Abstract
Therapeutic cancer vaccines rely on the immune system to eliminate tumor cells. In contrast to chemotherapy or passive (adoptive) immunotherapies with antibodies or ex vivo-expanded T cells, therapeutic vaccines do not have a direct anti-tumor activity, but aim to reset patients’ immune systems to achieve this goal. Recent identification of effective ways of enhancing immunogenicity of tumor-associated antigens, including the use of dendritic cells and other potent vectors of cancer vaccines, provide effective tools to induce high numbers of circulating tumor-specific T cells. However, despite indications that some of the new cancer vaccines may be able to delay tumor recurrence or prolong the survival of cancer patients, their ability to induce cancer regression remains low. Recent reports help to identify and prospectively remove the remaining obstacles towards effective therapeutic vaccination of cancer patients. They indicate that the successful induction of tumor-specific T cells by cancer vaccines is not necessarily associated with the induction of functional cytotoxic T lymphocytes, and that current cancer vaccines may promote undesirable expansion of Treg cells. Furthermore, recent studies also identify the tools to counteract such phenomena, in order to assure the desirable induction of Th1-cytotoxic T lymphocytes, NK-mediated type-1 immunity and appropriate homing of effector cells to tumors.
Keywords: breast cancer, cancer, clinical trials, colorectal cancer, CTL, dendritic cells, immunotherapy, melanoma, NK cells, ovarian cancer, prostate cancer, signal 3, signal 4, Th1, vaccines
Immune system as a means to fight cancer
Despite an overall progress in cancer therapy, substantial groups of cancer patients lack effective treatment options, and even larger groups lack curative therapies. Combined use of surgery, radio- and chemo-therapy is often highly active in eliminating the major tumor mass, but is less effective in eliminating residual cancer cells and in preventing disease recurrence. This particular deficit of the current treatments provides the rationale for the utilization of the immune system, specialized in eliminating such ‘rare events’ in our bodies as invading bacteria or the individual host’s cells hijacked by viruses, in order to identify and destroy cancer cells.
The goal of therapeutic cancer vaccines (or active immunotherapy) is to instruct the patient’s own immune system to kill cancer cells. Compared with chemotherapy, the theoretical advantages of such an approach are its higher ability to selectively eliminate the transformed cells, resulting in low toxicity, and the ability to recognize and attack multiple target molecules, even the newly arising antigens on rapidly mutating tumor cells (due to the phenomenon of epitope spreading).
The use of the immune system to fight tumors was proposed in the late 19th century by William Coley at the Memorial Sloan–Kettering Cancer Center in New York (NY, USA), who noted sporadic cases of spontaneous regression of advanced cancer attributable to infections (reviewed in [1]). Throughout the following century, repeated attempts to utilize the immune system to fight cancer in a systematic approach were met with limited success, prompting a century-long debate on the relevance of the immune system to cancer surveillance and therapy [2,3].
At the beginning of the 21st century, it has become evident that the immune system can be utilized to fight cancer, but it is also clear that the spontaneously arising responses against cancer are relatively ineffective [3], and that the effectiveness of currently available immunotherapies for cancer still trails the effectiveness of vaccination against infective agents [4–9].
The reasons for the above gap include the use of cancer vaccines in therapeutic settings (rather than as a preventive mode, relevant to antimicrobial vaccines), relative antigenic similarity of tumor cells to healthy cells from the same tissues (with only a low percentage of cell-associated antigenic epitopes being overexpressed on tumor cells and an even smaller percentage being unique to the tumor), and paucity of tissue damage and distress signals at early phases of tumor growth. Additionally, the high adaptability of tumors, such as their ability to discard highly immunogenic antigens and key molecules needed for antigen recognition and to produce multiple immunosuppressive factors [10,11], allows evasion from the immune response.
While the high number of active mechanisms used by tumors to evade the immune system and to induce immune dysfunction predict the difficulties in the development of effective cancer immunotherapies, it also points to the active role of the immune system in selecting the resistant tumor cell variants, and thus to the ability of immune cells to eliminate tumor cells. In accordance with this notion, even if the immune system often fails to prevent the initial tumor growth, different forms of immunotherapy have been shown to reduce tumor incidence, promote tumor regression and prolong the survival of experimental animals and patients with cancer, suggesting that a proper method of activating the immune system can be used to eliminate or control the residual disease and possibly to treat, or even cure, patients with macroscopic lesions.
Vaccines versus adoptive immunotherapies of cancer
Available immunotherapies of cancer can be roughly divided into adoptive immunotherapies that rely on administration of ex vivo prepared immune cells or antibodies, and active immunotherapies or vaccines (Table 1).
Table 1.
Vaccines versus ‘passive’ immunotherapies with antibodies and adoptively transferred T cells.
| Therapy | Vaccines | Antibodies | Adoptive T-cell transfer |
|---|---|---|---|
| Direct cytotoxic effects | No | Yes | Yes |
| T cell effectors able of tumor entry | ? | ? | Yes |
| ADCC | ? | Yes | No |
| Induction of immune surveillance | Yes | ? | ? |
| Induction of clinical responses | ? (Low) | Yes | Yes |
| Survival benefit | Likely (limited data) | Yes | ? |
| Toxicity | No | Yes | Yes |
| Targeting patient/tumor-unique Ags | Yes | No | Yes |
?: Inconclusive data.
ADCC: Antibody-dependent cell-mediated cytotoxicity; Ags: Antigens.
In contrast to passive (adoptive) immunotherapies that aim to directly destroy tumor cells using preformed immune effector molecules or cells, cancer vaccines aim to induce endogenous immune surveillance by exposing the patients’ immune system to tumor-relevant antigens delivered in an immunogenic form in the context of adjuvants, such as pathogen-derived pathogen-associated molecular patterns, proinflammatory cytokines or activated antigen-presenting cells (APCs). As expected, since the immune system specializes in eliminating ‘rare events’ while sparing the overall tissue, current cancer vaccines trail adoptive immunotherapies in inducing regression of bulky tumors [8], but show promise in inducing disease stabilization and prolonging patients’ survival [9,12–15].
While adoptive immunotherapies, particularly those involving preformed antibodies (that can be mass-produced and easily distributed in a lyophilized form), are highly feasible, their limitations include the need for their continued/repetitive administration in order to sustain the therapeutic effects and their relatively narrow specificity limited to individual tumor-related antigens. For these reasons, they are both relatively expensive and can be applied only to the patients with tumors that display a particular antigenic composition, limiting the scope of their applicability.
The intrinsic advantage of vaccines is the feasibility of targeting multiple antigenic targets, or even the whole antigenic repertoire of tumor cells, by including in the vaccines multiple tumor-related epitopes or whole tumor cells as sources of cancer-related antigens. In addition, recent observations of the induction of responses to tumor-relevant epitopes that are not included in the original vaccine, particularly relevant to dendritic cell (DC)-based vaccines [16,17], further support the ability of vaccines to target a wide population of tumor cells, despite the heterogeneity and adaptability of tumor cells within the individual cancer patient. In addition to the longevity of the vaccination-induced T-cell responses, the above findings indicate that vaccines may offer an advantage to adoptive immunotherapies with regard to inducing responses to the most relevant antigens in the individual patients, and limit the ability of tumors to escape immune surveillance by adapting their antigenic profiles.
Of importance for the feasibility of active immunotherapies for use in patients with reduced performance status, and older patients who are particularly prevalent in oncology clinics, is the fact that previous cancer vaccines have all been very well tolerated. This is in contrast to adoptive immunotherapies with tumor-infiltrating lymphocytes, which are associated with a high incidence of adverse side effects (mostly organ-specific autoimmune phenomena).
‘Off-the-shelf’ vaccines versus customized cell-based active immunotherapies
Two general approaches have been applied to the development of new immunotherapeutic interventions. The ‘off-the-shelf’ approach utilizes standardized vaccines, which are antigenic preparations capable of activating endogenous APCs, such as DCs, then being presented by DCs to tumor-specific T cells, and ultimately inducing T cell activation. The advantages of standardized vaccines (usually recombinant proteins, recombinant viruses or synthetic peptides containing one or several tumor-relevant epitopes) are that they can be mass-produced, and are easily stored and distributed. However, their limitation is the predetermined, usually limited, antigenic repertoire (making them applicable to only limited subsets of patients whose tumors express the particular tumor-related antigens), and in the case of the peptide-based vaccines, their applicability is often limited to an even narrower subset of patients who express a particular HLA type (usually HLA-A2 in the USA and Europe). Their applicability to the treatment of cancer is still limited by the current lack of universally over-expressed tumor rejection antigen(s) on many types of cancer. In addition, the limitation of both protein-based and peptide-based vaccines is their poor ability to include balanced activation of the CD4+ and CD8+ subsets of T lymphocytes, which is thought to be essential for the effectiveness of anti-tumor immunity [6,18–22]. The existing peptide-based vaccines preferentially induce (HLA-A2-restricted) CD8+ T-cell responses (able to directly kill tumor cells, but with limited lifespan in the absence of CD4+ T-cell help), while protein-based vaccines effectively induce MHC II-restricted CD4+ T-cell responses, but are less effective in inducing CD8+ cytotoxic T lymphocytes (CTLs) [6,18–22]. Furthermore, the ability of such vaccines to activate patients’ T cells depends on the characteristics and level of activation of local DCs, known to be negatively affected by the presence of tumor [23]. Despite these intrinsic limitations, recent studies in breast cancer demonstrated the ability of a standardized Her2/Neu peptide-based vaccine to delay the recurrence of completely resected breast cancer [15].
Many of the above limitations can be avoided by applying customized, patient-specific vaccines, involving a patient’s own tumor cells, which display the unique antigenic repertoire that is relevant to each particular patient, both with regard to the patient’s HLA type and the unique profile of the tumor-associated antigens expressed on the patient’s tumor cells. In addition, cell-based approaches that involve patients’ ex vivo-generated APCs (such as DC-based vaccines) also avoid the reliance on endogenous APCs, which are frequently dysfunctional in patients with advanced cancer [23].
Impaired functions of endogenous dendritic cells in cancer
Endogenous DCs in cancer-bearing patients are a target of tumor-associated suppressive factors, resulting in their aberrant functions and impaired development of effector functions in tumor-specific lymphocytes [24,25]. The mediators of such tumor-induced DC dysfunction include IL-10, TGF-β, VEGF, IL-6 and prostanoids, such as PGE2–6 [26–29], leading to impaired ability of DCs developing in their presence to undergo maturation, to elevate the expression of costimulatory molecules needed for T-cell activation and to produce cytokines needed to support survival and effector functions in tumor-specific T cells [30–33].
The dysfunction of endogenous DCs has been noted in patients with ovarian, breast, melanoma, renal cell and prostate carcinoma [34–37]. Similar findings have been reported in the blood of patients with head and neck, lung and breast cancer [31,38]. Tumor-derived factors were shown to modulate STAT-3 activity and disturb key intracellular signaling pathways required for DC activation and final maturation, including NF-κB activation [39,40].
The absence of adequate costimulation and cytokine secretion by DCs leads to anergy of naïve, memory and effector T cells, and their conversion into regulatory T(reg) cells, favoring tumor evasion. In addition to inducing aberrant functions of tumor-infiltrating DCs, tumor-derived factors also induce DC apoptosis [41,42], which can also promote T-cell unresponsiveness [43]. Such DC apoptosis-inducing factors include ceramides, gangliosides, nitric oxide and IL-10, all of which are capable of inducing DNA fragmentation in DCs and suppressing anti-tumor immunity [44–46].
Ex vivo -generated dendritic cells in cancer treatment: dendritic cell-based cancer vaccines
The deficit of endogenous DCs frequently observed in cancer patients, manifested by an overall reduction in stimulatory capacity or selective impairment in the ability to induce the desirable type-1 immune responses [24,25], suggested the use of ex vivo-generated DCs as carriers of cancer vaccines [47]. DCs, first identified by Ralph Steinman at the Rockefeller University in New York (NY, USA) in the 1970s [48–51], are APCs uniquely specialized in inducing primary immune responses, supporting the survival and effector functions in previously primed T cells, and mediating overall communication within the immune system [52,53].
Since, in contrast to the DCs that develop in the context of tumor-related suppressive factors, fully mature DCs acquire at least partial resistance to such factors [54–56], the attempts to restore normal immune functions in cancer-bearing patients led to the use of fully functional ex vivo-generated DCs from cancer patients as a therapeutic tool.
Following the initial success of the DC-based immunotherapy trials in follicular lymphoma and melanoma in the mid-1990s [57,58], DCs have been successfully used to treat patients with melanoma, lymphoma and renal cell carcinoma [4,6,7,22,59]. However, overall clinical response rates do not exceed the usual 10–15% observed in various types of immunotherapies [22,59–63], arguing for the need to improve the design of DC-based vaccines – notably the selection of the most appropriate types of DCs.
Fine-tuning of dendritic cell-based vaccines: polarized dendritic cells as carriers of signal 1, 2 & 3
DCs provide T cells with antigenic ‘signal 1’ and costimulatory ‘signal 2’ [64–66], needed for the activation and expansion of pathogen-specific T cells. DCs also provide an additional polarizing ‘signal 3’, driving the development of immune responses towards type-1 or type-2 immunity [53], associated with differential involvement of particular effector mechanisms and different abilities to induce cancer rejection [53,64–73]. Potentially, an additional signal (tentatively-termed ‘signal 4’) regulating organ-specific trafficking of immune cells [74–80] is also delivered by the DCs. In addition to their role as the initiators of Ag-specific responses of CD4+ and CD8+ T cells, DCs have also been shown to support the tumoricidal activity of natural killer (NK) cells [81].
Several features of DCs, including their maturation status, migratory potential and cytokine production, were shown to be important for the ability of DC-based cancer vaccines to induce high numbers of Th1-type CD4+ T cells and CD8+ CTLs. Effective induction of anti-tumor CTL responses requires mature DCs that express high levels of costimulatory molecules and can migrate in response to CCL19 or CCL21 – the lymph-node-produced CCR7 ligands [82–84]. In addition, high IL-12p70 secretion has been shown to dramatically enhance the ability of DCs to induce tumor-specific Th1 cells and CTLs, and to promote tumor rejection in therapeutic mouse models [85–87].
Unfortunately, obtaining DCs that possess the three desired features (high immuno-stimulatory function, high migratory activity and high capacity to produce IL-12p70) has been difficult. ‘First-generation’ DC-based vaccines utilized relatively immature or only partially mature DCs, which were immunogenic [57,58], but suboptimal with regard to their lymph-node homing ability and T-cell-stimulating potential [82,88]. ‘Second-generation’ DC-based vaccines, matured in the presence of an IL-1β/TNFα/IL-6/PGE2-containing cytokine cocktail [89], showed a desirable fully mature status, but a reduced ability to produce bioactive IL-12p70, also referred to as DC exhaustion [54,90,91]. Thus, although the ‘second-generation’ DC-based vaccines are clearly superior to immature DCs with respect to their immunostimulatory capacity [82,88] and migratory responses to lymph node-associated chemokines [84,92,93], the desirable combination of all the above three features has not been attained.
In accordance with the possibility of boosting the clinical efficacy of cancer vaccines, we and other groups have demonstrated the feasibility of inducing ‘nonexhausted’ mature DCs, by exposing immature DCs to type-1 and type-2 interferons and Toll-like receptor ligands, or alternatively, to properly-activated NK cells or memory-type CD8+ T cells [55, 91, 94–99]. The resulting ‘type-1 polarized’ DCs (DC1s) show dramatically enhanced capacity to induce long-lived tumor-specific T cells with strongly pronounced anti-tumor effector functions in human in vitro and mouse in vivo models, and high activity in enhancing tumoricidal functions in resting NK cells. Our original observations [55] and the data from the laboratory of Brian Czerniecki in Philadelphia (PA, USA) [97] and Marieke van Ham in Amsterdam (The Netherlands) [100] demonstrated that the combination of IFN-γ with LPS (including its clinical-grade form, MPLA) or DC maturation-inducing cytokines TNFα and IL-1β overcomes the maturation-associated DC ‘exhaustion’, yielding stable DC1s that produce highly elevated levels of IL-12p70 upon interaction with CD40L-expressing CD4+ Th cells and induce much stronger Th1-type and CTL responses [55, 97]. DC1s with similar properties can be effectively induced by ‘two-signal-activated’ autologous NK cells or memory-type CD8+ T cells ([95, 96, 99] and our unpublished data).
Further addition of IFNα and poly-inosinic:polycytidylic acid (poly-I:C) to the DC-maturation cocktail enhances the ability of maturing DCs to acquire CCR7 expression [91], and instruct the DCs to preferentially interact with naïve, memory and effector T cells, rather than with the undesirable T Treg cells [101]. These latest data suggest that polarized DCs may be able to avoid the undesirable expansion of Treg cells observed with the previously used vaccines [102–106]. In accordance with the ability of polarized DCs to induce qualitatively improved immune responses, ‘α-type-1-polarized DCs’ (αDC1s) induce up to 40-fold higher numbers of long-lived melanoma-specific CTLs in a single round of in vitro sensitization [91], when directly compared with standard (s)DCs matured by IL-1β/TNFα/IL-6/PGE2 [89], which are frequently used in ‘second-generation’ DC-based vaccines.
So far, our data from melanoma [91], CLL [107], follicular lymphoma, cervical, endometrial, ovarian and prostate cancer uniformly demonstrate the feasibility of generating polarized DC1s from patients with multiple forms of cancer and their loading with peptide antigens or autologous tumor cells [107]. These DCs showed a fully mature phenotype (as CD83, CD86 and CD80 expression), and also expressed moderate levels of CCR7 on their surface. Regardless of the source of antigen loaded (peptide antigens or apoptotic tumor cells), αDC1s were also superior to sDCs in in vitro expansion of tumor antigen-specific functional CTLs, and were also able to cross-present tumor epitopes, as tested by IFNγ enzyme-linked immunosorbent spot (ELISPOT) assays.
Our recently published data describe the first murine model of polarized DC1s [108], which provides a tool to further our understanding of the immune responses generated by DC1 vaccines in vivo. Murine bone marrow-derived DCs that are matured in IL-4/IFNγ/lipopoly-saccharide/granulocyte macrophage-colony stimulating factor (GM-CSF) have a mature phenotype and retain the capacity for high IL-12 production in vitro. Unlike many mouse models that use nonphysiologically high numbers of DCs for vaccinations, our data demonstrate that DC1s are superior inducers of antitumor immunity, even when used at extremely low numbers of DCs [108].
In accordance with the early indications of clinical activity of cancer vaccines incorporating polarized DCs in the clinical trials currently implemented at the University of Pittsburgh (PA, USA), these data suggest that the effectiveness of cancer vaccines may be increased by the use of DCs that selectively activate the desirable type of immune responses. Our additional efforts aim at the development of strategies to boost the ability of the vaccination-induced effector cells to enter into tumors.
In vivo polarization of endogenous dendritic cells in cancer vaccination
While the use of ex vivo generated DCs provides a unique opportunity to avoid tumor-induced DC dysfunction and allows for very precise manipulation of DC properties, the associated requirement for the ex vivo manipulation of patients’ cells and the resulting need for specialized cell culture facilities prompted attempts to develop cell-free vaccines capable of targeting endogenous DCs, and their subsets, within the bodies of cancer patients. The reported advantage of the combined use of tumor-specific antigen with therapies activating NKT cells, for example using α-galactosylceramide [47, 52, 109–113] in enhancing the IL-12p70-production by endogenous DCs [112], raises the possibility that vaccines engineered to deliver the antigens selectively to DCs can be coupled with strategies to induce DC polarization in vivo.
We have previously shown that two types of immune cells can promote type-1 polarization of DCs. Resting NK cells that are activated in the presence of IL-18 and IFNα or IL-2 can induce DC maturation and enhance IL-12p70 production, in a TNFα-mediated manner [96, 114]. Memory CD8+ T cells interacting with DCs in an antigen-specific manner can also secrete TNFα to promote the polarization and maturation of the DCs [95, 115, 116]. These observations suggest that by combining the delivery of tumor-relevant antigen to endogenous DCs with the strategies aimed to promote the interaction of those DCs with either NK cells or memory CD8+ T cells (rather than effector cells prevailing among tumor-specific cells in cancer patients), endogenous DCs that take up the vaccine-associated antigens in vivo could be type-1 polarized without any ex vivo manipulation. In support of this possibility, our recent observations show that cancer vaccines, including additional elements to promote the interaction of DCs with TNFα and IFNγ-producing tumor-unrelated viral- or xeno-antigen-specific memory type CD8+ T cells, enhances the immunogenic and therapeutic effects of vaccination against different tumors, in an IL-12-dependent mechanism [117]. While these experiments in a murine model did use ex vivo manipulated DCs, it is possible to target antigens to DCs in vivo. One example of such an approach is the targeting of endogenous DCs using tumor-relevant antigens physically linked to DC-specific antibodies, an approach that showed promise in mouse experiments [118, 119].
In remains to be tested if the strategies aimed at in vitro polarization of DCs may show therapeutic synergism with the previously proposed strategies to enhance the DC numbers, such as Flt3-ligand treatment, known to increase the DC numbers in mouse [120], favoring antigen cross-presentation [121]. Interestingly for potential clinical translation of such strategies, Flt3-ligand was shown to support the induction of immunogenic DCs from human peripheral blood [122, 123].
DCs regulate the migratory pattern of T cells: modulation of the ability of DCs to deliver ‘signal 4’ as a tool to boost the effectiveness of cancer vaccines?
While the differences in homing properties of different T-cell subsets have been known for over 15 years [124–130], a series of more recent studies demonstrated the key role of DCs in regulating T-cell homing properties [74–76, 78, 131]. Depending upon the tissue origin, DCs use such metabolites as vitamin D or vitamin A to induce CCR10 [132] or CCR9 [133] on T cells to preferentially home to skin or the intestine, respectively. DCs isolated from Peyers’ patches or treated with retinoids show the ability to induce gut-homing properties in naïve T cells [74–76, 78]. Similarly, migratory APCs have recently been shown to imprint the ability of T cells to home to the CNS [80].
In further support of the notion that the migratory capacity of human melanoma-specific T cells can be affected by DC-related factors (delivery of ‘signal 4’), it was shown that enhanced expression of functional CLA (cutaneous homing receptor; ligand for skin endothelium-expressed ELAM) and enhanced migration of effector CTLs to metastatic melanoma lesions in the skin can be induced by the treatment of patients with systemic IL-12 [134]. Berger and colleagues have recently reported that vaccination with monocyte-derived DCs can induce melanoma-specific T cells that home to both the skin and to visceral metastases [135].
The possibility that improved tumor homing may translate into better outcomes of active immunotherapies is supported by the observations that the level of T-cell infiltration is a strong independent prognostic marker of the survival of cancer patients with melanoma [136] and colorectal cancer [137–139]. A recent report suggested that the numbers of melanoma-infiltrating T cells are a better prognostic factor of response to tumor vaccination than the mere numbers of melanoma-specific T cells in circulation [140], suggesting that the ability of vaccines to induce melanoma-relevant homing properties is key to successful immunotherapy. Another recent report demonstrated a dramatic survival advantage of the CTL-associated CXCR3 expression for patients with advanced melanoma [141]. Moreover, high expression of CXCR3 on circulating CD8+ T cells was shown to be a strong positive prognostic factor predicting long-term survival of patients with stage III melanoma.
Therefore, the ability of DC vaccines to induce CXCR3-expressing CTLs is likely to be an important factor contributing to their ability to act as effective vaccines against melanoma and other tumors. Furthermore, it remains to be tested if the efficacy of cancer immunotherapy can be enhanced by modulating the pattern of chemokines at tumor sites to facilitate the tumor entry of the effector-type T cells induced by vaccines.
Dealing with regulatory T(reg) cells
In addition to the ability of DC-based vaccines to induce a desirable set of homing receptors on tumor-specific T cells, another aspect that requires a thorough evaluation is the possibility of manipulating tumor-infiltrating DC vaccines to selectively express chemokines that attract (and thus preferentially activate) the desirable types of immune cells, such as Th1, NK and CTL, while avoiding the interaction with suppressor/regulatory cells. Recently, we observed that the conditions of DC maturation imprint the ability of mature DCs to secrete different classes of chemokines and thus, selectively attract and interact with functionally distinct specific types of T cells [101]. DCs matured in the presence of PGE2 preferentially secrete CCL22/SDF1 and attract Tregs, possibly explaining the previously reported preferential expansion of undesirable Treg cells in cancer patients vaccinated with PGE2-matured ‘standard’ DCs [105]. In contrast, the inclusion of interferons in the DC maturation cocktails, particularly when combined with elimination of PGE2, suppressed CCL22 production and promoted the secretion of effector T-cell-attracting chemokines, such as CCL5 and CXCL10 (and other CXCR3 ligands). This ability to produce specific chemokines seems to be imprinted during their maturation, as the chemokine expression remains stable even after removal of original maturation factors. Therefore, it is possible that the use of DCs matured in different environments, such as PGE2-matured ‘standard’ DCs and type-1-polarized αDC1s, matured in the presence of IFNs and other NK cell-replacing factors, mimicking the conditions of acute infection, will preferentially amplify functionally different types of immunity.
Since tumor microenvironments are rich in PGE2 [26–29] and CCL22 [142] and have been shown to effectively recruit Tregs [142], it remains to be tested whether treatment may reduce CCL22 levels and Treg infiltration. The potential advantage of such tumor-specific chemokine modulation is supported by studies that show that DCs present in regressing tumors have particularly high expression of CXCL9 and show elevated ability to attract CXCR3+ T cells to tumor tissue [143, 144].
Future perspective: towards effective therapeutic cancer vaccines
Despite their relatively limited size, recent clinical studies have suggested a potential advantage of current cancer vaccines in reducing the rate of tumor recurrence and prolonging survival of patients with advanced cancer [12, 15]. However, their activity in inducing tumor regression is still limited.
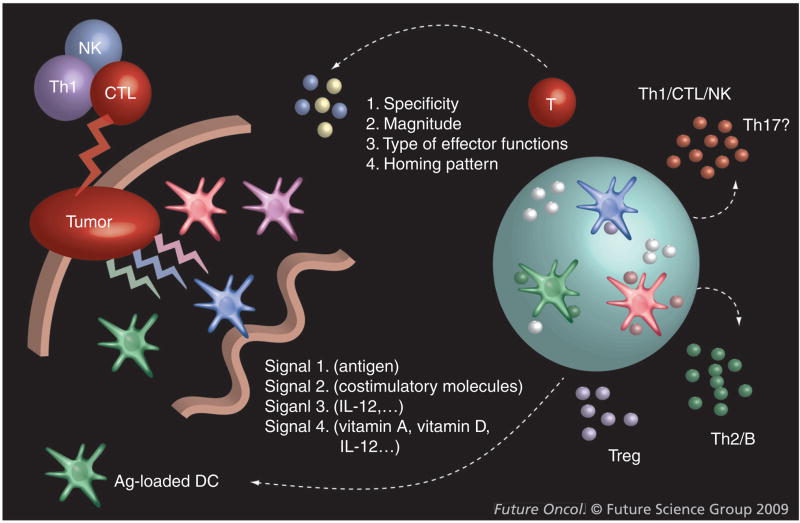
In addition to the constant need for the identification of additional antigens uniquely or preferentially expressed on cancer cells, and effective ways of bypassing the dysfunction of endogenous DCs in cancer patients, the areas that are critical for vaccine efficacy are the ability of DCs to induce T cells with the desirable effector functions and with the ability to enter tumor tissues (ability to deliver signal 3 and signal 4; Figure 1). Of additional impact can be the development of strategies of selectively, or at least preferentially, enhancing the effector arm of immune responses, without hyperactivating the regulatory cells.
Figure 1. Current model of anticancer immunity: roles of dendritic cells.
DCs provide T cells with antigenic ‘signal 1’ and costimulatory ‘signal 2’ [64–66], needed for the activation and expansion of pathogen-specific T cells. DCs also provide an additional polarizing ‘signal 3’, driving the development of immune responses towards type-1 or type-2 immunity [53], associated with differential involvement of particular effector mechanisms and different abilities to induce cancer rejection [53, 64–73]. Furthermore, recent studies indicate that DCs may also provide T cells with an additional signal (tentatively-termed ‘signal 4’) regulating organ-specific trafficking of immune cells [74–80]. The key role of DCs in regulating the expansion, acquisition of effector functions and or tumor-relevant homing properties suggest the possibility of exploiting these properties in the development of effective cancer immunotherapeutics.
Ag: Antigen; CTL: Cytotoxic T lymphocyte; DC: Dendritic cell; NK: Natural killer.
While we are clearly ‘not there yet’, it is likely that the road to the development of effective cancer vaccines will be measured in years, rather than decades. While current clinical trials are mostly conducted in the setting of advanced disease, the confirmation of even a limited advantage of such treatments for the survival of these groups of patients will pave the road to testing their activity in adjuvant or neoadjuvant settings in patients with resectable or resected tumors, or in patients with precancerous lesions, with the goal of establishing immune surveillance and preventing the onset of macroscopic disease or its recurrence.
Executive summary
▪ Recent identification of effective ways of enhancing immunogenicity of tumor-associated antigens, including the use of dendritic cells as potent vectors of cancer vaccines, provide effective tools to induce high numbers of circulating tumor-specific T cells.
▪ Despite the indications that some cancer vaccines may be able to delay tumor recurrence or prolong the survival of cancer patients, their ability to induce cancer regression remains low.
▪ Recent reports indicate that the successful induction of tumor-specific T cells by cancer vaccines is not necessarily associated with the induction of functional cytotoxic T lymphocytes, but instead lead to undesirable activation and expansion of regulatory T cells.
▪ In the current review, we discuss the possible ways of counteracting such negative phenomena using selected types of dendritic cells, in order to assure the desirable induction of cytotoxic T lymphocytes, Th1- and natural killer cells, their appropriate homing to tumor tissues and therapeutic effectiveness.
Acknowledgments
Financial & competing interests disclosure
This work was supported by the NIH grants CA095128, CA114931, CA101944, EA055944 and by the institutional funds in support of CA137214. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. No writing assistance was utilized in the production of this manuscript.
Contributor Information
Pawel Kalinski, Department of Surgery, University of Pittsburgh Cancer Institute, Hillman Cancer Center, Res. Pavilion, Suite 1.46, 5117 Center Avenue, PA 15213–1863, USA, Tel.: +1 412 623 7712; Fax: +1 412 623 7709; kalinskiP@upmc.edu.
Julie Urban, Department of Surgery, University of Pittsburgh Cancer Institute, Hillman Cancer Center, Res. Pavilion, Suite 1.46, 5117 Center Avenue, PA 15213–1863, USA.
Rahul Narang, Department of Surgery, University of Pittsburgh Cancer Institute, Hillman Cancer Center, Res. Pavilion, Suite 1.46, 5117 Center Avenue, PA 15213–1863, USA.
Erik Berk, Department of Surgery, University of Pittsburgh Cancer Institute, Hillman Cancer Center, Res. Pavilion, Suite 1.46, 5117 Center Avenue, PA 15213–1863, USA.
Ewa Wieckowski, Department of Surgery, University of Pittsburgh Cancer Institute, Hillman Cancer Center, Res. Pavilion, Suite 1.46, 5117 Center Avenue, PA 15213–1863, USA.
Ravikumar Muthuswamy, Department of Surgery, University of Pittsburgh Cancer Institute, Hillman Cancer Center, Res. Pavilion, Suite 1.46, 5117 Center Avenue, PA 15213–1863, USA.
Bibliography
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- 1.Nauts HC. Bacteria and cancer: antagonisms and benefits. Cancer Surv. 1989;8:713–723. [PubMed] [Google Scholar]
- 2.Burnet FM. The concept of immunological surveillance. Prog Exp Tumor Res. 1970;13:1–27. doi: 10.1159/000386035. [DOI] [PubMed] [Google Scholar]
- 3.Stutman O. Tumor development after 3-methylcholanthrene in immunologically deficient athymic-nude mice. Science. 1974;183:534–536. doi: 10.1126/science.183.4124.534. [DOI] [PubMed] [Google Scholar]
- 4.Banchereau J, Palucka AK. Dendritic cells as therapeutic vaccines against cancer. Nat Rev Immunol. 2005;5:296–306. doi: 10.1038/nri1592. [DOI] [PubMed] [Google Scholar]
- 5.Blattman JN, Greenberg PD. Cancer immunotherapy: a treatment for the masses. Science. 2004;305:200–205. doi: 10.1126/science.1100369. [DOI] [PubMed] [Google Scholar]
- 6.Figdor CG, de Vries IJ, Lesterhuis WJ, Melief CJ. Dendritic cell immunotherapy: mapping the way. Nat Med. 2004;10:475–480. doi: 10.1038/nm1039. [DOI] [PubMed] [Google Scholar]
- 7.Gilboa E. The promise of cancer vaccines. Nat Rev Cancer. 2004;4:401–411. doi: 10.1038/nrc1359. [DOI] [PubMed] [Google Scholar]
- 8.Rosenberg SA, Yang JC, Restifo NP. Cancer immunotherapy: moving beyond current vaccines. Nat Med. 2004;10:909–915. doi: 10.1038/nm1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Srivastava PK. Therapeutic cancer vaccines. Curr Opin Immunol. 2006;18:201–205. doi: 10.1016/j.coi.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 10.Rabinovich GA, Gabrilovich D, Sotomayor EM. Immunosuppressive strategies that are mediated by tumor cells. Annu Rev Immunol. 2007;25:267–296. doi: 10.1146/annurev.immunol.25.022106.141609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11▪.Gabrilovich D. Mechanisms and functional significance of tumour-induced dendritic-cell defects. Nat Rev Immunol. 2004;4:941–952. doi: 10.1038/nri1498. Comprehensive discussion of functional defects of endogenous dendritic cells (DCs) in cancer. [DOI] [PubMed] [Google Scholar]
- 12.Harzstark AL, Small EJ. Immunotherapy for prostate cancer using antigen-loaded antigen-presenting cells: APC8015 (Provenge) Expert Opin Biol Ther. 2007;7:1275–1280. doi: 10.1517/14712598.7.8.1275. [DOI] [PubMed] [Google Scholar]
- 13.Pilla L, Patuzzo R, Rivoltini L, et al. A Phase II trial of vaccination with autologous, tumor-derived heat-shock protein peptide complexes Gp96, in combination with GM-CSF and interferon-α in metastatic melanoma patients. Cancer Immunol Immunother. 2006;55:958–968. doi: 10.1007/s00262-005-0084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Small EJ, Schellhammer PF, Higano CS, et al. Placebo-controlled Phase III trial of immunologic therapy with sipuleucel-T (APC8015) in patients with metastatic, asymptomatic hormone refractory prostate cancer. J Clin Oncol. 2006;24:3089–3094. doi: 10.1200/JCO.2005.04.5252. [DOI] [PubMed] [Google Scholar]
- 15.Peoples GE, Holmes JP, Hueman MT, et al. Combined clinical trial results of a HER2/neu (E75) vaccine for the prevention of recurrence in high-risk breast cancer patients: U.S Military Cancer Institute Clinical Trials Group Study I-01 and I-02. Clin Cancer Res. 2008;14:797–803. doi: 10.1158/1078-0432.CCR-07-1448. [DOI] [PubMed] [Google Scholar]
- 16.Lurquin C, Lethe B, De Plaen E, et al. Contrasting frequencies of antitumor and anti-vaccine T cells in metastases of a melanoma patient vaccinated with a MAGE tumor antigen. J Exp Med. 2005;201:249–257. doi: 10.1084/jem.20041378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Godelaine D, Carrasco J, Lucas S, et al. Polyclonal CTL responses observed in melanoma patients vaccinated with dendritic cells pulsed with a MAGE-3.A1 peptide. J Immunol. 2003;171:4893–4897. doi: 10.4049/jimmunol.171.9.4893. [DOI] [PubMed] [Google Scholar]
- 18.Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392:245–252. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- 19.Rosenberg SA. Shedding light on immunotherapy for cancer. N Engl J Med. 2004;350:1461–1463. doi: 10.1056/NEJMcibr045001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schuler G, Steinman RM. Dendritic cells as adjuvants for immune-mediated resistance to tumors. J Exp Med. 1997;186:1183–1187. doi: 10.1084/jem.186.8.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steinman RM. The dendritic cell system and its role in immunogenecity. Annu Rev Immunol. 1991;9:271–296. doi: 10.1146/annurev.iy.09.040191.001415. [DOI] [PubMed] [Google Scholar]
- 22.Steinman RM, Banchereau J. Taking dendritic cells into medicine. Nature. 2007;449:419–426. doi: 10.1038/nature06175. [DOI] [PubMed] [Google Scholar]
- 23.Gabrilovich D, Pisarev V. Tumor escape from immune response: mechanisms and targets of activity. Curr Drug Targets. 2003;4:525–536. doi: 10.2174/1389450033490849. [DOI] [PubMed] [Google Scholar]
- 24.Yang L, Carbone DP. Tumor–host immune interactions and dendritic cell dysfunction. Adv Cancer Res. 2004;92:13–27. doi: 10.1016/S0065-230X(04)92002-7. [DOI] [PubMed] [Google Scholar]
- 25.Pinzon-Charry A, Maxwell T, Lopez JA. Dendritic cell dysfunction in cancer: a mechanism for immunosuppression. Immunol Cell Biol. 2005;83:451–461. doi: 10.1111/j.1440-1711.2005.01371.x. [DOI] [PubMed] [Google Scholar]
- 26.Uchida K, Schneider S, Yochim JM, et al. Intratumoral COX-2 gene expression is a predictive factor for colorectal cancer response to fluoropyrimidine-based chemotherapy. Clin Cancer Res. 2005;11:3363–3368. doi: 10.1158/1078-0432.CCR-04-1650. [DOI] [PubMed] [Google Scholar]
- 27.Williams C, Shattuck-Brandt RL, DuBois RN. The role of COX-2 in intestinal cancer. Ann N Y Acad Sci. 1999;889:72–83. doi: 10.1111/j.1749-6632.1999.tb08725.x. [DOI] [PubMed] [Google Scholar]
- 28.Inaba T, Sano H, Kawahito Y, et al. Induction of cyclooxygenase-2 in monocyte/macrophage by mucins secreted from colon cancer cells. Proc Natl Acad Sci USA. 2003;100:2736–2741. doi: 10.1073/pnas.0435410100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Soumaoro LT, Uetake H, Higuchi T, Takagi Y, Enomoto M, Sugihara K. Cyclooxygenase-2 expression: a significant prognostic indicator for patients with colorectal cancer. Clin Cancer Res. 2004;10:8465–8471. doi: 10.1158/1078-0432.CCR-04-0653. [DOI] [PubMed] [Google Scholar]
- 30.Almand B, Clark JI, Nikitina E, et al. Increased production of immature myeloid cells in cancer patients: a mechanism of immunosuppression in cancer. J Immunol. 2001;166:678–689. doi: 10.4049/jimmunol.166.1.678. [DOI] [PubMed] [Google Scholar]
- 31.Almand B, Resser JR, Lindman B, et al. Clinical significance of defective dendritic cell differentiation in cancer. Clin Cancer Res. 2000;6:1755–1766. [PubMed] [Google Scholar]
- 32.Gabrilovich DI, Velders MP, Sotomayor EM, Kast WM. Mechanism of immune dysfunction in cancer mediated by immature Gr-1+ myeloid cells. J Immunol. 2001;166:5398–5406. doi: 10.4049/jimmunol.166.9.5398. [DOI] [PubMed] [Google Scholar]
- 33.Young MR, Wright MA, Lozano Y, et al. Increased recurrence and metastasis in patients whose primary head and neck squamous cell carcinomas secreted granulocyte-macrophage colony-stimulating factor and contained CD34+ natural suppressor cells. Int J Cancer. 1997;74:69–74. doi: 10.1002/(sici)1097-0215(19970220)74:1<69::aid-ijc12>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 34.Bell D, Chomarat P, Broyles D, et al. In breast carcinoma tissue, immature dendritic cells reside within the tumor, whereas mature dendritic cells are located in peritumoral areas. J Exp Med. 1999;190:1417–1426. doi: 10.1084/jem.190.10.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Toriyama K, Wen DR, Paul E, Cochran AJ. Variations in the distribution, frequency, and phenotype of Langerhans cells during the evolution of malignant melanoma of the skin. J Invest Dermatol. 1993;100:269S–273S. doi: 10.1111/1523-1747.ep12470135. [DOI] [PubMed] [Google Scholar]
- 36.Troy AJ, Summers KL, Davidson PJ, Atkinson CH, Hart DN. Minimal recruitment and activation of dendritic cells within renal cell carcinoma. Clin Cancer Res. 1998;4:585–593. [PubMed] [Google Scholar]
- 37.Zou W, Machelon V, Coulomb-L’Hermin A, et al. Stromal-derived factor-1 in human tumors recruits and alters the function of plasmacytoid precursor dendritic cells. Nat Med. 2001;7:1339–1346. doi: 10.1038/nm1201-1339. [DOI] [PubMed] [Google Scholar]
- 38.Della Bella S, Gennaro M, Vaccari M, et al. Altered maturation of peripheral blood dendritic cells in patients with breast cancer. Br J Cancer. 2003;89:1463–1472. doi: 10.1038/sj.bjc.6601243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nefedova Y, Huang M, Kusmartsev S, et al. Hyperactivation of STAT3 is involved in abnormal differentiation of dendritic cells in cancer. J Immunol. 2004;172:464–474. doi: 10.4049/jimmunol.172.1.464. [DOI] [PubMed] [Google Scholar]
- 40.Oyama T, Ran S, Ishida T, et al. Vascular endothelial growth factor affects dendritic cell maturation through the inhibition of nuclear factor-κ B activation in hemopoietic progenitor cells. J Immunol. 1998;160:1224–1232. [PubMed] [Google Scholar]
- 41.Esche C, Lokshin A, Shurin GV, et al. Tumor’s other immune targets: dendritic cells. J Leukoc Biol. 1999;66:336–344. doi: 10.1002/jlb.66.2.336. [DOI] [PubMed] [Google Scholar]
- 42.Pirtskhalaishvili G, Shurin GV, Esche C, et al. Cytokine-mediated protection of human dendritic cells from prostate cancer-induced apoptosis is regulated by the Bcl-2 family of proteins. Br J Cancer. 2000;83:506–513. doi: 10.1054/bjoc.2000.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kitajima T, Ariizumi K, Bergstresser PR, Takashima A. Ultraviolet B radiation sensitizes a murine epidermal dendritic cell line (XS52) to undergo apoptosis upon antigen presentation to T cells. J Immunol. 1996;157:3312–3316. [PubMed] [Google Scholar]
- 44.Ludewig B, Graf D, Gelderblom HR, Becker Y, Kroczek RA, Pauli G. Spontaneous apoptosis of dendritic cells is efficiently inhibited by TRAP (CD40-ligand) and TNF-α, but strongly enhanced by interleukin-10. Eur J Immunol. 1995;25:1943–1950. doi: 10.1002/eji.1830250722. [DOI] [PubMed] [Google Scholar]
- 45.Bonham CA, Lu L, Li Y, Hoffman RA, Simmons RL, Thomson AW. Nitric oxide production by mouse bone marrow-derived dendritic cells: implications for the regulation of allogeneic T cell responses. Transplantation. 1996;62:1871–1877. doi: 10.1097/00007890-199612270-00033. [DOI] [PubMed] [Google Scholar]
- 46.Kanto T, Kalinski P, Hunter OC, Lotze MT, Amoscato AA. Ceramide mediates tumor-induced dendritic cell apoptosis. J Immunol. 2001;167:3773–3784. doi: 10.4049/jimmunol.167.7.3773. [DOI] [PubMed] [Google Scholar]
- 47▪.Mayordomo JI, Zorina T, Storkus WJ, et al. Bone marrow-derived dendritic cells pulsed with synthetic tumour peptides elicit protective and therapeutic antitumour immunity. Nat Med. 1995;1:1297–1302. doi: 10.1038/nm1295-1297. Original demonstration of antitumor activity of the therapeutic cancer vaccines utilizing ex vivo-generated DCs in multiple mouse models. [DOI] [PubMed] [Google Scholar]
- 48.Steinman RM, Adams JC, Cohn ZA. Identification of a novel cell type in peripheral lymphoid organs of mice IV Identification and distribution in mouse spleen. J Exp Med. 1975;141:804–820. [PMC free article] [PubMed] [Google Scholar]
- 49.Steinman RM, Cohn ZA. Identification of a novel cell type in peripheral lymphoid organs of mice I Morphology, quantitation, tissue distribution. J Exp Med. 1973;137:1142–1162. doi: 10.1084/jem.137.5.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Steinman RM, Cohn ZA. Identification of a novel cell type in peripheral lymphoid organs of mice II Functional properties in vitro. J Exp Med. 1974;139:380–397. doi: 10.1084/jem.139.2.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51▪.Steinman RM, Lustig DS, Cohn ZA. Identification of a novel cell type in peripheral lymphoid organs of mice. 3. Functional properties in vivo. J Exp Med. 1974;139:1431–1445. doi: 10.1084/jem.139.6.1431. References [49–51] are a three-part series that identify and describe mouse DCs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fujii S, Shimizu K, Hemmi H, et al. Glycolipid α-C-galactosylceramide is a distinct inducer of dendritic cell function during innate and adaptive immune responses of mice. Proc Natl Acad Sci USA. 2006;103:11252–11257. doi: 10.1073/pnas.0604812103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kalinski P, Hilkens CM, Wierenga EA, Kapsenberg ML. T-cell priming by type-1 and type-2 polarized dendritic cells: the concept of a third signal. Immunol Today. 1999;20:561–567. doi: 10.1016/s0167-5699(99)01547-9. [DOI] [PubMed] [Google Scholar]
- 54.Kalinski P, Schuitemaker JH, Hilkens CM, Wierenga EA, Kapsenberg ML. Final maturation of dendritic cells is associated with impaired responsiveness to IFN-γ and to bacterial IL-12 inducers: decreased ability of mature dendritic cells to produce IL-12 during the interaction with Th cells. J Immunol. 1999;162:3231–3236. [PubMed] [Google Scholar]
- 55▪▪.Vieira PL, de Jong EC, Wierenga EA, Kapsenberg ML, Kalinski P. Development of Th1-inducing capacity in myeloid dendritic cells requires environmental instruction. J Immunol. 2000;164:4507–4512. doi: 10.4049/jimmunol.164.9.4507. Original demonstration that DCs matured in the presence of IFN-γ avoid ‘exhaustion’, retain their ability to produce high levels of IL-12 upon interaction with T cells, and show strongly elevated activity in inducing Th1 responses. Such type-1-polarized DCs (DC1s) show enhanced resistance to suppressive factors, facilitating their potential use in immunotherapy. [DOI] [PubMed] [Google Scholar]
- 56.Kalinski P, Schuitemaker JH, Hilkens CM, Kapsenberg ML. Prostaglandin E2 induces the final maturation of IL-12-deficient CD1a+CD83+ dendritic cells: the levels of IL-12 are determined during the final dendritic cell maturation and are resistant to further modulation. J Immunol. 1998;161:2804–2809. [PubMed] [Google Scholar]
- 57▪▪.Hsu FJ, Benike C, Fagnoni F, et al. Vaccination of patients with B-cell lymphoma using autologous antigen-pulsed dendritic cells. Nat Med. 1996;2:52–58. doi: 10.1038/nm0196-52. First demonstration of the immunologic and clinical efficacy of DC-based therapeutic cancer vaccines in four cancer patients with B-cell lymphoma. [DOI] [PubMed] [Google Scholar]
- 58▪▪.Nestle FO, Alijagic S, Gilliet M, et al. Vaccination of melanoma patients with peptide- or tumor lysate-pulsed dendritic cells. Nat Med. 1998;4:328–332. doi: 10.1038/nm0398-328. First demonstration of the immunologic and clinical efficacy of DC-based therapeutic cancer vaccines in patients with melanoma (16 patients) [DOI] [PubMed] [Google Scholar]
- 59.Nestle FO, Farkas A, Conrad C. Dendritic-cell-based therapeutic vaccination against cancer. Curr Opin Immunol. 2005;17:163–169. doi: 10.1016/j.coi.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 60.Pardoll DM. Cancer vaccines. Nat Med. 1998;4:525–531. doi: 10.1038/nm0598supp-525. [DOI] [PubMed] [Google Scholar]
- 61.Parmiani G, Pilla L, Castelli C, Rivoltini L. Vaccination of patients with solid tumours. Ann Oncol. 2003;14:817–824. doi: 10.1093/annonc/mdg246. [DOI] [PubMed] [Google Scholar]
- 62.Steinman RM. Dendritic cells and immune-based therapies. Exp Hematol. 1996;24:859–862. [PubMed] [Google Scholar]
- 63.Steinman RM, Dhodapkar M. Active immunization against cancer with dendritic cells: the near future. Int J Cancer. 2001;94:459–473. doi: 10.1002/ijc.1503. [DOI] [PubMed] [Google Scholar]
- 64.Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392:245–252. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- 65.Schuler G, Schuler-Thurner B, Steinman RM. The use of dendritic cells in cancer immunotherapy. Curr Opin Immunol. 2003;15:138–147. doi: 10.1016/s0952-7915(03)00015-3. [DOI] [PubMed] [Google Scholar]
- 66.Schuler G, Steinman RM. Dendritic cells as adjuvants for immune-mediated resistance to tumors. J Exp Med. 1997;186:1183–1187. doi: 10.1084/jem.186.8.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kapsenberg ML. Dendritic-cell control of pathogen-driven T-cell polarization. Nat Rev Immunol. 2003;3:984–993. doi: 10.1038/nri1246. [DOI] [PubMed] [Google Scholar]
- 68.Ikeda H, Chamoto K, Tsuji T, et al. The critical role of type-1 innate and acquired immunity in tumor immunotherapy. Cancer Sci. 2004;95:697–703. doi: 10.1111/j.1349-7006.2004.tb03248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pulendran B. Modulating TH1/TH2 responses with microbes, dendritic cells, and pathogen recognition receptors. Immunol Res. 2004;29:187–196. doi: 10.1385/IR:29:1-3:187. [DOI] [PubMed] [Google Scholar]
- 70.Trinchieri G. Interleukin-12 and the regulation of innate resistance and adaptive immunity. Nat Rev Immunol. 2003;3:133–146. doi: 10.1038/nri1001. [DOI] [PubMed] [Google Scholar]
- 71.Palucka K, Banchereau J. How dendritic cells and microbes interact to elicit or subvert protective immune responses. Curr Opin Immunol. 2002;14:420–431. doi: 10.1016/s0952-7915(02)00365-5. [DOI] [PubMed] [Google Scholar]
- 72.Czerniecki BJ, Cohen PA, Faries M, Xu S, Roros JG, Bedrosian I. Diverse functional activity of CD83+ monocyte-derived dendritic cells and the implications for cancer vaccines. Crit Rev Immunol. 2001;21:157–178. [PubMed] [Google Scholar]
- 73.Kalinski P, Moser M. Consensual immunity: success-driven development of T-helper-1 and T-helper-2 responses. Nat Rev Immunol. 2005;5:251–260. doi: 10.1038/nri1569. [DOI] [PubMed] [Google Scholar]
- 74.Mora JR, Bono MR, Manjunath N, et al. Selective imprinting of gut-homing T cells by Peyer’s patch dendritic cells. Nature. 2003;424:88–93. doi: 10.1038/nature01726. [DOI] [PubMed] [Google Scholar]
- 75.Mora JR, Cheng G, Picarella D, Briskin M, Buchanan N, von Andrian UH. Reciprocal and dynamic control of CD8 T cell homing by dendritic cells from skin- and gut-associated lymphoid tissues. J Exp Med. 2005;201:303–316. doi: 10.1084/jem.20041645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mora JR, von Andrian UH. Retinoic acid: an educational “vitamin elixir” for gut-seeking T cells. Immunity. 2004;21:458–460. doi: 10.1016/j.immuni.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 77.Schaerli P, Loetscher P, Moser B. Cutting edge: induction of follicular homing precedes effector Th cell development. J Immunol. 2001;167:6082–6086. doi: 10.4049/jimmunol.167.11.6082. [DOI] [PubMed] [Google Scholar]
- 78.Stagg AJ, Kamm MA, Knight SC. Intestinal dendritic cells increase T cell expression of α4β7 integrin. Eur J Immunol. 2002;32:1445–1454. doi: 10.1002/1521-4141(200205)32:5<1445::AID-IMMU1445>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 79.Weninger W, Manjunath N, von Andrian UH. Migration and differentiation of CD8+ T cells. Immunol Rev. 2002;186:221–233. doi: 10.1034/j.1600-065x.2002.18618.x. [DOI] [PubMed] [Google Scholar]
- 80.Calzascia T, Masson F, Di Berardino-Besson W, et al. Homing phenotypes of tumor-specific CD8 T cells are predetermined at the tumor site by crosspresenting APCs. Immunity. 2005;22:175–184. doi: 10.1016/j.immuni.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 81▪.Fernandez NC, Lozier A, Flament C, et al. Dendritic cells directly trigger NK cell functions: cross-talk relevant in innate anti-tumor immune responses in vivo. Nat Med. 1999;5:405–411. doi: 10.1038/7403. First demonstration of the ability of DCs to promote anti-tumor activity of the innate immune system. [DOI] [PubMed] [Google Scholar]
- 82.Dhodapkar MV, Steinman RM, Sapp M, et al. Rapid generation of broad T-cell immunity in humans after a single injection of mature dendritic cells. J Clin Invest. 1999;104:173–180. doi: 10.1172/JCI6909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Adema GJ, de Vries IJ, Punt CJ, Figdor CG. Migration of dendritic cell based cancer vaccines: in vivo veritas? Curr Opin Immunol. 2005;17:170–174. doi: 10.1016/j.coi.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 84.De Vries IJ, Krooshoop DJ, Scharenborg NM, et al. Effective migration of antigen-pulsed dendritic cells to lymph nodes in melanoma patients is determined by their maturation state. Cancer Res. 2003;63:12–17. [PubMed] [Google Scholar]
- 85.Zitvogel L, Mayordomo JI, Tjandrawan T, et al. Therapy of murine tumors with tumor peptide-pulsed dendritic cells: dependence on T cells B7 costimulation, and T helper cell 1-associated cytokines. J Exp Med. 1996;183:87–97. doi: 10.1084/jem.183.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Furumoto K, Arii S, Yamasaki S, et al. Spleen-derived dendritic cells engineered to enhance interleukin-12 production elicit therapeutic antitumor immune responses. Int J Cancer. 2000;87:665–672. [PubMed] [Google Scholar]
- 87.Nishioka Y, Hirao M, Robbins PD, Lotze MT, Tahara H. Induction of systemic and therapeutic antitumor immunity using intratumoral injection of dendritic cells genetically modified to express interleukin 12. Cancer Res. 1999;59:4035–4041. [PubMed] [Google Scholar]
- 88.de Vries IJ, Lesterhuis WJ, Scharenborg NM, et al. Maturation of dendritic cells is a prerequisite for inducing immune responses in advanced melanoma patients. Clin Cancer Res. 2003;9:5091–5100. [PubMed] [Google Scholar]
- 89.Jonuleit H, Kuhn U, Muller G, et al. Pro-inflammatory cytokines and prostaglandins induce maturation of potent immunostimulatory dendritic cells under fetal calf serum-free conditions. Eur J Immunol. 1997;27:3135–3142. doi: 10.1002/eji.1830271209. [DOI] [PubMed] [Google Scholar]
- 90.Langenkamp A, Messi M, Lanzavecchia A, Sallusto F. Kinetics of dendritic cell activation: impact on priming of TH1 TH2 and nonpolarized T cells. Nat Immunol. 2000;1:311–316. doi: 10.1038/79758. [DOI] [PubMed] [Google Scholar]
- 91.Mailliard RB, Wankowicz-Kalinska A, Cai Q, et al. α-type-1 polarized dendritic cells: a novel immunization tool with optimized CTL-inducing activity. Cancer Res. 2004;64:5934–5937. doi: 10.1158/0008-5472.CAN-04-1261. [DOI] [PubMed] [Google Scholar]
- 92.Luft T, Jefford M, Luetjens P, et al. Functionally distinct dendritic cell (DC) populations induced by physiologic stimuli: prostaglandin E(2) regulates the migratory capacity of specific DC subsets. Blood. 2002;100:1362–1372. doi: 10.1182/blood-2001-12-0360. [DOI] [PubMed] [Google Scholar]
- 93.Scandella E, Men Y, Gillessen S, Forster R, Groettrup M. Prostaglandin E2 is a key factor for CCR7 surface expression and migration of monocyte-derived dendritic cells. Blood. 2002;100:1354–1361. doi: 10.1182/blood-2001-11-0017. [DOI] [PubMed] [Google Scholar]
- 94.Kalinski P, Mailliard RB, Giermasz A, et al. Natural killer-dendritic cell cross-talk in cancer immunotherapy. Expert Opin Biol Ther. 2005;5:1303–1315. doi: 10.1517/14712598.5.10.1303. [DOI] [PubMed] [Google Scholar]
- 95.Mailliard RB, Egawa S, Cai Q, et al. Complementary dendritic cell-activating function of CD8+ and CD4+ T cells: helper role of CD8+ T cells in the development of T helper type 1 responses. J Exp Med. 2002;195:473–483. doi: 10.1084/jem.20011662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mailliard RB, Son YI, Redlinger R, et al. Dendritic cells mediate NK cell help for Th1 and CTL responses: two-signal requirement for the induction of NK cell helper function. J Immunol. 2003;171:2366–2373. doi: 10.4049/jimmunol.171.5.2366. [DOI] [PubMed] [Google Scholar]
- 97.Xu S, Koski GK, Faries M, et al. Rapid high efficiency sensitization of CD8+ T cells to tumor antigens by dendritic cells leads to enhanced functional avidity and direct tumor recognition through an IL-12-dependent mechanism. J Immunol. 2003;171:2251–2261. doi: 10.4049/jimmunol.171.5.2251. [DOI] [PubMed] [Google Scholar]
- 98.Wesa A, Kalinski P, Kirkwood JM, Tatsumi T, Storkus WJ. Polarized type-1 dendritic cells (DC1) producing high levels of IL-12 family members rescue patient TH1-type antimelanoma CD4+ T cell responses in vitro. J Immunother. 2007;30:75–82. doi: 10.1097/01.cji.0000211316.15278.6e. [DOI] [PubMed] [Google Scholar]
- 99.Kalinski P, Nakamura Y, Watchmaker P, Giermasz A, Muthuswamy R, Mailliard RB. Helper roles of NK and CD8+ T cells in the induction of tumor immunity Polarized dendritic cells as cancer vaccines. Immunol Res. 2006;36:137–146. doi: 10.1385/IR:36:1:137. [DOI] [PubMed] [Google Scholar]
- 100.Ten Brinke A, Karsten ML, Dieker MC, Zwaginga JJ, van Ham SM. The clinical grade maturation cocktail monophosphoryl lipid A plus IFNγ generates monocyte-derived dendritic cells with the capacity to migrate and induce Th1 polarization. Vaccine. 2007;25:7145–7152. doi: 10.1016/j.vaccine.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 101▪▪.Muthuswamy R, Urban J, Lee JJ, Reinhart TA, Bartlett D, Kalinski P. Ability of mature dendritic cells to interact with regulatory T cells is imprinted during maturation. Cancer Res. 2008;68:5972–5978. doi: 10.1158/0008-5472.CAN-07-6818. Original demonstration that DCs maturing in different environments show propensity to preferentially interact with different types of immune cells. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tarbell KV, Petit L, Zuo X, et al. Dendritic cell-expanded, islet-specific CD4+ CD25+ CD62L+ regulatory T cells restore normoglycemia in diabetic NOD mice. J Exp Med. 2007;204:191–201. doi: 10.1084/jem.20061631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yamazaki S, Inaba K, Tarbell KV, Steinman RM. Dendritic cells expand antigen-specific Foxp3+ CD25+ CD4+ regulatory T cells including suppressors of alloreactivity. Immunol Rev. 2006;212:314–329. doi: 10.1111/j.0105-2896.2006.00422.x. [DOI] [PubMed] [Google Scholar]
- 104.Yamazaki S, Iyoda T, Tarbell K, et al. Direct expansion of functional CD25+ CD4+ regulatory T cells by antigen-processing dendritic cells. J Exp Med. 2003;198:235–247. doi: 10.1084/jem.20030422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105▪▪.Banerjee DK, Dhodapkar MV, Matayeva E, Steinman RM, Dhodapkar KM. Expansion of FOXP3high regulatory T cells by human dendritic cells (DCs) in vitro and after injection of cytokine-matured DCs in myeloma patients. Blood. 2006;108:2655–2661. doi: 10.1182/blood-2006-03-011353. Demonstration of the ability of commonly used DC-based vaccines generated in the presence of PGE2 to promote the expansion of Treg cells in vaccinated cancer patients. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dhodapkar MV, Steinman RM. Antigen-bearing immature dendritic cells induce peptide-specific CD8+ regulatory T cells in vivo in humans. Blood. 2002;100:174–177. doi: 10.1182/blood.v100.1.174. [DOI] [PubMed] [Google Scholar]
- 107.Lee JJ, Foon KA, Mailliard RB, Muthuswamy R, Kalinski P. Type 1-polarized dendritic cells loaded with autologous tumor are a potent immunogen against chronic lymphocytic leukemia. J Leukoc Biol. 2008;84(1):319–325. doi: 10.1189/jlb.1107737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Giermasz AS, Urban JA, Nakamura Y, et al. Type-1 polarized dendritic cells primed for high IL-12 production show enhanced activity as cancer vaccines. Clin Immunol Immunother. 2009 doi: 10.1007/s00262-008-0648-5. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cerundolo V, Salio M. Harnessing NKT cells for therapeutic applications. Curr Top Microbiol Immunol. 2007;314:325–340. doi: 10.1007/978-3-540-69511-0_13. [DOI] [PubMed] [Google Scholar]
- 110.Hermans IF, Silk JD, Gileadi U, et al. NKT cells enhance CD4+ and CD8+ T cell responses to soluble antigen in vivo through direct interaction with dendritic cells. J Immunol. 2003;171:5140–5147. doi: 10.4049/jimmunol.171.10.5140. [DOI] [PubMed] [Google Scholar]
- 111.Liu K, Idoyaga J, Charalambous A, et al. Innate NKT lymphocytes confer superior adaptive immunity via tumor-capturing dendritic cells. J Exp Med. 2005;202:1507–1516. doi: 10.1084/jem.20050956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hermans IF, Silk JD, Gileadi U, et al. Dendritic cell function can be modulated through cooperative actions of TLR ligands and invariant NKT cells. J Immunol. 2007;178:2721–2729. doi: 10.4049/jimmunol.178.5.2721. [DOI] [PubMed] [Google Scholar]
- 113.Fujii S, Shimizu K, Kronenberg M, Steinman RM. Prolonged IFN-γ-producing NKT response induced with α-galactosylceramide-loaded DCs. Nat Immunol. 2002;3:867–874. doi: 10.1038/ni827. [DOI] [PubMed] [Google Scholar]
- 114.Mailliard RB, Alber SM, Shen H, et al. IL-18-induced CD83+CCR7+ NK helper cells. J Exp Med. 2005;202:941–953. doi: 10.1084/jem.20050128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Watchmaker P, Urban J, Berk E, et al. Memory CD8+ T cells protect dendritic cells from CTL killing. J Immunol. 2008;180:3857–3865. doi: 10.4049/jimmunol.180.6.3857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Thomas MJ, Noble A, Sawicka E, Askenase PW, Kemeny DM. CD8 T cells inhibit IgE via dendritic cell IL-12 induction that promotes Th1 T cell counter-regulation. J Immunol. 2002;168:216–223. doi: 10.4049/jimmunol.168.1.216. [DOI] [PubMed] [Google Scholar]
- 117.Nakamura Y, Watchmaker P, Urban J, et al. Helper function of memory CD8+ T cells: heterologous CD8+ T cells support the induction of therapeutic cancer immunity. Cancer Res. 2007;67:10012–10018. doi: 10.1158/0008-5472.CAN-07-1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Steinman RM. Dendritic cells and the control of immunity: enhancing the efficiency of antigen presentation. Mt Sinai J Med. 2001;68:160–166. [PubMed] [Google Scholar]
- 119.Trumpfheller C, Finke JS, Lopez CB, et al. Intensified and protective CD4+ T cell immunity in mice with anti-dendritic cell HIV gag fusion antibody vaccine. J Exp Med. 2006;203:607–617. doi: 10.1084/jem.20052005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pulendran B, Smith JL, Caspary G, et al. Distinct dendritic cell subsets differentially regulate the class of immune response in vivo. Proc Natl Acad Sci USA. 1999;96:1036–1041. doi: 10.1073/pnas.96.3.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hildner K, Edelson BT, Purtha WE, et al. Batf3 deficiency reveals a critical role for CD8α+ dendritic cells in cytotoxic T cell immunity. Science. 2008;322:1097–1100. doi: 10.1126/science.1164206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ferlazzo G, Klein J, Paliard X, Wei WZ, Galy A. Dendritic cells generated from CD34+ progenitor cells with flt3 ligand, c-kit ligand GM-CSF IL-4, and TNF-α are functional antigen-presenting cells resembling mature monocyte-derived dendritic cells. J Immunother. 2000;23:48–58. doi: 10.1097/00002371-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 123.Min YH, Lee ST, Choi KM, et al. Ex vivo generation of functional dendritic cells from mobilized CD34+ hematopoietic stem cells. Yonsei Med J. 1998;39:328–338. doi: 10.3349/ymj.1998.39.4.328. [DOI] [PubMed] [Google Scholar]
- 124.Berg EL, Goldstein LA, Jutila MA, et al. Homing receptors and vascular addressins: cell adhesion molecules that direct lymphocyte traffic. Immunol Rev. 1989;108:5–18. doi: 10.1111/j.1600-065x.1989.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 125.Picker LJ, Kishimoto TK, Smith CW, Warnock RA, Butcher EC. ELAM-1 is an adhesion molecule for skin-homing T cells. Nature. 1991;349:796–799. doi: 10.1038/349796a0. [DOI] [PubMed] [Google Scholar]
- 126.Picker LJ, Terstappen LW, Rott LS, Streeter PR, Stein H, Butcher EC. Differential expression of homing-associated adhesion molecules by T cell subsets in man. J Immunol. 1990;145:3247–3255. [PubMed] [Google Scholar]
- 127.Picker LJ, Treer JR, Ferguson-Darnell B, Collins PA, Bergstresser PR, Terstappen LW. Control of lymphocyte recirculation in man II Differential regulation of the cutaneous lymphocyte-associated antigen, a tissue-selective homing receptor for skin-homing T cells. J Immunol. 1993;150:1122–1136. [PubMed] [Google Scholar]
- 128.Sallusto F, Lanzavecchia A. Understanding dendritic cell and T-lymphocyte traffic through the analysis of chemokine receptor expression. Immunol Rev. 2000;177:134–140. doi: 10.1034/j.1600-065x.2000.17717.x. [DOI] [PubMed] [Google Scholar]
- 129.Sallusto F, Mackay CR. Chemoattractants and their receptors in homeostasis and inflammation. Curr Opin Immunol. 2004;16:724–731. doi: 10.1016/j.coi.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 130.Sallusto F, Mackay CR, Lanzavecchia A. The role of chemokine receptors in primary, effector, and memory immune responses. Annu Rev Immunol. 2000;18:593–620. doi: 10.1146/annurev.immunol.18.1.593. [DOI] [PubMed] [Google Scholar]
- 131.Johansson-Lindbom B, Svensson M, Wurbel MA, Malissen B, Marquez G, Agace W. Selective generation of gut tropic T cells in gut-associated lymphoid tissue (GALT): requirement for GALT dendritic cells and adjuvant. J Exp Med. 2003;198:963–969. doi: 10.1084/jem.20031244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132▪▪.Sigmundsdottir H, Pan J, Debes GF, et al. DCs metabolize sunlight-induced vitamin D3 to ‘program’ T cell attraction to the epidermal chemokine CCL27. Nat Immunol. 2007;8:285–293. doi: 10.1038/ni1433. Elegant demonstration that skin-homing properties can be imprinted in T cells by DCs in the mechanism involving vitamin D. [DOI] [PubMed] [Google Scholar]
- 133▪▪.Iwata M, Hirakiyama A, Eshima Y, Kagechika H, Kato C, Song SY. Retinoic acid imprints gut-homing specificity on T cells. Immunity. 2004;21:527–538. doi: 10.1016/j.immuni.2004.08.011. Demonstration of the role of retinoic acid in imprinting of gut-homing properties in T cells, and the role of DCs in this process. [DOI] [PubMed] [Google Scholar]
- 134.Mortarini R, Borri A, Tragni G, et al. Peripheral burst of tumor-specific cytotoxic T lymphocytes and infiltration of metastatic lesions by memory CD8+ T cells in melanoma patients receiving interleukin 12. Cancer Res. 2000;60:3559–3568. [PubMed] [Google Scholar]
- 135.Berger TG, Haendle I, Schrama D, et al. Circulation and homing of melanoma-reactive T cells to both cutaneous and visceral metastases after vaccination with monocyte-derived dendritic cells. Int J Cancer. 2004;111:229–237. doi: 10.1002/ijc.20238. [DOI] [PubMed] [Google Scholar]
- 136.Piras F, Colombari R, Minerba L, et al. The predictive value of CD8 CD4 CD68, and human leukocyte antigen-D-related cells in the prognosis of cutaneous malignant melanoma with vertical growth phase. Cancer. 2005;104:1246–1254. doi: 10.1002/cncr.21283. [DOI] [PubMed] [Google Scholar]
- 137▪▪.Galon J, Costes A, Sanchez-Cabo F, et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313:1960–1964. doi: 10.1126/science.1129139. Demonstration that the level of T-cell infiltration (T-cell density in tumors and their effector phenotype) is a strong prognostic factor of long-term survival of colorectal cancer patients. [DOI] [PubMed] [Google Scholar]
- 138.Galon J, Fridman WH, Pages F. The adaptive immunologic microenvironment in colorectal cancer: a novel perspective. Cancer Res. 2007;67:1883–1886. doi: 10.1158/0008-5472.CAN-06-4806. [DOI] [PubMed] [Google Scholar]
- 139.Pages F, Berger A, Camus M, et al. Effector memory T cells, early metastasis, and survival in colorectal cancer. N Engl J Med. 2005;353:2654–2666. doi: 10.1056/NEJMoa051424. [DOI] [PubMed] [Google Scholar]
- 140.Haanen JB, Baars A, Gomez R, et al. Melanoma-specific tumor-infiltrating lymphocytes but not circulating melanoma-specific T cells may predict survival in resected advanced-stage melanoma patients. Cancer Immunol Immunother. 2006;55:451–458. doi: 10.1007/s00262-005-0018-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mullins IM, Slingluff CL, Lee JK, et al. CXC chemokine receptor 3 expression by activated CD8+ T cells is associated with survival in melanoma patients with stage III disease. Cancer Res. 2004;64:7697–7701. doi: 10.1158/0008-5472.CAN-04-2059. [DOI] [PubMed] [Google Scholar]
- 142.Curiel TJ, Coukos G, Zou L, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med. 2004;10:942–949. doi: 10.1038/nm1093. [DOI] [PubMed] [Google Scholar]
- 143▪.Kunz M, Toksoy A, Goebeler M, Engelhardt E, Brocker E, Gillitzer R. Strong expression of the lymphoattractant C-X-C chemokine Mig is associated with heavy infiltration of T cells in human malignant melanoma. J Pathol. 1999;189:552–558. doi: 10.1002/(SICI)1096-9896(199912)189:4<552::AID-PATH469>3.0.CO;2-I. Original demonstration of the correlation between the expression of pro-inflammatory chemokine CXCL9 and tumor infiltrating lymphocyte density in melanoma lesions. [DOI] [PubMed] [Google Scholar]
- 144.Ohtani H, Jin Z, Takegawa S, Nakayama T, Yoshie O. Abundant expression of CXCL9 (MIG) by stromal cells that include dendritic cells and accumulation of CXCR3+ T cells in lymphocyte-rich gastric carcinoma. J Pathol. 2009;217:21–31. doi: 10.1002/path.2448. [DOI] [PubMed] [Google Scholar]