Abstract
OBJECTIVE
It is unclear whether the coronary atherosclerotic plaque burden is similar in patients with type 1 and type 2 diabetes. By using multislice computed tomography (MSCT), the presence, degree, and morphology of coronary artery disease (CAD) in patients with type 1 and type 2 diabetes were compared.
RESEARCH DESIGN AND METHODS
Prospectively, coronary artery calcium (CAC) scoring and MSCT coronary angiography were performed in 135 asymptomatic patients (65 patients with type 1 diabetes and 70 patients with type 2 diabetes). The presence and extent of coronary atherosclerosis as well as plaque phenotype were assessed and compared between groups.
RESULTS
No difference was observed in average CAC score (217 ± 530 vs. 174 ± 361) or in the prevalence of coronary atherosclerosis (65% vs. 71%) in patients with type 1 and type 2 diabetes. However, the prevalence of obstructive atherosclerosis was higher in patients with type 2 diabetes (n = 24; 34%) compared with that in patients with type 1 diabetes (n = 11; 17%) (P = 0.02). In addition, a higher mean number of atherosclerotic and obstructive plaques was observed in patients with type 2 diabetes. In addition, the percentage of noncalcified plaques was higher in patients with type 2 (66%) versus type 1 diabetes (27%) (P < 0.001), resulting in a higher plaque burden for each CAC score compared with that in type 1 diabetic patients.
CONCLUSIONS
Although CAC scores and the prevalence of coronary atherosclerosis were similar between patients with type 1 and type 2 diabetes, CAD was more extensive in the latter. Also, a relatively higher proportion of noncalcified plaques was observed in patients with type 2 diabetes. These observations may be valuable in the development of targeted management strategies adapted to diabetes type.
Cardiovascular disease and coronary artery disease (CAD) in particular constitute a major cause of morbidity and mortality in patients with diabetes (1). However, management of this patient population remains challenging. Current European guidelines regard type 2 diabetes as a CAD equivalent, whereas type 1 diabetes is considered a high-risk state only in presence of microalbuminuria (2). In contrast, U.S. guidelines in primary prevention recommend stringent pharmacological therapy with lipid and blood pressure goals comparable to those in secondary prevention for all diabetic patients regardless of type of diabetes (3). Notably, these guidelines are based on clinical trials in patients with type 2 diabetes. However, CAD in type 1 diabetes, which has been studied less extensively, may have a pathophysiology distinct from that in patients with type 2 diabetes. As a result, caution is indicated when clinical observations obtained in patients with type 2 diabetes are extrapolated to patients with type 1 diabetes. To date, it is unclear whether asymptomatic type 1 diabetic patients benefit equally from the current preventive treatment strategies.
To optimize guidelines for type 1 diabetic patients, more detailed understanding of coronary atherosclerosis in type 1 diabetes is required. Thus far, most studies have evaluated the complications and risk factors associated with microvascular disease in this population (4). Studies of CAD have focused mainly on type 1 diabetic patients with kidney failure undergoing coronary angiography before kidney transplantation (5). Limited information is available on the presence and morphology of CAD in asymptomatic patients with type 1 diabetes in daily clinical practice (6).
Multislice computed tomography (MSCT) allows evaluation of the coronary artery calcium (CAC) score and direct assessment of coronary artery integrity. Importantly, in diabetic patients the diagnostic accuracy of MSCT coronary angiography for the detection of significant stenoses has been shown to be similar to that for the general population (7). In addition, the technique provides information on atherosclerotic plaque burden and to some extent on plaque composition (8–10). Previous studies with MSCT revealed an increased prevalence of noncalcified coronary plaques, which have been linked to unstable CAD, in patients with type 2 diabetes (11,12). However, thus far no studies have addressed plaque morphology in patients with type 1 diabetes. To improve understanding of potential differences in pathophysiology and atherosclerotic patterns as well as for development of more targeted management strategies, the evaluation of differences in plaque composition on MSCT may provide valuable information. Therefore, the purpose of the present study was to explore and compare the extent, degree, and morphology of coronary atherosclerosis by MSCT in asymptomatic patients with type 1 and type 2 diabetes recruited from a regular diabetes clinic.
RESEARCH DESIGN AND METHODS
A total of 135 consecutive asymptomatic patients with diabetes were prospectively included from an ongoing registry of new patients at the diabetes outpatient clinic. Diabetic patients were referred to the cardiology outpatient clinic for cardiovascular screening. Patients were stratified as having type 1 or type 2 diabetes according to the American Diabetes Association criteria (13). Plasma levels of C-peptide and autoantibodies to islet cells, insulin, and GAD were determined to distinguish between primary insulinopenia and immune destruction of pancreas β-cells (type 1 diabetes) and insulin resistance (type 2 diabetes).
Asymptomatic status was confirmed using the Rose questionnaire for angina (14). A structured interview, physical examination, and laboratory analysis were obtained for all patients. Cardiovascular risk factors were assessed according to the following criteria: 1) positive family history of CAD (CAD in first-degree family members aged <55 (men) or <65 (women) years), 2) smoking (current smoking or smoking in the past 2 years), 3) hypertension (blood pressure >140/90 mmHg or treatment with antihypertensive medication), 4) hypercholesterolemia (total cholesterol level >5.0 mmol/l or use of cholesterol-lowering medication), 5) obesity (estimated by BMI [weight in kilograms divided by the square of height in meters ]), 6) level of glycemic control defined by plasma A1C (millimoles per liter), 7) diabetic nephropathy (urinary albumin-to-creatinine ratio ≥35 mg/mmol), and 8) renal function (estimated by glomerular filtration rate [GFR]).
Noninvasive MSCT coronary angiography was performed in all patients as part of a clinical protocol. Exclusion criteria were ventricular and supraventricular arrhythmia and contraindications for the use of iodinated contrast media.
MSCT data acquisition
Imaging was performed with a 64-slice MSCT scanner (Toshiba Medical Systems, Tokyo, Japan). For patients with heart rate ≥65 bpm, oral β-blocking medication (50 or 100 mg metoprolol) was provided 1 h preceding the scan, if tolerated. First, a prospective CAC scan without contrast enhancement was performed, followed by MSCT coronary angiography according to protocols described previously (15).
Assessment of CAD by MSCT
CAC score.
The CAC score was assessed using dedicated software (Vitrea2; Vital Images, Minnetonka, MN). CAC was identified as a dense area in the coronary artery exceeding the threshold of 130 Hounsfield units. A total Agatston score was determined for each patient.
Coronary atherosclerosis.
All MSCT coronary angiograms were interpreted by two experienced observers blinded to the patient's characteristics. Discrepancies in interpretation were immediately resolved by consensus. The presence of coronary atherosclerosis was evaluated by scrolling through axial images, followed by visual assessment of curved multiplanar reconstructions in at least two orthogonal planes. Coronary plaques were defined as structures >1 mm2 within and/or adjacent to the coronary artery lumen, which could be clearly distinguished from the vessel lumen and the surrounding pericardial tissue (10).
First, the presence of any atherosclerosis (≥1 plaque in the coronary tree) or multivessel atherosclerosis (≥1 plaque in minimum two coronary arteries) and that of obstructive atherosclerosis (luminal narrowing ≥50%) were evaluated at the patient level in type 1 and type 2 diabetic patients. Thereafter, a more extensive analysis of plaque burden was obtained by registering the total number of atherosclerotic plaques and obstructive plaques for each patient (10). In addition, plaques were classified according to phenotype: 1) noncalcified plaques (plaques with lower density than contrast-enhanced lumen), 2) calcified plaques (plaques with higher density than contrast-enhanced lumen), and 3) mixed plaques (plaques with components of low- and high-density plaques) (8–10).
Statistical analysis
Continuous variables were expressed as means ± SD and compared between the groups of patients with type 1 and type 2 diabetes by using a two-tailed independent t test. Categorical variables were expressed as numbers (percentages) or medians (lower quartile, upper quartile) and compared with a χ2 test. Separate multivariate regression analyses with backward elimination were performed, correcting for all baseline clinical characteristics including age, male sex, BMI, smoking, positive family history of CAD, hypercholesterolemia, hypertension, A1C, GFR, and type of diabetes to identify independent predictors of each coronary atherosclerosis variable on MSCT.
The relationship between CAC scores and extent of coronary atherosclerosis was compared in patients with type 1 and type 2 diabetes. Patients were further classified according to CAC scores: 1) patients without coronary calcium, 2) patients with a CAC score in the range of 1–100, and 3) patients with a CAC score >100. The mean number of atherosclerotic lesions was determined for each CAC score category.
Statistical analyses were performed using SPSS software (version 12.0.1; SPSS, Chicago, IL) and SAS software (version 6.12; SAS Institute, Cary, NC). P < 0.05 was considered statistically significant.
RESULTS
Patient characteristics.
A total of 135 asymptomatic diabetic patients were included in the study. Mean age was 48 ± 10 years, and 79 patients (59%) were male. The study population consisted of 65 patients with type 1 and 70 patients with type 2 diabetes. Baseline characteristics are provided in Table 1. Importantly, age and sex distribution were comparable in patients with type 1 and type 2 diabetes. However, patients with type 2 diabetes had a significantly higher BMI and A1C and a shorter duration of diagnosed diabetes. Other baseline cardiovascular risk factors were similar in the two groups.
Table 1.
Characteristics of the study population
| Type 1 diabetes | Type 2 diabetes | P | |
|---|---|---|---|
| n | 65 | 70 | |
| Age (years) | 46.0 (38.0, 54.5) | 49.5 (45.0, 57.0) | 0.08 |
| Men | 42 (65) | 37 (53) | 0.17 |
| BMI (kg/m2) | 23.8 (22.2, 26.6) | 28.2 (24.9, 33.4) | <0.001 |
| Smokers | 17 (26) | 14 (20) | 0.40 |
| Family history of CAD | 30 (46) | 37 (53) | 0.44 |
| Hypercholesterolemia | 41 (63) | 50 (71) | 0.30 |
| Hypertension | 32 (49) | 43 (61) | 0.22 |
| Duration of diabetes (years) | 23.0 (9.5, 33.0) | 7.5 (2.0, 13.0) | <0.001 |
| A1C (mmol/l) | 7.6 (6.6, 8.6) | 8.3 (7.0, 9.5) | 0.04 |
| GFR (ml/min per 1.73m2) | 101.6 (84.7, 122.8) | 98.4 (81.8, 124.8) | 0.88 |
| Albuminuria* | 1 (2) | 4 (6) | 0.20 |
Data are medians (lower quartile, upper quartile) or number of patients (%). n = 135.
*Albuminuria was defined by a urine albumin-to-creatinine ratio ≥35 mg/mmol.
Assessment of CAD by MSCT
CAD at patient level.
Results of CAD assessment by MSCT are illustrated in Table 2. The mean CAC score and prevalence of atherosclerosis were similar among patients with type 1 and type 2 diabetes. However, the prevalence of multivessel atherosclerosis was higher in patients with type 2 (n = 41; 59%) than in patients with type 1 (n = 19; 29%) diabetes (P = 0.001). Finally, obstructive stenosis was more prevalent in patients with type 2 diabetes (n = 24; 34%) than in patients with type 1 diabetes (n = 11; 17%) (P = 0.02).
Table 2.
Results of MSCT coronary angiography
| Type 1 diabetes | Type 2 diabetes | P | |
|---|---|---|---|
| Patients | |||
| Coronary artery calcium scores | 217 ± 530 | 174 ± 361 | 0.59 |
| Atherosclerosis | 42 (65) | 50 (71) | 0.40 |
| Atherosclerosis, multivessel | 19 (29) | 41 (59) | 0.001 |
| Obstructive atherosclerosis* | 11 (17) | 24 (34) | 0.02 |
| Plaques | |||
| No. of plaques | 3.4 ± 4.8 | 9.9 ± 11.9 | <0.001 |
| No. of obstructive plaques | 0.5 ± 1.4 | 1.7 ± 3.9 | 0.02 |
| No. of noncalcified plaques | 1.0 ± 1.3 | 6.5 ± 9.5 | <0.001 |
| No. of mixed plaques | 0.7 ± 1.3 | 1.1 ± 1.9 | 0.25 |
| No. of calcified plaques | 1.8 ± 3.6 | 2.2 ± 3.9 | 0.52 |
Data are means ± SD or number of patients (%).
*Obstructive atherosclerosis was defined as luminal narrowing ≥50%.
Plaque analysis.
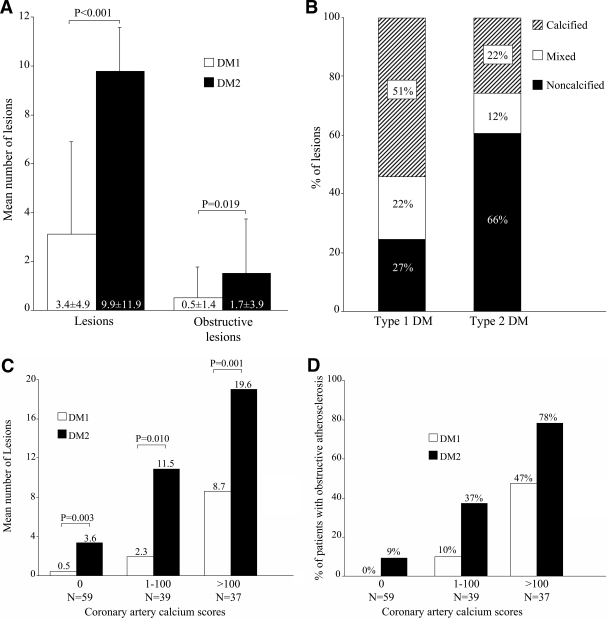
Quantification of the total number of atherosclerotic plaques for each patient revealed a significantly higher mean number of lesions in patients with type 2 diabetes (9.9 ± 11.9) compared with that in patients with type 1 diabetes (3.4 ± 4.8) (P < 0.001) (Fig. 1A). In addition, the mean number of obstructive plaques was significantly higher in patients with type 2 diabetes (1.7 ± 3.9) than in patients with type 1 diabetes (0.5 ± 1.4) (P = 0.02) (Fig. 1A).
Figure 1.
A: Clustered columns demonstrating average number of lesions and obstructive lesions in type 1 (DM1) and type 2 (DM2) diabetes. A significantly higher mean number of lesions and obstructive lesions were observed in type 2 diabetes. B: Bar graph illustrating plaque phenotype in type 1 and type 2 diabetes. A higher percentage of noncalcified plaques was observed in type 2 diabetes. C: Clustered bar graph illustrating the increase in number of lesions for each CAC score category among patients with type 1 and type 2 diabetes. The plaque burden was significantly higher in type 2 diabetes for each CAC score category. D: Clustered bar graph demonstrating the increase in prevalence of obstructive atherosclerosis for each CAC score category among patients with type 1 and type 2 diabetes. An absence of coronary calcium excluded obstructive atherosclerosis in type 1 diabetes, but not in type 2 diabetes. The prevalence of obstructive atherosclerosis was higher in type 2 diabetes for each CAC score category.
Analysis of plaque phenotype showed a higher mean number of noncalcified plaques in patients with type 2 diabetes (6.5 ± 9.5) versus patients with type 1 diabetes (1.0 ± 1.3) (P < 0.001), whereas the mean number of mixed and calcified plaques was not significantly different. Accordingly, a higher proportion of noncalcified plaques was observed in patients with type 2 diabetes (66%) compared with patients with type 1 diabetes (27%) (P < 0.001) (Fig. 1B).
Relation between type of diabetes and the presence and extent of CAD
To correct for baseline characteristics, the relation between type 2 diabetes (compared with type 1 diabetes) and the presence and extent of CAD were evaluated using multivariate regression analyses (Table 3 ). Although type of diabetes was not related to the presence of any atherosclerosis, type 2 diabetes was strongly related to the extent and degree of coronary atherosclerosis after correction for all other risk factors. In addition, an independent association was observed between the presence of type 2 diabetes and number of noncalcified coronary plaques.
Table 3.
Presence of type 2 diabetes (not type 1 diabetes) as a predictor of MSCT variables: results of multivariate analysis in a backward regression model
| Hazard ratio β (95% CI) | P | |
|---|---|---|
| Patients | ||
| Coronary artery calcium scores* | — | NS |
| Atherosclerosis† | — | NS |
| Atherosclerosis, multivessel† | 4.16 (1.76–9.93) | 0.001 |
| Obstructive atherosclerosis†‡ | 4.01 (1.38–11.60) | 0.01 |
| Plaques | ||
| No. of plaques* | 6.82 (3.51–10.13) | <0.001 |
| No. of obstructive plaques* | 1.40 (1.32–2.48) | 0.01 |
| No. of noncalcified plaques* | 6.27 (3.60–8.94) | <0.001 |
| No. of mixed plaques* | — | NS |
| No. of calcified plaques* | — | NS |
The predictive value of type 2 diabetes was tested in a separate multivariate regression model for each MSCT variable.
*Results of analysis in a multivariate linear regression model.
†Results of analysis in a multivariate binary logistic regression model.
‡Obstructive atherosclerosis was defined as luminal narrowing ≥50%.
Relation between CAC scores and atherosclerosis
Comparison of the CAC score versus coronary angiography findings showed that the number of atherosclerotic lesions paralleled the increase in coronary calcium (Fig. 1C). However, for each CAC score category the mean number of atherosclerotic lesions was significantly higher in patients with type 2 diabetes (Fig. 1C).
Similarly, the prevalence of obstructive atherosclerosis increased per CAC score category (Fig. 1D). Importantly, absence of coronary calcium excluded the presence of obstructive atherosclerosis in patients with type 1 diabetes, whereas obstructive atherosclerosis was identified in three patients with type 2 diabetes (9%). In patients with a CAC score ≤100, obstructive atherosclerosis was found in only 2 (4%) type 1 diabetic patients, whereas 10 (19%) type 2 diabetic patients showed obstructive CAD.
CONCLUSIONS
In the present study, no significant difference was observed in the prevalence of atherosclerosis in asymptomatic patients with type 1 and type 2 diabetes. However, in patients with type 1 diabetes, multivessel disease was less prevalent and a lower atherosclerotic plaque burden was observed. Moreover, the number of obstructive coronary lesions was significantly lower in patients with type 1 diabetes. The presence of type 2 diabetes (as opposed to type 1 diabetes) was shown to be an independent predictor of extent and degree of coronary atherosclerosis on MSCT angiography. Second, for each CAC score category a higher atherosclerotic plaque burden was observed in patients with type 2 diabetes. This observation was explained by the high proportion of noncalcified plaques in asymptomatic patients with type 2 diabetes compared with a high proportion of calcified plaques in patients with type 1 diabetes.
Plaque burden
Most previous studies on the prevalence of coronary atherosclerosis have used conventional coronary angiography to examine patients with a clinical suspicion of CAD and observed more extensive CAD in diabetic patients than in their nondiabetic counterparts (16,17). Limited studies have been performed in asymptomatic diabetic patients. MSCT provides accurate noninvasive evaluation of the extent and degree of coronary atherosclerosis and may be used in patients with a lower likelihood of CAD. Importantly, excellent sensitivity, specificity, and negative predictive values for detection of significant stenosis have also been shown in diabetic patients (7). Thus far, the technique has been used in several studies to explore the presence and extent of CAD in patients with type 2 diabetes. Scholte et al. (12) observed a high prevalence of coronary atherosclerosis (80%), which predominantly involved more than one coronary artery (74%), in asymptomatic type 2 diabetic patients. Obstructive CAD was observed in 26% of patients, similar to observations in the current study. Thus far, no MSCT studies have reported on the presence of CAD in asymptomatic type 1 diabetic patients.
However, using magnetic resonance imaging, Kim et al. (6) previously evaluated CAD in asymptomatic patients with type 1 diabetes and observed a higher atherosclerotic plaque burden in the presence of diabetic nephropathy compared with that in normoalbuminuria. In that particular study, an absence of diabetic nephropathy excluded the presence of subclinical obstructive CAD. In our current study, the prevalence of nephropathy was low (1%) in type 1 diabetic patients, suggesting that these patients were at relatively low risk. Interestingly, however, the absence of nephropathy did not exclude subclinical obstructive CAD on MSCT. Nevertheless, compared with type 2 diabetes, the extent of atherosclerosis was less severe with a lower prevalence of multivessel disease and fewer lesions. Moreover, a smaller proportion of patients with type 1 diabetes had obstructive atherosclerosis. Importantly, in this study, the presence of type 2 diabetes remained a significant predictor of the severity of atherosclerosis after correction for traditional cardiovascular risk factors including obesity, glycemic control, and renal function. Accordingly, the higher atherosclerotic plaque burden in patients with type 2 diabetes may warrant more aggressive antiatherosclerotic treatment. On the other hand, MSCT coronary angiography excluded atherosclerosis in ∼30% of both type 1 and type 2 diabetic patients. This finding raises the question of whether antiatherosclerotic medical therapy should be initiated in all asymptomatic diabetic patients and to what extent. It is possible that MSCT may be used to identify or exclude the presence of atherosclerosis and provide a basis for individually tailored therapy.
Plaque morphology and relation with CAC
In addition to increased severity of atherosclerosis, we also observed differences in relative plaque composition in patients with type 2 diabetes with a higher percentage of noncalcified plaques. This finding is in line with a previous study in which noncalcified plaques comprised 41% of atherosclerotic plaques in asymptomatic patients with type 2 diabetes (12). In retrospective studies, a higher proportion of noncalcified plaques has been associated with unstable CAD. Preliminary prognostic data also suggest that the presence of substantial noncalcified plaque indeed confers a worse outcome (18). Accordingly, it has been suggested that these plaques represent more active stages of CAD and may be more prone to rupture (15,19). Notably, the distribution of coronary plaque phenotype has not been examined previously in type 1 diabetes. In contrast with patients with type 2 diabetes, we found a higher proportion of calcified plaques and a lower proportion of noncalcified plaques in patients with type 1 diabetes, despite similar CAC scores. As a result, plaque burden was higher for each CAC score category in type 2 compared with type 1 diabetic patients.
Assessment of CAC score has been suggested as a primary step in cardiovascular risk stratification and screening of asymptomatic diabetic patients (20) because the presence of elevated CAC scores has been associated with a higher likelihood of myocardial ischemia (21). However, our current observations suggest that CAC score assessment may be more effective in identifying CAD in patients with type 1 diabetes. Indeed, the absence of coronary calcium accurately excluded the presence of obstructive coronary atherosclerosis in patients with type 1 diabetes. In contrast, this relation was distorted in patients with type 2 diabetes with a higher prevalence of obstructive CAD in patients without or only minor calcium. As both the prevalence of obstructive CAD and extent of CAD per CAC category were higher, it appears that CAC scores may underestimate CAD in patients with type 2 diabetes, in line with previous comparisons with nondiabetic patients (22). Accordingly, strategies using CAC scores to identify diabetic patients at higher risk should be developed with caution and should potentially be adjusted for type of diabetes.
Study limitations
Several limitations need to be acknowledged. The current analysis was restricted to evaluation of coronary atherosclerosis in patients with type 1 and type 2 diabetes, and the proatherogenic processes involved in each form of diabetes were not investigated. In addition, the lack of a control group without diabetes should be acknowledged. Because MSCT coronary angiography involves radiation exposure, it is not feasible to perform a similar assessment in asymptomatic subjects free of cardiovascular risk. Furthermore, MSCT coronary angiography requires administration of potentially nephrotoxic contrast media, rendering the technique unsuitable for use in asymptomatic diabetic patients with severe renal dysfunction. Finally, no follow-up data were available. Indeed, the prognostic implications of our observations should be evaluated in prospective follow-up studies.
In summary, although CAC scores and the prevalence of coronary atherosclerosis were similar between patients with type 1 and type 2 diabetes, CAD was more extensive in the latter. In addition, a relatively higher proportion of noncalcified plaques was observed in patients with type 2 diabetes. These observations may be valuable in the development of targeted management strategies adapted to diabetes type. It is possible that MSCT angiography may be useful to identify or exclude the presence of atherosclerosis and provide a basis for individually tailored therapy.
Acknowledgments
J.W.J. received grants from Biotronik (Berlin, Germany), Boston Scientific (Natick, MA), Astra Zeneca (London, U.K.), Pfizer (New York, NY), and Merck Sharp and Dohme (Rahway, NJ). J.J.B. received grants from Medtronic (Minneapolis, MN), Biotronik (Berlin, Germany), Boston Scientific (Natick, MA), BMS Medical Imaging (North Billerica, MA), St. Jude Medical (St. Paul, MN), GE Healthcare (Buckinghamshire, U.K.), and Edwards Lifesciences (Irvine, CA). No other potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H: Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia 44 Suppl 2001; 2: S14– S21 [DOI] [PubMed] [Google Scholar]
- 2. De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J, Ebrahim S, Faergeman O, Graham I, Mancia G, Manger Cats V, Orth-Gomér K, Perk J, Pyörälä K, Rodicio JL, Sans S, Sansoy V, Sechtem U, Silber S, Thomsen T, Wood D: European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J 2003; 24: 1601– 1610 [DOI] [PubMed] [Google Scholar]
- 3. Buse JB, Ginsberg HN, Bakris GL, Clark NG, Costa F, Eckel R, Fonseca V, Gerstein HC, Grundy S, Nesto RW, Pignone MP, Plutzky J, Porte D, Redberg R, Stitzel KF, Stone NJ. the American Heart Association, the American Diabetes Association. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care 2007; 30: 162– 172 [DOI] [PubMed] [Google Scholar]
- 4. Libby P, Nathan DM, Abraham K, Brunzell JD, Fradkin JE, Haffner SM, Hsueh W, Rewers M, Roberts BT, Savage PJ, Skarlatos S, Wassef M, Rabadan-Diehl C: Report of the National Heart, Lung, and Blood Institute-National Institute of Diabetes and Digestive and Kidney Diseases Working Group on Cardiovascular Complications of Type 1 Diabetes Mellitus. Circulation 2005; 111: 3489– 3493 [DOI] [PubMed] [Google Scholar]
- 5. Manske CL, Wilson RF, Wang Y, Thomas W: Prevalence of, and risk factors for, angiographically determined coronary artery disease in type I-diabetic patients with nephropathy. Arch Intern Med 1992; 152: 2450– 2455 [PubMed] [Google Scholar]
- 6. Kim WY, Astrup AS, Stuber M, Tarnow L, Falk E, Botnar RM, Simonsen C, Pietraszek L, Hansen PR, Manning WJ, Andersen NT, Parving HH: Subclinical coronary and aortic atherosclerosis detected by magnetic resonance imaging in type 1 diabetes with and without diabetic nephropathy. Circulation 2007; 115: 228– 235 [DOI] [PubMed] [Google Scholar]
- 7. Schuijf JD, Bax JJ, Jukema JW, Lamb HJ, Vliegen HW, Salm LP, de Roos A, van der Wall EE: Noninvasive angiography and assessment of left ventricular function using multislice computed tomography in patients with type 2 diabetes. Diabetes Care 2004; 27: 2905– 2910 [DOI] [PubMed] [Google Scholar]
- 8. Achenbach S, Moselewski F, Ropers D, Ferencik M, Hoffmann U, MacNeill B, Pohle K, Baum U, Anders K, Jang IK, Daniel WG, Brady TJ: Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: a segment-based comparison with intravascular ultrasound. Circulation 2003; 109: 14– 17 [DOI] [PubMed] [Google Scholar]
- 9. Leber AW, Becker A, Knez A, von Ziegler F, Sirol M, Nikolaou K, Ohnesorge B, Fayad A, Becker CR, Reiser M, Steinbeck G, Boekstegers P: Accuracy of 64-slice computed tomography to classify and quantify plaque volumes in the proximal coronary system: a comparative study using intravascular ultrasound. J Am Coll Cardiol 2006; 47: 672– 677 [DOI] [PubMed] [Google Scholar]
- 10. Leber AW, Knez A, Becker A, Becker C, von Ziegler F, Nikolaou K, Rist C, Reiser M, White C, Steinbeck G, Boekstegers P: Accuracy of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques: a comparative study with intracoronary ultrasound. J Am Coll Cardiol 2004; 43: 1241– 1247 [DOI] [PubMed] [Google Scholar]
- 11. Rivera JJ, Nasir K, Choi EK, Yoon YE, Chun EJ, Choi SI, Choi DJ, Brancati FL, Blumenthal RS, Chang HJ: Detection of occult coronary artery disease in asymptomatic individuals with diabetes mellitus using non-invasive cardiac angiography. Atherosclerosis 2009; 203: 442– 448 [DOI] [PubMed] [Google Scholar]
- 12. Scholte AJ, Schuijf JD, Kharagjitsingh AV, Jukema JW, Pundziute G, van der Wall EE, Bax JJ: Prevalence of coronary artery disease and plaque morphology assessed by multi-slice computed tomography coronary angiography and calcium scoring in asymptomatic patients with type 2 diabetes. Heart 2008; 94: 290– 295 [DOI] [PubMed] [Google Scholar]
- 13. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 20: 1183, 1997 [DOI] [PubMed] [Google Scholar]
- 14. Rose G, McCartney P, Reid DD: Self-administration of a questionnaire on chest pain and intermittent claudication. Br J Prev Soc Med 1977; 31: 42– 48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Henneman MM, Schuijf JD, Pundziute G, van Werkhoven JM, van der Wall EE, Jukema JW, Bax JJ: Noninvasive evaluation with multislice computed tomography in suspected acute coronary syndrome: plaque morphology on multislice computed tomography versus coronary calcium score. J Am Coll Cardiol 2008; 52: 216– 222 [DOI] [PubMed] [Google Scholar]
- 16. Pajunen P, Taskinen MR, Nieminen MS, Syvänne M: Angiographic severity and extent of coronary artery disease in patients with type 1 diabetes mellitus. Am J Cardiol 2000; 86: 1080– 1085 [DOI] [PubMed] [Google Scholar]
- 17. Koistinen MJ: Prevalence of asymptomatic myocardial ischaemia in diabetic subjects: BMJ 1990; 301: 92– 95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. van Werkhoven JM, Schuijf JD, Gaemperli O, Jukema JW, Boersma E, Wijns W, Stolzmann P, Alkadhi H, Valenta I, Stokkel MPM, Kroft LJ, de Roos A, Pundziute G, Scholte A, van der Wall EE, Kaufmann P, Bax JJ: Prognostic value of multi-slice computed tomography and gated single photon emission computed tomography in patients with suspected coronary artery disease. J Am Coll Cardiol 2009; 53: 623– 632 [DOI] [PubMed] [Google Scholar]
- 19. Hoffmann U, Moselewski F, Nieman K, Jang IK, Ferencik M, Rahman AM, Cury RC, Abbara S, Joneidi-Jafari H, Achenbach S, Brady TJ: Noninvasive assessment of plaque morphology and composition in culprit and stable lesions in acute coronary syndrome and stable lesions in stable angina by multidetector computed tomography. J Am Coll Cardiol 2006; 47: 1655– 1662 [DOI] [PubMed] [Google Scholar]
- 20. Moser KW, O'Keefe JH, Bateman TM, McGhie IA: Coronary calcium screening in asymptomatic patients as a guide to risk factor modification and stress myocardial perfusion imaging. J Nucl Cardiol 2003; 10: 590– 598 [DOI] [PubMed] [Google Scholar]
- 21. Anand DV, Lim E, Hopkins D, Corder R, Shaw LJ, Sharp P, Lipkin D, Lahiri A: Risk stratification in uncomplicated type 2 diabetes: prospective evaluation of the combined use of coronary artery calcium imaging and selective myocardial perfusion scintigraphy. Eur Heart J 2006; 27: 713– 721 [DOI] [PubMed] [Google Scholar]
- 22. Raggi P, Shaw LJ, Berman DS, Callister TQ: Prognostic value of coronary artery calcium screening in subjects with and without diabetes. J Am Coll Cardiol 2004; 43: 1663– 1669 [DOI] [PubMed] [Google Scholar]