Abstract
The purpose of this study was to define early events during the angiogenic response of the aortic wall to injury. Rat aortic rings produced neovessels in collagen culture but lost this capacity over time. These quiescent rings responded to vascular endothelial growth factor (VEGF) but not to a cocktail of macrophage-stimulatory cytokines and chemokines that was angiogenically active on fresh rings. Analysis of cytokine receptor expression revealed selective loss in quiescent rings of the proangiogenic chemokine receptor CXCR2, which was expressed predominantly in aortic macrophages. Pharmacologic inhibition of CXCR2 impaired angiogenesis from fresh rings but had no effect on VEGF-induced angiogenesis from quiescent explants. Angiogenesis was also impaired in cultures of aortic rings from CXCR2-deficient mice. Reduced CXCR2 expression in quiescent rat aortic rings correlated with marked macrophage depletion. Pharmacologic ablation of macrophages from aortic explants blocked formation of neovessels in vitro and reduced aortic ring-induced angiogenesis in vivo. The angiogenic response of macrophage-depleted rings was completely restored by adding exogenous macrophages. Moreover, angiogenesis from fresh rings was promoted by macrophage colony stimulating factor (CSF-1) and inhibited with anti-CSF-1 antibody. Thus aortic angiogenic sprouting following injury is strongly influenced by conditions that modulate resident macrophage numbers and function.
Keywords: chemokines, inflammation, leukocytes, monocytes, neovascularization
Introduction
Angiogenesis, the process of formation of neovessels from preexisting vessels, plays an important role in many physiologic, reactive and pathologic processes (1). Blood vessels actively proliferate during embryonic development and fetal growth to supply tissues with oxygen and nutrients, and dispose of metabolic waste products. The angiogenic process is regulated by many growth factors including vascular endothelial growth factor (VEGF) and angiopoietin-1 (Ang-1) (2–4). During postnatal life the vascular bed continues to expand and angiogenesis remains active in selected anatomical sites such as the retina and the growth plates of long bones (5,6). Once tissues and organs have reached full maturity, blood vessels cease to proliferate and become angiogenically quiescent, except in the female genital organs where neovessels are produced monthly during the menstrual cycle (7). The angiogenic process is reactivated in healing wounds (8), but the cellular and molecular mechanisms responsible for activating angiogenesis in injured tissues remain to be elucidated.
We have used ex vivo cultures of rat aortic rings to study the angiogenic mechanisms operating in the isolated vessel wall following mechanical injury. Rings of rat aorta embedded in collagen gels and cultured in serum-free medium produce a self-limited angiogenic response that is triggered by the wound of the dissection procedure (9,10). The angiogenic response of the aortic wall is preceded by upregulated expression of immune related genes including many inflammatory cytokines and chemokines which stimulate angiogenesis and macrophage efflux when added as recombinant molecules to the cultures (11). Among these are the CXC chemokines GRO-1 and MIP-2 which bind to and activate CXCR2, a G-protein coupled receptor that has been shown to transduce signals for cell proliferation and migration during angiogenesis, atherosclerosis, and wound healing (12–15). These findings suggest that the immune system is actively involved in the early stages of vessel formation during angiogenesis.
In this paper we studied the role of resident macrophages and the macrophage associated receptor CXCR2 in the rat aorta model of angiogenesis. Our results show that CXCR2 is an important transducer of angiogenic signals in this system and demonstrate that adventitial macrophages are required for the angiogenic response of the wounded aorta.
Materials and Methods
Preparation and Treatment of Aortic Ring Cultures
All animal procedures were performed with approval from the Veterans Administration Puget Sound Health Care System institutional animal care and use committee and according to NIH guidelines. Thoracic aortas were dissected from CO2 euthanized 1–2 month-old Fischer 344 male rats (Harlan, Indianapolis, IN), C57/Bl6 mice, mice deficient for CXCR2, CD11bDTR transgenic mice (Charles Alpers, U. Washington, Seattle, WA; originally developed from Richard Lang, U. Cincinnati, Cincinnati, OH) or age matched controls (Jackson Labs, Bar Harbor, ME). Aortas were cleaned of fibroadipose tissue and blood, and serially cross-sectioned into 1–2 mm rings as described (9). Angiogenically quiescent rat aortic rings were prepared by pre-incubation in serum free endothelial basal medium (EBM; Lonza, Walkersville, MD) as reported (10,16).
Aortic rings were embedded in collagen gel and cultured in 4-well dishes in serum-free EBM with or without cytokines and chemokines. The following cytokines and chemokines were added as a cocktail: growth related oncogene alpha (GRO-1/CXCL1),10 ng/ml, (Cedar Lane Labs, Hornby, Ontario, Canada); Interleukin-1 beta (IL-1β), 10 ng/ml, (Biosource International, Camarillo, CA); MIP-1 alpha, 10 ng/ml, (Biosource International); TNF alpha, 10 ng/ml, (R&D Systems, Minneapolis, MN); MIP-2, 50 ng/ml, (AbD Serotech, Raleigh, NC). The anti-inflammatory cytokines IL-4 and IL-13 (R&D Systems) were added individually in separate experiments. Negative control cultures were incubated in serum free EBM alone; positive controls were stimulated with 10 ng/ml recombinant VEGF (R&D Systems).
For CSF-1 stimulation studies, 10 mm long segments of rat aorta were preincubated for 24 hours in EBM containing 1 µg/ml recombinant rat M-CSF (CSF-1, PeproTech, Rocky Hill, NJ) prior to cutting individual rings. For blocking studies with antibodies against CSF-1, Rat anti-mouse anti-CSF-1 monoclonal (10 µg/ml; BD Pharmingen, San Diego, CA) was used to treat cultures of C57/Bl6 mouse aortic rings. Control cultures were treated with non-immune IgG (10 µg/ml).
In separate experiments, rat aortic cultures were treated with SB225002 (Calbiochem-EMD Biosciences, San Diego, CA), a CXCR2 receptor chemical inhibitor (17), in the absence or presence of VEGF or the cytokine cocktail. All treatments were started from the beginning of the experiment. Controls for SB225002 experiments were supplemented with DMSO vehicle.
For macrophage ablation experiments, rat aortic rings were pretreated with liposomal clodronate, which selectively kills macrophages (18). Liposomes containing either dichloromethylene diphosphonate (Cl2MDP, clodronate, a gift of Roche Diagnostics GmbH, Mannheim, Germany) or phosphate buffered saline (PBS) were prepared as described (18). Aortic rings were incubated on a rotating shaker with either 10% PBS–liposomes, 10% clodronate–liposomes (diluted in EBM), or EBM alone. After 24 hrs, rings were washed twice for 1 hour in EBM, embedded in collagen, and cultured for 10–14 days (9).
For macrophage ablation experiments with the CD11bDTR mouse model (19), aortic rings from transgenic mice or age matched controls were incubated overnight in either serum free EBM or EBM containing 100 ng/ml diphtheria toxin (List Biological, Campbell, CA). After 24 hours, aortic rings were washed in EBM and cultured as described above. Since the mouse aorta has a lower capacity to sprout spontaneously than the rat aorta due to its smaller size, mouse aortic rings were cultured in 96-well plates to obtain higher concentrations of endogenously released VEGF and other angiogenic factors.
For aortic ring-macrophage co-culture experiments, macrophages were isolated from rat femur and cultured for 6 days in RPMI 1640 (Invitrogen, Carlsbad, CA) with 10% fetal bovine serum, penicillin (100 U/ml), streptomycin (100 µg/ml), L-glutamine (2 mM), and 50 ng/ml recombinant human monocyte colony-stimulating factor (CSF-1, PeproTech). Bone marrow derived macrophages were lifted from tissue culture plates using ice cold PBS with 2 mM EDTA, washed, counted, and added to collagen gel cultures of clodronate-treated or control aortas at the concentration of 40,000 cells per aortic ring. Bone marrow macrophage preparations were determined to be greater than 95% CD45+ by FACS analysis (not shown).
For all collagen gel cultures of aorta, the angiogenic response was measured in living cultures by counting the number of neovessels over time, according to published criteria (9). At the end of the experiments, cultures were fixed in buffered formalin and processed for immunostaining.
In vivo aortic ring angiogenesis assay
Clodronate liposome- or PBS liposome-treated rat aortic rings were prepared as described above. Aortic rings were then embedded in collagen gels cast in gelatin sponge rings (Gelfoam, Pharmacia, Kalamazoo, MI) as reported (20). Recipient syngeneic animals were anesthetized with isoflurane in oxygen. A subcutaneous pouch was formed on the lateral dorsal skin on either side of recipient animals and a single aortic ring/collagen construct was inserted into each pouch.
Implants were removed after 14 days for quantification of angiogenesis. After excision, each implant was frozen in O.C.T. compound (Sakura, Torrance, CA), and serially cryosectioned. Expression of cell markers was evaluated on 8 µm frozen sections immunostained with an anti-CD31 mouse monoclonal antibody (BD-Pharmingen), followed by biotinylated secondary antibody and standard avidin-biotin complex-peroxidase method with 3,3’-diaminobenzidine as the chromogen (ABC kit, Vector Laboratories, Burlingame, CA). Following immunostaining, microvessel counts were performed on five 40X fields selected from the most vascularized areas of three sections in the central region of each implant.
Immunofluorescence Staining and Confocal Microscopy
Expression of proteins of interest in angiogenic outgrowths was evaluated in whole mount preparations of formalin-fixed thin prep cultures using double fluorescence staining (21). Cultures were reacted with either the Alexa Fluor 568-conjugated I-B4 endothelial cell marker (Invitrogen) or the anti-leukocyte/macrophage markers CD45, CD68, CD163 mouse monoclonal antibodies (AbD Serotech), together with a rabbit polyclonal antibody against CXCR2 (Abcam, Cambridge, MA) followed by Alexa Fluor 488-conjugated goat anti-rabbit and Alexa Fluor 568-conjugated goat anti-mouse secondaries. All cultures were stained with 50 ng/ml DAPI (Sigma, St. Louis, MO) for 5 minutes to visualize nuclei.
Peroxidase based immunostaining was performed on en face preparations of whole aortas using mouse anti-rat CD45 (AbD Serotech) or mouse anti-rat CD163 (AbD Serotech) antibodies followed by biotinylated secondary antibodies (Vector Laboratories) and standard avidin-biotin complex-peroxidase method with 3,3’-diaminobenzidine as the chromogen (Vector Laboratories). Immunostained samples were mounted in Aqua Polymount (Polysciences, Warrington, PA) on glass slides.
Images were taken with either a Leica TCS-SP laser scanning confocal microscope or an Olympus BX41 microscope equipped with an Optronics MicroFire SE digital camera. Confocal images were obtained by Z-plane analysis followed by projection and overlay using Leica software.
Real Time PCR analysis
Total RNA was isolated from three to six freshly isolated or quiescent rat aortic rings after snap freezing in liquid nitrogen and manual pulverization. RNA was extracted with Trizol® reagent (Invitrogen) followed by further purification with the RNAEasy Micro kit (Qiagen, Valencia, CA). To examine the relative expression of CXCR2, we used the two-step qRT-PCR SYBR Green method (Applied Biosystems, Foster City, CA). Random primed reverse transcription (RT) was carried out with 100 ng RNA and Superscript™ III Reverse Transcriptase (Invitrogen). 1/50 of the final RT reaction was used as template in qRT-PCR reactions containing oligonucleotide primers (Invitrogen). Primers for CXCR2 were 5-GCACGCTCTTTAAGGCCCAC AT-3’ and 5’-GTTAATCTCGT TCTGGCGTTCACA-3’ and for β-Actin were 5’-GGGAAATCGT GCGTGACATT-3’ and 5’-GCGGCAGTGGCCATCTC-3’. Each primer set produced a single product, as determined by melt-curve analysis. Relative quantification was carried out on an ABI 7000 thermal cycler (Applied Biosystems) in reactions containing 1× Universal SYBR green Master Mix (Applied Biosystems), 300 nM forward and reverse primers, and 5 µl cDNA template. The PCR cycling profile was: 2 min at 50°C, 10 min at 95°C followed by 35 cycles of 95°C for 15 s, 60°C for 1 min. Each PCR reaction was carried out in triplicate. qRT-PCR data were analyzed with Prizm software (Applied Biosystems). Relative ratios of fluorescent intensities of products from each treatment group were calculated by using the 2–ΔΔCt method (22). The mRNA expression levels of each sample were normalized to the levels of β-Actin expression measured in the same sample.
ELISA
An ELISA kit (R & D Systems) was used to measure VEGF protein levels in conditioned media according to the instructions of the manufacturer. This Rat ELISA kit can reliably measure concentrations as low as 3 pg/ml. Conditioned media was collected from cultures of freshly isolated or quiescent aortic rings treated with cytokines and compared to conditioned media from untreated controls. All reactions were carried out in triplicate.
Western analysis
Collagen gel cultures of aorta were lysed in 200–500 µl of radioimmuno-precipitation (RIPA) lysis buffer (50 mM Tris, 150 mM NaCl, 0.1% SDS, 1% NP-40, 1 mM EDTA containing a complete protease inhibitor mixture, Roche). Cell lysates were loaded on SDS-polyacrylamide Ready-gels (Bio-Rad Laboratories, Hercules, CA) and transferred to nitrocellulose membranes which were incubated with specific anti-CD45 (AbD Serotech) or anti-CD163 (AbD Serotech) antibodies. The antibodies were detected by appropriate horseradish peroxidase-conjugated secondary antibodies (Jackson Labs, West Grove, PA) followed by SuperSignal West Dura Extended Duration chemiluminescence (Pierce Endogen, Rockford, IL). Chemiluminescent images were recorded using a Chemidoc XRS CCD gel imaging system and Quantity One Software (Bio-Rad). To control for loading and transfer of proteins, blots were stripped and reprobed with anti-β-actin antibody (Sigma). A protein extract (10 µg / lane) of rat thymus was used as a positive control for both CD45 and CD163.
Statistical studies
Quantitative data from both in vitro and in vivo experiments were analyzed by ANOVA followed by Neumann-Keuls post test using Prism software (Graph Pad, Inc. San Diego, CA). Statistical significance between experimental groups was set at P < 0.05.
Results
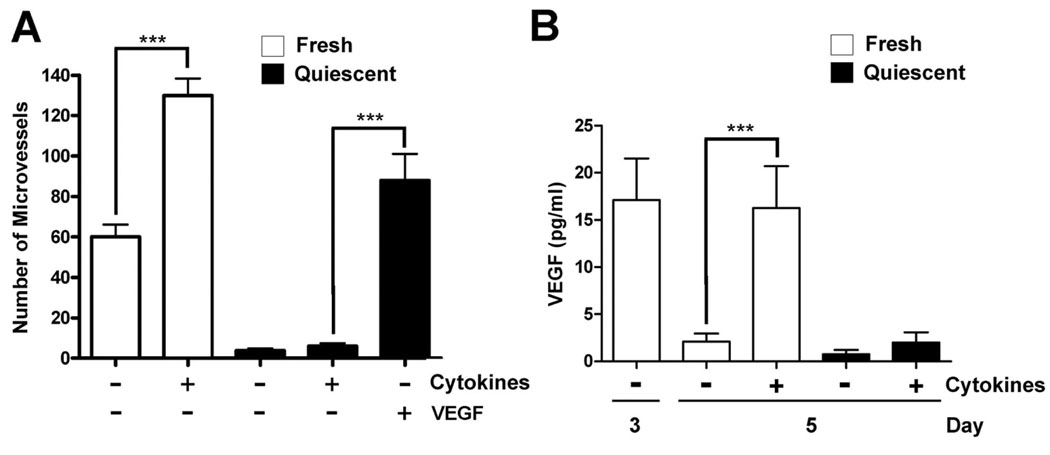
The rat aorta loses angiogenic activity and fails to respond to inflammatory cytokines in culture over time
We previously reported that aortic rings treated with VEGF or Ang-1 produced many inflammatory cytokines and chemokines including GRO-1, MIP-2, MIP-1α, IL-1β and TNFα (11). A cocktail of these factors enhanced the spontaneous angiogenic response of freshly cut aortic rings in collagen gel cultures, and synergized with low dose VEGF whereas treatment with individual cytokines and chemokines had no detectable stimulatory effects (11). To evaluate the capacity of this cytokine/chemokine cocktail to induce angiogenesis, we used a modification of the aortic ring assay in which aortic explants were made quiescent by a 13-day preincubation step in tri-weekly changes of serum-free medium prior to collagen embedding. Following this treatment, aortic rings lost their capacity to sprout spontaneously but remained responsive to angiogenic inducers such as VEGF (16). In contrast to its proangiogenic effect on freshly cut rings, the cytokine/chemokine cocktail failed to stimulate angiogenesis in cultures of quiescent aortic rings (Fig. 1A). In addition, quiescent rings produced significantly less VEGF than freshly cut rings, spontaneously or in response to the cytokine/chemokine cocktail (Fig. 1B). Quiescent rings also exhibited a significantly reduced angiogenic response to re-injury, following secondary surgical transection of their previously cut ends (not shown). Thus, aortic rings became refractory to proangiogenic inflammatory cytokines and hyporesponsive to injury upon induction of quiescence.
FIGURE 1.
Changes in spontaneous and inflammatory cytokine-mediated angiogenesis in rat aortic cultures over time. A: Inflammatory cytokines stimulate angiogenesis in collagen gel cultures of freshly cut aortic rings but have no effect on rings embedded in collagen 13 days following excision (quiescent rings). Quiescent aortic rings are viable and respond to angiogenic stimulation by VEGF. *** = P < 0.001; n = 8. B: VEGF levels in cultures of freshly cut aortic rings are maximal soon after injury and decline over time. Inflammatory cytokines stimulate VEGF production in collagen gel cultures of freshly cut rings (day 5) but have no effect on quiescent rings. *** = P < 0.001; n = 3.
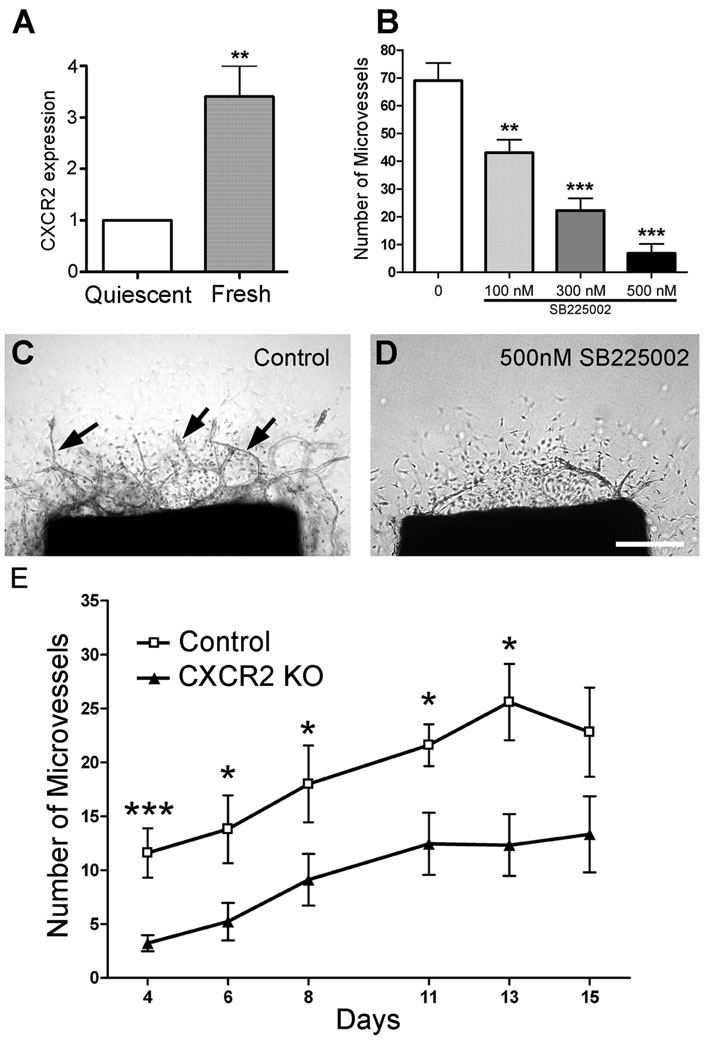
The inability of quiescent aortic rings to sprout correlates with reduced expression and function of CXCR2
To evaluate whether the inability of aortic rings to respond to the cytokine/chemokine cocktail following induction of quiescence was related to transcriptional changes in cytokine or chemokine receptors, we performed mRNA expression studies in fresh and quiescent aortic rings. These studies showed that the CXCR2 gene, which encodes for the GRO-1 and MIP-2 receptor, was expressed 3.5 fold more in fresh than in quiescent rings (Fig. 2A). In contrast, the individual receptor genes for the other components of the cytokine/chemokine cocktail (CCR1, CCR5, TNFα-R 1 and 2, IL1Rα and β) did not have reduced expression in quiescent rings (not shown). These results suggested that the inability of the quiescent rings to spontaneously produce neovessels was related to reduced expression of CXCR2. In keeping with these observations, treatment with the CXCR2 inhibitor SB225002 dose-dependently blocked the spontaneous angiogenic response of freshly cut aortic rings (Fig. 2 B and D), and completely abrogated the stimulatory effect of the cytokine/chemokine cocktail in these cultures. The SB225002 effect was not due to toxicity because treated aortic rings responded to VEGF after removal of the inhibitor (not shown). In addition, removal of the CXCR2 ligands GRO-1 and MIP-2 from the cytokine cocktail abolished its proangiogenic activity (11).
FIGURE 2.
Expression and function of CXCR2 in aortic ring model of angiogenesis. A: The relative expression of CXCR2 measured by quantitative RT-PCR is 3.5 fold higher in freshly cut rat aortic rings compared to quiescent rings; ** = P < 0.01; n = 3. B: The angiogenic response of freshly cut rat aortic rings is dose dependently blocked by a CXCR2 inhibitor (SB225002); ** = P < 0.01; *** = P < 0.001; n = 5. C and D: Images of control (C) and SB225002-treated (D) aortic cultures; neovessels are marked by arrows, scale bar = 200 µm. E: Angiogenesis in aortic ring cultures from CXCR2 deficient mice is significantly reduced compared to control cultures. ** = P < 0.01 *** P < 0.001, n = 9.
Cultures of aortic rings from genetically modified mice with disrupted CXCR2 showed a 50–70% reduction of angiogenic sprouting. This difference was particularly pronounced during the early stages of angiogenesis, and was maintained at significant levels throughout the two-week long experiment (Fig. 2E).
Taken together these findings implicated CXCR2 as an important angiogenic regulator in the aortic cultures, and revealed a close relationship between angiogenic quiescence, inability of quiescent rings to respond to inflammatory cytokines, and reduced expression or function of CXCR2.
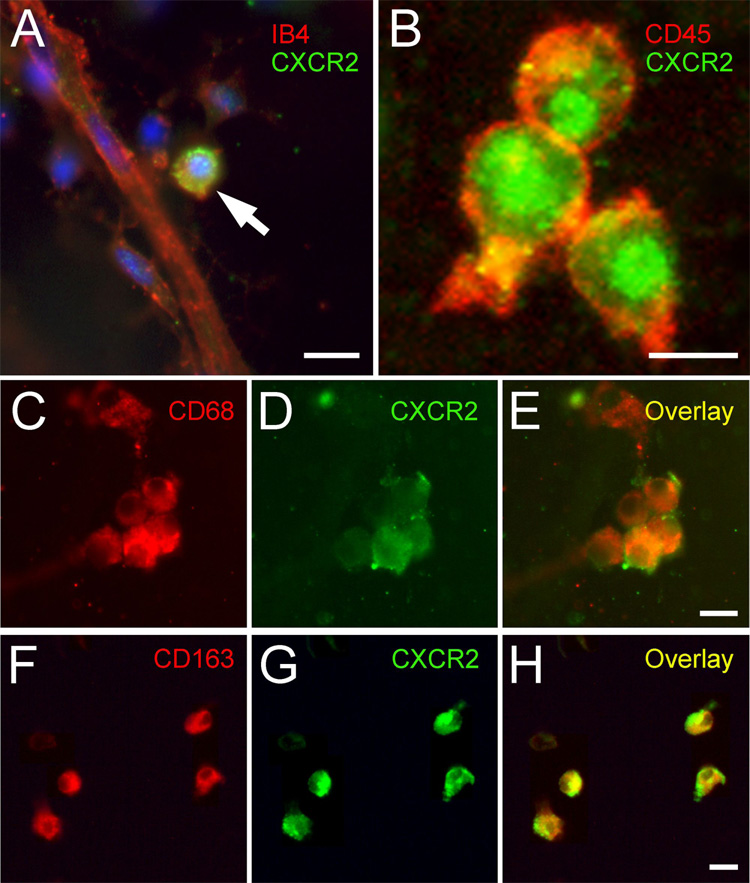
CXCR2 is highly expressed in macrophages associated with angiogenic outgrowths
To identify the cells types that express CXCR2, aortic cultures were immunostained for CXCR2 and specific markers of cell differentiation. Although endothelial cells and pericytes stained for CXCR2, macrophages had the strongest staining for this receptor. The CXCR2-positive macrophages were found around sprouting neovessels, and were particularly abundant at the root of the vascular outgrowths, near the aortic explants (Fig. 3).
FIGURE 3.
Immunocytochemical localization of CXCR2 in aortic cultures. A: Immunofluorescent staining of angiogenic outgrowth from cultured rat aortic ring shows expression of CXCR2 (green) in a round cell (arrow) next to a neovessel highlighted with the endothelial marker IB4 (red); nuclei are stained with DAPI (blue). B: Confocal image shows coexpression of CXCR2 (green, perinuclear staining) with the leukocyte marker CD45 (red) in small cluster of round cells found close to the roots of the angiogenic outgrowth, near the aortic explant. C–H: Double immunofluorescent staining of aortic cultures for CD68 (C, red) or CD163 (F, red) and CXCR2 (D, G green), demonstrates co-localization of CXCR2 in macrophages (overlays in E and H). Scale bars = 10 µm.
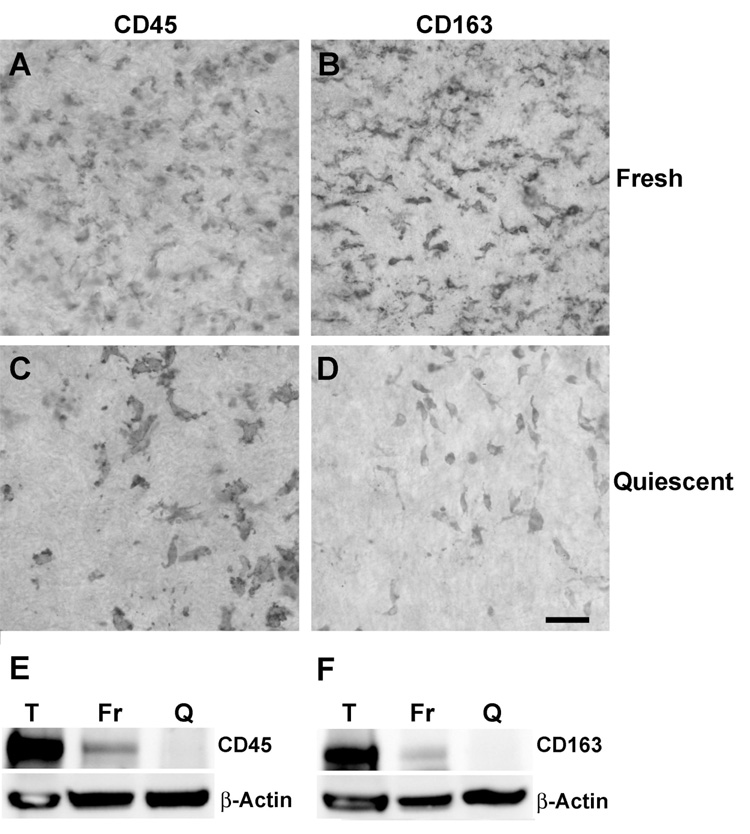
Angiogenic quiescence and reduced VEGF production in cultured aortic rings is associated with loss of adventitial macrophages
Our studies on inflammatory cytokines and CXCR2 implicated the adventitial-derived macrophages as potential regulators of angiogenesis in the aortic ring model. They also suggested that changes occurring over time in the aorta-associated innate immune system might be responsible for the development of angiogenic quiescence in cultured aortic rings. Immunohistochemical studies of whole mount preparations of aortic rings showed marked depletion of macrophages in quiescent aortic rings compared to freshly cut rings (Fig. 4). Loss of macrophages correlated with markedly reduced VEGF production by these rings (Fig. 1B). Endothelial cells of quiescent rings were intact as demonstrated by their robust angiogenic response to VEGF (Fig. 1A). Thus, changes associated with the development of quiescence in the aortic rings, i.e. loss of spontaneous angiogenic activity, failure to respond to inflammatory cytokines, reduced production of VEGF, and decreased expression of CXCR2, all correlated with the gradual disappearance of macrophages from the aortic explants.
FIGURE 4.
Angiogenically quiescent rat aortic rings are depleted of macrophages. A–D: En face images of the adventitial surface of freshly isolated (A, B) and quiescent (C, D) aortas stained by the immunoperoxidase method for the leukocyte marker CD45 (A, C) and the macrophage-specific marker CD163 (B, D). Staining for both markers shows marked depletion of macrophages in quiescent rings compared to fresh rings. Scale bar = 50 µm. E–F: Western analysis of protein expression in fresh (Fr) and quiescent (Q) aortas demonstrates that CD45 and CD163 are reduced in quiescent rings as compared to fresh rings. T= thymus positive control. A probe for β-actin was used on the same blot as loading control.
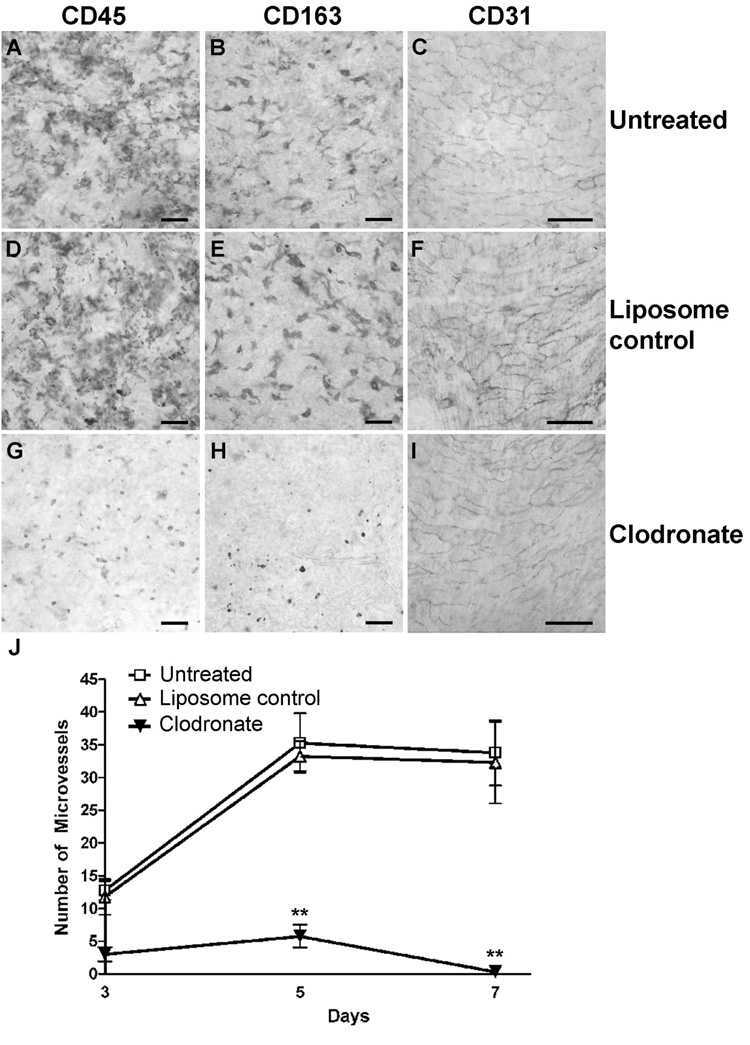
Pharmacologic ablation of macrophages abrogates the spontaneous angiogenic response of fresh aortic rings in vitro and reduces aortic ring induced angiogenesis in vivo
To further investigate the angiogenic role of resident adventitial macrophages, aortic rings were treated with liposomal clodronate, a liposome-encapsulated biphosphonate compound that is phagocytosed by macrophages and accumulates intracellularly, leading to their elimination by apoptosis (23).
Selective depletion of macrophages from the aortic wall following overnight incubation in clodronate was confirmed by immunohistochemistry. Specifically, the clodronate treatment depleted aortic rings of macrophages while leaving the intimal endothelial cells intact (Fig. 5). Loss of macrophages resulted in a ~70 % reduction in VEGF production, from 26 pg/ml to 7 pg/ml. When cultured in collagen gels, clodronate-treated rings exhibited a markedly reduced angiogenic response whereas aortic rings treated with the liposome vehicle behaved as the untreated control (Fig. 5J).
FIGURE 5.
Depletion of macrophages with liposomal clodronate abrogates angiogenesis in rat aortic cultures. A–I: En face images of the adventitial (A, B, D, E, G, H) and intimal (C, F, I) surfaces of freshly isolated aortic rings, left untreated (A–C), treated with empty liposomes (D–F) or liposomal clodronate (G–I), and stained by immunoperoxidase for the leukocyte marker CD45 (A, D, G), the macrophage marker CD163 (B, E, H), or the endothelial cell marker CD31 (C, F, I). Note: liposomal clodronate depletes the aortic adventitia of resident macrophages (G, H) but has no effect on intimal endothelial cells (I), which display an intact cobblestone pattern comparable to controls (C, F). Scale bar = 50 µm. (J) Liposomal clodronate treatment inhibits angiogenesis in cultures of freshly isolated aortic rings. ** = P < 0.01; n = 4.
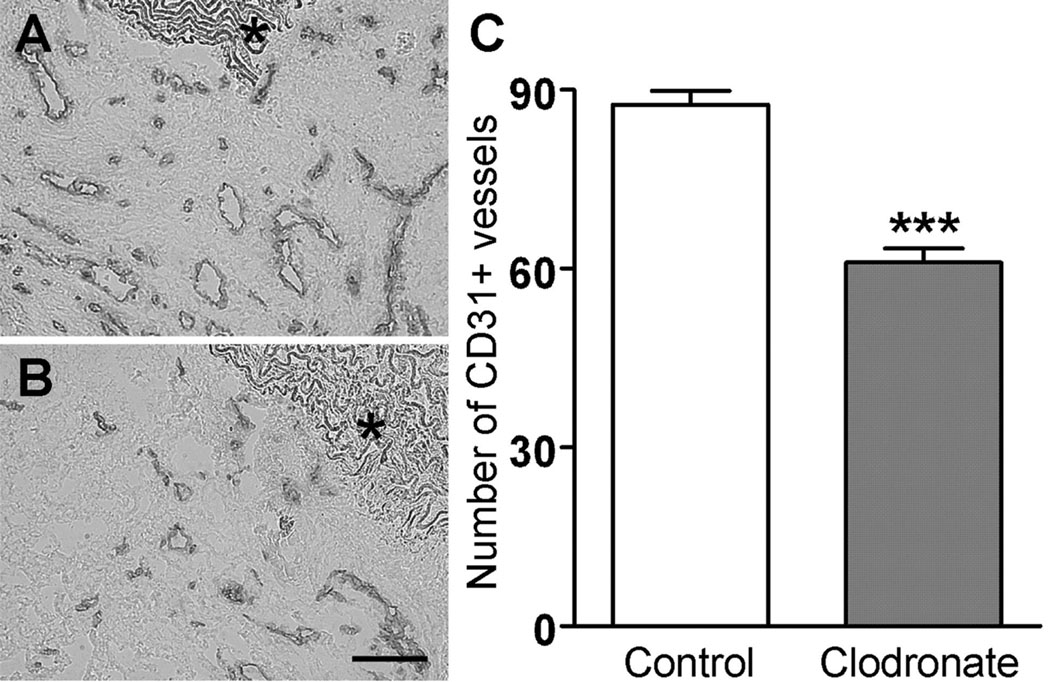
The effect of clodronate-mediated macrophage depletion on the angiogenic properties of the aortic wall was also evaluated in a newly developed in vivo model of aortic ring-induced angiogenesis (20). Subcutaneously implanted aortic rings embedded in collagen/Gelfoam stimulated a florid angiogenic response (20). Newly formed vessels invaded and penetrated deeply into the implants, resulting in extensive vascularization of the periaortic collagen and the aortic lumen by day 14. This angiogenic response was reduced by 30% in implants containing aortic rings that had been depleted of macrophages by clodronate treatment prior to the implant procedure (Fig. 6). Thus, pharmacologic ablation of aortic macrophages significantly hampered the angiogenic response of the aortic wall.
FIGURE 6.
Depletion of macrophages with liposomal clodronate reduces aortic ring induced angiogenesis in vivo. Representative frozen sections of subcutaneous implants from control (A) and clodronate treated (B) rat aortic rings immunostained for CD31 to demonstrate microvessels. Vessels appear in the region surrounding implanted aorta. Aortic wall is marked by asterisks. Scale bar = 100 µm. Quantitative analysis of microvascular density is shown in C. *** = P < 0.0001; n = 53.
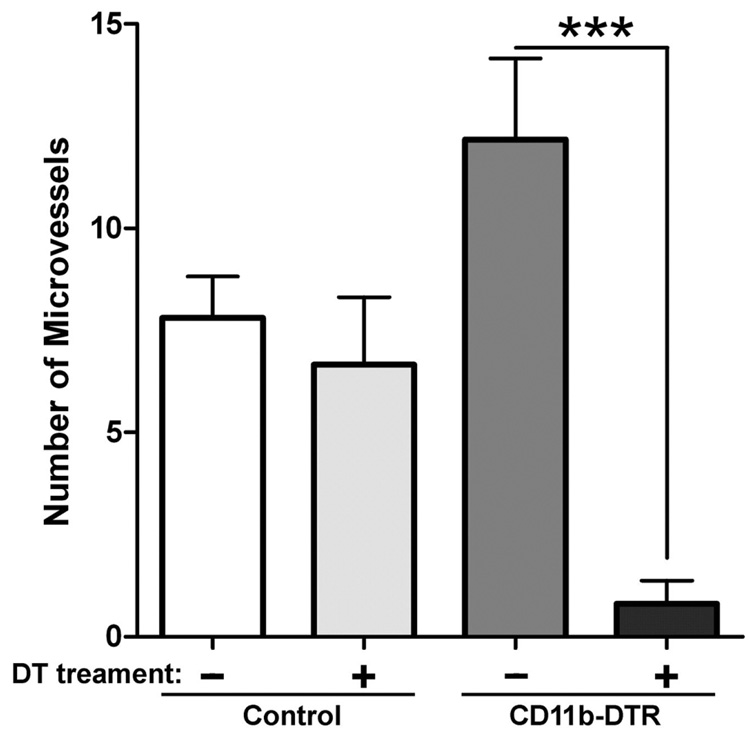
To further validate this conclusion we selectively ablated macrophages in cultures of aortic rings from CD11bDTR mice. These mice harbor a transgene that renders macrophages susceptible to cell death upon exposure to diphtheria toxin to which normal mouse cells are otherwise resistant (19). Diphtheria toxin treatment of rings from CD11bDTR mice caused a 94% reduction of angiogenic sprouting when compared to age matched untreated CD11bDTR aortic rings. Diphtheria toxin treatment of non-transgenic control animals had no effect on angiogenic sprouting (Fig. 7).
FIGURE 7.
The angiogenic response of aortic rings from CD11bDTR transgenic mice is markedly impaired following treatment with diphtheria toxin. The number of microvessels in these cultures is reduced by 94% compared to untreated controls. Angiogenesis in cultures of non-transgenic aortic rings is unaffected by the diphtheria toxin treatment. *** = P < 0.001; n = 5.
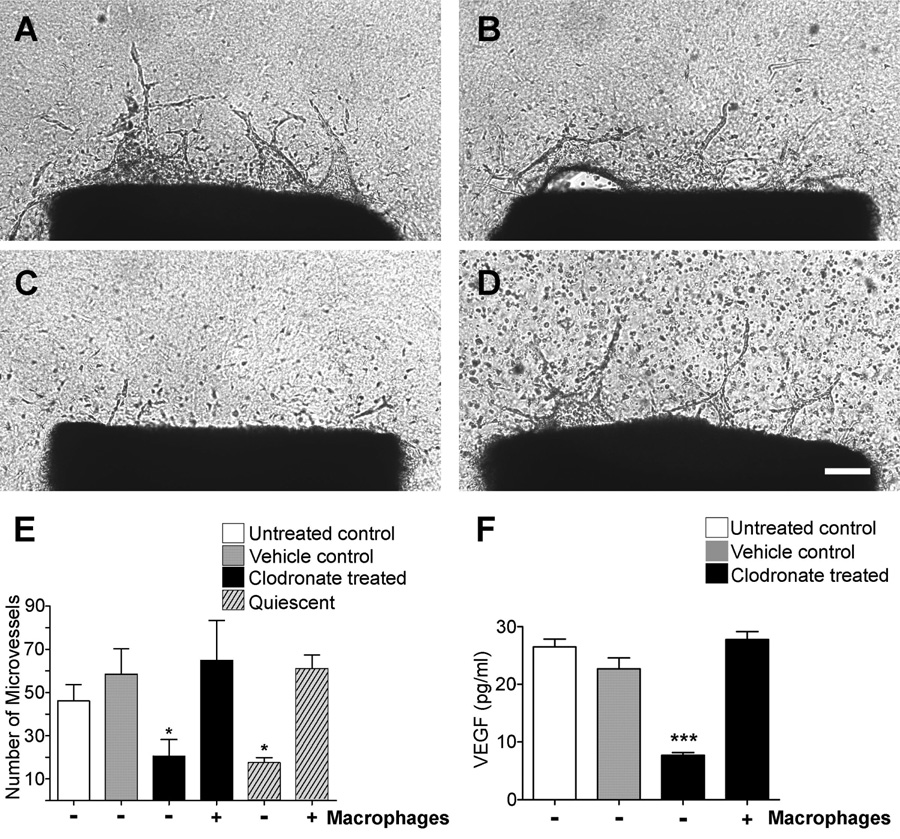
Exogenous macrophages restore the angiogenic response of macrophage-depleted aortic rings
To determine if angiogenic activity following loss of resident macrophages could be restored with exogenous macrophages, macrophage-depleted aortic rings were co-cultured with bone marrow-derived macrophages. Macrophage depletion was obtained spontaneously through induction of quiescence, or pharmacologically through liposomal clodronate treatment. Bone marrow-derived macrophages co-embedded with aortic rings in collagen gels markedly stimulated angiogenesis from both quiescent and clodronate-treated rings (Fig. 8). As a result, the angiogenic response of macrophage-depleted aortic rings was restored to values comparable to those of fresh rings replete with macrophages. Concurrently, VEGF levels were significantly increased by the addition of exogenous macrophages (Fig. 8F).
FIGURE 8.
Bone marrow-derived macrophages restore angiogenesis in collagen gel cultures of clodronate-treated rat aortic rings. A–D: Aortic ring cultures left untreated (A), treated with empty liposomes (B), or treated with liposomal clodronate and then cultured without (C) or with (D) rat bone marrow-derived macrophages (scale bar = 200 µm). Exogenous macrophages embedded in collagen restore the angiogenic response of clodronate-treated or quiescent rings to normal values (D, E: * = P < 0.05; n = 7). The proangiogenic effect of macrophages is associated with a corresponding increase in VEGF levels (F: *** = P < 0.001; n = 7).
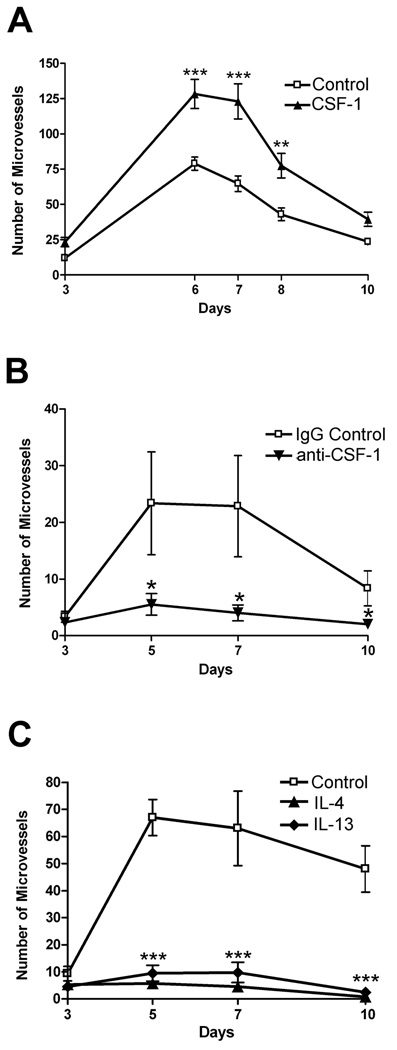
To further substantiate the contribution of the innate immune system to the angiogenic response of the aorta we performed experiments with CSF-1, a potent activator of macrophage function (24). Pretreatment of rat aortas overnight with CSF-1 enhanced the angiogenic response of aortic rings by 162% at the peak of growth (Fig 9A). Conversely antibody-mediated blockade of CSF-1 function resulted in a 77% reduction in the number of sprouting neovessels by day 5 (Fig 9B). Mouse rather than rat aortic ring cultures were used for blocking antibody experiments due to the lack of suitable anti-rat CSF-1 neutralizing antibody. The angiogenic response of aortic rings was also potently inhibited with the anti-inflammatory cytokines interleukin 4 and 13 (Fig 9C).
FIGURE 9.
Modulation of aortic angiogenesis by CSF-1, IL-4 and IL-13. A: The angiogenic response of aortic rings to injury is stimulated by recombinant CSF-1. B: Angiogenesis in cultures of mouse aortic rings is inhibited by a neutralizing anti-CSF-1 antibody. C: The angiogenic response of rat aortic rings is strongly inhibited by the anti-inflammatory cytokines IL-4 and IL-13. * = P < 0.05; ** = P < 0.01; *** = P < 0.001; n = 4.
Discussion
Isolated rat aortic explants have an intrinsic capacity to produce neovessels under serum-free conditions and in the absence of exogenous angiogenic factors. This process is activated by injury and potentiated by inflammatory cytokines (9–11). In this paper we demonstrate that this angiogenic response requires adventitial macrophages. Our conclusion is based on the following observations: 1. The rat aorta becomes angiogenically quiescent and fails to respond to inflammatory cytokines in culture over time. 2. Quiescent aortic rings are unable to produce VEGF spontaneously or in response to inflammatory cytokines. 3. Failure of quiescent aortic rings to sprout correlates with reduced expression of CXCR2, a macrophage associated chemokine receptor that promotes aortic angiogenesis. 4. Angiogenic quiescence in cultured aortic rings is associated with spontaneous depletion of adventitial macrophages. 5. Selective pharmacologic ablation of macrophages obtained with liposomal clodronate abrogates the spontaneous angiogenic response of fresh aortic rings ex vivo, and reduces aortic ring induced angiogenesis in vivo. 6. Depletion of macrophages with diphtheria toxin in aortic cultures from CD11b-DTR transgenic mice results in markedly reduced angiogenesis 7. Exogenous macrophages restore the angiogenic response of macrophage depleted aortic rings. 8. The angiogenic response of the aorta is promoted by stimulating macrophages with CSF-1 and inhibited by blocking endogenous CSF-1 with a neutralizing antibody.
We first hypothesized that the innate immune system regulates angiogenesis in the rat aorta assay based on a microarray study that showed upregulated expression of numerous immune-related genes in response to recombinant VEGF or Ang-1 (11). Among these genes were many immune-related cytokines and chemokines including GRO-1 and MIP-2, which bind to CXCR2, a G-coupled receptor that has been implicated in inflammatory angiogenesis (12–14). Since the induction of immune-related genes occurred prior to angiogenic sprouting, we reasoned that aorta-associated immune cells were involved in the early stages of the angiogenic response (11). Immunohistochemical studies showed that the aortic adventitia contains a rich population of CD45+, CD68+, and CD163+ macrophages, which become associated with the angiogenic outgrowths. The additional observation that a cocktail of inflammatory cytokines that were overexpressed in response to both Ang-1 and VEGF enhanced both angiogenesis and macrophage migration further supported the hypothesis that activation of the aortic immune system promoted angiogenesis in the aortic assay. In the present study we demonstrate that resident macrophages are required for the angiogenic response to injury and inflammatory cytokines.
We previously reported that angiogenic sprouting in aortic ring cultures is in part regulated by endogenous VEGF, and that an anti-VEGF neutralizing antibody significantly inhibited angiogenesis (16). Our current study demonstrates that resident macrophages of the aortic wall are an important source of VEGF. In fact, VEGF levels are significantly reduced in cultures of macrophage-depleted rings and become markedly elevated upon addition of exogenous macrophages. In addition to VEGF, macrophages release proangiogenic factors such as bFGF and TNF-α (25), which are part of the endogenous stimuli that contribute to the angiogenic response of the aortic cultures (11,26).
Our observation that macrophages play a key role during the early stages of aortic angiogenesis ex vivo supports the idea that these cells generate critical signals for angiogenic induction during wound healing and pathologic processes (27–30). Our results also provide a mechanistic explanation for the role of the adventitial layer in aortic angiogenesis and identify the macrophage as the requisite adventitial component that provides proangiogenic signals to the endothelium of the aortic wall. This interpretation corroborates a previous study indicating that the angiogenic response of isolated aortic explants requires an intact adventitia (31).
Of particular interest in this study was the observation that angiogenesis could be inhibited by blocking CXCR2, or through genetic disruption of this receptor, and that expression of CXCR2 directly correlated with both the angiogenic response and the presence of macrophages in the aortic explants. Our studies with a cytokine cocktail containing the CXCR2 ligands GRO-1 and MIP-2 indicate that stimulation of CXCR2 signaling contributes to a robust angiogenic response but is insufficient to induce angiogenesis in cultures of quiescent aortic rings which are macrophage-depleted and lack significant production of VEGF. These findings corroborate and expand our previous observation that the cytokine cocktail stimulates aortic angiogenesis and synergistically potentiates the angiogenic effect of VEGF. They are also in keeping with previous reports that CXCR2 and its ligands play an important role in wound healing (15) and tumor angiogenesis (32,33). The additional observation reported in this paper that aorta-associated CXCR2 is predominantly expressed in macrophages implicates the innate immune system of the aortic wall as a critical early regulator of angiogenesis. This conclusion is further substantiated by experiments showing that treatment with CSF-1, a macrophage stimulatory factor (34), significantly enhanced aortic angiogenesis whereas an anti-CSF-1 antibody markedly inhibited angiogenic sprouting. These results are consistent with previous reports indicating that CSF-1 stimulates VEGF production and angiogenesis (35–37).
The demonstration that VEGF levels in aortic ring cultures are markedly reduced following macrophage depletion and are restored to control values by addition of exogenous macrophages implicates these cells as the major producer of VEGF in the system. Recombinant VEGF upregulates the expression of GRO-1 and MIP-2 (11), which working in concert with other inflammatory cytokines stimulate in turn VEGF expression. On this basis we hypothesize that the angiogenic response of the rat aorta is mediated by a macrophage-driven cascade of cytokine production including VEGF and the CXCR2 ligands GRO-1 and MIP-2. These factors synergistically stimulate each other’s production through a positive feed back mechanism of transcriptional regulation. Macrophage depletion impairs this system by removing the key producers of these pro-angiogenic molecules. Inflammatory cytokines alone do not rescue angiogenesis from quiescent aortic rings because of the lack of sufficient number of VEGF-producing macrophages. This deficiency can be rectified by adding exogenous VEGF at higher doses than would otherwise be required in the presence of a fully functioning innate immune system (16) or by coculturing quiescent rings with bone marrow-derived macrophages. The capacity of exogenous macrophages to stimulate angiogenesis is based on their ability to produce a wide array of angiogenic growth factors including VEGF and cytokines which act synergistically to stimulate vessel sprouting (11). Exogenous macrophages also restore CXCR2 signaling which is otherwise impaired in quiescent ring cultures.
The finding that IL-4 and IL-13 potently inhibit the angiogenic response of rat aortic rings corroborates the idea that the innate immune system of the aortic adventitia is required for the initiation of angiogenesis in response to injury. These interleukins have previously been shown to polarize macrophages to an M2 phenotype which has been associated with stimulation of tissue repair and angiogenesis (38). IL-4 and IL-13 have also been reported to inhibit angiogenesis ex vivo and in vivo (39–43). These seemingly conflicting results may be related to the ability of macrophages to modulate their behavior and responsiveness to cytokines based on contextual cues. One possible explanation for the anti-angiogenic activity of these interleukins in the rat aorta model is that the pro-inflammatory activity of macrophages needed for induction of angiogenesis is blocked by IL-4 and IL-13 (44). It is also possible that IL-4 and IL-13 directly inhibit migration of endothelial cells (39). In addition, these interleukins have been reported to induce the formation of a dendritic cell subtype with anti-angiogenic properties (45).
In vivo studies with experimental animal models have shown that exogenous macrophages greatly potentiate tumor angiogenesis (46) while endogenous macrophage depletion markedly reduces it (47,48). Our results confirm these observations in an ex vivo model in which aortic explants have lost adventitial macrophages spontaneously or through pharmacologic treatment. The aortic ring assay has significant advantages over existing in vivo models because it reproduces angiogenesis in a chemically defined environment that can be easily manipulated. We have exploited the unique features of this model to prove that the angiogenic failure in cultures of quiescent or clodronate-treated aortic rings was caused by the loss of macrophages and could be reversed by replenishing the aortic cultures with exogenous macrophages. Interestingly, macrophage depleted aortic rings partially lost their ability to stimulate angiogenesis in vivo when implanted subcutaneously following treatment with liposomal clodronate. The residual angiogenic response in this in vivo model was likely driven by the reaction of the host innate immune system to the aortic ring.
In summary, our studies provide novel insights into the early mechanisms that regulate angiogenesis in the rat aorta model. Angiogenesis in this system is a self-limited process induced by the injury of the dissection procedure. Results presented in this paper demonstrate that adventitial macrophages and their cytokines function as requisite conductors of the angiogenic response to injury. This observation provides the foundation for further studies on macrophage-related sensors and molecular triggers that regulate angiogenesis following vascular injury.
Acknowledgments
Supported by National Heart, Lung, and Blood Institute Grant HL52585 and by a Merit Review Grant from the Department of Veterans Affairs Medical Research Service.
Abbreviations
- Ang-1
Angiopoietin-1
- EBM
Endothelial Basal Medium
- GRO-1
growth related oncogene-1
- I-B4
Isolectin-B4
- VEGF
vascular endothelial growth factor
Footnotes
Disclosures
None.
References
- 1.Carmeliet P. Angiogenesis in life, disease and medicine. Nature. 2005;438:932–936. doi: 10.1038/nature04478. [DOI] [PubMed] [Google Scholar]
- 2.Ferrara N. Vascular endothelial growth factor: basic science and clinical progress. Endocr.Rev. 2004;25:581–611. doi: 10.1210/er.2003-0027. [DOI] [PubMed] [Google Scholar]
- 3.Yancopoulos GD, Davis S, Gale NW, Rudge JS, Wiegand SJ, Holash J. Vascular-specific growth factors and blood vessel formation. Nature. 2000;407:242–248. doi: 10.1038/35025215. [DOI] [PubMed] [Google Scholar]
- 4.Gale NW, Thurston G, Davis S, Wiegand SJ, Holash J, Rudge JS, Yancopoulos GD. Complementary and coordinated roles of the VEGFs and angiopoietins during normal and pathologic vascular formation. Cold Spring Harb.Symp.Quant.Biol. 2002;67:267–273. doi: 10.1101/sqb.2002.67.267. [DOI] [PubMed] [Google Scholar]
- 5.Campochiaro PA. Retinal and choroidal neovascularization. J Cell Physiol. 2000;184:301–310. doi: 10.1002/1097-4652(200009)184:3<301::AID-JCP3>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 6.Gerber HP, Ferrara N. Angiogenesis and bone growth. Trends Cardiovasc.Med. 2000;10:223–228. doi: 10.1016/s1050-1738(00)00074-8. [DOI] [PubMed] [Google Scholar]
- 7.Groothuis PG. Angiogenesis and vascular remodelling in female reproductive organs. Angiogenesis. 2005;8:87–88. doi: 10.1007/s10456-005-0391-x. [DOI] [PubMed] [Google Scholar]
- 8.Li J, Zhang YP, Kirsner RS. Angiogenesis in wound repair: angiogenic growth factors and the extracellular matrix. Microsc.Res.Tech. 2003;60:107–114. doi: 10.1002/jemt.10249. [DOI] [PubMed] [Google Scholar]
- 9.Nicosia RF, Ottinetti A. Growth of microvessels in serum-free matrix culture of rat aorta. A quantitative assay of angiogenesis in vitro. Lab Invest. 1990;63:115–122. [PubMed] [Google Scholar]
- 10.Nicosia RF, Zhu WH. Rat Aortic Ring Assay of Angiogenesis. In: Augustin H, editor. Methods in Endothelial Cell Biology. Berlin Heidelberg: Springer-Verlag; 2004. [Google Scholar]
- 11.Aplin AC, Gelati M, Fogel E, Carnevale E, Nicosia RF. Angiopoietin-1 and vascular endothelial growth factor induce expression of inflammatory cytokines before angiogenesis. Physiol Genomics. 2006;27:20–28. doi: 10.1152/physiolgenomics.00048.2006. [DOI] [PubMed] [Google Scholar]
- 12.Addison CL, Daniel TO, Burdick MD, Liu H, Ehlert JE, Xue YY, Buechi L, Walz A, Richmond A, Strieter RM. The CXC chemokine receptor 2, CXCR2, is the putative receptor for ELR+ CXC chemokine-induced angiogenic activity. J Immunol. 2000;165:5269–5277. doi: 10.4049/jimmunol.165.9.5269. [DOI] [PubMed] [Google Scholar]
- 13.Strieter RM, Burdick MD, Mestas J, Gomperts B, Keane MP, Belperio JA. Cancer CXC chemokine networks and tumour angiogenesis. Eur.J Cancer. 2006;42:768–778. doi: 10.1016/j.ejca.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 14.Boisvert WA, Rose DM, Johnson KA, Fuentes ME, Lira SA, Curtiss LK, Terkeltaub RA. Up-regulated expression of the CXCR2 ligand KC/GRO-alpha in atherosclerotic lesions plays a central role in macrophage accumulation and lesion progression. Am J Pathol. 2006;168:1385–1395. doi: 10.2353/ajpath.2006.040748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Devalaraja RM, Nanney LB, Du J, Qian Q, Yu Y, Devalaraja MN, Richmond A. Delayed wound healing in CXCR2 knockout mice. J Invest Dermatol. 2000;115:234–244. doi: 10.1046/j.1523-1747.2000.00034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nicosia RF, Lin YJ, Hazelton D, Qian X. Endogenous regulation of angiogenesis in the rat aorta model. Role of vascular endothelial growth factor. Am.J.Pathol. 1997;151:1379–1386. [PMC free article] [PubMed] [Google Scholar]
- 17.White JR, Lee JM, Young PR, Hertzberg RP, Jurewicz AJ, Chaikin MA, Widdowson K, Foley JJ, Martin LD, Griswold DE, Sarau HM. Identification of a potent, selective non-peptide CXCR2 antagonist that inhibits interleukin-8-induced neutrophil migration. J Biol.Chem. 1998;273:10095–10098. doi: 10.1074/jbc.273.17.10095. [DOI] [PubMed] [Google Scholar]
- 18.Van Rooijen N, Sanders A. Liposome mediated depletion of macrophages: mechanism of action, preparation of liposomes and applications. J Immunol.Methods. 1994;174:83–93. doi: 10.1016/0022-1759(94)90012-4. [DOI] [PubMed] [Google Scholar]
- 19.Cailhier JF, Partolina M, Vuthoori S, Wu S, Ko K, Watson S, Savill J, Hughes J, Lang RA. Conditional macrophage ablation demonstrates that resident macrophages initiate acute peritoneal inflammation. J Immunol. 2005;174:2336–2342. doi: 10.4049/jimmunol.174.4.2336. [DOI] [PubMed] [Google Scholar]
- 20.Fogel E, Aplin AC, Nicosia RF. Aortic rings stimulate inflammatory angiogenesis in a subcutaneous implant in vivo model. Angiogenesis. 2007;10:287–295. doi: 10.1007/s10456-007-9082-0. [DOI] [PubMed] [Google Scholar]
- 21.Zhu WH, Nicosia RF. The thin prep rat aortic ring assay: a modified method for the characterization of angiogenesis in whole mounts. Angiogenesis. 2002;5:81–86. doi: 10.1023/a:1021509004829. [DOI] [PubMed] [Google Scholar]
- 22.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 23.Van Rooijen N, Kesteren-Hendrikx E. Clodronate liposomes: perspectives in research and therapeutics. J Liposome Res. 2002;12:81–94. doi: 10.1081/lpr-120004780. [DOI] [PubMed] [Google Scholar]
- 24.Chitu V, Stanley ER. Colony-stimulating factor-1 in immunity and inflammation. Curr.Opin.Immunol. 2006;18:39–48. doi: 10.1016/j.coi.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 25.Sunderkotter C, Steinbrink K, Goebeler M, Bhardwaj R, Sorg C. Macrophages and angiogenesis. J Leukoc.Biol. 1994;55:410–422. doi: 10.1002/jlb.55.3.410. [DOI] [PubMed] [Google Scholar]
- 26.Villaschi S, Nicosia RF. Angiogenic role of endogenous basic fibroblast growth factor released by rat aorta after injury. Am J Pathol. 1993;143:181–190. [PMC free article] [PubMed] [Google Scholar]
- 27.Dirkx AE, Egbrink MG, Wagstaff J, Griffioen AW. Monocyte/macrophage infiltration in tumors: modulators of angiogenesis. J Leukoc.Biol. 2006 doi: 10.1189/jlb.0905495. [DOI] [PubMed] [Google Scholar]
- 28.Mantovani A, Schioppa T, Porta C, Allavena P, Sica A. Role of tumor-associated macrophages in tumor progression and invasion. Cancer Metastasis Rev. 2006 doi: 10.1007/s10555-006-9001-7. [DOI] [PubMed] [Google Scholar]
- 29.Camussi G, Montrucchio G, Lupia E, Soldi R, Comoglio PM, Bussolino F. Angiogenesis induced in vivo by hepatocyte growth factor is mediated by platelet-activating factor synthesis from macrophages. J Immunol. 1997;158:1302–1309. [PubMed] [Google Scholar]
- 30.Anghelina M, Krishnan P, Moldovan L, Moldovan NI. Monocytes/macrophages cooperate with progenitor cells during neovascularization and tissue repair: conversion of cell columns into fibrovascular bundles. Am J Pathol. 2006;168:529–541. doi: 10.2353/ajpath.2006.050255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Diglio CA, Grammas P, Giacomelli F, Wiener J. Angiogenesis in rat aorta ring explant cultures. Lab Invest. 1989;60:523–531. [PubMed] [Google Scholar]
- 32.Keane MP, Belperio JA, Xue YY, Burdick MD, Strieter RM. Depletion of CXCR2 inhibits tumor growth and angiogenesis in a murine model of lung cancer. J Immunol. 2004;172:2853–2860. doi: 10.4049/jimmunol.172.5.2853. [DOI] [PubMed] [Google Scholar]
- 33.Rosenkilde MM, Schwartz TW. The chemokine system -- a major regulator of angiogenesis in health and disease. APMIS. 2004;112:481–495. doi: 10.1111/j.1600-0463.2004.apm11207-0808.x. [DOI] [PubMed] [Google Scholar]
- 34.Stanley ER, Berg KL, Einstein DB, Lee PS, Pixley FJ, Wang Y, Yeung YG. Biology and action of colony--stimulating factor-1. Mol.Reprod.Dev. 1997;46:4–10. doi: 10.1002/(SICI)1098-2795(199701)46:1<4::AID-MRD2>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 35.Okazaki T, Ebihara S, Takahashi H, Asada M, Kanda A, Sasaki H. Macrophage colony-stimulating factor induces vascular endothelial growth factor production in skeletal muscle and promotes tumor angiogenesis. J Immunol. 2005;174:7531–7538. doi: 10.4049/jimmunol.174.12.7531. [DOI] [PubMed] [Google Scholar]
- 36.Okazaki T, Ebihara S, Asada M, Yamanda S, Saijo Y, Shiraishi Y, Ebihara T, Niu K, Mei H, Arai H, Yambe T. Macrophage colony-stimulating factor improves cardiac function after ischemic injury by inducing vascular endothelial growth factor production and survival of cardiomyocytes. Am J Pathol. 2007;171:1093–1103. doi: 10.2353/ajpath.2007.061191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin EY, Nguyen AV, Russell RG, Pollard JW. Colony-stimulating factor 1 promotes progression of mammary tumors to malignancy. J Exp.Med. 2001;193:727–740. doi: 10.1084/jem.193.6.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gordon S. Alternative activation of macrophages. Nat.Rev.Immunol. 2003;3:23–35. doi: 10.1038/nri978. [DOI] [PubMed] [Google Scholar]
- 39.Volpert OV, Fong T, Koch AE, Peterson JD, Waltenbaugh C, Tepper RI, Bouck NP. Inhibition of angiogenesis by interleukin 4. J Exp.Med. 1998;188:1039–1046. doi: 10.1084/jem.188.6.1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nishimura Y, Nitto T, Inoue T, Node K. IL-13 Attenuates Vascular Tube Formation Via JAK2-STAT6 Pathway. Circ.J. 2008;72:469–475. doi: 10.1253/circj.72.469. [DOI] [PubMed] [Google Scholar]
- 41.Haas CS, Amin MA, Allen BB, Ruth JH, Haines GK, III, Woods JM, Koch AE. Inhibition of angiogenesis by interleukin-4 gene therapy in rat adjuvant-induced arthritis. Arthritis Rheum. 2006;54:2402–2414. doi: 10.1002/art.22034. [DOI] [PubMed] [Google Scholar]
- 42.Haas CS, Amin MA, Ruth JH, Allen BL, Ahmed S, Pakozdi A, Woods JM, Shahrara S, Koch AE. In vivo inhibition of angiogenesis by interleukin-13 gene therapy in a rat model of rheumatoid arthritis. Arthritis Rheum. 2007;56:2535–2548. doi: 10.1002/art.22823. [DOI] [PubMed] [Google Scholar]
- 43.Lee IY, Kim J, Ko EM, Jeoung EJ, Kwon YG, Choe J. Interleukin-4 inhibits the vascular endothelial growth factor- and basic fibroblast growth factor-induced angiogenesis in vitro. Mol.Cells. 2002;14:115–121. [PubMed] [Google Scholar]
- 44.Hart PH, Bonder CS, Balogh J, Dickensheets HL, Donnelly RP, Finlay-Jones JJ. Differential responses of human monocytes and macrophages to IL-4 and IL-13. J Leukoc.Biol. 1999;66:575–578. [PubMed] [Google Scholar]
- 45.Curiel TJ, Cheng P, Mottram P, Alvarez X, Moons L, Evdemon-Hogan M, Wei S, Zou L, Kryczek I, Hoyle G, Lackner A, Carmeliet P, Zou W. Dendritic cell subsets differentially regulate angiogenesis in human ovarian cancer. Cancer Res. 2004;64:5535–5538. doi: 10.1158/0008-5472.CAN-04-1272. [DOI] [PubMed] [Google Scholar]
- 46.Bingle L, Lewis CE, Corke KP, Reed MW, Brown NJ. Macrophages promote angiogenesis in human breast tumour spheroids in vivo. Br.J Cancer. 2006;94:101–107. doi: 10.1038/sj.bjc.6602901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zeisberger SM, Odermatt B, Marty C, Zehnder-Fjallman AH, Ballmer-Hofer K, Schwendener RA. Clodronate-liposome-mediated depletion of tumour-associated macrophages: a new and highly effective antiangiogenic therapy approach. Br.J Cancer. 2006;95:272–281. doi: 10.1038/sj.bjc.6603240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nakao S, Kuwano T, Tsutsumi-Miyahara C, Ueda S, Kimura YN, Hamano S, Sonoda KH, Saijo Y, Nukiwa T, Strieter RM, Ishibashi T, Kuwano M, Ono M. Infiltration of COX-2-expressing macrophages is a prerequisite for IL-1 beta-induced neovascularization and tumor growth. J Clin.Invest. 2005;115:2979–2991. doi: 10.1172/JCI23298. [DOI] [PMC free article] [PubMed] [Google Scholar]