Abstract
Objective
To evaluate the clinical utility of MR imaging of the temporal bone in patients with facial and audiovestibular dysfunction with particular emphasis on the importance of contrast enhancement.
Materials and Methods
We retrospectively reviewed the MR images of 179 patients [72 men, 107 women; average age, 44 (range, 1-77) years] who presented with peripheral facial palsy (n=15), audiometrically proven sensorineural hearing loss (n=104), vertigo (n=109), or tinnitus (n=92). Positive MR imaging findings possibly responsible for the patients clinical manifestations were categorized according to the anatomic sites and presumed etiologies of the lesions. We also assessed the utility of contrast-enhanced MR imaging by analyzing its contribution to the demonstration of lesions which would otherwise not have been apparent. All MR images were interpreted by two neuroradiologists, who reached their conclusions by consensus.
Results
MR images demonstrated positive findings, thought to account for the presenting symptoms, in 78 (44%) of 179 patients, including 15 (100%) of 15 with peripheral facial palsy, 43 (41%) of 104 with sensorineural hearing loss, 40 (37%) of 109 with vertigo, and 39 (42%) of 92 with tinnitus. Thirty (38%) of those 78 patients had lesions that could be confidently recognized only at contrast-enhanced MR imaging.
Conclusion
Even though its use led to positive findings in less than half of these patients, MR imaging of the temporal bone is a useful diagnostic procedure in the evaluation of those with facial and audiovestibular dysfunction. Because it was only at contrast-enhanced MR imaging that a significant number of patients showed positive imaging findings which explained their clinical manifestations, the use of contrast material is highly recommended.
Keywords: Temporal bone, MR; Temporal bone, abnormalities; Magnetic resonance(MR), contrast enhancement
In daily clinical practice, otolaryngologists encounter a significant number of patients with facial and audiovestibular dysfunction. In the past, the diagnostic yields of radiological examination in these patients were low, and conventional radiography and polytomography rarely demonstrated the specific cause. While computed tomography (CT) is usually used in the investigation of diseases of the bony labyrinth and cerebellopontine angle, its contribution to the diagnosis of diseases of the membranous labyrinth and small lesions of the internal auditory canal is limited. In contrast, magnetic resonance (MR) imaging, by virtue of its superior contrast resolution and multiplanar imaging capability, can demonstrate small lesions involving the membranous labyrinth and internal auditory canal, and is currently the diagnostic imaging modality of choice for the evaluation of patients with facial and audiovestibular dysfunction such as Bell's palsy, sensorineural hearing loss, vertigo, and tinnitus (1-4). It can display wide spectrums of disease, from the temporal bone to the cerebral cortex. In particular, the use of contrast material in MR imaging has proven to be a very powerful means of depicting soft tissue abnormalities of the temporal bone, and can reveal to better advantage a subtle inflammatory or neoplastic process involving neural structures and the membranous labyrinth (5, 6). The purpose of this study was to evaluate the clinical utility of MR imaging of the temporal bone in patients with facial and audiovestibular dysfunction with particular emphasis on the importance of contrast enhancement.
MATERIALS AND METHODS
MR images of the temporal bone and medical records were retrospectively reviewed in 179 patients [M:F=72:107; average age, 44 (range, 1-77) years] with facial or audiovestibular dysfunction. The results of audiometry, auditory brain stem response and vestibular function tests, performed in our otolaryngologic department and interpreted by experienced audiologists and vestibular physiologists under the supervision of an experienced otologic surgeon, were also available for review in 143, 21, and 95 patients, respectively. Fifteen patients presented with peripheral facial palsy, 104 with audiometrically proven sensorineural hearing loss, 109 with vertigo, and 92 with tinnitus as an isolated symptom or in combination. The average interval between the onset of symptoms and MR imaging was 11 (range, 0-100 days) days.
For all MR imaging, a 1.5-T scanner (Signa Advantage Horizon; GE Medical Systems, Milwaukee, Wis., U.S.A.) was used. Our routine MR imaging protocol for these patients included the acquisition of axial fast spin-echo T2-weighted [4000/98/2 (repetition time msec/echo time msec/excitations)] images of the brain, and axial spin-echo T1-weighted (400/9/3) and fast spin-echo T2-weighted (4000/98/4) images of the temporal bone, followed by axial, coronal, and sagittal spin-echo T1-weighted (400/9/3) imaging of the temporal bone, all after the administration of 0.1 mmol/kg gadopentetate dimeglumine (Magnevist®; Schering AG, Berlin, Germany). For brain imaging, a 20 cm × 20 cm field of view, 256 × 256 matrix size, and 7 mm slice thickness with no interslice gap were used, and a standard head coil. For temporal bone imaging, the parameters were a 16 cm × 16 cm field of view, 512 × 256 matrix size, and 2 mm slice thickness with no interslice gap, together with a 3-inch dual, circular, temporomandibular joint coil.
All MR images were interpreted by two neuroradiologists who were blinded to the varying clinical manifestations and diagnoses, and final decisions were reached by consensus. Positive MR imaging findings possibly responsible for the patients clinical manifestations were categorized according to the anatomic sites and presumed etiologies of the lesion, with particular attention paid to assessing the contribution of contrast enhancement to lesion detection at MR imaging. Any enhancement in the inner ear and along the course of the vestibulocochlear nerve and its branches was regarded as positive. As for the facial nerve, we considered the findings positive only when there was enhancement of the segment within the cerebellopontine angle cistern or the internal auditory canal. Within the labyrinth, we also documented unusually high signal intensity at T1-weighted imaging, as well as unusually low signal intensity at T2-weighted imaging: the former might represent intralabyrinthine fluid in which there was evidence of hemorrhage, or with high-protein content, and the latter might indicate obliterative labyrinthitis. Vascular loop or contact was considered significant if a prominent vasculature obviously impinged on the root exit or entry zone, or the cisternal segment of the facial or vestibulocochlear nerve, or if an unequivocal compression deformity of the brain stem caused by nearby vasculature was apparent.
RESULTS
Rates of positive MR imaging findings
The results of MR imaging according to the presenting symptoms and presumed causes of positive MR imaging findings are shown in Tables 1 and 2, respectively. Overal, MR images demonstrated positive findings, thought to account for the presenting symptoms, in 78 (44%) of 179 patients. Positive findings were demonstrated in all 15 patients (100%) with peripheral facial palsy (Fig. 1), in 43 of 104 (41%) with sensorineural hearing loss (Figs. 2-7), and in 40 of 109 (37%) with vertigo (Figs. 2, 3, 5, and 6), and causative lesions were apparent in 39 of 92 (42%) with tinnitus (Figs. 2-5).
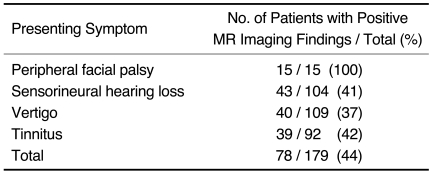
Table 1.
Rates of Positive MR Imaging Findings in Each Group of Presenting Symptoms
Table 2.
Number of Patients with Positive MR Imaging Findings Compared with Presenting Symptoms
Note.-*Indicates diseases that can be identified only at contrast-enhanced MR imaging
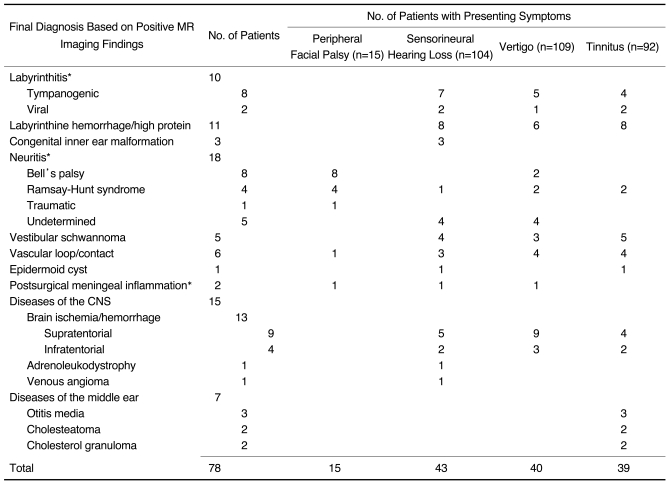
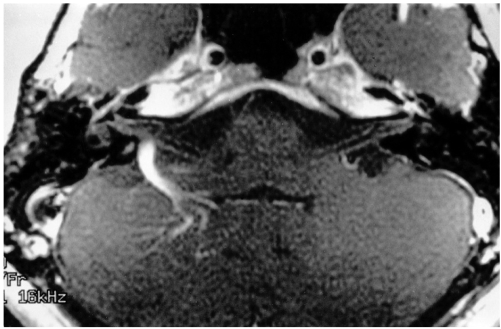
Fig. 1.
A 42-year-old man with right-sided Bell's palsy.
Axial pre- (A) and postcontrast (B) T1-weighted MR images demonstrate focal enhancement of the right facial nerve at the fundus of the internal auditory canal (arrow). Note the symmetric, intense enhancement of the facial nerves around the geniculate fossa on both sides (arrowheads), attributable to the prominent normal circumneural arteriovenous plexus located in this area.
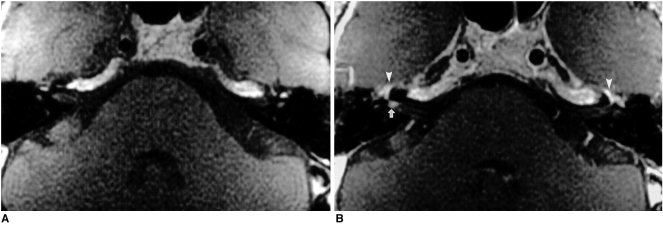
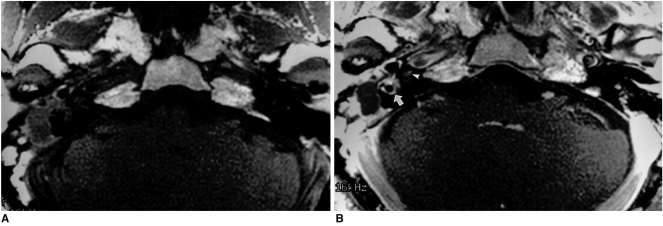
Fig. 2.
An 11-year-old girl with mumps who presented with sensorineural hearing loss, vertigo, and tinnitus. Axial pre- (A) and postcontrast (B) T1-weighted MR images show mild diffuse enhancement of the right cochlea and vestibule (arrows). No enhancement of the contralateral labyrinth is apparent, but on the right there is intense enhancement of the endolymphatic sac (arrowhead).
Fig. 7.
A 39-year-old woman with venous angioma of the right cerebellum who presented with sensorineural hearing loss. Axial postcontrast T1-weighted MR image shows a prominent draining vein caused by venous angioma of the right cerebellar hemisphere, which impinges on the vestibulocochlear nerve.
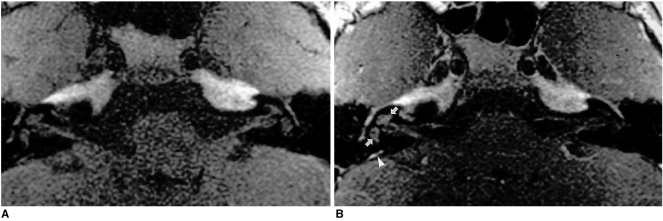
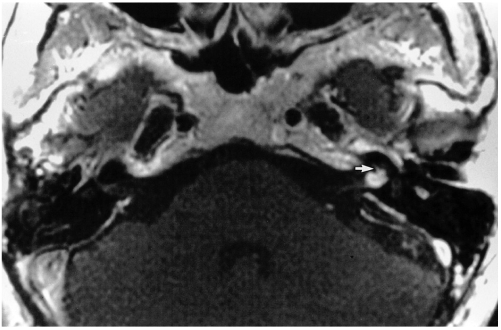
Fig. 3.
A 52-year-old man with labyrinthine fistula caused by middle ear cholesteatoma who presented with mixed hearing loss, vertigo, and tinnitus. Axial pre- (A) and postcontrast (B) T1-weighted MR images reveal that in the right ear, an atticoantral cholesteatoma showing predominant peripheral enhancement and central fluid-like material is present. As a result of infection spread through the labyrinthine fistula, there is intense enhancement of the right vestibule and lateral semicircular canal (arrow). Also noted is mild focal enhancement of the ipsilateral cochlea (arrowhead).
Fig. 5.
A 58-year-old woman with surgically proven vestibular schwannoma who presented with sensorineural hearing loss, vertigo, and tinnitus. Axial postcontrast T1-weighted MR image indicates that a small vestibular schwannoma in the left internal auditory canal extends to the basal turn of the cochlea (arrow).
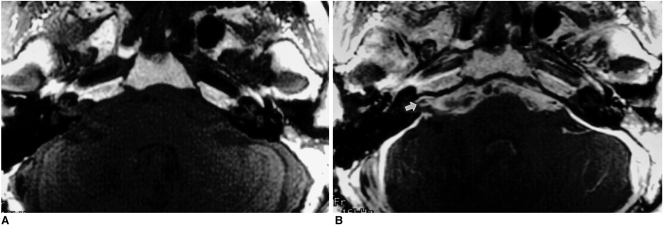
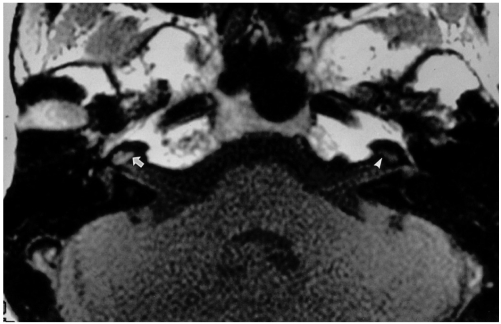
Fig. 6.
A 52-year-old man with leptomeningitis, and a history of ventriculoperitoneal shunt procedure, who presented with sensorineural hearing loss and vertigo. Axial pre- (A) and postcontrast (B) T1-weighted MR images demonstrate that diffuse enhancement of the subarachnoid space extends into the right internal auditory canal (arrow).
Of the 78 patients in whom positive findings were demonstrated by MR imaging, 30 (38%) had lesions that could be recognized with confidence only at contrast-enhanced MR imaging (Table 2). Without the use of contrast material, lesions would have been overlooked in 14 of 15 patients with peripheral facial palsy, 15 of 43 with sensorineural hearing loss, 15 of 40 with vertigo, and 8 of 39 with tinnitus.
MR imaging findings compared with final diagnosis
Ten patients were found to have tympanogenic (n=8) or viral (n=2) labyrinthitis: in the eight former cases, chronic middle ear infection was present and MR imaging revealed abnormal enhancement of the labyrinth (Fig. 3); in the other two, the results of a serological test for mumps antibody were abnormal and contrast-enhacned MR imaging also demonstrated abnormal labyrinthine enhancement (Fig. 2). The intralabyrinthine fluid of 11 other patients showed either evidence of hemorrhage or high protein content, as suggested by the high signal intensity seen at precontrast T1-weighted MR imaging (Fig. 4). In these 11, neither a past medical history of significant head trauma nor laboratory evidence of hematologic disorder was elucidated. Three patients had congenital inner ear malformations, all of which were clearly demonstrated by T2-weighted MR imaging. In 18, focal or linear enhancement along the vestibulocochlear nerve or at the fundus of the internal auditory canal was seen at contrast-enhanced MR imaging, and various forms of neuritis, namely Bell's palsy (n=8) (Fig. 1), Ramsay-Hunt syndrome (n=4), traumatic neuritis (n=1), and neuritis of undetermined origin (n=5) were diagnosed. For the first three conditions, diagnosis was based on the clinical history and typical symptoms and signs, while patients were assigned to the last category if the onset of symptoms was acute, but ameliorated by steroid treatment. Five patients had vestibular schwannomas, the presence of all of which was surgically proven (Fig. 5), and in six, significant vascular loop or contact responsible for the presenting symptoms was observed. One patient had a surgically proven epidermoid cyst in the cerebellopontine angle cistern and two were found to have postsurgical meningitis (Fig. 6). Fifteen were suffering from various diseases of the brain, including supratentorial (n=9) and infratentorial (n=4) ischemic or hemorrhagic diseases, adrenoleukodystrophy involving the periventricular white matter and the brain stem (n=1) , and venous angioma of the cerebellar hemisphere (n=1) (Fig. 7). Seven patients with tinnitus had diseases confined to the middle ear (Table 2).
Fig. 4.
A 51-year-old woman presenting with sensorineural hearing loss and tinnitus. Axial precontrast T1-weighted MR image depicts diffuse high signal intensity in the right cochlea (arrow), which is suggestive of hemorrhage or the presence of fluid with high protein content in the labyrinth. This should be compared with the normal signal intensity of the left cochlea (arrowhead).
DISCUSSION
The outcome of MR imaging for facial and audiovestibular dysfunction
In this study, the diagnostic yields of MR imaging of the temporal bone [overall, 44% (78/179)] in patients with facial and audiovestibular dysfunction were relatively high. The diagnostic yields for individual symptoms of such dysfunction, namely peripheral facial paralysis, sensorineural hearing loss, vertigo, and tinnitus were 100% (15/15), 41% (43/104), 37% (40/109), and 42% (39/92), respectively.
As for idiopathic peripheral facial paralysis, so-called Bell's palsy, the reported frequency with which contrast-enhanced MR imaging has shown positive findings, revealing abnomal enhancement along various segments of the facial nerve, has been relatively high, ranging from 43% to 100% (7-9). In this respect, care should be taken not to mistake normal enhancement of the intratemporal facial nerve for abnormal enhancement caused by a pathologic condition such as neuritis or a tumor. In their study involving 93 patients with 186 clinically normal bilateral facial nerves, Gebarski et al. (10) reported that at contrast-enhanced MR imaging, 142 nerves (76%) were visibly enhanced along at least one segment within the facial canal, and that enhanced images of the nerves of 64 of the 93 (69%) showed right-left asymmetry. This normal enhancement of the intratemporal facial nerve is attributed to the circumneural arteriovenous plexus which is inhomogeneously distributed along the facial canal, and is most prominently observed in the region of the geniculate ganglion (Fig. 1). However, enhancement of the facial nerve in the cerebellopontine angle cistern and the internal auditory canal should always be considered abnormal (2, 10).
In contrast to peripheral facial paralysis, the role of neuroimaging in patients referred for the evaluation of audiovestibular dysfunction is less clear-cut. After reviewing the neuroimaging studies and results of audiovestibular testing in 118 patients with audiovestibular dysfunction, Levy and Arts (11) concluded that clinical presentation and audiovestibular testing could not sensitively predict the outcome of neuroimaging. Only 15 of 118 (13%) patients had positive neuroimaging findings related to their presenting symptoms. If account is taken of the fact that in 11 of these 15 patients, vestibular schwannoma was either proven or presumed to be present, the diagnostic yield of imaging studies for demonstrating pathology other than vestibular schwannoma was surprisingly low in their series.
With regard to sensorineural hearing loss, Levy and Arts (11) demonstrated the presence of a pathological condition in only 18% (12/65) of patients, while in another series of 78 patients with sudden hearing loss, abnormal imaging findings were demonstrated in 24 (31%) (12). The role of neuroimaging in patients referred for the evaluation of vertigo is more perplexing. In a study of 20 elderly patients with dizziness, Day et al. (13) reported that the MR findings in these patients were not different from those in an age-matched control group. According to Levy and Arts (11), in only 9% (6/65) of patients with vertigo/dizziness/balance difficulty/dysequilibrium did neuroimaging studies showed positive findings. In a study involving 167 patients with vertigo and/or abnormal findings at vestibular testing, Casselman et al. (14) reported that MR imaging was able to detect the presence of a pathological condition, potentially explaining vertigo in 54 (32%) patients. In another series of 79 patients referred for dizziness or rotatory vertigo, neuroimaging studies were positive in 27 (34%) (15). To our knowledge, none of the literature except the abovementioned article by Levy and Arts (11) has mentioned the outcome of neuroimaging in patients with tinnitus. In their series, neuroimaging demonstrated positive findings possibly responsible for tinnitus in only eight (15%) of 55 patients, as compared with 42% in this study, a surprisingly high positive rate which seems to be attributable in part to the analytical method used in this study, that is, rather generous inclusion of middle ear disease as a possible cause of tinnitus. However, because tinnitus can be generated by any lesion or disturbance involving the auditory pathway from the external auditory canal to the central auditory cortex, and also because - except in the case of extra-auditory tinnitus, as commonly seen where the condition is vasculogenic or musculogenic - it is hard to distinguish the different origins of tinnitus by the physical characteristics, it seemed reasonable not to exclude lesions of the middle ear as its possible causes. We believe that the wide variations in positive imaging results in patients with audiovestibular dysfunction is most probably caused by the different fractions of disease entity included in different studies.
The role of contrast-enhanced MR imaging in facial and audiovestibular dysfunction
The high prevalence of positive MR imaging results in this study is attributed to the use of contrast material. We believe that 30 of the 78 (38%) patients whose MR imaging findings were positive would have been overlooked if contrast material had not been used. Non-identification is especially likely in cases in which an inflammatory condition involving the facial or vestibulocochlear nerve and the membranous labyrinth, one that at contrast-enhanced MR imaging can simulate a neoplasm, is present (16). Although several authors have advocated limited studies of the temporal bone using noncontrast high-resolution T2-weighted MR imaging in order to rule out vestibular schwannomas, and have done so principally on the basis of cost effectiveness (17), it is clear from the findings of this study and those of others (5, 12) that such an approach would fail to demonstrate significant numbers of inflammatory lesions of the facial or vestibulocochlear nerve and the membranous labyrinth.
In this study, contrast-enhanced MR imaging was most effective in patients with peripheral facial palsy; in 14 of 15 with this condition, lesions were demonstrated only by this modality. As mentioned above, a diagnosis of Bell's palsy on the basis of enhancement of the facial nerve within the facial canal can be erroneous (2); enhancement of the internal auditory canal (most commonly at the fundus) or cisternal portion of the facial nerve should instead be relied upon. Sometimes, a lesion in which the MR findings are identical to those observed in Bell's palsy may eventually prove to be malignant (18). While contrast-enhanced MR imaging is a valuable tool in the evaluation of patients with facial paralysis, its limitation should be recognized and the findings must be interpreted in conjunction with the clinical presentation.
In contrast to the imaging of patients with peripheral facial paralysis, the imaging of those with audiovestibular dysfunction has been reported to yield no positive findings in more than half of all patients, even though contrast material is used. Although enhancement of the membranous labyrinth is reported to be a highly specific finding of labyrinthine pathology, and there is close correlation between labyrinthine enhancement and audiovestibular symptoms, the sensitivity of this finding remains to be determined (4, 19). A possible explanation for this is that the offending deformity may reside at the level of the hair cells of the organ of Corti or the cupula, far beyond the resolution of current MR imaging. In addition, hearing loss in elderly patients is often secondary to presbycusis, for which there is no imaging correlate (20). As with enhancement in the meninges, there may be a threshold effect with only the most severe inflammatory processes consistently producing labyrinthine or neural enhancement (4). If contrast material had not been used in this study, lesions would have been overlooked at MR imaging in 15 of 43 patients with sensorineural hearing loss, 14 of 39 with vertigo, and eight of 39 with tinnitus.
Sometimes, if precontrast images are not obtained, lesions containing a hemorrhagic or lipid component can mimic enhancing lesions at contrast-enhanced MR imaging. Typically, this is so in cases of labyrinthine hemorrhage and intracanalicular lipoma (21). In this study, high signal intensity was observed at precontrast T1-weighted MR imaging in 11 of 78 patients with positive MR imaging findings. In all patients, clinical and laboratory findings were unremarkable for head trauma and hematologic disorder. Although clinical and histologic proof is lacking, we believe that the intralabyrinthine high signal intensity seen at precontrast MR imaging was caused by either hemorrhagic fluid resulting from forgotten minor head trauma or highly proteinaceous fluid resulting from labyrinthitis due to any cause. In the hope of clarifying this issue in the near future, a prospective study is warranted. We suggest that precontrast T1-weighted MR imaging procedures should be included in the evaluation of patients with suspected intralabyrinthine pathology.
Although rare, vascular lesions in the cerebellopontine angle cistern or internal auditory canal, such as vertebrobasilar dolichoectasia, aneurysm, and vascular loops, can produce facial palsy, sensorineural hearing loss, vertigo, or tinnitus (1, 2). In this study, the presenting symptoms of six patients were attributed to a vascular lesion. Although our criteria governing the inclusion of lesions were rather strict, a specific cause-and-effect relationship between these vascular lesions seen at MR imaging and the patients clinical symptoms may be clear only when there is surgical evidence for this. MR imaging using a three-dimensional fast gradient-echo technique such as constructive interference in steady-state MR imaging, which was not used in this study, may prove useful in this clinical setting.
In conclusion, MR imaging of the temporal bone is a useful diagnostic procedure for the evaluation of patients with facial and audiovestibular dysfunction, even though there were positive findings in less than half the patients involved. Because it was only at contrast-enhanced MR imaging that a significant number of patients showed positive imaging findings which explained their clinical manifestations, the use of contrast material is highly recommended. In a considerable number of patients, however, the supposed cause of audiovestibular symptoms cannot be identified even after contrast-enhanced MR imaging. A knowledge of the benefits and limitations of contrast-enhanced MR imaging of the temporal bone can help guide radiologists towards a correct interpretation of what they have observed at MR imaging.
References
- 1.Casselman JW. Temporal bone imaging. Neuroimag Clin N Am. 1996;6:265–289. [PubMed] [Google Scholar]
- 2.Swartz JD, Harnsberger HR, Mukherji SK. The temporal bone: contemporary diagnostic dilemma. Radiol Clin North Am. 1998;36:819–853. doi: 10.1016/s0033-8389(05)70066-x. [DOI] [PubMed] [Google Scholar]
- 3.Lane JI. Facial nerve disorders. Neuroimag Clin N Am. 1993;3:129–151. [Google Scholar]
- 4.Mark AS. Vestibulocochlear system. Neuroimag Clin N Am. 1993;3:153–170. [Google Scholar]
- 5.Mark AS, Seltzer S, Harnsberger HR. Sensorineural hearing loss: more than meets the eye? AJNR. 1993;14:37–45. [PMC free article] [PubMed] [Google Scholar]
- 6.Mark A. Contrast-enhanced magnetic resonance imaging of the temporal bone. Neuroimag Clin N Am. 1994;4:117–131. [PubMed] [Google Scholar]
- 7.Burgio DL, Siddique S, Haupert M, Meleca RJ. Magnetic resonance imaging of the facial nerve in children with idiopathic facial paralysis. Otolaryngol Head Neck Surg. 2000;122:556–559. doi: 10.1067/mhn.2000.102914. [DOI] [PubMed] [Google Scholar]
- 8.Sartoretti-Schefer S, Kollias S, Wichmann W, Valavanis A. T2-weighted three-dimensional fast spin-echo MR in inflammatory peripheral facial nerve palsy. AJNR. 1998;19:491–495. [PMC free article] [PubMed] [Google Scholar]
- 9.Saatci I, Sahinturk F, Sennaroglu L, Boyvat F, Gursel B, Besim A. MRI of the facial nerve in idiopathic facial palsy. Eur Radiol. 1996;6:631–636. doi: 10.1007/BF00187662. [DOI] [PubMed] [Google Scholar]
- 10.Gebarski SS, Telian SA, Niparko JK. Enhancement along the normal facial nerve in the facial canal: MR imaging and anatomic correlation. Radiology. 1992;183:391–394. doi: 10.1148/radiology.183.2.1561339. [DOI] [PubMed] [Google Scholar]
- 11.Levy RA, Arts AH. Predicting neuroradiologic outcome in patients referred for audiovestibular dysfunction. AJNR. 1996;17:1717–1724. [PMC free article] [PubMed] [Google Scholar]
- 12.Fitzgerald DC, Mark AS. Sudden hearing loss: frequency of abnormal findings on contrast-enhanced MR studies. AJNR. 1998;19:1433–1436. [PMC free article] [PubMed] [Google Scholar]
- 13.Day JJ, Freer CE, Dixon AK. Magnetic resonance imaging of the brain and brainstem in elderly patients with dizziness. Age Ageing. 1990;19:144–150. doi: 10.1093/ageing/19.2.144. [DOI] [PubMed] [Google Scholar]
- 14.Casselman JW, Kuhweide R, Dehaene I, Ampe W, Devlies F. Magnetic resonance examination of the inner ear and cerebellopontine angle in patients with vertigo and/or abnormal findings at vestibular testing. Acta Otolaryngol Suppl. 1994;513:15–27. doi: 10.3109/00016489409127322. [DOI] [PubMed] [Google Scholar]
- 15.Ojala M, Ketonen L, Palo J. The value of CT and very low-field MRI in the etiological diagnosis of dizziness. Acta Neurol Scand. 1988;78:26–29. doi: 10.1111/j.1600-0404.1988.tb03614.x. [DOI] [PubMed] [Google Scholar]
- 16.Han MH, Jabour BA, Andrews JC, et al. Nonneoplastic enhancing lesions mimicking intracanalicular vestibular schwannoma on gadolinium-enhanced MR images. Radiology. 1991;179:795–796. doi: 10.1148/radiology.179.3.2027994. [DOI] [PubMed] [Google Scholar]
- 17.Renowden SA, Anslow P. The effective use of magnetic resonance imaging in the diagnosis of acoustic neuromas. Clin Radiol. 1993;48:25–28. doi: 10.1016/s0009-9260(05)80102-3. [DOI] [PubMed] [Google Scholar]
- 18.Freije JE, Harvey SA, Haberkamp TJ. False-negative magnetic resonance imaging in the evaluation of facial nerve paralysis. Laryngoscope. 1996;106:239–242. doi: 10.1097/00005537-199602000-00026. [DOI] [PubMed] [Google Scholar]
- 19.Mark AS, Seltzer S, Nelson-Drake J, Chapman JC, Fitzgerald DC, Gulya AJ. Labyrinthine enhancement of gadolinium-enhanced magnetic resonance imaging in sudden deafness and vertigo: correlation with audiologic and electronystagmographic studies. Ann Otol Laryngol. 1992;101:459–464. doi: 10.1177/000348949210100601. [DOI] [PubMed] [Google Scholar]
- 20.Swartz JD. Sensorineural hearing deficit: a systematic approach based on imaging findings. Radiographics. 1996;16:561–574. doi: 10.1148/radiographics.16.3.8897624. [DOI] [PubMed] [Google Scholar]
- 21.Weissman JL, Curtin HD, Hirsch BE, Hirsch WL., Jr High signal from the otic labyrinth on unenhanced magnetic resonance imaging. AJNR. 1992;13:1183–1187. [PMC free article] [PubMed] [Google Scholar]