Abstract
Despite major advances in the long-term survival of premature infants, cognitive deficits occur in 30–50% of very preterm (<32 gestational weeks) survivors. Impaired working memory and attention despite average global intelligence are central to the academic difficulties of the survivors. Periventricular leukomalacia (PVL), characterized by periventricular necrosis and diffuse gliosis in the cerebral white matter, is the major brain pathology in preterm infants (7–10). We tested the novel hypothesis that pathology in thalamic nuclei critical for working memory and attention, i.e., mediodorsal nucleus and reticular nucleus, respectively, occurs in PVL. In 22 PVL cases (gestational age 32.5±4.8 weeks) and 16 non-PVL controls (36.7±5.2 weeks) who died within infancy, the incidence of thalamic pathology was significantly higher in PVL cases (59%; 13/22) compared to controls (19%; 3/16)(p=0.01), with substantial involvement of the mediodorsal and reticular nuclei in PVL. The prevention of thalamic damage may be required for the eradication of defects in survivors with PVL.
Keywords: limbic system, mediodorsal nucleus, oxidative stress, prefrontal cortex, reticular nucleus, working memory
Despite major advances in the long-term survival of premature infants, cognitive deficits occur in 30–50% of very preterm (<32 gestational weeks) survivors (1). Impaired working memory and attention despite average global intelligence are central to the academic difficulties of the survivors (2–6). Prevention of these deficits depends upon a firm understanding of their neuropathologic basis directly in the developing human brain. Periventricular leukomalacia (PVL), characterized by periventricular necrosis and diffuse gliosis in the cerebral white matter, is the major brain pathology in preterm infants (7–10). While long tract involvement by periventricular necrosis readily explains cerebral palsy (7), it is uncertain how PVL accounts for cognitive abnormalities. Situated deep in the brain’s center, the thalamus is strategically positioned to mediate cognition via reciprocal interconnections with the entire cerebral cortex (11–13). In a recent survey of the neuropathology of premature infants dying in the perinatal period (14), we reported semi-quantitative evidence of neuronal loss in the thalamus in 38% of the cases with PVL, in contrast to only 13% in cerebral cortex. These discordant findings suggested the possibility that the thalamus, and not the cerebral cortex, is the preferential site of cognitive dysfunction in preterm survivors with PVL. Germane to this possibility is the recognition that all thalamic nuclei, with the exception of the reticular nucleus, project to preferred targets in the cerebral cortex (11), and that the neurological consequences of damage to an individual thalamic nucleus mimic those related to the cortical target itself (11).
In the following study, we focused in-depth upon two thalamic nuclei, i.e., mediodorsal nucleus and reticular nucleus, because they are essential for working memory and attention, respectively, and lesions within them could significantly impair school performance as seen in survivors of prematurity (2–6). We tested the novel hypothesis that pathology in thalamic nuclei critical for working memory and attention, i.e., mediodorsal nucleus and reticular nucleus, respectively, occurs in PVL. We surveyed all thalamic nuclei but focused quantitative studies upon the mediodorsal nucleus (medial tier) compared to the lateral posterior nucleus (lateral tier) in order to establish regional specificity, analyzing the density of reactive astrocytes, activated microglia, and total neurons; we further determined the thalamic histopathology in the mediodorsal nucleus, the incidence of damaged axons, as indicated by fractin, a marker of axonal injury (15), and density and incidence of neurons expressing malondialdehyde (MDA), a marker of oxidative stress (16), in the mediodorsal nucleus.
Materials and Methods
Clinicopathologic Database
Thalamic tissue samples from a total of 36 fetal and neonatal cases were collected from the archival autopsy service of the Department of Pathology, Children’s Hospital Boston and Brigham and Women’s Hospital. Parental permission for research was given according to the guidelines of and permission of the Humans Protections Committee (Institutional Review Board). PVL was defined as histopathology in the immature cerebral white matter with a: 1) ‘focal’ necrotic component in the periventricular region and 2) ‘diffuse’ component characterized by reactive gliosis and activated microglia in the surrounding white matter (8, 9). Control cases did not demonstrate these white matter features, as in previous PVL studies utilizing similar controls from our laboratory (10, 14, 15). Tissue was fixed in 4% paraformaldehyde, paraffin-embedded, and cut on a conventional microtome at 4 µm. All cases were processed for standard histological examination (e.g. hematoxylin and eosin/Luxol fast blue staining). Age was expressed as postconceptional age (PCA) in weeks (gestational age plus post-natal age).
Neuropathologic Survey
Each case was reviewed blinded without knowledge of the presence or absence of PVL or other clinicopathologic features. We assessed each thalamus for the following histopathologic features (as defined by standard criteria (9)) in microscopic sections stained with hematoxylin-and-eosin/Luxol-fast-blue: neuronal loss, neuronophagia, gliosis, activated microglia/macrophages, microglial nodules, mineralization, axonal spheroids/fragments, micro-infarcts, macro-infarcts (apparent distribution of posterior cerebral artery), and hemorrhage. There was no evidence of thalamic infection in any case. Thalamic sections were analyzed at one of the following levels: I (anterior), level of the mammillary bodies; II (mid), level of the red nucleus; and III (posterior), level of the lateral geniculate nucleus (17). No significant differences in quantitative parameters were observed between the levels in PVL and non-PVL cases (data not shown). We defined Pattern 0 as no pathology; and Pattern 1 as gliosis with ≥5 glial fibrillary acidic protein (GFAP)-positive cells/hpf, the latter based upon the observation that the mean density of such cells in the controls was 1.93+3.6/hpf and pathologic gliosis was considered greater than this mean and standard deviation. Due to the unique structure of the reticular nucleus as a thin “rim” of small neuronal clusters encasing the thalamus, we characterized its pathology on a descriptive basis only: 1) mild gliosis without obvious neuronal loss; 2) moderate gliosis with obvious, focal neuronal loss; and 2) severe gliosis with complete neuronal loss.
Immunocytochemistry
Immunocytochemistry with appropriate antibodies was conducted to identify reactive astrocytes (GFAP) (Biogenex, San Ramon, CA, prediluted), activated microglia/macrophages (CD68, Biocare Medical, Concord, CA, prediluted), axonal damage (fractin, BD, Franklin Lakes, NJ, 1:500), and oxidative stress (malondialdehyde [MDA], Abcam, Cambridge, MA, 1:400). Standard immunocytochemistry procedures were applied. Sections were de-waxed and re-hydrated through an ethanol gradient. Antigen retrieval was performed by boiling in citrate buffer (pH 6.0) in a microwave for 15 minutes. Slides were cooled for 30 minutes and endogenous peroxidase activity was blocked with 3% hydrogen peroxide for 15 minutes. Non-specific immunostaining was reduced by applying a blocking solution (Phosphate buffer saline (PBS)/4% normal goat serum (NGS) / 0.1% Triton X-100) for 30 minutes. Sections were then incubated overnight at 4°C with primary antibodies diluted in PBS/NGS/Triton-X 100 buffer. Antibody binding was detected using ABC kits (Vector Laboratories, Inc., Burlingame, CA) and immunostaining visualized using 3, 3’-diaminobenzidine (DAB) chromogen. The number of immunopositive cells/ hpf at ×40 in the mediodorsal and lateral posterior nuclei were averaged over four representative fields to obtain the mean.
Statistical Analysis
Initial analyses looked at the effect of anatomic levels with reactive astrocytes (GFAP), activated microglia/macrophages (CD68), axonal damage (fractin), and oxidative stress (MDA) among PVL cases and controls separately, to determine whether anatomic levels need to be controlled for in all analyses. Analysis of variance (ANOVA) was used to determine if there were any significant means differences with the continuous measures of GFAP density, neuronal density, MDA density, and CD68 density between the anatomic levels. A Fisher’s Exact Test was conducted to examine the association incidence of fractin with anatomic level. There were, however, no significant differences between the levels in any of these variables. An analysis of covariance (ANCOVA) was used to examine the relationship of the continuous measures with case/control status after adjusting for postconceptional age (PCA). Using ANCOVA, least square means (means values adjusted for PCA) for PVL cases and controls were compared. Separate ANCOVA models were constructed adjusting for gestational age and postnatal age. These models are not discussed, as results were similar to PCA models. To test for PCA-adjusted results with fractin and case/control status, logistic regression models were conducted. Analysis of all neuropathologic data was adjusted for postconceptional age.
Results
Clinicopathologic Database
We examined autopsy reports and microscopic slides from 38 cases (22 PVL and 16 controls) autopsied in our pathology department between 1993 and 2007. A comparative analysis of selected clinicopathologic features in PVL compared to control cases revealed that the PVL cases were born significantly earlier (p=0.01) and tended to live a shorter period (p=0.07) than control cases (Table 1). Although there was no difference in the incidence of sepsis or necrotizing enterocolitis between the PVL cases and controls in the total sample, the majority of these two events occurred among PVL cases. Among infants with necrotizing enterocolitis, 86% (6/7) developed PVL compared to 14% (1/7) of the controls (Test of Equal Proportions, p=0.03). Similarly, among infants with sepsis, 88% (7/8) were PVL cases while 13% (1/8) were controls (Test of Equal Proportions, p=0.02).
Table 1.
Clinicopathologic features of PVL cases compared to control cases.
| Feature | PVL (n=22) | Non-PVL (n=16) | P-value* |
|---|---|---|---|
| Gestational Age (mean) | 32.5 ± 4.8 | 36.7 ± 5.2 | 0.01 |
| Postnatal Age (mean) | 4.1 ± 6.6 | 20.0 ± 39.3 | 0.13 |
| Postconceptional Age (mean) | 36.6 ± 6.6 | 56.7 ± 40.9 | 0.07 |
| Male | 46% (10/22) | 69% (11/16) | 0.15 |
| Apgar 5 minutes (mean) | 7.1 ± 2.2 | 6.9 ± 2.6 | 0.85 |
| Congenital Heart Disease | 23% (5/22) | 25% (4/16) | 0.99 |
| Necrotizing Enterocolitis | 27% (6/22) | 6% (1/16) | 0.20 |
| Sepsis | 32% (7/22) | 6% (1/16) | 0.11 |
| Mechanical Ventilation | 84% (16/19) | 66% (10/15) | 0.42 |
| Seizures any time | 23% (5/22) | 6% (1/16) | 0.37 |
T-tests for continuous measures and Chi Square or Fisher’s Exact test for categorical measures were applied. P-value <0.05 was considered significant.
Thalamic Pathology in PVL
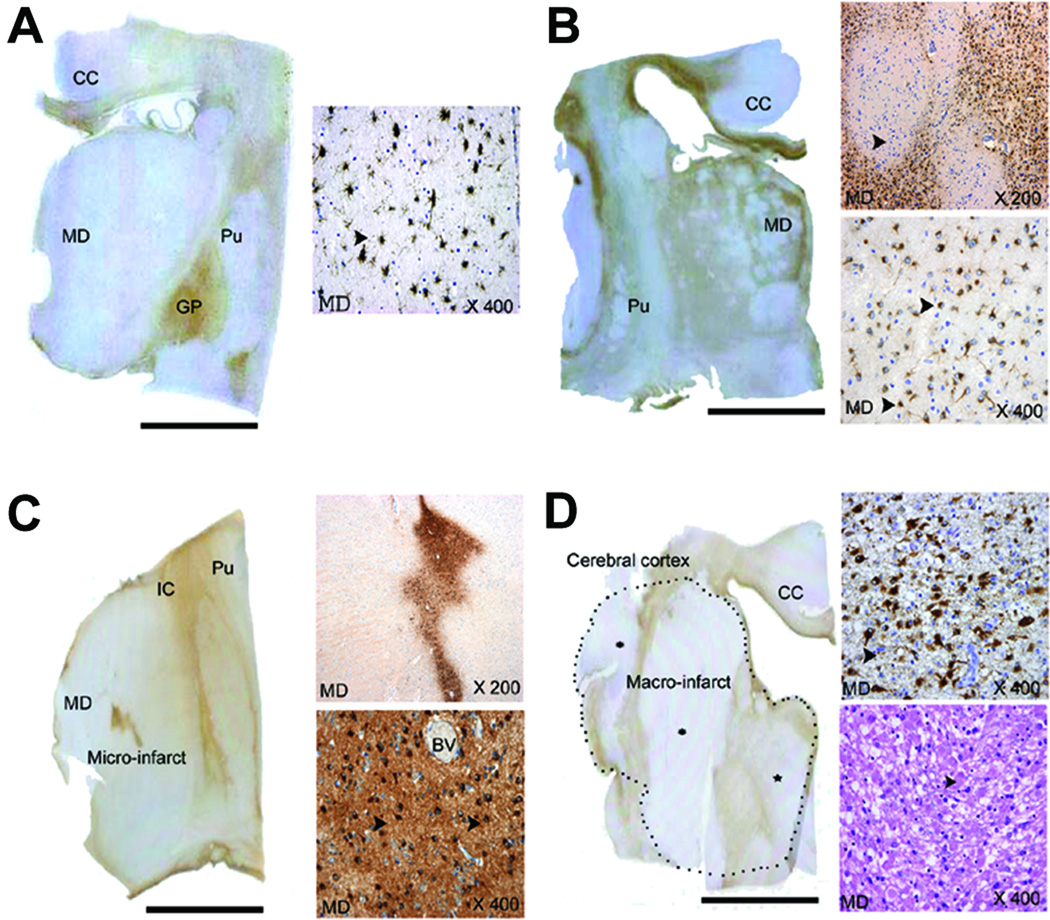
Overall, 59% of the PVL cases demonstrated damage of any type in the thalamus, a significant difference from 19% of control cases (p=0.01) (Table 2). Pattern 0 was defined as no pathologic changes. We recognized four patterns of thalamic histopathology: Pattern 1—diffuse gliosis with or without reduced neuronal density; Pattern 2—status marmoratus, chronic injury characterized by macroscopic linear scarring (“marbling”) and focal islands of profound neuronal loss and gliosis; Pattern 3—micro-infarcts (1–3 mm in diameter) characterized by focal neuronal loss and gliosis embedded in otherwise intact parenchyma; and Pattern 4—macro-infarcts (>5 mm) with extensive necrosis, macrophagocytic infiltration, astrogliosis, and axonal spheroids due to apparent posterior cerebral artery occlusion (Fig. 1). The density of reactive astrocytes was significantly increased in the mediodorsal nucleus in PVL cases (15.7+4.0 reactive astrocytes/hpf) compared to controls (1.7+4.7 reactive astrocytes/hpf) adjusted for postconceptional age (p=0.04), and was marginally increased in the lateral posterior nucleus in PVL cases (18.0+5.5 reactive astrocytes/hpf) compared to controls (0.0+7.1 reactive astrocytes/hpf) (p=0.05). The incidence of gliosis in the mediodorsal nucleus in PVL was 45% (10/22) compared to 13% (2/16) (p=0.04), but was not significantly different between the two groups in the lateral posterior nucleus. The density of activated microglia tended to be increased in PVL (7.0+2.2 CD68 cells/hpf) compared to control cases (2.12+2.5 CD68 cells/hpf)(p=0.16), but was low overall in PVL compared to reactive astrocyte density, indicating that the inflammatory component in thalamic injury in PVL is dominated by reactive astrocytes.
Table 2.
Tabulated incidence of the four patterns of injury in PVL compared to control (non-PVL) cases.
| Finding | PVL Cases (n=22) | Control Cases (n=16) |
|---|---|---|
| Thalamic Pathology* | 59% (13/22) | 19% (3/16) |
| Pattern 1: Diffuse Gliosis | 46% (6/13) | 67% (2/3) |
| Pattern 2: Status Marmoratus | 8% (1/13) | 0% (0/3) |
| Pattern 3: Micro-infarcts | 23% (3/13) | 33% (1/3) |
| Pattern 4: Macro-infarcts | 23% (3/13) | 0% (0/3) |
The difference in the incidence of overall thalamic pathology in the PVL cases compared to controls is significant (p=0.01)
Figure 1.
We observed four patterns of injury in the thalamus (Patterns 1–4) compared to no histopathology (Pattern 0)(not shown). The four patterns are: a. Pattern 1—Diffuse gliosis throughout the thalamus (left-hand whole mount) with arrows indicating reactive astrocytes immunostained with GFAP in the right-hand insert of mediodorsal nucleus at x400; of note, gliosis is striking in the globus pallidus in the left-hand whole mount. b. Pattern 2—Status marmoratus with linear scarring at low magnification (whole mount of tissue section) and islands of profound neuronal loss and gliosis (highlighted with GFAP immunostaining) interspersed with better preserved islands (arrow head, upper right-hand insert) detected microscopically in the mediodorsal and other nuclei at x200; reactive astrocytes immunostained with GFAP are demonstrated in the lower right insert at x400. Gliosis in the internal capsule, corpus callosum, and deep white matter are associated with the thalamic damage in the left-hand whole mount. c. Pattern 3—Micro-infarcts detected with GFAP immunostaining at low and high magnification and characterized by severe reactive gliosis (and neuronal loss) embedded in an otherwise intact parenchyma in the left-hand whole mount and in right hand inserts at x200 and x400; the sections are immunostained with GFAP; and d. Pattern 4—Macro-infarcts: here the dotted outline in the left-hand whole mount defines the outer boundary of the macro-infarct, and includes the dorsal thalamus, internal capsule, and insular cortex, i.e., regions in the distribution of the posterior and middle cerebral artery; the infarct in the mediodorsal nucleus in the right-hand inserts is characterized by reactive astrocytes (x400, upper right-hand insert, GFAP immunostaining), macrophagocytic infiltration, and axonal spheroids (lower right-hand insert, hematoxylin-and-eosin). Abbreviations: BV, blood vessels; CC, corpus callosum; GP, globus pallidus; IC, internal capsule; MD, mediodorsal nucleus; Pu, putamen. Scale bar=1 centimeter.
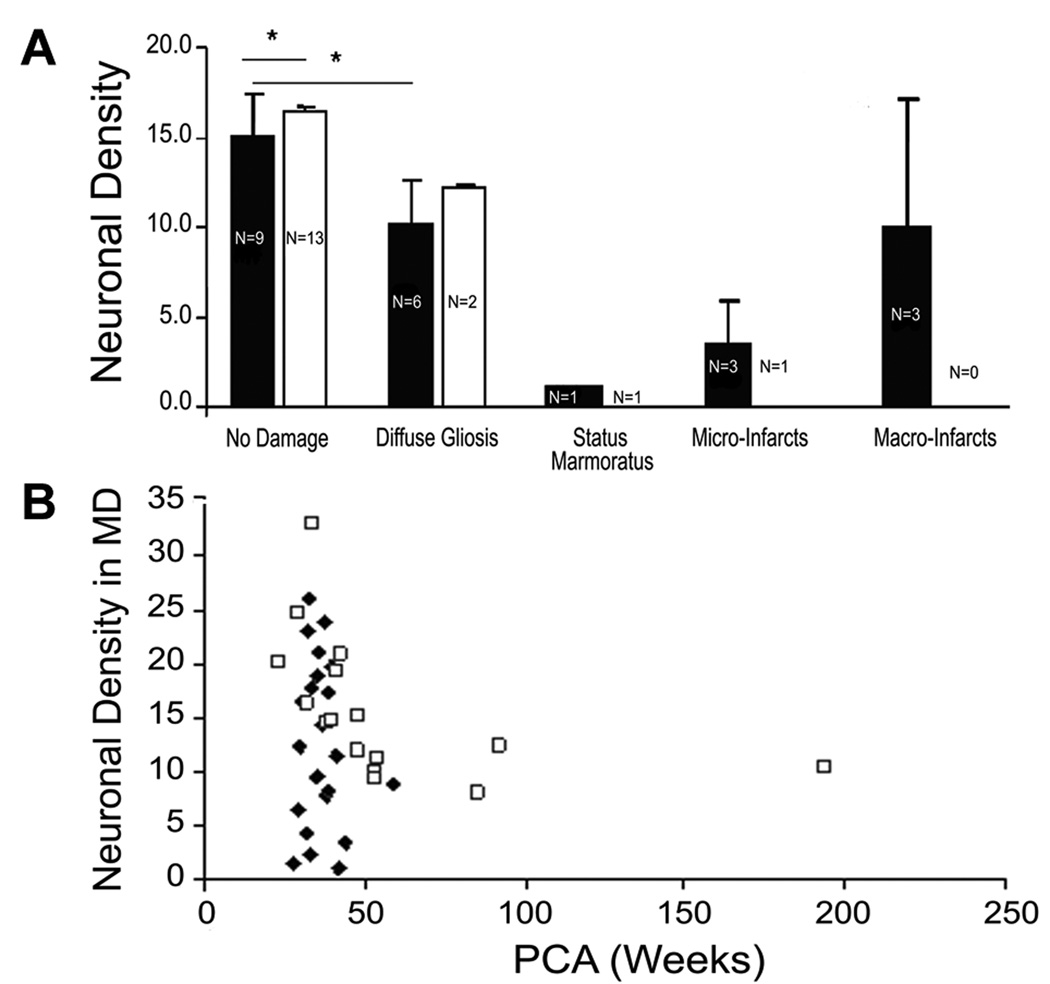
Each pattern of thalamic damage in PVL compared to controls was associated with reduced neuronal densities (Fig. 2), with a significant reduction in the mediodorsal nucleus in PVL cases without gliosis (Pattern 0) (14.3+2.4 neurons/hpf) compared to control cases without gliosis (Pattern 0) (17.2+2.0 neurons/hpf) (p<0.05). There was also a significant difference in neuronal density in the mediodorsal nucleus between Pattern 0 and Pattern 1 in PVL cases (p=0.001) but not controls (p=0.37). The combined neuronal and reactive astrocyte data suggest that susceptibility to injury may preferentially involve the medial tier compared to the lateral tier of thalamic nuclei but is nevertheless present in both regions. The most profound cellular injury in the mediodorsal nucleus appeared to involve axons, with a highly significant increase in the incidence of axonal damage in the PVL (55%; 12/22) compared to control cases (6.3%; 1/16)(p=0.002). Eighty-two percent of the PVL cases (18/22) had histopathologic changes in the reticular nucleus compared to 44% (7/16) of the control cases (p=0.01), with moderate and severe damage in 41% (7/17) of the PVL cases compared to none of the 16 controls. The analysis of the oxidative marker MDA unexpectedly revealed no difference in the density of MDA-immunopositive neurons or percent of MDA-immunopositive neurons relative to all neurons between PVL and control cases. Yet, the graphic depiction of the density of reactive astrocytes versus MDA-immunostained neuronal density (Fig. 3) suggests that lipid peroxidation and MDA-adduct formation represent very early neuronal injury with MDA protein adducts either being degraded or destabilized prior to the onset of gliosis.
Figure 2.
A. Neuronal density in the four patterns of injury (Patterns 1–4) in PVL and control cases compared to the neuronal density in PVL and control cases without histopathologic changes (Pattern 0) in the mediodorsal nucleus. The neuronal density in Pattern 0 and Pattern 1 is presented as the mean adjusted for postconceptional age. There was significantly reduced neuronal density in the PVL cases compared to controls (p<0.05) in Pattern 0 in the mediodorsal nucleus, but not in the lateral posterior nucleus (data not shown). There was also a significant difference in neuronal density in the mediodorsal nucleus between Pattern 0 and Pattern 1 in PVL cases (p=0.001) but not controls (p=0.37). Neuronal density was markedly reduced in status marmoratus, micro-infarcts within infarct itself), and macro-infarcts. PVL, ■; Control, □. B. In PVL cases without status marmoratus or micro- or macro-infarcts, the neuronal density tended to decrease with increasing postconceptional age in both PVL and control cases in the mediodorsal nucleus, with a marginal difference in the mean density adjusted for postconceptional age in the PVL cases (11.9±1.6 neurons/mm2) compared to controls (16.7 neurons/mm2) (p=0.07). PVL, ◆; Control, □
Figure 3.
The relationship of reactive astrocyte (GFAP-positive) density to MDA-immunopositive neuronal density. As the density of reactive astrocyte increases, the density of MDA-positive neurons decreases, suggesting that MDA expression is an early marker of neuronal injury (see text). PVL,◆; Control, □
A comparative analysis between the PVL cases without gliosis (Pattern 0, n=6) and with gliosis (Pattern 1, n=9) revealed that there was no difference in the mean gestational age between the two groups (31.8+5.8 weeks versus 32.1+4.4 weeks); both groups on average were born very preterm (<34 weeks)(Table 3). The Apgar score at 5 minutes was significantly lower in Pattern 1 (4.0+2.6) compared to Pattern 0 (7.8+0.8) (p=0.02)(Table 2). In addition, the incidence of seizures of any type were significantly higher in Pattern 1 (50%; 3/6) compared to Pattern 0 (0%; 0/9) (p=0.04).
Table 3.
Clinicopathologic features in Pattern 0 (no pathology) compared to Pattern 1 (diffuse gliosis) in the PVL cases.
| Feature | Pattern=1 (n=6) | Pattern=0 (n=9) | P-value* |
|---|---|---|---|
| Gestational Age (mean) | 31.8 ± 5.8 | 32.1 ± 4.4 | 0.89 |
| Postnatal Age (mean) | 7.8 ± 11.9 | 1.8 ± 1.5 | 0.28 |
| Postconceptional Age (mean) | 39.5 ± 10.5 | 33.9 ± 3.8 | 0.26 |
| Male | 67% (4/6) | 44% (4/9) | 0.61 |
| Apgar 5 minutes (mean) | 4.0 ± 2.6 | 7.8 ± 0.8 | 0.02 |
| Percent ≤34 weeks | 50% (3/6) | 78% (7/9) | 0.33 |
| Congenital. Heart Disease | 16.7% (1/6) | 22.2% (2/9) | 0.99 |
| Necrotizing Enterocolitis | 16.7% (1/6) | 33.3% (3/9) | 0.60 |
| Sepsis | 50.0% (3/6) | 22.2% (2/9) | 0.33 |
| Mechanical Ventilation | 100% (5/5) | 63% (5/8) | 0.23 |
| Seizures any time | 50% (3/6) | 0% (0/9) | 0.04 |
T-tests for continuous measures and Fisher’s Exact test for categorical measures were applied. P-value <0.05 was considered significant.
Discussion
The major finding in this autopsy study is that thalamic damage occurs in approximately 60% of infants with PVL dying in early life. This incidence is greater than that of thalamic abnormalities demonstrated by neuroimaging in 50% of preterm survivors with PVL (18–20) and in 25% of term infants with neonatal encephalopathy (21). Thus, neuroimaging studies may underestimate the magnitude of the problem and hence the potential major role of the thalamus in long-term cognitive deficits of survivors of perinatal disorders. We recognized four patterns of injury, which we label as diffuse gliosis, status marmaratous, micro-infarcts, and macro-infarcts. Irrespective of the pattern and/or mechanism, we found that neuronal loss appears to be the neuropathologic substrate of reduced thalamic volumes revealed by neuroimaging. In the following discussion, we highlight issues relevant to the major findings of this study.
Clinicopathologic Database
In this autopsy series, we examined the incidence of major clinicopathologic features that have been shown to be relevant to the pathogenesis of PVL in published studies (7–9). We found that the infants with PVL were born preterm and approximately 4 weeks earlier than the typically term non-PVL infants; moreover, the PVL cases tended to live approximately two weeks less than non-PVL cases. This observation reflects our autopsy service in which PVL is common in the preterm infants and occurs in the majority of preterm cases autopsied. To account for the differences in gestational and postnatal ages, we analyze means adjusted for postconceptional age. We found that the majority of cases of sepsis and necrotizing enterocolitis occurred in the PVL cases. This finding was not unanticipated since both are conditions that have been associated with PVL clinically (7). The association of thalamic damage with PVL in the majority of cases (59%) suggests that common mechanisms underlie co-existent gray and white matter injury, e.g., hypoxia-ischemia, excitotoxicity, free radical injury, infection, and cytokine toxicity (7–9). Nevertheless, we also identified thalamic damage in 19% of non-PVL cases, indicating potentially distinct mechanisms from PVL as well.
Thalamic Gliosis (Pattern 1) Associated with PVL
The major pattern of thalamic damage is diffuse gliosis (Pattern 1) associated with variable degrees of neuronal loss, microglial activation and axonal damage. Histopathologic examination of human tissue sections at autopsy, i.e., at one “stationary” time-point, obviously does not reveal the temporal sequences of cellular insults. Nevertheless, the thalamic damage in Pattern 1 may be potentially indicative of primary diffuse insults to vulnerable neurons. Of note, hypoxic-ischemic injury in a perinatal rat model demonstrates virtually isolated injury in the reticular nucleus (22), i.e., the nucleus with substantial involvement in the PVL cases reported here. Yet, secondary neuronal loss and gliosis may also result in this pattern from trans-synaptic degeneration from damaged cortical neurons, subplate neurons, and/or axons coursing through the cerebral white matter in PVL (14, 15, 22–24). The underpopulation of thalamic neurons in PVL may also result from “bystander” injury to GABAergic neurons which migrate through the white matter between 15 and 34 gestational weeks from the ganglionic eminence to provide GABAergic neurons to the thalamic association nuclei (25), including the mediodorsal nucleus, and likely the reticular nucleus that is comprised predominately of GABAergic neurons (12).
The cause(s) of thalamic gliosis is unknown but the histopathology is consistent with hypoxic-ischemic injury. A comparative analysis between the PVL cases without gliosis (Pattern 0, n=6) and with gliosis (Pattern 1, n=9) was performed in an effort to gain insight in the pathogenesis. This analysis revealed that there was no difference in the mean gestational age between the two groups; both groups on average were born very preterm (<34 weeks). Yet, the Apgar score at 5 minutes was on average less than 5 and significantly lower in Pattern 1 compared to Pattern 0, suggesting the possibility that perinatal asphyxia is involved, at least in part, in the pathogenesis of diffuse thalamic gliosis in PVL. Of note, the incidence of seizures of any type is approximately 50% in Pattern 1 compared to none in Pattern 0, suggesting a potential clinical correlate of diffuse thalamic gliosis in preterm infants with PVL that requires further study.
Other Patterns of Thalamic Damage in PVL
In addition to diffuse thalamic gliosis, the patterns of thalamic damage in PVL include status marmoratus (probable nonspecific end-stage damage), small vessel embolism (micro-infarcts), and large vessel thrombo-embolic occlusions (macro-infarcts), the latter two lesions occurring predominately in pre- or full-term infants with ganglionic eminence hemorrhages or congenital heart disease with cardiopulmonary bypass or extra-corporal membrane oxygenation. Clearly, no single insult accounts for all thalamic damage in PVL and no single experimental paradigm can model its complex spectrum.
Potential Clinicopathologic Correlations
Thalamic damage in PVL involves multiple nuclei, suggesting that it contributes to a complex constellation of neurobehavioral abnormalities, given that the thalamus is involved in virtually all brain functions. Indeed, multifaceted cognitive and social abnormalities are associated with generalized thalamic volume abnormalities detected by MRI/proton spectroscopy in idiopathic autism (26, 27), of particular interest as approximately 16% of autistic children are born prematurely (28). Still, the specific involvement of the mediodorsal nucleus and reticular nucleus found in this study is particularly relevant to the deficits in working memory and attention, respectively, that are common in long-term survivors of prematurity (2–6). Working memory involves the retrieval and holding of relevant information in mind long enough to perform a task with sequential parts (2–6); it is dependent upon the reciprocal connections between the mediodorsal nucleus and prefrontal lobe (11). Human mediodorsal pathology has been reported in schizophrenia (29), depression (30), and frontal lobe syndromes due to thiamine deficiency (11) and paramedian infarcts (11, 31) with memory loss, inappropriate social responses, and impaired judgment. By analogy to these disorders, the long-term neurobehavioral abnormalities in PVL may reflect in part dysfunction of the frontal and limbic connections of the mediodorsal nucleus, and potentially mimic adult frontal lobe syndromes in the developing child. In a series of preterm infants studied at two years, abnormal working memory is associated with bilateral reductions in the prefrontal and other cortices; yet, the possibility of trans-synaptic neuronal loss in the prefrontal cortex secondary to mediodorsal injury was not excluded (3). Attention, likewise essential for problem solving is the preferential focus upon relevant events (11). Its neuroanatomic substrate involves several cortical networks with subcortical components, including the mediodorsal nucleus (11). Yet, attention also depends upon overall wakefulness which is mediated in large part by the reticular nucleus, i.e., the key regulator of the ascending reticular activating pathways that exert a global influence upon attentional modulation without selectivity for any one sensory modality or cognitive domain (11). No specific syndrome or histopathology has been related to the human reticular nucleus. Nevertheless, its damage in PVL could interfere with the proper functioning of the reticular activating system and give rise to domain-independent attentional deficits. This study emphasizes the need for continued research into the thalamus’ role in cognitive deficits in infants with PVL.
Acknowledgments
The authors thank Mr. Richard A. Belliveau and Dr. Felicia L. Trachtenberg for assistance in this study.
Financial Support: This research was supported by grants from the National Institute of Neurological Diseases and Stroke (PO1-NS38475) (H.C.K., J.J.V.), Hearst Foundation (R.L.H.), and National Institute of Child Health and Development (Children’s Hospital Developmental Disabilities Research Center) (P30-HD18655).
Abbreviations
- GFAP
glial fibrillary acidic protein
- MDA
malondialdehyde
- PVL
Periventricular leukomalacia
Footnotes
Pediatric Research Articles Ahead of Print contains articles in unedited manuscript form that have been peer-reviewed and accepted for publication. As a service to our readers, we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting and review of the resulting proof before it is published in its final definitive form. Please note that during the production process errors may be discovered, which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Marlow N, Wolke D, Bracewell M, Samara M. Neurologic and developmental disability at six years after extremely preterm birth. N Engl J Med. 2005;352:9–19. doi: 10.1056/NEJMoa041367. [DOI] [PubMed] [Google Scholar]
- 2.Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ. Cognitive and behavioural outcomes of school-aged children who were born preterm: a meta-analysis. JAMA. 2002;288:728–737. doi: 10.1001/jama.288.6.728. [DOI] [PubMed] [Google Scholar]
- 3.Woodward LJ, Edgin JO, Thompson D, Inder TE. Object working memory deficits predicted by early brain injury and development in the preterm infant. Brain. 2005;128:2578–2587. doi: 10.1093/brain/awh618. [DOI] [PubMed] [Google Scholar]
- 4.Bayless S, Stevenson J. Executive functions in school-age children born very prematurely. Early Hum Dev. 2007;83:247–254. doi: 10.1016/j.earlhumdev.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 5.Böhm B, Smedler A-C, Forssberg H. impulse control, working memory and other executive functions in preterm children when starting school. Acta Paediatr. 2004;93:1363–1371. doi: 10.1080/08035250410021379. [DOI] [PubMed] [Google Scholar]
- 6.Lou HC. Etiology and pathogenesis of Attention-deficit Hyperactivity Disorders (ADHD): significance of prematurity and perinatal hypoxic-hemodynamic encephalopathy. Acta Paediatr. 1996;85:1266–1271. doi: 10.1111/j.1651-2227.1996.tb13909.x. [DOI] [PubMed] [Google Scholar]
- 7.Volpe JJ. Neurology of the Newborn. 5th Ed. Philadelphia: Elsevier Science; 2008. [Google Scholar]
- 8.Kinney HC, Haynes RL, Folkerth RD. White Matter Disorders in the Perinatal Period. In: Golden JA, Harding BN, editors. Pathology and Genetics: Acquired and Inherited Diseases of the Developing Nervous System. Basel: ISN Neuropathology Press; 2004. pp. 156–170. [Google Scholar]
- 9.Kinney HC, Armstrong DD. Perinatal Neuropathology. In: Graham DI, Lantos PL, editors. Greenfield’s Neuropathology. 7th edition. Vol. 1. London: Arnold; 2002. pp. 519–606. [Google Scholar]
- 10.Billiards SS, Haynes RL, Folkerth RD, Borenstein NS, Trachtenberg FL, Rowitch DH, Ligon KL, Volpe JJ, Kinney HC. Myelin abnormalities without oligodendrocyte loss in periventricular leukomalacia. Brain Pathol. 2008;18:153–163. doi: 10.1111/j.1750-3639.2007.00107.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mesulam MM. Principles of Behavioral and Cognitive Neurology. New York: Oxford University Press; 2000. pp. 1–120. [Google Scholar]
- 12.Jones EG. Thalamic circuitry and thalamocortical synchrony. Philos Trans R Soc Lond B Biol Sci. 2002;357:1659–1663. doi: 10.1098/rstb.2002.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kinney HC, Korein J, Panigrahy A, Dikkes P, Goode R. Neuropathologic findings in the brain of Karen Ann Quinlan: The role of the thalamus in the persistent vegetative state. N Engl J Med. 1994;330:1469–1475. doi: 10.1056/NEJM199405263302101. [DOI] [PubMed] [Google Scholar]
- 14.Pierson CR, Folkerth RD, Trachtenberg FL, Drinkwater ME, Volpe JJ, Kinney HC. Gray matter damage is associated with periventricular leukomalacia. Acta Neuropathol. 2007;114:619–631. doi: 10.1007/s00401-007-0295-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haynes RL, Billiards SS, Borenstein NS, Volpe JJ, Kinney HC. Diffuse axonal injury in periventricular leukomalacia as determined by pan-apoptotic marker fractin. Pediatr Res. 2008;63:656–661. doi: 10.1203/PDR.0b013e31816c825c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Esterbauer H, Schaur RJ, Zollner H. Chemistry and biochemistry of 4-hydroxynonenal, malonaldehyde and related aldehydes. Free Radic Biol Med. 1991;11:81–128. doi: 10.1016/0891-5849(91)90192-6. [DOI] [PubMed] [Google Scholar]
- 17.DeArmond SJ, Fusco MM, Dewey MM. Structure of the Human Brain: A Photographic Atlas. 3rd Ed. New York: Oxford University Press; 1989. [Google Scholar]
- 18.Ricci D, Anker S, Cowan F, Pane M, Gallini F, Luciano R, Donvito V, Baranellow G, Gesarini L, Bianco F, Rutherford M, Romagnoli C, Alkinson J, Braddick O, Guzzella F, Mercuri E. Thalamic atrophy in infants with PVL and cerebral visual impairment. Early Hum Dev. 2006;82:591–595. doi: 10.1016/j.earlhumdev.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 19.Yokochi K. Thalamic lesions revealed by MR associated with PVL and clinical profile of subjects. Acta Paediatr. 1997;86:493–496. doi: 10.1111/j.1651-2227.1997.tb08919.x. [DOI] [PubMed] [Google Scholar]
- 20.Giménez M, Junqué C, Narberhaus A, Botet F, Bargallo N, Mercader JM. Correlations of thalamic reductions with verbal fluency impairment in those born prematurely. Neuroreport. 2006;17:463–466. doi: 10.1097/01.wnr.0000209008.93846.24. [DOI] [PubMed] [Google Scholar]
- 21.Miller SP, Ramaswamy V, Michelson D, Barkovich AJ, Holshouser B, Wycliffe N, Glidden DV, Deming D, Partridge JC, Wu YW, Ashwal S, Ferriero DM. Patterns of brain injury in term encephalopathy. J Pediatr. 2005;146:453–460. doi: 10.1016/j.jpeds.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 22.McQuillen PS, Sheldon A, Shatz CJ, Ferriero DM. Selective vulnerability of subplate neurons after early hypoxia-ischemia. J Neurosci. 2003;23:3308–3315. doi: 10.1523/JNEUROSCI.23-08-03308.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghosh A, Shatz CJ. A role for subplate neurons in the patterning of connections from thalamus to neocortex. Development. 1993;117:1031–1047. doi: 10.1242/dev.117.3.1031. [DOI] [PubMed] [Google Scholar]
- 24.Northington FJ, Ferriero DM, Martin LJ. Neurodegeneration in the thalamus following neonatal hypoxia-ischemia is programmed cell death. Dev Neurosci. 2001;23:186–191. doi: 10.1159/000046141. [DOI] [PubMed] [Google Scholar]
- 25.Letinic K, Rakic P. Telencephalic origin of human thalamic GABAergic neurons. Nat Neurosci. 2001;4:931–936. doi: 10.1038/nn0901-931. [DOI] [PubMed] [Google Scholar]
- 26.Tsatsanis KD, Rourke BP, Klin A, Volkmar FR, Cicchetti D, Schultz RT. Reduced thalamic volume in high-functioning individuals with autism. Biol Psychiatry. 2003;53:121–129. doi: 10.1016/s0006-3223(02)01530-5. [DOI] [PubMed] [Google Scholar]
- 27.Hardan AY, Minshew NJ, Melhem NM, Srihari S, Jo B, Bansal R, Keshavan MS, Stanley JA. An MRI and proton spectroscopy study of the thalamus in children with autism. Psychiatry Res. 2008;163:97–105. doi: 10.1016/j.pscychresns.2007.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brimacombe M, Ming X, Lamendola M. Prenatal and birth complications in autism. Matern Child Health J. 2007;11:73–79. doi: 10.1007/s10995-006-0142-7. [DOI] [PubMed] [Google Scholar]
- 29.Popken GJ, Bunney WE, Jr, Potkin SG, Jones EG. Subnucleus-specific loss of neurons in medial thalamus of schizophrenics. Proc Natl Acad Sci USA. 2000;97:9276–9280. doi: 10.1073/pnas.150243397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Young KA, Holcomb LA, Yazdani U, Hicks PB, German DE. Elevated neuronal number in the limbic thalamus in major depression. Am J Psychiatry. 2004;161:1270–1277. doi: 10.1176/appi.ajp.161.7.1270. [DOI] [PubMed] [Google Scholar]
- 31.Weidauer S, Nichtweiss M, Zanell FE, Lanfermann H. Assessment of paramedian thalamic infarcts: MR imaging, clinical features and prognosis. Eur Radiol. 2004;14:1615–1626. doi: 10.1007/s00330-004-2303-7. [DOI] [PubMed] [Google Scholar]