Abstract
Purpose
To evaluate the monocular oral reading rate, accuracy, fluency and comprehension in 10-year-old children previously treated for amblyopia.
Design
Prospective observational case series
Methods
79 children (mean age 10.3 years) previously treated in a multicenter randomized trial comparing patching and atropine were tested at 7 sites using a modification of the Gray Oral Reading Test, Edition 4.0 (GORT-4).
Results
The mean visual acuities in the amblyopic and fellow eyes at the time of the reading assessment were 0.17 logMAR (approximately 20/32) and −0.03 logMAR (approximately 20/20), respectively. Compared with the sound eye, amblyopic eye performance was worse when reading orally with respect to rate (P <0.001), accuracy (P = 0.03), and fluency (P <0.001). Reading comprehension scores were similar with the amblyopic and fellow eyes (P=0.45). Similar results were found with respect to original treatment group assignment (atropine or patching). There was a modest correlation between interocular difference (IOD) of visual acuity at age 10 years and IOD in reading rate (r = 0.37, 95% confidence interval (CI) = 0.18 to 0.56) and fluency (r = 0.28, 95% CI = 0.08 to 0.49). There was no correlation between the IOD in visual acuity and IOD in accuracy (r=0.08, 95% CI = −0.14 to 0.30) or comprehension (r = 0.16, 95% confidence interval −0.05 to 0.37).
Conclusions
The monocular oral reading ability when measured with the GORT-4 was slightly worse when reading with previously treated amblyopic eyes compared with fellow eyes in terms of rate, accuracy and fluency, but reading comprehension testing was similar.
Introduction
Most reports of visual function outcomes following treatment of amblyopia have been limited to monocular high contrast visual acuity and in some cases stereoacuity and contrast sensitivity. Reading ability has been infrequently studied in children with a history of amblyopia.1, 2
Oral reading requires the recognition of phonemes using a number of strategies in a process referred to as decoding. Difficulty with decoding may lead to slow and inaccurate speech during oral reading. Fluency is a measure of reading that combines speed and accuracy. Fluent oral reading is a critical factor promoting comprehension of the content of the reading material.3 When there is poor fluency, the child directs more attention to decoding and less to comprehension.
The Pediatric Eye Disease Investigator Group (PEDIG) conducted a randomized trial comparing patching (6 hours to full time daily in fellow eye) with atropine (1% daily in fellow eye) as treatment for moderate amblyopia (20/40 to 20/100) in children younger than 7 years of age.4 A subset of children completed follow-up exams at age 10 years which included testing of high-contrast visual acuity, contrast sensitivity, and reading skills. We hypothesized that monocular reading skills of the amblyopic eye might remain deficient in a child having had treatment prescribed for amblyopia, even when visual acuity was nearly normal.
In this study we compared monocular oral reading rate, accuracy, fluency (equals rate plus accuracy), and comprehension between amblyopic and fellow eyes of 10-year-old children with treated amblyopia.
Methods
The study, supported through a cooperative agreement with the National Eye Institute of the National Institutes of Health (Bethesda, Maryland), was conducted by the Pediatric Eye Disease Investigator Group (PEDIG) at 47 clinical sites. The protocol and informed consent forms were approved by institutional review boards, and the parent or guardian of each study patient gave written informed consent. Study oversight was provided by an independent data and safety monitoring committee.
Subjects were enrolled between 1999 and 2001 in a randomized trial of atropine versus patching. Eligibility criteria for the randomized trial included age younger than 7 years, visual acuity in the amblyopic eye of 20/40 to 20/100, visual acuity in the fellow eye of 20/40 or better, interocular acuity difference of 3 or more logMAR (logarithm of the minimal angle of resolution) lines, and the presence or history of an amblyopiogenic factor meeting study-specified criteria for strabismus and/or anisometropia.4 The study protocol has been detailed in prior publications4, 5 and is available on the PEDIG website (www.pedig.net). A subset of seven sites took part in this ancillary study to evaluate oral reading when the subjects reached 10 years of age. These sites were chosen because they were participating in the long-term outcome study and had a large number of patients.
At approximately 10 years of age, children in this study completed a modified version of the Gray Oral Reading Test - Fourth Edition (GORT-4), a widely used and validated test of oral reading rate, accuracy, fluency, and comprehension appropriate for individuals age 6 to <19 years.6 The GORT-4 consists of two parallel versions (Form A, and Form B) each with 14 separate stories. The stories use age appropriate print size which decreases as the target age increases. The content, the complexity of sentence construction, and overall difficulty also increase with progression from story 1 to 14. There are five multiple choice questions about the content of each story. Forms A and B at each level are of similar difficulty and were scaled to each other by the test creators using a normal population. The entire test was not performed because of time constraints. Instead, each eye was tested with three stories (4, 5, and 6), which are designed with complexity and print size appropriate for ages 9, 10, and 11 years, respectively. Standardized instructions were prepared for the examiner to read aloud while administering the test. Each story and its questions required about 5 minutes to complete. Each child was to complete 6 stories.
Testing was performed monocularly with an opaque patch and without cycloplegia. The right eye was tested first. Habitual glasses were worn. The test booklet was held at the distance the child found comfortable. Testing for each story consisted of a timed oral reading after which the child was asked to answer the five multiple choice questions from the test booklet based upon what he/she had read to evaluate comprehension. Breaks were allowed as needed between stories. After completion of the three stories with the right eye, the child was given a 5-minute rest before the left eye was tested.
Performance on each story was measured by converting the time in seconds to complete the reading to a scaled ‘Rate’ score ranging from 0 to 5 (Table 1). The number of errors in the spoken word compared with the printed word was converted to a scaled ‘Accuracy’ score, also ranging from 0 to 5. A ‘Fluency’ score was calculated as the arithmetic sum of ‘Rate’ and ‘Accuracy’ scaled scores (range 0 to 10). A ‘Comprehension’ score was calculated as the number of questions answered correctly out of the five. For all scores, a higher scaled value indicated better performance.
Table 1.
Scoring Key for Form A – Story 4 used for Determining Scaled Scores for Accuracy and Rate of Oral Reading by Amblyopic and Fellow Eyes
| Form A – Story 4 | ||||||
|---|---|---|---|---|---|---|
| Deviations from Print | >6 | 5−6 | 4 | 2−3 | 1 | 0 |
| Accuracy Score | 0 | 1 | 2 | 3 | 4 | 5 |
| Time (in seconds) | >89 | 61−88 | 55−60 | 41−54 | 34−40 | <34 |
| Rate Score | 0 | 1 | 2 | 3 | 4 | 5 |
A scoring key is published by the test manufacturer for each story. This example is the scoring key for Form A – Story 4. The subject's data in terms of accuracy and rate are compared to the normative data and a scaled score in the second row is obtained.
Statistical Analysis
The scaled scores were combined for the three stories resulting in a rate, accuracy, and comprehension measure for that eye's performance from 0 to +15. A fluency score was calculated as the sum of rate and accuracy ranging from 0 to +30. For each reading measure, an interocular difference (IOD) was calculated ranging from −15 to +15 for rate, accuracy, and comprehension; and −30 to +30 for fluency (positive sign indicates sound eye better). A Wilcoxon Signed-Rank test was performed to evaluate whether there was a difference in reading ability between the amblyopic and fellow eyes. Wilcoxon rank-sum tests were performed to explore the association between IOD in reading abilities and the original randomized treatment group. The association between IOD in reading ability and IOD in visual acuity was evaluated by calculating a Spearman correlation coefficient with 95% exact confidence intervals (CI). Analyses were performed using SAS (version 9.0., SAS Institute, Cary, NC) and Stat-Exact version 6.0 (Cytel Inc., Cambridge, Massachusetts). Reported P values are two-sided.
Results
Reading testing was completed by 79 children. Their mean age was 4.9 years at enrollment (range 2.6 to 6.9) into the randomized trial and 10.3 years at the time of the reading test (range 9.3 to 11.7 years); 52% were female. Forty-eight percent of the patients were amblyopic in the left eye. The mean visual acuities in the amblyopic and fellow eyes at the time of the age 10 years reading exam were 0.17 logMAR (approximately 20/32, range 20/16 to 20/63) and −0.03 logMAR (approximately 20/20, range 20/16 to 20/50), respectively. The cohort was comparable to the 340 patients in the randomized trial who did not participate in the ancillary study with respect to the following characteristics at entry into the randomized trial: age, gender, race, cause of amblyopia (anisometropia, strabismus, or both), baseline visual acuity in the amblyopic and sound eyes, and refractive error. The participants were also similar to the non-participants in visual acuities of both eyes at the six-month and two-year outcome examinations of the randomized trial.
Reading Assessment
The scaled scores for monocular oral reading rate, accuracy, fluency, and comprehension for the amblyopic and fellow eyes are listed in Table 2. There was an IOD favoring the fellow eye in monocular oral reading rate (median IOD = +1 units, quartiles 0 to +2, P <0.001), reading accuracy (median IOD = 0 units, quartiles 0 to +1, P = 0.03), and fluency (median IOD = +1 units, quartiles −1 to +3, P<0.001) (Table 2). Reading comprehension scores were similar in the amblyopic and fellow eyes (median IOD = 0 units, quartiles −2 to +2, P=0.45) (Table 2). Reading assessment IOD scores did not differ with respect to original randomized treatment group (atropine or patching) (P=0.27 for oral reading rate, P=0.67 for accuracy, P=0.32 for fluency, and P=0.98 for comprehension, respectively).
Table 2.
Reading Assessment at the Age 10-year Visit of Amblyopic and Fellow Eyes
|
Reading Rate |
Reading Accuracy |
Reading Fluency‡ (Rate + Accuracy) |
Reading Comprehension |
|||||
|---|---|---|---|---|---|---|---|---|
|
Amblyopic Eye* N=79 |
Fellow Eye* N=79 |
Amblyopic Eye* N=79 |
Fellow Eye* N=79 |
Amblyopic Eye* N=79 |
Fellow Eye* N=79 |
Amblyopic Eye* N=79 |
Fellow Eye* N=79 |
|
| Sum of Scaled Scores† | % | % | % | % | % | % | % | % |
| 0 | 1 (1%) | 0 | 1 (1%) | 0 | 1 (1%) | 0 | 0 | 0 |
| 1 | 2 (3%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2 | 2 (3%) | 2 (3%) | 0 | 0 | 0 | 0 | 0 | 0 |
| 3 | 0 | 1 (1%) | 0 | 0 | 0 | 0 | 0 | 0 |
| 4 | 1 (1%) | 2 (3%) | 0 | 0 | 0 | 0 | 0 | 0 |
| 5 | 3 (4%) | 2 (3%) | 0 | 1 (1%) | 0 | 0 | 0 | 0 |
| 6 | 7 (9%) | 1 (1%) | 1 (1%) | 0 | 0 | 0 | 2 (3%) | 0 |
| 7 | 6 (8%) | 2 (3%) | 3 (4%) | 1 (1%) | 0 | 1 (1%) | 4 (5%) | 2 (3%) |
| 8 | 3 (4%) | 4 (5%) | 0 | 1 (1%) | 1 (1%) | 0 | 5 (6%) | 2 (3%) |
| 9 | 7 (9%) | 5 (6%) | 0 | 1 (1%) | 0 | 0 | 3 (4%) | 8 (10%) |
| 10 | 2 (3%) | 1 (1%) | 3 (4%) | 0 | 0 | 0 | 14 (18%) | 9 (11%) |
| 11 | 9 (11%) | 6 (8%) | 1 (1%) | 3 (4%) | 2 (3%) | 1 (1%) | 14 (18%) | 16 (20%) |
| 12 | 4 (5%) | 9 (11%) | 5 (6%) | 1 (1%) | 1 (1%) | 0 | 15 (19%) | 19 (24%) |
| 13 | 6 (8%) | 13 (16%) | 13 (16%) | 6 (8%) | 2 (3%) | 0 | 12 (15%) | 14 (18%) |
| 14 | 10 (13%) | 11 (16%) | 11 (14%) | 13 (16%) | 0 | 0 | 6 (8%) | 8 (10%) |
| 15 | 16 (20%) | 18 (23%) | 41 (52%) | 52 (66%) | 0 | 0 | 4 (5%) | 1 (1%) |
| 16 | - | - | - | - | 0 | 1 (1%) | - | - |
| 17 | - | - | - | - | 2 (3%) | 2 (3%) | - | - |
| 18 | - | - | - | - | 0 | 1 (1%) | - | - |
| 19 | - | - | - | - | 6 (8%) | 3 (4%) | - | - |
| 20 | - | - | - | - | 7 (9%) | 3 (4%) | - | - |
| 21 | - | - | - | - | 3 (4%) | 1 (1%) | - | - |
| 22 | - | - | - | - | 0 | 5 (6%) | - | - |
| 23 | - | - | - | - | 3 (4%) | 2 (3%) | - | - |
| 24 | - | - | - | - | 12 (15%) | 3 (4%) | - | - |
| 25 | - | - | - | - | 2 (3%) | 1 (1%) | - | - |
| 26 | - | - | - | - | 2 (3%) | 6 (8%) | - | - |
| 27 | - | - | - | - | 5 (6%) | 7 (9%) | - | - |
| 28 | - | - | - | - | 9 (11%) | 13 (16%) | - | - |
| 29 | - | - | - | - | 8 (10%) | 15 (19%) | - | - |
| 30 | - | - | - | - | 13 (16%) | 14 (18%) | - | - |
| Median (quartiles) | 11 (7, 14) | 13 (10, 14) | 15 (13, 15) | 15 (14, 15) | 24 (20, 29) | 28 (23, 29) | 11 (10, 13) | 12 (10, 13) |
| [Range] |
[0 to 15] |
[2 to 15] |
[0 to 15] |
[5 to 15] |
[0 to 30] |
[7 to 30] |
[6 to 15] |
[7 to 15] |
| Interocular Difference | ||||||||
| 1 or more units better in the amblyopic eye | 19 (24%) | 15 (19%) | 24 (30%) | 33 (42%) | ||||
| Tested the same in each eye | 19 (24%) | 37 (47%) | 14 (18%) | 12 (15%) | ||||
| 1 or more units better in the fellow eye | 41 (52%) | 27 (34%) | 41 (52%) | 34 (43%) | ||||
| Median IOD (quartiles) | +1 (0, +2) | 0 (0, +1) | +1 (−1, +3) | 0 (−2, +2) | ||||
| [Range] | [−4 to +15] | [−6 to +15] | [−6 to +30] | [−4 to +8] | ||||
‘Amblyopic’ eye and ‘Fellow’ eye refers to the study eye at the time of randomization
Sum is of the scaled scores for Forms 4, 5, and 6 (maximum sum for rate, accuracy, and comprehension is 15)
Fluency is the sum of the rate and accuracy scores for Forms 4, 5, and 6 (maximum sum = 30)
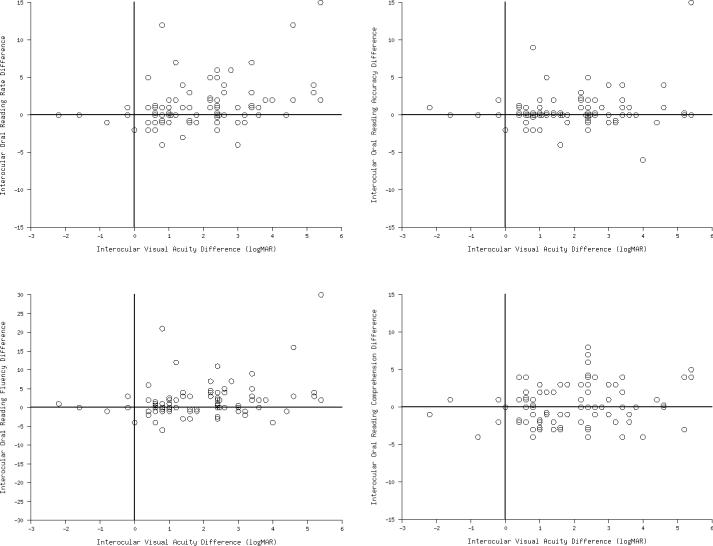
There was a modest correlation between IOD in visual acuity at age 10 years and IOD in rate and fluency (Spearman correlation for rate = 0.37, 95% CI 0.18 to 0.56; Spearman correlation for fluency = 0.28, 95% CI 0.08 to 0.49) (Figures 1A and 1B). There was no correlation between the IOD in visual acuity and IOD in accuracy (Spearman correlation = 0.08, 95% confidence interval −0.14 to 0.30) or comprehension (Spearman correlation = 0.16, 95% confidence interval −0.05 to 0.37) (Figures 1C and 1D). In subjects in whom amblyopia had resolved (interocular difference favoring sound eye no more than 1 line), the amblyopic eye's reading abilities were similar to those of the sound eye.
Discussion
We studied the monocular oral reading speed, accuracy, fluency and comprehension of 79 children with previously treated amblyopia at a mean age of 10.3 years. We found the amblyopic eyes to be slightly slower and less accurate compared with fellow eyes, while comprehension was similar. Results were similar when comparing the eyes by the two original treatment groups (atropine and patching).
When we designed the study we hypothesized that reading with previously treated amblyopic eyes might be poorer than with fellow eyes either because of the residual deficit in visual acuity or changes in the brain. There is a critical print size for efficient reading, which is larger than threshold visual acuity.7 Slower speed and accuracy might be expected when reading with the amblyopic eye compared with the fellow eye because the visual acuity of the amblyopic eye would be closer to the critical reading print size. In fact we did find modest correlations between poorer visual acuity of the amblyopic eye relative to the sound eye and reductions in rate and fluency. However, caution is needed in concluding that the reading differences were related to size. Most of the amblyopic eyes had a visual acuity of 20/40 or better and were within two lines of the sound eyes, limiting our ability to detect a stronger correlation. The grade-appropriate text used for the testing was 20/80 which may also have reduced our ability to detect a relationship. In addition, children in this study were allowed to use whatever testing distance was comfortable, rather than a fixed distance, possibly increasing effective print size by moving closer to the material.
Another possible cause of reading difficulty in amblyopia might be related to accommodation, which has been shown to be deficient in eyes with amblyopia.8 However, we did not compare accommodative ability in these eyes. Therefore, we do not know if there was a significant optical blur that impacted reading performance with the amblyopic eye. Lastly, reading requires substantial cortical function beyond simple letter recognition.7 It is possible that an important portion of the slowing of reading speed in eyes with amblyopia is related to abnormalities of central processing by the brain.
Prior to the study we had speculated that when reading with the amblyopic eye there would be reduced comprehension because the child would spend more time decoding the words and thus be less attentive to the content. This effect was not observed. As with oral reading speed, perhaps the depth of the residual amblyopia was not enough to affect this processing. Another reason for lack of difference in comprehension might be the test design. The validity of the comprehension component of the GORT-4 has recently been questioned by investigators who found that some of the comprehension questions could be answered correctly without reading the text.9 If their finding is substantiated, this could explain why our patients comprehended the stories equally well when reading with each eye.
Most studies of reading by amblyopic patients have tested binocularly, rather than monocularly as we did in this study. Some of these studies have indicated that binocular reading ability in children with amblyopia is impaired,1, 10 while others have reported that reading ability is not affected.2 Stifter and colleagues studied the monocular reading ability of 22 children with treated microstrabismic amblyopia.11 They studied reading speed and reading acuity with Radner Reading charts. These charts consist of 12 sentences, each 14 words in length. There is a progressive reduction in the size of the optotype from first to last sentence. The test does not include evaluation of comprehension or accuracy. The amblyopic eyes performed more poorly in reading speed and reading acuity compared with their fellow eyes. This finding was also true for the 8 subjects whose amblyopic and fellow eyes had equal acuity.
The strengths of our study are that it was prospective, enrolled a large number of children with known visual acuities, and treatment was largely complete with most of the subjects having only mild residual amblyopia. We administered a reading test commonly used in the educational community that is based on grade-appropriate print size and content complexity. The limitations of our study include the practical need to use a modified form of the GORT-4, rather than the entire test, as the latter was too time consuming to administer in our clinic settings. We thus cannot compare our results to those found in the large normative database of the GORT-4. There were few amblyopic eyes with poor visual acuity reducing our ability to explore the effect of the interocular visual acuity difference on reading. We also did not test binocularly, so we are unable to describe the reading abilities of our patients. Lastly, this is a test of oral reading from high contrast printed media and should not be generalized to other types of reading.
In summary, we found a 10-year old child's monocular oral reading ability with eyes previously treated for amblyopia, when measured with the modified GORT-4, to be slightly worse in terms of rate, accuracy and fluency compared with fellow eyes. However, performance on comprehension testing was similar. The residual visual acuity deficit was modestly correlated to poorer rate and fluency with the amblyopic eye.
Supplementary Material
Figure. Reading Ability Interocular Difference compared with Visual Acuity Interocular Difference at the Age 10-year Visit.
Interocular difference (IOD) of visual acuity is presented in logMAR lines, with minus values representing better acuity in the amblyopic eye and plus values representing better acuity in the fellow eye. Reading ability interocular differences are scaled with values ranging from −15 (better in amblyopic eye) to +15 (better in fellow eye) for rate, accuracy, and comprehension and from −30 to +30 for fluency (sum of rate and accuracy values for each eye)
(Top left) IOD in oral reading rate is compared with IOD in visual acuity, (top right) IOD in oral reading accuracy is compared with IOD in visual acuity, (bottom left) IOD in oral reading fluency is compared with IOD in visual acuity and (bottom right) IOD in oral reading comprehension is compared with IOD in visual acuity.
Acknowledgements
A. The study, supported through a cooperative agreement with the National Eye Institute of the National Institutes of Health (Bethesda, Maryland), Department of Health and Human Services (EY011751), was conducted by the Pediatric Eye Disease Investigator Group at 7 of the initial 47 participating clinical sites.
B. The authors indicate no financial conflict of interest.
C. The following authors were involved in the design of the study: M. Repka, R. Kraker, R. Beck, S. Cotter, J. Holmes, and R. Arnold. All of the authors were involved in the collection, management, analysis, and interpretation of the data and the preparation, review, and final approval of the manuscript.
D. The respective institutional review boards approved the protocol and Health Insurance Portability and Accountability Act- compliant informed consent forms. The protocol and informed consent forms were approved by the institutional review boards for each of the named authors, and the parent of each study patient gave written informed consent. Study oversight was provided by an independent data and safety monitoring committee. The study is registered at www.clinicaltrials.gov (registration number: NCT00000170) and the trial registry name is: Amblyopia Treatment Study: Occlusion Versus Pharmacologic Therapy for Moderate Amblyopia.
Sites are listed in order by number of patients completing reading testing (noted in parenthesis). Investigators (I) and Coordinators (C) for each site are listed.
Erie, PA - Pediatric Ophthalmology of Erie (16)
Nicholas A. Sala, (I); Rhonda M. Hodde, (C)
Calgary, - Alberta Children's Hospital (15)
William F. Astle, (I); Heather M. Vibert, (C); Heather J. Peddie, (C); Catriona I. Kerr, (C)
Anchorage, AK - Ophthalmic Associates (14)
Robert W. Arnold, (I); Mary Diane Armitage, (C)
Providence, RI - Pediatric Ophthalmology and Strabismus Associates (14)
David Robbins Tien, (I); Heidi C. Christ, (C)
Baltimore, MD - Wilmer Institute* (10)
Michael X. Repka (I)
Fullerton, CA - Southern California College of Optometry (6)
Susan A. Cotter, (I); Monique M. Nguyen, (I); Carmen N. Barnhardt, (I); Raymond H. Chu, (I)
Rochester, MN - Mayo Clinic* (4)
Jonathan M. Holmes, (I); Rebecca A. Nielsen, (C)
* Center received support utilized for this project from an unrestricted grant from Research to Prevent Blindness Inc., New York, New York.
REFERENCES
- 1.Stifter E, Burggasser G, Hirmann E, Thaler A, Radner W. Monocular and binocular reading performance in children with microstrabismic amblyopia. Br J Ophthalmol. 2005;89:1324–9. doi: 10.1136/bjo.2005.066688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koklanis K, Georgievski Z, Brassington K, Bretherton L. The prevalence of specific reading disability in an amblyopic population: A preliminary report. Binocul Vis Strabismus Q. 2006;21:27–32. [PubMed] [Google Scholar]
- 3.National Institute of Child Health and Human Development . Teaching children to read: An evidence-based assessment of the scientific research literature on reading and its implications for reading instruction (NIH Publication No. 00−4769) U.S. Government Printing Office; Washington, DC: 2000. Report of the National Reading Panel. [Google Scholar]
- 4.Pediatric Eye Disease Investigator Group A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120:268–78. doi: 10.1001/archopht.120.3.268. [DOI] [PubMed] [Google Scholar]
- 5.Pediatric Eye Disease Investigator Group Two-year follow-up of a 6-month randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2005;123:149–57. doi: 10.1001/archopht.123.2.149. [DOI] [PubMed] [Google Scholar]
- 6.Wiederhollt JL, Bryant BR. GORT4: Gray Oral Reading Tests. Pro-ed, Inc; Austin: 2001. pp. 1–131. [Google Scholar]
- 7.O'Brien BA, Mansfield JS, Legge GE. The effect of print size on reading speed in dyslexia. J Res Read. 2005;28:332–49. doi: 10.1111/j.1467-9817.2005.00273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ukai K, Ishii M, Ishikawa S. A quasi-static study of accommodation in amblyopia. Ophthalmic Physiol Opt. 1986;6:287–95. [PubMed] [Google Scholar]
- 9.Keenan JM, Betjemann RS. Comprehending the Gray oral reading test without reading it: why comprehension tests should not include passage-independent items. Scientific Studies of Research. 2006;10:363–80. [Google Scholar]
- 10.Zurcher B, Lang J. Reading capacity in cases of ‘cured’ strabismic amblyopia. Trans Ophthalmol Soc U K. 1980;100:501–3. [PubMed] [Google Scholar]
- 11.Stifter E, Burggasser G, Hirmann E, Thaler A, Radner W. Evaluating reading acuity and speed in children with microstrabismic amblyopia using a standardized reading chart system. Graefes Arch Clin Exp Ophthalmol. 2005;243:1228–35. doi: 10.1007/s00417-005-1187-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.