Abstract
The aims of the present study were to examine changes in health-related quality of life (HRQOL) and depressive symptoms in adolescents with extreme obesity undergoing Roux-en-Y gastric bypass (RYGBP) across the first postoperative year. A prospective longitudinal observational study of 31 adolescent patients undergoing RYGBP at a pediatric medical center (mean = 16.4 years; 64.5% females, mean BMI 63.5; 97% of study eligible and consecutive patients) was conducted. Participants completed two adolescent HRQOL measures, the PedsQL (generic) and the IWQOL-Kids (weight-related), the Beck Depression Inventory (BDI), and height and weight were measured at three time points: baseline, and 6 and 12 months following RYGBP. Prior to RYGBP, significant impairments in HRQOL were documented and 38.7% reported depressive symptomatology in the clinical range. As expected, BMI and depressive symptoms decreased and HRQOL improved from baseline to 12 months post-RYGBP. Linear mixed modeling analyses detected several nonlinear slopes in BMI, depressive symptoms, and the majority of HRQOL domains over time with deceleration in these postoperative changes beginning at the 6th month time point. In contrast, the rate of change in weight-related social relations was linear (e.g., no deceleration), indicating continued improvement across the first postoperative year. Adolescent RYGBP results in significant improvement in HRQOL and depressive symptomatology over the first postoperative year. Longer-term follow-up will be critical to determine adolescent weight and psychosocial trajectories, their interrelations, and what role psychosocial status plays in continued weight loss, maintenance, and regain.
INTRODUCTION
Adolescents with extreme obesity (BMI ≥40 kg/m2), estimated at 4% of today’s teenagers (1), are a growing subpopulation experiencing considerable health and psychosocial consequences. These individuals face future medical and psychological risks unless obesity can be successfully and durably treated. Adolescents with extreme obesity frequently must manage “adult” diseases, including type 2 diabetes (2), coronary heart disease (3), obstructive sleep apnea syndrome (4), early severe degenerative joint disease (5), and nonalcoholic fatty liver disease (6). Furthermore, adolescents with extreme obesity report significant impairment in health-related quality of life (HRQOL) across physical, social, and emotional domains (7,8), and many of these youth report clinically significant levels of depressive symptomatology (7,9).
Bariatric surgery, a viable intervention option for extreme obesity in adults, is now undergoing critical evaluation for use with adolescents (10). Recent estimates suggest a recent and noteworthy threefold increase in adolescent weight loss procedures (11). Currently, Roux-en-Y gastric bypass (RYGBP) remains the most common operation for adult and adolescent obesity in the United States. In adults, weight loss outcomes following RYGBP are impressive (12,13), with an associated improvement and/or resolution of medical and psychological comorbidities, including improved mood (14) and generic (15) and weight-related (16) HRQOL. Recent reports from the Swedish Obese Subjects study (17) demonstrated that the pattern of change in HRQOL across 10 years following RYGBP mirrors patterns of weight loss, weight regain, and weight stability.
Comprehensive studies of adolescent bariatric surgery outcomes are in their infancy and are critically needed. Six published studies to date have reported on the psychosocial outcomes of adolescent bariatric surgery, including impressive weight outcomes of RYGBP (18,19) and laparoscopic-adjustable gastric banding (20) in the United States as well as positive outcomes of laparoscopic-adjustable gastric banding in Austria (21) and Israel (22). However, many of these studies were based on retrospective chart reviews and were limited by small sample sizes or nonsystematic and/or significant loss to follow-up. Furthermore, objective measures of psychosocial status were either not utilized (22) or included measures lacked psychometric validation with adolescent age-groups (18,19). The present study is the first to prospectively and systematically examine the psychosocial outcomes of adolescent RYGBP and the rate of change in these outcomes. Based on the adult literature, we hypothesized that following RYGBP, adolescents would experience significant improvements in psychosocial status, including improved generic and weight-related HRQOL and a reduction in depressive symptoms, with some deceleration in these improvements by the end of the first postoperative year.
METHODS AND PROCEDURES
Participants
A total of 31 adolescent patients were enrolled prospectively into a longitudinal study documenting the psychosocial outcomes of adolescent RYGBP. Adolescents underwent RYGBP between May 2004 and January 2007. RYGBP candidacy was based on adolescent patient selection guidelines as previously described (10). Study inclusion criteria required participants to be 13–17 years of age and have no physical impairments unrelated to obesity (e.g., spinal anomaly), or developmental disability. Potential participants and their caregiver(s) were approached for participation after approval for RYGBP. Of the 32 consecutive patients meeting inclusion criteria, 97% agreed to participate in the study and completed baseline measures. One patient declined due to lack of interest in participation in research. A summary of demographic characteristics of participants at baseline are presented in Table 1.
Table 1.
Pre-RYGBP/baseline demographic information of adolescents (N = 31)
| N | Mean (s.d.) | % | Range | |
|---|---|---|---|---|
| Gender | ||||
| Girls | 20 | 64.5 | ||
| Boys | 11 | 35.5 | ||
| Race | ||||
| White | 25 | 80.6 | ||
| African American | 5 | 16.1 | ||
| Biracial/other | 1 | 3.2 | ||
| Age at baseline (years) | 16.4 (1.4) | 13.7–18.4 | ||
| BMI (kg/m2) | 63.5 (10.6) | 48.2–88.8 | ||
| Socioeconomic statusa | 40.8 (21.1) | |||
| N used in analyses | ||||
| Participants with all three time points | 27 | 87.0 | ||
| Participants with baseline and only 1 follow-up time point | 4 | 13.0 | ||
Based upon Duncan TSEI2 for head of household, a measure of occupational attainment.
Laparoscopic RYGBP was performed as previously described (23). Briefly, using minimally invasive laparoscopic techniques, a small gastric pouch was created just distal to the gastroesophageal junction. Next, a Roux-en-Y reconstruction was fashioned to drain the pouch, providing a significantly restrictive and diversionary procedure for weight loss.
Procedure
All personnel were trained to screen and recruit participants, obtain informed consent/assent, and administer questionnaires to adolescents and their primary caregiver. Instructions for each measure were read aloud to each adolescent and caregiver; however, the measures were completed independently. The adolescent’s current weight and height were also measured by research staff at each study time point. All baseline data were collected in a clinic room. However, to minimize patient burden and promote study retention, follow-up data were collected in locations most convenient for the family, including both hospital (80%) and home settings (20%). Participants were compensated for participating in the study. Institutional Review Board approval was obtained for this study.
Outcome measures
Anthropometrics
Research assistants completing data collection were trained in methods of obtaining accurate weight and height measurements. Weight was measured (0.1 kg) on a digital Scaletronic scale (Scale Tronic, Wheaton, IL). Standing height was measured with a Holtain stadiometer (Holtain, Crymych, UK). For those participants who had data collected in a home setting at a follow-up time point (20%), weight was measured on a portable SECA digital scale (SECA, Hamburg, Germany) with standing height measured with a calibrated custom portable stadiometer (Creative Health Products, Plymouth, MI). Weight and height measurements were taken in triplicate and the mean was used in analyses. Participants were weighed and measured in street clothing without shoes. These data were used to calculate BMI and data were expressed in kg/m2.
PedsQL
The PedsQL (24) is a widely used and psychometrically sound 23-item generic pediatric HRQOL measure that includes an adolescent self-report version for youth aged 13–18. The measure includes four subscales, including Physical, Emotional, Social, and School functioning, as well as a Psychosocial Health summary score (mean score of Emotional, Social, and School subscales) and a Total score. Scores are standardized and range from 0 to 100, with higher scores representing better quality of life. Minimal clinically important difference (MCID) scores, defined as the smallest change in score that patients perceive to be beneficial, have also been identified for the PedsQL. For the Physical and Psychosocial Health summary scales, the MCIDs are 6.66 and 5.30, respectively (25).
IWQOL-Kids
This 27-item instrument (26) was designed to assess aspects of weight-related quality of life in adolescents, aged 11–19 years. Factor analyses identified four factors, including Physical Comfort, Body Esteem, Social Life, and Family Relations, as well as a Total score. This measure has strong psychometric properties, discriminates among weight status groups, and is responsive to weight change. Scaled scores are standardized and range from 0 to 100, with higher scores representing better weight-related quality of life. No MCIDs have been established for this measure to date.
Beck Depression Inventory–II
The Beck Depression Inventory –II (BDI-II) (27) is a 21-item questionnaire that measures specific symptoms of depression for individuals ≥14 years. The BDI has well-established psychometric properties and is a reliable and valid screening tool for depressive symptoms in adolescents. The total raw score was utilized, with higher scores reflecting more depressive symptoms. Total Raw scores also correspond to ranges of symptom severity (0–13: “minimal” symptoms; 14–19: “mild” symptoms; 20–28: “moderate” symptoms; ≥29: “severe” symptoms). A total raw score of ≥17 is a conservative marker for depressive symptoms and represents a clinically elevated range recommended in clinical settings.
Demographic Background Questionnaire
Mothers completed a background questionnaire documenting family characteristics including parent marital status, level of education, and family income and size. Sufficient data were available to determine family socioeconomic status (SES) using the Revised Duncan (TSE12 (28,29)), with higher scores representing greater occupational attainment. For two-caregiver households, the higher TSEI2 was reported.
statistical analyses
Descriptive analyses, including means and standard deviations, were calculated for BMI, HRQOL scores, and depressive symptoms score at each time point (baseline, 6 month, 12 months). Response variables were then analyzed using linear mixed models (LMMs) for repeated measures data (30). To preserve experimental-wise α, we reduced the number of statistical tests to those response variables that imparted unique information. Based on hypotheses, we tested models for BMI, total depressive symptoms, two generic HRQOL summary scales (PedsQL: Physical Health, Psychosocial Health), and only three aspects of weight-related HRQOL (IWQOL-Kids: Physical Comfort, Body Esteem, Social Life). We excluded the Family Life variable from statistical evaluation because visual examination of mean plots suggested zero change over time.
As discussed above, a nonlinear trajectory was hypothesized for response variables. However, there were only three time points, and a traditional quadratic polynomial analysis with predictors, month and month2, would produce a saturated model that would perfectly fit the observed means. To avoid the saturated model, we used a transformation of time, loge(month), as a single nonlinear trajectory term. The log transformation is a member of the family of transformations known as fractional polynomials (31) and it produces a curve shape similar to the quadratic polynomial for monotonic curves (i.e., nonlinear but continually increasing or decreasing). For each response variable, we estimated a linear model (with intercept and a linear slope term) and a nonlinear log model (with intercept and a nonlinear slope term). The decision to use the linear or nonlinear term was determined by which produced the smallest value of the Akaike’s Information Criterion (32). Having selected a slope term, its associated parameter estimate was tested for statistical significance (i.e., tested against an intercept-only model). These tests were based on t-statistics with estimated degrees of freedom appropriate for small-sample inference (33). To account for individual variation and dependency due to repeated measures, each model had random effects for the intercept and slope (whether linear or nonlinear) indexing individual deviations from the mean parameters.
All models were estimated with the mixed procedure of SAS version 9.1 (SAS Institute, Cary, NC) using full maximum likelihood estimation for the model selection based on the Akaike’s Information Criterion, and restricted maximum likelihood estimation for the final model. Some variables had a small amount of missing data at various time points (maximum 8%) that was treated as ignorable in the maximum likelihood estimation, so participants with data for at least one time point were included in the analysis.
RESULTS
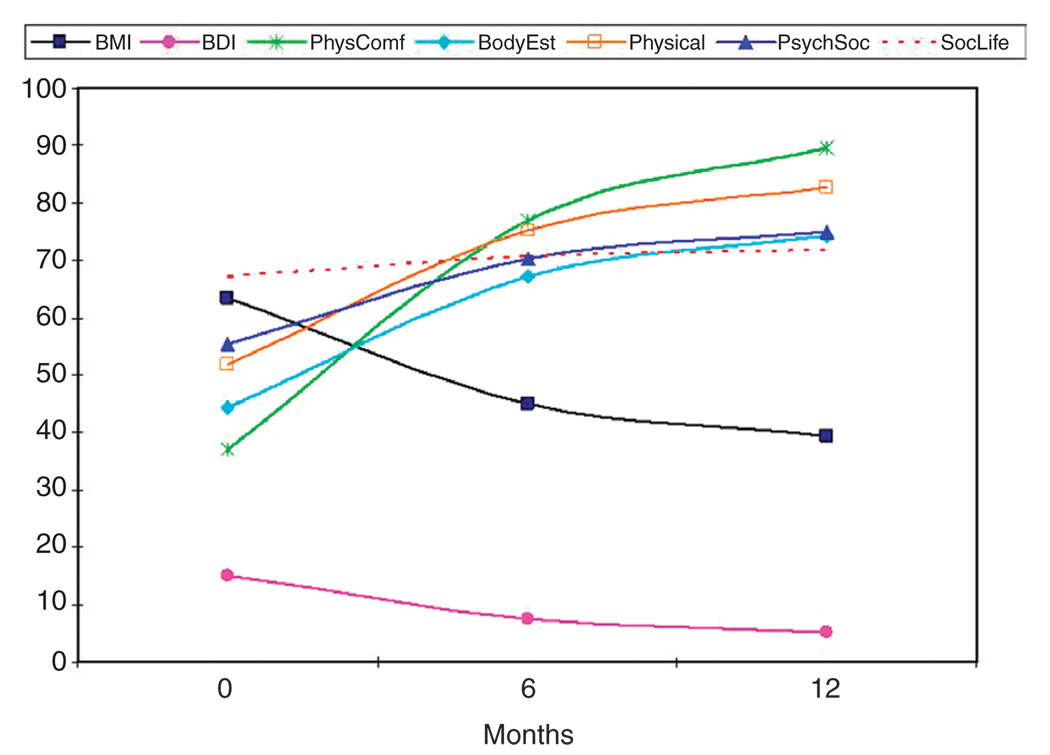
Descriptive data, including the observed means for all response variables at each time point, are presented in Table 2. The results of LMM analyses are presented in Table 3. Figure 1 demonstrates the predicted means for the response variables over time. As shown in Table 3 and illustrated in Figure 1, the nonlinear slope estimates of BMI and depressive symptoms (BDI) were negative indicating these response variables had a mean monotonic decrease over time. In contrast, the slope estimates of the HRQOL measures were positive indicating these response variables had a mean monotonic increase over time.
Table 2.
Observed means and standard deviations for adolescent BMI and self-report of pre-RYGBP/baseline and 6- and 12-month psychosocial status post-RYGBP
| Pre-RYGBP baseline (n = 31) |
6-month follow-up (n = 29) |
12-month follow-up (n = 28–29) |
||||
|---|---|---|---|---|---|---|
| Mean | s.d. | Mean | s.d. | Mean | s.d. | |
| Adolescent BMI | 63.5 | 10.6 | 44.6 | 8.9 | 39.4 | 7.8 |
| BDI total score | 15.2 | 12.4 | 7.3 | 9.0 | 5.3 | 5.6 |
| PedsQL | ||||||
| Total score | 53.9 | 17.3 | 73.2 | 13.1 | 77.2 | 12.4 |
| Physical health | 51.3 | 19.0 | 78.0 | 14.7 | 81.5 | 13.8 |
| Psychosocial health | 55.4 | 18.4 | 70.4 | 14.8 | 74.9 | 13.9 |
| Emotional functioning | 50.6 | 20.4 | 66.9 | 19.9 | 69.8 | 18.3 |
| Social functioning | 59.5 | 22.2 | 76.0 | 21.0 | 84.6 | 16.1 |
| School functioning | 60.6 | 19.9 | 68.9 | 19.5 | 70.2 | 18.3 |
| IWQOL-Kids | ||||||
| Total score | 58.6 | 20.1 | 78.2 | 20.5 | 86.9 | 14.5 |
| Physical comfort | 36.9 | 22.3 | 77.2 | 21.1 | 90.4 | 12.7 |
| Body esteem | 44.4 | 30.3 | 67.1 | 29.8 | 74.9 | 26.8 |
| Social life | 66.5 | 29.3 | 80.7 | 24.5 | 89.2 | 16.1 |
| Family life | 92.7 | 12.8 | 93.1 | 17.3 | 97.8 | 5.5 |
BDI, Beck Depression Inventory.
Table 3.
Linear mixed models analysis of change in adolescent BMI and self-report of psychosocial status pre-/post-RYGBP
| Response Variable | Intercept | SE | Slope | SE |
|---|---|---|---|---|
| BMI | 63.40 | 1.89 | −9.37 | 0.34 |
| PedsQL | ||||
| Physical health | 51.78 | 3.28 | 12.10 | 1.11 |
| Psychosocial health | 55.40 | 3.30 | 7.62 | 1.15 |
| IWQOL-Kids | ||||
| Physical comfort | 36.94 | 4.00 | 20.58 | 1.38 |
| Body esteem | 44.26 | 5.41 | 11.75 | 1.41 |
| Social lifea | 67.10 | 5.28 | 1.84 | 0.30 |
| BDI total score | 15.11 | 2.14 | −3.87 | 0.78 |
Linear slope; all estimates were significant, P ≤ 0.001.BDI, Beck Depression Inventory.
Figure 1.
Predicted means for response variables based on LMM parameter estimates at baseline (pre-surgery) and at 6 and 12 months postoperatively.
Preliminary results not presented indicated that the Akaike’s Information Criterion value for the log transformation of month was lower than for the untransformed time metric for all variables except Social Life. Thus, month was the predictor for social life and loge(month) was the predictor for the remaining variables. All parameters estimates were significant at the α = 0.001 level.
BMI
The observed mean change in BMI from baseline to 12 months was −24.1 kg/m2 (n = 28). This represents a mean BMI loss of 38%. At 12 months post-RYGBP, 96.4% (n = 27) of adolescents remained obese (BMI ≥95th percentile for age and gender (34)), and 46.4% (n = 13) had BMIs which remained in the extreme (>40 kg/m2) range (n = 28; BMI range 12 months post-RYGBP: 28.1–64.7 kg/m2). LMM analyses revealed a significant negative nonlinear slope indicating a significant monotonic decrease (or consistent downward trend) over time with deceleration in BMI change beginning at the 6th month time point (Table 3, Figure 1).
Depressive symptoms
At baseline, the mean total raw score of depressive symptoms on the BDI (Table 2) was in the “mild” range based on instrument normative guidelines. Twelve adolescents (38.7%) exhibited depressive symptoms within a clinical range (raw scores ≥17), which included 45% (n = 9) of females and 27.3% (n = 3) of male participants. At 6 months post-RYGBP, no males and three females (10.3%) reported clinical range symptoms. At 12 months post-RYGBP, only two females (6.9%) remained with symptoms in the clinical range. LMM analyses (Table 3, Figure 1) revealed a significant negative nonlinear slope indicating a monotonic decrease over time. This result was highly similar to the BMI result—adolescents experience substantial symptom reduction across the first postoperative 6 months with substantial deceleration by 12 months.
HRQOL
Prior to RYGBP, adolescent generic PedsQL and weight-related IWQOL-Kids scores were markedly impaired, with the exception of the weight-related Family Relations scale (Table 2). By 12 months post-RYGBP, generic- and weight-related HRQOL improved substantially. LMM analyses (Table 3, Figure 1) showed a significant positive nonlinear slope for weight-related physical comfort and generic physical health indicating a significant monotonic increase (or consistent upward trend) over time with a deceleration in these improvements beginning at the 6th month time point. Similar nonlinear increases were seen on the generic psychosocial health and the weight-related Body Esteem scales. However, change in social life was consistently linear and showed no significant deceleration over the 12 months. It is important to note that clinically meaningful improvements (e.g., MCID scores) were found for the PedsQL Physical Health and Psychosocial scales from baseline to 6 months post-RYGBP; however, the improvement from 6 to 12 months post-RYGBP was not perceived to be clinically meaningful by patients.
DISCUSSION
The present data are from the first prospective longitudinal study to document psychosocial outcomes of RYGBP surgery in adolescents with extreme levels of obesity. Our data demonstrate that RYGBP is an effective weight loss intervention for adolescents, which also results in significant improvement in overall and weight-related HRQOL, and depressive symptomatology across the first postoperative year. Prior to RYGBP, adolescents with extreme obesity present with the most significant and global impairments in HRQOL relative to other pediatric chronic illness populations (35). Similarly, the number of adolescents presenting for RYGBP with depressive symptoms in the clinical range is at a rate 3–4 times higher than national base rates for adolescent males (7.4%) and females (13.9%) (36).
At 1 year post-RYGBP, teens reported generic HRQOL within 1 s.d. of healthy adolescent normative comparisons (24). These findings of more normative adolescent psychosocial status at 1 year post-RYGBP are similar to those reported by Dymek and colleagues (16) in their cross-sectional study comparing adults pre-/postbariatric surgery. These marked psychosocial improvements for adolescents following RYGBP are quite notable given that the vast majority of adolescents remain obese or even extremely obese at 1 year following their procedure. These data suggest that from the psychosocial standpoint, the change in weight may be more important than the final BMI achieved following surgery.
At 6 and 12 months after RYGBP, adolescents reported a significant improvement in their day-to-day weight-related physical comfort (e.g., “Because of my weight it is hard to… bend over”, “move around”, “fit in public seats”), their general physical capabilities (e.g., “It is hard for me to…walk more than a block”, “run”), and their weight-related body esteem (e.g., “Because of my weight I am…ashamed of my body”). Furthermore, teens reported significant improvements in their overall psychosocial health and weight-related social relations (e.g., “Because of my weight people…tease me”, “avoid spending time with me”), as well as “minimal” depressive symptoms. Interestingly, a post hoc chart abstraction revealed a decrease in the use of antidepressant or mood stabilizing medications over time. Specifically, 6 of the 31 (19.4%) adolescents were taking an antidepressant or mood stabilizing medication at baseline with only two remaining on medication at the 12-month follow-up. Thus, despite a decrease in use of pharmacological treatment for depression, patients reported clinical improvements in depressive symptomatology over time.
Our statistical approach (LMM analyses) allowed for examination of the rate of change over time in BMI and psychosocial status from baseline through the first postoperative year. Consistent with reports on adult RYGBP outcomes in Sweden (37), our analyses detected a deceleration of BMI change from 6 to 12 months postoperatively. As hypothesized and in parallel with initial weight loss phases, the rates of improvement in the majority of psychosocial domains substantially slowed down beginning at 6 months postoperatively. Furthermore, for scales in which established MCID scores exist (e.g., general physical capabilities and general psychosocial health), the statistical findings and clinically meaningful improvements mirrored each other. In other words, as the rate of improvement in PedsQL scores began to decelerate during the 6- to 12-month postoperative period, patients also did not perceive meaningful improvements during this time. Interestingly, adolescents’ social relations with peers in the context of their weight (e.g., stigmatization, friendships) demonstrated no slowing in the rate of improvement across the first postoperative year.
Although these initial findings of marked improvements in psychosocial functioning for adolescents who have undergone RYGBP are quite promising, the adult literature would suggest caution. Longitudinal trends for adults suggests HRQOL changes parallel patterns of weight loss, weight regain, and weight stability (17). Furthermore, initial improvements in depressive symptoms may dissipate for some individuals 18–24 months after bariatric surgery (17,38) and new onset of depressive symptoms may occur despite good weight loss outcome (39). Weight regain trends after adolescent gastric bypass are not yet adequately characterized, although may be as high as 10–20% (40,41). If longer-term adolescent bariatric outcomes are found to be similar to those described in adults, it is crucial to identify and provide intervention to adolescents who may experience weight regain after undergoing RYGBP to prevent relapse in behavioral and psychosocial functioning.
Finally, what role medical comorbidities and their resolution play in an adolescent’s psychosocial improvements following RYGBP remains an important area of future research. For example, there is sound evidence that adolescent RYGBP leads to resolution of medical comorbidities (40–43). Given the developing pediatric literature which has suggested obese youth with medical comorbidities may experience poorer HRQOL relative to those whose health status is less impaired (44), future work with larger samples should explore whether changes in comorbid conditions might be mediating the changes in HRQOL.
Longer-term adolescent studies are critically needed to document adolescent RYGBP weight, health, and psychosocial trajectories, and their interrelations. Furthermore, clinical practice and postoperative adolescent treatment models will benefit from understanding which, if any, psychosocial components drive BMI change dynamically. Specifically, are there psychosocial factors which, if monitored and addressed, would improve (or help sustain) adolescent postoperative weight loss outcomes. Unfortunately, this type of dynamic modeling (i.e., multilevel mixed longitudinal modeling with dynamic or time-varying predictors (30)) was not possible in the present study given there were only three time points. These types of questions will be addressed through our adolescent bariatric research consortium (Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS)) (45) with a considerably larger multi-site sample. Designed as a prospective, longitudinal cohort observational study, the main objectives of Teen-LABS are to document the safety of bariatric surgery in adolescence and postoperative health and psychosocial outcomes at 6-, 12- and annually in comparison to adult outcomes (46).
Finally, it is noteworthy that adolescent bariatric surgery occurs at an important time in psychosocial development—a period of rapid change in emotional, interpersonal, social, and career/vocational domains in which good adaptation bodes well for continued positive adaptation in the transition to emerging adulthood (aged 18–20) (47,48). We argue that bariatric surgery has the potential to positively alter the psychosocial and resultant developmental trajectory of this unique adolescent subpopulation. To fully understand the impact of adolescent bariatric surgery on psychosocial and developmental outcomes, we must examine their interactions within these age-salient contexts (e.g., peers, family, romantic relationships, co-workers, school, work). Thus, a more comprehensive assessment of psychosocial factors, contexts, and outcomes particularly salient to youth as they transition from adolescence to young adulthood is needed. Only long-term, prospective and controlled studies utilizing a nonoperative extremely obese adolescent comparison group will provide such evidence.
ACKNOWLEDGMENTS
This research was funded by a grant from the National Institutes of Health awarded to M.H.Z. (R03 DK0788901). Additional funds (CReFF award) were provided to M.H.Z. by the Cincinnati Children’s Hospital Medical Center—General Clinical Research Center, which is supported in part by USPHS grant no. M01 RR 08084 from the General Clinical Research Centers Program, National Center for Research Resources/NIH. We thank Christina Ramey, Lindsay Wilson, Kate Grampp and Jennifer Reiter-Purtil for assistance with data collection, participant retention efforts, and database management. We extend our gratitude to Jenny Sweeney, Clinical Nurse Coordinator.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1.Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity. 2006;14:301–308. doi: 10.1038/oby.2006.39. [DOI] [PubMed] [Google Scholar]
- 2.Pinhas-Hamiel O, Dolan LM, Daniels SR, et al. Increased incidence of non-insulin-dependent diabetes mellitus among adolescents. J Pediatr. 1996;128(5 Pt 1):608–615. doi: 10.1016/s0022-3476(96)80124-7. [DOI] [PubMed] [Google Scholar]
- 3.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108:712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 4.Kalra M, Inge T, Garcia V, et al. Obstructive sleep apnea in extremely overweight adolescents undergoing bariatric surgery. Obesity Res. 2005;13:1175–1179. doi: 10.1038/oby.2005.139. [DOI] [PubMed] [Google Scholar]
- 5.Karlson EW, Mandl LA, Aweh GN, et al. Total hip replacement due to osteoarthritis: The importance of age, obesity, and other modifiable risk factors. Am J Med. 2003;114:93–98. doi: 10.1016/s0002-9343(02)01447-x. [DOI] [PubMed] [Google Scholar]
- 6.Schwimmer JB, Deutsch R, Rauch JB, et al. Obesity, insulin resistance, and other clinicopathological correlates of pediatric nonalcoholic fatty liver disease. J Pediatr. 2003;143:500–505. doi: 10.1067/S0022-3476(03)00325-1. [DOI] [PubMed] [Google Scholar]
- 7.Zeller MH, Roehrig HR, Modi AC, Daniels SR, Inge TH. Health-related quality of life and depressive symptoms in adolescents with extreme obesity presenting for bariatric surgery. Pediatrics. 2006;117:1155–1161. doi: 10.1542/peds.2005-1141. [DOI] [PubMed] [Google Scholar]
- 8.Modi AC, Loux TJ, Bell SK, et al. Weight-specific health-related quality of life in adolescents with extreme obesity. Obesity. 2008;16:2266–2271. doi: 10.1038/oby.2008.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim RJ, Langer JM, Baker AW, et al. Psychosocial status in adolescents undergoing bariatric surgery. Obes Surg. 2008;18:27–33. doi: 10.1007/s11695-007-9285-x. [DOI] [PubMed] [Google Scholar]
- 10.Inge TH, Krebs NF, Garcia VF, et al. Bariatric surgery for severely overweight adolescents: Concerns and recommendations. Pediatrics. 2004;114:217–223. doi: 10.1542/peds.114.1.217. [DOI] [PubMed] [Google Scholar]
- 11.Tsai W, Inge TH, Burd R. Bariatric surgery in adolescents: recent national trends in use and in-hospital outcomes. Arch Pediatr Adolesc Med. 2007;161:217–221. doi: 10.1001/archpedi.161.3.217. [DOI] [PubMed] [Google Scholar]
- 12.Wittgrove AC, Clark GW. Laparoscopic gastric bypass, Roux-en-Y- 500 patients: technique and results, with 3–60 month follow-up. Obes Surg. 2000;10:233–239. doi: 10.1381/096089200321643511. [DOI] [PubMed] [Google Scholar]
- 13.DeMaria EJ, Sugerman HJ, Kellum JM, Meador JG, Wolfe LG. Results of 281 consecutive total laparoscopic Roux-en-Y gastric bypasses to treat morbid obesity. Ann Surg. 2002;235:640–645. doi: 10.1097/00000658-200205000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dixon JB, Dixon ME, O’Brien PE. Depression in association with severe obesity: changes with weight loss. Arch Intern Med. 2003;163:2058–2065. doi: 10.1001/archinte.163.17.2058. [DOI] [PubMed] [Google Scholar]
- 15.De Zwaan M, Lancaster BA, Mitchell JE, et al. Health-related quality of life in morbidly obese patients: Effect of gastric bypass surgery. Obes Surgery. 2002;12:773–780. doi: 10.1381/096089202320995547. [DOI] [PubMed] [Google Scholar]
- 16.Dymek MP, Le Grange D, Neven K, Alverdy J. Quality of life after gastric bypass surgery: A cross-sectional study. Obes Res. 2002;10:1135–1142. doi: 10.1038/oby.2002.154. [DOI] [PubMed] [Google Scholar]
- 17.Karlsson J, Taft C, Ryden A, Sjostrom L, Sullivan M. Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: the SOS intervention study. Int J Obes. 2007;31:1248–1261. doi: 10.1038/sj.ijo.0803573. [DOI] [PubMed] [Google Scholar]
- 18.Collins J, Mattar S, Qureshi F, et al. Initial outcomes of laparoscopic Roux-en-Y gastric bypass in morbidly obese adolescents. Surg Obes Rel Disord. 2007;3:147–152. doi: 10.1016/j.soard.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Loux TJ, Haricharan RN, Clements RH, et al. Health-related quality of life before and after bariatric surgery in adolescents. J Pediatr Surg. 2008;43:1275–1279. doi: 10.1016/j.jpedsurg.2008.02.078. [DOI] [PubMed] [Google Scholar]
- 20.Holterman AX, Browne A, Dillard BE, et al. Short-term outcome in the first 10 morbidly obese adolescent patients in the FDA-approved trial for laparoscopic adjustable gastric banding. J Pediatr Gastronenterol Nutr. 2007;45:465–473. doi: 10.1097/MPG.0b013e318063eef6. [DOI] [PubMed] [Google Scholar]
- 21.Widhalm K, Dietrich S, Prager G, et al. Bariatric surgery in morbidly obese adolescents: A 4-year follow-up of ten patients. Int J Pediatr Obes. 2008;3:78–92. doi: 10.1080/17477160801897208. [DOI] [PubMed] [Google Scholar]
- 22.Abu-Abeid S, Gavert N, Klausner JM, Szoid A. Bariatric surgery in adolescence. J Pediatr Surg. 2003;38:1279–1282. doi: 10.1016/s0022-3468(03)00400-7. [DOI] [PubMed] [Google Scholar]
- 23.Higa KD, Boone KB, Davies OG. Laparoscopic Roux-en-Y gastric bypass for morbid obesity: technique and preliminary results of our first 400 patients. Arch Surg. 2000;135:1029–1033. doi: 10.1001/archsurg.135.9.1029. [DOI] [PubMed] [Google Scholar]
- 24.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3:329–341. doi: 10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 26.Kolotkin RL, Zeller MH, Modi AC, et al. Assessing weight-related quality of life in adolescents. Obesity. 2006;14:448–457. doi: 10.1038/oby.2006.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beck AT, Steer RA, Brown GK. Manual for Beck Depression Inventory-II. San Antonio, TX: Psychological Corp; 1996. [Google Scholar]
- 28.Stevens G, Featherman DL. A revised socioeconomic index of occupational status. Soc Sci Res. 1981;10:364–395. [Google Scholar]
- 29.Nakao K, Treas J. The 1989 Socioeconomic Index of Occupations: Construction from the 1989 Occupational Prestige Scores. Chicago: University of Chicago, National Opinion Research Center; 1992. [Google Scholar]
- 30.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. New York: Wiley; 2004. [Google Scholar]
- 31.Royston P, Altman DO. Regression using fractional polynomial of continuous covariates: parsimonious parametric modelling. Appl Stat. 1994;43:429–467. [Google Scholar]
- 32.Kuha J. AIC and BIC: comparisons of assumptions and performance. Sociol Methods Res. 2004;33:188–229. [Google Scholar]
- 33.Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–997. [PubMed] [Google Scholar]
- 34.Expert Committee. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120 Suppl 4:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 35.Varni JW, Limbers CA, Burwinkle TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL™ 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:43. doi: 10.1186/1477-7525-5-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kilpatrick DG, Ruggiero KJ, Acierno R, et al. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the national survey of adolescents. J Consult Clin Psychol. 2003;71:692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- 37.Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–2693. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 38.Karlsson J, Sjostrom L, Sullivan M. Swedish obese subjects (SOS)—an intervention study of obesity. Two-year follow-up of health-related quality of life (HRQOL) and eating behavior after gastric surgery for severe obesity. Int J Obes Relat Metab Disord. 1998;22:113–126. doi: 10.1038/sj.ijo.0800553. [DOI] [PubMed] [Google Scholar]
- 39.Kodama K, Noda S, Murakami A, et al. Depressive disorders as psychiatric complications after obesity surgery. Psychiatr Clin Neurosci. 1998;52:471–476. doi: 10.1046/j.1440-1819.1998.00447.x. [DOI] [PubMed] [Google Scholar]
- 40.Lawson ML, Kirk S, Mitchell T, et al. One-year outcomes of Roux-en-Y gastric bypass for morbidly obese adolescents: a multi-center study from the Pediatric Bariatric Study Group. J Pediatr Surg. 2006;41:137–143. doi: 10.1016/j.jpedsurg.2005.10.017. discussion 143. [DOI] [PubMed] [Google Scholar]
- 41.Sugerman HJ, Sugerman EL, DeMaria EJ, et al. Bariatric surgery for severely obese adolescents. J Gastrointest Surg. 2003;7:102–107. doi: 10.1016/S1091-255X(02)00125-7. [DOI] [PubMed] [Google Scholar]
- 42.Kalra M, Mannaa M, Fitz K, et al. Effect of surgical weight loss on sleep architecture in adolescents with severe obesity. Obes Surg. 2008;18:675–679. doi: 10.1007/s11695-008-9472-4. [DOI] [PubMed] [Google Scholar]
- 43.Ippisch HM, Inge TH, Daniels SR, et al. Reversibility of cardiac abnormalities in morbidly obese adolescents. J Am Coll Cardiol. 2008;51:1342–1348. doi: 10.1016/j.jacc.2007.12.029. [DOI] [PubMed] [Google Scholar]
- 44.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289:1813–1819. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 45.Inge TH, Zeller M, Harmon C, et al. Teen-Longitudinal Assessment of Bariatric Surgery: methodological features of the first prospective multi-center study of adolescent bariatric surgery. J Pediatr Surg. 2007;42:1969–1971. doi: 10.1016/j.jpedsurg.2007.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Belle SH, Berk PD, Courcoulas AP, et al. Safety and efficacy of bariatric surgery: Longitudinal Assessment of Bariatric Surgery. Surg Obes Relat Dis. 2007;3:116–126. doi: 10.1016/j.soard.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Masten AS, Coatsworth JD, Neemann J, et al. The structure and coherence of competence from childhood through adolescence. Child Dev. 1995;66:1635–1659. [PubMed] [Google Scholar]
- 48.Roisman GI, Masten AS, Coatsworth JD, Tellegen A. Salient and emerging developmental tasks in the transition to adulthood. Child Dev. 2004;75:123–133. doi: 10.1111/j.1467-8624.2004.00658.x. [DOI] [PubMed] [Google Scholar]