Abstract
Goals
We sought to identify factors associated with gastroenterology clinic attendance in an urban safety net healthcare system.
Background
Missed clinic appointments reduce the efficiency and availability of healthcare, but subspecialty clinic attendance among patients with established healthcare access has not been studied.
Study
We performed an observational study using secondary data from administrative sources to study patients referred to, and scheduled for an appointment in, the adult gastroenterology clinic serving the safety net healthcare system of San Francisco, California. Our dependent variable was whether subjects attended or missed a scheduled appointment. Analysis included multivariable logistic regression and classification tree analysis. 1,833 patients were referred and scheduled for an appointment between 05/2005 and 08/2006. Prisoners were excluded. All patients had a primary care provider.
Results
683 patients (37.3%) missed their appointment; 1,150 (62.7%) attended. Language was highly associated with attendance in the logistic regression; non-English speakers were less likely than English speakers to miss an appointment (adjusted odds ratio 0.42 [0.28,0.63] for Spanish, 0.56 [0.38,0.82] for Asian language, p < 0.001). Other factors were also associated with attendance, but classification tree analysis identified language to be the most highly associated variable.
Conclusions
In an urban safety net healthcare population, among patients with established healthcare access and a scheduled gastroenterology clinic appointment, not speaking English was most strongly associated with higher attendance rates. Patient related factors associated with not speaking English likely influence subspecialty clinic attendance rates, and these factors may differ from those affecting general healthcare access.
Introduction
When patients miss outpatient clinic appointments, the efficiency of healthcare is reduced and patients experience longer wait times for appointments. 1 Longer waiting times may reduce healthcare quality; in geriatric populations, longer waiting times have been associated with increased mortality rates. 2 Missed clinic appointments place economic strain on the healthcare system, 3 and patients who routinely miss clinic appointments experience poorer health outcomes. 4 Despite the increasing importance of subspecialty care, missed clinic appointments among subspecialty clinics have been scarcely studied. 5,6,7
Gastroenterology is an important specialty in which to examine clinic attendance because of its limited availability among many patient populations, including uninsured Californians, where availability continues to worsen. 8 Even in the general United States population, demand for endoscopic colorectal cancer screening exceeds supply. 9 Missed outpatient appointments may further limit patient access to gastroenterology care. Reducing missed appointments could increase efficiency and availability of gastroenterology care, and possibly improve patient outcomes. Only one study of clinic attendance has been performed in a gastroenterology clinic, and this was small and survey-based. 10
Because factors contributing to missed gastroenterology clinic appointments likely vary among different populations, groups at high risk of adverse health outcomes, such as patients served by safety net healthcare systems, should be studied. Many safety net healthcare systems experience significant shortages in subspecialty care. 11 Patients within the healthcare safety net experience reduced healthcare access, 12,13 which is thought to be a major contributor to healthcare inequities repeatedly demonstrated among non-English speakers and non-white patients. 14,15,16,17,18,19,20,21,22,23,24 Because most studies examine access to healthcare, it is not known how these variables affect appointment attendance among patients with established healthcare access. A better understanding of these patient-related variables could provide a basis for public health interventions to increase gastroenterology clinic attendance rates, which could increase efficiency and availability of gastroenterologic care among vulnerable populations. Findings might also be applicable to other subspecialty clinic types.
We sought to evaluate factors associated with missed gastroenterology clinic appointments within the vulnerable patient population served by the safety net healthcare system of San Francisco with a primary focus on language and race/ethnicity. Based on the existing literature on healthcare access, we hypothesized that non-English speakers and non-white subjects would be less likely to attend scheduled gastroenterology clinic appointments than English speakers and white subjects.
Materials and Methods
Study design
We performed an observational study using secondary data from administrative sources. We studied patients referred to, and scheduled for an appointment in, the adult gastroenterology clinic serving the safety net healthcare system of San Francisco, California. Our dependent variable was whether subjects attended or missed a scheduled appointment in the gastroenterology clinic. We considered subjects who were not seen by a physician in the gastroenterology clinic at any time after the date of referral to have missed their appointment. We defined subjects who were seen by a physician in the gastroenterology clinic after the date of referral to have attended their clinic appointment. Subjects who did not present for the initial scheduled clinic appointment had the option of rescheduling. Subjects who attended a rescheduled appointment were included in the “attended an appointment” group. We permitted subjects at least seven additional weeks to reschedule.
Study population
San Francisco General Hospital provides subspecialty care for the safety net healthcare system of the City and County of San Francisco, which includes multiple primary care clinics run by the San Francisco Department of Public Health, and affiliated independent Federally Qualified Health Centers and Federally-Funded 300(h) Grantee Centers. Patients are ethnically diverse (20% African American, 20% Asian/Pacific Islander, 25% Caucasian, and 30% Hispanic), and many are immigrants. Patients speak more than 20 different languages. Approximately 36% of outpatients at San Francisco General Hospital lack insurance, 34% have MediCal (California’s Medicaid program), 16% have Medicare, and 14% report commercial payers or other sources. 25
We studied all patients referred to, and scheduled for an appointment in, the adult gastroenterology clinic at San Francisco General Hospital between 05/25/2005 and 08/22/2006. Patients were excluded if they were prisoners at the time of referral because of ethical issues associated with studying prisoners. When a patient was referred more than once, we included only the initial referral.
Patient referral and clinic scheduling
Patients were referred via an internet-based, electronic referral program (eReferral) to the gastroenterology clinic by their primary care provider or, less commonly, at discharge from the hospital by inpatient physicians. All patients had a primary care provider. Referring providers entered patient-related data, including reason for consultation, history of present illness, past medical history, and medical workup. An experienced gastroenterologist (HFY) reviewed all referrals and scheduled clinic visits for appropriately referred patients. Primary care providers for scheduled patients received an email with appointment information to permit patients to be notified of the appointment. Patients also received an automatically generated English-language appointment notification letter at the time of scheduling and a reminder letter two weeks before the scheduled appointment, or, in the case of patients whose appointments were within two weeks of the time of scheduling, a telephone call and an appointment letter. Patients and providers were able to call and reschedule appointments if patients missed the initial scheduled appointment. Scheduling staff spoke English, Spanish, and Chinese dialects (Cantonese and Mandarin).
Data studied and data sources
We obtained data from three sources: the eReferral system database, the electronic medical record at San Francisco General Hospital, and the clinic scheduling database. We linked all subject data using unique identification numbers, and compiled data electronically into a single database. We removed identifying information and assigned each subject a random, unique number. No subjects were contacted for the purposes of this study.
The dependent variable was whether a patient attended their clinic appointment. Independent variables included covariates with potential significance based upon the findings of other studies of healthcare access and utilization.22,23,,26,27,28,29,30,31,32,33,34 Demographic data included age, gender, self-reported primary language, self-reported race/ethnicity, several measures of socioeconomic status, history of substance abuse or psychiatric diagnoses, distance from subjects’ home to the clinic, and insurance status. We used self-report to define race/ethnicity, as this has been used as the gold standard in previous research and is the recommended standard.35,36,37 Responses were closed-ended, including Asian, black, Hispanic, Native American/Eskimo, white, and other. Primary language was self-reported and open-ended. Major categories were as follows: English, Spanish, Asian language, and other. We grouped together Cantonese, Korean, Laotian, Mandarin, Thai, or Vietnamese speakers as “Asian language” since there were few patients speaking each of these languages. We calculated distance from subjects’ residence to the clinic using an internet mapping program from subjects’ zip code to the clinic. We include histories of substance abuse and psychiatric disease as independent variables, because these have been associated with reduced healthcare access in other studies. Subjects were considered to have a psychiatric disease or substance abuse if a relevant ICD-9 code had been entered into their medical record during the six months prior to referral. We obtained data regarding primary clinic type and referring provider level of training from the eReferral system. The number of days between referral and appointment date and whether the patient was seen in clinic were obtained from the clinic scheduling database. Although reasons for patient referral were available, there was not a feasible method for categorizing reasons for referral or severity of patient complaints.
Data analysis
We compared patients who attended or missed their clinic appointment using bivariate and multivariable statistical methods. For bivariate analyses, categorical variables were compared using χ-square tests, and continuous variables were analyzed using two-tailed t-tests and ANOVA. We performed logistic regression for multivariable analysis, using dummy variables when necessary. Bivariate analyses and logistic regression analysis used Stata, version 9.2 (Statacorp, College Station, TX) and SAS, version 9.1 (SAS Institute, Cary, NC).
To identify the patients at highest risk of missing appointments, we employed classification tree analysis, which is a method used to better identify subgroups that are statistically alike with respect to covariates and outcome. 38 Such subgroup elicitation is not readily obtained through the use of conventional regression procedures. 39
The outcome was not attending a clinic appointment, and all covariates employed for the logistic regression were evaluated. Because there were proportionately fewer patients who did not attend an appointment, equal prior proportions for the two outcome categories were specified, which upweighted the relative effect of misclassifying non-attendees. 38 At each step, the algorithm evaluated all potential “splits,” or divisions into subgroups. Potential splits were evaluated both within and between individual covariates. A large tree was constructed and then pruned back using cross validation. Cross validation proceeded as follows: (i) data were randomly partitioned into ten subsets, (ii) one subset was withheld, and the model was fitted on the remaining nine subsets, (iii) the model was applied to the withheld subset, and (iv) this was repeated with each of the ten subsets serving as the withheld subset. This established what sized tree produced the fewest misclassification errors. Fitting of the classification tree models was via the rpart function of the R (2007) statistical language (R Development Core Team, Vienna Austria).
This study was approved by the University of California San Francisco Committee on Human Research, the General Clinical Research Center at San Francisco General Hospital, and the San Francisco Department of Public Health Privacy Board.
Results
Study population
One thousand eight hundred forty-nine patients were referred to the gastroenterology clinic and scheduled for an appointment during the study period. We excluded sixteen subjects were because they were prisoners, so 1,833 subjects comprise our study population.
Six hundred eighty-three subjects (37.3%) never attended a clinic appointment. The remaining 1,150 subjects (62.7%) did attend a clinic appointment. Of these, 187 were subjects who missed their initial appointment but presented for a subsequent appointment. Subjects missing the initial appointment but presenting later were similar to subjects presenting for the initial appointment.
Bivariate analysis
There were significant bivariate differences between patients who missed and attended their appointment (Table 1).
Table 1.
Population characteristics.
| Characteristics | Total Population (n = 1,833) | Patients who did not attend an appointment (n = 683, 37.3%) | Patients who did attend an appointment (n = 1,150, 62.7%) | P Value* |
|---|---|---|---|---|
| Age, mean (SD), y | 53.0 (12.6) | 52.1 (12.9) | 53.6 (12.4) | 0.02 |
| Women, No. (%) | 957 (52.2) | 336 (49.2) | 621 (54.0) | 0.05 |
| Race/ethnicity, No. (%) | ||||
| White | 424 (23.1) | 166 (24.3) | 258 (22.4) | |
| Black | 348 (19.0) | 176 (25.8) | 172 (15.0) | |
| Asian | 550 (30.0) | 153 (22.4) | 397 (34.5) | |
| Hispanic | 453 (24.7) | 160 (23.4) | 293 (25.5) | |
| Other | 35 (1.9) | 15 (2.2) | 20 (1.7) | < 0.001† |
| Primary Language, No. (%) | ||||
| English | 1,053 (57.4) | 469 (68.7) | 583 (50.7) | |
| Asian language | 381 (20.8) | 93 (13.6) | 288 (25.0) | |
| Spanish | 296 (16.1) | 84 (12.3) | 212 (18.4) | |
| Other | 73 (4.0) | 23 (3.4) | 50 (4.4) | < 0.001† |
| Socioeconomic status measures | ||||
| Homeless, No. (%) | 101 (5.5) | 56 (8.2) | 45 (3.9) | < 0.001† |
| Telephone access, No. (%) | 1,819 (99.2) | 676 (99.0) | 1,143 (99.4) | 0.32 |
| Any insurance, No. (%) | 976 (53.4) | 366 (54.0) | 610 (53.0) | 0.70 |
| Type of insurance, No. (%) | ||||
| Public | 961 (52.4) | 357 (52.3) | 604 (52.5) | |
| Private | 15 (0.8) | 9 (1.3) | 6 (0.5) | |
| Uninsured | 852 (46.5) | 312 (45.7) | 540 (47.0) | 0.008 |
| Monthly income, mean (SD), $ | 790 (702) | 717 (648) | 833 (729) | < 0.001† |
| Employed, No. (%) | 810 (45.1) | 246 (37.3) | 564 (49.7) | < 0.001† |
| Any income source, No. (%) | 1,078 (60.0) | 349 (52.9) | 729 (64.2) | < 0.001† |
| Distance from home to clinic, mean (SD), miles | 4.3 (3.9) | 4.0 (3.5) | 4.4 (4.1) | 0.05 |
| Substance abuse, No. (%) | 125 (6.8) | 64 (9.4) | 61 (5.3) | 0.001† |
| Psychiatric diagnosis, No. (%) | 313 (17.1) | 130 (19.0) | 183 (15.9) | 0.09 |
| Primary clinic, No. (%) | ||||
| Internal medicine | 743 (40.6) | 326 (47.7) | 417 (36.3) | |
| Family practice | 1,037 (56.6) | 333 (48.9) | 704 (61.3) | |
| Other | 52 (2.8) | 24 (3.5) | 28 (2.4) | < 0.001† |
| Type of referring provider, No. (%) | ||||
| Attending physician | 1,139 (62.1) | 422 (61.8) | 717 (62.4) | |
| Trainee physician | 406 (22.1) | 164 (24.0) | 242 (21.0) | |
| Mid-level provider | 286 (15.6) | 97 (14.2) | 189 (16.4) | 0.23 |
| Time from referral to scheduled appointment date, mean (SD), days | 114.6 (59.8) | 119.0 (59.1) | 112.1 (60.1) | 0.02 |
| Days from referral to actual clinic visit, mean (SD), days | --- | --- | 122.1 (71.3) | --- |
P Values cited compare attendees with non-attendees; total population data are listed for reference only.
P < 0.0016, the level of statistical significance using the Bonferroni correction.
Role of language
Table 2 compares subjects based on language. English speakers were more likely to be male (56.6%), homeless (8.4%), and unemployed (63.9%) and to have histories of substance abuse (10.5%) or psychiatric disorders (21.8%) compared with other groups (p < 0.001 for all comparisons). English speakers were less likely to attend a clinic appointment (55.4% attended) compared with non-English speakers (73.3% attended, p < 0.001).
Table 2.
Characteristics of subject according to primary language spoken.
| Characteristics | English (n = 1,053) | Asian Language (n = 381) | Spanish (n = 296) | Other (n = 73) | All Non-English Speakers (n = 750)‡ | P Value |
|---|---|---|---|---|---|---|
| Age, mean (SD), y | 51.7 (12.1) | 57.1 (10.1) | 52.2 (15.2) | 54.5 (13.6) | 54.8 (13.0) | < 0.001* |
| Women, No. (%) | 456 (43.4) | 246 (64.6) | 197 (66.6) | 39 (53.4) | 482 (64.3) | < 0.001† |
| Homeless, No. (%) | 88 (8.4) | 2 (0.5) | 8 (2.7) | 1 (1.4) | 11 (1.5%) | < 0.001† |
| Telephone access, No. (%) | 1,044 (99.2) | 378 (99.2) | 294 (99.3) | 73 (100.0) | 745 (99.3) | 0.55† |
| Any insurance, No. (%) | 543 (51.7) | 242 (63.7) | 126 (42.7) | 49 (68.1) | 417 (55.8) | < 0.001† |
| Monthly income, mean (SD), $ | 734 (648) | 954 (716) | 771 (798) | 866 (866) | 864 (763) | < 0.001* |
| Employed, No. (%) | 371 (36.1) | 216 (57.1) | 167 (57.2) | 43 (60.6) | 426 (57.5) | < 0.001† |
| Any income source, No. (%) | 567 (55.2) | 247 (65.3) | 198 (67.8) | 48 (67.6) | 493 (66.5) | < 0.001† |
| Distance from home to clinic, mean (SD), miles | 4.1 (3.9) | 5.3 (3.4) | 2.9 (2.9) | 6.5 (6.6) | 4.5 (3.8) | < 0.001* |
| Substance abuse, No. (%) | 110 (10.5) | 0 (0.0) | 11 (3.7) | 3 (4.1) | 14 (1.9) | < 0.001† |
| Psychiatric diagnosis, No. (%) | 229 (21.8) | 35 (9.2) | 34 (11.5) | 11 (15.1) | 80 (10.7) | < 0.001† |
| Primary clinic, No. (%) | ||||||
| Internal medicine | 509 (48.4) | 92 (24.2) | 111 (37.5) | 16 (21.9) | 219 (29.2) | |
| Family practice | 518 (49.2) | 273 (71.8) | 176 (59.5) | 57 (78.1) | 506 (67.6) | |
| Other | 25 (2.4) | 15 (4.0) | 9 (3.0) | 0 (0.0) | 24 (3.2) | < 0.001† |
| Did not attend an appointment, No. (%) | 469 (44.6) | 93 (24.4) | 84 (28.4) | 23 (31.5) | 200 (26.7) | < 0.001† |
P value calculated by ANOVA.
P value calculated by chi-square.
Non-English speaker category not included in statistical analysis, is present for reference only.
Role of race/ethnicity
Table 3 compares subjects based on self-reported race/ethnicity. Subjects of Asian descent had the highest attendance rates, and black subjects had the lowest attendance rates (72.2% versus 49.4%, p < 0.001). Asian and Hispanic subjects were more likely than whites or blacks to be employed (54.7% of Asians and 53.0% of Hispanics versus 21.4% of blacks and 43.1% of whites, p < 0.001) and to have any source of income (66.2% of Asians and 66.2% of Hispanics versus 45.1% of blacks and 58.5% of whites, p < 0.001). Asian and Hispanic subjects were less likely to speak English than blacks or whites (27.6% of Asians and 34.0% of Hispanics versus 96.3% of blacks and 89.4% of whites, p < 0.001).
Table 3.
Characteristics of subjects according to race/ethnicity.
| Characteristics | White (n = 424) | Black (n = 348) | Asian (n = 550) | Hispanic (n = 453) | Other (n = 35) | Total Non-White (n = 1,386) ‡ | P Value |
|---|---|---|---|---|---|---|---|
| Age, mean (SD), y | 50.7 (10.9) | 52.8 (11.1) | 56.7 (11.5) | 51.4 (14.9) | 49.6 (13.9) | 53.8 (12.9) | < 0.001* |
| Women, No. (%) | 158 (37.3) | 152 (43.7) | 339 (61.6) | 275 (60.7) | 20 (57.1) | 786 (56.7) | < 0.001† |
| English-speaking, No. (%) | 379 (89.4) | 335 (96.3) | 152 (27.6) | 154 (34.0) | 21 (60.0) | 662 (47.8) | < 0.001† |
| Homeless, No. (%) | 38 (9.0) | 40 (11.5) | 3 (0.6) | 15 (3.3) | 2 (5.7) | 60 (4.3) | < 0.001† |
| Telephone access, No. (%) | 421 (99.3) | 346 (99.4) | 545 (99.1) | 449 (99.1) | 35 (100) | 1,375 (99.2) | 0.97† |
| Any insurance, No. (%) | 215 (50.7) | 198 (56.9) | 337 (61.3) | 205 (45.3) | 16 (45.7) | 756 (54.6) | < 0.001† |
| Monthly income, mean (SD), $ | 761 (675) | 652 (525) | 938 (746) | 766 (768) | 580 (511) | 801 (709) | < 0.001* |
| Employed, No. (%) | 180 (43.1) | 72 (21.4) | 298 (54.7) | 238 (53.0) | 16 (47.1) | 624 (45.7) | < 0.001† |
| Any income source, No. (%) | 244 (58.5) | 152 (45.1) | 361 (66.2) | 297 (66.2) | 17 (50.0) | 827 (60.6) | < 0.001† |
| Distance from home to clinic, mean (SD), miles | 4.5 (4.8) | 4.0 (3.6) | 5.1 (3.6) | 3.1 (3.3) | 4.4 (2.4) | 4.2 (3.6) | < 0.001* |
| Substance abuse, No. (%) | 52 (12.3) | 47 (13.5) | 3 (0.6) | 21 (4.6) | 1 (2.9) | 72 (5.2) | < 0.001† |
| Psychiatric diagnosis, No. (%) | 98 (23.1) | 76 (21.8) | 61 (11.1) | 70 (15.5) | 3 (8.6) | 210 (15.2) | < 0.001† |
| Primary clinic, No. (%) | |||||||
| Internal medicine | 220 (51.9) | 168 (48.3) | 153 (27.9) | 176 (38.9) | 16 (45.7) | 513 (37.0) | |
| Family practice | 196 (46.2) | 176 (50.6) | 377 (68.7) | 261 (57.6) | 16 (45.7) | 830 (59.9) | |
| Other | 8 (1.9) | 4 (1.2) | 19 (3.5) | 16 (3.5) | 3 (8.6) | 42 (3.0) | < 0.001† |
| Did not attend an appointment, No. (%) | 166 (39.2) | 176 (50.6) | 153 (27.8) | 160 (35.3) | 15 (42.9) | 504 (36.4) | < 0.001† |
P value calculated by ANOVA.
P value calculated by chi-square.
Non-White speaker category not included in statistical analysis, is present for reference only.
Multivariable logistic regression
In the logistic regression, language and race/ethnicity were associated with appointment attendance, but language was more strongly associated (Table 4). Subjects speaking Spanish (adjusted odds ratio [AOR] 0.42, 95% confidence interval [CI] 0.28, 0.63) or an Asian language (AOR 0.56, 95% CI 0.38, 0.82) were less likely than English-speaking subjects to miss their appointment. Black (AOR 1.55, 95% CI 1.15, 2.08) and Hispanic (AOR 1.53, 95% CI 1.06, 2.22) subjects were more likely than white subjects to miss their appointment. Other factors that were significantly associated with missed appointments included the absence of any source of income, higher number of days between referral and scheduled appointment, and primary clinic type other than Family Practice.
Table 4.
Logistic regression of factors associated with missing clinic appointment.
| Independent Variables | Unadjusted Odds Ratio (95% Confidence Interval) | Adjusted Odds Ratio (95% Confidence Interval) | P Value† |
|---|---|---|---|
| Language* | <0.001 | ||
| English | 1 (reference) | 1 (reference) | |
| Spanish | 0.49 (0.37, 0.65) | 0.42 (0.28, 0.63) | |
| Asian language | 0.40 (0.31, 0.52) | 0.56 (0.38, 0.82) | |
| Race/ethnicity* | 0.01 | ||
| White | 1 (reference) | 1 (reference) | |
| Black | 1.59 (1.19, 2.12) | 1.55 (1.15, 2.08) | |
| Hispanic | 0.85 (0.65, 1.12) | 1.53 (1.06, 2.22) | |
| Asian | 0.60 (0.46, 0.78) | 0.95 (0.66, 1.38) | |
| No source of income | 1.60 (1.31, 1.94) | 1.42 (1.16, 1.74) | <0.001 |
| Primary clinic* | <0.001 | ||
| Internal medicine | 1 (reference) | 1 (reference) | |
| Family practice | 0.61 (0.50, 0.74) | 0.70 (0.57, 0.87) | |
| Other | 1.10 (0.62, 1.93) | 1.45 (0.80, 2.63) | |
| Time from referral to scheduled appointment date, days | 1.002 (1.000, 1.003) | 1.003 (1.001, 1.004) | <0.001 |
P-value represents significance of entire set of responses.
P-value refers to the adjusted odds ratio.
English speakers were more likely to be male and younger compared with non-English speakers, but neither of these variables remained significant in the logistic regression. Language, however, remained strongly associated with attendance rates when analysis was controlled for sex and age as potential confounders. English speakers were also more likely to have multiple indicators of low socioeconomic status, including homelessness, unemployment, substance abuse, psychiatric disease and lack of income. All these variables were evaluated, but only lack of income was significant in the controlled multivariable analysis. We created a composite socioeconomic status variable that integrated these five variables. When the composite variable was added to the logistic regression depicted in table 4, it was not statistically significant and did not improve the fit of the model. When lack of an income source was removed from the model, the composite socioeconomic status variable gained significance, but the model fit did not improve compared with the original model. Lack of income is therefore the socioeconomic variable most highly associated with clinic attendance, and was the only socioeconomic variable retained in the final regression model.
Classification analysis
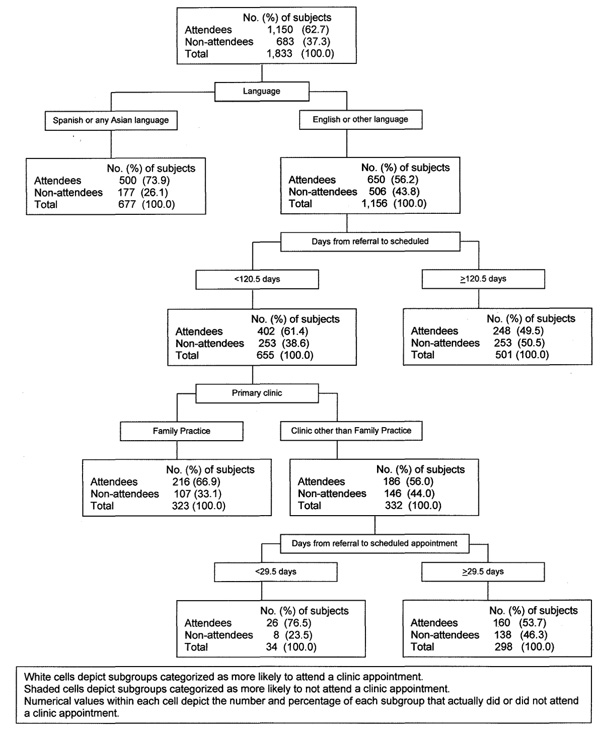
The top node in the classification tree (figure 1) includes all subjects in the study. The first split was made on the basis of primary language, identifying language as the variable most highly associated with appointment attendance. 73.9% of Spanish and Asian language speakers attended versus 56.2% of other subjects. Among Spanish and Asian language speakers, no further splits were made. Among speakers of English or “other” languages, a scheduled appointment in 120.5 days or less was predictive of attendance. Further subgroups are interpreted in a similar fashion. Only the initial split on language withstood cross-validation; other splits were not reliably reproducible from a classification perspective, reinforcing the strength of the association between language and attendance rates in this patient population.
Figure 1.
Classification tree analysis evaluating subjects likelihood of attending or not attending an appointment.
Discussion
Among patients served by the safety net healthcare system of San Francisco, patients speaking languages other than English attended scheduled gastroenterology clinic appointments at higher rates than English speakers. Although other variables contributed to attendance rates, language was the variable most highly associated with attendance.
We chose a priori to focus on the role of language and race/ethnicity for several reasons. These patient-related variables are of sufficient significance to merit inclusion as a prominent component of Healthy People 2010, 40 because non-English speakers and nonwhite patients have been repeatedly found to experience significant barriers to healthcare resulting in reduced healthcare access. Because all the patients in our population have healthcare access, we wanted to determine whether barriers to clinic attendance also existed on the basic of language and race/ethnicity. Multiple inputs, including measures of socioeconomic status, language, transportation, insurance status, and psychiatric comorbidities likely contribute to clinic attendance, and we included many of these in our analyses. We did not intend to identify a causal role for language or race/ethnicity in determining clinic attendance rates, but sought to determine whether these were associated with clinic attendance. The identification of groups at higher risk of nonattendance may facilitate development of interventions to improve attendance, which could increase clinic efficiency and improve patient outcomes.
We found other studies of race/ethnicity and language to be of limited applicability to safety net populations, since most have not been performed among these specific populations. In other studies, there are significant differences in income and other measures of socioeconomic status between English and non-English speakers and between whites and nonwhites. 15,16,17,19,20 The magnitude of such differences in our population was small (for example, mean monthly income was $734 for English speakers versus $864 for non-English speakers, and $761 for whites versus $801 for nonwhites), and we adjusted for these in the multivariable analyses.
Our results differ from most prior studies of language, which document lower rates of healthcare access and utilization among non-English speakers compared with English speakers.19,20,21,22,23 Differences in our study population compared with other studies of healthcare access and utilization may partially explain our findings, because our study was undertaken within a safety net healthcare setting. Our findings may reflect differences in the selective forces that lead English speakers and non-English speakers to seek care in a safety net healthcare system. Non-English speakers are more likely than English speakers to be first-generation immigrants.41 An individual who successfully immigrates to the United States may have beliefs, practices, and social networks that helped them navigate the complex immigration system and a new country of residence (the “healthy immigrant effect”42), and those factors may facilitate attendance at clinic appointments. Such social networks might also provide practical assistance with appointment-related tasks such as reminding patients of appointments and providing transportation and child- or elder-care. Conversely, English speakers in our study had significantly higher rates of homelessness, joblessness, substance abuse, and mental illness. None of these variables remained significant in the multivariable analyses (either independently or when constructed as a composite socioeconomic status variable), but taken together, they may represent higher levels of marginalization among English speakers compared with non-English speakers, which may contribute to lower clinic attendance rates.
Differences in our research question compared with prior studies may also explain our distinct findings. Most studies evaluate differences in access to healthcare among different patient groups. As a recent example for comparison, Ananthakrishnan et al studied colorectal cancer screening in Medicare beneficiaries, comparing rates of screening in white versus nonwhite patients.18 To receive screening, patients had to have a provider who offered screening, patients had to schedule an appointment, and they had to attend the appointment and receive screening; it was not possible to separate patient, provider, and systems related factors that affected utilization of colorectal cancer screening. Our study, alternatively, looked at the more specific question of what patient factors were associated with attendance at scheduled gastroenterology clinic appointments among patients with established healthcare access and a scheduled clinic appointment. The presence of a primary care provider and an established appointment in the gastroenterology clinic minimized access barriers and systems related factors that have been the focus of other studies. Referrals were reviewed and judged to be appropriate by both a primary care provider and a gastroenterologist. This minimized inappropriate referrals and provider related factors that may affect other studies. Our more focused analysis may therefore have revealed patient related factors affecting subspecialty clinic attendance that were previously obscured by systems and provider related factors relating to healthcare access, and this may explain the uniqueness of our findings.
SFGH has employed multiple efforts to improve healthcare access among non-English speakers and has won several awards for their interpreter services. Many employees, including front desk staff, nurses, and physicians, speak Spanish, Chinese dialects, and other non-English languages. Educational materials and forms are available in multiple languages. SFGH has one of the most comprehensive interpreter services in the nation, including a large trained interpreter staff, video medical interpreters, and phone interpreter services. Many clinics are located in neighborhoods where non-English speakers live, and these often employ persons from similar racial/ethnic groups to the populations that utilize them. All of these efforts may increase the attractiveness of the SFGH system to non-English speakers, and this may partially account for their higher attendance rates.
Because the patient population in which we performed our study is highly selected, our results are not universally generalizable, but may be generalizable to other safety net systems in diverse urban communities. We evaluated only a single clinic type, but our findings may be applicable to other subspecialty clinic types, especially those within safety net healthcare populations. Because all referrals were evaluated by a single gastroenterologist (HFY), selection bias may affect our results, but it is unclear how this would occur on the basis of language. All patients were sent notification of their appointment date and time by telephone and/or mailed postcards, but we were unable to determine which patients actually received notification, and there was no mechanism to determine reasons for missed appointments. We were unable to systematically evaluate reasons for, or urgency of, patient referral, owing to lack of a standardized categorization scheme. Patients with urgent or symptomatic reasons for referral might be more likely to attend appointments, but it is not clear how this would relate to language.
Subspecialty care may improve outcomes for specific diseases when compared with generalist care and may lower mortality rates among patients receiving both subspecialty and general care compared with either alone. 43,44 Gastroenterology is a limited subspecialty resource throughout the United States, and with supply expected to further decrease among vulnerable patient populations, 8 it is vital that attendance at scheduled appointments be optimized in these patient groups. Even when applied to other, more privileged populations, our study underscores the importance of evaluating which patients attend clinic appointments and which patients fail to attend, so that the efficiency and quality of subspecialty healthcare provided may be increased.
Acknowledgement
We thank Mark Segal, PhD and Barbara Grimes, PhD, University of California San Francisco Division of Biostatistics, for their assistance with statistical analysis; Scott Biggins, MD, MAS, University of California San Francisco Division of Gastroenterology, for his help with interim analysis; Jennifer Thomas, University of California San Francisco Department of Medicine, for her administrative assistance. The services of Drs. Segal and Grimes were compensated through the University of California San Francisco Biostatistical Unit. None of the other individuals in this acknowledgment received additional compensation for their work with this article.
Funding sources:
- This study was supported in part by the William and Mary Ann Rice Memorial Distinguished Professorship (HY) and the Dean Craig Endowed Chair (JI).
- This study was supported in part by Grant Number R01 CA106773 from the National Cancer Institute.
- This study was supported in part by Grant Number 1 UL1 RR024131-01 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research, and its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR of NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Footnotes
Conflicts of interest: none to report.
Contributor Information
Justin L. Sewell, Email: justin.sewell@ucsf.edu, Department of Medicine, University of California San Francisco, San Francisco, California..
Margot B. Kushel, Email: mkushel@medsfgh.ucsf.edu, Division of General Internal Medicine, San Francisco General Hospital, Department of Medicine, University of California San Francisco, San Francisco, California..
John M. Inadomi, Email: jinadomi@medsfgh.ucsf.edu, Division of Gastroenterology and Hepatology, San Francisco General Hospital, Department of Medicine, University of California San Francisco, San Francisco, California..
Hal F. Yee, Jr., Division of Gastroenterology and Hepatology, San Francisco General Hospital, Department of Medicine, University of California San Francisco, San Francisco, California..
REFERENCES
- 1.Turner AG, Cooke H. Are patients’ attitudes the cause of long waiting lists? Br J Clin Pract. 1991;45:97–98. [PubMed] [Google Scholar]
- 2.Prentice JC, Pizer SD. Delayed access to health care and mortality. Health Serv Res. 2007;42:644–662. doi: 10.1111/j.1475-6773.2006.00626.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nancollas C, Foster R, Minns S. Should doctors charge patients for missed appointments? BMJ Careers. 2005;331:gp85. [Google Scholar]
- 4.Rhee MK, Slocum W, Ziemer DC, et al. Patient adherence improves glycemic control. Diabetes Educ. 2005;31:240–250. doi: 10.1177/0145721705274927. [DOI] [PubMed] [Google Scholar]
- 5.Catz SL, McClure JB, Jones GN, et al. Predictors of outpatient medical appointment attendance among persons with HIV. AIDS Care. 1999;11:361–373. doi: 10.1080/09540129947983. [DOI] [PubMed] [Google Scholar]
- 6.Campbell JD, Chez RA, Queen T, et al. The no-show rate in a high-risk obstetric clinic. J Womens Health Gend Based Med. 2000;9:891–895. doi: 10.1089/152460900750020928. [DOI] [PubMed] [Google Scholar]
- 7.Catz SL, McClure JB, Jones GN, et al. Predictors of outpatient medical appointment attendance among persons with HIV. AIDS Care. 1999;11:361–373. doi: 10.1080/09540129947983. [DOI] [PubMed] [Google Scholar]
- 8.California HealthCare Foundation. [Accessed July 27];Examining Access to Specialty Care for California’s Uninsured: Full Report. 2007 http://www.fachc.org/cd_AccessToSpecialtyCareForCalifUninsuredReport.pdf.
- 9.Brown ML, Klabunde CN, Mysliwiec P. Current capacity for endoscopic colorectal cancer screening in the United States: data from the National Cancer Institute survey of colorectal cancer screening practices. Am J Med. 2003;115:129–133. doi: 10.1016/s0002-9343(03)00297-3. [DOI] [PubMed] [Google Scholar]
- 10.Murdock A, Rodgers C, Lindsay H, et al. Why do patients not keep their appointments? Prospective study in a gastroenterology outpatient clinic. J R Soc Med. 2002;95:284–286. doi: 10.1258/jrsm.95.6.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Regenstein M, Huang JH. Stresses to the safety net: the public hospital perspective. [Accessed 12/23/2007];Report of the Kaiser Commission on Medicaid and the Uninsured. 2005 September; Available online at http://www.kff.org/medicaid/upload/Stresses-to-the-Safety-Net.pdf.
- 12.Phillips KA, Mayer ML, Aday LA. Barriers to care among racial/ethnic groups under managed care. Health Aff. 2000;19:65–75. doi: 10.1377/hlthaff.19.4.65. [DOI] [PubMed] [Google Scholar]
- 13.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 14.Bertoni AG, Goonan KL, Bonds DE, et al. Racial and ethnic disparities in cardiac catheterization for acute myocardial infarction in the United States, 1995–2001. J Natl Med Assoc. 2005;97:317–323. [PMC free article] [PubMed] [Google Scholar]
- 15.Hemingway H, Crook AM, Feder G, et al. Underuse of coronary revascularization procedures in patients considered appropriate candidates for revascularization. New Engl J Med. 2001;344:645–654. doi: 10.1056/NEJM200103013440906. [DOI] [PubMed] [Google Scholar]
- 16.Sonel AF, Good CB, Mulgund J, et al. Racial variations in treatment and outcomes of black and white patients with high-risk non-ST-elevation acute coronary syndromes. Circulation. 2005;111:1225–1232. doi: 10.1161/01.CIR.0000157732.03358.64. [DOI] [PubMed] [Google Scholar]
- 17.Bach PB, Cramer LD, Warren JL, et al. Racial differences in the treatment of early-stage lung cancer. New Engl J Med. 1999;341:1198–1205. doi: 10.1056/NEJM199910143411606. [DOI] [PubMed] [Google Scholar]
- 18.Ananthakrishnan AN, Schellhase KG, Sparapani RA, et al. Disparities in colon cancer screening in the Medicare population. Arch Int Med. 2007;167:258–264. doi: 10.1001/archinte.167.3.258. [DOI] [PubMed] [Google Scholar]
- 19.DuBard CA, Garrett J, Gizlice Z. Effect of language on heart attack and stroke awareness of U.S. Hispanics. Am J Prev Med. 2006;30:189–196. doi: 10.1016/j.amepre.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 20.Ponce NA, Hays RD, Cunningham WE. Linguistic disparities in health care access and health status among older adults. J Gen Int Med. 2006;21:786–791. doi: 10.1111/j.1525-1497.2006.00491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu SM, Huang ZJ, Schwalberg RH, et al. Parental English proficiency and children’s health services access. Am J Public Health. 2006;96:1449–1455. doi: 10.2105/AJPH.2005.069500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fiscella K, Franks P, Doescher MP, et al. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care. 2002;40:52–59. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Ponce NA, Ku L, Cunningham WE, et al. Language barriers to health care access among Medicare beneficiaries. Inquiry. 2006;43:66–76. doi: 10.5034/inquiryjrnl_43.1.66. [DOI] [PubMed] [Google Scholar]
- 24.Gaskin DJ, Hadley J. Population characteristics of markets of safety-net and non-safety-net hospitals. J Urban Health. 1999;76:351–370. doi: 10.1007/BF02345673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. [Accessed July 17, 2007];UCSF School of Medicine - San Francisco General Hospital. http://www.medschool.ucsf.edu/sfgh/Facts/
- 26.Lee VJ, Earnest A, Chen MI, et al. Predictors of failed attendance in a multi-specialty outpatient centre using electronic databases. BMC Health Serv Res. 2005;5:51. doi: 10.1186/1472-6963-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Druss BG, Rosenheck RA. Mental disorders and access to medical care in the United States. Am J Psychiatry. 1998;155:1775–1777. doi: 10.1176/ajp.155.12.1775. [DOI] [PubMed] [Google Scholar]
- 28.Adamson J, Ben-Shlomo Y, Chaturvedi N, et al. Ethnicity, socio-economic position and gender – do they affect reported health-care seeking behaviour? Soc Sci Med. 2003;57:895–904. doi: 10.1016/s0277-9536(02)00458-6. [DOI] [PubMed] [Google Scholar]
- 29.Raine R. Does gender bias exist in the use of specialist health care? J Health Serv Res Policy. 2000;5:237–249. doi: 10.1177/135581960000500409. [DOI] [PubMed] [Google Scholar]
- 30.Rahimi AR, Spertus JA, Reid KJ, et al. Financial barriers to health care and outcomes after myocardial infarction. JAMA. 2007;297:1063–1072. doi: 10.1001/jama.297.10.1063. [DOI] [PubMed] [Google Scholar]
- 31.Palepu A, Cheng DM, Kim T, et al. Substance abuse treatment and receipt of liver specialty care among persons coinfected with HIV/HCV who have alcohol problems. J Subst Abuse Treat. 2006;31:411–417. doi: 10.1016/j.jsat.2006.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schillinger D, Chen AH. Literacy and language: disentangling measures of access, utilization, and quality. J Gen Intern Med. 2004;19:288–290. doi: 10.1111/j.1525-1497.2004.40102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baker DW, Gazmararian JA, Williams MV, et al. Health literacy and the use of outpatient physician services by Medicare managed care enrollees. J Gen Intern Med. 2004;19:215–220. doi: 10.1111/j.1525-1497.2004.21130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krahn GL, Hammond L, Turner A. A cascade of disparities: health and health care access for people with intellectual disabilities. Ment Retard Dev Disabil Res Rev. 2006;12:70–82. doi: 10.1002/mrdd.20098. [DOI] [PubMed] [Google Scholar]
- 35.Caveney AF, Smith MA, Morgenstern LB, et al. Use of death certificates to study ethnic-specific mortality. Public Health Rep. 2006;121:275–281. doi: 10.1177/003335490612100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morgan RO, Wei II, Virnig BA. Improving identification of Hispanic males in Medicare: use of surname matching. Med Care. 2004;42:810–816. doi: 10.1097/01.mlr.0000132392.49176.5a. [DOI] [PubMed] [Google Scholar]
- 37.Winker MA. Measuring race and ethnicity: why and how? JAMA. 2004;292:1612–1614. doi: 10.1001/jama.292.13.1612. [DOI] [PubMed] [Google Scholar]
- 38.Breiman L, Freidman JH, Olshen RA, Stone CJ. The Wadsworth Statistics/Probability Series. Belmont, CA: Wadsworth; 1984. Classification and Regression Trees. [Google Scholar]
- 39.Segal MR, Bloch DA. A comparison of estimated proportional hazards models and regression trees. Stat Med. 1989;8:539–550. doi: 10.1002/sim.4780080503. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: US Government Printing Office; 2000. Nov, [Google Scholar]
- 41.Carliner G. The language ability of U.S. immigrants: assimilation and cohort effects. International Migration Review. 2000;34:158–182. [Google Scholar]
- 42.Antecol H, Bedard K. Unhealthy assimilation: who do immigrants converge to American health status levels? Demography. 2006;43:437–460. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- 43.Smetana GW, Landon BE, Bindman AB, et al. A comparison of outcomes from generalist vs specialist care for a single discrete medical condition. Arch Int Med. 2007;167:10–20. doi: 10.1001/archinte.167.1.10. [DOI] [PubMed] [Google Scholar]
- 44.Indridason OS, Coffman CJ, Oddone EZ. Is specialty care associated with improved survival of patients with congestive heart failure? Am Heart J. 2003;145:300–309. doi: 10.1067/mhj.2003.54. [DOI] [PubMed] [Google Scholar]