg. 2002;12:773–780. doi: 10.1381/096089202320995547. [DOI] [PubMed] [Google Scholar]
- 29.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000:1–27. [PubMed] [Google Scholar]
- 30.Puhl RM, Latner JD. Stigma, obesity, and the health of the nation's children. Psychol Bull. 2007;133:557–580. doi: 10.1037/0033-2909.133.4.557. [DOI] [PubMed] [Google Scholar]
- 31.Field AE, Colditz GA, Peterson KE. Racial/ethnic and gender differences in concern with weight and in bulimic behaviors among adolescents. Obes Res. 1997;5:447–454. doi: 10.1002/j.1550-8528.1997.tb00669.x. [DOI] [PubMed] [Google Scholar]
- 32.Thomas K, Ricciardelli LA, Williams RJ. Gender traits and self-concept as indicators of problem eating and body dissatisfaction among children. Sex Roles. 2000;43:441–458. [Google Scholar]
- 33.Muth JL, Cash TF. Body-image attitudes: what difference does gender make? J Appl Soc Psychol. 1997;27:1438–1452. [Google Scholar]
- 34.Feingold A, Mazzella R. Gender differences in body image is increasing. Psychol Sci. 1998;9:190–195. [Google Scholar]
- 35.Galambos NL, Leadbeater BJ, Barker ET. Gender differences in and risk factors for depression in adolescence: a 4-year longitudinal study. Int J Behav Dev. 2004;28:16–25. [Google Scholar]
- 36.Wichstrom L. The emergence of gender difference in depressed mood during adolescence: the role of intensified gender socialization. Dev Psychol. 1999;35:232–245. [PubMed] [Google Scholar]
- 37.Thompson SH, Corwin SJ, Sargent RG. Ideal body size beliefs and weight concerns of fourth-grade children. Int J Eat Disord. 1997;21:279–284. doi: 10.1002/(sici)1098-108x(199704)21:3<279::aid-eat8>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 38.Wilson GT. Behavioral treatment of obesity: thirty years and counting. Adv Behav Res Ther. 1994;16:31–75. [Google Scholar]
- 39.Parnell K, Sargent R, Thompson S, et al. Black and white adolescent females’ perceptions of ideal body size. J Sch Health. 1996;66 [PubMed] [Google Scholar]
- 40.Kemper KA, Sargent RG, Drane JW, Valois RF, Hussey JR. Black and white females’ perceptions of ideal body size and social norms. Obes Res. 1994;2:117–126. doi: 10.1002/j.1550-8528.1994.tb00637.x. [DOI] [PubMed] [Google Scholar]
- 41.Neff LJ, Sargent RG, McKeown RE, Jackson KL, Valois RF. Black-white differences in body size perceptions and weight management practices among adolescent females. J Adolesc Health. 1997;20:459–465. doi: 10.1016/S1054-139X(96)00273-X. [DOI] [PubMed] [Google Scholar]
- 42.Fitzgibbon ML, Blackman LR, Avellone ME. The relationship between body image discrepancy and body mass index across ethnic groups. Obes Res. 2000;8:582–589. doi: 10.1038/oby.2000.75. [DOI] [PubMed] [Google Scholar]
- 43.Thompson JK, Heinberg LJ, Altable M, Tantleff-Dunn S. Exacting Beauty: Theory, Assessment, and Treatment of Body Image Disturbance. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- 44.Story M, French SA, Resnick MD, Blum RW. Ethnic/racial and socioeconomic differences in dieting behaviors and body image perceptions in adolescents. Int J Eat Disord. 1995;18:173–179. doi: 10.1002/1098-108x(199509)18:2<173::aid-eat2260180210>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 45.Brown KM, McMahon RP, Biro FM, et al. Changes in self-esteem in black and white girls between the ages of 9 and 14 years. The NHLBI Growth and Health Study. J Adolesc Health. 1998;23:7–19. doi: 10.1016/s1054-139x(97)00238-3. [DOI] [PubMed] [Google Scholar]
- 46.Strauss RS. Childhood obesity and self-esteem. Pediatrics. 2000;105:e15. doi: 10.1542/peds.105.1.e15. [DOI] [PubMed] [Google Scholar]
- 47.Young-Hyman D, Schlundt DG, Herman-Wenderoth L, Bozylinski K. Obesity, appearance, and psychosocial adaptation in young African American children. J Pediatr Psychol. 2003;28:463–472. doi: 10.1093/jpepsy/jsg037. [DOI] [PubMed] [Google Scholar]
- 48.Strauss RS, Pollack HA. Social marginalization of overweight children. Arch Pediatr Adolesc Med. 2003;157:746–752. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- 49.Xie B, Chou CP, Spruijt-Metz D, et al. Effects of perceived peer isolation and social support availability on the relationship between body mass index and depressive symptoms. Int J Obes (Lond) 2005;29:1137–1143. doi: 10.1038/sj.ijo.0803006. [DOI] [PubMed] [Google Scholar]