Abstract
OBJECTIVE
The potential benefits of continuous glucose monitoring (CGM) in the management of adults and children with well-controlled type 1 diabetes have not been examined.
RESEARCH DESIGN AND METHODS
A total of 129 adults and children with intensively treated type 1 diabetes (age range 8–69 years) and A1C <7.0% were randomly assigned to either continuous or standard glucose monitoring for 26 weeks. The main study outcomes were time with glucose level ≤70 mg/dl, A1C level, and severe hypoglycemic events.
RESULTS
At 26 weeks, biochemical hypoglycemia (≤70 mg/dl) was less frequent in the CGM group than in the control group (median 54 vs. 91 min/day), but the difference was not statistically significant (P = 0.16). Median time with a glucose level ≤60 mg/dl was 18 versus 35 min/day, respectively (P = 0.05). Time out of range (≤70 or >180 mg/dl) was significantly lower in the CGM group than in the control group (377 vs. 491 min/day, P = 0.003). There was a significant treatment group difference favoring the CGM group in mean A1C at 26 weeks adjusted for baseline (P < 0.001). One or more severe hypoglycemic events occurred in 10 and 11% of the two groups, respectively (P = 1.0). Four outcome measures combining A1C and hypoglycemia data favored the CGM group in comparison with the control group (P < 0.001, 0.007, 0.005, and 0.003).
CONCLUSIONS
Most outcomes, including those combining A1C and hypoglycemia, favored the CGM group. The weight of evidence suggests that CGM is beneficial for individuals with type 1 diabetes who have already achieved excellent control with A1C <7.0%.
Over the past 15 years, the use of rapid and long-acting insulin analogs, improvements in insulin pumps, and more frequent home blood glucose monitoring have had a positive impact on the ability to achieve target A1C levels in type 1 diabetes. However, the rates of severe hypoglycemia remain too high and the occurrence of such events is often followed by a decline in glycemic control due to fears of further hypoglycemic episodes (1). Hypoglycemia remains the major limiting factor for achieving euglycemia in type 1 diabetes (2).
The introduction of new real-time continuous glucose monitoring (CGM) systems has generated great interest because these devices may have the potential to increase the proportion of patients who are able to maintain target A1C values while simultaneously limiting the risk of severe hypoglycemia. In a randomized trial of 322 adults and children with type 1 diabetes and baseline A1C level ≥7.0%, our Juvenile Diabetes Research Foundation (JDRF) Continuous Glucose Monitoring Study Group reported that CGM substantially improved A1C levels without increasing the frequency of hypoglycemia in adults ≥25 years of age, whereas the lowering of A1C levels in children and adolescents was more limited (3). As with virtually every other study of a new drug or device in the treatment of type 1 diabetes, this study excluded individuals already reaching target A1C levels <7.0% because lowering of A1C was the primary outcome of interest. Consequently, our study group also conducted a separate, concurrent randomized trial to evaluate the efficacy and safety of CGM in adults and children with type 1 diabetes who already had successfully achieved A1C levels <7.0% with intensive insulin therapy.
RESEARCH DESIGN AND METHODS
The protocol was approved by the institutional review boards of the 10 participating centers, which included academic-, community-, and managed care–based practices. Written informed consent was obtained from adult subjects and parents/guardians of minor subjects. Minor subjects provided written assent. Study procedures were identical to those of a companion trial of individuals with type 1 diabetes and A1C ≥7.0% (3,4). Key aspects of the study protocol are described in the following.
Major eligibility criteria included age ≥8 years, type 1 diabetes for at least 1 year, use of either an insulin pump or at least three daily insulin injections, and baseline A1C level <7.0%. Subjects who successfully completed a run-in phase of “blinded” CGM use (a modified device in which glucose values were recorded in the receiver but were not visible to the subject) were randomly assigned to either the CGM group or the control group, using a permuted-blocks design stratified by clinical center.
Subjects assigned to the CGM group were provided with one of the following devices: the DexCom SEVEN (DexCom, San Diego, CA), the MiniMed Paradigm REAL-Time Insulin Pump and Continuous Glucose Monitoring System (Medtronic MiniMed, Northridge, CA), or the FreeStyle Navigator (Abbott Diabetes Care, Alameda, CA). Subjects were instructed to use the device on a daily basis and to verify the accuracy of the glucose measurement with a home blood glucose meter (provided by the study) before making management decisions (as per the regulatory labeling of the devices). Subjects in the control group were given blood glucose meters and test strips and asked to perform blood glucose monitoring at least four times daily.
Subjects in both the CGM and control groups were provided with written instructions on how to use the CGM and blood glucose meter data, respectively, to make real-time insulin dose adjustments and on how to use computer software to retrospectively review the glucose data to alter insulin dosing (4,5). Although not required, all subjects had a home computer.
The number of scheduled contacts was identical for both treatment groups. Visits were conducted at 1, 4, 8, 13, 19, and 26 weeks (±1 week), with one scheduled phone contact between each visit, to review glucose data and adjust diabetes management. For 1 week, after the 13- and 26-week visits, the control group used one of the three real-time CGM devices, modified such that the glucose values were recorded but not visible. An additional sensor was used if fewer than 96 h of glucose values overall or 24 h overnight were obtained. Central laboratory A1C was measured at baseline, 13 weeks, and 26 weeks at the University of Minnesota using the Tosoh A1c 2.2 Plus Glycohemoglobin Analyzer method (6). Reportable adverse events included severe hypoglycemia (defined as an event that required assistance from another individual to administer carbohydrate, glucagon, or other resuscitative actions) (7), hyperglycemia resulting in ketoacidosis, unexpected study-related or device-related events, and serious adverse events regardless of causality.
Statistical methods
The primary outcome was the change in the time per day with glucose values ≤70 mg/dl, comparing baseline sensor values with those obtained after the 26-week visit. A sample size of 120 subjects was planned to have 90% power to detect a difference in this outcome between treatment groups, assuming a population difference of 29 min/day, SD of the 26-week values of 59 min/day, correlation between baseline and 26-week values of 0.66 (based on data from a prior study [(8)]), an α level of 0.05, and no more than 15% losses to follow-up.
Analyses followed the “intent-to-treat” principle. Percentages of values less than or greater than a given threshold were converted to minutes per day by multiplying by 1,440. As a result of the skewness of the primary outcome data (P < 0.001 with the Shapiro-Wilk test), a nonparametric approach was followed for the primary analysis using an ANCOVA model based on ranks of the 26-week values using van der Waerden scores, adjusted for the baseline value, clinical center, and type of continuous glucose monitor. To assess for consistency, two other analytic approaches were used in ANCOVA models. In one, outlier values were truncated at 288 min/day (20% of the day), and in the other, a square root transformation was performed. Other outcomes based on the CGM data obtained in both groups at baseline and 26 weeks were analyzed similarly. Treatment group differences in the rate of CGM-based hypoglycemic events, defined as ≥20 min with a blood glucose of <54 mg/dl (3.0 mmol/l) (9), were compared with the nonparametric approach that was used in the primary analysis.
Other preplanned secondary outcomes included change in A1C from baseline to 26 weeks in an ANCOVA model (adjusted for baseline A1C and clinical center) and 26-week binary A1C outcomes (decrease in A1C from baseline by ≥0.3%, increase in A1C from baseline by ≥0.3%, and 26-week value <7.0%) evaluated similarly in logistic regression models. The 0.3% change was selected because it exceeded the laboratory's measurement error and was considered to be a clinically meaningful change for an A1C level <7.0%.
Analyses also were performed to assess consistency of the treatment effect in subgroups based on age (8–14, 15–24, and ≥25 years). Change in CGM use over time was evaluated with a repeated-measurements regression model. The association of CGM use and age was evaluated with a Kruskal-Wallis test.
The proportions of subjects experiencing one or more severe hypoglycemic events in each treatment group were compared using Fisher's exact test. Incidences of hypoglycemic events were compared, and 95% CIs for the treatment group difference were calculated using permutation tests. Similar analyses were performed for the subset of hypoglycemic events associated with seizure or coma.
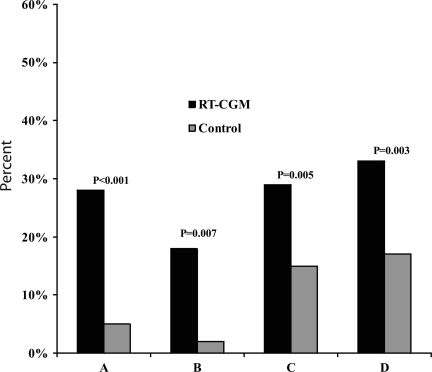
On a subject level, a reduction in time ≤70 mg/dl was defined as a decrease from baseline of ≥43 min/day (3% of the day), and an increase likewise was defined as an increase from baseline of ≥43 min/day (representing an ∼50% change from the average baseline level). Four outcome measures were created by combining A1C and hypoglycemia data (as defined in the legend to Fig. 1) and compared between treatment groups, using a logistic regression model adjusting for baseline A1C.
Figure 1.
Combined A1C and hypoglycemia outcomes. Four outcomes are shown: A, combined outcome of A1C improved by ≥0.3% from baseline to 26 weeks and no severe hypoglycemic events; B, combined outcome of A1C improved by ≥0.3% from baseline to 26 weeks and CGM-measured hypoglycemia (≤70 mg/dl) not increased from baseline to 26 weeks by ≥43 min/day (3% of the day); C, combined outcome of A1C not worse by ≥0.3% and CGM-measured hypoglycemia (≤70 mg/dl) decreased from baseline to 26 weeks by ≥43 min/day (3% of the day); D, combined outcome of either B or C.
Analyses were performed using SAS (version 9.1; SAS Institute, Cary, NC). All P values are two-sided. Adjusting for imbalances between baseline factors and imputing for missing data using Rubin's method (10) did not alter the results (data not shown).
RESULTS
Between February and December 2007, 129 children and adults with type 1 diabetes were randomly assigned in the trial: 67 were assigned to the CGM group and 62 to the control group. Baseline characteristics of the participants are summarized in Table 1.
Table 1.
Baseline characteristics of study subjects by treatment group
| Treatment group |
||
|---|---|---|
| CGM | Control | |
| n | 67 | 62 |
| Female sex | 36 (54) | 32 (52) |
| Age (years) | 29.3 ± 16.3 | 32.0 ± 17.7 |
| ≥25 | 34 (51) | 33 (53) |
| 15–24 | 15 (22) | 18 (29) |
| 8–14 | 18 (27) | 11 (18) |
| Race: non-Hispanic white | 63 (94) | 58 (94) |
| Duration of diabetes by age-group | ||
| ≥25 years old | 25.6 ± 16.6 | 28.6 ± 12.7 |
| 15–24 years old | 8.7 ± 5.3 | 8.1 ± 4.5 |
| 8–14 years old | 4.9 ± 2.6 | 4.4 ± 3.2 |
| Insulin modality | ||
| Pump | 62 (93) | 49 (79) |
| Multiple daily injections | 5 (7) | 13 (21) |
| Total daily dose of insulin by age-group (units/kg) | ||
| ≥25 years old | 0.5 ± 0.1 | 0.5 ± 0.1 |
| 15–24 years old | 0.7 ± 0.2 | 0.8 ± 0.2 |
| 8–14 years old | 0.8 ± 0.1 | 0.8 ± 0.3 |
| A1C (%) | 6.4 ± 0.5 | 6.5 ± 0.3 |
| One or more severe hypoglycemia events* in last 6 months | 7 (10) | 7 (11) |
| Home glucose meter readings per day† | 7.3 ± 2.4 | 6.8 ± 2.4 |
| College graduate (subject or primary care giver) | 58 (87) | 55 (89) |
Data are n (%) or means ± SD.
*A severe hypoglycemia event was defined as an event that required assistance from another person to administer carbohydrate, glucagon, or other resuscitative actions.
†Data were missing for six subjects in the CGM group and four in the control group.
The visit completion rate was >99% in the CGM group and 98% in the control group (supplementary Fig. A1, available in an online appendix at http://care.diabetesjournals.org/cgi/content/full/dc09-0108/DC1), and the phone contact completion rates were 98 and 95%, respectively. The 26-week visit was completed by all CGM group subjects and by all but two subjects in the control group. No subjects in the CGM group discontinued sensor use before the 26-week visit, and no subjects in the control group self-initiated CGM use before completing the 26-week visit. Self-reported home glucose meter use was 7.3 ± 2.4 measurements per day before study entry and 7.1 ± 3.5 measurements per day at 26 weeks in the CGM group compared with 6.8 ± 2.4 and 6.4 ± 2.4 measurements per day, respectively, in the control group.
Glycemic control
Median time per day with a glucose level ≤70 mg/dl (as measured with CGM) decreased from 91 min at baseline to 54 min at 26 weeks in the CGM group (P = 0.002) and from 96 to 91 min in the control group (P = 0.43) (P = 0.16 using ranks, P = 0.04 truncating outliers, and P = 0.06 using square root transformation). As seen in Table 2, there was stronger statistical evidence of a treatment group difference favoring the CGM group for other definitions of hypoglycemia (time ≤60 mg/dl, time ≤50 mg/dl, and area under the curve for 70 mg/dl) and when the CGM data collected after the 13- and 26-week visits were pooled to provide a better indication of glycemic control over the 6 months than either time point alone (supplementary Fig. A2, available in an online appendix). A more complete indication of the treatment group difference can be seen in the cumulative distribution curves (supplementary Figs. A3 and A4, available in the online appendix). The CGM-based hypoglycemia event rate (≥20 min with glucose level <54 mg/dl [3.0 mmol/l], using the CGM data collected during the week after the 13- and 26-week visits) was 0.25 ± 0.40 events per 24 h in the CGM group and 0.47 ± 0.68 events per 24 h in the control group (P = 0.07).
Table 2.
CGM-measured outcomes by treatment group
| CGM group |
Control group |
P* |
||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 13 weeks | 26 weeks† | Baseline | 13 weeks | 26 weeks‡ | 26 weeks | 13 and 26 weeks combined | |
| n | 67 | 67 | 66 | 62 | 58 | 60 | ||
| Glucose level (min/day) | ||||||||
| ≤70 mg/dl | 91 (40–147) | 61 (24–118) | 54 (28–108) | 96 (37–225) | 89 (33–198) | 91 (27–188) | 0.16/0.04/0.06 | 0.05/0.03/0.03 |
| ≤60 mg/dl | 40 (9–73) | 21 (3–52) | 18 (5–40) | 40 (9–130) | 37 (12–100) | 35 (7–116) | 0.05/0.02/0.02 | 0.01/0.007/0.008 |
| ≤50 mg/dl | 7 (0–38) | 3 (0–18) | 4 (0–15) | 9 (0–45) | 7 (0–51) | 8 (0–55) | 0.12/0.05/0.04 | 0.05/0.03/0.01 |
| 71–180 mg/dl | 1,063 (921–1,174) | 1,092 (947–1,200) | 1,063 (948–1,185) | 972 (809–1,089) | 951 (778–1,079) | 949 (784–1,106) | 0.003/0.002/0.004 | <0.001/<0.001/0.001 |
| >180 mg/dl | 255 (151–420) | 268 (179–410) | 283 (173–423) | 331 (206–489) | 362 (221–527) | 341 (232–502) | 0.10/0.09/0.13 | 0.03/0.03/0.04 |
| >250 mg/dl | 40 (10–101) | 42 (8–77) | 48 (11–103) | 63 (27–118) | 76 (29–173) | 82 (22–149) | 0.12/0.05/0.10 | 0.005/0.003/0.006 |
| Area under the curve (70 mg/dl) | 0.64 (0.19–1.24) | 0.32 (0.09–0.80) | 0.26 (0.11–0.64) | 0.60 (0.18–1.88) | 0.48 (0.17–1.80) | 0.49 (0.13–1.73) | 0.09/0.02/0.02 | 0.03/0.01/0.008 |
| SD of values | 48 (42–58) | 49 (40–58) | 50 (41–63) | 56 (48–67) | 58 (48–69) | 60 (46–67) | 0.17/0.13/0.21 | 0.008/0.02/0.03 |
| MAGE | 93 (80–110) | 95 (82–111) | 96 (84–113) | 106 (84–130) | 103 (90–129) | 108 (86–126) | 0.77/0.78/0.87 | 0.26/0.27/0.31 |
| Absolute rate of change (mg/dl per min) | 0.60 (0.50–0.71) | 0.65 (0.50–0.73) | 0.66 (0.53–0.76) | 0.65 (0.56–0.80) | 0.63 (0.54–0.79) | 0.66 (0.54–0.87) | 0.35/0.51/0.51 | 0.39/0.63/0.57 |
Data are medians (interquartile range). CGM glucose data were obtained after completion of the 13- and 26-week visits with the CGM group using an unblinded device and the control group using a blinded device.
*P values were from three methods described in research design and methods: ANCOVA model based on van der Waerden scores, ANCOVA model with truncation of outliers, and ANCOVA model with square root transformation.
†One subject in the CGM group was missing sensor data.
‡Two subjects in the control group dropped out before the 26-week visit. MAGE, mean amplitude of glycemic excursion.
There was a significant difference between treatment groups in the mean A1C level at 26 weeks adjusted for baseline (P < 0.001) (Table 3 ). Compared with the control group, more subjects in the CGM group had an improvement in A1C of ≥0.3% (31 vs. 5%, P < 0.001), fewer had a worsening of A1C ≥0.3% (28 vs. 52%, P = 0.002), and more had an A1C level <7.0% at 26 weeks (88 vs. 63%, P < 0.001).
Table 3.
A1C at 26 weeks by treatment group
| Treatment group |
P | ||
|---|---|---|---|
| CGM | Control | ||
| n | 67 | 62 | |
| A1C* | |||
| Baseline (%) | 6.4 ± 0.5 | 6.5 ± 0.3 | |
| 26 weeks (%) | 6.4 ± 0.5 | 6.8 ± 0.5 | |
| Change from baseline to 26 weeks (%) | +0.02 ± 0.45 | +0.33 ± 0.43 | |
| Treatment group difference (%)† | −0.34 (−0.49 to −0.20) | <0.001 | |
| Decrease by ≥0.3% from baseline to 26 weeks | 21 (31) | 3 (5) | <0.001 |
| Increase by ≥0.3% from baseline to 26 weeks | 19 (28) | 31 (52) | 0.002 |
| Subjects who maintained A1C <7.0 at 26 weeks | 59 (88) | 38 (63) | <0.001 |
Data are means ± SD, difference (95% CI), or n (%).
*26-week A1C data were not available for 2 subjects in the control group.
†ANCOVA model adjusted for baseline A1C and site. The negative value denotes lower A1C in the CGM group compared with that in the control group.
In three prespecified age-groups (≥25, 15–24, and 8–14 years), results of treatment group comparisons generally were similar to those of the overall analysis for the amount of time per day ≤70 mg/dl. Results also appeared similar in subjects using multiple daily insulin injections and in those using an insulin pump, but the number of subjects using injections was too small for a meaningful comparison.
Severe hypoglycemia and other adverse events
Seven subjects (10%) in the CGM group and seven (11%) in the control group experienced at least one severe hypoglycemic event, with no significant differences comparing treatment groups (supplementary Table A1, available in an online appendix). Likewise, there were no significant differences comparing the incidence rate of severe hypoglycemic events between treatment groups. There were no serious adverse events attributable to the study interventions.
Combined outcome measures
More subjects in the CGM group than in the control group had a decrease in A1C of ≥0.3% without experiencing a severe hypoglycemic event (28 vs. 5%, P < 0.001). As seen in Fig. 1 (also supplementary Fig. A4, available in an online appendix), more subjects in the CGM group than in the control group also had a decrease in A1C of ≥0.3% without an increase of ≥43 min/day (3% of the day) in CGM-measured glucose values ≤70 mg/dl (18 vs. 2%, P = 0.007) and more had a ≥43 min/day decrease in the time per day with the glucose level ≤70 mg/dl without an increase in A1C of ≥0.3% (29 vs. 15%, P = 0.005).
Frequency of sensor use in the CGM group
In the CGM group, all subjects were using CGM at the end of the 26 weeks of the study. The amount of CGM use decreased slightly over the 26 weeks of the study (P < 0.001) but was still quite high after 26 weeks. During the first 13 weeks of the study, 78% of subjects averaged at least 6 days/week of CGM use compared with 67% during the final 4 weeks. Only 13% of subjects averaged <4 days a week during the final 4 weeks. Over the 26 weeks of the study, median CGM use was 6.8 days/week in subjects ≥25 years old, 6.2 days/week in the 15–24 year olds, and 6.4 days/week in the 8–14 year olds (P = 0.07), averaging ≥6 days/week in 79, 53, and 61%, respectively.
CONCLUSIONS
In this randomized trial, we evaluated the effect of CGM on glycemic control in adults and children with well-controlled type 1 diabetes using conventional blood glucose monitoring, as evidenced by a baseline A1C level <7.0%. For the primary outcome, the median time per day ≤70 mg/dl as measured with CGM was 37 min lower in the CGM group than in the control group after 6 months of intervention. Although the prespecified primary analysis method failed to reach statistical significance, other methods accounting for the skewness of the data had smaller P values, and significant differences between groups were seen with almost all other CGM-measured biochemical hypoglycemic and hyperglycemic outcomes as well as A1C outcomes and outcomes combining A1C and hypoglycemia.
In planning this study, the change in A1C was not selected as the primary outcome measure because we did not anticipate being able to lower A1C levels in the CGM group in view of their exquisite level of control on entry in the study (4). Indeed, we expected that there might even be small and clinically insignificant increases in A1C values in the CGM group if we were able to reduce the frequency of glucose levels ≤70 mg/dl. Instead, the CGM group was able to maintain A1C levels at baseline values with less biochemical hypoglycemia, whereas A1C levels rose over time in the control group. Moreover, all of the other A1C outcomes favored the CGM group over the control group. The increases in A1C in the control group might have been expected because of regression to the mean from the effective floor on the A1C level of ∼6.0% for most patients and from the 6.9% A1C cutoff point required for eligibility as well as the difficulties in maintaining a near-normal A1C level.
Lower A1C values in the CGM group than in the control group were not associated with an increased frequency of severe hypoglycemic events, although the trial was not formally powered to assess for a treatment group difference in the rate of severe hypoglycemia. It also is noteworthy that the rates of severe hypoglycemia in both the CGM and control groups in this study were less than half those reported by the Diabetes Control and Complications Trial, which may reflect the benefits of insulin analogs and greater frequency of use of insulin pumps in our population (7,11).
This study included a unique population of children, adolescents, and adults with type 1 diabetes as noted by their entry A1C levels being <7.0% and their attention to intensive diabetes management principles with frequent blood glucose monitoring at baseline, averaging about seven times per day. Consistent with prestudy management behaviors, adherence to CGM use was high during this study in subjects of all ages, although it was slightly higher in adults than in children and adolescents. This finding contrasts with the results of our randomized trial evaluating CGM in patients with type 1 diabetes and baseline A1C level ≥7.0%. In that trial, CGM use was substantially higher in adults than in children, and, as a presumed consequence, the benefit of CGM in lowering A1C was greater in adults than in children (3).
In summary, almost all analyses, although not the method preselected for the primary analysis, including the time per day ≤60 mg/dl, time per day between 71 and 180 mg/dl, and analysis involving A1C coupled with hypoglycemia, favored the CGM group compared with the control group. Based on the weight of evidence, CGM is beneficial for adults and children with type 1 diabetes who already have achieved excellent control with home glucose monitoring.
Supplementary Material
Acknowledgments
Study funding was provided by the Juvenile Diabetes Research Foundation (grants 22-2006-1107, 22-2006-1117, 22-2006-1112, 22-2006-1123 and 01-2006-8031).
Continuous glucose monitors and sensors were purchased at a bulk discount price from DexCom (San Diego, CA), Medtronic MiniMed (Northridge, CA), and Abbott Diabetes Care (Alameda, CA). Home glucose meters and test strips were provided to the study by LifeScan and Abbott Diabetes Care. A listing of relationships of the investigators with companies that make products relevant to the manuscript between 1 July 2006 and 30 June 2008 follows. Research funds listed below were provided to the legal entity that employs the individual and not directly to the individual. Bruce W. Bode reports having received consulting fees, honoraria, travel reimbursement, and research funds from Abbott Diabetes Care and Medtronic MiniMed, and grant support from DexCom. Bruce Buckingham reports having received a speaker honorarium and research funding from Abbott Diabetes Care, a fee for serving on a medical advisory board for LifeScan, a speaker honorarium, consulting fees, research funding from Medtronic MiniMed, and a consulting fee from Novo Nordisk. H. Peter Chase reports having received a speaker honorarium from Abbott Diabetes Care and sanofi-aventis and grant support from Symlin. Rosanna Fiallo-Scharer reports having received supplies for research from Abbott Diabetes Care and Medtronic MiniMed. Larry A. Fox reports having received supplies for research from Abbott Diabetes Care and Smiths Medical. Irl B. Hirsch reports having received consulting fees and travel reimbursement from Abbott Diabetes Care and grant support from Medtronic MiniMed. Lori Laffel reports having received consulting fees from LifeScan, consulting fees and a speaker honorarium from Abbott Diabetes Care, consulting fees and research funding from Medtronic MiniMed, and consulting and speaker fees from Roche. Nelly Mauras reports having received grant support from Medtronic MiniMed. William V. Tamborlane reports having received consulting fees from Abbott Diabetes Care and LifeScan and consulting fees, a speaker honorarium, and research funding from Medtronic MiniMed. Stuart A. Weinzimer reports having received research support, a speaker honorarium and travel reimbursement from Medtronic MiniMed, and a speaker honorarium from Animas Corp/LifeScan. Howard Wolpert reports having received consulting fees from Abbott Diabetes Care and research funding from Medtronic MiniMed. Daniel M. Wilson reports having received equipment and software from Abbott Diabetes Care and Medtronic MiniMed and research support from Medtronic MiniMed and The Elizabeth Glaser Pediatric AIDS Foundation. No other potential conflicts of interest relevant to this article were reported.
DexCom, Medtronic MiniMed, and Abbott Diabetes Care had no involvement in the design, conduct, or analysis of the trial or the preparation of this article.
The writing committee members (alphabetical) are as follows: lead authors: Roy W. Beck, MD, PhD; Irl B. Hirsch, MD; Lori Laffel, MD, MPH; and William V. Tamborlane, MD; additional authors: Bruce W. Bode, MD; Bruce Buckingham, MD; H. Peter Chase, MD; Robert Clemons, MD; Rosanna Fiallo-Scharer, MD; Larry A. Fox, MD; Lisa K. Gilliam, MD, PhD; Elbert S. Huang, MD, MPH; Craig Kollman, PhD; Aaron J. Kowalski, PhD; Jean M. Lawrence, ScD, MPH, MSSA; Joyce Lee, MD, MPH; Nelly Mauras, MD; Michael O'Grady, PhD; Katrina J. Ruedy, MSPH; Michael Tansey, MD; Eva Tsalikian, MD; Stuart A. Weinzimer, MD; Darrell M. Wilson, MD; Howard Wolpert, MD; Tim Wysocki, PhD; and Dongyuan Xing, MPH.
The Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group recognizes the efforts of the subjects and their families and thank them for their participation.
Footnotes
Clinical trial reg. no. NCT00406133, clinicaltrials.gov.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Irvine AA, Cox D, Gonder-Frederick L: Fear of hypoglycemia: relationship to physical and psychological symptoms in patients with insulin-dependent diabetes mellitus. Health Psychol 1992; 11: 135– 138 [DOI] [PubMed] [Google Scholar]
- 2.Cryer PE: Banting Lecture: Hypoglycemia: the limiting factor in the management of IDDM. Diabetes 1994; 43: 1378– 1389 [DOI] [PubMed] [Google Scholar]
- 3.Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 2008; 359: 1464– 1476 [DOI] [PubMed] [Google Scholar]
- 4.JDRF CGM Study Group JDRF randomized clinical trial to assess the efficacy of real-time continuous glucose monitoring in the management of type 1 diabetes: research design and methods. Diabetes Technol Ther 2008; 10: 310– 321 [DOI] [PubMed] [Google Scholar]
- 5.Diabetes Research in Children Network (DirecNet) Study Group Use of the DirecNet applied treatment algorithm (DATA) for diabetes management with a real-time continuous glucose monitor (the FreeStyle Navigator). Pediatr Diabetes 2008; 9: 142– 147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gibb I, Parnham A, Fonfrede M, Lecock F: Multicenter evaluation of Tosoh glycohemoglobin analyzer. Clin Chem 1999; 45: 1833– 1841 [PubMed] [Google Scholar]
- 7.Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329: 977– 986 [DOI] [PubMed] [Google Scholar]
- 8.Diabetes Research in Children Network Study Group Continuous glucose monitoring in children with type 1 diabetes. J Pediatr 2007; 151: 388– 393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.UK Hypoglycaemia Study Group Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia 2007; 50: 1140– 1147 [DOI] [PubMed] [Google Scholar]
- 10.Little RJA, Rubin DB: Statistical Analysis with Missing Data New York, John Wiley & Sons, 1987 [Google Scholar]
- 11.Diabetes Control and Complications Trial Research Group Hypoglycemia in the Diabetes Control and Complications Trial. Diabetes 1997; 46: 271– 286 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.