Abstract
OBJECTIVE
Continuous intraperitoneal insulin infusion (CIPII) with an implantable pump has been available for the past 25 years. CIPII, with its specific pharmacodynamic properties, may be a viable treatment alternative to improve glycemic control in patients with type 1 diabetes for whom other therapies have failed. There have been few studies in which CIPII was compared with subcutaneous insulin treatment for patients with type 1 diabetes with poor glycemic control.
RESEARCH DESIGN AND METHODS
In an open-label, prospective, crossover, randomized, 16-month study, the effects of CIPII and subcutaneous insulin were compared in 24 patients. The primary outcome measure was the incidence of hypoglycemia. Secondary outcome measures were A1C, and glucose profile, including time in euglycemia, as measured by continuous glucose monitoring.
RESULTS
The incidence of grade 1 hypoglycemic events was 4.0 ± 2.6 per week with subcutaneous insulin compared with 3.5 ± 2.3 per week during CIPII (P = 0.13). The absolute mean difference in A1C with CIPII compared with subcutaneous treatment was −0.76% (95% CI −1.41 to −0.11) (P = 0.03). Baseline time spent in euglycemia was 45.2 ± 12.6% and increased 10.9% (4.6–17.3) with CIPII compared with subcutaneous treatment (absolute value; P = 0.003). There were no differences in the occurrence rate for severe hypoglycemic events, daily insulin use, or BMI. No pump or catheter malfunction was observed during the study.
CONCLUSIONS
Although we did not observe a significant reduction in hypoglycemic events, improved glycemic control was achieved with the use of CIPII. We saw a 0.8% decrease in A1C and an 11% increase in the time spent in euglycemia.
Meta-analyses conclude that continuous subcutaneous insulin infusion (CSII) is somewhat better than multiple daily injections (MDIs) for obtaining glycemic control in patients with type 1 diabetes (1–4). These differences tend to be smaller when synthetic insulin analogs are used. The absorption of subcutaneous infused insulin is influenced by many factors, sometimes responsible for unexpected hypo- and hyperglycemic events (5,6). In some patients with type 1 diabetes, this form of therapy does not yield acceptable and stable long-term glycemic control (7).
The intraperitoneal administration of insulin allows blood glucose values to normalize more rapidly after a meal with more predictable insulin profiles than with subcutaneous insulin (8–10). Much of the intraperitoneal insulin is absorbed through the portal system, which more closely mimics normal physiological action, resulting in improved hepatic uptake and lower peripheral plasma insulin levels (11). Intraperitoneal insulin may lead to improved glucagon secretion and hepatic glucose production in response to hypoglycemia (12).
The effects of continuous intraperitoneal insulin infusion (CIPII) in type 1 diabetes have been investigated in few randomized controlled trials, and all were done before the era of rapidly acting insulin analogs. The objective of our study was to assess the safety and efficacy of CIPII compared with intensified subcutaneous insulin therapy in patients with inadequately controlled type 1 diabetes.
RESEARCH DESIGN AND METHODS
Subjects with type 1 diabetes with low fasting C-peptide concentrations (<0.20 nmol/l) and intermediate or poor glycemic control, defined as A1C ≥7.5% and/or ≥5 incidents of hypoglycemia (<4.0 mmol/l) per week, who were aged 18–70 years and treated with MDIs or CSII, were eligible for the study. The exclusion criteria included impaired renal function (plasma creatinine ≥150 μmol/l or glomerular filtration rate as estimated by the Cockcroft-Gault formula ≤50 ml/min) (13); cardiac problems (unstable angina or myocardial infarction within the previous 12 months or New York Heart Association class III or IV congestive heart failure); insulin allergy; mental handicaps; current or past psychiatric treatment for schizophrenia or a cognitive or bipolar disorder; severe untreated proliferative retinopathy; current use of oral corticosteroids or a condition that necessitated oral or systemic corticosteroid use more than once in the previous 12 months; substance abuse other than nicotine; a history of cancer, excluding well-differentiated thyroid carcinoma, breast carcinoma without lymph node metastases, and skin carcinoma; and plans to engage in activities that require going >25 feet below sea level.
The study has a crossover, randomized design and was conducted at a single center (Isala Clinics, Zwolle, the Netherlands). The study consisted of four phases: the qualification phase, the first treatment phase, the crossover phase, and the second treatment phase. During the 3-month qualification phase, the patients' prestudy diabetic therapy was used to attempt optimization of their glycemic control. The patients were then randomly allocated to one of two groups, which differed only in the sequence of the two therapies. Randomization was performed in blocks of four.
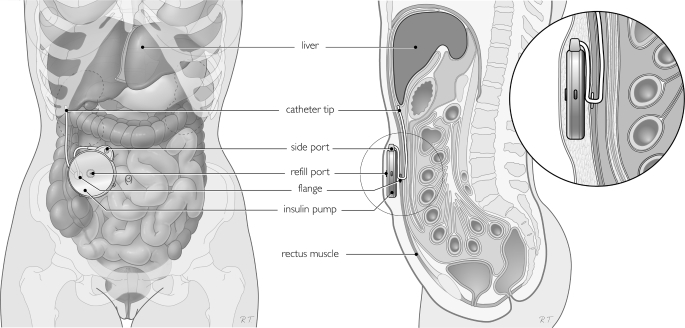
Insulin (U400 semisynthetic human insulin of porcine origin; Hoechst [recently sanofi-aventis], Frankfurt, Germany) was administered with an implanted pump (MIP 2007C; Medtronic/Minimed, Northridge, CA). The CIPII pump was implanted under general anesthesia at the start of the CIPII phase in all subjects. Figure 1 is a schematic representation of the pump and its location. For subjects who received subcutaneous insulin during the second treatment phase, the CIPII pump was filled with an inert fluid at the end of the first treatment phase. Subcutaneous insulin was delivered with either MDIs or CSII, according to what was used before the study.
Figure 1.
Schematic view of the position of the insulin pump and catheter in vivo.
Both treatment phases were 6 months in duration. A crossover phase of 4 weeks was instituted in between to minimize the carryover effects of CIPII. During the crossover phase, insulin was administered subcutaneously. After completion of the trial, subjects were given the option of continuing with their preferred mode of therapy.
Patients monitored their own glucose levels (One Touch Ultra; LifeScan, Milpitas, CA) four times every day (fasting, before meals, and bedtime) and seven times daily 2 days per week (fasting, before and after meals, and bedtime). If nocturnal hypoglycemia was suspected, subjects would perform an additional blood glucose measurement between 2:00 and 3:00 a.m. Furthermore, subjects recorded all episodes of hypoglycemia grade 1, defined as glucose <4.0 mmol/l; grade 2, defined as glucose <3.5 mmol/l; and grade 3, defined as the patient requiring third-party help and/or losing consciousness or requiring intravenous glucose or glucagon treatment. To limit the risk of data-entry error, the data from the self-monitored blood glucose meters were downloaded to a computer during every clinic visit.
Twice per month, the study subjects were in contact with a nurse specializing in diabetes, alternating telephone and clinic visits. The subjects were in contact with the medical team as necessary.
If the subject was using >40 IU s.c. insulin per day before starting the CIPII phase of the study, his or her starting dose was set at 90% of the prior subcutaneous dose. Subjects using <40 IU s.c. insulin received a starting dose of 80% of the prior subcutaneous dose. Initially, the dose was equally divided between a basal rate (50%) and a bolus before meals. During all study visits, the seven-point glucose readings were used to adjust the dose regimen if necessary to achieve preprandial glucose levels between 4.0 and 7.0 mmol/l and postprandial levels between 4.0 and 9.0 mmol/l.
The study was performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all patients, and the protocol was approved by the medical ethics committee of the Isala Clinics in Zwolle.
Measurements
Demographic and clinical parameters were recorded at baseline. These data included smoking and alcohol habits, year of diagnosis of diabetes, the presence of complications, any comorbidity, and height and weight. The A1C level was measured at baseline, at the end of the qualification phase, and at the start, at the halfway point, and at the end of both treatment phases with a Primus Ultra2 system using high-performance liquid chromatography (reference value 4.0–6.0%). In addition, 5- to 7-day 24-h blood glucose profiles were recorded with a continuous glucose monitoring (CGM) system (Medtronic/Minimed, Northridge, CA) at baseline, at the halfway point, and at the end of both treatment phases. Time spent in the hypoglycemic range was defined as the percentage of CGM recordings <4.0 mmol/l, time spent in euglycemic range was defined as the percentage of CGM recordings from 4.0 to 10.0 mmol/l, and time spent in hyperglycemic range was defined as the percentage of CGM recordings >10.0 mmol/l.
Primary and secondary outcomes
The primary outcome was the incidence of hypoglycemic episodes. The secondary outcome was glycemic control (as indicated by A1C levels). Other prespecified outcomes included time spent in hypoglycemia, euglycemia, and hyperglycemia; daily insulin usage; adverse events; and device complications. Adverse events of CIPII and device complications were subdivided according to the following categories: pump malfunction, including catheter obstruction; pump-site infection, defined as a culture-proven infection in the subcutaneous pocket of the insulin pump; prolonged pain, defined as pain at the pump site, which lasted for >6 weeks after surgery; cutaneous erosion of the skin, defined as redness with signs of imminent perforation of the overlying skin at the pump site; and postoperative hematoma, defined as a swelling at the pump site caused by (re)bleeding.
Statistical analysis
The incidence of hypoglycemia grade 1 in potentially eligible patients at our clinic of 3.7 ± 2.2 per week was used for sample size calculation. To be able to detect a 30% decrease in hypoglycemic events with a power of 0.80 and a two-sided α of 0.05, 34 patients would be needed. To compensate for nonevaluable patients, the initial goal was to enroll 40 patients.
Descriptive summaries included the mean ± SD or SEM for normally distributed variables and the median with the interquartile range for other variables. Time variables, such as times spent in the different glycemic states, are presented as absolute values. Normality was examined using Q-Q plots. Planned analyses were conducted to address the study objectives as defined, using a nominal significance level of 0.05. General linear models were used to test differences, taking the order of the two treatments into account. To calculate the mean difference with a 95% CI, the Hills-Armitage approach was used (14), which accounts for any period effect (15). If assumptions for the general linear models were not met, nonparametric tests were used, without obtaining a 95% CI. Statistical analyses were performed with SPSS software (versions 15.0 and 16.0). All reported P values are two sided.
RESULTS
Of 50 patients who were screened, 25 entered the qualification phase, after which 1 patient was excluded as having attained acceptable glycemic control. Therefore, 24 patients were randomly assigned and started the first treatment phase between June 2006 and March 2007; 12 patients were assigned to start with subcutaneous insulin and 12 patients to start with CIPII during the first phase (supplementary Fig. 1, available in an online appendix at http://care.diabetesjournals.org/cgi/content/full/dc08-2340/DC1).
Patient characteristics are listed in Table 1. The mean age was 43.6 ± 11.8 years, and the mean diabetes duration was 22.6 ± 10.6 years. The mean numbers of hypoglycemic events grades 1 and 2 were 4.0 ± 2.7 and 2.7 ± 1.9 per week, respectively. The mean A1C level was 8.6 ± 1.1%.
Table 1.
Baseline characteristics
| All | Treatment mode in first phase |
||
|---|---|---|---|
| CIPII | Subcutaneous insulin | ||
| n | 24 | 12 | 12 |
| Male sex | 11 (46) | 6 (50) | 5 (42) |
| Age (years) | 43.6 ± 11.8 | 43.3 ± 11.9 | 43.9 ± 12.2 |
| Diabetes duration (years) | 22.6 ± 10.6 | 20.6 ± 9.5 | 24.7 ± 11.6 |
| Current smoker (%) | 5 (21) | 2 (17) | 3 (25) |
| Systolic blood pressure (mmHg) | 138.5 ± 21.8 | 141.5 ± 20.2 | 135.5 ± 23.7 |
| Diastolic blood pressure (mmHg) | 80.1 ± 7.8 | 82.7 ± 6.5 | 77.6 ± 8.4 |
| Body weight (kg) | 81.5 ± 15.7 | 81.3 ± 18.0 | 81.8 ± 13.9 |
| BMI (kg/m2) | 26.4 ± 4.7 | 26.3 ± 5.3 | 26.4 ± 4.3 |
| Hypoglycemia during qualification phase (n/week)* | |||
| Grade 1 | 4.0 ± 2.7 | 4.1 ± 2.9 | 3.8 ± 2.7 |
| Grade 2 | 2.7 ± 1.9 | 2.8 ± 1.8 | 2.6 ± 2.0 |
| Time spent in glucose range (%)† | |||
| Hypoglycemia | 8.1 ± 7.7 | 7.2 ± 6.9 | 9.0 ± 8.6 |
| Euglycemia | 45.2 ± 12.6 | 44.2 ± 10.6 | 46.1 ± 14.8 |
| Hyperglycemia | 46.7 ± 18.0 | 48.6 ± 15.2 | 44.9 ± 20.9 |
| A1C (%) | 8.6 ± 1.1 | 8.5 ± 1.0 | 8.6 ± 1.2 |
| Previous mode of insulin therapy | |||
| CSII | 20 (83) | 11 (92) | 9 (75) |
| MDI | 4 (9) | 1 (8) | 3 (25) |
| Insulin dose during qualification phase (IU/day) | 46.3 (35.5–70.2) | 44.1 (35.8–80.0) | 47.0 (35.1–56.2) |
Data are n (%), means ± SD, or median (interquartile range).
*Hypoglycemia grade 1 is defined as a blood glucose value <4.0 mmol/l; hypoglycemia grade 2 is defined as a blood glucose value <3.5 mmol/l.
†Time spent in hypoglycemia is defined as the percentage of CGM recordings of <4.0 mmol/l, time spent in euglycemia is defined as the percentage of CGM recordings between 4.0 and 10.0 mmol/l, and time spent in hyperglycemia is defined as the percentage of CGM recordings >10.0 mmol/l.
One patient withdrew consent during the first treatment phase while receiving CIPII because of admission to a psychiatric hospital for a depressive disorder. The patient chose to continue CIPII treatment after withdrawal from the trial, as did all the patients who completed the study.
Hypoglycemia
The rate of hypoglycemia grade 1 with CIPII was 3.5 ± 2.3 per week compared with 4.0 ± 2.6 per week during subcutaneous insulin treatment (mean difference −0.50, 95% CI −1.16 to 0.17) (Table 2 ). The rate of hypoglycemia grade 2 was 2.3 ± 1.7 per week with CIPII compared with 2.7 ± 1.9 per week during subcutaneous insulin treatment (mean difference −0.43, −0.89 to 0.04). Two episodes of hypoglycemia grade 3 occurred during CIPII treatment and five episodes during subcutaneous treatment (all in a single patient).
Table 2.
Change per treatment mode and overall CIPII treatment effect
| Change with treatment mode |
Treatment effect adjusted for treatment order* | P | ||
|---|---|---|---|---|
| CIPII | Subcutaneous insulin | |||
| n | 23 | 23 | ||
| A1C (%) | −0.73 ± 1.25 | 0.05 ± 0.54 | −0.76 (−1.41 to −0.11) | 0.03 |
| Hypoglycemia grade 1 (n/week)†‡ | −0.64 ± 2.11 | −0.15 ± 1.33 | −0.50 (−1.16 to 0.17) | 0.13 |
| Hypoglycemia grade 2 (n/week) †‡ | −0.49 ± 1.68 | −0.07 ± 1.07 | −0.43 (−0.89 to 0.04) | 0.07 |
| Time spent in glucose range (%)†§ | ||||
| Hypoglycemia | −3.0 ± 6.2 | −1.3 ± 8.3 | −2.0 (−5.4 to 1.3) | 0.22 |
| Euglycemia | 7.8 ± 18.9 | −4.1 ± 17.2 | 10.9 (4.6 to 17.3) | 0.002 |
| Hyperglycemia | −4.7 ± 22.0 | 5.4 ± 19.5 | −8.9 (−16.7 to −1.2) | 0.03 |
| Insulin dose (IU/day)† | 0.5 (−6.8 to −5.0) | 0.3 (−6.7 to −5.8) | 0.57 | |
| Systolic blood pressure (mmHg)† | 0.4 ± 17.6 | −4.0 ± 16.3 | 3.0 (−2.6 to 8.7) | 0.28 |
| BMI (kg/m2)† | −0.4 ± 1.2 | 0.2 ± 0.9 | −0.4 (−0.9 to 0.2) | 0.18 |
Data for change are mean ± SD or median (interquartile range).
*Data for treatment effect are mean differences (95% CI) adjusted for treatment order calculated using the Hills-Armitage method (14).
†Change from baseline is reported.
‡Hypoglycemia grade 1 is defined as a blood glucose value <4.0 mmol/l; hypoglycemia grade 2 is defined as a blood glucose value <3.5 mmol/l.
§Time spent in hypoglycemia is defined as the percentage of CGM recordings of <4.0 mmol/l, time spent in euglycemia is defined as the percentage of CGM recordings between 4.0 and 10.0 mmol/l, and time spent in hyperglycemia is defined as the percentage of CGM recordings >10.0 mmol/l.
Glycemic control
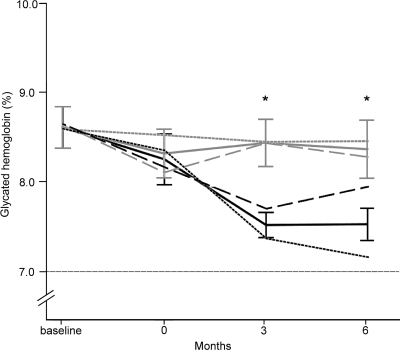
A1C decreased with CIPII from 8.6 ± 1.1 to 7.5 ± 0.7% after 3 months and remained stable at 6 months (7.5 ± 0.9%). During subcutaneous treatment there was no change in glycemic control (Fig. 2). When the effect of the treatment order was taken into account, A1C improved −0.76% (95% CI −1.41 to 0.11) with CIPII compared with subcutaneous insulin treatment (absolute values) (Table 2). The effect of treatment order was 0.37 (−0.28 to 1.02) after 6 months.
Figure 2.
Mean A1C (percentage) at baseline and during subcutaneous insulin therapy (gray lines) and intraperitoneal insulin therapy (black lines). *P < 0.05 between therapy groups (solid lines). Dashed lines indicate A1C in the two treatment order groups; smallest dashes indicate subcutaneous insulin first and CIPII second group; larger dashes indicate CIPII first and subcutaneous insulin second. The I bars represent SEM.
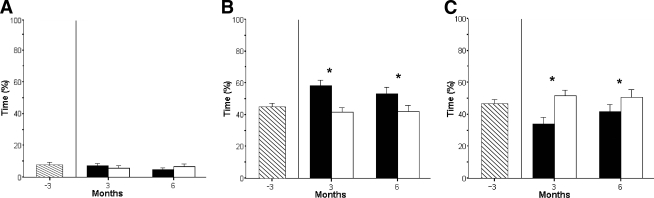
Glucose profile (CGM recording)
The time spent in hypoglycemia was not significantly different between CIPII and subcutaneous treatment (−2.0%, 95% CI −5.4 to 1.3). However, the time spent in euglycemia was 10.9% (4.6–17.3) more with CIPII than with subcutaneous treatment. Subjects spent −8.9% (−16.7 to −1.1) time in hyperglycemia with CIPII than with subcutaneous insulin treatment (Table 2, Fig. 3).
Figure 3.
Mean ± SEM time spent in different glucose ranges: time spent in the hypoglycemic range (A; <4.0 mmol/l), the euglycemic range (B; 4.0–;10.0 mmol/l), and the hyperglycemic range (C; >10.0 mmol/) at baseline (▧) and during subcutaneous insulin therapy (□), and intraperitoneal insulin therapy (■). *P < 0.05 between therapy groups.
Insulin usage and clinical parameters
There were no significant differences between CIPII and subcutaneous insulin treatment with respect to daily insulin usage and clinical parameters (Table 2).
Adverse events and device complications
There were no incidences of intraperitoneal pump or catheter malfunction. One subject developed a postoperative pump pocket hematoma requiring surgical drainage, but neither insulin delivery nor its action was affected. In three subjects, prolonged pain occurred, which was successfully treated with oral analgesics (n = 2) and relocation of the catheter (n = 1).
During the crossover phase, after receiving subcutaneous insulin, myocardial ischemia was diagnosed in one patient who was subsequently treated with coronary artery bypass grafting. After an extension of the crossover phase, this subject continued with the trial.
CONCLUSIONS
With CIPII there was no significant decrease in the number of hypoglycemic events. Nevertheless, treatment with CIPII did reduce A1C levels by 0.76% compared with subcutaneous insulin (absolute value). The improvement in A1C was accompanied by increased time spent in euglycemia and less time spent in hyperglycemia, both without any increase in either daily insulin dose or BMI. At the end of the study, all patients opted to continue with CIPII.
Haardt et al. (16) performed a randomized study comparing CIPII in a crossover manner with subcutaneous human insulin by MDIs in nine patients with type 1 diabetes (16). They reported a 1.3% difference in A1C levels after 6 months in favor of CIPII as well as a reduction in glucose variability and hypoglycemic episodes with CIPII treatment (16). The only other randomized controlled trial comparing CIPII with subcutaneous insulin in patients with type 1 diabetes (n = 21) had a parallel design and showed no difference in A1C levels (17). Since these two studies were published, insulin analogs with more physiological profiles have become widely available and when used in CSII improve glycemic control (18–23). No randomized trial comparing regimens based on insulin analogs with CIPII was published previously. A 45-day retrospective open-label trial in 14 patients with type 1 diabetes compared CIPII with CSII using insulin Lispro and reported a 0.5% lower average A1C with CIPII (24).
One major limitation of this study is that because of budget constraints, we were only able to include 24 patients in our study, instead of the projected 40, which severely reduced the statistical power. Furthermore, four patients used MDIs instead of CSII in the control phase, which may have affected the results. Another possible source of bias that we tried to minimize by using a crossover design is the influence of subject preferences and expectations.
Taking recent price increases into account, it is not likely that the CIPII option will be cost-effective in the near future, although a formal cost-benefit analysis has not been done. However, based on our results, we recommend consideration of CIPII as a treatment option for those patients with type 1 diabetes who fail to achieve satisfactory glycemic control with other intensive insulin treatment regimens.
Supplementary Material
Acknowledgments
This study was supported by Medtronic. No other potential conflicts of interest relevant to this article were reported.
We thank Harma Israël and Anita van Linde for their help with conducting the study.
Footnotes
Clinical trial reg. no. NCT00286962, clinicaltrials.gov.
The sponsor had no role in the study design, data collection, analysis, interpretation, or writing of the report.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N: Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes. Health Technol Assess 2004; 43: iii1– iii171 [DOI] [PubMed] [Google Scholar]
- 2. Pickup J, Mattock M, Kerry S: Glycaemic control with continuous subcutaneous insulin infusion compared with intensive insulin injections in patients with type 1 diabetes: meta-analysis of randomized controlled trials. BMJ 2002; 324: 705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Weissberg-Benchell J, Antisdel-Lomaglio J, Seshadri R: Insulin pump therapy: a meta-analysis. Diabetes Care 2003; 26: 1079– 1087 [DOI] [PubMed] [Google Scholar]
- 4. Retnakaran R, Hochman J, DeVries JH, Hanaire-Broutin H, Heine RJ, Melki V, Zinman B: Continuous subcutaneous insulin infusion versus multiple daily injections: the impact of baseline A1c. Diabetes Care 2004; 27: 2590– 2596 [DOI] [PubMed] [Google Scholar]
- 5. Holleman F, Hoekstra JB: Insulin lispro [published correction appears in N Engl J Med 2003;349:1487]. N Engl J Med 1997; 337: 176– 183 [DOI] [PubMed] [Google Scholar]
- 6. Guerci B, Sauvanet JP: Subcutaneous insulin: pharmacokinetic variability and glycemic variability. Diabetes Metab 2005; 31: 4S7– 4S24 [DOI] [PubMed] [Google Scholar]
- 7. Shalitin S, Phillip M: Hypoglycemia in type 1 diabetes: a still unresolved problem in the era of insulin analogs and pump therapy Diabetes Care 2008; 31: S121– S124 [DOI] [PubMed] [Google Scholar]
- 8. Wredling R, Liu D, Lins PE, Adamson U: Variation of insulin absorption during subcutaneous and peritoneal infusion in insulin dependent diabetic patients with unsatisfactory long-term glycaemic response to continuous subcutaneous insulin infusion. Diabetes Metab 1991; 17: 456– 459 [PubMed] [Google Scholar]
- 9. Micossi P, Cristallo M, Librenti MC, Petrella G, Galimberti G, Melandri M, Monti L, Spotti D, Scavini M, Di Carlo V, Pozza G: Free-insulin profiles after intraperitoneal intramuscular, subcutaneous insulin administration. Diabetes Care 1986; 9: 575– 578 [DOI] [PubMed] [Google Scholar]
- 10. Nathan DM, Dunn FL, Bruch J, McKitrick C, Larkin M, Haggan C, Lavin-Tompkins J, Norman D, Rogers D, Simon D: Postprandial insulin profiles with implantable pump therapy may explain decreased frequency of severe hypoglycaemia, compared with intensive subcutaneous regimens, in insulin-dependent diabetes mellitus patients. Am J Med 1996; 100: 412– 417 [DOI] [PubMed] [Google Scholar]
- 11. Giacca A, Caumo A, Galimberti G, Petrella G, Librenti MC, Scavini M, Pozza G, Micossi P: Peritoneal and subcutaneous absorption of insulin in type I diabetic subjects. J Clin Endocrinol Metab 1993; 77: 738– 742 [DOI] [PubMed] [Google Scholar]
- 12. Wan CK, Giacca A, Matsuhisa M, El-Bahrani B, Lam L, Rodgers C, Shi ZQ: Increased responses of glucagon and glucose production to hypoglycemia with intraperitoneal versus subcutaneous insulin treatment. Metabolism 2000; 49: 984– 989 [DOI] [PubMed] [Google Scholar]
- 13. Cockcroft DW, Gault MH: Prediction of creatinine clearance from serum creatinine. Nephron 1976; 16: 31– 41 [DOI] [PubMed] [Google Scholar]
- 14. Hills M, Armitage P: The two period cross-over clinical trial. Br J Clin Pharmacol 1979; 8: 7– 20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Díaz-Uriarte R: Incorrect analysis of crossover trials in animal behaviour research. Anim Behav 2002; 63: 815– 822 [Google Scholar]
- 16. Haardt MJ, Selam JL, Slama G, Bethoux JP, Dorange C, Mace B, Ramaniche ML, Bruzzo F: A cost-benefit comparison of intensive diabetes management with implantable pumps versus multiple subcutaneous injections in patients with type I diabetes. Diabetes Care 1994; 17: 847– 851 [DOI] [PubMed] [Google Scholar]
- 17. Selam JL, Raccah D, Jean-Didier N, Lozano JL, Waxman K, Charles MA: Randomised comparison of metabolic control achieved by intraperitoneal insulin infusion with implantable pumps versus intensive subcutaneous insulin therapy in type I diabetic patients. Diabetes Care 1992; 15: 53– 58 [DOI] [PubMed] [Google Scholar]
- 18. Brange J, Owens DR, Kang S, Vølund A: Monomeric insulins and their experimental and clinical implications. Diabetes Care 1990; 13: 923– 954 [DOI] [PubMed] [Google Scholar]
- 19. Melki V, Renard E, Lassmann-Vague V, Boivin S, Guerci B, Hanaire-Broutin H, Bringer J, Belicar P, Jeandidier N, Meyer L, Blin P, Augendre-Ferrante B, Tauber JP: Improvement of HbA1c and blood glucose stability in IDDM patients treated with lispro insulin analog in external pumps. Diabetes Care 1998; 21: 977– 982 [DOI] [PubMed] [Google Scholar]
- 20. Renner R, Pfützner A, Trautmann M, Harzer O, Sauter K, Landgraf R: Use of insulin lispro in continuous subcutaneous insulin infusion treatment: results of a multicenter trial German Humalog-CSII Study Group. Diabetes Care 1999; 22: 784– 788 [DOI] [PubMed] [Google Scholar]
- 21. Colquitt J, Royle P, Waugh N: Are analogue insulins better than soluble in continuous subcutaneous insulin infusion? Results of a meta-analysis. Diabet Med 2003; 20: 863– 866 [DOI] [PubMed] [Google Scholar]
- 22. Pickup J, Keen H: Continuous subcutaneous insulin infusion at 25 years: evidence base for the expanding use of insulin pump therapy in type 1 diabetes. Diabetes Care 2002; 25: 593– 598 [DOI] [PubMed] [Google Scholar]
- 23. Siebenhofer A, Plank J, Berghold A, Horvath K, Sawicki PT, Beck P, Pieber TR: Meta-analysis of short-acting insulin analogues in adult patients with type 1 diabetes: continuous subcutaneous insulin infusion versus injection therapy. Diabetologia 2004; 47: 1895– 1905 [DOI] [PubMed] [Google Scholar]
- 24. Catargi B, Meyer L, Melki V, Renard E, Jeandidier N. the EVADIAC Study Group. Comparison of blood glucose stability and HbA1C between implantable insulin pumps using U400 HOE 21PH insulin and external pumps using lispro in type 1 diabetic patients: a pilot study. Diabetes Metab 28: 133– 137, 2002 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.