Abstract
Glandular odontogenic cyst (GOC) is an uncommon jaw bone cyst of odontogenic origin described in 1987 by Gardner et al. It is a cyst having an unpredictable and potentially aggressive behaviour. It also has the propensity to grow to a large size and tendency to recur with only 111 cases having been reported thus far. The first case occurred in a 42-year-old female and presented as a localized swelling extending from 19 to 29 regions. There was a history of traumatic injury at the site. There was evidence of bicortical expansion and radiographs revealed a multilocular radiolucency. The second case occurred in a 21-year-old male, as a large swelling in the mandible and radiograph revealed radiolucency in the region. On histopathological examination, these lesions were diagnosed as GOC. It was concluded that, two cases submitted by us correlate with the existing literature that GOC’s affect more commonly in the middle age group, having predilection for mandible and that trauma could be a precipitating factor for its occurrence. The increased recurrence rates can be due to its intrinsic biological behavior, multilocularity of the cyst, and incomplete removal of the lining following conservative treatment.
Keywords: Glandular odontogenic cyst, Mucous cells, Cilia
Introduction
Glandular odontogenic cyst (GOC) is an uncommon jaw bone cyst of odontogenic origin, first described in 1988 by Gardner et al. [1] as a distinct clinicopathologic entity. In 1987, Padayachee and Van Wyk [2] reported two cases that were similar to Botryoid odontogenic cyst (BOC) but with a glandular element and proposed the term ‘Sialo odontogenic cyst’. The GOC is included in the WHO histologic typing of odontogenic tumors under the terms GOC or Sialo odontogenic cyst [3]. To the best of our knowledge, only 111 cases of GOC has been reported in the literature [4] and Magnusson et al. [5] observed that only 0.012% of the cysts seen on the oral cavity have fulfilled the criteria of GOC microscopically.
Clinically, the most common site of occurrence is mandibular anterior region, presenting as an asymptomatic slow growing swelling [6]. GOC occurs mostly in the middle age and has a slight male predilection [5, 7–12]. Radiologically, these cysts may be unilocular or multilocular with a well-defined border [6, 11, 13]. Histologically, GOC is characterized by a cyst wall lining of non-keratinized epithelium, with papillary projections, nodular thickenings, mucous filled clefts, and ‘mucous lakes’. It also includes cuboidal basal cells, sometimes vacuolated [7, 12]. Treatment of GOC includes curettage and enucleation, although some authors believe marginal resection to be more reliable treatment, due to tendency of the cyst to recur after curettage and enucleation [7].
In this article, we present two new cases of GOC and focus on the review of clinico-pathologic features, biologic behavior, and features of the lesion considered in the differential diagnosis, which can be often challenging.
Case Report 1
A 42-year-old Indian female patient was referred to our hospital for the complaint of swelling in the anterior mandible for the past 15 years. The patient was asymptomatic except for mild pain for the past 2 years. She had suffered trauma to the chin 2 years earlier and subsequently had undergone surgery to treat a swelling in that area. She was unable to provide further information regarding that surgery and histopathological report of the biopsy was not available.
Intraoral examination, revealed an expansile fluctuant swelling extending from 19 to 29 regions (Fig. 1). The overlying mucosa was of normal colour and appearance. Patient had a removable denture replacing the missing anteriors. There was no sensory loss or any other obvious signs of infection.
Fig. 1.
Clinical picture showing fluctuant swelling extending from 19 to 29 regions
Panoramic radiograph revealed multilocular radiolucency extending from 19 to 29 regions along with expansion and thinning of buccal and lingual cortical plates (Fig. 2). The provisional diagnosis of Ameloblastoma was given. Aspiration yielded a serous brownish red colored fluid. An incisional biopsy was done and the specimen was sent for histopathological examination. On macroscopic examination, there were two irregular fragments of tissue which was 0.5 × 0.1 cm in dimension, brownish in color, and firm in consistency.
Fig. 2.
Panoramic radiograph showing large multilocular radiolucency and thinning of buccal and lingual cortex extending from 19 to 29 regions
Histopathologic examination revealed fragments of cyst wall lined by stratified squamous epithelium of varying thickness along with epithelial whorls in few areas. The superficial layer of the epithelium showed eosinophilic cuboidal and columnar ciliated cells. PAS staining revealed numerous PAS positive mucous cell and few pseudo glandular structures were seen throughout the lining epithelium. The connective tissue wall consisted of numerous cholesterol clefts, moderate chronic inflammatory cell infiltrate, and hemorrhage. The histopathological diagnosis was GOC (Figs. 3, 4, 5). The lesion was treated by en bloc resection. The specimen was analyzed microscopically and histopathology was consistent with the incisional biopsy report.
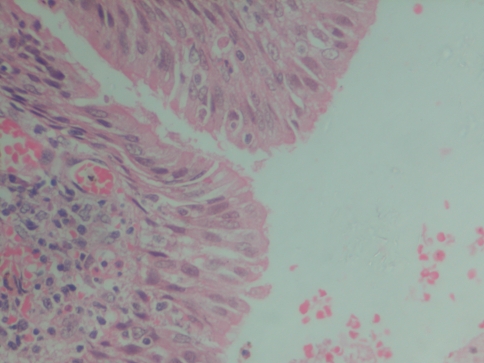
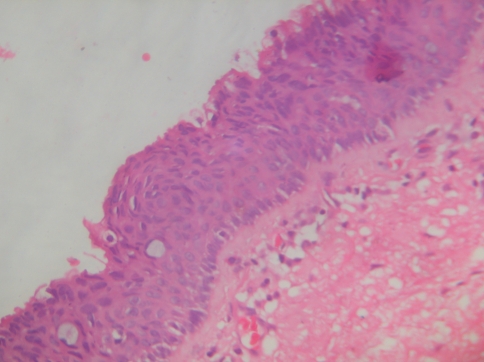
Fig. 3.
Photomicrograph showing superficial layer of the epithelium with eosinophilic cuboidal and columnar ciliated cells along with papillary projections (40×)
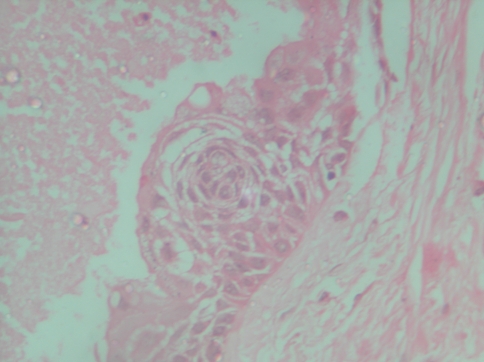
Fig. 4.
Photomicrograph showing epithelial whorls within the lining epithelium (40×)
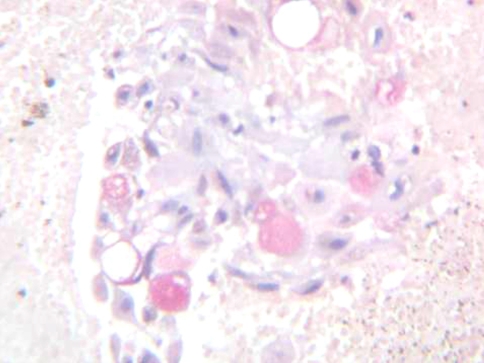
Fig. 5.
Photomicrograph showing Periodic Acid Schiff positive mucous cells within the epithelium (40×)
Case Report 2
A 21-year-old Indian male patient reported with an asymptomatic diffuse swelling in the left side of the face extending superiorly from the middle third of face, inferiorly to the lower border of the mandible, anteriorly to the corner of mouth, and posteriorly to the tragus of the ear (Fig. 6).
Fig. 6.
Extra oral picture showing a diffuse swelling in the left side of the face extending from lower border of the mandible to the middle third of face
Intra oral examination revealed 3 × 2 cm swelling obliterating the buccal vestibule extending from 17 to 21 regions. A panoramic radiograph revealed a 7 × 3 cm, multilocular radiolucency extending into the ramus region with no apparent root resorption of the involved teeth (Fig. 7). The clinical provisional diagnosis was Ameloblastoma.
Fig. 7.
Panoramic radiograph showing multilocular radiolucency extending from midline till ascending ramus region
Further an incisional biopsy was performed and sent for histopathological examination. Grossly, the specimen was grayish white in colour measuring 2 × 1 cm in size and firm in consistency.
Histopathological examination showed non-keratinized stratified squamous epithelium of variable thickness with evidence of pseudo glandular structures with PAS positive mucous cells. Epithelial theques and papillary projections were evident in few areas. There was also evidence of few inflammatory cells and few cholesterol clefts within the connective tissue wall. Histopathology was suggestive of GOC (Figs. 8, 9, 10).
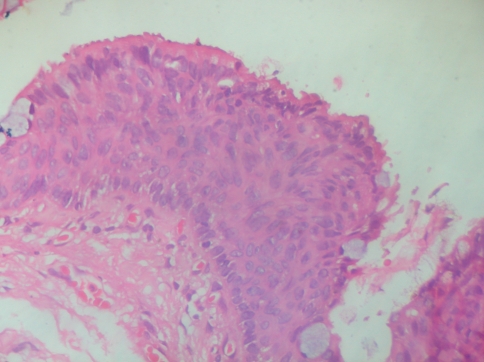
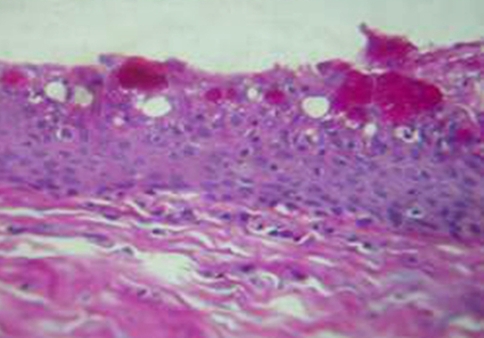
Fig. 8.
Photomicrograph showing papillary projections, epithelial whorls, and mucous cells (40×)
Fig. 9.
Photomicrograph showing superficial columnar cells and whorling of the epithelial cells (40×)
Fig. 10.
Photomicrograph showing pseudo glandular structures with PAS positive mucous cells (40×)
Based on histopathology the patient underwent en bloc resection. Microscopic examination of the resected specimen confirmed the previous diagnosis. Both the patients are under follow-up and are symptom free for past 2 years.
To assess the proliferate nature of both the cases an immunohistochemical staining was done using Ki 67 and was found to be not reactive.
Discussion
The GOC is a rare lesion with a frequency rate of only 0.012% [5] to 1.3% [14] of all the jaw cysts and its prevalence is 0.17% [15]. Literature review shows that GOC may mimic a wide clinicopathologic spectrum ranging from lateral periodontal cyst to a destructive malignant neoplasm such as Central Mucoepidermoid Carcinoma [1–3, 5–7, 11–13, 16–21].
Our literature search revealed 111 cases of GOC in the English literature [4, 15, 22–24]. There is a slight male predilection and lesions occur mostly in middle aged patients. In our cases, one was middle aged female and other was a young male patient. This corroborates with what has been reported in the literature that is males are generally affected at a younger age as compared to females [9, 10, 13, 25].
Earlier reports indicate that GOC’s were found predominantly reported in the anterior mandible, but in the current case reports one case showed extension from left mandibular premolar to molar region [2, 5, 7, 9, 10, 15, 25].
Radiographically, the GOC is localized intraosseously and may appear as a multilocular or unilocular radiolucent lesion with well-defined borders. Sometimes it may present with peripheral osteosclerotic border and scalloping, root resorption and displacement of the teeth. The clinical and radiographic findings of GOC are varied and often not pathognomonic and usually, it presents as asymptomatic slow growing lesion but occasionally may be accompanied by pain [13, 26].
The water clear, low viscosity aspiration fluid content may be a helpful clinical indication of GOC, and a preoperative aspiration and fluid inspection may be advisable. But in contrast, brownish-red aspirate was obtained from one of our case, which can be attributed to blood, perhaps because of previous surgery [6, 27].
Histopathologically the present two cases consisted of certain characteristic features of GOC like non-keratinized stratified epithelium, epithelial whorls or spheres within the lining, eosinophilic cuboidal or columnar cells which are occasionally ciliated and presence of mucous cells with microcystic areas [1, 2, 28].
The mucous cells in the present case reports were PAS positive and are considered to be of metaplastic in origin. Mucous cells occur in many intraosseous odontogenic cysts; however, in GOC’s they are remarkably abundant. The vacuolated and clear cells observed near the mucous cells may represent an initial stage in the histogenesis of mucous cell metaplasia [29–31].
Epithelial plaques or whorls may also be seen in lateral periodontal cyst and BOC, thereby pointing towards the odontogenic nature of GOC [1, 2]. These areas of epithelial thickening may be comparable to the proliferative changes seen in dental lamina [6]. Immunohistochemical studies using cytokeratin-7, 13, 14 and 19 and their positivity strongly support the odontogenic nature of GOC [32]. The identification of osteodentin [27] and negative reaction for EMA [33] in the area of glandular structures suggest that these features are not of glandular origin and support the concept of odontogenic differentiation in GOC.
Histopathologically GOC should be differentiated from Lateral Periodontal Cyst, BOC, and Central Mucoepidermoid Carcinoma as they exhibit considerable overlap of histological features. LPC is a developmental odontogenic cyst lined by thin non-keratinized epithelium and also exhibits focal epithelial thickenings and glycogen rich epithelial cells, similar to those observed in GOC’s [18, 34]. BOC is a locally aggressive polycystic variant of LPC [18], shows similar histomorphologic feature with those of GOC, like epithelial plaques and areas of glycogen rich clear cells [35]. However, the identification of ciliated epithelium and duct like spaces with mucous cells specifically differentiated from LPC and BOC and favors the diagnosis of GOC’s [3, 27, 32].
The differentiation of low grade Central Mucoepidermoid Carcinoma from GOC especially its multicystic variant is more important and difficult. Significant histological overlap exists between GOC and CMEC. However, superficial cuboidal cells, epithelial whorls, ciliated cells, and intraepithelial microcyst or duct like structures are not typical for CMEC and their presence or absence can help in establishing a definitive diagnosis [36]. Immunostaining with CK-18 and 19 and their positivity in GOC may help in differentiating GOC from CMEC [37]. Certain studies demonstrated that the use of IHC for p-53 and Ki-67 can help the clinician in differentiating GOC from CMEC. GOC exhibited decreased p-53 positivity and increased Ki-67 index when compared to CMEC [36].
Several studies indicate that GOC is a relatively aggressive lesion with a high tendency for erosion or perforation of the cortical plates as well as a high recurrence rate [12]. The aggressive biologic behavior of GOC and its propensity for recurrence might be associated with cell kinetics in the lining epithelium [36].
Certain studies have reported an increased Ki-67 index and decreased P53 positivity suggesting that GOC lining displays increased proliferation, but not malignant transformation potential [36]. Tosios et al. [38] demonstrated increased Bcl2 which is an anti-apoptotic protein suggesting that the biological behavior of GOC is associated with dysregulation of cell death in lining epithelium.
But in contrast, few studies based on immunostaining using P53, Ki-67, and Bcl2 have suggested that biologic behavior of GOC was not associated with cell proliferation and high recurrence rate is due to its multilocular nature and the tendency of the epithelium to separate from the connective tissue [15, 38]. The non reactivity of Ki-67 in our cases can be attributed to the above suggested explanation.
Another factor responsible for increased recurrence rate is the conservative treatment method [7, 8, 25]. Multicystic lesions treated by curettage or enucleation demonstrated increased recurrence rate of 55% with an average of 4.9 years [8]. The mechanism of recurrence may be partly attributed to the thinness of the cyst wall and to the presence of microcysts making the complete removal at surgery difficult.
The treatment of choice is still controversial and ranges from curettage, enucleation, en bloc [26] and partial osteotomy [17, 39]. The present two cases underwent en bloc resection due to their clinical and pathological aggressive behavior. In view of high recurrence rate associated with conservative treatment of the cysts and their invasive potential, we suggest a more aggressive removal over conservative approach and a careful long follow up is also essential.
In conclusion this case report of GOC’s will add to the existing knowledge of these rare cysts. GOC’s are common in middle age group, having predilection for mandible and trauma could be a precipitating factor for its occurrence. The increased recurrence rates can be due to its intrinsic biological behavior, multilocularity of the cyst and incomplete removal of the lining following conservative treatment.
References
- 1.Gardner DG, Kessler HP, Morency R, Schaner DL. The glandular odontogenic cyst: an apparent entity. J Oral Pathol. 1988;17:359–366. doi: 10.1111/j.1600-0714.1988.tb01298.x. [DOI] [PubMed] [Google Scholar]
- 2.Padayachee A, Wyk CW. Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumour: sialo-odontogenic cyst? J Oral Pathol. 1987;16:499–504. doi: 10.1111/j.1600-0714.1987.tb00680.x. [DOI] [PubMed] [Google Scholar]
- 3.Kramer IRH, Pindborg JJ, Shear M. Histological typing of odontogenic tumors. 2. Berlin: Springer; 1992. [DOI] [PubMed] [Google Scholar]
- 4.Kaplan I, Anavi Y, Hirshberg A. Glandular odontogenic cyst: a challenge in diagnosis and treatment. Oral Dis. 2008;14:575–581. doi: 10.1111/j.1601-0825.2007.01428.x. [DOI] [PubMed] [Google Scholar]
- 5.Magnussson B, Goransson L, Odesjo B, Grondahl K, Hirsch JM. Glandular odontogenic cyst: report of seven cases. Dentomaxillofac Radiol. 1997;26:26. doi: 10.1038/sj.dmfr.4600205. [DOI] [PubMed] [Google Scholar]
- 6.Junior OF, Azevedo LR, Sant’ana E, et al. Case report and review of literature. Quintessence Int. 2004;35:385. [PubMed] [Google Scholar]
- 7.Gardner GD, Morency R. The glandular odontogenic cyst, a rare lesion that tends to recur. J Can Dent Assoc. 1993;59:929. [PubMed] [Google Scholar]
- 8.Hussain K, Edmondson HD, Browne RM. Glandular odontogenic cysts: diagnosis and treatment—Review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79(5):593–602. doi: 10.1016/S1079-2104(05)80101-5. [DOI] [PubMed] [Google Scholar]
- 9.Patron M, Colmero C, Larrauri J. Glandular odontogenic cyst: clinicopathologic analysis of three cases. Oral Surg Oral Med Oral Pathol. 1991;72:71–74. doi: 10.1016/0030-4220(91)90192-F. [DOI] [PubMed] [Google Scholar]
- 10.Toida M, Nakashima E, Okumura Y, Tatematsu N. Glandular odontogenic cyst: a case report and literature review. J Oral Maxillofac Surg. 1994;52:1312–1316. doi: 10.1016/0278-2391(94)90054-X. [DOI] [PubMed] [Google Scholar]
- 11.Tran PT, Cunningham CJ, Baughman RA. Glandular odontogenic cyst. J Endod. 2004;30:182. doi: 10.1097/00004770-200403000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Manor R, Anavi Y, Kaplan I, Calderon S. Radiological features of glandular odontogenic cyst. Dentomaxillofac Radiol. 2003;32:73–79. doi: 10.1259/dmfr/22912856. [DOI] [PubMed] [Google Scholar]
- 13.Noffke C, Raubenheimer EJ. The glandular odontogenic cyst: clinical and Radiological features; review of literature and report of nine cases. Dentomaxillofac Radiol. 2002;31:333. doi: 10.1038/sj.dmfr.4600730. [DOI] [PubMed] [Google Scholar]
- 14.Heerden WFP, Raubenheimer EJ, Turner MJ. Glandular odontogenic cyst. Head Neck. 1992;14:316–320. doi: 10.1002/hed.2880140412. [DOI] [PubMed] [Google Scholar]
- 15.Shen J, Fan M, Chen X, Wang S, Wang L, Li Y. Glandular odontogenic cyst in China: report of 12 cases and immunohistochemical study. J Oral Pathol Med. 2006;35:175–182. doi: 10.1111/j.1600-0714.2006.00389.x. [DOI] [PubMed] [Google Scholar]
- 16.Chavez JA, Richter KJ. Glandular odontogenic cyst of the mandible: review. J Oral Maxillofac Surg. 1999;57(4):461–464. doi: 10.1016/S0278-2391(99)90291-4. [DOI] [PubMed] [Google Scholar]
- 17.Takeda Y. Glandular odontogenic cyst mimicking a lateral periodontal cyst: a case report. Int J Oral Maxillofac Surg. 1994;23:96–97. doi: 10.1016/S0901-5027(05)80600-9. [DOI] [PubMed] [Google Scholar]
- 18.Regezi JA. Odontogenic cysts, odontogenic tumors, fibrosseous and giant cell lesions of the jaws. Mod Pathol. 2002;15:33. doi: 10.1038/modpathol.3880527. [DOI] [PubMed] [Google Scholar]
- 19.Geist J, Gordon S, Wesley R. Oral pathology quiz: an unusual pericoronal cyst. J Mich Dent Assoc. 2003;85:40. [PubMed] [Google Scholar]
- 20.Ide F, Shimoyama T, Horie N. Glandular odontogenic cyst with hyaline bodies: an unusual dentigerous presentation. J Oral Pathol Med. 1996;25:401. doi: 10.1111/j.1600-0714.1996.tb00286.x. [DOI] [PubMed] [Google Scholar]
- 21.Waldron CA, Koh ML. Central mucoepidermoid carcinoma of the jaws: a report of four cases with analysis of the literature and discussion of the relationship to mucoepidermoid, sialodontogenic, and glandular odontogenic cysts. J Oral Maxillofac Surg. 1990;48:871–877. doi: 10.1016/0278-2391(90)90349-7. [DOI] [PubMed] [Google Scholar]
- 22.Velez I. Glandular odontogenic cyst. Report of two cases and review of the literature. N Y State Dent J. 2006;72(1):44–45. [PubMed] [Google Scholar]
- 23.Sittitavornwong S, Koehler JR, Said-Al-Naief N. Glandular odontogenic cyst of the anterior maxilla: case report and review of the literature. J Oral Maxillofac Surg. 2006;64:740–745. doi: 10.1016/j.joms.2005.12.024. [DOI] [PubMed] [Google Scholar]
- 24.Kasaboglu O, Basal Z, Usubutun A. Glandular odontogenic cyst presenting as a dentigerous cyst: a case report. J Oral Maxillofac Surg. 2006;64:731–733. doi: 10.1016/j.joms.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 25.Ramer M, Montazem A, Lane SL, Lumerman H. Glandular odontogenic cyst. Report of a case and review of the literature. Oral Surg Oral Med Oral Pathol. 1997;84:54–57. doi: 10.1016/s1079-2104(97)90295-x. [DOI] [PubMed] [Google Scholar]
- 26.Economopoulou P, Patrikiou A. Glandular odontogenic cyst of the maxilla: report of case. J Oral Maxillofac Surg. 1995;53(7):834–837. doi: 10.1016/0278-2391(95)90345-3. [DOI] [PubMed] [Google Scholar]
- 27.Koppang HS, Johannessen S, Haugen LIC, Haanaes HR, Solheim T, Donath K. Glandular odontogenic cyst (sialo-odontogenic cyst): a report of two cases and literature review of 45 previously reported cases. J Oral Pathol Med. 1998;27:455–462. doi: 10.1111/j.1600-0714.1998.tb01984.x. [DOI] [PubMed] [Google Scholar]
- 28.Ficarra G, Chou L, Panzoni E. Glandular odontogenic cyst (sialo-odontogenic cyst) Int J Oral Maxillofac Surg. 1990;19:331–333. doi: 10.1016/S0901-5027(05)80074-8. [DOI] [PubMed] [Google Scholar]
- 29.Bhatt V, Monaghan A, Brown AM, Rippin JW. Does the glandular odontogenic cyst require aggressive management? Oral Surg Oral Med Oral Pathol. 2001;92:249–251. doi: 10.1067/moe.2001.116510. [DOI] [PubMed] [Google Scholar]
- 30.Takeda Y, Oikawa Y, Furuya I, Satoh M, Yamamoto H. Mucous and ciliated cell metaplasia in epithelial linings of odontogenic inflammatory and developmental cysts. J Oral Sci. 2005;47(2):77–81. doi: 10.2334/josnusd.47.77. [DOI] [PubMed] [Google Scholar]
- 31.Slabbert H, Shear M, Altini M. Vacoulated cells and mucous metaplasia in the epithelial cell lining of residual and radicular cysts. J Oral Pathol Med. 1995;24:309–312. doi: 10.1111/j.1600-0714.1995.tb01190.x. [DOI] [PubMed] [Google Scholar]
- 32.Soussa SO, Cabexas NT, Oliveira PT, Araujo VC. Glandular odontogenic cyst report of a case with cytokeratin expression. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:478–483. doi: 10.1016/S1079-2104(97)90149-9. [DOI] [PubMed] [Google Scholar]
- 33.Semba I, Kitano M, Mimura T, Sonoda S, Miyawaki A. Case report. Glandular odontogenic cyst: analysis of cytokeratin expression and clinicopathological features. J Oral Pathol Med. 1994;23:377–382. doi: 10.1111/j.1600-0714.1994.tb00079.x. [DOI] [PubMed] [Google Scholar]
- 34.Shear M, Pindborg JJ. Microscopic features of the lateral periodontal cyst. Scand J Dent Res. 1975;83:103. doi: 10.1111/j.1600-0722.1975.tb00425.x. [DOI] [PubMed] [Google Scholar]
- 35.Gurol M, Burkes EJ, Jr, Jacoway J. Botryoid odontogenic cyst. Analysis of 33 cases. J Periodontol. 1995;66:1069. doi: 10.1902/jop.1995.66.12.1069. [DOI] [PubMed] [Google Scholar]
- 36.Kaplan I, Anavi Y, Manor R, Sulkes J, Calderon S. The use of molecular markers as an aid in the diagnosis of glandular odontogenic cyst. Oral Oncol. 2005;41:895–902. doi: 10.1016/j.oraloncology.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 37.Pires FR, Chen SY, Perez DEC, Almedia OP, Kowalski LP. Cytokeratin expression in central mucoepidermoid carcinoma and glandular odontogenic cyst. Oral Oncol. 2004;40:545–551. doi: 10.1016/j.oraloncology.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 38.Tosios KI, Kakarantza-Angelopoulou E, Kapranos N. Immunohistochemical study of Bcl2 protein, Ki 67 antigen and p53 protein in epithelium of glandular odontogenic cysts and dentigerous cysts. J Oral Pathol Med. 2000;29:139–144. doi: 10.1034/j.1600-0714.2000.290306.x. [DOI] [PubMed] [Google Scholar]
- 39.Kaplan I, Gal G, Anavi Y, Manor R, Calderon S. Glandular odontogenic cyst: treatment and recurrence. J Oral Maxillofac Surg. 2005;63:435–441. doi: 10.1016/j.joms.2004.08.007. [DOI] [PubMed] [Google Scholar]