Abstract
Duchenne muscular dystrophy (DMD) affects both skeletal and cardiac muscle. It is currently unclear whether the strategies developed for skeletal muscle can ameliorate cardiomyopathy. Synthetic mini-/micro-dystrophin genes have yielded impressive skeletal muscle protection in animal models. The 6-kb ΔH2-R19 minigene is particularly promising because it completely restores skeletal muscle force to wild-type levels. Here, we examined whether expressing this minigene in the heart, but not skeletal muscle, could normalize cardiac function in the mdx model of DMD cardiomyopathy. Transgenic mdx mice were generated to express the ΔH2-R19 minigene under the control of the α-myosin heavy-chain promoter. Heart structure and function were examined in adult and very old mice. The ΔH2-R19 minigene enhanced cardiomyocyte sarcolemmal strength and prevented myocardial fibrosis. It also restored the dobutamine response and enhanced treadmill performance. Surprisingly, heart-restricted ΔH2-R19 minigene expression did not completely normalize electrocardiogram and hemodynamic abnormalities. Overall, systolic function and ejection fraction were restored to normal levels but stroke volume and cardiac output remained suboptimal. Our results demonstrate that the skeletal muscle–proven ΔH2-R19 minigene can correct cardiac histopathology but cannot fully normalize heart function. Novel strategies must be developed to completely restore heart function in DMD.
Introduction
The lack of dystrophin in the heart leads to life-threatening dilated cardiomyopathy in Duchenne muscular dystrophy (DMD) patients. Current treatment strategy relies on symptom-relieving medicines.1 The efficacy of these palliative treatments remains under debate.2 A few patients have benefited from heart transplantation. However, for the majority of patients there is no effective treatment. Gene replacement therapy holds the promise of restoring dystrophin expression in the heart. If successful, it may recover cardiac function in all patients.3
A key issue in gene therapy is to express a functional gene in the target tissue. Adeno-associated virus is by far the most powerful gene delivery vehicle for the heart. However, a full-length dystrophin expression cassette cannot fit into a single adeno-associated virus virion. For this reason, tremendous effort has been directed toward designing minimized synthetic genes.
The dystrophin gene is one of the largest genes in the genome. It expresses a 427 kd membrane-associated cytoskeletal protein in striated muscles. The dystrophin protein contains four structural domains including the N-terminal, rod, cysteine-rich, and C-terminal domains. These domains participate in three major functional interactions with cytoskeletal protein F-actin, transmembrane protein β-dystroglycan, and several cytosolic proteins, respectively.3 The rod domain can be further divided into 24 spectrin-like repeats and 4 hinges. The N-terminal domain and spectrin-like repeats 11–17 represent two independent actin-binding sites.4 At least one of these sites is required for proper function.5 The end of hinge 4 and the cysteine-rich domain form the critical β-dystroglycan-binding site. This interaction links dystrophin and the extracellular matrix. The C-terminal domain contains binding sites for syntrophin and dystrobrevin. However, this domain is dispensable in skeletal muscle.6 Recent studies suggest that syntrophin and dystrobrevin can be recruited to the sarcolemma through the C-terminal domain independent pathway(s).7,8
A number of mini- and micro-dystrophin genes have been constructed after stripping out less important regions.9,10 Among these, the 6-kb ΔH2-R19 minigene carries the maximal amount of coding information. This minigene is molded after a truncated gene found in an extremely mild human patient, and it completely normalizes skeletal muscle force to wild-type levels.11,12 To determine whether the ΔH2-R19 minigene can normalize heart function, we generated a series of cardiac-specific transgenic mice. After backcrossing to the congenic mdx background, we characterized dystrophin expression and heart function.
Mini-dystrophin expression in the heart was confirmed by western blot and immunostaining. Structural studies showed that the ΔH2-R19 minigene strengthened the cardiomyocyte sarcolemmal integrity and prevented myocardial fibrosis. In functional analysis, the ΔH2-R19 minigene recovered stress-induced hemodynamic responses and improved treadmill performance. However, electrocardiogram (ECG) and hemodynamic defects were only partially normalized. Taken together, our results provide the first clear evidence that a minigene that can fully restore skeletal muscle force cannot completely normalize heart function when expressed only in the heart. Gene therapy for dystrophin-deficient muscle diseases must be carefully tailored to meet the different needs of the heart and skeletal muscle.
Results
Characterizing cardiac-specific ΔH2-R19 mini-dystrophin transgenic mice
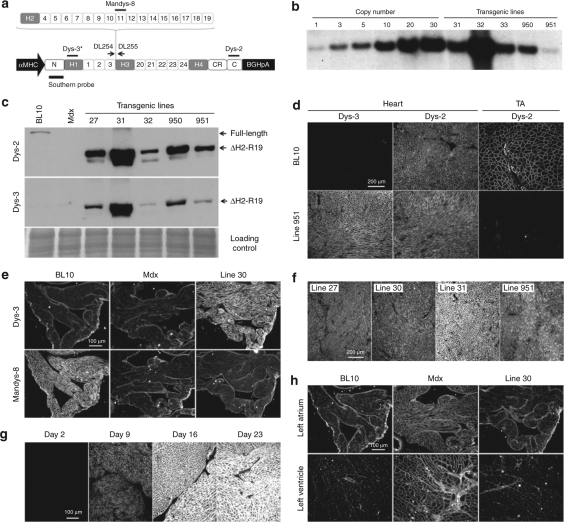
To determine the therapeutic efficacy of ΔH2-R19 mini-dystrophin for Duchenne cardiomyopathy, we generated a series of independent transgenic mdx mice. In these mice, a human version of the ΔH2-R19 minigene was expressed under the transcriptional regulation of the α-myosin heavy-chain promoter (Figure 1a). This promoter has been previously shown to drive transgene expression throughout the entire heart (including ventricles, atria, and the conduction system).13,14,15,16 Different minigene copies (from 1 copy to >30 copies) were found in different founder lines (Figure 1b and data not shown). Western blot also showed different expression levels, although protein level did not always correlate with the gene copy number (Figure 1c and data not shown). Immunofluorescence staining confirmed cardiac-specific minigene expression throughout the entire heart (Figure 1d,e and Supplementary Figure S1). Immunostaining also confirmed the expression-level differences seen in western blot (Figure 1f and data not shown). Furthermore, the dystrophin-associated glycoprotein complex was restored in the hearts of transgenic mice (data not shown).
Figure 1.
Characterization of cardiac-specific ΔH2-R19 mini-dystrophin transgenic mice. (a) Schematic outline of the transgenic construct. Dotted lines denote the regions deleted (from H2 to R19) from the full-length gene. The locations of the PCR primers (DL254 and DL255) and the origin of the Southern probe are marked. The regions recognized by Dys-2, Dys-3, and Mandys-8 antibodies are also marked. Asterisk, Dys-3 antibody only recognizes human dystrophin. C, C-terminal domain; CR, cysteine-rich domain; H, hinge; N, N-terminal domain; numerical numbers, spectrin-like repeats. (b) A representative Southern blot result from transgenic lines 31, 32, 33, 950, and 951. (c) A representative heart western blot from BL10, mdx, and transgenic lines 27, 31, 32, 950, and 951. Top panel, Dys-2 antibody reveals both the endogenous full-length mouse dystrophin in the BL10 heart and human mini-dystrophin in transgenic mice; middle panel, Dys-3 antibody only reveals human mini-dystrophin; bottom panel, loading control (rapid blue staining of a duplicate gel). (d) Representative Dys-2 and Dys-3 immunofluorescence staining images of the hearts and the tibialis anterior (TA) muscles from BL10 and transgenic line 951 mice. (e) Representative Dys-3 and Mandys-8 immunofluorescence staining images of the left atrium from BL10, mdx, and transgenic line 30 mice. (f) Representative Dys-3 immunofluorescence staining photomicrographs from transgenic lines 27, 30, 31, and 951. (g) Representative photomicrographs of Dys-2 heart immunofluorescence staining from line 32 at different postnatal development stages. (h) Representative left-heart utrophin immunofluorescence staining images from BL10, mdx, and transgenic line 30 mice. To facilitate the comparison of relative expression levels, images in the same panel were taken under the exact same exposure conditions.
The α-myosin heavy-chain promoter is turned on after birth. We did not detect minigene expression in 2-day-old mice. Moderate expression was seen in 9-day-old mice and it became higher in 16-day-old mice. The level reached the peak after 3 weeks and stabilized thereafter (Figure 1f).
Compensatory utrophin upregulation has been shown in the mdx heart.17 This was suppressed in the transgenic heart (Figure 1h).
Next, we examined the anatomic features of 2-month-old female mice and 20- to 22-month-old male mice (Table 1). Transgenic mice had the same body weight (BW), tibialis anterior, muscle weight, and the muscle weight/BW ratio as mdx mice. No significant difference was found in heart weight and ventricular weight among BL10, mdx, and transgenic mice (Table 1). Interestingly, old male mdx and transgenic mice had a significantly higher heart weight/BW ratio (Table 1). We also quantified the serum creatine kinase level in 20-month-old male mice. Transgenic mice and mdx mice showed the same creatine kinase level. Both were significantly higher than that of BL10 mice (Supplementary Figure S2).
Table 1.
Weights and weight ratios
Mini-dystrophin prevented sarcolemmal leakage in the heart
A basic function of dystrophin is to maintain the sarcolemmal integrity. Evans blue dye (EBD) accumulates in damaged myofibers when the muscle cell membrane is broken. We performed a comprehensive EBD uptake assay in 2-month-old female mice. A considerable amount of EBD was found in the hearts of mdx mice but was barely observed in the hearts of transgenic mice (Figure 2). PCR-negative transgenic littermates did not carry the minigene. These mice showed the same level of cardiac EBD uptake as mdx mice (Figure 2). In contrast to the heart, skeletal muscle cell membrane was not protected in transgenic mice. Widespread skeletal muscle EBD uptake was seen in both mdx and transgenic mice (Supplementary Figure S3).
Figure 2.
ΔH2-R19 mini-dystrophin stabilizes sarcolemmal integrity in the heart. (a) Representative heart Evans blue dye (EBD) uptake photomicrographs. Numbers denote transgenic line. Neg, transgene-negative littermate from the same breeding. (b) Quantification of the EBD-positive area. N, sample size. Asterisk, results from mdx mice and transgene-negative littermates are significantly different from BL10 and transgenic mice. There was no statistical difference between BL10 and different lines of transgenic mice.
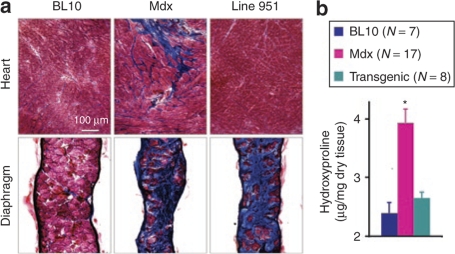
Cardiac-specific minigene expression eliminated myocardial fibrosis
In the aged mdx heart, necrotic myocardium is replaced by connective tissue.17 We evaluated fibrosis by Masson trichrome staining and hydroxyproline quantification, a measure of collagen content, in 22-month-old male mice (Figure 3). Mdx hearts showed prominent fibrotic staining (Figure 3a) and an elevated hydroxyproline level (Figure 3b). The hearts of transgenic mice were indistinguishable from those of BL10 mice. We did not see visible myocardial fibrosis, and the hydroxyproline content was not statistically different from that of BL10 hearts. In contrast to the heart, the transgenic mouse diaphragms were severely fibrotic (Figure 3a).
Figure 3.
Cardiac-specific ΔH2-R19 mini-dystrophin expression eliminates fibrosis in the heart but not in the diaphragm. (a) Representative Masson trichrome staining photomicrographs from the heart (top row) and the diaphragm (bottom row) in 22-month-old BL10, mdx, and transgenic line 951 mice. Connective tissue is in blue color. (b) Heart hydroxyproline content normalized by dry tissue weight. N, sample size. Asterisk, result from mdx mice was significantly different from both BL10 and transgenic mice. There was no statistical difference between BL10 and transgenic mice.
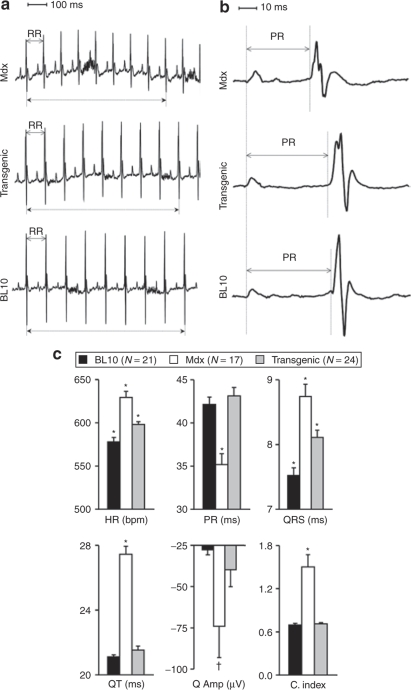
Mini-dystrophin improved but did not normalize the ECG profile
The absence of dystrophin results in several characteristic ECG changes in mdx mice. In particular, the heart rate, QRS duration, QT interval, and Q wave were increased, and the PR interval was reduced.17,18 We examined ECG in 8- and 22-month-old male mice (Figure 4 and Supplementary Figure S4). We first compared four independent transgenic lines (note, relative expression levels were shown in Figure 1c for lines 27, 32, and 951. Mini-dystrophin expression in line 29 was comparable to that of line 27, data not shown). Despite the difference in the expression level, all four lines showed the same ECG profile (Supplementary Table S1).
Figure 4.
Electrocardiogram (ECG) profiles in 22-month-old BL10, mdx, and transgenic mice. (a) Representative serial lead II ECG tracings. The dotted lines mark the time from the first to ninth R waves in each ECG tracing. (b) Representative serial lead II ECG tracings. (c) Quantitative evaluation of ECG profile. The results for transgenic mice are combined data from line 27 (five mice), line 29 (four mice), line 32 (eight mice), line 30 (one mouse), and line 951 (six mice). C. index, the cardiomyopathy index; HR, heart rate; Q Amp, the Q wave amplitude. Asterisk, significantly different from the other two groups; dagger, mdx was significantly different from BL10.
Next, we compared BL10, mdx, and transgenic mice (Figure 4 and Supplementary Figure S4). The most impressive corrections were seen in the PR interval, which was completely normalized (Figure 4 and Supplementary Figure S4). The heart rate and QRS duration were partially corrected in transgenic mice. The QT interval and the cardiomyopathy index were improved in 8-month-old transgenic mice and completely normalized in 22-month-old transgenic mice. We have previously shown an increase in the absolute amplitude of the Q wave in 21-month-old female mdx mice.17 In 8- and 22-month-old male mdx mice, the Q wave amplitude was significantly higher than that of age/sex-matched BL10 mice (ANOVA, P = 0.038 for 8-month-old mice and P = 0.024 for 22-month-old mice). In 8-month-old transgenic mice, the Q wave amplitude was normalized. In 22-month-old transgenic mice, the Q wave amplitude showed a trend toward normalization (ANOVA, P = 0.716 versus BL10, P = 0.104 versus mdx).
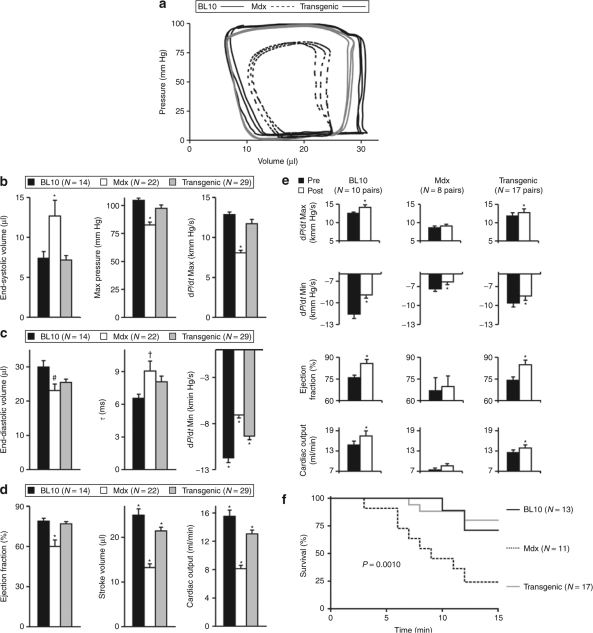
In aged mdx mice, mini-dystrophin restored the dobutamine stress response, but baseline hemodynamic defects were only partially improved
Defects in baseline systolic function (including end-systolic volume, maximal pressure, and dP/dt maximal) were fully corrected in transgenic mice (Figure 5a,b). However, we observed an interesting baseline diastolic profile in 22-month-old male mice. Compared with BL10 mice, mdx mice showed a decreased, rather than an increased, end-diastolic volume. Further, the heart relaxation constant (τ) in mdx mice was only marginally prolonged over that in BL10 mice (P = 0.043 by two-tailed t-test; P = 0.065 by Tukey post hoc analysis in one-way ANOVA) (Figure 5a,c). Nevertheless, the significant decrease in the minimal rate of left-ventricle relaxation (dP/dt minimal) revealed diastolic dysfunction in old male mdx mice. In minigene transgenic mice, dP/dt minimal was improved but did not reach BL10 levels (Figure 5c). The minigene also enhanced but did not completely normalize overall cardiac performance. Stroke volume and cardiac output were increased but were still significantly lower than those of BL10 mice. Only ejection fraction was restored to normal levels (Figure 5d).
Figure 5.
Characterization of hemodynamic changes in 22-month-old male BL10, mdx, and transgenic mice. (a) Representative PV loops. (b) Baseline hemodynamic profile during systole. (c) Baseline diastolic profile. (d) Overall heart function evaluation. The transgenic group in panels b to d includes four mice from line 27, eight mice from line 29, one mouse from line 30, one mouse from line 31, six mice from line 32, two mice from line 950, and seven mice from line 951. (e) Hemodynamic responses to dobutamine challenge. Pre, hemodynamic information before dobutamine administration; post, hemodynamic information at 5 minutes after dobutamine administration. The transgenic group in panels e and f includes six mice from line 27, five mice from line 29, one mouse from line 30, one mouse from line 31, and four mice from line 951. Max, maximal; Min, minimal. Asterisk (a–c), significantly different from the other two groups; asterisk (e), significantly different from pre-dobutamine stress; hash, significantly different from BL10 on ANOVA analysis; dagger, multiple group comparison by ANOVA shows no significant difference among three groups. However, t-test shows a significant difference between BL10 and mdx mice. (f) Kaplan–Meier survival analysis in mice stressed with dobutamine.
Additional comparison among different transgenic lines revealed similar baseline hemodynamic profiles among lines 29, 32, and 951 (Supplementary Table S2). Line 27 had a smaller end-diastolic volume than that of line 29. Line 27 also had a lower stroke volume and a lower cardiac output than those of lines 29 and 951. The reason for these differences is not clear. It could be due to the small sample (N = 4 for line 27 group) or the difference in mouse age (line 27 mice were the oldest).
The lack of dystrophin renders the heart sensitive to dobutamine stress.17,19 At 5 minutes after dobutamine administration, the heart contractility, ejection fraction, and cardiac output were all increased in BL10 mice (Figure 5e). Heart function was also significantly enhanced in transgenic mice (Figure 5e). Mdx mice barely responded to dobutamine stress (Figure 5e). At 15 minutes after dobutamine administration, the majority of the BL10 mice (73%) and transgenic mice (82%) were still alive while most of the mdx mice (75%) died (Kaplan–Meier analysis) (Figure 5f). There was no significant difference in the survival rate between transgenic and BL10 mice (Mantel–Cox log-rank test).
Heart-specific ΔH2-R19 mini-dystrophin expression enhanced uphill treadmill running performance
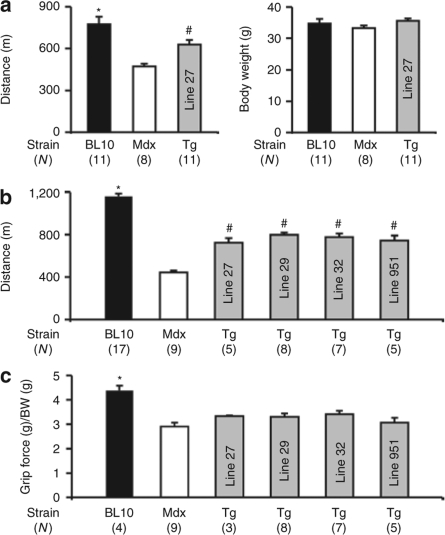
Uphill treadmill is another commonly used stress assay to evaluate murine heart function.20 We compared running performance among BL10, mdx, and transgenic mice in a 7° uphill treadmill. We first examined 8-month-old male mice. At this age, all three groups had similar BWs (Figure 6a). BL10 mice ran the longest distance. Interestingly, line 27 transgenic mice performed significantly better than mdx mice (Figure 6a). To further confirm this observation, we carried out a comprehensive study in multiple transgenic lines in 18-month-old male mice. This time we used a less demanding protocol. We started with a lower speed and applied a smaller scale of speed increase. Consistent with our results in 8-month-old mice, 18-month-old transgenic mice ran significantly farther than the age- and sex-matched mdx mice (Figure 6b). While improved over mdx mice, transgenic mice running distance did not reach the levels of BL10 mice.
Figure 6.
Cardiac-specific ΔH2-R19 mini-dystrophin expression improves uphill running performance without enhancing limb muscle strength. (a) Running distance and body weight in 8-month-old male mice. (b) Running distance in 18-month-old male mice (note, different treadmill protocols were used for 8- and 18-month-old mice). (c) Body weight normalized forelimb grip-strength in 18-month-old mice. N, sample size; Tg, transgenic mice; asterisk, significantly higher than all other groups; hash, significantly higher than that of mdx mice but lower than that of BL10 mice.
In DMD, both skeletal muscle and the heart are affected. To further define the cardiac contribution in our treadmill finding, we measured skeletal muscle function in 18-month-old mice. In a forelimb grip-strength assay, BL10 mice generated significantly higher force. There was not a significant difference between mdx and transgenic mice (Figure 6c). Taken together, these studies suggest that the enhanced uphill running performance in cardiac transgenic mice was most likely due to minigene expression in the heart.
Discussion
The large size of the dystrophin gene presents a unique challenge for DMD gene therapy. It has been noticed that patients with in-frame deletion of the dystrophin gene often display mild clinical manifestations.11 Based on these observations, a number of abbreviated dystrophin genes were developed.9,10 These microgenes and minigenes only carry 30–50% of the coding sequences of the full-length gene, yet they were able to reduce skeletal muscle disease in mouse models.
Heart failure is a leading cause of death in DMD patients. However, the truncated dystrophin genes have rarely been evaluated for their potential to rescue the heart.3 The heart has different structural and functional needs for dystrophin.3 One should be cautious in generalizing the skeletal muscle findings to the heart. To develop an effective gene therapy for DMD cardiomyopathy, we evaluated the ΔH2-R19 minigene. Prior to this study, a massively truncated ΔR4-23 microgene (3.8 kb) has been evaluated in young mdx hearts.18,21,22 Because this microgene cannot fully restore skeletal muscle function,12,23 it can be reasonably expected that microgene therapy cannot fully compensate heart function either. In contrast to the microgene, the ΔH2-R19 minigene is derived from a very mild human patient who was ambulant at the age of 61 years.11 More important, this minigene can be delivered by the trans-splicing adeno-associated virus vectors.12,24 In limb muscles and the diaphragm, the ΔH2-R19 minigene results in specific muscle forces that were indistinguishable from those of wild-type mice.12 To determine whether this minigene can also prevent cardiomyopathy, we selectively expressed it in the hearts of mdx mice. Mdx mice develop severe skeletal muscle and heart disease at old age (Figure 3).17 The ΔH2-R19 minigene significantly strengthened the cardiomyocyte sarcolemmal integrity (Figure 2). It also eliminated cardiac fibrosis (Figure 3). However, in contrast to a full functional recovery seen in skeletal muscle,12 we only observed partial heart function correction (Figures 4 and 5 and Supplementary Figure S4). ECG abnormalities such as tachycardia and QRS prolongation were improved but not normalized (Figure 4 and Supplementary Figure S4). Hemodynamic assay revealed normal maximal pressure, maximal rate of ventricular contraction (dP/dt maximal), and end-systolic volume. However, dP/dt minimal was only moderately improved. Stroke volume and cardiac output also did not reach normal levels (Figure 5).
Why does a gene that works so well in skeletal muscle fail to fully compensate for heart function? Dystrophin is a modular structural protein. Despite years of study, we still do not have a clear understanding of the roles every component plays. This is particularly true for the mid-rod domain. This domain was initially thought to merely act as a spacer between the critical F-actin-binding site at the N terminus and the β-dystroglycan-binding site near the C-terminal end. However, it is now known that this domain contains at least three important functional regions. First, spectrin-like repeat 11–17 constitutes a second F-actin-binding site. This site is sufficient to maintain the dystrophin–cytoskeleton linkage and provide mechanical support.5 Second, a viral protease cleavage site in hinge 3 has been implicated in coxsackievirus myocarditis.25 Third, one or several yet undefined regions in the rod domain are required to localize neuronal nitric oxide synthase (nNOS) to the sarcolemma.24,26,27,28 The deletion in the ΔH2-R19 minigene removes the second F-actin-binding site and the nNOS interaction subdomain.12,24 It is possible that the loss of these interactions may have compromised heart function. The loss of sarcolemmal nNOS leads to ischemia in contracting skeletal muscle.29 A similar mechanism has not been established in the heart. However, some clinical reports suggest that acute myocardial ischemia may contribute to the progression of DMD cardiomyopathy.30,31
A tantalizing hypothesis is the existence of heart-specific regions in the rod domain. In support of this hypothesis, studies have shown a correlation between exons 48 and 49 deletion and cardiac involvement in human patients.32,33 These two exons encode spectrin-like repeat 19. A recent study lends further support to this hypothesis.34 Investigators found a significant correlation between dilated cardiomyopathy and rod domain mutations. In particular, mutations in exon 12 and exons 14–17 predispose patients to dilated cardiomyopathy. Mutations in exons 31–42 may also favor heart disease. Interestingly, most of exon 17 and exons 31–42 are deleted in the ΔH2-R19 minigene. In addition to DMD and BMD patients, rod domain deletion has also been implicated in a subgroup of X-linked dilated cardiomyopathy patients.35 Based on these observations, one would not be surprised if there exists a cardiac subdomain between H2 and R19.
Another important factor is the interplay between cardiomyopathy and skeletal muscle disease. In our study, mini-dystrophin expression was restricted to the heart while skeletal muscle disease remained untreated (Figures 1d, 3, and 6c). Results from X-linked dilated cardiomyopathy patients have provided convincing evidence that normal skeletal muscle cannot prevent cardiac disease.36 However, damaged skeletal muscle may precipitate heart disease. Young mdx mice are mildly affected. When the skeletal muscles–specific transcription factor MyoD is inactivated, these mice not only show severe skeletal muscle disease but they also develop early-onset cardiomyopathy.3,37 Thus, there is a possibility that the presence of skeletal muscle disease may have limited heart recovery in our study. Future study with double transgenic mice that express the minigene in both cardiac and skeletal muscle will provide an answer to this intriguing hypothesis.
Clinically, it is still an arguable issue whether the severity of skeletal muscle impairment correlates with the degree of cardiac dysfunction. Conflicting results have been reported. Some studies suggest a positive association38 and others show no correlation.39,40 Crossing minigene transgenic mice with MyoD knockout mdx mice may provide a clue.
Considerable progress has been made in the last few years in DMD gene therapy. A recent phase I trial revealed excellent restoration of dystrophin expression after local skeletal muscle delivery.41 Although this certainly raises the hope of future clinical application to improve skeletal muscle function, one cannot ignore the need to treat Duchenne cardiomyopathy. Our results clearly show that a candidate gene that is fully functional in skeletal muscle is not sufficient to completely restore heart function when it is selectively expressed in the heart. Therapeutic strategies developed for skeletal muscle need to be carefully evaluated for their efficacy in the heart.
Materials and Methods
Experimental mice. All animal experiments were approved by the Animal Care and Use Committee of the University of Missouri and were in accordance with the National Institutes of Health guidelines. C57Bl/10SnJ (BL10) and dystrophin-deficient C57Bl/10ScSn-Dmdmdx/J (mdx) mice were purchased from The Jackson Laboratory (Bar Harbor, ME). The cardiac-specific mini-dystrophin transgenic mice were generated at the University of Missouri transgenic core. The ΔH2-R19 mini-dystrophin gene was released from pCK6. ΔH2ΔC-SV40pA (a gift from Dr. Jeffrey Chamberlain at the University of Washington, Seattle, WA).12 Standard molecular cloning procedures were used to insert the minigene between the α-myosin heavy-chain promoter and the BGH pA in a multicloning vector (a gift from Dr. Jeffrey Robbins at Cincinnati Children's Hospital Research Foundation, Cincinnati, OH) (detailed cloning procedure available on request).16 The final construct was confirmed by sequencing the cloning junction and by restriction analysis. A total of 10 FVB strain founder mice (lines 26, 27, 28, 29, 30, 31, 32, 33, 950, and 951) were identified by PCR and confirmed by Southern blot (Supplementary Materials and Methods). Transgene copy number was determined by Southern blot. Nine founder lines were backcrossed onto the mdx background for five to seven generations to reach incipient congenic status (founder 28 was euthanized by accident). The functional assays were performed in seven lines that showed uniform dystrophin expression in the hearts. These included lines 27, 29, 30, 31, 32, 950, and 951.
PCR and Southern blot. Genomic DNA was extracted from the tail using a previously described high salt precipitation protocol.42 PCR was used to identify the founder and the transgene-positive offspring. The forward PCR primer DL254 (5′-GTCAGTGACCCAGAAGA CGGAAGC-3′) is located in exon 16 in the dystrophin gene. The reverse PCR primer DL255 (5′-CCGGTTGAAATCTGCCA GAGCAGG-3′) is located in exon 51 in the dystrophin gene. The transgene-specific PCR product migrated at 262 bp. Southern blot was used to determine the transgene copy number. A 414 bp BamHI (exon 4)/EcoRV (exon 7) double-digested DNA fragment was used as the template for the Southern probe. Tail genomic DNA was digested with BamH I. After transfer to nylon membrane, the blot was hybridized with a 32P-labeled dystrophin N-terminal probe according to a previously published protocol.42 The diagnostic band migrated at 3.4 kb.
Western blot. A 50-µg aliquot of cardiac microsomal preparation was separated on a 6% sodium dodecyl sulfate–polyacrylamide gel. The membrane was first probed with an antibody against the C-terminal domain (Dys-2, 1:100; Novocastra, Newcastle, UK). After stripping, the membrane was reprobed with a human dystrophin hinge 1–specific antibody (Dys-3, 1:100; Novocastra).
Immunofluorescence staining and Masson trichrome staining. Antibodies used in dystrophin immunostaining included the Dys-2 (1:30), Dys-3 (1:20), and Mandys-8 (a mouse monoclonal antibody against spectrin-like repeat 11; 1:200; Sigma, St. Louis, MO) (Supplementary Table S3). Utrophin immunostaining was performed using a mouse monoclonal antibody against the utrophin N-terminal domain (VP-U579, 1:20; clone DRP3/20C5, IgG1; Vector Laboratories, Burlingame, CA). Immunostaining was performed essentially as we described before.8,21 Masson trichrome staining was performed according to a published protocol.17
EBD uptake. EBD uptake assay was performed in 2-month-old female mice according to a previously published protocol with modification.43 Mice were challenged with three doses of β isoproterenol (500 ng/g BW) at 18, 20, and 22 hours after tail-vein EBD injection (200 µg/g BW in phosphate-buffered saline). The heart was harvested 2 hours after the last β-isoproterenol administration in Tissue-Tek optimal cutting temperature compound (Sakura Finetek, Torrance, CA). EBD was visualized in 10-µm cross-sections from the middle portion of the heart under the Texas Red channel. The percentage of EBD-positive area was quantified from digitized images with ImageJ software (version 1.36b) (National Institutes of Health). For each heart, at least three random cross-sections were examined.
Hydroxyproline content assay. Lyophilized individual whole mouse heart was weighed and hydrolyzed in 6 N HCl for 18 hours at 106 °C. After pH neutralization, hydroxyproline content was determined using the method of Stegemann and Stalder.44 Briefly, a 2 ml heart lysate was oxidized with 1 ml chloramine-T at room temperature for 20 minutes. One millimeter of p-dimethylaminobenzaldehyde/perchloric acid was then added to the mixture and incubated for 15 minutes at 60 °C. The absorbency at 558 nm was measured with a Beckman Coulter DU640 spectrophotometer. Hydroxyproline concentration was determined using a standard curve.
ECG and hemodynamic assay. Cardiac physiology function assays were performed in age-matched male mice. A 12-lead ECG assay was performed with an ECG recording system from ADInstruments (Colorado Springs, CO) according to a procedure published previously.17 The amplitude of the Q wave was analyzed using the lead I tracing. Other parameters were analyzed using the lead II tracing. Cardiomyopathy index is calculated by dividing the QT interval with the PQ segment.17,18,43 Left-ventricular hemodynamic assay was performed in a closed-chest preparation as we described before.17,43 Pressure–volume loop data were analyzed with the PVAN software (Millar Instruments, Houston, TX). Dobutamine stress assay was performed using a published protocol.17 Hemodynamic measurements were performed at 5 minutes after dobutamine administration (5 µg/g BW, intraperitoneal injection). Mouse survival was monitored for at least 15 minutes after dobutamine administration or until mouse died. Mouse survival was defined as systolic pressure >30 mm Hg and heart rate >250 bpm.
Treadmill. A 7 ° uphill treadmill protocol was performed using an Exer-3/6 open treadmill (Columbus Instruments, Columbus, OH) according to guidelines from the American Physiological Society.45 The treadmill protocol consisted of five continuous days of incremental training followed by experimental determination of maximal running distance on day 6. On the experimental day, two different protocols were used for 8- and 18-month-old mice. For 8-month-old time point, mice were first run at 10 m/min for 20 minutes. Treadmill speed was then increased by 1 m/minutes every 2 minutes until mice were exhausted. For 18-month-old time point, we used a less stressful protocol. Briefly, mice were first run at 5 m/min for 5 minutes. Treadmill speed was then increased by 1 m/min every 5 minutes until mice were exhausted. Continuous nudging was used during treadmill to help mice stay on the track. Exhaustion was defined as spending >10 seconds on the shocker without attempting to re-enter the treadmill.
Forelimb grip strength. A computerized grip-strength meter (Columbus Instruments, Columbus, OH) was used to measure forelimb grip strength in conscious mice. Mice were acclimatized for 5 minutes before starting test. The mouse was allowed to grab the metal pull bar with the forepaws. The mouse was then gently pulled backward in the horizontal plane until it could no long grasp the bar. The force at the time of release was recorded as the peak tension. Each mouse was tested 5 times with a 20–40 seconds break between tests. The average peak tension from three best attempts was defined as forelimb grip strength.
Statistical analysis. Data are presented as mean ± SEM. Statistical analysis was performed with the SPSS software (SPSS, Chicago, IL) and the Prism 4 software (GraphPad, San Diego, CA). For multiple group comparison, statistical significance was determined by one-way ANOVA followed by Tukey post hoc analysis. For two-group comparison, statistical significance was determined by paired or two-tailed t-test. Difference was considered significant when P < 0.05. Dobutamine stress survival results were analyzed using Kaplan–Meier method. Statistical significance was determined by Mantel–Cox log-rank test. The Bonferroni corrected threshold was used to set the significance level for the survival study.
Supplementary MaterialFigure S1. The ΔH2-R19 mini-dystrophin gene was expressed throughout the entire heart in transgenic mice.Figure S2. Heart-specific expression of the ΔH2-R19 mini-dystrophin gene does not reduce the serum CK level in transgenic mice.Figure S3. Expressing ΔH2-R19 mini-dystrophin in the heart does not increase the sarcolemmal integrity in skeletal muscle.Figure S4. ECG profiles in 8-month-old male BL10, mdx, and transgenic mice.Table S1. ECG features in different lines of old transgenic mice.Table S2. Hemodynamic profiles in different lines of old transgenic mice.Table S3. Antibodies used in the study.Materials and Methods.
Supplementary Material
The ΔH2-R19 mini-dystrophin gene was expressed throughout the entire heart in transgenic mice.
Heart-specific expression of the ΔH2-R19 mini-dystrophin gene does not reduce the serum CK level in transgenic mice.
Expressing ΔH2-R19 mini-dystrophin in the heart does not increase the sarcolemmal integrity in skeletal muscle.
ECG profiles in 8-month-old male BL10, mdx, and transgenic mice.
ECG features in different lines of old transgenic mice.
Hemodynamic profiles in different lines of old transgenic mice.
Antibodies used in the study.
Acknowledgments
We thank Elizabeth S Critser and Natalia Karasseva at the University of Missouri Transgenic Animal Core for the help with generating the founder transgenic mice. This work was supported by grants from the National Institutes of Health (AR-49419, AR-57209, and NS-62934; DD) and the Muscular Dystrophy Association (D.D.).
REFERENCES
- American Academy of Pediatrics Section on Cardiology and Cardiac Surgery (2005) Cardiovascular health supervision for individuals affected by Duchenne or Becker muscular dystrophy. Pediatrics. 116:1569–1573. doi: 10.1542/peds.2005-2448. [DOI] [PubMed] [Google Scholar]
- Baxter P. Treatment of the heart in Duchenne muscular dystrophy. Dev Med Child Neurol. 2006;48:163. doi: 10.1017/S0012162206000351. [DOI] [PubMed] [Google Scholar]
- Duan D.Challenges and opportunities in dystrophin-deficient cardiomyopathy gene therapy Hum Mol Genet 200615R253–R261.spec. 2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ervasti JM. Dystrophin, its interactions with other proteins, and implications for muscular dystrophy. Biochim Biophys Acta. 2007;1772:108–117. doi: 10.1016/j.bbadis.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Warner LE, DelloRusso C, Crawford RW, Rybakova IN, Patel JR, Ervasti JM, et al. Expression of Dp260 in muscle tethers the actin cytoskeleton to the dystrophin-glycoprotein complex and partially prevents dystrophy. Hum Mol Genet. 2002;11:1095–1105. doi: 10.1093/hmg/11.9.1095. [DOI] [PubMed] [Google Scholar]
- Crawford GE, Faulkner JA, Crosbie RH, Campbell KP, Froehner SC., and , Chamberlain JS. Assembly of the dystrophin-associated protein complex does not require the dystrophin COOH-terminal domain. J Cell Biol. 2000;150:1399–1410. doi: 10.1083/jcb.150.6.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S, Kimura E, Ng R, Fall BM, Meuse L, Reyes M, et al. A highly functional mini-dystrophin/GFP fusion gene for cell and gene therapy studies of Duchenne muscular dystrophy. Hum Mol Genet. 2006;15:1610–1622. doi: 10.1093/hmg/ddl082. [DOI] [PubMed] [Google Scholar]
- Yue Y, Liu M., and , Duan D. C-terminal truncated microdystrophin recruits dystrobrevin and syntrophin to the dystrophin-associated glycoprotein complex and reduces muscular dystrophy in symptomatic utrophin/dystrophin double knock-out mice. Mol Ther. 2006;14:79–87. doi: 10.1016/j.ymthe.2006.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blankinship MJ, Gregorevic P., and , Chamberlain JS. Gene therapy strategies for Duchenne muscular dystrophy utilizing recombinant adeno-associated viral vectors. Mol Ther. 2006;13:241–249. doi: 10.1016/j.ymthe.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Foster K, Foster H., and , Dickson JG. Gene therapy progress and prospects: Duchenne muscular dystrophy. Gene Ther. 2006;13:1677–1685. doi: 10.1038/sj.gt.3302877. [DOI] [PubMed] [Google Scholar]
- England SB, Nicholson LV, Johnson MA, Forrest SM, Love DR, Zubrzycka-Gaarn EE, et al. Very mild muscular dystrophy associated with the deletion of 46% of dystrophin. Nature. 1990;343:180–182. doi: 10.1038/343180a0. [DOI] [PubMed] [Google Scholar]
- Harper SQ, Hauser MA, DelloRusso C, Duan D, Crawford RW, Phelps SF, et al. Modular flexibility of dystrophin: implications for gene therapy of Duchenne muscular dystrophy. Nat Med. 2002;8:253–261. doi: 10.1038/nm0302-253. [DOI] [PubMed] [Google Scholar]
- Kasahara H, Ueyama T, Wakimoto H, Liu MK, Maguire CT, Converso KL, et al. Nkx2.5 homeoprotein regulates expression of gap junction protein connexin 43 and sarcomere organization in postnatal cardiomyocytes. J Mol Cell Cardiol. 2003;35:243–256. doi: 10.1016/s0022-2828(03)00002-6. [DOI] [PubMed] [Google Scholar]
- Wei L, Taffet GE, Khoury DS, Bo J, Li Y, Yatani A, et al. Disruption of Rho signaling results in progressive atrioventricular conduction defects while ventricular function remains preserved. FASEB J. 2004;18:857–859. doi: 10.1096/fj.03-0664fje. [DOI] [PubMed] [Google Scholar]
- Lim BK, Xiong D, Dorner A, Youn TJ, Yung A, Liu TI, et al. Coxsackievirus and adenovirus receptor (CAR) mediates atrioventricular-node function and connexin 45 localization in the murine heart. J Clin Invest. 2008;118:2758–2770. doi: 10.1172/JCI34777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramaniam A, Jones WK, Gulick J, Wert S, Neumann J., and , Robbins J. Tissue-specific regulation of the alpha-myosin heavy chain gene promoter in transgenic mice. J Biol Chem. 1991;266:24613–24620. [PubMed] [Google Scholar]
- Bostick B, Yue Y, Long C., and , Duan D. Prevention of dystrophin-deficient cardiomyopathy in twenty-one-month-old carrier mice by mosaic dystrophin expression or complementary dystrophin/utrophin expression. Circ Res. 2008;102:121–130. doi: 10.1161/CIRCRESAHA.107.162982. [DOI] [PubMed] [Google Scholar]
- Bostick B, Yue Y, Lai Y, Long C, Li D., and , Dongsheng D. AAV-9 micro-dystrophin gene therapy ameliorates electrocardiographic abnormalities in mdx mice. Hum Gene Ther. 2008;19:851–856. doi: 10.1089/hum.2008.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danialou G, Comtois AS, Dudley R, Karpati G, Vincent G, Des Rosiers C, et al. Dystrophin-deficient cardiomyocytes are abnormally vulnerable to mechanical stress-induced contractile failure and injury. FASEB J. 2001;15:1655–1657. doi: 10.1096/fj.01-0030fje. [DOI] [PubMed] [Google Scholar]
- Bernstein D. Exercise assessment of transgenic models of human cardiovascular disease. Physiol Genomics. 2003;13:217–226. doi: 10.1152/physiolgenomics.00188.2002. [DOI] [PubMed] [Google Scholar]
- Yue Y, Li Z, Harper SQ, Davisson RL, Chamberlain JS., and , Duan D. Microdystrophin gene therapy of cardiomyopathy restores dystrophin-glycoprotein complex and improves sarcolemma integrity in the mdx mouse heart. Circulation. 2003;108:1626–1632. doi: 10.1161/01.CIR.0000089371.11664.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend D, Blankinship MJ, Allen JM, Gregorevic P, Chamberlain JS., and , Metzger JM. Systemic administration of micro-dystrophin restores cardiac geometry and prevents dobutamine-induced cardiac pump failure. Mol Ther. 2007;15:1086–1092. doi: 10.1038/sj.mt.6300144. [DOI] [PubMed] [Google Scholar]
- Liu M, Yue Y, Harper SQ, Grange RW, Chamberlain JS., and , Duan D. Adeno-associated virus-mediated micro-dystrophin expression protects young mdx muscle from contraction-induced injury. Mol Ther. 2005;11:245–256. doi: 10.1016/j.ymthe.2004.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai Y, Yue Y, Liu M, Ghosh A, Engelhardt JF, Chamberlain JS, et al. Efficient in vivo gene expression by trans-splicing adeno-associated viral vectors. Nat Biotechnol. 2005;23:1435–1439. doi: 10.1038/nbt1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badorff C, Lee GH, Lamphear BJ, Martone ME, Campbell KP, Rhoads RE, et al. Enteroviral protease 2A cleaves dystrophin: evidence of cytoskeletal disruption in an acquired cardiomyopathy. Nat Med. 1999;5:320–326. doi: 10.1038/6543. [DOI] [PubMed] [Google Scholar]
- Wells KE, Torelli S, Lu Q, Brown SC, Partridge T, Muntoni F, et al. Relocalization of neuronal nitric oxide synthase (nNOS) as a marker for complete restoration of the dystrophin associated protein complex in skeletal muscle. Neuromuscul Disord. 2003;13:21–31. doi: 10.1016/s0960-8966(02)00191-8. [DOI] [PubMed] [Google Scholar]
- Torelli S, Brown SC, Jimenez-Mallebrera C, Feng L, Muntoni F., and , Sewry CA. Absence of neuronal nitric oxide synthase (nNOS) as a pathological marker for the diagnosis of Becker muscular dystrophy with rod domain deletions. Neuropathol Appl Neurobiol. 2004;30:540–545. doi: 10.1111/j.1365-2990.2004.00561.x. [DOI] [PubMed] [Google Scholar]
- Judge LM, Haraguchi M., and , Chamberlain JS. Dissecting the signaling and mechanical functions of the dystrophin-glycoprotein complex. J Cell Sci. 2006;119:1537–1546. doi: 10.1242/jcs.02857. [DOI] [PubMed] [Google Scholar]
- Thomas GD, Sander M, Lau KS, Huang PL, Stull JT., and , Victor RG. Impaired metabolic modulation of alpha-adrenergic vasoconstriction in dystrophin-deficient skeletal muscle. Proc Natl Acad Sci USA. 1998;95:15090–15095. doi: 10.1073/pnas.95.25.15090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnecchi-Ruscone T, Taylor J, Mercuri E, Paternostro G, Pogue R, Bushby K, et al. Cardiomyopathy in Duchenne, Becker, and sarcoglycanopathies: a role for coronary dysfunction. Muscle Nerve. 1999;22:1549–1556. doi: 10.1002/(sici)1097-4598(199911)22:11<1549::aid-mus10>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- Ramaciotti C, Iannaccone ST., and , Scott WA. Myocardial cell damage in Duchenne muscular dystrophy. Pediatr Cardiol. 2003;24:503–506. doi: 10.1007/s00246-002-0408-9. [DOI] [PubMed] [Google Scholar]
- Melacini P, Fanin M, Danieli GA, Fasoli G, Villanova C, Angelini C, et al. Cardiac involvement in Becker muscular dystrophy. J Am Coll Cardiol. 1993;22:1927–1934. doi: 10.1016/0735-1097(93)90781-u. [DOI] [PubMed] [Google Scholar]
- Nigro G, Politano L, Nigro V, Petretta VR., and , Comi LI. Mutation of dystrophin gene and cardiomyopathy. Neuromuscul Disord. 1994;4:371–379. doi: 10.1016/0960-8966(94)90073-6. [DOI] [PubMed] [Google Scholar]
- Jefferies JL, Eidem BW, Belmont JW, Craigen WJ, Ware SM, Fernbach SD, et al. Genetic predictors and remodeling of dilated cardiomyopathy in muscular dystrophy. Circulation. 2005;112:2799–2804. doi: 10.1161/CIRCULATIONAHA.104.528281. [DOI] [PubMed] [Google Scholar]
- Cohen N., and , Muntoni F. Multiple pathogenetic mechanisms in X linked dilated cardiomyopathy. Heart. 2004;90:835–841. doi: 10.1136/hrt.2003.023390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towbin JA, Hejtmancik JF, Brink P, Gelb B, Zhu XM, Chamberlain JS, et al. X-linked dilated cardiomyopathy. Molecular genetic evidence of linkage to the Duchenne muscular dystrophy (dystrophin) gene at the Xp21 locus. Circulation. 1993;87:1854–1865. doi: 10.1161/01.cir.87.6.1854. [DOI] [PubMed] [Google Scholar]
- Megeney LA, Kablar B, Perry RL, Ying C, May L., and , Rudnicki MA. Severe cardiomyopathy in mice lacking dystrophin and MyoD. Proc Natl Acad Sci USA. 1999;96:220–225. doi: 10.1073/pnas.96.1.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunsaker RH, Fulkerson PK, Barry FJ, Lewis RP, Leier CV., and , Unverferth DV. Cardiac function in Duchenne's muscular dystrophy. Results of 10-year follow-up study and noninvasive tests. Am J Med. 1982;73:235–238. doi: 10.1016/0002-9343(82)90184-x. [DOI] [PubMed] [Google Scholar]
- Takenaka A, Yokota M, Iwase M, Miyaguchi K, Hayashi H., and , Saito H. Discrepancy between systolic and diastolic dysfunction of the left ventricle in patients with Duchenne muscular dystrophy. Eur Heart J. 1993;14:669–676. doi: 10.1093/eurheartj/14.5.669. [DOI] [PubMed] [Google Scholar]
- Nigro G, Comi LI, Politano L, Limongelli FM, Nigro V, De Rimini ML, et al. Evaluation of the cardiomyopathy in Becker muscular dystrophy. Muscle Nerve. 1995;18:283–291. doi: 10.1002/mus.880180304. [DOI] [PubMed] [Google Scholar]
- van Deutekom JC, Janson AA, Ginjaar IB, Frankhuizen WS, Aartsma-Rus A, Bremmer-Bout M, et al. Local dystrophin restoration with antisense oligonucleotide PRO051. N Engl J Med. 2007;357:2677–2686. doi: 10.1056/NEJMoa073108. [DOI] [PubMed] [Google Scholar]
- Duan D, Yue Y, Zhou W, Labed B, Ritche TC, Grosschedl R, et al. Submucosal gland development in the airway is controlled by lymphoid enhancer binding factor 1 (LEF1) Development. 1999;126:4441–4453. doi: 10.1242/dev.126.20.4441. [DOI] [PubMed] [Google Scholar]
- Yue Y, Skimming JW, Liu M, Strawn T., and , Duan D. Full-length dystrophin expression in half of the heart cells ameliorates beta-isoproterenol-induced cardiomyopathy in mdx mice. Hum Mol Genet. 2004;13:1669–1675. doi: 10.1093/hmg/ddh174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stegemann H., and , Stalder K. Determination of hydroxyproline. Clin Chim Acta. 1967;18:267–273. doi: 10.1016/0009-8981(67)90167-2. [DOI] [PubMed] [Google Scholar]
- Kregel KC, Allen DL, Booth FW, Fleshner MR, Henriksen EJ, Musch TL, et al. Resource Book for the Design of Animal Exercise Protocols 2006. American Physiological SocietyBethesda, MD
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The ΔH2-R19 mini-dystrophin gene was expressed throughout the entire heart in transgenic mice.
Heart-specific expression of the ΔH2-R19 mini-dystrophin gene does not reduce the serum CK level in transgenic mice.
Expressing ΔH2-R19 mini-dystrophin in the heart does not increase the sarcolemmal integrity in skeletal muscle.
ECG profiles in 8-month-old male BL10, mdx, and transgenic mice.
ECG features in different lines of old transgenic mice.
Hemodynamic profiles in different lines of old transgenic mice.
Antibodies used in the study.