Abstract
The potential spread of prion infectivity in secreta is a crucial concern for prion disease transmission. Here, serial protein misfolding cyclic amplification (sPMCA) allowed the detection of prions in milk from clinically affected animals as well as scrapie-exposed sheep at least 20 months before clinical onset of disease, irrespective of the immunohistochemical detection of protease-resistant PrPSc within lymphoreticular and central nervous system tissues. These data indicate the secretion of prions within milk during the early stages of disease progression and a role for milk in prion transmission. Furthermore, the application of sPMCA to milk samples offers a noninvasive methodology to detect scrapie during preclinical/subclinical disease.
PrPSc, a disease-specific marker for prion diseases and the likely infectious agent, is widely distributed within the central nervous system (CNS) and lymphoreticular tissues (LRS) in ovine scrapie, human variant Creutzfeldt-Jakob disease (vCJD), and cervine chronic wasting disease (CWD) during both clinical and preclinical stages (4, 11, 25). Furthermore, while the LRS distribution of PrPSc is much more restricted in bovine spongiform encephalopathy (BSE), sheep experimentally infected with BSE display a PrPSc tissue distribution more akin to that of ovine scrapie (11).
For rodent-adapted scrapie and cervine CWD, the disease agent is detected in excreta when animals are in the clinical stages of disease, a process likely to contribute to environmental reservoirs of infectivity and lateral disease transmission (5, 13, 21). Within an experimental rodent model, it has also been demonstrated that the shedding of PrPSc and concomitant infectivity in feces occurs during preclinical scrapie (21).
Evidence now also demonstrates that milk provides a vehicle for the transmission for prion diseases. Scrapie-free lambs fed milk from clinical scrapie-affected ewes propagate PrPSc within their LRS (8). Additionally, a recent study using a transgenic mouse bioassay demonstrated the secretion of infectivity in milk from preclinical animals where scrapie infectivity was found in milk months before the onset of clinical signs in animals with an ARQ/VRQ PrP genotype (10). The presence of scrapie infectivity within milk was irrespective of mammary gland pathology or PrPSc accumulation, and these animals were estimated to have considerable accumulation of immunohistochemically (IHC) detectable PrPSc within the LRS at the time of sampling.
Here, we applied serial protein misfolding cyclic amplification (sPMCA) to the in vitro detection of PrPSc within sheep milk (Fig. 1) (Table 1).
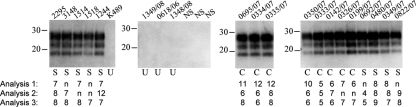
FIG. 1.
sPMCA analysis of ovine milk samples. Milk was clarified and seeded into brain homogenate from sheep unexposed to the scrapie agent. Samples underwent sPMCA, and products were digested with proteinase K before analysis of 10 μl of each sample. PrP was detected with monoclonal antibodies SHA31 and P4; molecular mass markers are indicated (kDa). Milk was sampled from animals not exposed to the scrapie agent (U), those displaying clinical signs of scrapie (C), or those exposed to a scrapie-positive farm environment but not displaying clinical disease (S). NS, non-seeded PMCA brain substrate subjected to identical sPMCA conditions at the same time as positive samples were analyzed. Samples from the four nonexposed animals were analyzed 18 to 20 times each by sPMCA. Samples from clinically affected or clinically normal scrapie-exposed animals were analyzed in triplicate. For this triplicate analysis of each sample, the sPMCA round at which samples became positive is indicated under the appropriate lane. n, negative at round 12. Each sample was PrPSc negative until the stated round and thereafter was positive.
TABLE 1.
Timeline of exposure of animals to a scrapie-positive farm environment, sample collection, and scrapie status
| Animala (PrP genotypeb) | Age at exposurec | Days postexposure at lactation | Days postlactation to clinical scrapied | Clinical statuse | PrPSc detection at postmortemf | PrPSc detection in milk (positive tests/total tests)g |
|---|---|---|---|---|---|---|
| 1349/08 (VRQ/VRQ) | Not exposed | NAh,i | NA | Negative | Negative | 0/20 |
| K489 (VRQ/VRQ) | Not exposed | NAi | NA | Negative | NA (still alive) | 0/18 |
| 0618/06 (VRQ/VRQ) | Not exposed | NAi | NA | Negative | Negative | 0/20 |
| 1348/08 (VRQ/VRQ) | Not exposed | NAi | NA | Negative | Negative | 0/20 |
| 0695/07 (VRQ/VRQ) | Birth | 666-680 | 0 | Positive | Positive | 3/3 |
| 0334/07 (VRQ/VRQ) | Birth | 661-666 | 0 | Positive | Positive | 3/3 |
| 0335/07 (VRQ/VRQ) | Birth | 666-674 | 0 | Positive | Positive | 3/3 |
| 0350/07 (VRQ/VRQ) | Birth | 663-676 | 0 | Positive | Positive | 3/3 |
| 0333/07 (VRQ/VRQ) | Birth | 667-675 | 0 | Positive | Positive | 3/3 |
| 0142/07 (VRQ/VRQ) | Birth | 665-673 | 0 | Positive | Positive | 3/3 |
| 0326/07 (VRQ/VRQ) | Birth | 670-676 | 0 | Positive | Positive | 2/3 |
| 0199/07 (VRQ/VRQ) | Birth | 664 | 0 | Positive | Positive | 2/3 |
| 0692/07 (ARQ/VRQ) | ∼480 days | 1,003 | >450 | Negative | Positive | 2/3 |
| 0480/07 (ARQ/VRQ) | ∼480 days | 1,003 | >355 | Negative | Positive | 3/3 |
| 0349/07 (ARQ/VRQ) | ∼480 days | 1,003 | >348 | Negative | Positive | 3/3 |
| 0822/07 (ARQ/VRQ) | Birth | 760 | >564 | Negative | Negative | 2/3 |
| 2295 (AHQ/VRQ) | ∼120 days | 1,376 | >621 | Negative | Negative | 3/3 |
| 3148 (ARR/VRQ) | Birth | 1,288 | >621 | Negative | NA (still alive) | 2/3 |
| 1514 (ARR/VRQ) | Unknown | 597 | >621 | Negative | NA (still alive) | 2/3 |
| 1518 (ARR/VRQ) | Unknown | 597 | >621 | Negative | NA (still alive) | 1/3 |
| 1244 (ARR/VRQ) | Birth | 1,130 | >621 | Negative | NA (still alive) | 3/3 |
All animal procedures were performed under Home Office (United Kingdom) and local ethical review committee approval and compliance with the Animal (Scientific Procedures) Act of 1986.
Amino acid residues at positions 136, 154, and 171 of the PRNP gene.
Introduction into a scrapie-affected flock.
Days postlactation to postmortem or as of 12 December 2008 for animals that were still alive at the time this paper was written.
Clinical disease usually included head tremors and pruritus with associated wool loss and nervousness. The indicated clinical status was applicable throughout lactation to either postmortem or as of 12 December 2008 for animals that were still alive at the time this paper was written.
PrPSc was analyzed by IHC, Western blot analysis, or enzyme-linked immunosorbent assay. All animals with a positive result contained PrPSc within both brain and lymphatic tissues.
sPMCA was used for PrPSc detection and the results are tallied within this column. Replica analysis of a single milk sample from each animal was carried out. For animals 0695/07, 0334/07, 0335/07, 0350/07, 0333/07, 0142/07, and 0326/07, multiple milk samples were collected during the lactation period indicated and multiple samples from an individual animal were pooled before analysis.
NA, not applicable.
Nonexposed animals were 750 to 1,110 days old at lactation and where applicable were 1,200 to 1,650 days old at postmortem.
PMCA was first described by Saborio and colleagues (20) and allows the amplification of minute quantities of PrPSc (18). In rodent scrapie models, this methodology has detected PrPSc in both blood (2, 18) and brain (22) material in the clinical and preclinical stages of disease as well as in urine excreted during clinical disease (14). This technique has recently been applied to the high-level amplification of PrPSc from natural hosts of prion diseases, including vCJD (7), CWD (9), and scrapie (23). Fresh ovine milk was obtained from individual sheep at least 7 days postpartum. Milk was collected from individual animals into sterile containers and stored on ice for shipping. Within 48 h of collection, milk samples were stored at −80°C. Colostrum was not analyzed. After thawing milk samples, samples from the same individual animal were pooled and EDTA, Nonidet P-40, and sodium deoxycholate were added to final concentrations of 50 mM, 0.5% (vol/vol), and 0.5% wt/vol, respectively. Samples (1 ml) were centrifuged for 10 min at 16,000 × g. After cooling on ice for 5 min, clarified milk supernatant was withdrawn from under the solidified fat layer.
sPMCA was carried out as described by Thorne and Terry (23), who demonstrated that samples from a range of animals containing at least one VRQ PrP allele could be amplified by this technique. Clarified milk supernatant was diluted 1 in 10 into PMCA brain homogenate substrate (10% [wt/vol] brain homogenate from a VRQ/VRQ PrP genotype animal within 150 mM NaCl, 4 mM EDTA, pH 8.0, 1.0% [wt/vol] Triton X-100, and miniprotease inhibitor; Roche) to a final volume of 100 μl. Samples contained within sealed 0.2-ml PCR tubes were placed in a rack within an ultrasonicating water bath (model 3000; Misonix) that held the bottom of the tubes 0.4 cm above the sonicator horn. Water was added to the water bath up to the rack surface, immersing the sonicator horn. The water bath was held at 37°C, and sonications were performed for 40 s at 200 W, equivalent to 80% of the maximum power output of the machine. Sonications were repeated once every 30 min for 24 h (one PMCA round), after which the amplified samples were diluted 1 in 3 with PMCA substrate in a final volume of 100 μl and the sample was subjected to further rounds of PMCA. Twelve PMCA rounds were performed for each sample, a total of 576 sonications over 12 days. PMCA samples were digested with 50 μg/ml proteinase K for 1 h at 37°C before analysis of 10 μl of each sample by Western blotting using 12% (wt/vol) acrylamide NuPAGE precast Bis-Tris gels (as described in reference 15). All clinical scrapie-affected animals or those exposed to the scrapie agent were challenged by introduction into the Ripley flock (Veterinary Laboratories Agency, United Kingdom), where natural scrapie is endemic with a high incidence since 1996. Ryder and coworkers (17) reported that all animals with PrP genotypes VRQ/VRQ and ARQ/VRQ that were born into this flock developed scrapie, with incubation periods of 21 to 28 months and 28 to 39 months, respectively. When ARQ/VRQ animals were introduced into the flock at 6 to 26 months of age, 77% of the animals had subclinical scrapie 24 to 30 months later, as detected by IHC analysis of the LRS. Here, PrPSc was detected in the milk from clinically affected animals at a rate of 92% (24 analyses; triplicate analyses of samples from 8 animals) and from scrapie-exposed, clinically normal sheep at a rate of 78% (27 analyses; triplicate analyses of samples from 9 animals) (Fig. 1) (Table 1). All scrapie-exposed sheep, both clinically affected and clinically normal, tested positive for PrPSc in at least one sPMCA reaction. PrPSc was amplified from the milk of sheep with VRQ/VRQ, ARR/VRQ, ARQ/VRQ, and AHQ/VRQ PrP genotypes (Table 1). It required at least four to eight rounds of sPMCA to produce detectable PrPSc within a milk sample from each of the scrapie-exposed sheep (Fig. 1). Replica analysis of a pooled milk sample from each individual sheep occasionally demonstrated high variability in the round that samples became positive for PrPSc (Fig. 1); this result may indicate the presence of very low levels of PrPSc (19) and/or heterogeneity within milk samples. Analyses of ovine milk from a New Zealand-derived scrapie-free flock kept under strict biosecurity conditions (ADAS, United Kingdom) did not amplify PrPSc within 12 rounds of sPMCA (78 analyses; up to 20 replica analyses of samples from 4 animals). For each of the sPMCA analyses, both positive and negative samples were analyzed concurrently within the same run on the same sonicator. These data demonstrate that PrPSc amplified from samples from scrapie-exposed animals is not due to spontaneous PrPSc formation or cross-contamination between samples within the sPMCA procedure. It is of note that prions were shed within milk from clinically normal, scrapie-exposed animals with multiple PrP genotypes. The ARQ/VRQ genotype is indicative of a high level of disease penetrance and widespread preclinical PrPSc accumulation within the LRS system, whereas AHQ/VRQ and ARR/VRQ genotype animals typically have much lower disease penetrance (24) and LRS involvement (11). This indicates the secretion of prions within milk regardless of high-level PrPSc accumulation within the LRS and also the very likely detection of subclinical as well as preclinical disease in some of these animals.
No clinical scrapie-affected animals displayed clinical mastitis, and PrPSc was not detected within mammary gland tissue from five sheep with clinical scrapie (Fig. 2 and data not shown). This is in agreement with the study by Lacroux et al. (10), indicating that while the accumulation of PrPSc within mammary gland tissue can occur, it is not a prerequisite for its deposition within milk. Here, postmortem detection of PrPSc was carried out by routine diagnosis using IHC and Western blot analysis of the obex. Exceptions were animals 1349/08 and 1348/08, where obex tissue was analyzed by Bio-Rad TeSeE enzyme-linked immunosorbent assay (Table 1). Postmortem IHC examination of palatine tonsil, ileal Peyer's patches, medial retropharyngeal lymph node, and mesenteric lymph node tissue was also carried out. Scrapie-exposed animals were shown to secrete PrPSc within their milk irrespective of whether they could be confirmed as scrapie positive by postmortem immunoassay detection of PrPSc within the CNS and LRS (Table 1). This discrepancy in PrPSc detection may well reflect the greater sensitivity of sPMCA compared to immunoassay detection of PrPSc; these results also indicate that PrPSc is secreted during the early stages of disease progression. Scrapie-exposed animals had PrPSc detected within their milk at least 20 months prior to possible clinical onset of disease, and this was not apparently influenced by the PrP genotype.
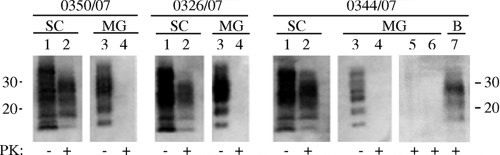
FIG. 2.
Detection of protease-resistant PrPSc within CNS and mammary gland tissues of animals displaying clinical scrapie. Tissues were prepared as 10% or 40% (wt/vol) homogenates for spinal cord and mammary gland tissue, respectively, as described previously elsewhere (15). Native or proteinase K-digested homogenates (25 μg/ml; 1 h at 37°C) were analyzed as indicated. Protease-resistant PrPSc was readily detectable within spinal cord tissue (SC; lanes 1 to 2) but was not detectable within mammary gland samples (MG; lanes 3 to 6). Either 0.33 mg (0350/07) or 0.165 mg (0326/07 and 0344/07) of spinal cord tissue and 1.32 mg (lanes 3 and 4) and 6 mg (lane 5) of mammary gland tissue was analyzed per lane. Protease-resistant PrPSc was still undetectable from 20 mg of mammary gland tissue following precipitation with sodium phosphotungstic acid (25) prior to analysis (lane 6). PrPSc within scrapie-positive brain tissue (63 μg) was readily detected by this method after spiking into 20 mg of mammary gland homogenate (B, lane 7). Full-length and fragmented protease-sensitive PrPC was readily detected within mammary gland tissue (lane 3). Animal numbers are indicated. PrP was detected with monoclonal antibody SHA31; molecular mass markers are indicated (kDa).
These data clearly demonstrate that the secretion of PrPSc within milk occurs in natural scrapie. There are several routes through which the prion protein could be secreted into milk. Evidence suggests that within ovine mammary gland tissue, PrPC is actively produced within epithelial cells, and its secretion is most likely by exocytosis and the apocrine secretion of fat globules (3). It is unknown whether PrPSc is produced within epithelial cells and secreted into milk through similar mechanisms. Alternative mechanisms are through vesicular transcytosis or paracellular transport of PrPSc from the blood. It is established that prion-infected animals harbor infectivity and PrPSc within the blood during preclinical disease (6, 18) and that blood components are secreted within milk, including cell types known to colocalize with PrPSc within ovine mammary glands (12).
Results indicate the potential transmission of scrapie in the milk of infected sheep for a prolonged period prior to clinical onset. As well as ewe-to-lamb disease transmission, this process is also likely to contribute to lateral transmission, as lambs fed milk from clinically infected ewes were the source for the transmission of scrapie between lambs within the first few months after birth (8). It is unknown whether other prion diseases result in the secretion of prions within milk. CWD, vCJD, and experimental ovine BSE share similarities with scrapie in the tissue distribution of infectivity, and it seems plausible that an analogous secretion mechanism may occur. Given the extended preclinical stages and the purported importance of subclinical states for these diseases (16), such an outcome would have significant implications for the transmission of prion diseases from apparently healthy animals and humans.
With regard to ovine milk and milk products, scrapie is not transmissible to humans, and to date there is no evidence of the natural occurrence of ovine BSE. As such, the reported findings do not indicate the likely introduction of zoonotic prions from sheep into the human food chain. Nevertheless, the presented data do indicate caution in the risk assessment associated with such foods. Also, it is unknown if analogous shedding of prions into milk occurs with bovine BSE; evidence from previous epidemiological and bioassay studies would suggest that such a scenario seems unlikely to cause clinical disease (1, 26). However, the present report demonstrates that prions are secreted within the milk of sheep with PrP genotypes not typically associated with LRS accumulation of PrPSc and that prions were secreted from animals devoid of IHC-detectable PrPSc within their LRS. Such PrPSc tissue distribution is similar to bovine BSE, and given the importance of bovine milk in the human diet, the potential presence of low levels of prions within bovine milk warrants further investigation.
Finally, analyzing milk samples by sPMCA offers a methodology with a clear potential for the identification of clinically sick animals and those with preclinical/subclinical scrapie. Such a noninvasive live-animal assay has the potential to contribute to the epidemiological study, management, and control of prion diseases within farmed animals.
Footnotes
Published ahead of print on 3 June 2009.
REFERENCES
- 1.Castilla, J., A. Brun, F. Días-San Segundo, F. J. Salguero, A. Gutiérrez-Adán, B. Pintado, M. A. Ramírez, L. del Riego, and J. M. Torres. 2005. Vertical transmission of bovine spongiform encephalopathy prions evaluated in a transgenic mouse model. J. Virol. 79:8665-8668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Castilla, J., P. Saá, and C. Soto. 2005. Detection of prions in blood. Nat. Med. 11982-985. [DOI] [PubMed] [Google Scholar]
- 3.Didier, A., R. Gebert, R. Dietrich, M. Schweiger, M. Gareis, E. Märtlbauer, and W. M. Amselbruber. 2008. Cellular prion protein in mammary gland and milk fractions of domestic ruminants. Biochem. Biophys. Res. Commun. 369841-844. [DOI] [PubMed] [Google Scholar]
- 4.Fox, K. A., J. E. Jewell, E. S. Williams, and M. W. Miller. 2006. Patterns of PrPCWD accumulation during the course of chronic wasting disease infection in orally inoculated mule deer (Odicoileus hemionus). J. Gen. Virol. 873451-3461. [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez-Romero, D., M. A. Barria, P. Leon, R. Morales, and C. Soto. 2008. Detection of infectious prions in urine. FEBS Lett. 5823161-3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Houston, F., J. D. Foster, A. Chong, N. Hunter, and C. J. Bostock. 2000. Transmission of BSE by blood transfusion in sheep. Lancet 356999-1000. [DOI] [PubMed] [Google Scholar]
- 7.Jones, M., A. H. Peden, C. V. Prowse, A. Gröner, J. C. Manson, M. L. Turner, J. W. Ironside, I. R. MacGregor, and M. W. Head. 2007. In vitro amplification and detection of variant Creutzfeldt-Jakob disease PrPSc. J. Pathol. 21321-26. [DOI] [PubMed] [Google Scholar]
- 8.Konold, T., S. J. Moore, S. J. Bellworthy, and H. A. Simmons. 2008. Evidence of scrapie transmission via milk. BMC Vet. Res. 414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurt, T. D., M. R. Perrott, C. J. Wilusz, J. Wilusz, S. Supattapone, G. C. Telling, M. D. Zabel, and E. D. Hoover. 2007. Efficient amplification of chronic wasting disease PrPRES. J. Virol. 819605-9608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lacroux, C., S. Simon, S. L. Benestad, S. Maillet, J. Mathey, S. Lugan, F. Carbière, H. Cassard, P. Costes, D. Bergonier, J.-L. Weisbecker, T. Moldal, H. Simmons, F. Lantier, C. Feraudet-Tarisse, N. Morel, F. Schelcher, J. Grassi, and O. Andréoletti. 2008. Prions in milk from ewes incubating natural scrapie. PLoS Pathog. 4e1000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Langeveld, J. P. M., J. G. Jacobs, J. H. F. Erkens, A. Bossers, F. G. van Zijderveld, and L. J. M. van Keulen. 2006. Rapid and discriminatory diagnosis of scrapie and BSE in retro-pharyngeal lymph nodes of sheep. BMC Vet. Res. 219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ligios, C., C. J. Sirgurdson, C. Santucciu, G. Carcassola, G. Manco, M. Basagni, C. Maestrale, M. G. Cancedda, L. Madau, and A. Aguzzi. 2005. PrPSc in mammary glands of sheep affected by scrapie and mastitis. Nat. Med. 111137-1138. [DOI] [PubMed] [Google Scholar]
- 13.Mathiason, C. K., J. G. Powers, S. J. Dahmes, D. A. Osborn, K. V. Miller, R. J. Warren, G. L. Mason, S. A. Hays, J. Hayes-Klug, D. M. Seelig, M. A. Wild, L. L. Wolfe, T. R. Spraker, M. W. Miller, C. J. Sigurdson, G. C. Telling, and E. A. Hoover. 2006. Infectious prions in the saliva and blood of deer with chronic wasting disease. Science 314133-136. [DOI] [PubMed] [Google Scholar]
- 14.Murayama, Y., M. Yoshioka, H. Okada, M. Takata, T. Yokoyama, and S. Mohri. 2007. Urinary excretion and blood levels of prions in scrapie-infected hamsters. J. Gen. Virol. 882890-2898. [DOI] [PubMed] [Google Scholar]
- 15.Owen, J. P., R. H. Rees, B. C. Maddison, L. A. Terry, L. Thorne, R. Jackman, G. C. Whitelam, and K. C. Gough. 2007. Molecular profiling of ovine prion diseases by using thermolysin-resistant PrPSc and endogenous C2 PrP fragments. J. Virol. 8110532-10539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Race, R., A. Raines, G. J. Raymond, B. Caughey, and B. Chesebro. 2001. Long-term subclinical carrier state precedes scrapie replication and adaptation in a resistant species: analogies to bovine spongiform encephalopathy and variant Creutzfeldt-Jakob disease in humans. J. Virol. 7510106-10112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ryder, S., G. Dexter, S. Bellworthy, and S. Tongue. 2004. Demonstration of lateral transmission of scrapie between sheep kept under natural conditions using lymphoid tissue biopsy. Res. Vet. Sci. 76211-217. [DOI] [PubMed] [Google Scholar]
- 18.Saá, P., J. Castilla, and C. Soto. 2006. Presymptomatic detection of prions in blood. Science 31392-94. [DOI] [PubMed] [Google Scholar]
- 19.Saá, P., J. Castilla, and C. Soto. 2006. Ultra-efficient replication of infectious prions by automated protein misfolding cyclic amplification. J. Biol. Chem. 28135245-35252. [DOI] [PubMed] [Google Scholar]
- 20.Saborio, G. P., B. Permanne, and C. Soto. 2001. Sensitive detection of pathological prion protein by cyclic amplification of protein misfolding. Nature 411810-813. [DOI] [PubMed] [Google Scholar]
- 21.Safar, J. G., P. Lessard, G. Tamgüney, Y. Freyman, C. Deering, F. Letessier, S. J. DeArmond, and S. B. Prusiner. 2008. Transmission and detection of prions in feces. J. Infect. Dis. 19881-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soto, C., L. Anderes, S. Suardi, F. Cardone, J. Castilla, M.-J. Frossard, S. Peano, P. Saá, L. Limido, M. Carbonatto, J. Ironside, J.-M. Torres, M. Pocchiari, and F. Tagliavini. 2005. Pre-symptomatic detection of prions by cyclic amplification of protein misfolding. FEBS Lett. 579638-642. [DOI] [PubMed] [Google Scholar]
- 23.Thorne, L., and L. A. Terry. 2008. In vitro amplification of PrPSc derived from the brain and blood of sheep infected with scrapie. J. Gen. Virol. 893177-3184. [DOI] [PubMed] [Google Scholar]
- 24.Tongue, S. C., D. U. Pfeiffer, R. Warner, H. Elliot, and V. Del Rio Vilas. 2006. Estimation of the relative risk of developing clinical scrapie: the role of prion protein (PrP) genotype and selection bias. Vet. Rec. 15843-50. [DOI] [PubMed] [Google Scholar]
- 25.Wadsworth, J. D. F., S. Joiner, A. F. Hill, T. A. Campbell, M. Desbruslais, P. J. Luthert, and J. Collinge. 2001. Tissue distribution of protease resistant prion protein in variant Creutzfeldt-Jakob disease using a highly sensitive immunoblotting assay. Lancet 358171-180. [DOI] [PubMed] [Google Scholar]
- 26.Wilesmith, J. W., and J. M. B. Ryan. 1997. Absence of BSE in the offspring of pedigree suckler cows affected by BSE in Great Britain. Vet. Rec. 141250-251. [DOI] [PubMed] [Google Scholar]