Abstract
Objectives
To investigate financial capacity in patients with mild cognitive impairment (MCI) and Alzheimer’s disease (AD) using a clinician interview approach.
Design
Cross-sectional.
Setting
Tertiary care medical center.
Participants
Healthy older adults (N=75), patients with amnestic MCI (N=58), mild AD (N=97), and moderate AD (N=31).
Measurements
The investigators and five study physicians developed a conceptually based, semi-structured clinical interview for evaluating seven core financial domains and overall financial capacity (Semi-Structured Clinical Interview for Financial Capacity; SCIFC). For each participant, a physician made capacity judgments (capable, marginally capable, or incapable) for each financial domain and for overall capacity.
Results
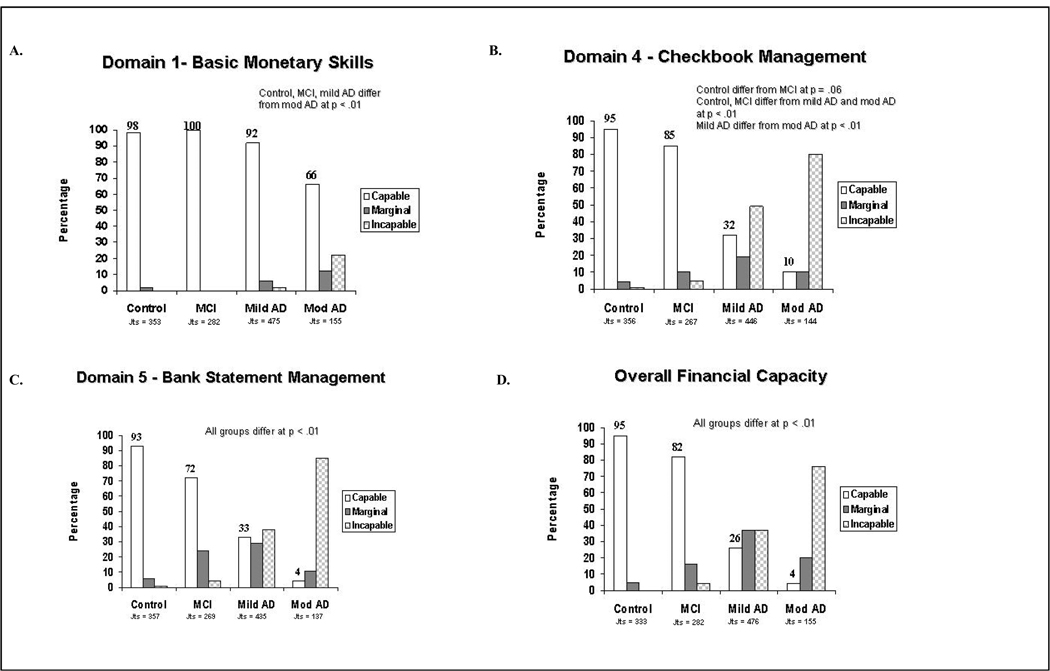
Study physicians made a total of over 11,000 capacity judgments across the study sample (N=261). Very good inter-rater agreement was obtained for the SCIFC judgments. Increasing proportions of marginal and incapable judgment ratings were associated with increasing disease severity across the four study groups. For overall financial capacity, 95 percent of physician judgments for older controls were rated as capable, as compared to only 82% for patients with MCI, 26% for patients with mild AD, and 4% for patients with moderate AD.
Conclusion
Financial capacity in cognitively impaired older adults can be reliably evaluated by physicians using a relatively brief, semi-structured clinical interview. Financial capacity shows mild impairment in MCI, emerging global impairment in mild AD, and advanced global impairment in moderate AD. MCI patients and their families should proactively engage in financial and legal planning given these patients’ risk of developing AD and accelerated loss of financial abilities.
Keywords: financial capacity, competency, clinical assessment, mild cognitive impairment, Alzheimer’s disease
INTRODUCTION
As our society ages, increasing numbers of older adults will experience impairment of higher order functional abilities as a result of Alzheimer’s disease and related disorders (AD). In areas such as medical decision-making, driving, managing finances, and making testamentary dispositions, families and society as a whole have a strong interest in distinguishing intact from impaired functioning1–4. Clinical assessment of such key functional capacities by physicians and other health care practitioners is an important but often overlooked aspect of geriatric practice.
Among higher order abilities, the capacity to manage financial affairs has particular significance to independent functioning of older adults5, 6. Financial capacity comprises a broad range of conceptual, pragmatic, and judgment abilities, ranging from basic skills like counting coins and currency, to more complex skills such as paying bills, managing a checkbook, and exercising financial judgment7. Similar to driving and mobility, it is a core aspect of individual autonomy in our society and represents a cognitively complex set of knowledge and skills vulnerable to cognitive aging and dementia 5, 8–11.
Impairment of financial abilities occurs in patients with AD and to a lesser extent in patients with mild cognitive impairment (MCI)5. Using a psychometric measure of financial capacity, our group has previously found that patients with amnestic MCI demonstrate mild impairments in financial abilities such as conceptual knowledge, bill payment, and bank statement management12. In contrast, patients with mild AD show impairments across a range of both simple and complex financial abilities5, and these abilities show further rapid decline over a one year period13. Patients with moderate AD, in turn, demonstrate severe and global impairment in all financial skills13. This progressive loss of financial skills in older patients with MCI and AD mirrors the problems of financial judgment, exploitation, and elder abuse that plague the elderly population and that are targets of public policy measures14.
The financial capacity of older adults is also a growing clinical issue for physicians and other health care professionals15. Families frequently look to health care providers to address issues of declining financial skills and decision-making in their loved ones. These clinical judgments, while not legal adjudications, have important ethical and legal implications, as they often result in restriction or removal of a patient’s freedom to manage their financial affairs7. These judgments are also challenging to make, as physicians and other clinicians have had little or no education or training in financial capacity assessment2. In contrast to areas such as medical-decision-making capacity, there are no published studies of clinician assessment of financial capacity. In addition, there are few if any clinician-administered instruments available with which to assess financial capacity. The availability of such instruments could improve clinical care and promote both autonomy and protection of older adults.
The present study examined assessment of financial capacity in older adults using a clinician-administered interview (Semi-Structured Clinical Interview for Financial Capacity) (SCIFC). We describe the development of the SCIFC as an assessment tool and then present data concerning its reliability and validity in a clinical sample representing the dementia spectrum (cognitively healthy older controls, and patients with MCI, mild AD, and moderate AD).
METHODS
Conceptual Model of Financial Capacity
Financial capacity involves a broad range of declarative, procedural, and judgment-based knowledge and skills7. We previously have developed a conceptual model that views financial capacity at three levels: specific financial abilities (task level) such as counting coins/currency or prioritizing bills for payment; broader areas of financial activity each having clinical relevance for independent functioning (domain level) such as conducting cash transactions or exercising financial judgment; and overall financial capacity (global level). This conceptual model is discussed in more detail elsewhere5, 7, 16.
Development of a Clinician Assessment Measure
The SCIFC was developed as a clinician-oriented, semi-structured interview distinct from existing standardized psychometric capacity measures5, 17, 18 which are quantified and require trained technicians for administration. Primary considerations were to develop a relatively brief interview assessing a range of financial domains and affording the clinician both structure and autonomy. The SCIFC was developed by the investigators (D.C.M., V.W., and S.S.) and five study physicians (B.A., P.G., C.K., A.P.N., and T.S.). Phases of development included : (1) identifying and discussing constituent skills and abilities related to the financial domains of the conceptual model5; (2) generating and refining test items for each domain; (3) creation of a 25-minute, semi-structured interview based on test item selection; (4) identification of core items and also optional supplemental test items for each domain; (5) development of administration and scoring procedures; and (6) piloting and final revision of the interview. Table 1 presents a schematic of the SCIFC instrument and its core items.
Table 1.
Schematic of the Semi-Structured Clinical Interview for Financial Capacity (SCIFC)
| Item Description | |
|---|---|
| Domain 1 Basic Monetary Skills | |
| Core Questions: | |
| 1. Naming coins/currency | Identify specific coins and currency |
| 2. Coin/currency relationships | Identify relative worth of coins/currency |
| 3. Counting coins/currency | Accurately count coins and currency |
| Domain 2 Financial Conceptual Knowledge | |
| Core Questions | |
| 1. Define term money | Define a variety of financial concepts |
| 2. Define ways people obtain money | |
| 3. Define term loan | |
| Domain 3 Cash Transactions | |
| Core Questions | |
| 1. Identify item cost | Identify cost of single item from price tag |
| 2. one item grocery purchase | One item transaction; verify change |
| 3. Addition of sales tax | Explain additional charge regarding purchase |
| Domain 4 Checkbook Management | |
| Core Questions | |
| 1. Understand checkbook | Define check |
| 2. Use checkbook | Simulated transaction; pay by check |
| 3. Use checkbook register | Simulated register entry and balancing |
| Domain 5 Bank Statement Management | |
| Core Questions | |
| 1. Identify bank statement | Explain purpose of bank statement |
| 2. Identify bank statement balance | Calculate bank statement balance |
| 3. Identify deposit | Identify monthly checkbook deposit |
| 4. Identify balance differences | Identify balance differences |
| Domain 6 Financial Judgment | |
| Core Questions | |
| 1. Detect telephone fraud risk | Detect and explain risk |
| 2. Determine appropriate value | Explain how to determine worth of automobile |
| 3. Advertising automobile | Indicate how to advertise automobile |
| 4. Receiving payment | Explain how to obtain appropriate payment |
| Domain 7 Bill Payment | |
| Core Questions | |
| 1. Understand bills | Explain meaning and purpose of bills |
| 2. Identify bill amount | Identify money owed on bill |
| 3. Questioning amount of bills | Explain how to question amount of bill |
| 4. Unpaid bills | Explain consequence of unpaid bills |
| Domain 8 Knowledge of Personal Assets and Estate Arrangements | |
| Core Questions | |
| 1. Income | Identify source of income |
| 2. Assets and will/trust | Identify valuables and will/trust |
| Overall Financial Capacity | Functioning across all skills and domains |
The SCIFC contains both verbally administered items (question/answer) and also performance items using financial stimuli and other testing materials materials. Some illustrative items from the SCIFC and its domains are presented below:
| Domain 1: Basic Monetary Skills | |
| • | “Please identify these coins and currency” |
| Domain 2: Financial Conceptual Knowledge | |
| • | “What is money?” |
| Domain 3: Cash Transactions | |
| • | “Please give me the exact amount of money needed to buy this box of tissues” |
| Domain 4: Checkbook Management | |
| • | “What is a check?” |
| Domain 5: Bank Statement Management | |
| • | What are some of the ways John Doe spent money during this month? |
| Domain 6: Financial Judgment | |
| • | “How could you be sure the price for the car is fair? ” |
| Domain 7: Bill Payment | |
| • | “If you had a question about this bill, what would you do?” |
| Domain 8: Knowledge of Personal Financial Assets and Estate Arrangements | |
| • | “Do you have a will or a living trust?” |
The final version of the SCIFC interview comprised seven core domains (Domains 1–7) and one experimental domain (Domain 8). The clinician directly judges performance on the core domains, while Domain 8 (Knowledge of Assets and Estate) also requires the clinician to obtain corroborating information from a reliable informant. Because informant availability and report accuracy were variable across study participants, we treated Domain 8 as experimental. Clinicians follow general scoring criteria for individual core and supplemental items within each domain, but retain autonomy regarding domain and overall capacity judgments. The SCIFC elicits a total of nine capacity judgments (one for each domain and for overall financial capacity). In making a judgment, a clinician assigns one of three possible outcomes (capable, marginally capable, or incapable) based upon their assessment and clinical judgment. This judgment outcome classification has been used successfully in prior financial capacity5, 13 and other capacity research19, 20.
Study Participants
Participants consisted of 75 healthy older controls, 58 patients with amnestic MCI, 97 mild AD patients, and 31 moderate AD patients. All participants were recruited through the Alzheimer's Disease Research Center (ADRC) at the University of Alabama at Birmingham (UAB) and were part of an associated NIH research project (Financial Capacity Project; 1R01MH55247).
Healthy community dwelling older adults were clinically evaluated by a neurologist and neuropsychologist to ensure the absence of medical, neurologic, and psychiatric conditions affecting cognition. Controls in this study received a Clinical Dementia Rating (CDR)21 staging scores and completed standardized tests of mental status (Mini-Mental State Examination; MMSE22), and global cognitive status (Dementia Rating Scale; DRS23). Controls were characterized as cognitively normal in the UAB ADRC diagnostic clinical consensus conference.
Patients with amnestic MCI were recruited through the Memory Disorders Clinic at UAB and were well-characterized based upon the medical, neurologic, psychiatric, and neuropsychological screening described above. Diagnosis of amnestic MCI was made in ADRC diagnostic consensus conference using original Mayo criteria24.
Patients with probable AD were also recruited from the Memory Disorders Clinic and their dementia was well characterized based on the above screening procedures. Diagnosis of probable AD was made in the ADRC diagnostic consensus conference using NINCDS-ADRDA criteria25. Dementia severity (mild- moderate) was assigned in consensus conference and was based both on clinical information and CDR score21.
Informed consent was obtained from all participants and their caregivers. This study was approved by the UAB Institutional Review Board.
Study Physicians
As discussed above, five UAB physicians (two geriatric psychiatrists, one geriatrician, and two neurologists) served as study collaborators and assisted with both development of the SCIFC and its application in the study. Each physician had extensive clinical experience with geriatric and dementia assessment, and also with competency assessment in clinical settings. Each physician was board certified in their specialty. Physicians were blinded to participant diagnosis at the time of their interview.
Procedures for SCIFC Administration and Scoring
Using the SCIFC, each study physician evaluated the capacity of each participant using a live interview/videotape review methodology successfully employed in prior studies26. Specifically, each study participant was directly interviewed with the SCIFC by one study physician. The interview was videotaped, and the other four physicians each independently reviewed the videotaped interview. In this way, all study physicians evaluated each study participant, while at the same time avoiding potential confounds involved with multiple physician assessments of the same participant. The interviewing physician was randomly assigned to preclude any systematic interviewing bias.
Statistical Analyses
Demographic and Clinical Variables
Group differences in terms of age, education, DRS-2 total score, CDR sum of boxes, and Mini-Mental State Exam (MMSE22) score were analyzed employing ANOVA with Tukey’s Studentized Range (HSD) test. Analyses of the distribution of CDR staging, gender, and ethnicity group differences were performed with chi-square.
Estimates of Physician Judgment Agreement
Physician judgment agreement was defined at two levels. Excellent judgment agreement was defined as 100% or “exact” agreement for a specific capacity outcome for a participant on an SCIFC variable. As a hypothetical example, all five physicians agree that Participant X is capable on Domain 1. Very good judgment agreement was defined as 80%+ agreement for a specific capacity outcome for a participant on an SCIFC variable. As a hypothetical example, four (or five) of the five physicians agree that Participant Y is marginally capable on Domain 6. We used the 80%+ judgment agreement level as the basis for evaluating judgment reliability in the study. This approach to estimating agreement was chosen for ease of interpretation and to avoid unstable and artificially lowered statistical estimates of agreement due to restricted range of the capacity judgment data across groups.
Comparison of Capacity Judgment Outcomes Across Groups
Group differences in financial capacity outcomes on the SCIFC variables (with physician judgments within the same patient treated as a cluster) were analyzed using a Generalized Estimating Equations (GEE) approach for ordinal data27. GEE is an extension of the general linear model and is used to analyze clustered data in which the multiple scores from the same patient are likely to be correlated. The GEE method accounts for the correlation among observations from the same participant and provides more efficient and less biased regression parameters than the fixed ordinal logistic regression method. The GEE analyses were carried out using SAS (version 9.2) PROC GENMOD procedure.
For each SCIFC variable, a separate GEE analysis was conducted for participants in each of the four groups. In each model, the SCIFC judgment score, classified as an ordinal variable (capable/marginally capable/incapable) served as the dependent variable and group (Control/MCI/Mild AD/Moderate AD) was entered as the predictor variable. Each model adjusted for age and education, and the Holm’s adjustment was used to adjust for multiple comparisons. A p value of .01 was employed as the criterion for statistical significance.
Data Exclusion: Prior/Premorbid Financial Experience
Because individual financial experience can vary across individuals5, we accounted for lack of financial skills and experience. The Prior/Premorbid Financial Capacity Form (PFCF)5, a measure that rates the level of prior (control) or premorbid (MCI or AD patient) experience across each SCIFC domain, was administered separately to participants and their informants (i.e., family member). We used the PFCF results to exclude data of participants lacking experience on specific SCIFC variables. These procedures resulted in the exclusion of one control from Bank Statement Management analysis. In the MCI group the following domain related exclusions occurred: Financial Concepts (n=1), Checkbook Management (n=4), Bank Statement Management (n=3). In the mild AD group, the following exclusions occurred: Financial Concepts (n=2), Checkbook Management (n=6), Bank Statement (n=8), Financial Judgment (n=6), Bill Payment (n=4). In the moderate AD group, the following exclusions were identified: Checkbook Management (n=2), Bank Statement (n=3), Financial Judgment (n=2), and Bill Payment (n=2).
RESULTS
Demographic and Mental Status Variables
Results are set forth in Table 2. Controls and MCI patients were younger than mild AD patients, who in turn were younger than moderate AD patients. The control group had higher education levels than the mild and moderate AD patients. The MCI and mild AD group had similar levels of education, with both having higher education levels than the moderate AD group. More men than women composed the mild AD group. The groups did not significantly differ in the proportion of Caucasians and African-Americans. The MMSE and DRS-2 total scores were worse for the mild and moderate AD patients compared to MCI patients and controls.
Table 2.
Demographic variables of study participants
| Controls | MCI | Mild AD | Moderate AD | |||
|---|---|---|---|---|---|---|
| N = 75 | N = 58 | N = 97 | N = 31 | |||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | F | p value | |
| Age (years) b,c,d,e | 66.1 (7.7) | 68.0 (8.3) | 72.4 (8.4) | 75.3 (8.4) | 14.3 | < .001 |
| Education (years) b,c,e,f | 14.3 (1.6) | 13.7 (2.0) | 13.4 (2.1) | 11.1 (3.7) | 15.5 | < .001 |
| Gender (m/f) c,d,e,f | 24 / 51 | 18 / 40 | 52 / 45 | 10 / 21 | 12.2* | < .007 |
| Race** | ||||||
| Caucasian | 65 | 44 | 85 | 23 | 8.3 * | 0.21 |
| African American | 9 | 14 | 11 | 8 | ||
| Other | 1 | 0 | 1 | 0 | ||
| MMSE b,c,d,e,f | 29.3 (1.0) | 28.2 (1.9) | 24.0 (3.1) | 16.4 (4.2) | 196.9 | < .001 |
| DRS Total Score | ||||||
| (max = 144) a,b,c,d,e,f | 138.7 (3.8) | 131.3 (7.4) | 114.0 (12.1) | 90.7 (19.6) | 178.5 | < .001 |
| CDR Staging, n | ||||||
| 0.0 | 70 | 8 | 00 | 00 | ||
| 0.5 | 04 | 48 | 17 | 00 | ||
| 1.0 | 00 | 2 | 80 | 10 | ||
| 2.0 | 00 | 00 | 00 | 18 | ||
| 3.0 | 00 | 00 | 00 | 1 | ||
| CDR sum of boxes a,b,c,d,e,f | ||||||
| Max = 18, mean (SD) | 0 (.2) | 1.2 (1.3) | 5.0 (1.8) | 9.8 (3.4) | 290.7 | < .001 |
Note. Missing data for DRS: n = 1 MCI group, n = 3 moderate AD group. Missing data for CDR rating: n = 1 control group, n = 2 moderate AD group.
MMSE = Mini-Mental State Examination, DRS = Dementia Rating Scale, CDR = Clinical Dementia Rating.
Post-hoc analyses
-- controls differ significantly from MCI at p < .01
– controls differ significantly from mild AD at p < .01
– controls differ significantly from moderate AD at p < .01
– MCI differ significantly from mild AD at p < .01
– MCI differ significantly from moderate AD at p < .01
– mild AD differ significantly from moderate AD at p < .01
Chi-square value.
Statistical comparison between the Caucasian and African-American groups only.
Physician Capacity Judgments
A total of 11,118 individual capacity judgments were made by the five physicians across the nine SCIFC domains and overall sample (n=261). Each physician made an average of 2,224 capacity judgments, attesting to their effort and commitment. A total of 627 ratings were not obtained (missing data) out of 11,745 possible ratings [5 physicians ×261 participants ×9 SCIFC variables]. This represented a 94.7% judgment outcome completion rate.
Physician Judgment Agreement
Table 3 presents SCIFC inter-rater judgment findings using the exact (100%) and 80%+ agreement levels. As previously described, the standard for evaluating judgment agreement was set at 80%+ agreement. For participants as a whole, acceptable inter-rater agreement was found for all domains and for overall capacity. For overall capacity, 80%+ agreement was obtained in 78% of cases (203 of 261 participants). At the total group level and across the core domains, 80%+ agreement levels ranged from a high of 95% of cases (Basic Monetary Skills) to a low of 76% (Financial Judgment). As discussed above, the reliability level for experimental Domain 8 (Knowledge of Personal Assets/Estate Arrangements) was lower due in part to missing corroborating informant report.
Table 3.
Observed Inter-Rater Judgment Agreement for the Five Physicians Using the SCIFC
| Domain | Controls N= 79 | MCI N = 58 | Mild AD N = 97 | Moderate AD N = 31 | Total N = 261 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 100% Interrater Agreement | 80%+ Interrater Agreement | 100% Interrater Agreement | 80%+ Interrater Agreement | 100% Interrater Agreement | 80%+ Interrater Agreement | 100% Interrater Agreement | 80%+ Interrater Agreement | 100% Interrater Agreement | 80%+ Interrater Agreement | |
| D1Basic Monetary Skills Observed | 73/75 | 75/75 | 57/58 | 58/58 | 87/97 | 91/97 | 20/31 | 25/31 | 237/261 | 249/261 |
| Percentage Agreement | 97% | 100% | 98% | 100% | 90% | 92% | 66% | 81% | 91% | 95% |
| D2Financial Concepts Observed | 71/75 | 74/75 | 56/57 | 57/57 | 68/95 | 81/95 | 12/31 | 23/31 | 207/258 | 235/258 |
| Percentage Agreement | 95% | 99% | 98% | 100% | 72% | 86% | 39% | 74% | 80% | 91% |
| D3 Cash Transactions Observed | 73/75 | 74/75 | 57/58 | 58/58 | 72/97 | 83/97 | 17/31 | 29/31 | 219/261 | 244/261 |
| Percentage Agreement | 97% | 99% | 99% | 100% | 74% | 86% | 55% | 94% | 84% | 93% |
| D4 Checkbook Management Observed | 69/75 | 75/75 | 44/54 | 50/54 | 58/91 | 74/91 | 23/29 | 24/29 | 194/249 | 223/249 |
| Percentage Agreement | 92% | 100% | 81% | 93% | 64% | 81% | 79% | 83% | 75% | 90% |
| D5 Bank Statement Mgmt Observed | 68/74 | 71/74 | 34/55 | 44/55 | 43/89 | 61/89 | 20/28 | 23/28 | 165/246 | 199/246 |
| Percentage Agreement | 92% | 96% | 62% | 80% | 48% | 68% | 71% | 82% | 67% | 80% |
| D6 Financial Judgment Observed | 60/75 | 67/75 | 36/58 | 47/58 | 35/97 | 67/97 | 11/29 | 17/29 | 142/256 | 196/256 |
| Percentage Agreement | 80% | 89% | 62% | 81% | 36% | 69% | 38% | 59% | 55% | 76% |
| D7 Bill Payment Observed | 72/75 | 73/75 | 51/58 | 54/58 | 55/93 | 71/93 | 15/29 | 20/29 | 193/255 | 218/255 |
| Percentage Agreement | 96% | 97% | 88% | 93% | 59% | 76% | 52% | 69% | 75% | 85% |
| D8 Assets/Estate Arrangement Observed | 63/75 | 68/75 | 41/58 | 51/58 | 35/97 | 58/97 | 2/31 | 12/31 | 141/261 | 189/261 |
| Percentage Agreement | 84% | 91% | 71% | 88% | 36% | 60% | 6% | 39% | 54% | 72% |
| D1–7 Total Score Observed | 64/75 | 68/75 | 37/58 | 51/58 | 35/97 | 67/97 | 17/31 | 26/31 | 153/261 | 203/261 |
| Percentage Agreement | 85% | 91% | 64% | 90% | 36% | 69% | 55% | 84% | 59% | 78% |
Across study groups, mean 80%+ judgment agreement for the seven core domains was 97% of control cases, versus 92% of MCI cases, 80% of mild AD cases, and 77% of moderate AD cases. For overall capacity, 80%+ agreement was obtained in 91% of control cases, 90% of MCI cases, 69% of mild AD cases, and 84% of moderate AD cases. The lower agreement level for the mild AD group is interesting and is discussed further below.
For all SCIFC variables combined across all groups, 80%+ agreement was obtained in 85% of cases (1966 of 2308 cases).
Capacity Judgment Outcomes Across Groups
Table 4 presents physician capacity judgment outcomes (capable, marginally capable, or incapable) across SCIFC variables and groups. Between group differences (p<.01) were found for all domains and overall capacity, with increasing proportions of impairment (marginally capable and incapable outcomes) on the SCIFC variables associated with increasing disease severity.
Table 4.
Group Differences in SCIFC Judgment Outcomes across All Physician Raters
| Controls N = 75 | MCI N = 58 | Mild AD N = 97 | Moderate AD N = 31 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Capable | Marginally Capable | Incapable | Capable | Marginally Capable | Incapable | Capable | Marginally Capable | Incapable | Capable | Marginally Capable | Incapable | |
| D1 Basic Monetary Skills c,d,e,f | 344 (98%) |
8 | 1 | 281 (99%) |
1 | 0 | 435 (92%) |
27 | 13 | 102 (66%) |
18 | 35 |
| D2 Financial Knowledge b,c,d,e,f | 348 (99%) |
5 | 0 | 280 (99%) |
1 | 0 | 379 (82%) |
72 | 11 | 77 (50%) |
49 | 29 |
| D3 Cash Transactions b,c,d,e,f | 341 (97%) |
12 | 0 | 273 (97%) |
9 | 0 | 333 (70%) |
92 | 50 | 50 (32%) |
49 | 56 |
| D4 Checkbook Mgmt b,c,d,e | 339 (95%) |
15 | 2 | 226 (85%) |
27 | 14 | 144 (32%) |
82 | 220 | 15 (10%) |
14 | 115 |
| D5 Bank Statement Mgmt a,b,c,d,e,f | 333 (93%) |
22 | 2 | 193 (72%) |
65 | 11 | 145 (33%) |
128 | 162 | 6 (4%) |
15 | 116 |
| D6 Financial Judgment b,c,d,e,f | 306 (92%) |
27 | 0 | 234 (83%) |
41 | 7 | 215 (47%) |
126 | 119 | 27 (19%) |
48 | 70 |
| D7 Bill Payment b,c,d,e,f | 326 (98%) |
7 | 0 | 262 (93%) |
16 | 4 | 294 (65%) |
105 | 56 | 32 (22%) |
49 | 64 |
| D8 Knowledge Assets/Estate b,c,d,e,f | 319 (96%) |
13 | 1 | 256 (91%) |
25 | 1 | 296 (62%) |
141 | 38 | 44 (28%) |
71 | 40 |
| Overall Financial Capacity a,b,c,d,e,f |
315 (95%) |
18 (05%) |
0 (0%) |
231 (82%) |
44 (16%) |
7 (2%) |
125 (26%) |
175 (37%) |
176 (37%) |
6 (4%) |
32 (21%) |
117 (75%) |
Note. Cell numbers reflect capacity judgments drawn from all five physician raters. Percentage (%) indicates percentage of capacity judgments rated as capable by group and SCIFC variable across all raters. For overall financial capacity, percentages (%) for all three capacity judgments were included.
Post-hoc analyses
Control judgment outcome distribution significantly different than MCI judgment outcome distribution at p < .01.
Control judgment outcome distribution significantly different than mild AD at p < .01.
Control judgment outcome distribution significantly different than moderate AD at p < .01
MCI judgment outcome distribution significantly different than mild AD at p < .01.
MCI judgment outcome distribution significantly different than moderate AD p < .01.
Mild AD judgment outcome distribution significantly different than moderate AD at p < .01.
Relative to controls, MCI patients were impaired on Bank Statement Management and on overall financial capacity. In addition, trends emerged on Checkbook Management (p=.060) and Financial Judgment (p=.062). Relative to controls and MCI patients, mild AD patients were impaired on all domains (except Basic Monetary Skills) and on overall financial capacity. Relative to controls and MCI patients, moderate AD patients were impaired on all SCIFC variables. In addition, relative to mild AD patients, moderate AD patients were impaired on all domains (except Checkbook Management and Bill Payment), and on overall financial capacity.
Examination of judgment outcomes by group revealed that for overall financial capacity, controls were rated as capable in 95% of judgments (see Table 4 and Figure 1). At the domain level, controls had as high as 99% capable judgments (Financial Concepts), with a low of 92% (Financial Judgment). Marginally capable outcomes constituted between 2% and 8% of judgments, while incapable outcomes represented less than 1%.
Figure 1.
Judgment Outcomes by Percentage and Group for Selected SCIFC Variables
In contrast, judgments for MCI patients reflected the emergence of mild impairments in financial capacity (Table 4 and Figure 1). While MCI patients were rated as capable in at least 93% of judgments on four domains (Basic Monetary Skills, Financial Concepts, Cash Transactions, and Bill Payment), they performed less well on domains of Checkbook Management (85% capable judgments) and Financial Judgment (83%), and showed a statistically significant deficit on Bank Statement Management (72% capable and 24% marginally capable judgments). In addition, a deficit emerged for overall financial capacity, with only 82% of judgments for MCI patients rated capable, and another 16% rated marginally capable. These findings suggest emerging financial deficits in MCI patients.
Mild AD patients demonstrated global deficits in financial capacity (Table 4 and Figure 1). For overall financial capacity, only 26% of judgments were rated capable (37% marginally capable and 37% incapable judgments), reflecting a marked loss of financial skills relative to controls and MCI patients. At the domain level, there were 70% or less capable judgments on five domains, with less than 50% capable judgments for three complex domains (Checkbook Management, Bank Statement Management, and Financial Judgment).
The moderate AD group demonstrated advanced global impairment on the SCIFC variables. For overall financial capacity, only 4% of judgments were rated capable. At the domain level, there was less than 50% capable judgment ratings on six of seven core domains, and less than 25% capable outcomes on four complex domains (Checkbook Management, Bank Statement Management, Financial Judgment, and Bill Payment).
DISCUSSION
In our aging society, physicians and other clinicians are increasingly asked to address issues of financial capacity in older adults with cognitive impairment and dementia. However, clinicians have lacked the training, experience, and clinical tools for undertaking these important assessments28, 29. The present study used a clinician-based interview to assess financial capacity in older adults representing the dementia spectrum. Using this interview, experienced physicians reliably distinguished the financial skills of cognitively normal older adults, patients with amnestic MCI, and patients with mild and moderate AD.
The present study found that the SCIFC achieved very good levels of judgment consistency in a sample representing the dementia continuum. Across the seven core financial domains, the mean level of acceptable judgment agreement (80%+) occurred in 97% of cases for older controls, 92% of cases for MCI, 80% of cases for mild AD, and 77% of cases for moderate AD. For overall financial capacity, acceptable agreement occurred in 91% of control cases, 90% of MCI cases, 84% of moderate AD cases, and 69% of mild AD cases. The agreement level was somewhat lower for mild AD patients, as this group with its mixture of deficits and preserved skills generally presents the greatest ambiguity for physician raters30. As a reflection of this, physician ratings of overall capacity were effectively dichotomous for the control and MCI groups (almost entirely capable vs. marginally capable outcomes), dichotomous for moderate AD patients (marginally capable vs. incapable outcomes), but fully trichotomous for mild AD patients (relatively equal proportions of capable, marginally capable, and incapable outcomes).
The SCIFC demonstrated construct validity by discriminating judgment outcomes across the four groups, with increasing impairment of financial skills (higher proportions of marginal and incapable outcomes) corresponding to dementia stage and increasing disease severity. MCI patients demonstrated impairments on the Bank Statement Management domain and on overall financial capacity, with trends for the domains of Financial Judgment and Checkbook Management. Thus, as judged by experienced physicians, some patients with MCI showed mild impairments on more complex financial domains and on overall financial capacity. These findings replicate several findings from our group’s prior psychometric study of financial capacity in MCI12. The clinical implication is that upon receiving a diagnosis of amnestic MCI, patients and their families should proactively engage in financial and legal planning, in anticipation of possibly developing AD and corresponding increased loss of financial abilities.
Compared to both older controls and MCI patients, mild AD patients demonstrated significant impairments on all financial domains (with the exception of Basic Monetary Skills) and on overall financial capacity. The findings also replicate findings from our prior psychometric study of financial capacity13 indicating that in mild AD there is emerging global impairment of financial skills. In comparison to mild AD patients, moderate AD patients showed impairment on all SCIFC variables (except possibly Checkbook Management). These findings were indicative of advanced, global impairment of financial skills found at the moderate dementia stage13.
The present study has several limitations. First, the study physicians served in dual roles of assisting with instrument development and of rating the capacity of study participants. Their collaborative efforts in instrument development may have inflated judgment reliability levels to some degree. Future studies should examine SCIFC rater agreement using non-study related physicians, and also other clinician disciplines (eg., clinical psychologists, nurses, social workers), in order to strengthen the generalizability of current findings regarding the SCIFC’s reliability and validity, and evaluate its broader utility in clinical settings. Many busy physicians may not be able to conduct a 25 minute interview themselves, whereas one of their clinical staff could. In our judgment, the SCIFC has the potential to be used effectively by a range of clinical staff with varying experience levels, if such clinicians are provided with an administration protocol and appropriate training.
Second, although physician capacity outcomes varied as anticipated across disease severity, they were not evaluated in terms of an external validity criterion. This makes it difficult to assess how well the SCIFC performance corresponds to actual “real world” financial capacity outcomes. Currently there is not an accepted gold standard for evaluating clinical judgments of financial capacity, or other capacities for that matter. MCI and AD patient self report, and also family report, of financial capacity have not always proven to be a reliable criterion31, 32. Psychometric testing of financial capacity in a laboratory setting is a possible external criterion31, 32, but is also limited by issues of ecological validity and psychometric norming techniques. The issue of establishing external validity in capacity studies is important, as it affects the ultimate confidence that can be extended to use of capacity measures in clinical practice.
Third, the number of physician raters was limited to five. However, each physician had experience in geriatric assessment, had diverse training backgrounds (e.g., geriatrics, psychiatry, neurology), and had clinical experience making capacity judgments. In prior research26, 30 we have found that using five physicians with varied specialty backgrounds supports a stable consensus judgment outcome, and provides a stronger modal central tendency than a smaller number.
Fourth, the interview/videotaping format limited the ability of the four reviewing clinicians to fully apply their own clinical skills and knowledge to the case. However, videotaping was essential methodologically to avoid confounds and logistical challenges associated with multiple clinician interviews of the same participant. Finally, the study sample, although relatively large, was obtained from a single clinical setting with limited generalization of findings.
Our study provides initial support for the value of a semi-structured, interview approach for assessing financial capacity in older adults with cognitive impairment and dementia. This approach provides the structure necessary for attaining reliable and valid assessments, but also permits the clinical flexibility needed for individualized assessments of patients in clinical care settings2, 33. The clinician is able to draw upon their experience and intuition in making these important clinical decisions34. The SCIFC also has the advantage of being derived from a conceptual model of financial capacity35 with clinically relevant financial domains. A domain-based approach allows the clinician to pre-select areas of assessment, and also to determine areas of independent function and preserved autonomy versus areas of deficit requiring supervision or direct intervention. Finally, as noted above, additional study of the SCIFC instrument and approach is needed to extend and strengthen the current findings of reliability and validity, in particular studies in naturalistic clinical settings involving both physician and non-physician clinicians.
ACKNOWLEDGMENT
Funding Sources: Supported by research grants MH55247 (National Institute of Mental Health) and AG024525, AG021927, P50AG16582 (National Institute on Aging)
The authors thank the staff of the Neuropsychology Laboratory for their assistance with testing participants. The authors also express particular gratitude to Dr. Jonathan Williams of the Department of Pharmacology at Oxford University, England for his valuable statistical advice and consultation.
Role of the Sponsor: The funding source had no role in the design or conduct of the study, data management or analysis, or manuscript preparation
Footnotes
Portions of this paper were presented at the 10th International Conference on Alzheimer’s Disease held in Madrid, Spain on July 15–20, 2006.
The capacity assessment measure used in this study is copyrighted and owned by the UAB Research Foundation. None of the authors or the UAB Research Foundation receives royalty or other income regarding this instrument.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Financial Disclosures: No relationships reported.
REFERENCES
- 1.Appelbaum P, Grisso T, Frank E, et al. Competence of depressed patients for consent to resesearch. Am J Psychiatry. 1999;156:1380–1384. doi: 10.1176/ajp.156.9.1380. [DOI] [PubMed] [Google Scholar]
- 2.Kim S, Karlawish JH, Caine E. Current state of research on decision-making competence of cognitively impaired elderly persons. Am J Geriatr Psychiatry. 2002;10:151–165. [PubMed] [Google Scholar]
- 3.Kim S, Cox C, Caine E. Impaired decision-making ability in subjects with Alzheimer's disease and willingness to participate in research. American Journal of Psychiatry. 2002;159:797–802. doi: 10.1176/appi.ajp.159.5.797. [DOI] [PubMed] [Google Scholar]
- 4.Etchells E, Darzins P, Silberfeld M, et al. Assessment of patient capacity to consent to treatment. J Gen Intern Med. 1999;14:27–34. doi: 10.1046/j.1525-1497.1999.00277.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marson D, Sawrie S, Snyder S, et al. Assessing financial capacity in patients with Alzheimer disease: A conceptual model and prototype instrument. Arch Neurol. 2000;57:877–884. doi: 10.1001/archneur.57.6.877. [DOI] [PubMed] [Google Scholar]
- 6.Melton G, Petrila J, Poythress N. Psychological Evaluations for the Courts. New York: Guilford Press; 1987. [Google Scholar]
- 7.Marson D. Loss of financial capacity in dementia: Conceptual and empirical approaches. Aging Neuropsychol Cogn. 2001;8:164–181. [Google Scholar]
- 8.Kane R, Kane R. Assessing the Elderly: A Practical Guide to Measurement. Lexington, MA: Lexington: 1981. [Google Scholar]
- 9.Lawton MP. Competence, environmental press, and adaptation of older people. In: Lawton MP, Windley P, Byerts I, editors. Aging and the Environment: Theoretical Approaches. New York: Springer; 1982. pp. 33–59. [Google Scholar]
- 10.Marson D, Zebley L. The other side of the retirement years: Cognitive decline, dementia, and loss of financial capacity. J Retirement Planning. 2001;4:30–39. [Google Scholar]
- 11.Willis S. Everyday cognitive competence in elderly persons: Conceptual issues and empirical findings. Gerontologist. 1996b;36:595–601. doi: 10.1093/geront/36.5.595. [DOI] [PubMed] [Google Scholar]
- 12.Griffith HR, Belue K, Sicola A, et al. Impaired financial abilities in mild cognitive impairment: A direct assessment approach. Neurology. 2003;60:449–457. doi: 10.1212/wnl.60.3.449. [DOI] [PubMed] [Google Scholar]
- 13.Martin R, Griffith HR, Belue K, et al. Declining Financial Capacity in Patients With Mild Alzheimer Disease: A One-Year Longitudinal Study. Am J Geriatr Psychiatry. 2008;16:209–219. doi: 10.1097/JGP.0b013e318157cb00. [DOI] [PubMed] [Google Scholar]
- 14.Nerenberg L. Financial Abuse of the Elderly. Washington, D.C:: National Center on Elder Abuse; 1996. [Google Scholar]
- 15.As A. New research points to methods of improving primary care in Alzheimer's. Alzheimers Association Media Line. 2006 [Google Scholar]
- 16.Earnst K, Wadley V, Aldridge T, et al. Loss of financial capacity in Alzheimer's disease: The role of working memory. Aging Neuropsychol Cogn. 2001;8:109–119. [Google Scholar]
- 17.Loeb P. Independent Living Scales Manual. San Antonio: The Psychological Corporation; 1996. [Google Scholar]
- 18.Mahurin R, DeBettignies B, Pirozzolo F. Structured assessment of independent living skills: Preliminary report of a performance measure of functional abilities in dementia. J Gerontol. 1991;46:P58–P66. doi: 10.1093/geronj/46.2.p58. [DOI] [PubMed] [Google Scholar]
- 19.Okonkwo O, Griffith HR, Belue K, et al. Medical decision-making capacity in patients with mild cognitive impairment. Neurology. 2007;69:1528–1535. doi: 10.1212/01.wnl.0000277639.90611.d9. [DOI] [PubMed] [Google Scholar]
- 20.Marson DC, Ingram KK, Cody HA, et al. Assessing the competency of patients with Alzheimer's disease under different legal standards. Arch Neurol. 1995;52:949–954. doi: 10.1001/archneur.1995.00540340029010. [DOI] [PubMed] [Google Scholar]
- 21.Morris J. The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology. 1993;43:2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 22.Folstein M, Folstein S, McHugh P. Mini-Mental State: A practical guide for grading the cognitive state of the patient for the physician. J Psychiatry Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 23.Mattis S. Dementia rating scale. In: Bellack R, Karasu B, editors. Geriatric Psychiatry. New York: Grune & Stratton; 1976. [Google Scholar]
- 24.Petersen RC, Doody R, Kurz A, et al. Current concepts in mild cognitive impairment. Arch Neurol. 2001 Dec;58(12):1985–1992. doi: 10.1001/archneur.58.12.1985. [DOI] [PubMed] [Google Scholar]
- 25.McKhann G, Drachman D, Folstein M, et al. Clinical diagnosis of Alzheimer's disease: Report of the NINCDS-ADRDA work group under the auspices of the Department of Health and Human Services Task Force on Alzheimer's disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 26.Marson DC, McInturff B, Hawkins L, et al. Consistency of physician judgments of capacity to consent in mild Alzheimer's disease. J Am Geriatr Soc. 1997;45:453–457. doi: 10.1111/j.1532-5415.1997.tb05170.x. [DOI] [PubMed] [Google Scholar]
- 27.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 28.Ganzini L, Volicer L, Nelson W, et al. Pitfalls in assessment of decision -making capacity. Psychosomatics. 2003;44:237–243. doi: 10.1176/appi.psy.44.3.237. [DOI] [PubMed] [Google Scholar]
- 29.Carrese J. Refusal of care: Patients' well-being and physicians' ethical obligations. JAMA. 2006;296:691–695. doi: 10.1001/jama.296.6.691. [DOI] [PubMed] [Google Scholar]
- 30.Marson D, Earnst K, Jamil F, et al. Consistency of physicians' legal standard and personal judgments of competency in patients with Alzheimer's disease. J Am Geriatr Soc. 2000;48:911–918. doi: 10.1111/j.1532-5415.2000.tb06887.x. [DOI] [PubMed] [Google Scholar]
- 31.Okonkwo O, Griffith H, Copeland J, et al. Medical decision-making capacity in mild cognitive impairment: A 3-year longitudinal study. Neurology. 2008;71:1474–1480. doi: 10.1212/01.wnl.0000334301.32358.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wadley VG, Harrell LE, Marson DC. Self- and informant report of financial abilities in patients with Alzheimer's disease: Reliable and valid? J Am Geriatr Soc. 2003;51:1621–1626. doi: 10.1046/j.1532-5415.2003.51514.x. [DOI] [PubMed] [Google Scholar]
- 33.Grisso T, Appelbaum P, Hill-Fotouhi C. The MacCAT-T: A clinical tool to assess patients' capacities to make treatment decisions. Psychiatric Serv. 1997;48:1315–1319. doi: 10.1176/ps.48.11.1415. [DOI] [PubMed] [Google Scholar]
- 34.Epstein RM, Alper BS, Quill TE. Communicating evidence for participatory decision making. JAMA. 2004;291:2359–2366. doi: 10.1001/jama.291.19.2359. [DOI] [PubMed] [Google Scholar]
- 35.Marson D, Dymek M, Geyer J. Ethical and legal issues of clinical care and research. In: Clark C, Trojanowski, editors. Neurodegenerative Dementias. 2000. [Google Scholar]