Abstract
Although neighborhood disadvantage has been linked to the development of cardiovascular disease, the mechanism through which living in impoverished neighborhoods is associated with poor cardiovascular health is not well understood. Additionally, it is not clear whether individual socioeconomic status (SES) interacts with neighborhood factors to influence cardiovascular outcomes. Using multilevel modeling, we examined the interaction between neighborhood poverty and individual SES on pressor responses to an alpha agonist, Phenylephrine (PE), in an adult sample of 105 African-Americans and 106 Caucasian-Americans. Neighborhood poverty was assessed using census block data gathered from the Census Bureau. Education and occupation were used to assess individual SES. Pressor responsiveness was calculated as the systolic and diastolic blood pressure (BP) response to a 100-microgram PE bolus administered intravenously. There was a significant interaction between education and neighborhood poverty on pressor responses. Higher education was associated with smaller BP responses to PE; but only in individuals who lived in neighborhoods in which less than 5% of the residents lived below the poverty line. Occupation was unrelated to pressor responses to PE. These results suggest that neighborhood characteristics play an important role in cardiovascular functioning.
Keywords: blood pressure, ethnicity, socioeconomic status, pressor sensitivity, neighborhood poverty, education, occupation
Introduction
Neighborhood disadvantage has been linked to the development of cardiovascular disease. There is a higher incidence of cardiovascular disease (CVD) in lower SES individuals compared to higher SES individuals (Singh & Siahpush, 2002). Additionally, neighborhood poverty is associated with more CVD risk factors, such as diabetes, tobacco smoking, and obesity (Chen & Paterson, 2006; Cubbin, Hadden, & Winkleby, 2001). Epidemiological studies using census data reveal higher rates of hypertension and stroke among individuals who live in low SES neighborhoods (Anand et al., 2007; Bravata et al., 2005; Loucks, Rehkopf, Thurston, & Kawachi, 2007; McClellan, 2005; Nzerue, Demissochew, & Tucker, 2002). Additionally, recent evidence suggests that neighborhood disadvantage is associated with carotid artery atherosclerosis in untreated hypertensives (Petersen et al., 2006).
Living in disadvantaged communities may be associated with poor health due to poor neighborhood safety and lack of resources within the community to support healthy lifestyles. Compared to affluent neighborhoods, poor neighborhoods are more likely to have higher crime rates (Sundquist et al., 2006), lack of access to healthy foods (Echeverria, Diez-Roux, & Link, 2004; Krummel et al., 2001; Morland, Diez Roux, & Wing, 2006), limited recreation and environments that discourage physical activity (Echeverria et al., 2004), as well as lack of access to health care and health information (Blair, Lloyd-Williams, & Mair, 2002). These characteristics may contribute to the higher rates of CVD among those who live in low SES neighborhoods.
It is clear that living in impoverished neighborhoods is associated with increased cardiovascular morbidity (Anand et al., 2007; Cozier et al., 2007). However, the mechanism through which this occurs is not well understood. Few studies have examined whether individuals who live in more impoverished neighborhoods have greater blood pressure responsiveness than those who live in wealthier neighborhoods, and among those studies conducted in this area the findings have been mixed, with some researchers finding more reactivity among those who live in low SES neighborhoods (Kapuku, Treiber, & Davis, 2002) and others not finding such as association (Suchday, Krantz, & Gottdiener, 2005). Given that research suggests blood pressure reactivity predicts the future development of hypertension in normotensive individuals (Flaa, Eide, Kjeldsen, & Rostrup, 2008; Williams, 2006), more research is needed to understand the relationship between neighborhood SES and vascular reactivity, as a potential mechanism leading to higher CVD among those living in impoverished neighborhoods.
One way of examining vascular reactivity is to measure blood pressure (BP) after infusing a standard dose of Phenylephrine (PE), a drug that stimulates the same vasoconstricting α receptors that Norepinephrine does. Similar to other laboratory tests of vascular reactivity, research consistently demonstrates that α agonists such as PE lead to a transient increase in BP that mimics the effects of short term stress (Dimsdale, Graham, Ziegler, Zusman, & Berry, 1987; Sherwood & Hinderliter, 1993; Stein, Lang, Singh, He, & Wood, 2000). Although PE infusions lead to increases in BP, the magnitude of this effect is influenced by demographic factors, such as hypertension status, age, gender, and ethnicity (Dimsdale et al., 1987; Elliott, Sumner, McLean, & Reid, 1982; Sherwood & Hinderliter, 1993). In this study, we examine whether SES also influences BP responses to PE.
Evidence suggests that neighborhood poverty may interact with individual-level SES and ethnicity to influence health. For instance, the effect of neighborhood poverty on self-reported health status is worst among those with lower individual income (Kobetz, Daniel, & Earp, 2003). Additionally, there is a higher mortality rate among African Americans living in impoverished neighborhoods than among Caucasian Americans in impoverished neighborhoods (Subramanian, Chen, Rehkopf, Waterman, & Krieger, 2005). Exploring interactions between neighborhood poverty and individual-level factors on vascular reactivity is a critical next step in obtaining a complete picture of the process through which socioeconomic factors influence cardiovascular health. In particular, it is unclear whether individual socioeconomic factors, such as educational attainment or occupation, can buffer the effect of neighborhood poverty on vascular reactivity. This question is especially important for African Americans, an ethnic group that is more likely to live in lower SES neighborhoods than their Caucasian American counterparts with similar income and education levels (Iceland, Sharpe, & Steinmetz, 2005).
Skills and social benefits associated with increasing occupation and education levels, such as greater access to health information, a greater sense of control, and socialization to adopt health-promoting behaviors (Yen & Moss, 1999) may have positive cardiovascular effects. Thus, it is possible that African Americans in higher educational brackets may adapt a healthier lifestyle, through increased physical activity and engaging in healthier eating habits. This may serve as a protective factor against the negative effects of living in socioeconomically disadvantaged neighborhoods on cardiovascular functioning.
To date, no published study has examined the interaction between neighborhood SES and individual level factors on vascular reactivity in adult participants. However, a study conducted with African American adolescents revealed that although African American youth who lived in poorer neighborhoods had higher BP reactivity to a video game challenge, this effect was buffered by individual-level SES, such that those whose parents had a higher education or income had lower BP reactivity (Wilson, Kliewer, Plybon, & Sica, 2000). This suggests that individual level SES may buffer the effects of neighborhood poverty on vascular reactivity. The current study extends this work by examining whether neighborhood poverty interacts with individual-level factors to predict pressor responses to PE in an adult sample.
Individual-level factors examined in this study included education, occupation, and ethnicity (African American, Caucasian American). We predicted that individual socioeconomic factors would interact with neighborhood poverty to predict pressor responses to PE. Specifically, we expected that pressor responses to PE would be greatest for participants who had low individual SES and lived in neighborhoods with higher poverty levels; whereas, high individual SES would buffer the effects of neighborhood poverty on pressor responses. We also examined the 3 way interaction between ethnicity, neighborhood poverty, and individual SES. We expected that the protective effect of high individual SES on those who live in neighborhoods with more poverty would be strongest for African Americans, given that they are more likely to live in lower SES neighborhoods.
Methods
Participants
Participants for the current study included 211 employed individuals who participated in two protocols of research on stress, ethnicity, and BP (1995–1999 and 2000–2004; see Table 2 for differences in sample characteristics between the two protocols). There were 105 African-Americans and 106 Caucasian-Americans. The sample consisted of 117 males and 94 females. Participants were recruited from the San Diego community via advertisement and referrals. Participants were between the ages of 25 and 52 (Mean=37.6, SEM=0.50), with an ideal body weight between 90% and 130% (MetropolitanLifeFoundation, 1983) and resting BP<180/110 mm Hg at screening. Screening BP was defined as the average of 3 seated BP’s. Women were excluded if postmenopausal, diagnosed with premenstrual syndrome, taking oral contraceptives, or pregnant. Individuals with major medical conditions other than hypertension or with a psychiatric disorder were excluded from the study. Screening BP was taken using Dinamap model 1846-SZ with appropriate size cuffs. Participants whose systolic BP was above 140 mmHg and/or whose diastolic BP was above 90 mmHg were considered hypertensive. Concerning BP status, 50 of the participants were hypertensive (32 African-Americans, 18 Caucasian-Americans) and 160 were normotensive. No patients were taking antihypertensive medications.
Table 2.
Differences in Sample Characteristics Between the 2 Protocols
| Variable | 1995–1999 Protocol (N=62) | 2000–2004 Protocol (N=149) |
|---|---|---|
| Ethnicity | ||
| African-American | 39 (62.9%) | 66 (44.3%) |
| Caucasian-American | 23 (37.1%) | 83 (55.7%) |
| Education2 | ||
| BA and Above | 6 (10%) | 64 (43.5%) |
| Partial College | 23 (38.3%) | 42 (28.6%) |
| High School Graduate | 25 (41.7%) | 36 (24.5%) |
| Partial High School | 6 (10%) | 5 (3.4%) |
| % of Individuals in Block Identified as Black2 | 16.4% (SEM=2.2%) | 8.7% (SEM=.87%) |
| % of Individuals in Block Living Below Poverty Level1 | 22.2% (SEM=1.9%) | 16.0% (SEM=.91%) |
| Hypertensive1 | 22 (35.5%) | 28 (18.9%) |
| Gender | ||
| Men | 41 (66.1%) | 76 (51.0%) |
| Women | 21 (33.9%) | 73 (49.0%) |
| M±SEM | M±SEM | |
| Age | 39.2 ± 0.7 | 36.9 ± 0.6 |
| BMI2 | 26.6 ± 0.5 | 26.9 ± 0.5 |
| Baseline SBP (mmHg)1 | 130.0 ± 2.4 | 126.4 ± 1.2 |
| Baseline DBP | 78.6 ± 1.6 | 75.4 ± .8 |
| Occupational Status | 2.27 ± 0.20 | 4.16 ± 0.14 |
| SBP Pressor Change (mmHg)2 | 33.1 ± 2.5 | 28.1 ± 0.9 |
| DBP Pressor Change (mmHg)2 | 21.7 ± 1.5 | 16.9 ± 0.6 |
| Per Capita Income in Block2 | $17,398 ± $1019 | $23,718 ± $790 |
p<.05
p<.01
Socioecomonic Status
Individual-Level SES
Individual SES was measured using education and the occupation factor of the Hollingshead two factor index of social position (Hollingshead, 1958a).. Education was measured on a 5 point scale, with responses ranging from 1 (partial high school) to 5 (graduate degree). Scores on the occupation factor ranged from 1–7, with higher scores representing higher social status occupations. A ranking of 7 was given to someone whose reported occupation is classified as a higher executive or major professional, such as a bank president or a judge. In contrast, a ranking of 1 was given to someone whose reported occupation is classified as an unskilled employee such as a janitor or factory worker. Validation studies support the utility of the Hollingshead scale as a reliable and valid measure of social status (Hollingshead, 1958a).
Neighborhood Demographic Characteristics
Census block data were gathered from the Census Bureau American Fact Finder Census 2000 datasets (2000, 2001; Census, 2001) and used to characterize neighborhood SES. Census block, which is a subdivision of a census tract, is the smallest geographic unit created by the Census Bureau and enables researchers to determine neighborhood SES with greater precision than using zip code data alone. Percentage of individuals living below the poverty line in the census block was used to determine neighborhood SES. Poverty statistics were calculated by the Census Bureau using a weighted average threshold which is based on family income and the number of individuals in the household. In a single person household, income levels below $8,501 were considered below the poverty line. Using information collected from each household, the Census Bureau calculates the percentage of households in each census block living below the poverty line.
Pressor Sensitivity
Data from baroreflex testing was used to assess pressor sensitivity. During baroreflex testing, a Finapres BP cuff (Ohmeda, 2300) was used to measure BP signals which were relayed to an A/D converter (Data Translation, DT2801), sampling at 1 kHz per channel (Global laboratory software, Data Translation) and stored in an IBM PC compatible computer in 3-minute epochs. The Finapres BP cuff was placed on the third or fourth digit of the hand opposite the venous injection site. Hand position and cuff location were adjusted so that the Finapres readings were within 5 mmHg of casual BP determinations.
The participants were tested for their response to PE in the UCSD General Clinical Research Center in the afternoon. After resting supine for at least twenty minutes, baseline data were collected over the last three minutes of the twenty minute resting period. Immediately following baseline, a 100 μg PE bolus was administered intravenously. Pressor sensitivity was assessed by recording the changes in BP in response to PE and was calculated as peak level BP in response to PE dosage minus baseline BP.
Statistical Analysis
Group Comparisons
Independent samples t-tests were conducted to examine differences in sample characteristics between African Americans and Caucasian Americans (see Table 1) as well as between the 1996–1999 and 2000–2004 protocols (see Table 2).
Table 1.
Ethnic Differences in Sample Characteristics in the Total Sample
| Variable | African-Americans (N=105) | Caucasian-Americans (N=106) |
|---|---|---|
| Education2 | ||
| BA and Above | 24 (23.1%) | 46 (44.7%) |
| Partial College | 36 (34.6%) | 29 (28.2%) |
| High School Graduate | 34 (32.7%) | 27 (26.2%) |
| Partial High School | 10 (9.6%) | 1 (1.0%) |
| % of Individuals in Block Identified as Black2 | 16.35% (SEM=1.6%) | 6.0% (SEM=.84%) |
| % of Individuals in Block Living Below Poverty Level1 | 19.9% (SEM=1.3%) | 15.8% (SEM=1.1%) |
| Hypertensive1 | 32 (30.5%) | 18 (17.1%) |
| Gender | ||
| Men | 55 (58.5%) | 62 (52.4%) |
| Women | 50 (41.5%) | 44 (47.6%) |
| M±SEM | M±SEM | |
| Age | 38.3 ± 0.7 | 36.8 ± 0.7 |
| BMI2 | 28.6 ± 0.6 | 25.1 ± 0.4 |
| Baseline SBP (mmHg)1 | 130.4 ± 1.6 | 124.3 ± 1.5 |
| Baseline DBP | 77.6 ± 1.1 | 75.0 ± 1.0 |
| Occupational Status | 4.76 ± 0.17 | 3.90 ± 0.18 |
| SBP Pressor Change (mmHg)2 | 32.2 ± 1.6 | 26.6 ± 1.3 |
| DBP Pressor Change (mmHg)2 | 20.3 ± 0.9 | 16.3 ± 0.8 |
| Per Capita Income in Block2 | $16,520 ± $855 | $23,718.58 ± $863 |
p<.05
p<.01
Multilevel Model
Hierarchical Linear and Nonlinear Modeling (HLM 6.04, Student Version; Raudenbush, Bryk, Congdon, 2005) statistical software was used to examine whether neighborhood poverty interacts with individual SES and ethnicity to predict pressor responses to PE. Specifically, we were interested in determining whether the effects of individual SES (education, occupation), and ethnicity on pressor responses were the same in neighborhoods with different poverty levels. Since we were interested in the effects of each individual SES factor independent of the other one, education and occupation were each tested in a separate model. In these analyses, ethnicity and individual SES (education/occupation) were entered as level-1 variables.
Preliminary analyses were conducted examining relationships between pressor responses to PE and several potential confounding variables (i.e., age, BMI, study cohort (1995 versus 2001), baseline BP, gender, and, smoking). Only BMI and baseline BP emerged as being significantly related to pressor responses to PE (p’s<.05). To control for these potential confounding effects, BMI and baseline BP were entered as level-1 covariates in analyses. Percentage of neighborhood poverty was entered as a level-2 predictor variable in these analyses.
The interaction between level-1 (ethnicity, education, occupation) and level-2 variables (neighborhood poverty) was examined by testing whether the effect of level-1 variables was the same in neighborhoods with different poverty levels. HLM automatically tests the interaction between these level-1 and level-2 variables once they are entered into the model and no additional steps are needed to perform these tests (Raudenbush, Bryk, Cheong, & Congdon, 2004) for a complete explanation of HLM). Outcome variables included systolic and diastolic pressor responses to PE.
Analyses were then conducted to examine the three-way interaction between ethnicity, individual SES (education, occupation) and neighborhood poverty. To do so, we re-ran the above analyses with the ethnicity × education/occupation interaction term entered on level-1 of these analyses. HLM automatically examines the 3-way by testing ethnicity × education/occupation across neighborhood with different poverty levels.
Chi square tests examined whether slopes depicting the influence of BMI, baseline BP, education, occupation, and ethnicity on pressor responses to PE randomly varied across neighborhoods. Because, these tests revealed that slopes associated with the effects of ethnicity and baseline BP on systolic and diastolic pressor responses varied by neighborhoods, these variables were treated as random effects. All other variables in the model were treated as fixed effects because their associated chi square tests were non-significant.
Results
Sample Characteristics
Ethnic differences in sample characteristics are listed in Table 1 using combined data from the two protocols. African-Americans had higher baseline systolic BP (t1, 198 = −2.85, p < .01), a higher BMI (t1, 202 = −4.75, p < .01), and were more likely to be hypertensive (t1, 202 = −2.26, p < .05) than Caucasian-Americans. African-Americans also had a higher systolic (t1, 146 =−2.65, p < .01) and diastolic (t1, 146 = −3.03, p < .01) pressor responses to PE. Concerning SES, African-American had less education (t1, 204 = 3.70, p < .01) and less skilled occupations (t1, 204 =3.31, p < .01) than Caucasian-Americans. They were also more likely to live in neighborhoods with more poverty (t1, 192 = −2.40, p < .05) than Caucasian-Americans.
Multilevel Model: Effect of Individual SES within Neighborhoods with Different Poverty Levels
Systolic Pressor Response
Table 3 demonstrates the results of the multilevel analysis relating ethnicity, individual SES (education, occupation), and neighborhood SES to systolic pressor responses, with baseline SBP and BMI entered as covariates in the model. Of the covariates, only BMI was significantly related to systolic pressor responses to PE (B=−2.34, t16, 106 = −2.34, p = .04). Higher BMI was associated with less of an increase in systolic blood pressure following the PE injection.
Table 3.
Effects of Education and Neighborhood SES on Systolic Pressor Response*
| Fixed Effects | Coefficient | Std Error | T-ratio | Df | p-value |
|---|---|---|---|---|---|
| Intercept 1 (B0) | |||||
| Intercept 2, G00 | 34.60 | 8.71 | 3.9 | 16 | 0.001 |
| % Below Poverty, G01 | −0.12 | 0.44 | −0.28 | 16 | 0.79 |
| Baseline SBP (B1) | |||||
| Intercept 2, G10 | −0.44 | 0.42 | −1.03 | 106 | 0.31 |
| % Below Poverty, G11 | 0.020 | 0.018 | 1.13 | 106 | 0.26 |
| BMI (B2) | |||||
| Intercept 2, G20 | −2.34 | 1.12 | −2.09 | 106 | 0.04 |
| % Below Poverty, G21 | 0.097 | 0.054 | 1.81 | 106 | 0.09 |
| Ethnicity (B3) | |||||
| Intercept 2, G30 | 1.50 | 11.32 | 0.13 | 106 | 0.89 |
| % Below Poverty, G31 | −.066 | 0.53 | −0.13 | 106 | 0.90 |
| Educational Attainment (B4) | |||||
| Intercept 2, G40 | −13.34 | 5.61 | −2.38 | 106 | 0.019 |
| % Below Poverty, G41 | 0.554 | 0.249 | 2.23 | 106 | 0.028 |
Table 3 demonstrates the interaction between level-1 predictors (associated beta weights: B1, B2, B3, B4) and the level-2 predictor (G01) on systolic pressor responses to PE. As shown in the final block of the table, educational attainment (B4) interacts with % below poverty to predict systolic pressor responses to PE (G41). Overall, education is associated with less of an increase in SBP in response to PE (G40). However, as % below poverty increases, the beneficial effect of education on systolic pressor responses diminishes.
Overall, less education was associated with a greater increase in SBP in response to PE (B=−13.34, t16, 106 = −2.38, p = .019). There was not a significant main effect of neighborhood poverty on systolic pressor responses to PE. However, there was a significant interaction between neighborhood poverty on systolic pressor response. Analysis of the multilevel model revealed that the effect of educational attainment on systolic pressor response was dependent on neighborhood poverty level (B=.554, t16, 106 = 2.23, p = .028).
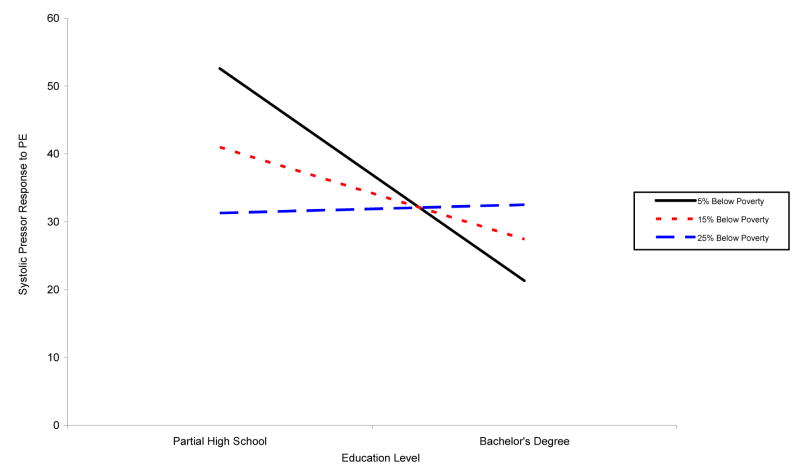
Simple slope analyses were calculated to determine the nature of this interaction. These analyses revealed that higher education was associated with a smaller increase in systolic BP in response to PE only in individuals who lived in neighborhoods in which less than 5% of the residents lived below the poverty line (B= −12.23, t16, 106 = −2.03, p = .044). The effect of education on systolic pressor response to PE was not significant in individuals who lived in neighborhoods where >5% of the residents lived below the poverty line (see Figure 1).
Figure 1.
Predicted slopes denoting the interaction between education and neighborhood poverty level on systolic pressor responses to PE. Higher education was associated with lower systolic pressor responses to PE in neighborhoods with less than 5% of individuals living below the poverty level (p<.05). As neighborhood poverty increased, the protective effect of education on systolic pressor responses was no longer apparent.
There was no significant 3-way interaction between neighborhood poverty, individual education, and ethnicity on systolic pressor responses to PE. Occupation was unrelated to systolic pressor responses to PE, and it did not interact with neighborhood poverty or ethnicity to predict systolic pressor responses to PE.
Diastolic Pressor Response
Table 4 demonstrates the results of the multilevel analysis relating ethnicity, education, and neighborhood SES to diastolic pressor responses, with baseline DBP and BMI entered as covariates in the model. BMI was significantly related to diastolic pressor responses to PE (B=−2.07, t16, 106 = −3.08, p = .003), such that higher BMI was associated with less of an increase in systolic blood pressure following the PE injection. Additionally, there was a significant interaction between BMI and neighborhood poverty on diastolic BP responses to PE (B= .092, t16, 106 = −2.89, p = .003), demonstrating that as neighborhood poverty increased, the effect of BMI on diastolic pressor responses to PE became non-significant. Overall, less education was associated with a greater increase in DBP when given PE (B=−7.66, t16, 106 = −2.21, p = .029). There was not a significant main effect of neighborhood poverty on diastolic pressor response. However, there was a significant interaction between neighborhood poverty and individual education on diastolic pressor response. The effect of educational attainment on diastolic pressor response was dependent on neighborhood poverty level (B=.35, t16, 106 = 2.32, p = .022).
Table 4.
Effects of Education and Neighborhood SES on Diastolic Pressor Response*
| Fixed Effects | Coefficient | Std Error | T-ratio | Df | p-value |
|---|---|---|---|---|---|
| Intercept 1, B0 | |||||
| Intercept 2, G00 | 23.43 | 5.28 | 4.4 | 16 | 0.001 |
| % Below Poverty, G01 | −0.16 | 0.27 | −0.61 | 16 | 0.55 |
| Baseline SBP, B1 | |||||
| Intercept 2, G10 | 0.12 | 0.35 | .34 | 16 | 0.73 |
| % Below Poverty, G11 | 0.016 | 0.015 | −1.06 | 16 | 0.30 |
| BMI, B2 | |||||
| Intercept 2, G30 | −2.07 | 0.67 | −3.08 | 106 | 0.003 |
| % Below Poverty, G21 | 0.092 | 0.032 | 2.89 | 106 | 0.005 |
| Ethnicity, B3 | |||||
| Intercept 2, G20 | 0.91 | 7.02 | 0.13 | 16 | 0.89 |
| % Below Poverty, G31 | 0.085 | 0.32 | 0.26 | 16 | 0.79 |
| Educational Attainment, B4 | |||||
| Intercept 2, G40 | −7.66 | 3.47 | −2.21 | 106 | 0.02 |
| % Below Poverty, G41 | 0.35 | 0.15 | 2.32 | 106 | 0.02 |
Table 4 demonstrates the interaction between level-1 predictors (associated beta weights: B1, B2, B3, B4) and the level-2 predictor (G01) on diastolic pressor responses to PE. As shown in the final block of the table, educational attainment (B4) interacts with % below poverty to predict diastolic pressor responses to PE (G41). Overall, education is associated with less of an increase in DBP in response to PE (G40). However, as % below poverty increases, the beneficial effect of education on diastolic pressor responses diminishes.
Simple slope analyses revealed that higher education was associated with a smaller increase in diastolic BP in response to PE only in individuals who lived in neighborhoods in which less than 5% of the residents lived below the poverty line (B= −6.96, t16, 106 = −2.08, p = .039). The effect of education on diastolic pressor response to PE was not significant in individuals who lived in neighborhoods where more than 5% of the residents lived below the poverty line (see Figure 2).
Figure 2.
Predicted slopes denoting the interaction between education and neighborhood poverty levelon diastolic pressor responses to PE. Higher education was associated with lower diastolic pressor responses to PE in neighborhoods with less than 5% of individuals living below the poverty level (p<.05). As neighborhood poverty increased, the protective effect of education on diastolic pressor responses was no longer apparent.
There was no significant 3-way interaction between neighborhood poverty, individual education, and ethnicity on diastolic pressor responses to PE. Occupation was unrelated to diastolic pressor responses to PE, and it did not interact with neighborhood poverty or ethnicity to predict diastolic pressor responses to PE.
Discussion
This study examined the interaction between individual-level SES and neighborhood poverty on pressor responses to PE. Multilevel analyses revealed a significant 2-way interaction between neighborhood poverty and individual education. Specifically, higher education was associated with a smaller increase in BP in response to PE only in individuals who lived in neighborhoods in which less than 5% of the residents lived below the poverty line. When neighborhood poverty level increased, higher education was no longer associated with diminished pressor responsiveness. This was the case for both systolic and diastolic pressor responses to PE. These findings support the results of a review conducted by Krieger and Fee (Krieger & Fee, 1994) in which the authors concluded that education has little effect on health in individuals living below the poverty line.
Based on data from the National Center for Health Statistics’s National Health Interview Survey of self reported illness, which demonstrated that there is a stronger relationship between education and health status among those living above the poverty line than among those living below the poverty line, Krieger and Fee (1994) concluded that education has little effect on health among those with household incomes that are below the poverty line. This suggests that although education may be associated with positive health outcomes, its ability to buffer the negative health effects of poverty is weakened as poverty level increases.
To determine whether our inability to observe an effect of education among individuals who lived in lower SES neighborhoods was due to restricted variability in education in lower SES neighborhoods, we examined the means and standard deviations of education when neighborhood SES was stratified by 5%, 15%, and 25% poverty level. These analyses revealed that although individuals who lived in neighborhoods with 5% or less poverty were more likely to have at least a college degree than those in lower SES neighborhoods, there was no difference in standard deviations across the 3 groups (means and SD’s in groups with 5%, 15%, and 25% poverty: 4.64 (.91), 3.94 (1.0), and 3.96 (1.10), respectively). This suggests that our findings were not simply due to limited variability in lower SES neighborhoods.
Our results differ from the results of Wilson and colleagues (Wilson et al., 2000) in which individual-level SES served as a protective factor against increase cardiovascular reactivity among individuals living in low SES neighborhoods. Substantial age differences between the two samples may account for these divergent findings. The study by Wilson and colleagues (Wilson et al., 2000) was conducted using an adolescent sample of African Americans between the ages of 13–16 years old and parental income and education level was used to measure individual SES. In contrast, the current study was conducted with African American and Caucasian American adults between the ages of 25–52 years old, with participant education and occupation used to measure individual SES. There is evidence that SES in childhood and adulthood differentially predict health outcomes (Campbell, Key, Ireland, Bacon, & Ditto, 2008; Luo & Waite, 2005). To our knowledge, no study has examined differences in the mental and physical health effects of living in impoverished neighborhoods between adolescent and adult samples. Thus, these cohort differences should be further explored in future research. In addition, our study and that of Wilson and colleagues (Wilson et al., 2000) differed profoundly in terms of the reactivity challenges; ours employed a pharmacological challenge, whereas Wilson’s employed a behavioral challenge.
Contrary to what we expected, there was no 3-way interaction between ethnicity, individual education, and neighborhood poverty, suggesting that the impact of education and neighborhood poverty on BP responses to PE was the same in African-Americans and Caucasian-Americans. It is possible that there was limited power to detect 3-way interactions and that the null findings do not accurately reflect relationships between these variables in the general population. Alternatively, these findings suggest that regardless of ethnicity, education had less protective effects on BP when it was superimposed on poverty. Even after controlling for ethnicity, BMI, and baseline BP, education was only associated with pressor response to PE in individuals who reside in neighborhoods in which less than 5% of individuals live below the poverty line.
Occupation was unrelated to pressor responses to PE in multilevel models. Methodological issues associated with our measure of occupational status may have obscured our ability to assess relationships between this factor and pressor responses to PE. The Hollingshead index of social position was used to measure occupational status. The categories used in this scale may be outdated and unable to capture some individuals’ social position in society (i.e., retirees and homemakers) (Shavers, 2007). Additionally, there may be a wide variation in education, income, and prestige associated with some occupational categories (Shavers, 2007). These issues may explain our null findings concerning relationships between occupation and pressor responses to PE.
Unexpected findings emerged concerning relationships between our covariate, BMI, and pressor responses to PE. Higher BMI was associated with less of an increase in systolic and diastolic BP following the PE injection, especially in neighborhoods with less poverty. These findings are intriguing given that obesity is a risk factor for CVD (Adams et al., 2006) and it is associated with greater cardiovascular reactivity (Steptoe & Wardle, 2005; Waldstein, Burns, Toth, & Poehlman, 1999). However, the relationship between obesity and cardiovascular reactivity seems to be strongest when abdominal adiposity is used as a marker of obesity (Goldbacher, Matthews, & Salomon, 2005; Jern, Bergbrant, Bjorntorp, & Hansson, 1992; Steptoe & Wardle, 2005). In studies using BMI, findings have been less consistent (Steptoe & Wardle, 2005), and some researchers have found that higher BMI is been associated with less reactivity (Carroll, Phillips, & Der, 2008; Jern et al., 1992). Clearly, more work needs to be done to understand the role that BMI plays in cardiovascular reactivity, an important issue that is beyond the scope of this study.
The current findings are noteworthy for several reasons. They suggest that the health benefits associated with educational attainment alone may not be potent enough to counteract the adverse effects of living in neighborhoods with more poverty. Some characteristics of the neighborhood that may have adverse effects on cardiovascular health include higher crime rates (Sundquist et al., 2006), lack of access to healthy foods (Echeverria et al., 2004; Krummel et al., 2001), limited recreation and environments that discourage physical activity (Echeverria et al., 2004), as well as lack of access to health care and health information (Blair et al., 2002).
Additionally, individuals who reside in low SES neighborhoods may have more exposure to stressful experiences with limited resources to counteract the psychophysiological effects of these stressors. There is evidence that socioeconomically disadvantaged individuals have more depression and anger (Haukkala, 1999; Lorant et al., 2003), which may result from their greater exposure to stressors (i.e., higher crime rates, quarrels with neighbors, noise pollution, and overcrowding). Further, these psychological responses have been associated with more sympathetic nervous system activation (Carney, Freedland, & Veith, 2005; Chida & Hamer, 2008; Vella & Friedman, 2007; Why & Johnston, 2008; Yu, Kang, Ziegler, Mills, & Dimsdale, 2008). Based on these findings, it is plausible that psychological distress may mediate relationships between the socioeconomic variables in this study and pressor responses to PE. Depression and anger among individuals who live in impoverished neighborhoods may result in increased sympathetic nervous system activation in response to stress. Repeated activation of the sympathetic nervous system in response to stress may lead to hypertrophied blood vessels that respond to pressors such as norepinephrine and PE with exaggerated vasoconstriction, increasing the risk for cardiovascular disease. It was beyond the scope of this study to determine whether these factors contributed a significant proportion of variability in cardiovascular functioning. However, future research should “un-package” neighborhood poverty to determine which of the above aspects should be targeted in public health interventions and public policies designed to eliminate health disparities.
There are several methodological issues that should be considered when interpreting the results of the current analyses. This study was conducted using a modest sample size. In the current study, multilevel analyses were conducted on only 137 individuals who had complete data on all variables entered into the analyses. Thus, reduced power may have limited our ability to detect relationships, particularly interactions, among variables. Future studies should be conducted using larger sample sizes. It should also be noted that women in the current study were slightly younger (mean age = 36.49 versus 38.46, p=.054) and were more likely to have higher skilled occupations than men (mean occupational status = 4.76 versus 3.90, p=.001). However, there were no gender differences in pressor responses to PE. Thus, gender differences do not seem to be impacting the results of the study.
There a number of medical conditions that cause hypertension and can lead to heightened vascular reactivity (e.g., diabetes, obstructive sleep apnea). Including individuals with these conditions would have confounded relationships between SES and pressor responses to PE, inhibiting our ability to obtain a clear picture of associations between neighborhood poverty and vascular reactivity. Thus, we chose to exclude individuals from this study with medical conditions other than hypertension. It should be cautioned that this limits the ability to generalize the current results to medical populations.
Another limitation of the current study was that data were combined from two different protocols to conduct this study. Descriptive statistics conducted prior to performing analyses revealed SES differences between the samples; the 1995 sample had lower SES than the 2000 sample. Combining the samples may have introduced additional error variance into the study, resulting in less power to detect effects. However, in spite of limited power, analyses revealed a significant interaction between neighborhood poverty and education on pressor responses to PE. The fact that this effect emerged with the above power issues suggests that it is a salient effect and worthy of further examination in future studies.
This is the first study that has examined the association between neighborhood poverty and vascular reactivity in a multilevel model, and the current results suggest that the relationship between SES and pressor responsiveness is complex with individual and neighborhood SES factors interacting to predict pressor responses to PE. Since neighborhood poverty seems to play an important role in cardiovascular health (Krieger, Chen, Waterman, Rehkopf, & Subramanian, 2005), research should continue examining its association with pressor responsiveness as well as other cardiovascular indicators.
Acknowledgments
This work was supported by grants HL36005, RR00827, and M01RR00827 from the National Institutes of Health and was partially supported by Grant P60 MD00220, from the San Diego EXPORT Center, National Center of Minority Health and Health Disparities, National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Census 2000 (2001). American Factfinder. Retrieved January, 2006, from factfinder.census.gov
- Anand K, Shah B, Yadav K, Singh R, Mathur P, Paul E, et al. Are the urban poor vulnerable to non-communicable diseases? A survey of risk factors for non-communicable diseases in urban slums of Faridabad. Natl Med J India. 2007;20(3):115–120. [PubMed] [Google Scholar]
- Blair AS, Lloyd-Williams F, Mair FS. What do we know about socioeconomic status and congestive heart failure? A review of the literature. J Fam Pract. 2002;51(2):169. [PubMed] [Google Scholar]
- Bravata DM, Wells CK, Gulanski B, Kernan WN, Brass LM, Long J, et al. Racial disparities in stroke risk factors: the impact of socioeconomic status. Stroke. 2005;36(7):1507–1511. doi: 10.1161/01.STR.0000170991.63594.b6. [DOI] [PubMed] [Google Scholar]
- Campbell TS, Key BL, Ireland AD, Bacon SL, Ditto B. Early socioeconomic status is associated with adult nighttime blood pressure dipping. Psychosom Med. 2008;70(3):276–281. doi: 10.1097/PSY.0b013e3181647e30. [DOI] [PubMed] [Google Scholar]
- Carney RM, Freedland KE, Veith RC. Depression, the autonomic nervous system, and coronary heart disease. Psychosom Med. 2005;67(Suppl 1):S29–33. doi: 10.1097/01.psy.0000162254.61556.d5. [DOI] [PubMed] [Google Scholar]
- Carroll D, Phillips AC, Der G. Body mass index, abdominal adiposity, obesity, and cardiovascular reactions to psychological stress in a large community sample. Psychosom Med. 2008;70(6):653–660. doi: 10.1097/PSY.0b013e31817b9382. [DOI] [PubMed] [Google Scholar]
- Census. (2001). American Factfinder. Retrieved January, 2006, from factfinder.census.gov
- Chida Y, Hamer M. Chronic psychosocial factors and acute physiological responses to laboratory-induced stress in healthy populations: a quantitative review of 30 years of investigations. Psychol Bull. 2008;134(6):829–885. doi: 10.1037/a0013342. [DOI] [PubMed] [Google Scholar]
- Cozier YC, Palmer JR, Horton NJ, Fredman L, Wise LA, Rosenberg L. Relation between neighborhood median housing value and hypertension risk among black women in the United States. Am J Public Health. 2007;97(4):718–724. doi: 10.2105/AJPH.2005.074740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimsdale JE, Graham RM, Ziegler MG, Zusman RM, Berry CC. Age, race, diagnosis, and sodium effects on the pressor response to infused norepinephrine. Hypertension. 1987;10(6):564–569. doi: 10.1161/01.hyp.10.6.564. [DOI] [PubMed] [Google Scholar]
- Echeverria SE, Diez-Roux AV, Link BG. Reliability of self-reported neighborhood characteristics. J Urban Health. 2004;81(4):682–701. doi: 10.1093/jurban/jth151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott HL, Sumner DJ, McLean K, Reid JL. Effect of age on the responsiveness of vascular alpha-adrenoceptors in man. J Cardiovasc Pharmacol. 1982;4(3):388–392. doi: 10.1097/00005344-198205000-00008. [DOI] [PubMed] [Google Scholar]
- Flaa A, Eide IK, Kjeldsen SE, Rostrup M. Sympathoadrenal stress reactivity is a predictor of future blood pressure: an 18-year follow-up study. Hypertension. 2008;52(2):336–341. doi: 10.1161/HYPERTENSIONAHA.108.111625. [DOI] [PubMed] [Google Scholar]
- Goldbacher EM, Matthews KA, Salomon K. Central adiposity is associated with cardiovascular reactivity to stress in adolescents. Health Psychol. 2005;24(4):375–384. doi: 10.1037/0278-6133.24.4.375. [DOI] [PubMed] [Google Scholar]
- Haukkala A. Socioeconomic differences in measures of hostility. Ann N Y Acad Sci. 1999;896:448–450. doi: 10.1111/j.1749-6632.1999.tb08166.x. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Two factor index of social position. New Haven, CT: Yale Univeristy Press; 1958a. [Google Scholar]
- Iceland J, Sharpe C, Steinmetz E. Class differences in African American residential patterns in US metropolitan area: 1990–2000. Soc Sci Res. 2005;34(1):252–266. [Google Scholar]
- Jern S, Bergbrant A, Bjorntorp P, Hansson L. Relation of central hemodynamics to obesity and body fat distribution. Hypertension. 1992;19(6 Pt 1):520–527. doi: 10.1161/01.hyp.19.6.520. [DOI] [PubMed] [Google Scholar]
- Kapuku GL, Treiber FA, Davis HC. Relationships among socioeconomic status, stress induced changes in cortisol, and blood pressure in African American males. Ann Behav Med. 2002;24(4):320–325. doi: 10.1207/S15324796ABM2404_08. [DOI] [PubMed] [Google Scholar]
- Kobetz E, Daniel M, Earp JA. Neighborhood poverty and self-reported health among low-income, rural women, 50 years and older. Health Place. 2003;9(3):263–271. doi: 10.1016/s1353-8292(02)00058-8. [DOI] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005;95(2):312–323. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Fee E. Social class: the missing link in U.S. health data. Int J Health Serv. 1994;24(1):25–44. doi: 10.2190/2JG7-YMD5-WCP2-XXNT. [DOI] [PubMed] [Google Scholar]
- Krummel DA, Gordon P, Newcomer RR, Lui X, Christy DM, Holmes A. Dietary intakes and leisure-time physical activity in West Virginians. W V Med J. 2001;97(6):295–301. [PubMed] [Google Scholar]
- Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157(2):98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Loucks EB, Rehkopf DH, Thurston RC, Kawachi I. Socioeconomic disparities in metabolic syndrome differ by gender: evidence from NHANES III. Ann Epidemiol. 2007;17(1):19–26. doi: 10.1016/j.annepidem.2006.07.002. [DOI] [PubMed] [Google Scholar]
- Luo Y, Waite LJ. The impact of childhood and adult SES on physical, mental, and cognitive well-being in later life. J Gerontol B Psychol Sci Soc Sci. 2005;60(2):S93–S101. doi: 10.1093/geronb/60.2.s93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClellan WM. Epidemiology and risk factors for chronic kidney disease. Med Clin North Am. 2005;89(3):419–445. doi: 10.1016/j.mcna.2004.11.006. [DOI] [PubMed] [Google Scholar]
- MetropolitanLifeFoundation. Metropolitan Height and Weight Tables. New York: Metropolitin Life Insurance Company; 1983. [Google Scholar]
- Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am J Prev Med. 2006;30(4):333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Nzerue CM, Demissochew H, Tucker JK. Race and kidney disease: role of social and environmental factors. J Natl Med Assoc. 2002;94(8 Suppl):28S–38S. [PMC free article] [PubMed] [Google Scholar]
- Petersen KL, Bleil ME, McCaffery J, Mackey RH, Sutton-Tyrrell K, Muldoon MF, et al. Community socioeconomic status is associated with carotid artery atherosclerosis in untreated, hypertensive men. Am J Hypertens. 2006;19(6):560–566. doi: 10.1016/j.amjhyper.2005.12.008. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon RT. Hierarchical Linear and Nonlinear Modeling. Lincolnwood: Scientific Software International, Inc; 2004. [Google Scholar]
- Shavers VL. Measurement of socioeconomic status in health disparities research. J Natl Med Assoc. 2007;99(9):1013–1023. [PMC free article] [PubMed] [Google Scholar]
- Sherwood A, Hinderliter AL. Responsiveness to alpha- and beta-adrenergic receptor agonists. Effects of race in borderline hypertensive compared to normotensive men. Am J Hypertens. 1993;6(7 Pt 1):630–635. doi: 10.1093/ajh/6.7.630. [DOI] [PubMed] [Google Scholar]
- Singh GK, Siahpush M. Increasing inequalities in all-cause and cardiovascular mortality among US adults aged 25–64 years by area socioeconomic status, 1969–1998. Int J Epidemiol. 2002;31(3):600–613. doi: 10.1093/ije/31.3.600. [DOI] [PubMed] [Google Scholar]
- Stein CM, Lang CC, Singh I, He HB, Wood AJ. Increased vascular adrenergic vasoconstriction and decreased vasodilation in blacks. Additive mechanisms leading to enhanced vascular reactivity. Hypertension. 2000;36(6):945–951. doi: 10.1161/01.hyp.36.6.945. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Wardle J. Cardiovascular stress responsivity, body mass and abdominal adiposity. Int J Obes (Lond) 2005;29(11):1329–1337. doi: 10.1038/sj.ijo.0803011. [DOI] [PubMed] [Google Scholar]
- Subramanian SV, Chen JT, Rehkopf DH, Waterman PD, Krieger N. Racial disparities in context: a multilevel analysis of neighborhood variations in poverty and excess mortality among black populations in Massachusetts. Am J Public Health. 2005;95(2):260–265. doi: 10.2105/AJPH.2003.034132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchday S, Krantz DS, Gottdiener JS. Relationship of socioeconomic markers to daily life ischemia and blood pressure reactivity in coronary artery disease patients. Ann Behav Med. 2005;30(1):74–84. doi: 10.1207/s15324796abm3001_9. [DOI] [PubMed] [Google Scholar]
- Sundquist K, Theobald H, Yang M, Li X, Johansson SE, Sundquist J. Neighborhood violent crime and unemployment increase the risk of coronary heart disease: a multilevel study in an urban setting. Soc Sci Med. 2006;62(8):2061–2071. doi: 10.1016/j.socscimed.2005.08.051. [DOI] [PubMed] [Google Scholar]
- Vella EJ, Friedman BH. Autonomic characteristics of defensive hostility: reactivity and recovery to active and passive stressors. Int J Psychophysiol. 2007;66(2):95–101. doi: 10.1016/j.ijpsycho.2007.03.014. [DOI] [PubMed] [Google Scholar]
- Waldstein SR, Burns HO, Toth MJ, Poehlman ET. Cardiovascular reactivity and central adiposity in older African Americans. Health Psychol. 1999;18(3):221–228. doi: 10.1037//0278-6133.18.3.221. [DOI] [PubMed] [Google Scholar]
- Why YP, Johnston DW. Cynicism, anger and cardiovascular reactivity during anger recall and human-computer interaction. Int J Psychophysiol. 2008;68(3):219–227. doi: 10.1016/j.ijpsycho.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Williams RB. Blood pressure reactivity to psychological stress: a new risk factor for coronary disease? Hypertension. 2006;47(3):329–330. doi: 10.1161/01.HYP.0000200688.37802.01. [DOI] [PubMed] [Google Scholar]
- Wilson DK, Kliewer W, Plybon L, Sica DA. Socioeconomic status and blood pressure reactivity in healthy black adolescents. Hypertension. 2000;35(1 Pt 2):496–500. doi: 10.1161/01.hyp.35.1.496. [DOI] [PubMed] [Google Scholar]
- Yen IH, Moss N. Unbundling education: A critical discussion of what education confers and how it lowers risk for disease and death. In: Adler NE, Marmot M, MCEwen BS, Stewart J, editors. Socioeconomic Status and Health in Industrial Nations: Social, Psychological and Biological Pathways. Annals of the New York Academy of Sciences; 1999. pp. 350–351. [DOI] [PubMed] [Google Scholar]
- Yu BH, Kang EH, Ziegler MG, Mills PJ, Dimsdale JE. Mood states, sympathetic activity, and in vivo beta-adrenergic receptor function in a normal population. Depress Anxiety. 2008;25(7):559–564. doi: 10.1002/da.20338. [DOI] [PMC free article] [PubMed] [Google Scholar]