Abstract
A disadvantage of several old vaccines is that the genetic events resulting in the attenuation are often largely unknown and reversion to virulence cannot be excluded. In the 1950s, a live vaccine strain, LVS, was developed from a type B strain of Francisella tularensis, the causative agent of tularemia. LVS, which is highly attenuated for humans but still virulent for mice by some infection routes, has been extensively studied and found to protect staff from laboratory-acquired tularemia. The efforts to improve biopreparedness have identified a demand for a vaccine against tularemia. Recently the rapid progress in genomics of different Francisella strains has led to identification of several regions of differences (RDs). Two genes carried within RDs, pilA, encoding a putative type IV pilin, and FTT0918, encoding an outer membrane protein, have been linked to virulence. Interestingly, LVS has lost these two genes via direct repeat-mediated deletions. Here we show that reintroduction of the two deleted regions restores virulence of LVS in a mouse infection model to a level indistinguishable from that of virulent type B strains. The identification of the two attenuating deletion events could facilitate the licensing of LVS for use in humans.
Francisella tularensis is the causative agent of tularemia, and natural infections have been reported in a range of vertebrates and invertebrates (22). Infections can occur by many different routes, via ingestion of contaminated food or water, contact with infected animals, bites by infected arthropods including mosquitoes or ticks, or via inhalation (36). F. tularensis is further divided into three subspecies and one proposed subspecies, where F. tularensis subsp. holarctica (type B) is found in most of Europe, Asia, and North America and F. tularensis subsp. tularensis (type A) is found in North America. F. tularensis subsp. mediasiatica has been identified only in Central Asia, and “Francisella tularensensis subsp. novicida” has been isolated in several locations in North America and Australia (25, 39). Human infections are mainly caused by type A and type B strains, where type A strains cause severe infections and are significantly more virulent than type B strains. In mouse infection models, F. tularensis subsp. mediasiatica is as virulent as, or even slightly more virulent than, type B strains (unpublished results). However, infections with F. tularensis subsp. mediasiatica appear to be rare in humans (30). F. tularensis subsp. novicida is significantly less pathogenic than the other subspecies in humans and is only known to cause infection in immunocompromised persons. Due to the high infectivity and potential for airborne transmission, F. tularensis has been designated a category A agent of bioterrorism (4, 14). Still, relatively little is known about the virulence determinants of F. tularensis. The recent development of genomics and genetic tools (9) has been the key to increasing the understanding of the molecular mechanisms of F. tularensis infections.
In a recent study, comparisons of different strains revealed the presence of regions of differences (RDs) (35). These RDs are flanked by direct-repeat sequences that are assumed to have facilitated deletion events in certain strains. Two RDs are particularly interesting, since they have been linked to virulence. One region, denoted RD19, encodes a putative type IV pilin (PilA) that has been shown to contribute to virulence in a type B strain, FSC354 (7). Type IV pili (Tfp) are complex adhesins involved in important host cell interactions and are required for virulence in many human pathogens, such as Neisseria spp., Pseudomonas aeruginosa, and Vibrio cholerae (8, 18, 37). Tfp have also been shown to be involved in twitching motility, biofilm formation, and cell signaling (13, 17, 23). The second region, RD18, has been shown to be essential for virulence of a highly virulent type A strain, SCHU S4 (38). One spontaneous avirulent variant of SCHU S4, FSC043, was found to lack RD18 (35, 38). Two genes, FTT0918 and FTT0919 (SCHU S4 nomenclature), were identified as defective in FSC043, and DNA sequencing showed that the deletion event resulted in an in-frame fusion consisting of the N terminus of the FTT0918 protein and the C terminus of the FTT0919 protein (35, 38). Both the FTT0918 and FTT0919 proteins belong to a novel protein family that is unique to Francisella and without any known function so far (38). Importantly, Twine and colleagues were able to establish the attenuation of strain FSC043 as being directly linked to FTT0918, since mutation of this gene in the highly virulent strain SCHU S4 resulted in attenuation (38). In contrast, mutation of FTT0919 had no effect on virulence.
Even though these two RDs have been studied in two different subspecies (FTT0918 in type A and pilA in type B), it is reasonable to assume that these two loci are of significance for virulence of both type A and type B strains. Indeed, here we verify that FTT0918 is important for virulence of type B strains, and in another study, PilA has been demonstrated to be required for full virulence of a type A strain (unpublished results). A striking observation is that the extensively studied live vaccine strain of type B origin, LVS, lacks both the FTT0918 gene and pilA. Interestingly, in a genomic study with the aim of identifying mutations in the genome of LVS, Rohmer and colleagues found seven proteins with either an altered or lost function as likely candidates for the attenuation of LVS (27). Among the genes encoding these seven proteins, the two deletions described above, pilA and FTT0918, were included, as well as a third deletion of 93 bp in the part of the FTT0086 gene encoding the C terminus (SCHU S4 nomenclature) (FTL_1773 in LVS) (27). FTT0086 encodes a protein showing homology to numerous proteins denoted dyp-type peroxidases, known to be important to counter oxidative stress.
There has been a significant interest in vaccine development in recent years, and LVS is frequently used in comparative studies. LVS appears to provide some protection as judged from animal infection experiments and from experience with vaccination of laboratory staff, but the protection may be more limited against airborne type A strains (2, 5, 12). However, in the absence of new vaccines, LVS could be an attractive alternative. One major argument against licensing LVS is that the genetic determinants causing the attenuation have not been identified. In this work, we set out to determine the contributions of the three different gene deletion events to the attenuation of LVS. To avoid any influence of expression from nonnative promoters or effects of plasmid copy number, we used a strategy whereby each deleted region was restored by complementation in cis. Complementation of the gene FTT0086 had no impact on mouse virulence, while reintroduction of either the FTT0918 or pilA gene resulted in increased virulence. Complementation of LVS with both FTT0918 and pilA restored virulence to a level indistinguishable from that of a recently isolated virulent clinical type B isolate.
MATERIALS AND METHODS
Bacterial strains, plasmids, and growth conditions.
The F. tularensis and Escherichia coli strains used in this study are listed in Table 1. F. tularensis strains were grown on modified Thayer-Martin agar plates (31) at 37°C in a 5%-CO2 atmosphere. E. coli strains were grown on blood agar base (Merck) plates or in Luria-Bertani broth at 37°C. Where appropriate, antibiotics were used at the following concentrations; kanamycin, 10 μg/ml (F. tularensis) or 50 μg/ml (E. coli); tetracycline, 10 μg/ml; chloroamphenicol, 2.5 μg/ml (F. tularensis) or 25 μg/ml (E. coli); and polymyxin B, 75 μg/ml. Preparation of plasmid DNA, restriction enzyme digests, ligations, and transformations into E. coli were performed essentially as described previously (29).
TABLE 1.
Strains and plasmids used in this study
| Strain | Subspecies/alternative strain designation(s)/genotype/phenotype | Source/reference |
|---|---|---|
| F. tularensisa | ||
| FSC155 (LVS1) | F. tularensis subsp. holarctica, live vaccine strain, LVS (in strain collection since 1993) | ATCC 29684, |
| FSC458 (LVS2) | Past tularemia vaccine, code no. NDBR 101, lot no. 11; vial reconstituted and used, in strain collection since June 2004 | The National Drug Company |
| FSC200 | F. tularensis subsp. holarctica | Human ulcer, 1998, Sweden |
| FSC352 | F. tularensis subsp. holarctica | Hare, 1974, Sweden |
| FSC237 | F. tularensis subsp. tularensis, SCHU S4 | Human ulcer, 1941, Ohio |
| FSC472 | FSC155/pAL10, FSC155 expressing pilA in trans, Tcr | This study |
| FSC681 | FSC458/pAL10, FSC458 expressing pilA in trans, Tcr | This study |
| FSC688 | FSC458/pilA+, FSC458 expressing pilA in cis | This study |
| FSC741 | FSC458/FTT0086+, FSC458 expressing FTT0086 in cis | This study |
| FSC693 | FSC458/FTT0918+, FSC458 expressing FTT0918 in cis | This study |
| FSC694 | FSC458/pilA+/FTT0918+, FSC458 expressing pilA and FTT0918 in cis | This study |
| FSC767 | FSC200 /FTT0918−, FTT0918 insertion mutant | This study |
| E. coli | ||
| Top10 | F−mcrA Δ(mrr-hsdRMS-mcrBC), φ80lacZΔM15 ΔlacX74 recA1 deoR araD139 (Δara-leu)7697 galU galK rpsL (Smr) endA1 nupG | Invitrogen |
| S17-1λpir | recA thi pro hsdR−M+, <RP4:2-Tc:Mu:Km:Tn7>Tpr Smr | 32 |
| BL21 Star (DE3) | F−ompT hsdSB (rB− mB−) gal dcm rne-131 (DE3) | Invitrogen |
| Plasmids | ||
| pCR2.1-TOPO | Topo cloning vector, Ampr Kmr | Invitrogen |
| pCR4.0-TOPO | Topo cloning vector, Ampr Kmr | Invitrogen |
| pKK214GFP | groELS promoter, Ft ori, p15A ori, GFP,b Tcr | 1 |
| pDM4 | Suicide plasmid. sacB, mobRP4, oriR6K, Cmr | 21 |
| pDMK2 | Suicide plasmid. sacB, mobRP4, oriR6K, Kmr | K. Kadzhaev, unpublished |
| pFTKan1 | EZ-Tn5, pMOD-2 F. tularensis codon-optimized KanR clone sequence, F. tularensis groELS promoter | T. Kawula, unpublished |
| pET-30a(+) | Cloning vector carrying an N-terminal His-tag/thrombin/S-tag/enterokinase configuration and an optional C-terminal His tag sequence, Kmr | Novagen |
| pAL10 | pilA gene cloned into NdeI and EcoRI sites of pKK214GFP, Tcr | 7 |
| pAL11 | pilA gene and additionally 1 kb upstream and downstream of pilA cloned into XhoI and SacI sites of pDM4, Cmr | 7 |
| pEMS36 | FTT0086 gene and additionally 1 kb upstream and downstream of FTT0086 cloned into the XhoI and SalI sites of pDM4, Cmr | This study |
| pKK223 | The cis complementation construct for FTT0918 cloned into SaII and NotI sites of pDMK2, Kmr | This study |
| pKK224 | PvuII fragment generated by PCR using primers groELS/KanR/E-C cloned into blunt-ended pDM4, Cmr | This study |
All Francisella strains are from the Francisella Strain Collection at FOI, Umeå, and each strain has been given a strain collection number.
GFP, green fluorescent protein.
Cis and trans complementation of pilA, FTT0086, and FTT0918 in strains LVS1 and LVS2.
For complementation in trans, pilA was amplified with the primers PilAcomp-1F and PilAcomp-1R using FSC352 as a template (Table 2). The resulting fragment was sequenced and cloned into pKK214GFP (NdeI-EcoRI) downstream of the groELS promoter. This construct, denoted pAL10 (7), was introduced into strain FSC155 (here denoted LVS1) and FSC458 (here denoted LVS2) by cryotransformation (24), and the resulting mutant strains were denoted FSC472 and FSC681, respectively (Table 1). The cis complementation constructs were generated by PCR with the primer pairs pilAcomp-4F and pilAcomp-4R, using strain FSC352 as a template (pilA) (7), FTT0086-F and FTT0086-R, using strain FSC200 as a template (FTT0086), and 0918cis_F and 0918cis_R, using FSC200 as a template (FTT0918) (Table 2). The two fragments with pilA and FTT0086, including approximately 2-kb flanking regions, were sequenced and inserted into the suicide vector pDM4 (XhoI-SalI). The FTT0918 construct was sequenced and cloned into pDMK2 (SalI-NotI). The resulting clones, pAL11, pEMS36, and pKK223, were introduced into E. coli S17-1λpir and conjugated into strains LVS1 or LVS2 essentially as described previously (9). The resulting mutant strains, denoted FSC688 (pilA), FSC741 (FTT0086), and FSC693 (FTT0918), were verified by PCR and sequencing (Eurofins MWG Operon) (Table 1). The cis complementation ensured chromosomal integration of the functional gene and expression regulated by its native promoter.
TABLE 2.
Primers used in this study
| Primer | Primer sequencea (5′-3′) | RE site |
|---|---|---|
| pilAcomp_1F | GCATGTCATATGAAAAAGAAAATGCAAAAAGGT | NdeI |
| pilAcomp_1R | GCATGTGAATTCGATTAGATAGCATTACAGTTAGA | EcoRI |
| pilAcomp_4F | CAACGCCAAAGATTACATCAC | |
| pilAcomp_4R | TTCTGTCATTCCTGACTCGAC | |
| FTT0086_F | CATTGCTATGGCTTGAGTTAT | |
| FTT0086_R | GGTTTGTATTGTTGAAGAAGT | |
| 0918cis_F | GGACAAATGGTAAGGCTCTAA | |
| 0918cis_R | GTTACTGTTACTAATACTTCTTAA | |
| Tn918E_F | AACCGAATTCTAGGAGGCGTCTTTAACCAA | EcoRI |
| Tn918C_R | TTTCAGTCGACGAGTTACCAGCACCAGCAAT | SalI |
| A1b | GATCCCGATGTACTCTAACTA | |
| A2c | TTCTCACTAGTTGAGTTAATG | |
| B | GGGGTAGTACTTTAAATCCT | |
| C | TTATTGCGCATGGTGTCTC | |
| D | GTGCCTTTGATCGTGCTTAC | |
| E | AAGGTAGTATTGATGCTGACAC | |
| F | ACCAACAACACCACCTAAGAC | |
| G | CTGGGGATTGATAAGCAACA | |
| H | CATTAGTACGCTTAGCAACAA | |
| I | GTCACAAGATGGCTATACACT | |
| J | GCCTGAGCAGTAGTATAGTTT | |
| K | ATGATGCGAGATTTAGGGTA | |
| L | CAGCAGGTGGAAATACAGAT | |
| M | CTTGAGATGCTGATACACCT |
Restriction sites (RE) are underlined. Generally, the primers were designed by using the SCHU S4 (16) or FSC200 genome (University of Washington Genome Center, UWGC).
Primer A1 is specific for the FSC200 genome.
Primer A2 is specific for the LVS genome.
Construction of an insertion mutation in gene FTT0918 in strain FSC200.
The FTT0918 insertion mutant was generated by PCR using the primers Tn918E_F and Tn918C_R and strain FSC200 as a template (Table 2). Nucleotides between bases 497 and 1208 of the 1,674 bp intact gene FTT0918 were inserted into the vector pFTKan1 (Table 1). The entire fragment groES/FTKan1E-C was isolated from the pFTKan1 vector by digestion with PvuII, cloned into the linearized blunt-ended suicide vector pDM4, and denoted pKK224. pKK224 was introduced into E. coli S17-1λpir and conjugated into strain FSC200 as described previously (9). The mutant strain, denoted FSC767, was verified by PCR (Table 1). The insertion mutation resulted in a truncation of the FTT0918 protein by 154 amino acids (see Fig. 1C).
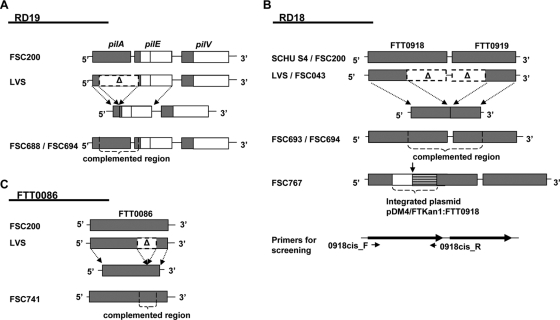
FIG. 1.
Comparison of the RD19, RD18, and FTT0086 regions in different Francisella subspecies and strains. (A) RD19, containing pilA, pilE, and pilV in FSC200 (type B), LVS (type B), FSC688 (LVS2 cis complemented with pilA), and FSC694 (LVS2 cis complemented with pilA and FTT0918). A deletion spanning the pilA gene and the N-terminus-encoding part of pilE results in an in-frame fusion consisting of the N-terminus-encoding part of pilA and the C-terminus-encoding part of pilE in LVS. (B) RD18, containing FTT0918 and FTT0919 in SCHU S4 (type A), FSC200 (type B), LVS (type B), FSC043 (type A), FSC693 (LVS2 cis complemented with FTT0918), FSC694 (LVS2 cis complemented with pilA and FTT0918), and FSC767 (FSC200 with a FTT0918 insertion mutation). In LVS and FSC043, a deletion overlapping the genes FTT0918 and FTT0919 results in an in-frame fusion consisting of the N-terminus-encoding part of FTT0918 and the C-terminus-encoding part of FTT0919. The solid arrow indicates the truncation of the FTT0918 insertion mutant (FSC767). (C) FTT0086 in FSC200 (type B), LVS (type B), and FSC741 (LVS2 cis complemented with FTT0086). In LVS, FTT0086 has undergone a deletion of 93 nucleotides in the middle part of the gene.
Cloning, expression, and purification of recombinant FTT0918 protein.
Primers were designed to amplify the FTT0918 gene, introducing a BamHI site at the 5′ end and a SalI site at the 3′ end. The PCR-amplified fragment was ligated to the BamHI/SalI-digested expression vector pET-30a(+) (Novagen) and transformed into E. coli BL21(DE3) (Invitrogen). Protein expression was induced by the addition of isopropyl-β-d-thiogalactopyranoside, and bacterial cultures were harvested by centrifugation at 6,000 rpm for 20 min 4 h upon addition of isopropyl-β-d-thiogalactopyranoside. The bacterial pellet was resuspended in resuspension buffer (1.5 M KCl, 0.5% Triton X-100, 1 EDTA-free protease inhibitor cocktail tablet, 10 mM Tris-HCl, pH 8) and then freeze/thawed in liquid nitrogen three times, sonicated, and centrifuged at 24,000 rpm for 30 min at 4°C. The pellet was dissolved in wash buffer (0.15 M NaCl, 10 mM Tris-HCl, pH 8) and centrifuged at 24,000 rpm for 30 min at 4°C. The pellet, containing the inclusion bodies of FTT0918, was dissolved in extraction buffer (8 M urea, 70 mM dithiothreitol, 10 mM Tris-HCl, pH 8) and centrifuged at 24,000 rpm for 30 min at room temperature, and the supernatant containing the protein was collected. This supernatant was further purified by affinity chromatography with nickel-nitrilotriacetic acid agarose (Qiagen). The purified protein was then used for immunization, and chicken anti-FTT0918 antibodies were generated by Agrisera (Vännäs, Sweden).
Gel electrophoresis and Western blot analysis.
Samples containing sodium dodecyl sulfate and β-mercaptoethanol were boiled for 5 min and separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis on either a 10 or 12% gel as described previously (15). Proteins were transferred to Immobilon-P transfer membranes (Millipore) using a Trans-Blot semidry transfer cell (Bio-Rad). Membranes were blocked in Tris-buffered saline with 5% nonfat dry milk. The primary antibodies used in Western blot analysis were a polyclonal anti-PilA serum (7) and anti-FTT0918 (Agrisera, Vännäs, Sweden). An alkaline phosphatase-conjugated (Roche) secondary antibody system was used, and bands were visualized by incubating the filters with 0.1% (wt/vol) Nitro Blue tetrazolium (Sigma) and 0.05% (wt/vol) 5-bromo-4-chloro-3-indolyl phosphate (Sigma).
RNA isolation and reverse transcription (RT)-PCR.
Bacteria were grown for 16 h in Chamberlain medium (3). For RNA extraction, the TRIzol reagent (Life Technologies) was used. Total RNA was extracted from 0.5 ml of bacterial culture, treated with RNase-free DNase I (Roche), phenol extracted, and precipitated by ethanol. An aliquot of the RNA (3 μg) was used to synthesize cDNA using random hexamers (final concentration, 25 ng/μl) and Superscript III reverse transcriptase as described by the manufacturer (Life Technologies). In control experiments, samples processed without addition of reverse transcriptase enzyme were used.
Animal infections.
For virulence studies, C57BL/6 female mice, aged 6 to 9 weeks, were used (Scanbur BK AB, Sollentuna, Sweden). Mice were housed under conventional conditions, given food and water ad libitum, and allowed to acclimatized for at least 7 days before infection. The study was approved by the Local Ethical Committee on Laboratory Animals in Umeå, Sweden. F. tularensis strains were grown for 16 h on plates and diluted in phosphate-buffered saline (pH 7.4), and 100 μl was injected subcutaneously into the groin area or alternatively intraperitoneally. The infection doses were determined by viable counts. The infected mice were observed twice a day for 2 weeks and sacrificed when showing severe symptoms (hunched carriage and tousled fur).
RESULTS
One isolate of LVS1 shows defects in expression of Tfp proteins.
In a recent study, several regions that differ between different Francisella strains were identified (35). These RDs were flanked by direct-repeat sequences that are assumed to readily mediate deletion of the RDs. Two RDs have been shown to be required for virulence in a mouse infection model. One region, denoted RD19, encoding a putative type IV pilin (PilA), was shown to contribute to virulence in a type B strain (7), and one protein, FTT0918, encoded within the region RD18, was verified to be essential for virulence of a type A strain (38). Interestingly, the live vaccine strain, LVS, lacks both pilA and the FTT0918 gene (Fig. 1A and B). Since the genetic determinants causing the attenuation of LVS are still unknown, we wanted to examine the contribution of these two deletions to the attenuation of LVS. First, we attempted to complement the LVS strain from the Francisella Strain Collection, FSC155 (here denoted LVS1), with pilA in trans. However, trans-complemented LVS1 (FSC472) expressed only low, barely detectable levels of PilA (Fig. 2). Furthermore, we tried to accomplish the complementation in cis but without any success (data not shown). This was somewhat surprising, since an in-cis complementation of another attenuated type B strain, FSC354, fully restored the expression of PilA (7). In order to determine whether the pilin genes were transcribed in LVS, RNA was prepared and transcription was monitored by RT-PCR. The transcriptional analysis revealed that all genes postulated to be important for Tfp expression, secretion, and assembly were transcribed in the LVS1 strain (Fig. 3). Therefore, the defect seen in LVS1 is most likely at the level of protein expression and/or stability.
FIG. 2.
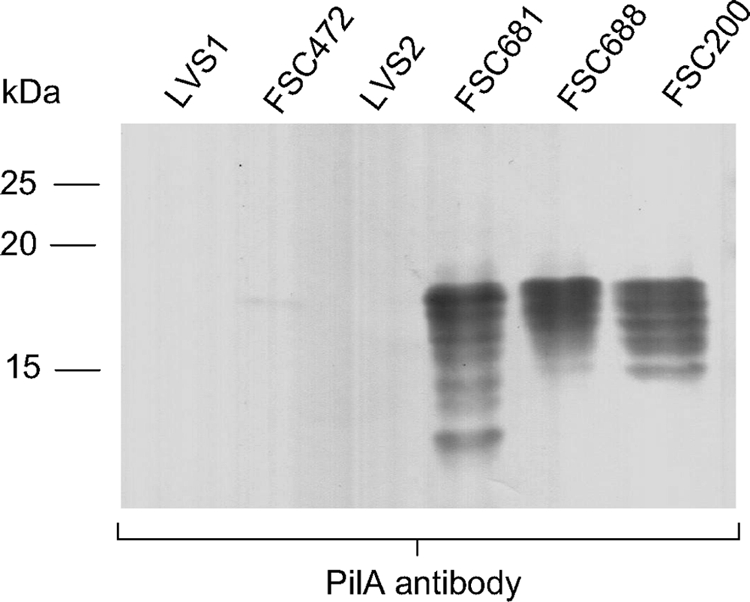
Expression of PilA in different strains of F. tularensis analyzed by Western blotting using an anti-PilA antiserum. Lanes: 1, LVS1; 2, FSC472 (LVS1 trans complemented with pilA); 3, LVS2; 4, FSC681 (LVS2 trans complemented with pilA); 5, FSC688 (LVS2 cis complemented with pilA); 6, FSC200.
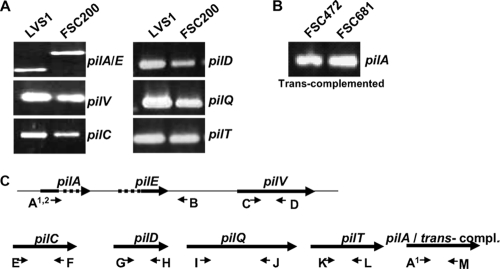
FIG. 3.
Transcription of pilin genes in wild-type and mutated strains of F. tularensis. (A) RT-PCR on mRNA demonstrates the pilin genes, pilA, pilE, and pilV, and several pilus genes involved in assembly/secretion of type IV pili, pilC, pilD, pilQ, and pilT, to be equally well transcribed in LVS1 and in the virulent type B strain FSC200. As a result of the repeat-mediated deletion of pilA in LVS, the transcript is shorter. (B) Transcription studies of FSC472 (LVS1 trans complemented with pilA) and FSC681 (LVS2 trans complemented with pilA) demonstrate pilA to be transcribed in both strains. (C) The locations of the different primers used (A to M) are indicated by small arrows.
pilA contributes to virulence of LVS2 by subcutaneous route of infection.
Since the history and handling of LVS1 were somewhat uncertain, we decided to include another LVS isolate, FSC458 (here denoted LVS2), in our studies. While LVS1 has routinely been used in the laboratory over the years, LVS2 was obtained from a recently opened vial which was used in vaccination of staff. In contrast to LVS1, LVS2 can be verified to not have been passaged in vitro after the vaccine vial was reconstituted and the strain was included in the strain collection. First, we sequenced the regions encoding the two identified deletions involving pilA and FTT0918 in both LVS1 and LVS2 to verify that the two deletions were identical (data not shown). In order to establish if the defects seen in PilA expression for LVS1 also applied to LVS2, this strain was complemented both in trans and in cis with pilA. Interestingly, expression was restored both for trans-complemented (FSC681) and cis-complemented (FSC688) LVS2 (Fig. 2). The complementation in trans resulted in slightly elevated levels of PilA and the appearance of several low-molecular-weight bands that possibly could have resulted from incomplete glycosylation (7). Complementation of LVS2 with pilA in cis resulted in significantly increased virulence by the subcutaneous route of infection in a mouse model to a level intermediate between that of LVS2 and that of the virulent type B strain FSC200 (Table 3). However, there was no detectable change in virulence using the intraperitoneal route of infection. Thus, pilA also contributes to virulence in the attenuated type B strain LVS. Moreover, these results show that there are additional defects in LVS1 which most likely can be attributed to in vitro passages over the years.
TABLE 3.
Infection doses for different F. tularensis strains in C57BL micea
| Strain | Genotype
|
Phenotype or complementation | No. of CFU (lethal dose)b
|
|||
|---|---|---|---|---|---|---|
| FTT0918 | pilA | FTT0086 | Subcutaneous | Intraperitoneal | ||
| LVS1 | − | − | Δ93 bp | LVS wt | 3 × 107 | 1 × 101 |
| LVS2 | − | − | Δ93 bp | LVS wt | 1 × 106 | 5 × 101 |
| FSC688 | − | + | Δ93 bp | LVS2, pilA in cis | 5 × 103 | 3 × 101 |
| FSC741 | − | − | + | LVS2, FTT0086 in cis | 2 × 106 | NT |
| FSC693 | + | − | Δ93 bp | LVS2, FTT0918 in cis | <5c | <5 |
| FSC694 | + | + | Δ93 bp | LVS2, pilA and FTT0918 in cis | <5 | <5 |
| FSC200 | + | + | + | Type B wt | <5 | <5 |
| FSC767 | − | + | + | FSC200, insertion mutation in FTT0918 | 2 × 102 | <5 |
Mice in groups of five were infected subcutaneously. The result is from one single experiment representative of three experiments of similar design. wt, wild type; Δ, deletion; NT, not tested.
The CFU value is a 50% lethal dose (LD50) calculation (26), but this should not be seen as a standard LD50 experiment since mice were sacrificed if they showed severe sickness. A lethal dose indicated as <5 CFU was used for strains where all animals showed lethal symptoms of infection for doses between two and five bacteria.
The infection kinetics was delayed compared to that for the pilA/FTT0918 double complementation (Fig. 5).
Deletion within gene FTT0086 does not contribute to attenuation of LVS2.
FTT0086 (SCHU S4 nomenclature) (FTL_1773 in LVS) shows homology to numerous proteins denoted dyp-type peroxidases, and the gene is highly conserved among different Francisella strains. Upon phagocytosis by macrophages, some microorganisms have developed effective enzymatic pathways, such as the use of peroxidases to counteract oxidative stress (20). Interestingly, in LVS this locus (FTT0086) has undergone a deletion of 93 nucleotides in a region encoding several of the residues conserved in homologues between many different bacteria (27) (Fig. 1C). Since Francisella is an intracellular pathogen, this could potentially render LVS less able to survive and replicate within macrophages. In order to establish a possible contribution of the deletion of FTT0086 to the attenuation of LVS, LVS2 was complemented in cis with an intact FTT0086 gene, and the mutant strain was denoted FSC741. The full restoration of the gene was verified by PCR and sequencing (data not shown). However, the complementation did not result in any significant increase in virulence in the mouse infection model (Table 3).
Deletion of FTT0918 is a major cause of attenuation of LVS.
In a recent study, a spontaneous avirulent variant of SCHU S4, FSC043, was analyzed (38). Comparative proteomics demonstrated two proteins, FTT0918 and FTT0919 (RD18) (SCHU S4 nomenclature), to be defective in FSC043 and LVS. DNA sequencing indicated a deletion overlapping the genes, resulting in an in-frame fusion consisting of the N-terminal half of the FTT0918 protein and the C-terminal half of the FTT0919 protein (FTL_0439 in LVS) (35) (Fig. 1B). This deletion was verified to span the same nucleotides in the two LVS variants used in this study (data not shown). Both FTT0918 and FTT0919 belong to a novel protein family that is unique to Francisella and with no known function so far. However, both proteins are predicted to contain signal peptides and coiled-coil domains, indicating that they could be membrane associated (38). FTT0918 was established to be responsible for the virulence attenuation of a type A strain, while FTT0919 had no apparent effect on virulence. In order to establish the importance of FTT0918 in the virulence of type B strains, an FTT0918 insertion mutant was constructed using the virulent type B isolate FSC200 (FSC767) (Fig. 1B). Interestingly, the FTT0918 mutant was attenuated in the mouse infection model, confirming that FTT0918 is also a virulence determinant in type B strains (Table 3). At this point we cannot exclude that FTT0919 also contributes to virulence. The lower level of attenuation seen with the type B strain, FSC200, than with the type A strains (38) is most likely due to the truncated FTT0918 gene (1,208 bp in length, compared to the full-length gene of 1,674 bp) having retained some function (Table 3).
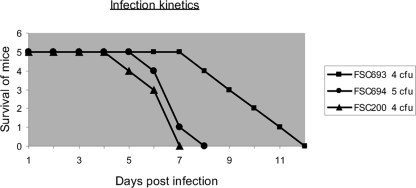
To discern the contribution of FTT0918 to the attenuation of LVS, LVS2 was complemented in cis with an intact FTT0918 gene (FSC693). The complementation was verified by Western blot analysis and PCR (Fig. 4A and B, respectively). Interestingly, virulence increased by both the subcutaneous and intraperitoneal infection routes, and the infection dose in this case was similar to that of the virulent type B strain FSC200 (Table 3). This verifies that FTT0918 is also a major virulence determinant in type B strains. Since the infection dose for the FTT0918-positive strain was very low, it was difficult to discern the contribution of the pilA region to the virulence of LVS in this genetic background. However, the single FTT0918-complemented strain (FSC693) showed slower infection kinetics than the LVS2 strain complemented in cis with both pilA and FTT0918 (FSC694), as well as the virulent strain FSC200 (Table 3 and Fig. 5). In the doubly complemented strain, the virulence was restored both by the subcutaneous and intraperitoneal routes of infection to a level similar to that of the clinical isolate FSC200 (Table 3). In addition, the infection kinetics was also comparable to that for FSC200 (Fig. 5). Taken together, our results indicate that the attenuation of LVS2 seen in the mouse infection model is the result of repeat-mediated loss of pilA and FTT0918.
FIG. 4.
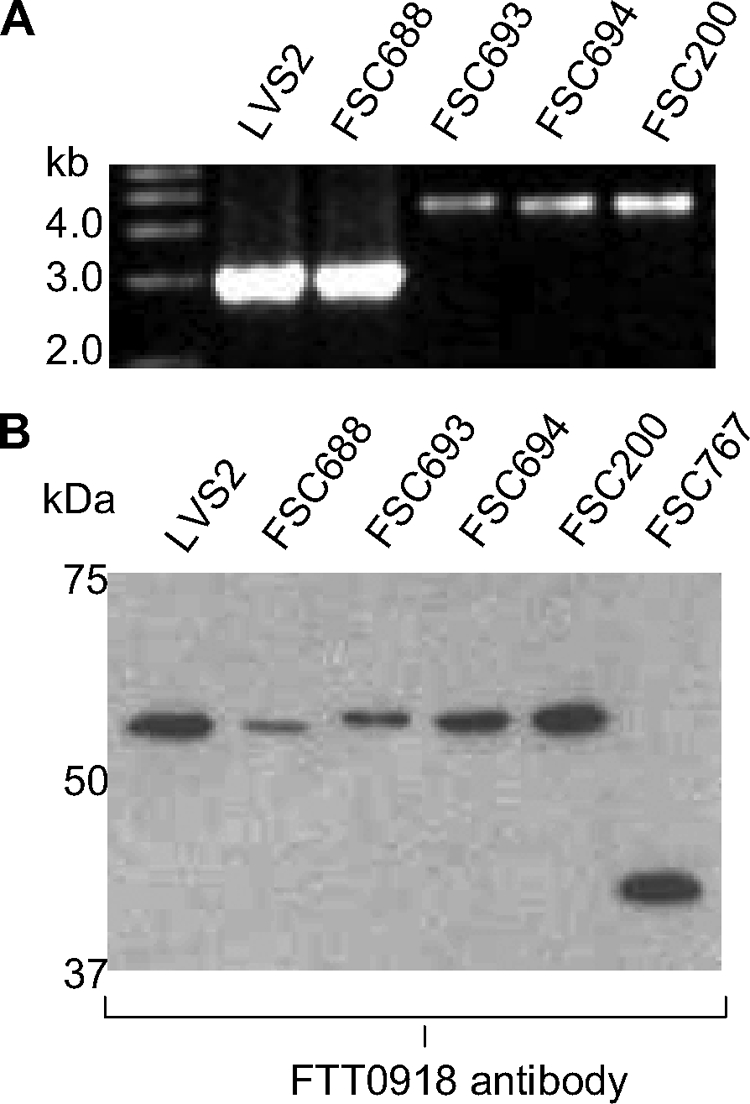
PCR and Western blot analysis of FTT0918. (A) PCR analysis of FTT0918 in different strains of F. tularensis. Lanes: 1, LVS2; 2, FSC688 (LVS2 cis complemented with pilA); 3, FSC693 (LVS2 cis complemented with FTT0918); 4, FSC694 (LVS2 cis complemented with pilA and FTT0918); 5, FSC200. An intact FTT0918 gene gives a PCR fragment of 4.4 kb, while the FTT0918 deletion gives a PCR fragment of 2.8 kb. (B) Expression of FTT0918 in different strains of F. tularensis analyzed by Western blotting using an anti-FTT0918 antiserum. Lanes: 1, LVS2; 2, FSC688 (LVS2 cis complemented with pilA); 3, FSC693 (LVS2 cis complemented with FTT0918); 4, FSC694 (LVS2 cis complemented with pilA and FTT0918); 5, FSC200; 6, FSC767 (FTT0918 insertion mutant of FSC200). The size of the intact FTT0918 protein is 58.8 kDa, the FTT0918-0919 fusion protein is 58.5 kDa, and the truncated FTT0918 protein is 42 kDa.
FIG. 5.
Infection kinetic study of a mouse model. Infection of mice with FSC693 (LVS2 cis complemented with FTT0918), FSC694 (LVS2 cis complemented with pilA and FTT0918), and FSC200 of F. tularensis. Groups of five mice were infected via the subcutaneous route, and the infection was followed over time. The exact dose for each strain was determined by viable count and is shown beside the key for the respective strain.
DISCUSSION
Live attenuated F. tularensis vaccines were developed in Russia in the 1950s by in vitro passage of different type B strains. One strain, the live vaccine strain (LVS), provided effective protection against laboratory-acquired tularemia (19). The introduction of the use of the LVS vaccine in laboratory workers at the U.S. Army Medical Research Institute of Infectious Diseases yielded a significant decrease in incidences of laboratory-acquired tularemia (2, 28). It was also concluded that aerogenic vaccination appeared to induce better protection than vaccination via acupuncture (12, 19). However, the nature of the genetic lesions responsible for the attenuation of LVS has remained unknown. Human and animal studies, where systemic vaccinations with LVS have been performed, indicated that LVS provided limited protection against aerosol challenge with the highly virulent type A strains of F. tularensis (5, 12). For these reasons, together with the concern for possible reversion to virulence, mixed colony morphology, and variable immunogenicity, LVS has not been licensed as a vaccine (10). Genome comparisons of different subspecies and strains have identified regions that differ between Francisella strains (27, 35). Several strains, including LVS, seem to accumulate virulence-attenuating mutations during in vitro passage, and these mutations include large repeat-mediated deletions of RDs. Two RDs were verified to be deleted in LVS, and both have been linked to virulence. Region RD19, encoding a putative type IV pilin (PilA), was shown to contribute to virulence in the type B strain FSC354 (7), and one of the genes contained within RD18, FTT0918, was verified to be essential for virulence of the type A strain FSC043 (38). It is not obvious what role a pilin could play in the virulence of an intracellular pathogen like Francisella. Tfp have been associated with virulence in the intracellular pathogens Burkholderia pseudomallei (6, 11) and Legionella pneumophila (33, 34). In B. pseudomallei, the Tfp was found to be important for adherence to human epithelial cells and for virulence in a nematode and mouse infection model (6). In L. pneumophila, the Tfp system has no affect on intracellular growth but promotes attachment to host cells and is involved in competence for DNA transformation, a property recognized from other Tfp-expressing bacteria, such as Neisseria gonorrhoeae (33, 34). In a previous study, we found that a pilA mutant of Francisella was attenuated via the subcutaneous route of infection and impaired in its ability to spread from the initial site of infection to the spleen (7). However, the mutant was still able to survive and replicate in macrophages. This implies that the pilin mediates critical interactions during the initial stages of infection and could be important for attachment to host cells.
The second major deletion in LVS, RD18, containing the gene FTT0918, was first identified in the avirulent type A strain FSC043 (35, 38). The encoded protein belongs to a novel protein family unique to Francisella and without any known function so far. The cis complementation of FTT0918 in LVS2 resulted in increased virulence, by both the subcutaneous and intraperitoneal routes of infection, similar to the virulent type B strain FSC200. Hence, in this genetic background, it was difficult to distinguish the contribution of pilA to the virulence of LVS2. Importantly, the FTT0918 singly complemented strain showed delayed infection kinetics compared to that of LVS2 with both pilA and FTT0918 restored. Even if the contribution of pilA to virulence in the FTT0918 cis-complemented LVS2 strain is not readily recognized, it is clear that pilA contributes to virulence, since our pilA cis complementation of LVS2 resulted in significantly increased virulence. Further support for a role of PilA in virulence is provided by a recent study involving competitive infection experiments with mice and a virulent type A strain, where a pilA mutant strain was outcompeted by the wild-type strain in the mouse infection model (unpublished results). The third deletion identified in LVS, FTT0086, encoding a dyp-type peroxidase, was established not to be involved in the attenuation. Yet it is very intriguing that two out of the three deletions identified in the LVS genome are demonstrated to have an impact on the virulence of the vaccine strain. Furthermore, our work with PilA in LVS also verified that in vitro passage could attenuate Francisella, and these findings stress how important it is to know the history of the strains and minimize in vitro passage to reduce the risk of virulence attenuation.
Our study suggests that PilA contributes to virulence of LVS2 by the subcutaneous route but not by the intraperitoneal route of infection. FTT0918 contributes to virulence of LVS2 both by the subcutaneous and by the intraperitoneal route of infection. Reintroduction of both pilA and the FTT0918 gene into LVS2 fully restored virulence of LVS2 by both infection routes to a level comparable to that of virulent type B isolates. Conclusively, the attenuation of LVS2 seen in the mouse infection model is mainly the result of a repeat-mediated loss of pilA and FTT0918. Importantly, the attenuation of LVS is the result of a loss of the pilA and FTT0918 DNA, and this makes it unlikely that LVS could revert to higher virulence by restoring the function of these two regions. Our findings may well facilitate licensing of LVS, which could be an interesting alternative until new vaccines become available. In addition, our work also provides important insight for development of new defined and efficient vaccines against tularemia. The two genes identified here as deleted and nonfunctional in LVS clearly have distinct roles in infection. FTT0918 has a major impact on mouse virulence both in type A and type B strains but still allows for induction of protective immunity in the mouse infection model (38). pilA appears mainly to affect virulence by the subcutaneous route of infection (also the commonly used route for human vaccinations) and to slow the progress and spread of the infection from its initial site. The importance of PilA for virulence has varied in the strains investigated so far, but there is a tendency for PilA to appear to be less important in highly virulent type A and type B strains. Here it is important to bear in mind that the mouse infection model has limitations in predicting effects on humans. The significance of both PilA and FTT0918 as a target for vaccine development will require work with other animal infection models, but the previous vast experience of LVS vaccinations certainly holds the promise that LVS could serve as a model for development of a new defined live vaccine against tularemia.
Acknowledgments
We thank Solveig Linder for skillful assistance with animal infection experiments. We are indebted to T. Kawula for the gift of the plasmid pFTKan1.
This work was supported by grants from the Kempe Foundation to Emelie Salomonsson and the Swedish Research Council (VR).
Editor: W. A. Petri, Jr.
Footnotes
Published ahead of print on 8 June 2009.
REFERENCES
- 1.Abd, H., T. Johansson, I. Golovliov, G. Sandström, and M. Forsman. 2003. Survival and growth of Francisella tularensis in Acanthamoeba castellanii. Appl. Environ. Microbiol. 69600-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burke, D. 1977. Immunization against tularemia: analysis of the effectiveness of live Francisella tularensis vaccine in prevention of laboratory-acquired tularemia. J. Infect. Dis. 13555-60. [DOI] [PubMed] [Google Scholar]
- 3.Chamberlain, R. 1965. Evaluation of live tularemia vaccine prepared in a chemically defined medium. Appl. Microbiol. 13232-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dennis, D., T. Inglesby, D. Henderson, J. Bartlett, M. Ascher, E. Eitzen, A. Fine, A. Friedlander, J. Hauer, M. Layton, S. Lillibridge, J. McDade, M. Osterholm, T. O'Toole, G. Parker, T. Perl, P. Russell, and K. Tonat. 2001. Tularemia as a biological weapon: medical and public health management. JAMA 2852763-2773. [DOI] [PubMed] [Google Scholar]
- 5.Eigelsbach, H., J. Tulis, E. Overholt, and W. Griffith. 1961. Aerogenic immunization of the monkey and guinea pig with live tularemia vaccine. Proc. Soc. Exp. Biol. Med. 108732-734. [DOI] [PubMed] [Google Scholar]
- 6.Essex-Lopresti, A., J. Boddey, R. Thomas, M. Smith, M. Hartley, T. Atkins, N. Brown, C. Tsang, I. Peak, J. Hill, I. Beacham, and R. Titball. 2005. A type IV pilin, PilA, contributes to adherence of Burkholderia pseudomallei and virulence in vivo. Infect. Immun. 731260-1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forslund, A., K. Kuoppa, K. Svensson, E. Salomonsson, A. Johansson, M. Byström, P. Oyston, S. Michell, R. Titball, L. Noppa, E. Frithz-Lindsten, M. Forsman, and A. Forsberg. 2006. Direct repeat-mediated deletion of a type IV pilin gene results in major virulence attenuation of Francisella tularensis. Mol. Microbiol. 591818-1830. [DOI] [PubMed] [Google Scholar]
- 8.Fullner, K., and J. Mekalanos. 1999. Genetic characterization of a new type IV-A pilus gene cluster found in both classical and El Tor biotypes of Vibrio cholerae. Infect. Immun. 671393-1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Golovliov, I., A. Sjöstedt, A. Mokrievich, and V. Pavlov. 2003. A method for allelic replacement in Francisella tularensis. FEMS Microbiol. Lett. 222273-280. [DOI] [PubMed] [Google Scholar]
- 10.Griffin, K., P. Oyston, and R. Titball. 2007. Francisella tularensis vaccines. FEMS Immunol. Med. Microbiol. 49315-323. [DOI] [PubMed] [Google Scholar]
- 11.Holden, M., R. Titball, S. Peacock, A. Cerdeño-Tárraga, T. Atkins, L. Crossman, T. Pitt, C. Churcher, K. Mungall, S. Bentley, M. Sebaihia, N. Thomson, N. Bason, I. Beacham, K. Brooks, K. Brown, N. Brown, G. Challis, I. Cherevach, T. Chillingworth, A. Cronin, B. Crossett, P. Davis, D. DeShazer, T. Feltwell, A. Fraser, Z. Hance, H. Hauser, S. Holroyd, K. Jagels, K. Keith, M. Maddison, S. Moule, C. Price, M. Quail, E. Rabbinowitsch, K. Rutherford, M. Sanders, M. Simmonds, S. Songsivilai, K. Stevens, S. Tumapa, M. Vesaratchavest, S. Whitehead, C. Yeats, B. Barrell, P. Oyston, and J. Parkhill. 2004. Genomic plasticity of the causative agent of melioidosis, Burkholderia pseudomallei. Proc. Natl. Acad. Sci. USA 10114240-14245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hornick, R., and H. Eigelsbach. 1966. Aerogenic immunization of man with live tularemia vaccine. Bacteriol. Rev. 30532-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Källström, H., M. Islam, P. Berggren, and A. Jonsson. 1998. Cell signaling by the type IV pili of pathogenic Neisseria. J. Biol. Chem. 27321777-21782. [DOI] [PubMed] [Google Scholar]
- 14.Khan, A., S. Morse, and S. Lillibridge. 2000. Public-health preparedness for biological terrorism in the USA. Lancet 3561179-1182. [DOI] [PubMed] [Google Scholar]
- 15.Laemmli, U. K. 1970. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227680-685. [DOI] [PubMed] [Google Scholar]
- 16.Larsson, P., P. Oyston, P. Chain, M. Chu, M. Duffield, H. Fuxelius, E. Garcia, G. Hälltorp, D. Johansson, K. Isherwood, P. Karp, E. Larsson, Y. Liu, S. Michell, J. Prior, R. Prior, S. Malfatti, A. Sjöstedt, K. Svensson, N. Thompson, L. Vergez, J. Wagg, B. Wren, L. Lindler, S. Andersson, M. Forsman, and R. Titball. 2005. The complete genome sequence of Francisella tularensis, the causative agent of tularemia. Nat. Genet. 37153-159. [DOI] [PubMed] [Google Scholar]
- 17.Mattick, J. 2002. Type IV pili and twitching motility. Annu. Rev. Microbiol. 56289-314. [DOI] [PubMed] [Google Scholar]
- 18.Mattick, J., C. Whitchurch, and R. Alm. 1996. The molecular genetics of type-4 fimbriae in Pseudomonas aeruginosa—a review. Gene 179147-155. [DOI] [PubMed] [Google Scholar]
- 19.McCrumb, F. 1961. Aerosol infection of man with Pasteurella tularensis. Bacteriol. Rev. 25262-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller, R., and B. Britigan. 1997. Role of oxidants in microbial pathophysiology. Clin. Microbiol. Rev. 101-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Milton, D., R. O'Toole, P. Horstedt, and H. Wolf-Watz. 1996. Flagellin A is essential for the virulence of Vibrio anguillarum. J. Bacteriol. 1781310-1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mörner, T. 1992. The ecology of tularaemia. Rev. Sci. Tech. 111123-1130. [PubMed] [Google Scholar]
- 23.O'Toole, G., and R. Kolter. 1998. Flagellar and twitching motility are necessary for Pseudomonas aeruginosa biofilm development. Mol. Microbiol. 30295-304. [DOI] [PubMed] [Google Scholar]
- 24.Pavlov, V., A. Mokrievich, and K. Volkovoy. 1996. Cryptic plasmid pFNL10 from Francisella novicida-like F6168: the base of plasmid vectors for Francisella tularensis. FEMS Immunol. Med. Microbiol. 13253-256. [DOI] [PubMed] [Google Scholar]
- 25.Petersen, J., and M. Schriefer. 2005. Tularemia: emergence/re-emergence. Vet. Res. 36455-467. [DOI] [PubMed] [Google Scholar]
- 26.Reed, L. J., and H. Muench. 1938. A simple method on estimating fifty per cent endpoints, Am. J. Hyg. 27493-497. [Google Scholar]
- 27.Rohmer, L., M. Brittnacher, K. Svensson, D. Buckley, E. Haugen, Y. Zhou, J. Chang, R. Levy, H. Hayden, M. Forsman, M. Olson, A. Johansson, R. Kaul, and S. Miller. 2006. Potential source of Francisella tularensis live vaccine strain attenuation determined by genome comparison. Infect. Immun. 746895-6906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rusnak, J., M. Kortepeter, R. Hawley, A. Anderson, E. Boudreau, and E. Eitzen. 2004. Risk of occupationally acquired illnesses from biological threat agents in unvaccinated laboratory workers. Biosecur. Bioterror. 2281-293. [DOI] [PubMed] [Google Scholar]
- 29.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY.
- 30.Sandström, G., A. Sjöstedt, M. Forsman, N. Pavlovich, and B. Mishankin. 1992. Characterization and classification of strains of Francisella tularensis isolated in the central Asian focus of the Soviet Union and in Japan. J. Clin. Microbiol. 30172-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sandström, G., A. Tärnvik, H. Wolf-Watz, and S. Löfgren. 1984. Antigen from Francisella tularensis: nonidentity between determinants participating in cell-mediated and humoral reactions. Infect. Immun. 45101-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Simon, R., U. B. Priefer, and A. Pühler. 1983. A broad host range mobilization system for in vitro genetic engineering transposon mutagenesis in gram negative bacteria. Bio/Technology 1784-791. [Google Scholar]
- 33.Stone, B., and Y. Abu Kwaik. 1998. Expression of multiple pili by Legionella pneumophila: identification and characterization of a type IV pilin gene and its role in adherence to mammalian and protozoan cells. Infect. Immun. 661768-1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stone, B., and Y. Kwaik. 1999. Natural competence for DNA transformation by Legionella pneumophila and its association with expression of type IV pili. J. Bacteriol. 1811395-1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Svensson, K., P. Larsson, D. Johansson, M. Byström, M. Forsman, and A. Johansson. 2005. Evolution of subspecies of Francisella tularensis. J. Bacteriol. 1873903-3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tärnvik, A. 1989. Nature of protective immunity to Francisella tularensis. Rev. Infect. Dis. 11440-451. [PubMed] [Google Scholar]
- 37.Tønjum, T., and M. Koomey. 1997. The pilus colonization factor of pathogenic neisserial species: organelle biogenesis and structure/function relationships—a review. Gene 192155-163. [DOI] [PubMed] [Google Scholar]
- 38.Twine, S., M. Byström, W. Chen, M. Forsman, I. Golovliov, A. Johansson, J. Kelly, H. Lindgren, K. Svensson, C. Zingmark, W. Conlan, and A. Sjöstedt. 2005. A mutant of Francisella tularensis strain SCHU S4 lacking the ability to express a 58-kilodalton protein is attenuated for virulence and is an effective live vaccine. Infect. Immun. 738345-8352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Whipp, M., J. Davis, G. Lum, J. de Boer, Y. Zhou, S. Bearden, J. Petersen, M. Chu, and G. Hogg. 2003. Characterization of a novicida-like subspecies of Francisella tularensis isolated in Australia. J. Med. Microbiol. 52839-842. [DOI] [PubMed] [Google Scholar]