Abstract
Background: Traditionally, distal radial fractures in the elderly have been treated nonoperatively with casting. However, since the introduction of the volar locking plating system in 2000, there has been an interest in the use of more aggressive treatment methods. The purpose of the present study was to assess changing trends in the treatment of distal radial fractures in elderly patients in the United States.
Methods: We evaluated a 5% sample of Medicare data from 1996 to 1997 and a 20% sample from 1998 to 2005. Information on four treatment methods (closed treatment, percutaneous pin fixation, internal fixation, and external fixation) was extracted from the dataset. Other available data were diagnosis, physician specialty, and patient age, sex, and race. We calculated frequencies and rates to compare the utilization of different treatments over time.
Results: Over the ten-year time period examined, the rate of internal fixation of distal radial fractures in the elderly increased fivefold, from 3% in 1996 to 16% in 2005. Closed treatment, however, remained the predominant method (used for 82% of the fractures in 1996 and 70% in 2005). Fractures in patients with an age of eighty-five years or more were significantly more likely to be treated in a closed fashion (p < 0.0001). There was a large variation among physician specialties with regard to the fixation methods that were used. Orthopaedic surgeons were significantly more likely to use closed treatment than hand surgeons were, whereas hand surgeons were significantly more likely to use internal fixation than orthopaedic surgeons were.
Conclusions: Since 2000, although the majority of distal radial fractures are still treated nonoperatively, there has been an increase in the use of internal fixation and a concurrent decrease in the rate of closed treatment of distal radial fractures in the elderly in the United States.
Distal radial fracture is a public health concern, particularly among the elderly, who often experience fragility fractures. Approximately 10% of sixty-five-year-old white women in the United States will sustain a distal radial fracture during the remainder of their lifetime1. Traditionally, these fractures in the elderly have been treated nonoperatively with use of casting alone2. The use of nonoperative treatment has been based on the perceived low functional demands in the elderly population; however, it has been shown that casting alone for the treatment of unstable osteoporotic distal radial fractures can result in collapse of the fracture fragments and the development of a malunion3,4. Interestingly, despite the development of a malunion, many elderly patients function relatively well, but the majority of studies showing acceptable function involved elderly patients who were frail or had low functional demands5-9.
Recently, there has been an interest in more aggressive fracture fixation in the elderly in the hopes of speeding the rate of recovery in order to preserve the ability of patients to live independently2,10-12. The introduction of the volar locking plating system in 2000 has spurred this interest. A recent prospective study evaluating the rate of functional improvement after treatment with the volar locking plating system demonstrated similar rates of recovery between patients in two age groups (twenty to forty years and more than sixty years)13. The volar locking plating system imparts sufficiently stable fixation to maintain good anatomic reduction, even in the elderly14. This stability makes it easier for elderly patients to resume activities of daily living earlier than is the case after treatment with use of the traditional, more conservative approaches that require a longer period of immobilization14.
Despite their high prevalence, the epidemiology of distal radial fractures is not well-characterized and the treatment of these fractures in the elderly population remains ill-defined. The specific purpose of the present investigation was to study a random sample of United States Medicare claims from a ten-year period (1996 to 2005) in order (1) to examine the changing trend in the treatment of distal radial fractures in the Medicare population and (2) to evaluate physician specialty experiences in the treatment of these fractures.
Materials and Methods
For the present study, we used a 5% sample of claims data from 1996 and 1997 and a 20% sample of claims data from 1998 to 2005 from the United States Centers for Medicare and Medicaid Services, obtained by means of a formal request. We obtained this dataset from The Dartmouth Institute for Health Policy and Clinical Practice; investigators at that institution have previously used this particular dataset to track practice variations for a variety of diseases. The dataset has undergone extensive “cleaning” to allow ease of analysis and is most relevant for studying distal radial fractures. The United States Centers for Medicare and Medicaid Services draws the samples from the claims data for fee-for-service Medicare patients who are sixty-five to ninety-nine years of age. Both samples were of Medicare Part B claims, which cover physicians' services and were randomly selected on the basis of the last two digits of the Health Insurance Claim number15. From this sample, we first extracted claims including an ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) code indicating a closed distal radial fracture. Using this smaller group of claims, we then filtered for claims with Current Procedural Terminology codes for closed treatment (with or without manipulation), percutaneous pin fixation, external fixation (uniplane or multiplane), and open treatment (Table I). Because of the coding terminology, we were unable to determine if fixation took place during open treatment. However, it is rare that open treatment is pursued without internal fixation. For these reasons, we will refer to open treatment as internal fixation throughout the present report.
TABLE I.
ICD-9-CM and CPT Codes Used for Filtering Medicare Datasets*
| ICD-9-CM code | |
| 813.41 | Closed Colles fracture |
| 813.42 | Other closed fracture of the distal part of the radius, alone |
| CPT code | |
| 20690 | Application of a uniplane unilateral external fixation system |
| 20692 | Application of a multiplane unilateral external fixation system |
| 25600 | Closed treatment of distal radial fracture, without manipulation |
| 25605 | Closed treatment of distal radial fracture, with manipulation |
| 25611 | Percutaneous skeletal fixation of distal radial fracture |
| 25620 | Open treatment of distal radial fracture |
ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification, and CPT = Current Procedural Terminology.
Each claim contained the Current Procedural Terminology code of the procedure (treatment method) performed, the year in which the claim was filed, the sex of the patient, the age group of the patient (sixty-five to sixty-nine years, seventy to seventy-four years, seventy-five to seventy-nine years, eighty to eighty-four years, and eighty-five years or more), and the racial category of the patient (white or nonwhite). In addition, each claim contained the self-designated primary specialty of the treating physician. The United States Centers for Medicare and Medicaid Services allows the physician to designate as many as three specialties in the order that he or she chooses. For instance, a surgeon may identify himself or herself as an orthopaedic surgeon primarily and as a hand surgeon secondarily. Alternatively, the same surgeon could identify himself or herself as a hand surgeon primarily and as an orthopaedic surgeon secondarily. The dataset that we obtained contained only the primary specialty designation. It is quite possible that an orthopaedic hand surgeon may identify himself or herself as an orthopaedic surgeon primarily and as a hand surgeon secondarily.
Frequencies were calculated for 1996 to 1997 by multiplying the 5% sample by 20. Likewise, frequencies for 1998 to 2005 were calculated by multiplying the 20% sample by 5. This is a standard and often-used method to determine overall frequencies from small samples16-18. The significance of differences between groups was analyzed with use of the Student t test and odds ratios.
Source of Funding
The present study was supported in part by a grant from the American Foundation for Surgery of the Hand, the National Institute of Arthritis and Musculoskeletal and Skin Diseases Exploratory/Developmental Research Grant Award (R21 AG030526), a Clinical Trial Planning Grant (R34 AR055992-01), and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) to one of the authors (K.C.C.). Funds were used to purchase the dataset and for salary support.
Results
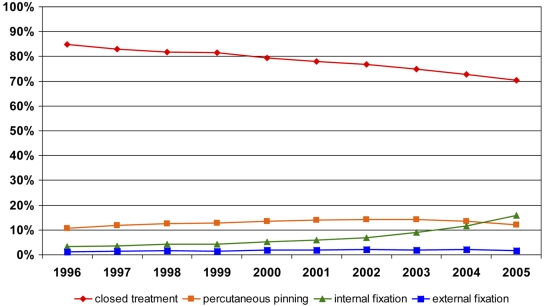
The 5% dataset (1996 to 1997) and the 20% dataset (1998 to 2005) represented an average of 81,008 Medicare claims (range, 76,080 to 87,315 claims) for distal radial fracture treatment per year. The tabulation of this ten-year dataset is presented in Table II. Closed treatment was the predominant method of distal radial fracture fixation in these patients (Fig. 1). In 2005, 70% of the Medicare claims were for closed treatment. The rate of percutaneous pin fixation, the second-most-frequently used method of treatment, remained flat before decreasing slightly between 2004 and 2005. The rate of external fixation use was very low, with little change occurring over the study period. There was an increasing trend in the use of internal fixation (from 3% to 16%), which corresponded with a decrease in the use of closed treatment (from 82% to 70%).
TABLE II.
Estimated Frequency and Percentage of Fractures Treated Each Year According to Physician Specialty*
| Frequency in Dataset | Estimated Frequency† | Orthopaedic Surgery‡ | Hand Surgery‡ | Other Surgery‡§ | Other Specialty‡# | |
|---|---|---|---|---|---|---|
| 1996 | 4074 | 81,480 | 70,540 (86.6%) | 640 (0.8%) | 1520 (1.9%) | 8780 (10.8%) |
| 1997 | 3804 | 76,080 | 66,340 (87.2%) | 1100 (1.4%) | 1220 (1.6%) | 7420 (9.8%) |
| 1998 | 15,286 | 76,430 | 66,255 (86.7%) | 895 (1.2%) | 695 (0.9%) | 8585 (11.2%) |
| 1999 | 15,510 | 77,550 | 66,735 (86.1%) | 1050 (1.4%) | 700 (0.9%) | 9065 (11.7%) |
| 2000 | 15,648 | 78,215 | 66,675 (85.2%) | 1070 (1.4%) | 505 (0.6%) | 9965 (12.7%) |
| 2001 | 16,102 | 80,510 | 66,470 (82.6%) | 1460 (1.8%) | 565 (0.7%) | 12,015 (14.9%) |
| 2002 | 15,996 | 79,980 | 66,625 (83.3%) | 1745 (2.2%) | 660 (0.8%) | 10,950 (13.7%) |
| 2003 | 17,127 | 85,635 | 71,465 (83.5%) | 2165 (2.5%) | 630 (0.7%) | 11,375 (13.3%) |
| 2004 | 17,463 | 87,315 | 71,565 (82.0%) | 2670 (3.1%) | 615 (0.7%) | 12,465 (14.3%) |
| 2005 | 17,377 | 86,885 | 70,185 (80.8%) | 3415 (3.9%) | 585 (0.7%) | 12,700 (14.6%) |
1996 and 1997 are 5% sample Medicare data; 1998 to 2005 are 20% sample Medicare data.
Frequencies were calculated for 1996 to 1997 by multiplying the 5% sample by 20. Frequencies for 1998 to 2005 were calculated by multiplying the 20% sample by 5.
The percentages are based on the values shown in the “Estimated Frequency” column for each year.
Other Surgery includes General Surgery and Plastic and Reconstructive Surgery.
Other Specialty includes Emergency Medicine, Family Practice, General Practice, and Internal Medicine.
Fig. 1.
Line graph illustrating the rate of each fixation method according to year.
There was very little variation in fixation method according to sex. Male patients were 1% more likely to be managed with closed reduction, and female patients were 2% more likely to be managed with percutaneous pinning. There was no difference between the sexes with regard to the use of internal or external fixation. There was also no notable difference in the utilization of fixation techniques according to racial group. White patients were 1% more likely to be managed with percutaneous pinning, whereas nonwhite patients were 1% more likely to be managed with both closed reduction and internal fixation. As with sex, there were no racial differences in terms of the percentage of patients who received external fixation. As patients aged, the rate of nonoperative treatment increased (Table III). Overall, the rate of closed reduction increased from 70.9% of all patients who were sixty-five to sixty-nine years of age to 87.0% in patients who were more than eighty-five years of age (p < 0.0001). Likewise, the rate of internal fixation decreased from 10.9% in the youngest age group to 1.0% in the oldest age group.
TABLE III.
| Frequency in Dataset | Estimated Frequency | <70 Years‡ | 70 to 74 Years‡ | 75 to 79 Years‡ | 80 to 84 Years‡ | ≥85 Years‡ | |
|---|---|---|---|---|---|---|---|
| Closed treatment | 106,755 | 632,985 | 93,105 (70.9%) | 121,250 (73.6%) | 139,655 (76.6%) | 132,675 (81.0%) | 146,300 (87.0%) |
| Percutaneous pinning | 18,348 | 104,985 | 20,805 (15.8%) | 25,020 (15.2%) | 25,315 (13.9%) | 19,415 (11.9%) | 14,430 (8.6%) |
| Internal fixation | 10,788 | 58,050 | 14,340 (10.9%) | 15,175 (9.2%) | 13,865 (7.6%) | 8965 (5.5%) | 5705 (3.4%) |
| External fixation | 2491 | 14,060 | 3040 (2.3%) | 3195 (1.9%) | 3375 (1.9%) | 2685 (1.6%) | 1765 (1.0%) |
Frequencies were calculated for 1996 to 1997 by multiplying the 5% sample by 20. Frequencies for 1998 to 2005 were calculated by multiplying the 20% sample by 5.
Age groups are as reported in the sample datasets.
The values are given as the number of fractures treated with each method in each age group; the percentages are based on the total number of fractures in each age group.
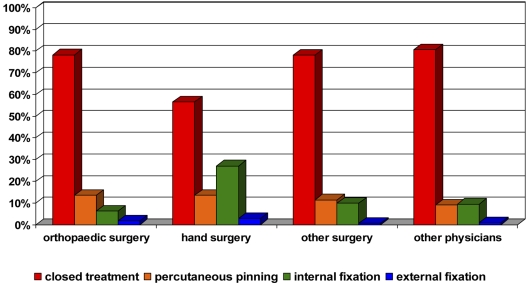
There was a considerable difference among physician specialties with regard to the fixation methods used (Fig. 2). Orthopaedic surgeons were significantly more likely to use closed reduction than hand surgeons were; specifically, closed reduction was used for 78.2% of fractures treated by orthopaedic surgeons, compared with 56.5% of fractures treated by hand surgeons (p < 0.0001). Similarly, hand surgeons were significantly more likely to use internal fixation than orthopaedic surgeons were; specifically, internal fixation was used for 27.1% of fractures treated by hand surgeons, compared with 6.3% of fractures treated by orthopaedic surgeons (p < 0.0001). The odds of performing closed treatment as opposed to internal fixation were 5.7 times greater for an orthopaedic surgeon as compared with a hand surgeon (95% confidence interval, 5.3 to 6.1; p < 0.0001). There was no difference between the specialties with regard to the rate of use of percutaneous pinning, and both specialties seldom used external fixation.
Fig. 2.
Bar graph illustrating the use of each fixation method according to primary self-designated physician specialty.
Ten percent of distal radial fractures were treated by nonsurgeons (Fig. 2); this finding was unexpected. Most commonly, these individuals were physicians with the primary designation of emergency medicine and family practice. However, the treatment provided by these individuals was limited almost exclusively to closed reduction. It is probable that physicians in these two specialties are treating distal radial fractures in the emergency department or in outpatient clinics in the acute setting.
Discussion
Changing trends in the treatment of distal radial fractures in elderly patients in the United States are evident in this ten-year review of Medicare data. It is well known that closed reduction may not adequately restore anatomic alignment11,12; at least 50% of the fractures that are treated in this manner lead to malunion3,4. Furthermore, closed reduction requires four to six weeks of wrist immobilization, which can lead to stiffness. Disuse of the hand and wrist can result in osteopenia that may result in fracture collapse7. However, through 2005, closed reduction remained the predominant method of treatment of distal radial fractures in the elderly in the United States. The present study also demonstrates that despite the common use of closed treatment, distal radial fractures in the Medicare population are increasingly treated with internal fixation methods. Because of the general nature of the Current Procedural Terminology coding, we are unable to ascertain exactly which internal fixation technique was used. However, the rapid increase in the use of internal fixation corresponded with the earliest report on the volar locking plating system, which was published in 200019. Before the introduction of the volar locking plating system, internal fixation was accomplished with a variety of methods, including dorsal plating, which today is viewed less favorably because of complications related to implant loosening, tendon rupture, and wrist stiffness20-24.
These results are corroborated by an examination of American Board of Orthopaedic Surgery Part II oral examination data from 1999 to 2007. Koval et al. found that internal fixation of distal radial fractures increased dramatically over this eight-year period, and they postulated that this increase may have been due to the introduction of the volar locking plating system25,26. With internal fixation, elderly patients require less immobilization time and may be able to return to normal activities sooner. However, one study that compared two weeks of wrist immobilization with six weeks of immobilization following fixation with the volar locking plating system demonstrated no significant difference between the two groups with regard to the final range of wrist motion27. Internal fixation techniques require more operative dissection and may be technically challenging. The invasiveness of the operation also may be associated with more complications. Nevertheless, a randomized controlled trial by Leung et al.24 demonstrated that patients managed with plate fixation had significantly better outcomes than patients managed with external fixation and pin fixation. Furthermore, three retrospective studies supported the use of internal fixation for the treatment of distal radial fractures in the elderly; two studies supported its use in general2,12, and one supported the use of the volar locking plating system specifically11. The present study confirms the increasing popularity of this fixation method. However, because our data provided no information on outcomes, the popularity of this mode of treatment does not necessarily indicate its superiority.
The present study revealed that most physicians with the primary designation of orthopaedic surgeon still predominantly employed closed methods for the treatment of distal radial fractures. Conversely, physicians with the primary designation of hand surgeon were much more inclined to apply internal fixation methods. This finding was observed in the study by Koval et al. as well, in which hand-fellowship-trained surgeons employed open treatment 84% of the time, whereas those without hand-fellowship training used open treatment only 57% of the time25.
The present study has several limitations. The most obvious limitations are the generality of coding for internal fixation and the imprecision of coding for the medical specialty of the treating physician. A single code for all internal fixation techniques cannot discern the type of fixation procedures used. It would be interesting to know if the rapid increase in internal fixation from 2002 to 2005 mainly comprised fixation with the volar locking plating system. The dataset that we obtained included only the primary identifier for specialty, although physicians are allowed to designate both a primary and a secondary specialty. This means that the accuracy of the specialty designations was very dependent on how the providing physician entered the data. Physicians who identified themselves as orthopaedic surgeons primarily and hand surgeons secondarily would be coded as orthopaedic surgeons in this dataset, whereas physicians who reported hand surgery first and orthopaedic surgery second would be coded as hand surgeons. It is possible that some hand surgeons identified themselves as orthopaedic surgeons primarily and that the information that their practices are predominantly composed of hand surgery was not available to us. However, the large difference in the rate of utilization of the surgical procedures between the self-designated orthopaedic surgeons and the self-designated hand surgeons cannot be accounted for by the specialty coding issue alone. Finally, because there were no patient identifiers in our dataset, some patients may have been counted more than once. This may have occurred if a patient received closed treatment in an emergency department and was later referred for surgical intervention. We believe that although this is possible, it is not especially likely. As noted, emergency medicine physicians accounted for only 6% of the closed treatment cases.
The Dartmouth Atlas of Musculoskeletal Health Care explored geographic variations in the incidence and surgical treatment of various musculoskeletal injuries (including distal radial fractures) in the United States by examining the Medicare database from 1996 to 199728. The investigators reported evidence of marked geographic variations and found that surgical intervention rates varied as much as tenfold. However, the investigators did not examine the change in rates over time. We examined changes in the treatment of distal radial fractures in the elderly population in the United States over time. The elderly population is growing at an ever-increasing rate29, and elderly individuals are now more active than ever30. They often prefer medical treatments that do not hamper their activities. These factors all point to a shift toward the increased use of more aggressive treatments of distal radial fractures in elderly patients, including internal fixation, which had previously been reserved for younger patients. 
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants in excess of $10,000 from the American Foundation for Surgery of the Hand, the National Institute of Arthritis and Musculoskeletal and Skin Diseases Exploratory/Developmental Research Grant Award (R21 AG030526), a Clinical Trial Planning Grant (R34 AR055992-01), and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120). Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated.
Investigation performed at the University of Michigan, Ann Arbor, Michigan
References
- 1.Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles', or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149:2445-8. [PubMed] [Google Scholar]
- 2.Beharrie AW, Beredjiklian PK, Bozentka DJ. Functional outcomes after open reduction and internal fixation for treatment of displaced distal radius fractures in patients over 60 years of age. J Orthop Trauma. 2004;18:680-6. [DOI] [PubMed] [Google Scholar]
- 3.Mackenney PJ, McQueen MM, Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006;88:1944-51. [DOI] [PubMed] [Google Scholar]
- 4.Strange-Vognsen HH. Intraarticular fractures of the distal end of the radius in young adults. A 16 (2-26) year follow-up of 42 patients. Acta Orthop Scand. 1991;62:527-30. [DOI] [PubMed] [Google Scholar]
- 5.Grewal R, MacDermid JC. The risk of adverse outcomes in extra-articular distal radius fractures is increased with malalignment in patients of all ages but mitigated in older patients. J Hand Surg [Am]. 2007;32:962-70. [DOI] [PubMed] [Google Scholar]
- 6.Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg [Am]. 2000;25:19-28. [DOI] [PubMed] [Google Scholar]
- 7.Beumer A, McQueen MM. Fractures of the distal radius in low-demand elderly patients: closed reduction of no value in 53 of 60 wrists. Acta Orthop Scand. 2003;74:98-100. [DOI] [PubMed] [Google Scholar]
- 8.Anzarut A, Johnson JA, Rowe BH, Lambert RGW, Blitz S, Majumdar SR. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated fractures. J Hand Surg [Am]. 2004;29:1121-7. [DOI] [PubMed] [Google Scholar]
- 9.Hegeman JH, Oskam J, Vierhout PAM, ten Duis HJ. External fixation for unstable intra-articular distal radial fractures in women older than 55 years. Acceptable functional end results in the majority of the patients despite significant secondary displacement. Injury. 2005;36:339-44. [DOI] [PubMed] [Google Scholar]
- 10.Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg [Am]. 2002;27:205-15. [DOI] [PubMed] [Google Scholar]
- 11.Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg [Am]. 2004;29:96-102. [DOI] [PubMed] [Google Scholar]
- 12.Jupiter JB, Ring D, Weitzel PP. Surgical treatment of redisplaced fractures of the distal radius in patients older than 60 years. J Hand Surg [Am]. 2002;27:714-23. [DOI] [PubMed] [Google Scholar]
- 13.Chung KC, Squitieri L, Kim HM. Comparative outcomes study using the volar locking plating system for distal radius fractures in both young adults and adults older than 60 years. J Hand Surg [Am]. 2008;33:809-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ring D, Jupiter JB. Treatment of osteoporotic distal radius fractures. Osteoporos Int. 2005;16 Suppl 2:S80-4. [DOI] [PubMed] [Google Scholar]
- 15.Department of Health and Human Services. Centers for Medicare and Medicaid Services. Standard analytical files. http://www.cms.hhs.gov/IdentifiableDataFiles/02_StandardAnalyticalFiles.asp. Accessed 2008 Nov 3.
- 16.University of Minnesota. Research Data Assistance Center. http://www.resdac.umn.edu/CCW/CCWFAQ.asp. Accessed 2008 Nov 7.
- 17.Murphy TP, Soares G, Kim M. Increase in utilization of percutaneous renal artery interventions by Medicare beneficiaries, 1996-2000. AJR Am J Roentgenol. 2004;183:561-8. [DOI] [PubMed] [Google Scholar]
- 18.McBean M, Rajamani S. Increasing rates of hospitalization due to septicemia in the US elderly population, 1986-1997. J Infect Dis. 2001;183:596-603. [DOI] [PubMed] [Google Scholar]
- 19.Orbay JL. The treatment of unstable distal radius fractures with volar fixation. Hand Surg. 2000;5:103-12. [DOI] [PubMed] [Google Scholar]
- 20.Kreder HJ, Hanel DP, Agel J, McKee M, Schemitsch EH, Trumble TE, Stephen D. Indirect reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular fractures of the distal radius: a randomised, controlled trial. J Bone Joint Surg Br. 2005;87:829-36. [DOI] [PubMed] [Google Scholar]
- 21.Grewal R, Perey B, Wilmink M, Stothers K. A randomized prospective study on the treatment of intra-articular distal radius fractures: open reduction and internal fixation with dorsal plating verses mini open reduction, percutaneous fixation, and external fixation. J Hand Surg [Am]. 2005;30:764-72. [DOI] [PubMed] [Google Scholar]
- 22.Westphal T, Piatek S, Schubert S, Winckler S. Outcome after surgery of distal radius fractures: no differences between external fixation and ORIF. Arch Orthop Trauma Surg. 2005;125:507-14. [DOI] [PubMed] [Google Scholar]
- 23.Kambouroglou GK, Axelrod TS. Complications of the AO/ASIF titanium distal radius plate system (pi plate) in internal fixation of the distal radius: a brief report. J Hand Surg [Am]. 1998;23:737-41. [DOI] [PubMed] [Google Scholar]
- 24.Leung F, Tu YK, Chew WY, Chow SP. Comparison of external and percutaneous pin fixation with plate fixation for intra-articular distal radial fractures. A randomized study. J Bone Joint Surg Am. 2008;90:16-22. [DOI] [PubMed] [Google Scholar]
- 25.Koval KJ, Harrast JJ, Anglen JO, Weinstein JN. Fractures of the distal part of the radius. The evolution of practice over time. Where's the evidence? J Bone Joint Surg Am. 2008;90:1855-61. [DOI] [PubMed] [Google Scholar]
- 26.Drobetz H, Kutscha-Lissberg E. Osteosynthesis of distal radius fractures with a volar locking screw plate system. Int Orthop. 2003;27:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lozano-Calderon SA, Souer S, Mudgal C, Jupiter JB, Ring D. Wrist mobilization following volar plate fixation of fractures of the distal part of the radius. J Bone Joint Surg Am. 2008;90:1297-1304. [DOI] [PubMed] [Google Scholar]
- 28.Weinstein JN, Birkmeyer JD. The Dartmouth atlas of musculoskeletal health care. Chicago, IL: American Hospital Association; 2000. [PubMed]
- 29.US Census Bureau. National population estimates—characteristics. National sex and age. April 1, 2000, to July 1, 2006. http://www.census.gov/popest/national/asrh/NC-EST2006-sa.html. Accessed 2008 July 17.
- 30.Manton KG, Gu X, Lamb VL. Change in chronic disability from 1982. to 2004/2005 as measured by long-term changes in function and health in the U.S. elderly population. Proc Natl Acad Sci U S A. 2006;103:18374-9. [DOI] [PMC free article] [PubMed] [Google Scholar]