Abstract
Objective
To measure the effects of atypical antipsychotic medication on psychiatric and behavioral symptoms in patients with Alzheimer’s disease (AD) and psychosis or agitated behavior.
Method
The CATIE-AD effectiveness study included 421 outpatients with AD and psychosis or agitated/aggressive behavior. Patients were assigned randomly to masked flexible-dose treatment with olanzapine, quetiapine, risperidone, or placebo for up to 36 weeks. Patients could be re-randomized to a different medication treatment at the clinician’s discretion, which ended the Phase 1 period. Psychiatric and behavioral symptoms, functional abilities, cognition, care needs, and quality of life were measured at regular intervals.
Results
At the last observation in Phase 1 compared to placebo, there was greater improvement in patients treated with olanzapine or risperidone on the Neuropsychiatric Inventory total score, with risperidone on the Clinical Global Impression of Change, with olanzapine or risperidone on the Brief Psychiatric Rating Scale (BPRS) Hostile Suspiciousness factor, and with risperidone on the BPRS Psychosis factor. There was worsening with olanzapine on the BPRS Withdrawn Depression factor.
Among patients continuing Phase 1 treatment at 12 weeks, there were no significant antipsychotic – placebo group differences on measures of cognition, functional skills, care needs, or quality of life, except for worsening of functional skills in the olanzapine treatment group compared to placebo.
Conclusion
In this descriptive analysis of clinical outcomes in AD outpatients in usual care settings, some clinical symptoms improved with atypical antipsychotic treatment. Antipsychotic medications may be more effective for particular symptoms, such as anger, aggression, and paranoid ideas. Functional abilities, care needs, or quality of life do not appear to improve with antipsychotic treatment.
Introduction
Psychiatric and behavioral symptoms are common in patients with Alzheimer’s disease (AD) and contribute substantially to morbidity (1–3). Delusions or hallucinations appear in 30–50%, and as many as 70% demonstrate agitated or aggressive behaviors. These symptoms contribute to patient and caregiver distress (4, 5), can compromise safety or lead to institutionalization (6, 7), and add to healthcare costs (8, 9).
Optimal treatments for psychosis and agitated behavior have been elusive. Interventions that address environmental or interpersonal factors can be helpful (10, 11) and should be attempted in all cases, although their overall effectiveness and applicability are not entirely clear. Cholinesterase inhibitor drugs and memantine may have some beneficial impact on noncognitive symptoms in AD (12, 13), although effects may not be significant in those with active behavioral disturbances (14). The majority of controlled medication trials for psychosis and behavioral disturbances in AD have examined the efficacy of atypical antipsychotic medications over 6 to 12 weeks in patients with advanced disease. Several trials found modest efficacy of individual atypical antipsychotic medications compared to placebo (15). However, efficacy is not seen in all trials or for all symptoms, adverse events can occur, comparative efficacy is not known, and overall effectiveness in usual clinical populations is uncertain.
The National Institute of Mental Health (NIMH) Clinical Antipsychotic Trials of Intervention Effectiveness – Alzheimer’s Disease (CATIE-AD) project was designed to compare the effectiveness of antipsychotic medications and placebo in patients with AD and psychosis or agitated/aggressive behavior (16). In contrast to typical efficacy trials, CATIE-AD included outpatients in usual care settings, and assessed treatment effectiveness on several clinical outcome measures over a nine-month intervention period. Initial CATIE-AD treatment (olanzapine, quetiapine, risperidone, or placebo) was randomized and masked, yet the protocol allowed medication dose adjustments or switch to a different treatment based on the clinician’s judgment. The primary CATIE-AD Phase 1 outcome was time to discontinuation of the initially-assigned medication for any reason, intended as an overall measure of effectiveness that incorporated the judgments of patients, caregivers, and clinicians reflecting therapeutic benefits in relation to undesirable effects. The two primary hypotheses were: 1) there would be pairwise differences between the three antipsychotic treatment groups and the placebo group in the time to discontinuation for any reason, and 2) among those antipsychotics that were different from placebo, none would be inferior to the others. The results revealed no pairwise treatment differences in all-cause discontinuation. Benefits of olanzapine and risperidone, seen as longer time to discontinuation for lack of efficacy compared to placebo (Kaplan-Meier estimate of median time: olanzapine 22.1 weeks, quetiapine 9.1 weeks, risperidone 26.7 weeks, placebo 9.0 weeks), were offset by shorter time to discontinuation due to adverse effects in the antipsychotic groups (discontinuations due to intolerability: 24% olanzapine, 16% quetiapine, 18% risperidone, 5% placebo) (17).
This report presents results of the CATIE-AD Phase 1 clinical symptom measures. Here, the analysis examined pairwise differences between antipsychotic treatment groups and the placebo group on change in clinical symptoms at the last observation while taking the initially-assigned Phase 1 treatment. Additional analyses explored clinical symptom changes in the four treatment groups among those patients who continued the Phase 1 treatment for up to 12 weeks. This approach can help to characterize treatment effects on psychosis and behavioral symptoms, and also allows the principal CATIE-AD effectiveness outcome, treatment discontinuation, to be viewed in the context of symptom change.
Methods
Study design and participants
The CATIE-AD research design and methods have been described previously (16, 18). Forty-two clinical sites enrolled 421 patients who were randomized initially to masked treatment with olanzapine, quetiapine, risperidone, or placebo (2:2:2:3 ratio). The treating physician could adjust the dosage, as indicated clinically, over the 36 weeks of the trial. At any time after the first two weeks of treatment, the clinician could discontinue the initially assigned (Phase 1) medication due to insufficient efficacy, adverse effects, or other reason. At that point, Phase 1 ended and the patient could enter Phase 2 and be assigned randomly to masked treatment with an atypical antipsychotic medication that had not been assigned in Phase 1 or with citalopram. Patients could also go directly to an open-choice treatment.
To participate in the trial, patients met DSM-IV criteria for dementia of the Alzheimer’s type (19) or met NINCDS-ADRDA criteria for probable AD (20), after a thorough history, physical and cognitive examination, and laboratory assessment were completed. Enrolled patients were outpatients living at home or in an assisted-living facility, had a knowledgeable informant, and were ambulatory. Patients in skilled nursing homes were not included. Mini-Mental State Exam (MMSE) (21) score was 5 to 26. Entry criteria required that delusions, hallucinations, agitation, or aggression had occurred nearly every day over the previous week or intermittently over 4 weeks. Symptoms had to have been rated at least moderate in severity on the Brief Psychiatric Rating Scale (BPRS) conceptual disorganization, suspiciousness, or hallucinatory behavior item (22), or had occurred at least weekly with moderate severity or greater on the delusion, hallucination, agitation, or aberrant motor behavior item of the Neuropsychiatric Inventory (NPI) (23).
Patients could be taking stable cholinesterase inhibitor medication; memantine had not been approved in the U.S. during the enrollment period. Patients were excluded if they were taking antidepressants or anticonvulsants for mood stabilization.
The study was reviewed and approved by the Institutional Review Board (IRB) at each site. Consent was documented according to IRB guidelines.
Treatments
Medications were prepared in low-dose and high-dose identically-appearing capsules that contained either olanzapine (2.5mg or 5mg), quetiapine (25mg or 50mg), risperidone (0.5mg or 1mg), or placebo. The clinician selected the number of low- or high-dose capsules for initial treatment and could subsequently adjust the number of capsules prescribed according to clinical judgment. If difficult behaviors emerged acutely, the clinician could increase the study medication, prescribe a benzodiazepine for short-term use, or prescribe parenteral haloperidol for behavioral emergency.
Patients and caregivers received basic information and education about AD, behavioral symptoms, and behavioral management strategies. Caregivers were offered two counseling sessions and could speak with clinical staff as needed.
Clinical outcome measures
Two sets of clinical outcomes were measured:
1) Psychiatric and behavioral symptoms
were assessed at study baseline and after 2 weeks, 4 weeks, 8 weeks, 12 weeks, 24 weeks, and 36 weeks of treatment. Rating instruments were:
NPI
The NPI measures the frequency and severity of 12 psychiatric symptoms, based on caregiver report (23). The items are delusions, hallucinations, agitation/aggression, depression/dysphoria, anxiety, elation, apathy/indifference, disinhibition, irritability/lability, aberrant motor behavior, sleep disturbance, and appetite and eating disorder.
BPRS
The BPRS measures severity of 18 psychiatric and behavioral symptoms (22). Individual items were scored by a trained clinician after a semi-structured patient interview, and used additional information from the caregiver. Factor analysis in a geropsychiatry sample revealed a five-factor structure: Agitation (anxiety, tension, excitement); Hostile Suspiciousness (hostility, suspiciousness, uncooperativeness); Psychosis (unusual thought content, hallucinations); Withdrawn Depression (emotional withdrawal, depressed mood, motor retardation, blunted affect); and Cognitive Dysfunction (disorientation, conceptual disorganization) (24).
Cornell Scale for Depression in Dementia
The Cornell Scale is a 19-item instrument that measures mood symptoms, ideational disturbances of depression, and neurovegetative signs in patients with dementia (25). Items are rated based on patient report, caregiver report, and the rater’s observations of the patient.
AD Cooperative Study - Clinician’s Global Impression of Change (CGIC)
The CGIC is a global assessment of clinical change over time, based on the clinician’s overall impression of change in cognitive, behavioral, and functional symptoms (26). Change over time is rated on a 7-point scale from “very much improved” to “very much worse.”
2) Cognitive skills, functional abilities, care needs, and quality of life
were assessed at baseline, and after 12 weeks, 24 weeks, and 36 weeks of treatment. Rating instruments were:
AD Assessment Scale – Cognitive Subscale (ADAS-Cog) and MMSE
The 11-item ADAS-Cog assesses memory, language, visuoconstructive skill, and ideational praxis (27). The MMSE is a brief 30-item measure of global cognitive ability (21).
AD Cooperative Study – Activities of Daily Living Scale (ADCS-ADL)
The ADCS-ADL scale is a 23-item, hierarchically-scaled inventory of basic (e.g., eating, toileting, bathing) and instrumental (e.g., using the telephone, going shopping) functional skills and abilities (28). Ratings are based on an informant’s observations.
Dependence Scale
The Dependence Scale is a 13-item measure of the amount of caregiver assistance needed by the patient to accomplish daily activities (29) and has been used as a predictor of nursing home placement (7). Based on the Dependence Scale interview with an informant, the clinician rates the patient’s Equivalent Institutional Care (EIC) level: Level 1= Limited home care (needs some help with activities such as shopping or housekeeping); Level 2= Supervised adult home care (supervised setting with constant companionship and regular help with cooking and housekeeping); Level 3= Health-related facility (24-hour supervision for personal care and safety).
Caregiver Activity Scale
The Caregiver Activity Scale measures the time that caregivers spend providing care for a patient with AD (30). The time spent by care providers over the past 24 hours is recorded for each of five care-need domains: using transportation, dressing, eating, looking after one’s appearance, and general supervision. Caregiving time was the sum of time for the four specific domains, excluding general supervision.
Alzheimer’s Disease Related Quality of Life (ADRQL)
The ADRQL measures health-related quality of life in patients with AD, based on a structured interview with the caregiver (31). Items assess behaviors that reflect social interaction, maintained interests, participation in activities, cheerfulness, and freedom from distress. Forty-seven items in five domains (Social Interaction, Awareness of Self, Feelings and Mood, Enjoyment of Activities, Response to Surroundings) are rated and the total score is a weighted sum of the item scores.
Data analysis
The intent-to-treat sample included those patients who were assigned randomly to a treatment group (n=421) and received at least one dose of study medication (n=416). Discontinuation from Phase 1 occurred when the study physician judged that the patient’s response to the assigned medication was not adequate due to insufficient efficacy, adverse effects, or other reason, or the patient or family chose to discontinue the treatment. This report presents the clinical outcome measures during Phase 1 treatment.
For the psychiatric and behavioral symptom measures, the primary analysis was the difference in change scores between the antipsychotic treatment groups and the placebo treatment group at the last observation in Phase 1. The last observation analysis was chosen because of the substantial percentage of patients who discontinued Phase 1 treatment, in order to provide a concise summary of patient status immediately prior to discontinuation. Pairwise comparisons of each antipsychotic vs. placebo were evaluated using an analysis of covariance (ANCOVA), adjusting for pooled site and the baseline rating scale score. Pairwise comparisons used a Hochberg modification of the Bonferroni adjustment for multiple comparisons (32), in which the largest of the p-values is compared to 0.05 and the smallest is compared to 0.05/3=0.017. An additional descriptive analysis also compared the active treatments to one another. If a 2 degree of freedom test comparing the 3 antipsychotic treatment groups had p< 0.05, then pairwise comparisons among the active treatments were performed, also using the Hochberg adjustment for multiple comparisons. A further sensitivity analysis for key outcomes also adjusted for the duration of treatment in Phase 1, since patients discontinued Phase 1 at various times, and the NPI baseline score, which was found to be different across the groups at baseline. ANCOVA analyses for the CGIC were confirmed by an analysis of the distribution of ordinal CGIC scores at the last observation using a Mantel-Haenszel mean score chi-square test for ordinal data.
A confirmatory mixed model repeated measures analysis was also performed for change from baseline on two measures: the NPI total score and BPRS total score. This strategy compares treatment groups across all time points together; it assumes that missing data from subjects who discontinued can be represented by subjects who remained in the phase at that visit. The model had fixed effects for treatment, baseline value, classification of time (weeks 2, 4, 8, and 12), the interaction between baseline value and time and between treatment and time, if significant, and used a random patient intercept and spatial power covariance structure to account for the correlation of the repeated measurements within a subject. The mixed model excluded visits after week 12 because the sample sizes declined substantially at later visits.
Finally, a secondary set of ANCOVA analyses compared treatment groups at each of weeks 2, 4, 8, and 12 (observed-case), in order to further characterize the response patterns for those patients who had not yet discontinued by that visit. The distribution of ordinal CGIC scores across the treatment groups for observed cases at week 12 was also assessed using a Mantel-Haenszel mean score chi-square test for ordinal data. For descriptive purposes, the proportion responders in the treatment groups were calculated, where those with CGIC score of “much improved” or “very much improved” at week 12 were considered responders. This approach is different from the previous analysis (17) that included the entire intent-to-treat sample, defined a response as at least “minimal improvement” on the CGIC, and considered all patients who ended Phase 1 prior to week 12 to be “nonresponders”. The current analysis of observed cases continuing on Phase 1 treatment at week 12 used the higher threshold for response, because this group tended to have fewer symptoms since those with more symptoms were more likely to have ended Phase 1 prior to week 12.
For measures of cognition, functional skills, and care needs, which were completed only at weeks 12, 24, and 36, change scores were examined with ANCOVA only for observed cases who were continuing the Phase 1 assigned treatment at week 12. Scores on these measures at the last observation during Phase 1 were often not available because a high proportion of patients had discontinued Phase 1 prior to week 12 and thus had no post-baseline assessment.
Results
Patient characteristics and treatment
Patient characteristics, treatments prescribed, time to Phase 1 discontinuation, and adverse events were reported previously (17, 33). Mean age of participants was 77.9 (SD 7.5) years; 56% were female; 21% were non-white. Overall, 77–85% of patients discontinued the Phase 1 medication treatment prior to the end of the 36-week study period. The median duration of Phase 1 treatment was 7.1 weeks and did not differ significantly across the treatment groups (median duration ranged from 5.3 to 8.1 weeks in the four groups). The mean last prescribed medication dose was 5.5 mg/day of olanzapine, 56.5 mg/day of quetiapine, and 1.0 mg/day of risperidone. There was no difference in the numbers or sizes of capsules prescribed across treatments. Rescue medications were prescribed rarely and there were no significant differences among treatment groups: 3/421 patients were prescribed a conventional antipsychotic and 21/421 patients were prescribed a benzodiazepine (three in olanzapine group, eight in quetiapine group, three in risperidone group, and seven in placebo group).
Clinical symptoms at baseline
The baseline scores on clinical symptom measures are shown in Table 1. There was no difference on any baseline symptom score across the treatment groups, except for NPI total score (p=0.02; ANOVA).
Table 1.
Baseline scores on clinical measures in CATIE-AD (randomized patients).
| Olanzapine N=100 | Quetiapine N=94 | Risperidone N=85 | Placebo N=142 | Total N=421 | |
|---|---|---|---|---|---|
| Clinical Measure | |||||
| NPI Total Score* | 31.8 (16.3) | 37.6 (18.4) | 38.3 (20.2) | 39.1 (17.8) | 36.9 (18.3) |
| BPRS Total Score | 27.0 (11.8) | 28.0 (12.3) | 27.7 (13.6) | 28.2 (12.0) | 27.8 (12.3) |
| Hostile Suspiciousness Factor | 2.1 (1.2) | 2.2 (1.3) | 2.2 (1.3) | 2.3 (1.2) | 2.2 (1.3) |
| Psychosis Factor | 1.7 (1.5) | 2.0 (1.4) | 2.0 (1.6) | 1.8 (1.5) | 1.9 (1.5) |
| Agitation Factor | 1.7 (1.2) | 1.7 (1.1) | 1.6 (1.3) | 1.7 (1.1) | 1.7 (1.2) |
| Withdrawn Depression Factor | 1.3 (0.9) | 1.2 (0.9) | 1.3 (1.0) | 1.2 (0.9) | 1.2 (0.9) |
| Cognitive Dysfunction Factor | 2.6 (1.1) | 2.7 (1.2) | 2.7 (1.3) | 2.7 (1.2) | 2.7 (1.2) |
| Cornell Depression Scale | 8.8 (5.4) | 9.8 (5.5) | 10.3 (5.4) | 10.6 (5.6) | 9.9 (5.5) |
| ADAS-Cog | 34.6 (12.7) | 36.1 (13.6) | 31.1 (13.6) | 35.7 (13.2) | 34.6 (13.3) |
| MMSE | 15.0 (5.4) | 14.9 (6.1) | 15.7 (6.1) | 14.7 (5.8) | 15.0 (5.8) |
| ADCS ADL Total | 39.4 (17.4) | 39.0 (17.8) | 40.0 (18.1) | 38.2 (16.3) | 39.0 (17.2) |
| Equivalent Institutional Care | |||||
| Limited home care (%) | 30% | 29% | 27% | 21% | 26% |
| Supervised adult home (%) | 47% | 55% | 60% | 64% | 57% |
| Health-related facility (%) | 23% | 16% | 13% | 15% | 17% |
| ADRQL Total | 69.2 (14.6) | 66.9 (13.2) | 68.1 (16.3) | 65.7 (14.6) | 67.3 (14.7) |
| Caregiver Activity Survey (time in hours) | 5.1 (4.7) | 4.8 (3.1) | 5.0 (6.4) | 5.7 (4.6) | 5.2 (4.8) |
Values shown are mean score (SD), except for Caregiver Activity Survey (value is mean hours per day, excluding hours spent in general supervision) and Equivalent Institutional Care (value is percent needing specified level of care)
p=.02 for the overall comparison of treatment groups, one-way ANOVA
Clinical symptom scores – Change from baseline to the last observation in Phase 1 (Table 2)
Table 2.
Change in clinical symptoms from baseline to last observation in phase 1 (Intent-to-treat sample)‡
| Outcome | Olanzapine N† = 99 | Quetiapine N = 94 | Risperidone N = 84 | Placebo N = 139 | P Value (overall comparison) |
|---|---|---|---|---|---|
| NPI total score, mean change (SD) | −7.0 (18.1) | −7.3 (20.2) | −11.6 (15.4) | −4.2 (20.0) | 0.004 |
| Comparisons vs. Placebo, LS Mean Difference | −6.3 | −4.0 | −8.2 | --- | |
| [95% CI]# | [−10.8, −1.7] | [−8.7, 0.7] | [−13.0, −3.4] | ||
| P-value | P = 0.007* | P = 0.097 | P < 0.001* | ||
| CGIC, mean score (SD) | 3.9 (1.5) | 3.8 (1.5) | 3.5 (1.4) | 4.2 (1.3) | 0.005 |
| Comparisons vs. Placebo, LS Mean Difference | −0.36 | −0.43 | −0.70 | --- | |
| [95% CI]# | [−0.73, 0.01] | [−0.81, −0.04] | [−1.10, −0.30] | ||
| P-value | P = 0.057 | P = 0.031 | P < 0.001* | ||
| BPRS total score, mean change (SD) | −2.9 (11.8) | −4.2 (9.2) | −4.3 (9.2) | −2.9 (10.0) | 0.387 |
| Comparisons vs. Placebo, LS Mean Difference | −0.6 | −1.6 | −2.0 | --- | |
| [95% CI]# | [−3.0, 1.8] | [−4.1, 0.9] | [−4.5, 0.6] | ||
| P-value | P = 0.623 | P = 0.203 | P = 0.125 | ||
| BPRS Hostile Suspiciousness factor score, mean change (SD) | −0.6 (1.3) | −0.5 (1.3) | −0.7 (1.2) | −0.3 (1.2) | 0.010 |
| Comparisons vs. Placebo, LS Mean Difference | −0.4 | −0.3 | −0.5 | --- | |
| [95% CI]# | [−0.7, −0.1] | [−0.6, 0.0] | [−0.8, −0.2] | ||
| P-value | P = 0.006* | P = 0.072 | P = 0.003* | ||
| BPRS Psychosis factor score, mean change (SD) | −0.3 (1.6) | −0.4 (1.2) | −0.7 (1.3) | −0.2 (1.3) | 0.078 |
| Comparisons vs. Placebo, LS Mean Difference | −0.2 | −0.2 | −0.5 | --- | |
| [95% CI]# | [−0.5, 0.1] | [−0.5, 0.2] | [−0.8, −0.1] | ||
| P-value | P = 0.199 | P = 0.352 | P = 0.010* | ||
| BPRS Agitation factor score, mean change (SD) | −0.4 (1.2) | −0.3 (1.0) | −0.2 (1.1) | −0.1 (1.0) | 0.085 |
| Comparisons vs. Placebo, LS Mean Difference | −0.3 | −0.2 | −0.2 | --- | |
| [95% CI]# | [−0.5, 0.0] | [−0.5, 0.0] | [−0.5, 0.0] | ||
| P-value | P = 0.021 | P = 0.078 | P = 0.082 | ||
| BPRS Withdrawn Depression factor score, mean change (SD) | 0.2 (1.0) | −0.1 (0.8) | 0.1 (0.9) | −0.1 (0.8) | 0.010 |
| Comparisons vs. Placebo, LS Mean Difference | 0.3 | 0.0 | 0.2 | --- | |
| [95% CI]# | [0.1, 0.5] | [−0.2, 0.2] | [0.0, 0.4] | ||
| P-value | P = 0.003* | P = 0.987 | P = 0.088 | ||
| BPRS Cognitive Dysfunction factor score, mean change (SD) | 0.1 (0.9) | 0.0 (0.9) | −0.1 (0.9) | −0.1 (1.0) | 0.143 |
| Comparisons vs. Placebo, LS Mean Difference | 0.2 | 0.1 | 0.0 | --- | |
| [95% CI]# | [0.0, 0.4] | [−0.2, 0.3] | [−0.2, 0.2] | ||
| P-value | P = 0.036 | P = 0.603 | P = 0.932 | ||
| Cornell Depression Scale total score, mean change (SD) | −0.9 (5.8) | −0.8 (5.5) | −2.0 (5.3) | −1.2 (4.5) | 0.643 |
| Comparisons vs. Placebo, LS Mean Difference | −0.4 | −0.1 | −0.8 | --- | |
| [95% CI]# | [−1.5, 0.8] | [−1.4, 1.1] | [−2.0, 0.5] | ||
| P-value | P = 0.533 | P = 0.841 | P = 0.216 | ||
Change score <0 reflects clinical improvement on each measure in this Table. P-value and differences of Least Squares mean are based on ANCOVA model with adjustment for pooled site and baseline value. P-value (overall comparison) is for the overall 3 degree of freedom F test for treatment group; P-values in each medication group column are for medication-placebo comparisons.
Some patients discontinued prior to assessment, so the actual sample size used in the last observation analysis is lower (Olanzapine 97, Quetiapine 84, Risperidone 77, and Placebo 130). N varies slightly by score; reported N here is for CGIC. Range (min,max) per treatment is as follows: Olanzapine (94,97), Quetiapine (82,84), Risperidone (76,78), Placebo (129,130).
P-value for comparison vs. placebo is significant at 0.05 in accordance with the Hochberg adjustment for multiple comparisons.
CI denotes confidence interval.
Global symptom measures
On the NPI total score, patients treated with olanzapine or risperidone showed greater improvement from baseline at the last Phase 1 observation than those treated with placebo (olanzapine p=0.007; risperidone p<0.001). On the CGIC, patients treated with risperidone had greater global improvement than those in the placebo group (p<0.001). Overall group differences were confirmed in an analysis of the distribution of ordinal CGIC scores at the last observation in Phase 1 (p=.007; Mantel-Haenszel mean score chi-square test for ordinal data). Improvement on the BPRS total score at last observation was no different in those treated with antipsychotic medication from those treated with placebo. Including baseline NPI total score and the duration of Phase 1 treatment as additional covariates in the ANCOVA model did not impact these results.
Individual symptom measures - BPRS factors and Cornell Depression Scale
Patients treated with olanzapine or risperidone showed greater improvement on the BPRS Hostile Suspiciousness factor at the end of Phase 1 than those treated with placebo (olanzapine p=0.006; risperidone p=0.003). Patients treated with risperidone had greater improvement on the BPRS Psychosis factor than those treated with placebo (p=0.010). On the BPRS Withdrawn Depression factor, patients treated with olanzapine showed worsening of symptoms compared to placebo (p=0.003). There was no difference in those treated with antipsychotic medication compared to placebo on the BPRS Cognitive Dysfunction factor or the Cornell Depression Scale.
Clinical symptom scores – repeated measures analysis
The mixed model analysis of both the NPI and BPRS total score change for time points between baseline and week 12 found no overall time-by-treatment interaction. The reduced model without this interaction term, which compared the treatment groups across the average of all time-points, revealed an overall effect of treatment group (mixed model, repeated measures, df=3; NPI: p=.03; BPRS: p=.04), with a significant pairwise difference between risperidone and placebo treatment (NPI: estimated mean difference=5.7, SE 1.9, p=.003; BPRS: estimated mean difference=2.9, SE 1.1, p=.007).
Clinical symptom scores – Change from baseline to week 12, observed cases in Phase 1
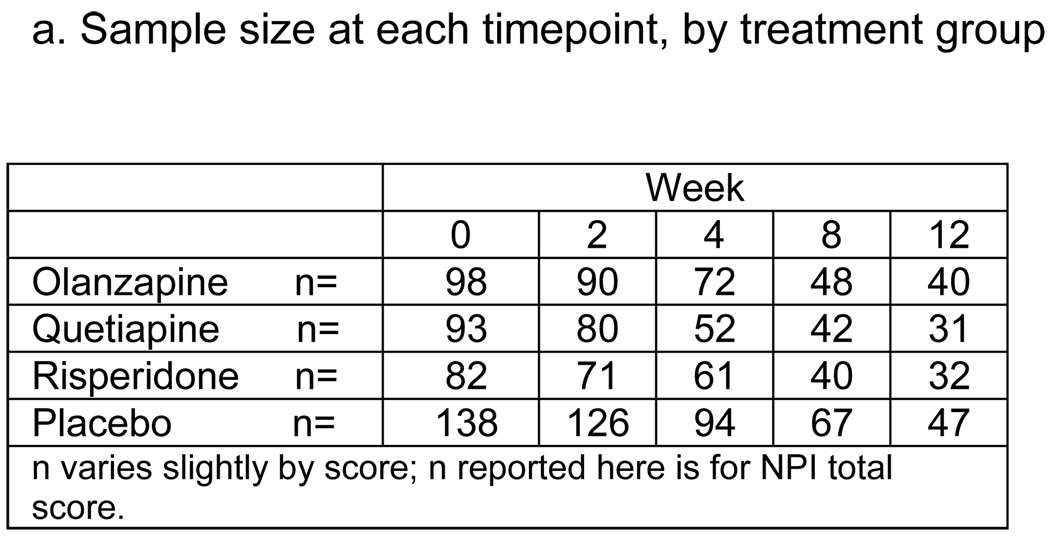
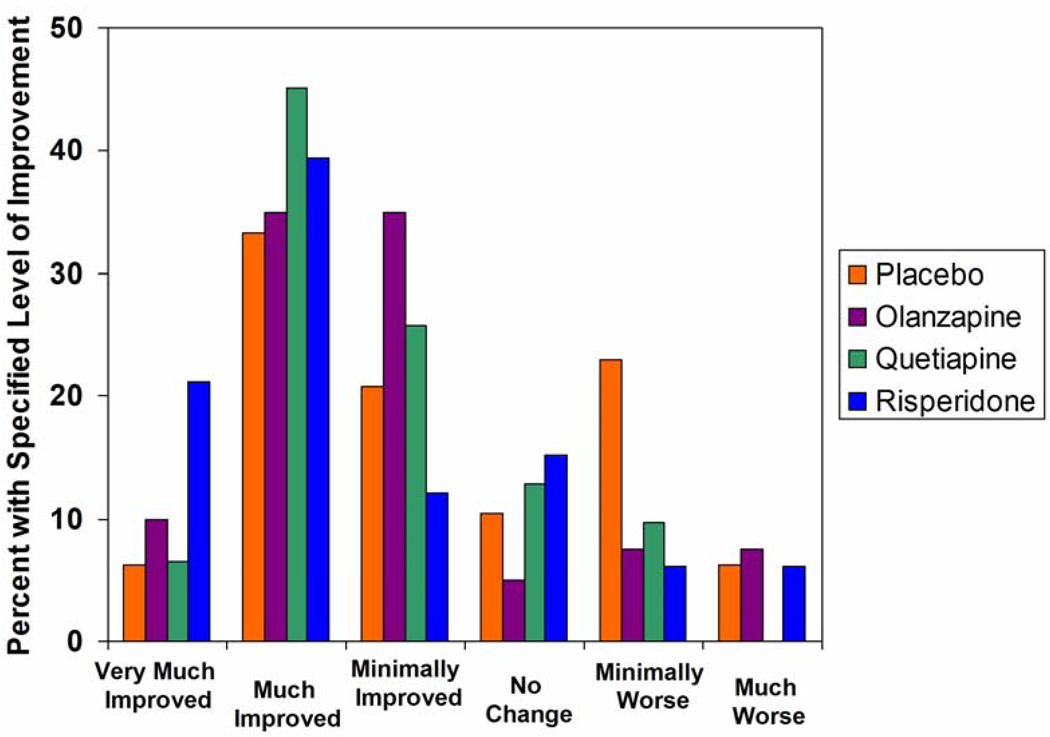
Mean change scores on the NPI total, BPRS total, and BPRS factors over 12 weeks of Phase 1 treatment are shown in Figure 1. Only patients continuing on the assigned Phase 1 treatment were included at each time point, so sample sizes declined over the 12 week period (Figure 1a). Change over time among observed cases seen on these curves generally supports the results of the last observation and mixed model analyses.
Figure 1.
Change on clinical symptom measures between baseline and treatment week 12. ^
^ Mean change scores for those patients continuing to take the assigned phase 1 medication at week 2, 4, 8, and 12 (observed cases at each timepoint) are shown. Change scores <0 reflect clinical improvement. Standard error bars are shown for week 12 results.
Pairwise comparisons of least squares mean change score for each antipsychotic group vs. placebo group at each timepoint are shown here for descriptive purposes: *p<.05, **p<.01 (ANCOVA, adjusted for baseline score and pooled site, no adjustment for multiple comparisons). Significant pairwise comparisons between antipsychotic treatment groups are provided in the text.
Discrepancies between the magnitude of between-group differences shown on the graphs and the results of antipsychotic-placebo pairwise comparisons are due to differences between observed means and least squares means, which adjust for baseline score and site variations.
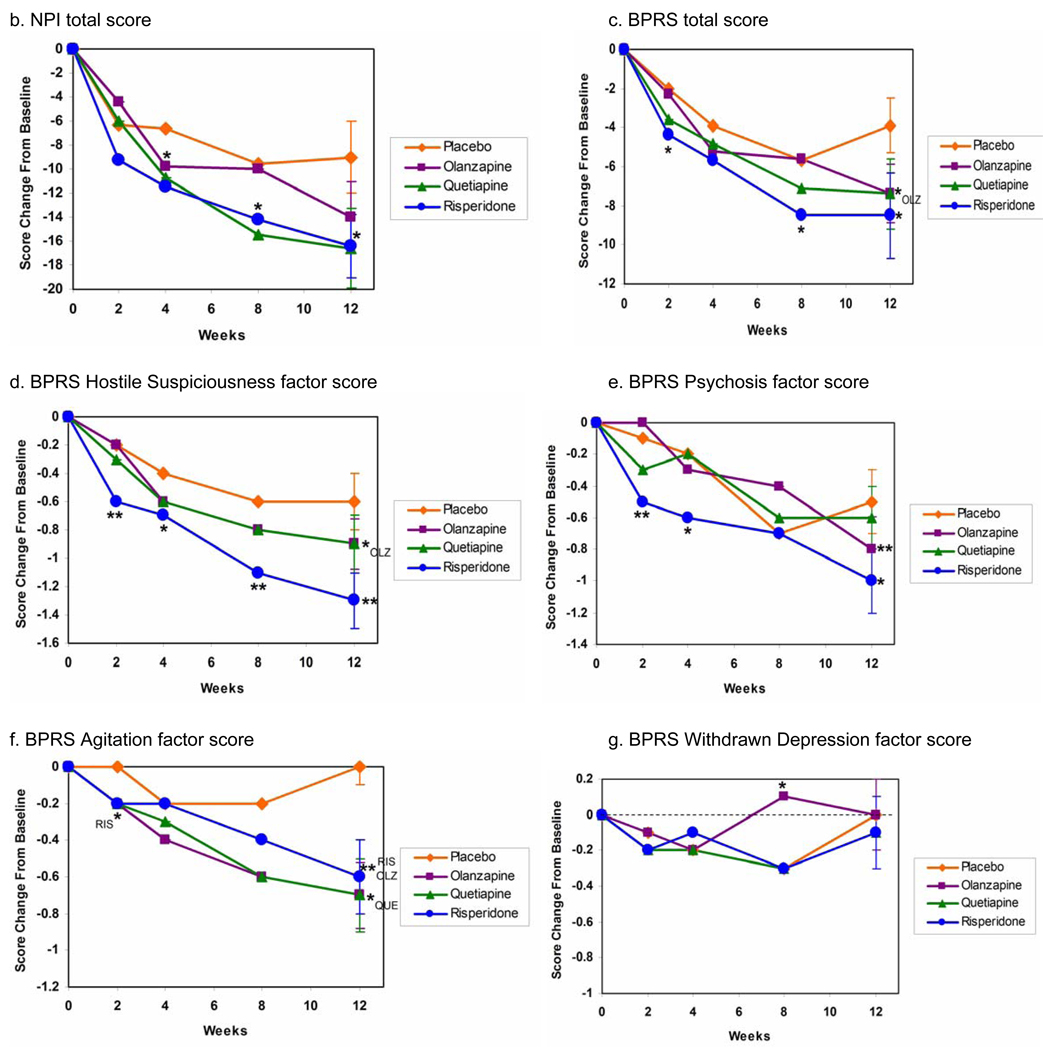
The distribution of CGIC scores in observed cases after 12 weeks of treatment (Figure 2) was not significantly different between the groups (p=.14). The proportion of patients with CGIC score of “much improved” or “very much improved” was 45%, 52%, 61%, and 40% in the olanzapine, quetiapine, risperidone, and placebo groups respectively.
Figure 2.
Distribution of CGI-C scores after 12 weeks of treatment in Phase 1.
Structured ratings of functional abilities, care needs, cognitive skills, and quality of life were assessed only at baseline and week 12 during the CATIE-AD early treatment period. On the ADCS-ADL scale, patients in the olanzapine treatment group showed worsening of functional ability compared to those in the placebo group at week 12 (p<0.001) (Table 3). Change scores were no different at week 12 in those treated with an antipsychotic medication compared to those treated with placebo on the ADAS-Cog, MMSE, ADRQL, or Caregiver Activity Survey. On the Equivalent Institutional Care rating, there was no overall difference among the treatment groups in change in the level of care from baseline to week 12.
Table 3.
Change on clinical symptom measures between baseline and treatment week 12. ^
| Olanzapine (N = 40) | Quetiapine (N = 31) | Risperidone (N = 33) | Placebo (N = 47) | |
|---|---|---|---|---|
| ADCS-ADL total score, mean change (SD) | −6.1 (8.2) * | −1.0 (7.7) | −1.1 (8.8) | 0.5 (8.4) |
| ADAS-Cog total score, mean change (SD) | 0.7 (6.1) | 0.8 (6.9) | 1.7 (5.2) | 1.3 (5.7) |
| MMSE score, mean change (SD) | −0.1 (3.7) | −0.8 (3.8) | −0.8 (3.2) | −0.7 (2.7) |
| ADRQL total score, mean change (SD) | 6.4 (12.6) | 6.7 (11.7) | 2.1 (12.1) | 4.1 (15.8) |
| Caregiver Activity Survey, mean change in hours (SD) | 0.2 (4.8) | −0.7 (4.3) | −1.1 (4.7) | −0.6 (4.1) |
Mean change score for those patients taking the assigned phase 1 medication at week 12 are shown.
For ADCS-ADL, MMSE, and ADRQL, a change score >0 reflects clinical improvement. For ADAS-Cog and Caregiver Activity Survey, a change score <0 reflects clinical improvement.
p<.001, pairwise comparison vs. placebo; ANCOVA model with adjustment for pooled site and baseline score.
Clinical symptom scores – active drug comparisons
At the last observation in Phase 1, there were no differences among the three antipsychotic treatment groups on any clinical outcome measure, except the BPRS Withdrawn Depression factor (overall antipsychotic treatment group comparison: df=2, p=.031; olanzapine group showed worsening of symptoms compared to quetiapine group: LS mean difference=0.3, p=.009).
In the analysis of observed cases at weeks 2, 4, 8, and 12, there were no differences among the three antipsychotic treatment groups on any clinical outcome measure at any time point, except 1) on the BPRS Withdrawn Depression factor at week 8 (overall antipsychotic treatment group comparison: df=2, p=.012; olanzapine group showed worsening of symptoms compared to quetiapine group [LS mean difference=0.4, p=.010] and risperidone group [LS mean difference=0.4, p=.012]), and 2) on the ADCS-ADL scale at week 12 (overall antipsychotic treatment group comparison: df=2, p=.015); olanzapine group showed a greater decline (worsening) compared to quetiapine group [LS mean difference=−5.2, p=.015] and risperidone group [LS mean difference=−5.4, p=.011]).
Discussion
Several clinical outcome measures in CATIE-AD indicate that patients may benefit symptomatically from treatment with atypical antipsychotic medications. Beneficial effects of olanzapine and risperidone were apparent on the NPI total score, a summary measure of psychiatric and behavioral symptoms. Improvement on the clinician-rated CGIC global rating in the risperidone group provides convergent support for the improvements on symptom scores.
The magnitude of mean global score improvements with active medication compared to placebo was usually small. Significant group differences were not seen on the BPRS total score at the last observation, although the mixed model analysis revealed a significant effect of risperidone vs. placebo, with a larger estimated mean difference in the mixed model than was measured at the last Phase 1 observation. Some analyses revealed pairwise group differences that were near the statistical threshold for significance after adjustment for multiple comparisons, suggesting that while group differences cannot be excluded their magnitude is small. In contrast, other group differences were probably clinically meaningful. For example, the mean baseline NPI total score (36.9) was improved at the last observation in Phase 1 by 11.6 points in the risperidone group and 7.0 points in the olanzapine group, compared to 4.2 points in the placebo group. Also, the CGIC ratings at last observation in Phase 1 and at 12 weeks indicate that some individuals were likely benefiting from antipsychotic treatment. Beneficial effects of quetiapine compared to placebo did not appear on most CATIE-AD symptom outcomes, although Figure 1 indicates that a quetiapine effect cannot be entirely ruled out. Limited quetiapine impact on symptoms may have been due to the low dose of quetiapine prescribed. However, sedation occurred in this group at rates comparable to the other drugs (17), suggesting at least some medication effect. Use of rescue medication (haloperidol, lorazepam) did not likely contribute to clinical outcomes, since these medications were prescribed rarely and equally across the treatment groups (17).
These clinical symptom ratings in CATIE-AD complement and extend the findings from the primary effectiveness analysis that showed benefits of olanzapine and risperidone reflected in longer time to discontinuation due to lack of efficacy, which were offset by discontinuations due to adverse effects (17). The clinical symptoms ratings reported here also show some antipsychotic efficacy during Phase 1, yet these improved last observation ratings occurred at or very near the time when the clinician decided that Phase 1 treatment was not optimal and intended to change the treatment, except for the 19% of patients who completed the entire study on Phase 1. Notably, Phase 1 discontinuations were due predominantly to insufficient efficacy. Thus, clinical symptom ratings reveal some beneficial antipsychotic effects, despite the frequent coincident decision to change treatment. This distinction suggests that clinicians were seeking a level of clinical improvement that was greater than the change detected on the clinical scales, were mindful of possible placebo assignment in Phase 1, or were balancing symptom change with other clinical considerations such as adverse effects. Treatment expectations and patient circumstances likely contributed to the perception of effectiveness. As applied to clinical practice, these findings support an individualized approach, where the value of an individual patient’s symptomatic improvement needs to be assessed in the context of that person’s particular clinical circumstances.
The analyses that used the last clinical rating in Phase 1 are conceptually different from the descriptive analyses that used scores from observed cases continuing Phase 1 treatment through week 12. The last observation analysis includes a preponderance of data from patients who, for a variety of reasons, were not doing particularly well on the assigned treatment. By contrast, the results from observed cases continuing on Phase 1 treatment apply to those who are doing reasonably well on their first prescribed medication, because Phase 1 would have ended earlier for these patients had the clinicians felt the assigned treatment was not overall effective. This is reflected in the larger improvement from baseline generally seen in all treatment groups among observed cases at week 12 compared to the last observation sample. Despite this important difference, the results using the two analytic approaches are not substantially different.
The BPRS factor scores provide a view of antipsychotic treatment effects on distinct symptoms. Patients treated with risperidone or olanzapine showed improvement on the BPRS Hostile Suspiciousness factor, which assesses hostility, aggression, mistrust, and uncooperativeness. This subscale had the highest mean score at baseline among noncognitive measures, and the mean score improved by more than 50% in the risperidone group in those continuing Phase 1 treatment at week 12. The BPRS Psychosis Factor score also improved with risperidone treatment. In contrast, antipsychotic treatment effects on the BPRS Agitation Factor score, which includes excitability, tension, and anxiety, were not as robust. This observation conforms to some clinical opinion that antipsychotics might be particularly useful for suspicious thoughts, paranoid delusions, and hostile or aggressive behaviors that occur commonly in AD.
On measures of depression or cognition, the magnitude of changes was small and there were no differences across treatments except for increased symptoms in the olanzapine group on the BPRS Withdrawn Depression factor at last observation in Phase 1. Taken together, these findings suggest that antipsychotic medication may have differential effects on specific symptoms in AD. Better understanding of specific effects can help clinicians to select optimal pharmacotherapy.
Beneficial effects were not apparent on measures of functional abilities, quality of life, or caregiving time needed. Thus, improved clinical symptoms with antipsychotic treatment did not translate to functional benefits or improved quality of life in the context of the CATIE-AD effectiveness design. This may be due to additional factors that contribute to functional disability and poor life quality, such as progression of dementia, caregiver interactions, environmental factors, and perhaps adverse effects of the drugs. Nonetheless, improved psychiatric and behavioral symptoms may be clinically meaningful for individual patients without impacting function.
There are several limitations to the study design and analyses. CATIE-AD did not follow a usual clinical efficacy trial design and while the effectiveness design has several advantages, results of these analyses should be interpreted carefully. For example, the end of Phase 1 is not defined by a specific time point, but the clinician’s judgment that continued treatment with the assigned medication is not optimal. The protocol invited medication switches based on clinical judgment and, in fact, Phase 1 treatment was often discontinued relatively quickly. In this respect, CATIE-AD results reflect clinician expectations and behaviors as well as pharmacologic efficacy. Also, the brief treatment exposure for many patients may not have captured all beneficial or adverse medication effects. Moreover, mild sedation may have contributed to behavioral improvement with antipsychotic treatment, but its specific role cannot be defined. Finally, the data analyses included many measures and comparisons, and there was no adjustment to statistical testing for the number of parameters evaluated overall.
The results presented here are predominantly group mean scores on clinical rating instruments, and this approach can obscure important treatment effects in individual patients. Subgroups of participants may respond to individual treatments particularly well or particularly poorly, as a result of distinct neurobiological factors (34), baseline symptom patterns, or sensitivity to treatment. Additional research is needed to clarify patient- or symptom-specific responses in order to maximize benefit and minimize harm of any available treatment.
The clinical outcomes in CATIE-AD contribute to the evolving understanding of psychopharmacological interventions for psychiatric symptoms in AD. Some antipsychotic efficacy trials and these analyses indicate that clinical symptoms may improve. The extent of mean improvement on rating scales is modest, however, it is not apparent for all symptoms or in all treatment studies, and beneficial effects on mean ratings of functional ability, quality of life, or cost-effectiveness (35) were not seen in CATIE-AD. Due to the unique design, the results of CATIE-AD are probably more generalizable to usual outpatient clinical settings than results from efficacy trials. Whether the potentially beneficial effects of symptom reduction with antipsychotic treatment outweigh other undesirable clinical or adverse effects depends on an individual patient’s circumstances, including severity of symptoms, vulnerability to adverse effects, and the effectiveness or opportunity for behavioral interventions. Additional studies to understand better the risk/benefit profile and effectiveness of specific treatments in individual patients will be valuable.
Acknowledgments
Supported by a research contract from the National Institute of Mental Health (N01 MH9001) and supported in part by the Department of Veterans Affairs. Astra-Zeneca Pharmaceuticals, Forest Pharmaceuticals, Janssen Pharmaceutica, and Eli Lilly provided medications for the study.
Author’s Disclosure of Competing Interests
Dr. Sultzer has received research funding from Forest Research Institute and Pfizer; lecture honorarium from Forest Laboratories; and has consulted to Eli Lilly and AstraZeneca.
Dr. Davis is employed by Quintiles, Inc.
Dr. Tariot has received consulting fees from AstraZeneca, Eisai Inc., Forest Laboratories, Pfizer Inc, and Sanofi-Aventis; consulting fees and research support from Abbott Laboratories, GlaxoSmithKline, Merck and Co., Merz, Takeda Pharmaceuticals, and Wyeth; and educational fees from Lundbeck.
Dr. Lyketsos has received research funding from Forest, GlaxoSmithKline, Eisai, Pfizer, Astra-Zeneca, Eli Lilly, Ortho-McNeil, Bristol-Myers Squibb, and Novartis; lecture honoraria or travel support from Pfizer, Forest, and GlaxoSmithKline; and has served as consultant/advisor to Astra-Zeneca, GlaxoSmithKline, Eisai, Novartis, Forest, Supernus Phramaceuticals, Adlyfe Inc., Takeda Pharmaceuticals, and Wyeth.
Dr. Rosenheck has received research support from Eli Lilly, Janssen Pharmaceutica, Astra-Zeneca, and Wyeth; and has consulted to GlaxoSmithKline, Bristol-Myers Squibb, Janssen Pharmaceutica, and Organon.
Dr. Lieberman has received research funding from Acadia, Bristol-Myers Squibb, GlaxoSmithKline, Janssen Pharmaceutica, Merck, Organon, and Pfizer; and has participated as consultant or advisory board member for Astra-Zeneca, Eli Lilly, GlaxoSmithKline, Lundbeck, Organon, and Pfizer.
Dr. Schneider has consulted to Pfizer, Eli Lilly, Johnson & Johnson, Astra-Zeneca, and Bristol-Myers Squibb.
Ms. Dagerman, Dr. Lebowitz, and Dr. Hsiao report no competing interests.
Footnotes
The content of this article does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government.
ClinicalTrials.gov number NCT00015548
References
- 1.Lyketsos CG, Steinberg M, Tschanz JT, Norton MC, Steffens DC, Breitner JC. Mental and behavioral disturbances in dementia: findings from the Cache County study on memory in aging. Am J Psychiatry. 2000;157:708–714. doi: 10.1176/appi.ajp.157.5.708. [DOI] [PubMed] [Google Scholar]
- 2.Ropacki SA, Jeste DV. Epidemiology of and risk factors for psychosis of Alzheimer's Disease: a review of 55 studies published from 1990–2003. Am J Psychiatry. 2005;162:2022–2030. doi: 10.1176/appi.ajp.162.11.2022. [DOI] [PubMed] [Google Scholar]
- 3.Lopez OL, Becker JT, Sweet RA, Klunk W, Kaufer DI, Saxton J, Habeych M, DeKosky ST. Psychiatric symptoms vary with the severity of dementia in probable Alzheimer's disease. J Neuropsychiatry Clin Neurosci. 2003;15:346–353. doi: 10.1176/jnp.15.3.346. [DOI] [PubMed] [Google Scholar]
- 4.Craig D, Mirakhur A, Hart DJ, McIlroy SP, Passmore AP. A cross sectional study of neuropsychiatric symptoms in 435 patients with Alzheimer's disease. Am J Geriatr Psychiatry. 2005;13:460–468. doi: 10.1176/appi.ajgp.13.6.460. [DOI] [PubMed] [Google Scholar]
- 5.Schulz R, O'Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: prevalence, correlates and causes. The Gerontologist. 1995;35:771–791. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- 6.Magni E, Binetti G, Bianchetti A, Trabucchi M. Risk of mortality and institutionalization in demented patients with delusions. J Geriatr Psychiatry Neurol. 1996;9:123–126. doi: 10.1177/089198879600900303. [DOI] [PubMed] [Google Scholar]
- 7.Stern Y, Tang M-X, Albert MS, Brandt J, Jacobs DM, Bell K, Marder K, Sano M, Devanand D, Albert SM, Bylsma F, Tsai W-Y. Predicting time to nursing home care and death in individuals with Alzheimer disease. JAMA. 1997;227:806–812. [PubMed] [Google Scholar]
- 8.Murman DL, Chen Q, Powell MC, Kuo SB, Bradley CJ, Colenda CC. The incremental direct costs associated with behavioral symptoms in Alzheimer's disease. Neurology. 2002;59:1721–1729. doi: 10.1212/01.wnl.0000036904.73393.e4. [DOI] [PubMed] [Google Scholar]
- 9.Ryu S, Katoma C, Rive B, Livingston G. Persistence of and changes in neuropsychiatric symptoms in Alzheimer's disease over 6 months. Am J Geriatr Psychiatry. 2005;13:976–983. doi: 10.1176/appi.ajgp.13.11.976. [DOI] [PubMed] [Google Scholar]
- 10.Livingston G, Johnston K, Katona C, Paton J, Lyketsos CG. Systematic review of psychological approaches to the management of neuropsychiatric symptoms of dementia. Am J Psychiatry. 2005;162:1996–2021. doi: 10.1176/appi.ajp.162.11.1996. [DOI] [PubMed] [Google Scholar]
- 11.Ayalon L, Gum AM, Feliciano L, Arean PA. Effectiveness of nonpharmacological interventions for the management of neuropsychiatric symptoms in patients with dementia. Archives of Internal Medicine. 2006;166:2182–2188. doi: 10.1001/archinte.166.20.2182. [DOI] [PubMed] [Google Scholar]
- 12.Trinh NH, Hoblyn J, Mohanty S, Yaffe K. Efficacy of cholinesterase inhibitors in the treatment of neuropsychiatric symptoms and functional impairment in Alzheimer disease: a meta-analysis. JAMA. 2003;289:210–216. doi: 10.1001/jama.289.2.210. [DOI] [PubMed] [Google Scholar]
- 13.Cummings JL, Schneider E, Tariot PN, Graham SM. Behavioral effects of memantine in Alzheimer disease patients receiving donepezil treatment. Neurology. 2006;67:57–63. doi: 10.1212/01.wnl.0000223333.42368.f1. [DOI] [PubMed] [Google Scholar]
- 14.Howard RJ, Juszczak E, Ballard CG, Bentham P, Brown RG, Bullock R, Burns AS, Holmes C, Jacoby R, Johnson T, Knapp MJ, Lindesay J, O'Brien JT, Wilcock GK, Katona C, Jones RW, DeCesare J, Rodger M. for the CALM-AD Trial Group: Donepezil for the treatment of agitation in Alzheimer's disease. N Engl J Med. 2007;357:1382–1392. doi: 10.1056/NEJMoa066583. [DOI] [PubMed] [Google Scholar]
- 15.Schneider LS, Dagerman K, Insel PS. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trials. Am J Geriatr Psychiatry. 2006;14:190–209. doi: 10.1097/01.JGP.0000200589.01396.6d. [DOI] [PubMed] [Google Scholar]
- 16.Schneider LS, Ismail MS, Dagerman K, Davis S, Olin J, McManus D, Pfeiffer E, Ryan JM, Sultzer DL, Tariot PN. Clinical antipsychotic trials of intervention effectiveness (CATIE): Alzheimer's disease trial. Schizophr Bull. 2003;29:57–72. doi: 10.1093/oxfordjournals.schbul.a006991. [DOI] [PubMed] [Google Scholar]
- 17.Schneider LS, Tariot PN, Dagerman KS, Davis SM, Hsiao JK, Ismail S, Lebowitz BD, Lyketsos CG, Ryan JM, Stroup TS, Sultzer DL, Weintraub D, Lieberman JA. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer's disease. N Engl J Med. 2006;355:1525–1538. doi: 10.1056/NEJMoa061240. [DOI] [PubMed] [Google Scholar]
- 18.Schneider LS, Tariot PN, Lyketsos CG, Dagerman KS, Davis KL, Davis S, Hsiao JK, Jeste DV, Katz IR, Olin JT, Pollock BG, Rabins PV, Rosenheck RA, Small GW, Lebowitz B, Lieberman JA. National Institute of Mental Health Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE): Alzheimer disease trial methodology. Am J Geriatr Psychiatry. 2001;9:346–360. [PubMed] [Google Scholar]
- 19.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 20.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of the Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 21.Folstein M, Folstein S, McHugh P. "Mini-Mental State": A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 22.Overall JE, Gorham DR. The Brief Psychiatric Rating Scale (BPRS): recent developments in ascertainment and scaling. Psychopharmacol Bull. 1988;24:97–99. [PubMed] [Google Scholar]
- 23.Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44:2308–2314. doi: 10.1212/wnl.44.12.2308. [DOI] [PubMed] [Google Scholar]
- 24.Overall JE, Belle SA. The Brief Psychiatric Rating Scale (BPRS) in geropsychiatric research: I. Factor structure on an inpatient unit. J Gerontol. 1984;39:187–193. doi: 10.1093/geronj/39.2.187. [DOI] [PubMed] [Google Scholar]
- 25.Alexopoulos GS, Abrams RC, Young RC, Shamoian CA. Cornell Scale for Depression in Dementia. Biol Psychiatry. 1988;23:271–284. doi: 10.1016/0006-3223(88)90038-8. [DOI] [PubMed] [Google Scholar]
- 26.Schneider LS, Olin JT, Clark CM, Morris JC, Reisberg B, Schmitt FA, Grundman M, Thomas RG, Ferris SH. Validity and reliability of the Alzheimer's Disease Cooperative Study-Clinical Global Impression of Change. Alzheimer Dis Assoc Disord. 1997;11(Suppl 2):S22–S32. doi: 10.1097/00002093-199700112-00004. [DOI] [PubMed] [Google Scholar]
- 27.Rosen WG, Mohs RC, Davis KL. A new rating scale for Alzheimer's disease. Am J Psychiatry. 1984;141:1356–1364. doi: 10.1176/ajp.141.11.1356. [DOI] [PubMed] [Google Scholar]
- 28.Galasko D, Bennett D, Sano M, Ernesto C, Thomas R, Grundman M, Ferris S. An inventory to assess activities of daily living for clinical trials in Alzheimer's disease. The Alzheimer's Disease Cooperative Study. Alzheimer Dis Assoc Disord. 1997;11 Suppl 2:S33–S39. [PubMed] [Google Scholar]
- 29.Stern Y, Albert SM, Sano M, Richards M, Miller L, Folstein M, Albert M, Bylsma F, Lafleche G. Assessing patient dependence in Alzheimer's disease. J Gerontol. 1994;49:M216–M222. doi: 10.1093/geronj/49.5.m216. [DOI] [PubMed] [Google Scholar]
- 30.Davis KL, Marin DB, Kane R, Patrick D, Peskind ER, Raskind MA, Puder KL. The caregiver activity survey (CAS): development and validation of a new measure for caregivers of persons with Alzheimer's disease. Int J Geriatr Psychiatry. 1997;12:978–988. doi: 10.1002/(sici)1099-1166(199710)12:10<978::aid-gps659>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 31.Rabins PV, Kasper JD, Kleinman L, Black BS, Patrick DL. Concepts and methods in the development of the ADRQL: an instrument for assessing health-related quality of life in persons with Alzheimer disease. J Ment Health Aging. 1999;5:33–48. [Google Scholar]
- 32.Hochberg YA. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75:800–802. [Google Scholar]
- 33.Ismail MS, Dagerman K, Tariot PN, Abbott S, Kavanagh S, Schneider LS. National Institute of Mental Health Clinical Antipsychotic Trials of Intervention Effectiveness-Alzheimer's Disease (CATIE-AD): Baseline characteristics. Curr Alzheimer Res. 2007;4:325–335. doi: 10.2174/156720507781077214. [DOI] [PubMed] [Google Scholar]
- 34.Sultzer DL, Brown C, Mandelkern MA, Mahler ME, Mendez MF, Chen ST, Cummings JL. Delusional thoughts and regional frontal/temporal cortex metabolism in Alzheimer's disease. Am J Psychiatry. 2003;160:341–349. doi: 10.1176/appi.ajp.160.2.341. [DOI] [PubMed] [Google Scholar]
- 35.Rosenheck RA, Leslie DL, Sindelar J, Miller EA, Tariot PN, Dagerman KS, Davis S, Lebowitz BD, Rabins P, Hsiao JK, Lieberman JA, Schneider LS. investigators ftC-A: A randomized trial of the cost-effectiveness of second generation antipsychotics and placebo in the treatment of psychosis and aggression in Alzheimer's disease. Arch Gen Psychiatry. 2007;64:1259–1268. doi: 10.1001/archpsyc.64.11.1259. [DOI] [PubMed] [Google Scholar]