Abstract
Context
Treating hypertension decreases mortality and disability from cardiovascular disease; but most hypertension remains inadequately controlled.
Objective
To determine if a new model of care that uses patient Web services, and adds home BP monitoring and pharmacist-assisted care, improves blood pressure control.
Design
The Electronic Communications and Home Blood Pressure Monitoring (e-BP) study was a three-arm randomized controlled trial based on the Chronic Care Model and delivered over a secure patient website from June 2005 to December 2007.
Setting
Integrated group practice in Washington state.
Participants
778 participants age 25–75 with uncontrolled essential hypertension and Internet access.
Interventions
Participants were randomly assigned to: (1) usual care (UC); (2) home BP monitoring and secure patient website training (BPM-Web); (3) this plus pharmacist care management delivered through Web communications (BPM-Web-Pharm).
Main Outcome Measures
Percentage of patients with controlled BP (<140/90 mm Hg) and changes in systolic and diastolic BP at 12 months.
Results
730 patients (94%) completed the 1-year follow-up visit. Patients assigned to BPM-Web had a nonsignificant increase in the percentage with controlled BP (<140/90 mm Hg) compared to UC (36%; [95% CI, 30% to 42%] versus 31% [95% CI, 25% to 37%], P = .21). Adding Web-based pharmacy care to home BP monitoring (BPM-Web-Pharm) significantly increased the percentage with controlled BP (56% [95% CI, 49% to 62%]) compared to usual care (P <.001) and home BP monitoring (P <.001). Diastolic BP was also decreased with BPM-Web-Pharm compared to UC and BPM-Web; and systolic BP was decreased stepwise from UC to BPM-Web to BPM-Web-Pharm. For patients with baseline systolic BP ≥160 mm Hg, BPM-Web-Pharm had greater net reduction in systolic BP (−13.3 mm Hg [95% CI, −19.5 to −7.1], P <.001) and diastolic BP (−5.1 mm Hg [95% CI, −8.5 to −1.8], P <.001), and BP control improved by 34.2% (95% CI, 15.7% to 50.2%).
Conclusions
Pharmacist care management delivered through secure patient Web communications improved BP control in patients with hypertension.
Hypertension is one of the leading causes of death worldwide.1 Almost one in three U.S. adults have hypertension, defined as a sustained blood pressure (BP) of ≥140/90 mm Hg.2,3 Lowering BP with antihypertensive medications decreases mortality and major disability from cardiovascular and renal disease. Hypertension, however, remains inadequately treated in the majority of affected individuals.4–6 In recent meta-analyses7,8 of quality improvement strategies to lower BP, those targeting patients (education and self-monitoring) or adding a healthcare team member, such as a nurse or a pharmacist, to focus specifically on hypertension had the largest BP reductions. Optimal methods for integrating these strategies into routine care were less certain.
Electronic medical records (EMRs) and secure patient websites increasingly let patients view portions of their medical record, access healthcare services, and communicate with their healthcare team online. Over 75% of adults nationally have Internet access9 and most want to use the Internet to contact doctors, make appointments, refill prescriptions, and receive laboratory results.10 However, little is known about the effectiveness of Web services in the care of chronic conditions.
Web-based care might be particularly suitable for improving hypertension care. Conventional office BP measurement is subject to error and bias11–13 and physicians often make medication decisions based on one or two office measurements, despite the known variability of BP.14 Self-monitoring of BP by patients provides similar accuracy, is less expensive, and provides direct feedback as to BP control.14,15
We hypothesized that hypertension care could be provided asynchronously and remotely over the Web without in-person clinic visits. Electronic Communications and Home Blood Pressure Monitoring (e-BP) was a three-arm randomized controlled trial designed to test whether hypertension control improved with home BP monitoring and training to use patient Web services, or this plus care management by a pharmacist over the Web.
METHODS
Design
A complete description of the design and methods of the e-BP study has been published elsewhere.16 A brief description follows.
The e-BP study was a three-armed randomized controlled trial designed to compare two interventions to improve hypertension control. Patients who had uncontrolled hypertension and were on antihypertensive medication were randomly assigned to: (1) usual care (UC); (2) home BP monitoring and secure patient Web services training (BPM-Web); or (3) this plus pharmacist care management delivered through Web communications (BPM-Web-Pharm). The study design was based on the Chronic Care Model.17 The model specifies six domains: self-management support, clinical information systems, delivery system redesign, decision support, healthcare organization, and community resources. According to the model, paying attention to these domains and integrating them can produce system changes in which informed activated patients interact collaboratively with prepared practice teams. The primary study outcomes were change in systolic and diastolic BP, and percentage of patients with controlled BP (<140/90 mm Hg) at 12 months. Secondary outcomes included changes in number of classes of antihypertensive medications, aspirin use, body mass index (BMI), physical activity, health-related quality of life, satisfaction with the health plan, and utilization of health care services from baseline until the 12-month follow-up. The institutional review board and a data safety monitoring board (DSMB) approved the protocol and monitored adverse events.
Setting
The trial was a single-site study conducted at 10 medical centers within Group Health, a large, nonprofit, integrated group practice that provides both medical coverage and care to more than 530,000 residents of Washington State and Idaho. A commercially available EMR integrated with patient website services was available at all Group Health-owned primary care clinics and hospitals at the beginning of the study. Patient Web services include the ability to refill medications, make appointments, view portions of their EMR (current health conditions, laboratory test results, clinic visit summaries, and lists of allergies, immunizations, and medications), and use secure messaging to contact healthcare team members.18
Recruitment and Baseline Assessment
We used clinical and administrative data sources to identify patients age 25–75 with a hypertension diagnosis and on antihypertensive medications, with no diagnoses of diabetes, cardiovascular or renal disease, or other serious conditions. Research assistants telephoned potential participants to confirm eligibility, including the ability to use a computer, regular access to the Web, an email address, and willingness to attend screening visits and obtain all their antihypertensive medications at Group Health-owned pharmacies. Eligible and willing patients were invited to two screening visits at their clinic where a research assistant measured BP using the validated Omron Hem-705CP automated monitor.19,20 If mean BP (last two of three BP recordings, with the first measurement dropped) was 90–109 mm Hg diastolic or 140–199 mm Hg systolic at both screening visits, the participant was eligible for the study and written informed consent was obtained.
To assure blinding for the primary outcomes—changes in systolic and diastolic BPs and control of BP—at baseline (T0), BP measurements from both screening visits (four measurements total) were averaged and recorded before consent and randomization. Baseline height, weight, and self-reported data were also obtained prior to randomization. Randomized patients had only one more study-related clinic visit, at 12 months (T1), to obtain blinded outcome assessments. Study interventions were provided via the secure patient website.
Randomization
We used a single-blind block independent randomization design to ensure balance within medical centers and baseline systolic BP measurements. We stratified participants into two groups: baseline systolic BP 160–199 mm Hg and 140–159 mm Hg. Within these two groups, we randomly assigned sequential blocks of three, six, or nine to the three study groups. To assure the research assistant was blinded to study group assignment during initial training interventions, random assignment occurred in two steps. After consent, the research assistant opened a sequentially numbered opaque envelope with the pre-assigned random study group allocating patients to either the UC group or the combined intervention group. After receipt of the BP monitor and Web training, a second opaque envelope was opened assigning them to BPM-Web or BPM-Web-Pharm.
Interventions
Before randomization, all participants were registered to use Group Health’s secure patient Web services if they had not already done so. Patients in all groups also received Group Health’s hypertension pamphlet (“High Blood Pressure and You”), which describes definitions for BP control, the importance of medication, and lifestyle behaviors that influence BP and cardiovascular risk (i.e., sodium intake, weight, and physical activity) and Group Health’s pamphlet (“The No-Waiting Room”), which describes the patient website and utilities available to registered users. After the first randomization, those assigned to UC were told their BP was not in control and were encouraged to work with their physician to improve it. Those assigned to the other two study arms received additional interventions.
Home BP Monitor Receipt and Training and Patient Website Training
Patients assigned to active interventions were first given a home BP monitor (the validated Omron Hem-705CP, with the cuff size based on upper arm measurements19,20 and training on its use, demonstrating they could use it without help. They were instructed to use this monitor to check their BP at least two days a week with two measurements each time. They were told the goal for average home BP was <135/85 mm Hg, lower than the goal for clinic measurements of <140/90 mm Hg (based on observational data demonstrating that BP readings in subjects tend to be about 5 mm Hg lower when taken at home).21 Second, they received training on use of the website. They received a tour of the different utilities (secure email, refilling medications, viewing portions of their medical record, use of the health library, and links to Group Health and community resources for lifestyle behavior change).
After the initial training, the second opaque envelope was opened and patients assigned to BPM-Web were told their BP was not controlled and advised to work with their physician to improve this. They were given the following verbal and written instructions: “As a participant in Group 2, you have two additional resources (the home BP monitor and MyGroupHealth) to help manage your high blood pressure. We encourage you to use the MyGroupHealth website. It gives you access to a suite of online services so you can e-mail your doctor, refill prescriptions, request appointments, get test results, and look up health information. Sending a message to your provider on MyGroupHealth is an easy way to report your home BP readings”. Those assigned to BPM-Web-Pharm were told a pharmacist would be assisting them to improve their BP control via home BP monitoring and Web communications.
Pharmacist Care Management (BPM-Web-Pharm Intervention)
Three Group Health pharmacists performed all pharmacy interventions. They were “clinical pharmacists” with experience and time separate from “front-line” customer service to assist with “team-based” care management activities (such as collaborating with physicians and patients to assure adequate lipid lowering in patients with cardiovascular disease). They received two half-days of additional training on evidence-based care of hypertension, the stepped medication protocols used in the intervention [based on Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) and Group Health guidelines],3 and patient-centered techniques for addressing behavioral issues related to adherence and lifestyle change. The e-BP study interventions were included in the pharmacists’ usual daily activities and, depending on their average patient load (about 50 patients each), took them from two to eight hours a week.
The pharmacist welcomed the patient to the study with a secure message and informed the patient’s physician of their participation with a staff message. The pharmacist also arranged a time for one planned telephone visit to obtain a more detailed medication history and review allergies, intolerances, and cardiovascular risk factors. At the end of the telephone call, the pharmacist introduced the patient to the “action plan”. Used for Web communications, the action plan was a template with five components: instructions for home BP monitoring; a list of current medications; and at least one patient-selected lifestyle goal(s) from the list in the Group Health hypertension pamphlet (such as increasing physical activity); recommended medication changes based on the stepped medication protocols; and the follow-up plan. Each patient and his or her physician received an electronic copy of the action plan. Then all planned communication occurred over the Web every 2 weeks until BP was controlled (mean home BP of <135/85 mm Hg) and less often thereafter. Patients were asked to provide BP measurements, concerns about medications, and progress related to their lifestyle goal(s). Pharmacists responded with specific recommendations (including medication changes) and patients were encouraged to provide feedback and collaboratively change the action plan. All clinical concerns or potential deviations from the medication protocol were referred back to the patient’s physician. All secure messages between pharmacists and patients and staff messages between the pharmacist and the patient’s physician were part of the EMR.
Blinded Outcome Assessments
At the 12-month follow-up visit at the patient’s clinic, trained research assistants blinded to the patients study group measured BP using the same protocol as baseline. Automated databases were utilized to obtain use of antihypertensive medications, with five pre-defined classes: diuretics, angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers, calcium channel blockers, beta-blockers, and others (alpha-blockers, hydralazine, minoxidil, clonidine, reserpine, guanethidine, and methyldopa, which were used infrequently). Use of a medication class was defined as patient procurement of ≥60 days’ supply of medication during a 182-day period. Aspirin use was measured by self-report at baseline and 12-month follow-up. Health-related quality of life was measured using the SF-12.22,23 BMI was calculated from height and weight at baseline and weight at the follow-up visit. Physical activity was measured using the Stages of Change questionnaire by Marcus et al.24 Satisfaction with the health plan was assessed using the Consumer Assessment of Healthcare Providers and Systems (CAHPS) instrument.25 Secure message use was measured by the number of message threads between providers and patients. A message thread is defined as an initial message sent by either the patient or the provider and the series of subsequent replies from both parties.26 Utilization of outpatient primary and specialty care, emergency department, hospital services, and telephone encounters was obtained from clinical and administrative databases that Group Health maintains.
We collected demographic characteristics and prior use of home BP monitoring at the time of the telephone survey. When participants chose more than one category for race, coding precedence was given to African American, Asian American, Other, and Caucasian categories, in that order.
Sample Size
The study was designed to enroll 780 patients equally to each of the three intervention groups. The sample size was powered to detect clinically meaningful differences in mean changes in systolic BP of 4 mm Hg and diastolic BP of 3 mm Hg between UC and BPM-Web-Pharm at 12-month follow-up (T1). It was assumed that BPM-Web-Pharm was equivalent to BPM-Web in the sample-size calculations; therefore, we powered on only one comparison. This sample size provided 80% and 86% power to detect differences in systolic and diastolic BP, respectively, and assumed a normal approximation to compare two independent means, standard deviation for systolic BP of 14.5 mm Hg and diastolic BP of 10 mm Hg, and an 80% follow-up rate. This sample size provided 80% power to detect 11.7% improvement in BP control in BPM-Web-Pharm compared to UC at T1 and assumed that 20% of the UC group would attain BP control at T1 due to regression to the mean and changes in treatment regimen, 80% follow-up, and normal approximation without the continuity correction. The sample size did not take into account adjustment for precision variables in our primary analyses; therefore, this calculation was conservative.
Statistical Analysis
TABLE 1 presents summary statistics (frequencies, means, and standard deviations) for baseline patient characteristics—age, sex, race/ethnicity, education, employment, number of hypertension medication classes, tobacco use, BMI, exercise, having a home BP monitor prior to study enrollment), clinic, and baseline systolic, and diastolic BP—and stratified by intervention group and baseline systolic BP ≥160 mm Hg subgroup. To assess for any differences between intervention groups by baseline characteristics, we performed Pearson’s chi-square test for categorical variables27 and F-tests for continuous variables.28,29
Table 1.
Baseline Characteristics of the e-BP Trial Patients (N = 778) Randomly Assigned to 3 Intervention Groups
| Characteristic | Total | Usual Care (n = 258) |
BPM-Web (n = 259) |
BPM-Web- Pharm (n = 261) |
P Valuea | ||||
|---|---|---|---|---|---|---|---|---|---|
| Age, mean (SD), y | 59.1 | (8.5) | 58.6 | (8.5) | 59.5 | (8.3) | 59.3 | (8.6) | 0.41 |
| Female, No. (%) | 406 | (52.2) | 141 | (54.7) | 119 | (45.9) | 146 | (55.9) | 0.05 b |
| Race, No. (%) | |||||||||
| White | 644 | (82.8) | 214 | (82.9) | 223 | (86.1) | 207 | (79.3) | 0.34 |
| African American | 61 | (7.8) | 22 | (8.5) | 18 | (6.9) | 21 | (8.0) | |
| Asian American | 29 | (3.7) | 8 | (3.1) | 9 | (3.5) | 12 | (4.6) | |
| Other/Refused to say | 44 | (5.7) | 14 | (5.4) | 9 | (3.5) | 21 | (8.0) | |
| Education, No. (%) | |||||||||
| ≤12-y or GED | 62 | (8.0) | 22 | (8.5) | 19 | (7.3) | 21 | (8.0) | 0.11 |
| Some post high school | 324 | (41.6) | 117 | (45.3) | 110 | (42.5) | 97 | (37.2) | |
| 4-y college degree | 195 | (25.1) | 48 | (18.6) | 72 | (27.8) | 75 | (28.7) | |
| Post 4-y college degree | 197 | (25.3) | 71 | (27.5) | 58 | (22.4) | 68 | (26.1) | |
| Employment, No. (%) | |||||||||
| Full-time | 435 | (55.9) | 158 | (61.2) | 130 | (50.2) | 147 | (56.3) | 0.13 |
| Retired | 270 | (34.7) | 75 | (29.1) | 103 | (39.8) | 92 | (35.2) | |
| Part-time | 51 | (6.6) | 16 | (6.2) | 21 | (8.1) | 14 | (5.4) | |
| Other/Refused to say | 22 | (2.8) | 9 | (3.5) | 5 | (1.9) | 8 | (3.1) | |
| Antihypertensive medication classes, No. (%) | |||||||||
| 0 | 28 | (3.6) | 13 | (5.0) | 5 | (1.9) | 10 | (3.8) | 0.16 |
| 1 | 366 | (47.0) | 127 | (49.2) | 120 | (46.3) | 119 | (45.6) | |
| 2 | 261 | (33.5) | 89 | (34.5) | 86 | (33.2) | 86 | (33.0) | |
| 3+ | 123 | (15.8) | 29 | (11.2) | 48 | (18.5) | 46 | (17.6) | |
| Current smoker, No. (%) | 52 | (6.8) | 20 | (8.1) | 14 | (5.5) | 18 | (6.9) | 0.51 |
| Missing | 15 | ||||||||
| Body mass index (BMI), No. (%) | |||||||||
| Normal (18.5–24.9) | 54 | (7.2) | 16 | (6.5) | 14 | (5.6) | 24 | (9.5) | 0.37 |
| Overweight (25–29.9) | 237 | (31.6) | 72 | (29.4) | 84 | (33.3) | 81 | (32.1) | |
| Obese (≥30) | 458 | (61.1) | 157 | (64.1) | 154 | (61.1) | 147 | (58.3) | |
| Missing | 29 | ||||||||
| Already had home BPM, No. (%) | 437 | (56.2) | 137 | (53.1) | 160 | (61.8) | 140 | (53.6) | 0.08 b |
| Systolic BP, mean (SD), mm Hg | 151.9 | (10.3) | 151.3 | (10.6) | 152.2 | (10.0) | 152.2 | (10.4) | 0.55 |
| Diastolic BP, mean (SD), mm Hg | 89.1 | (8.0) | 89.4 | (8.0) | 89.0 | (7.9) | 88.9 | (8.1) | 0.74 |
Abbreviations: e-BP, Electronic Communications and Home Blood Pressure Monitoring; BPM-Web, home BP monitoring and secure patient Web services training (BPM-Web); BPM-Web-Pharm, home BP monitoring and secure patient Web services training plus pharmacist care management delivered through Web communications; SD, standard deviation; GED, general equivalency degree; BMI, body mass index; BPM, blood pressure monitor; BP, blood pressure.
P value from an F-test for continuous outcomes and chi-square test for binary outcomes comparing a difference between any of the 3 intervention groups
Significant at P <.10 level.
Following the a priori primary analysis plan, we evaluated the differences between intervention groups and continuous primary outcomes using linear regression models adjusted for baseline outcome measures (e.g., systolic BP at T0 for the outcome systolic BP at T1 and diastolic BP at T0 for the outcome diastolic BP at T1) and baseline characteristics that were significantly related, at the α = .10 level, to either the outcome of interest or intervention group. All statistical tests were performed using F-tests. To protect against multiple comparisons, we used Fisher’s protected least-significant-difference approach.30 This approach makes pair-wise comparisons between the three treatment groups only if the overall F-test is significant. Pre-specified secondary analyses were also presented for unadjusted linear regression models.
For the binary primary outcome, BP control (BP <140/90 mm Hg), we applied generalized linear models with a log link and robust sandwich variance estimator using modified Poisson regression.31 Logistic regression models were not used, because controlled BP was not rare. We adjusted for baseline characteristics in the same manner as for continuous outcomes. All P values for binary outcomes are from a chi-square test. Pre-specified unadjusted analyses are also presented as proportion controlled with Wald 95% CI. 32
For the primary outcomes, we also repeated the planned analyses on the subgroup of participants with baseline systolic BP ≥160 mm Hg to assess the intervention’s effectiveness for more extreme hypertension. Secondary outcomes followed a similar modeling scheme to the primary analyses except all analyses were unadjusted. All secondary outcome analyses were conducted on the subset of patients who attended a T1 visit.
All analyses were performed using the statistical package R, Version 2.6.133 except for the modified Poisson regression, which was generated using SAS, Version 9 of the SAS System for Windows. All reported P values and confidence intervals are two-sided. All analyses assumed intention-to-treat principles, i.e., comparing patients in the groups to which they were originally randomly assigned. We attempted follow-up with all patients, and we included all patients who completed follow-up in their randomized intervention assignment, regardless of whether they received the intervention, or subsequently withdrew or deviated from the protocol.34 Our primary analyses apply intention-to-treat principles to those patients for whom we obtained complete follow-up. We adjusted those analyses for any baseline covariates that may influence the outcome, to remove potential bias due to loss to follow-up, which was low. Because the loss to follow-up was only 6%, these procedures introduce less bias than the alternative of imputing missing values, which would preclude adjusting for baseline covariates.
RESULTS
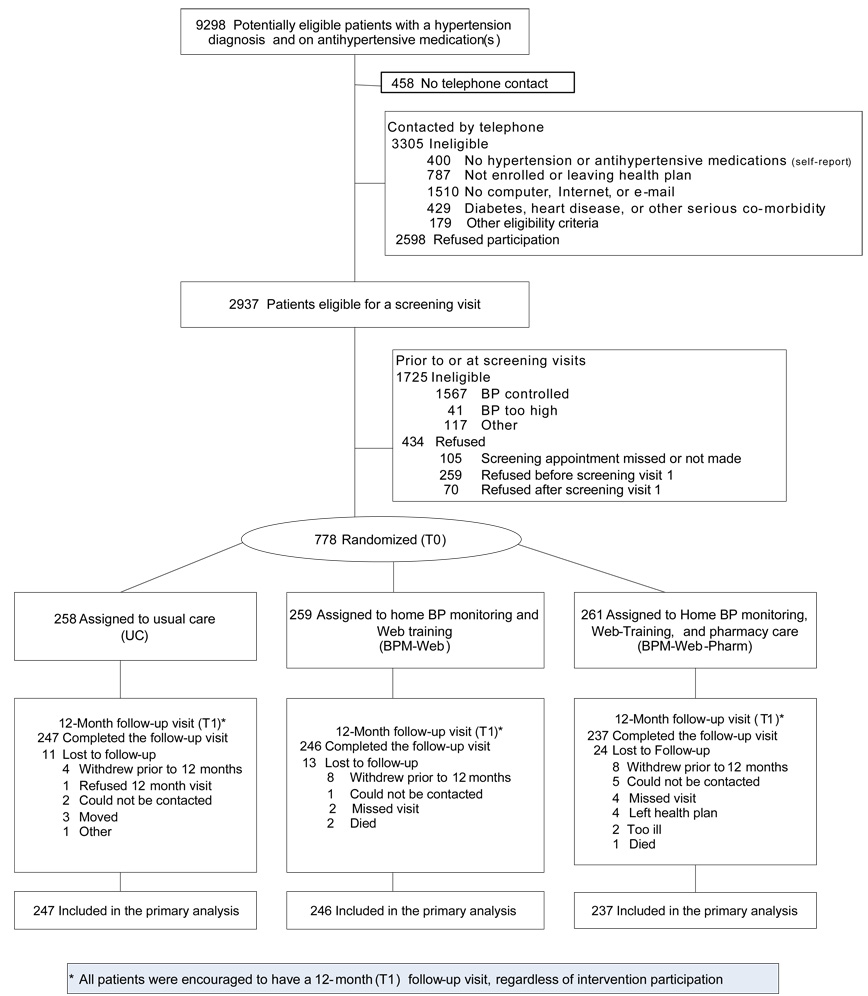
FIGURE 1 shows the flow of participants through the study. Letters were mailed to 9298 patients with an ICD-9 diagnosis of hypertension. Of those answering the telephone survey questions, 78.2% (1574/7279) were “computer able” (based on the percent answering these questions). Of those who had a screening appointment and had their BP measured, 60.9% (1567/2573) had controlled hypertension, making them ineligible. Of the total sample contacted who remained eligible, 20.4% (778/3810) consented to participate. A total of 778 computer-able patients with uncontrolled essential hypertension were enrolled from 10 medical centers, of whom 730 (94%) completed the 12-month follow-up visit. Completion rates did not differ significantly by study group and were higher than the assumed 80% follow-up rate in the sample size determination.
Figure 1.
Flow of e-BP Trial Patients Through Recruitment, Intervention, and Blinded Follow-up Assessments
Patient Characteristics
Demographic characteristics of the study groups were comparable at baseline (P >.10), except for sex and already having a home BP monitor (TABLE 1). To account for these differences, we adjusted for these variables in the primary analyses. Overall, racial minorities were better represented than is typical for Group Health and the surrounding Puget Sound area. By definition, all patients had uncontrolled hypertension: 44.6% had elevated systolic BP only, 7.6% had elevated diastolic BP only, and 47.8% had combined systolic and diastolic BP elevation, with a group mean of 151.9 mm Hg systolic and 89.1 mm Hg diastolic BP. Baseline BPs were similar in all three groups. For the pre-specified subgroup with baseline systolic BP ≥160 mm Hg, mean systolic BP was 167.6 mm Hg and mean diastolic BP was 90.7 mm Hg at baseline.
Primary Outcomes
Compared to patients receiving usual care (UC), the BP control (<140/90 mm Hg) of those receiving home BP monitoring, Web training, and encouragement to send BP numbers to their physician (BPM-Web) did not improve; however, they had a nonsignificant trend in that direction and a modest reduction in systolic BP (net change −2.9 mm Hg [95% CI −5.4 to −0.4], P =.02) (TABLE 2). The addition of Web-based pharmacy care (BPM-Web-Pharm) resulted in 25% more patients with controlled BP compared to UC and 20% more patients with controlled BP compared to BPM-Web (UC 31% [95% CI, 25% to 37%]; BPM-Web 36% [95% CI, 30% to 42%], P <.001; and BPM-Web-Pharm 56% [95% CI, 49% to 62%], P <.001). Adjusted analyses found a 1.8 times increase in BP control for BPM-Web-Pharm (RR 1.8 [95% CI, 1.5 to 2.3] P <.001) and a 1.2 times increase for BPM-Web (RR 1.2 [95% CI, 0.95 to1.6] P <.001) compared to UC. BPM-Web-Pharm resulted in greater reductions in systolic BP compared to UC (mean net change −8.9 mm Hg ([95% CI, −11.4 to −6.3] P <.001) and BPM-Web (mean net change −6.0 mm Hg [95% CI −8.5 to −3.5], P <.001). BPM-Web-Pharm also led to significant decreases to diastolic BP compared to UC (net change −3.5 mm Hg [95% CI −4.9 to −2.1] P <.001). For the subgroup with baseline systolic BP ≥160 mm Hg, BPM-Web-Pharm had 3.3 times more patients in BP control (RR 3.3 [95% CI, 1.9 to 5.9], P <.001), −13.2 mm Hg lower systolic BP (95% CI, −19.2 to −7.1, P <.001), and −4.6 mm Hg lower diastolic BP (95% CI, −8.0 to −1.2, P <.001) compared to UC.
Table 2.
Primary Outcomes at 12 Months for All Patients Completing Follow-up in e-BP Trial by Intervention Group, Then Stratified by Elevated Blood Pressure
| P valuese for Testing Difference Between Intervention Groups |
||||||||
|---|---|---|---|---|---|---|---|---|
| 12-Month BP Outcomes for All Patients Completing Follow-up, n = 730 | Usual Care (n = 247) | BMP-Web (n = 246) | BPM-Web-Pharm (n = 237) | Overall P valued | BPM-Web to Usual Care | BPM-Web-Pharm to Usual Care | BPM-Web-Pharm to BPM-Web | |
| Systolic BP (95 % CI) | ||||||||
| Unadjusted, mean | 146.3 (144.5, 148.2) | 143.8 (141.9, 145.6) | 137.9 (136.0, 139.8) | <.001 | .06 | <.001 | <.001 | |
| Adjusted, mean changea | −5.3 (−7.1, −3.5) | −8.2 (−10.0, −6.4) | −14.2 (−16.0, −12.4) | <.001 | .02 | <.001 | <.001 | |
| Diastolic BP (95 % CI) | ||||||||
| Unadjusted, mean | 85.7 (84.5, 86.9) | 84.5 (83.3, 85.7) | 81.6 (80.4, 82.9) | <.001 | .18 | <.001 | <.001 | |
| Adjusted, mean changea | −3.5 (−4.5, −2.5) | −4.4 (−5.4, −3.4) | −7.0 (−8.0, −6.0) | <.001 | .21 | <.001 | <.001 | |
| BP controlled (95% CI)b | ||||||||
| Unadjusted, Yes/No, % | 0.31 (0.25, 0.37) | 0.36 (0.30, 0.42) | 0.56 (0.49, 0.62) | <.001 | .20 | <.001 | <.001 | |
| Adjusted RR, Yes/Noc | 1 | 1.22 (0.95, 1.56) | 1.84 (1.48, 2.29) | <.001 | .20 | <.001 | <.001 | |
| Subanalysis of patients in trial whose systolic BP at baseline was ≥160 mm Hg, completing follow-up, n = 150 | Usual Care (n = 51) | BPM-Web (n = 47) | BPM-Web-Pharm (n = 52) | Overall P valued | BPM-Web to Usual Care | BPM-Web-Pharm to Usual Care | BPM-Web-Pharm to BPM-Web | |
| Systolic BP (95 % CI) | ||||||||
| Unadjusted, mean | 152.4 (148.2, 156.6) | 151.0 (146.6, 155.4) | 139.8 (135.6, 144.0) | <.001 | .64 | <.001 | <.001 | |
| Adjusted, mean changea | −14.4 (−18.6, −10.1) | −17.8 (−22.2, −13.4) | −27.6 (−31.8, −23.4) | <.001 | .30 | <.001 | <.001 | |
| Diastolic BP (95 % CI) | ||||||||
| Unadjusted, mean | 84.4 (81.6, 87.2) | 83.8 (80.9, 86.7) | 81.0 (78.2, 83.8) | .21 | .78 | .10 | .10 | |
| Adjusted, mean changea | −5.6 (−8.0, −3.2) | −6.3 (−8.8, −3.8) | −10.2 (−12.6, −7.8) | .02 | .70 | .01 | .03 | |
| BP controlled (95%CI)b | ||||||||
| Unadjusted, Yes/No, % | 0.20 (0.11, 0.33) | 0.26 (0.15, 0.40) | 0.54 (0.40, 0.67) | <.001 | .20 | <.001 | <.001 | |
| Adjusted RR, Yes/Noc | 1 | 1.88 (0.94, 3.78) | 3.32 (1.86, 5.94) | <.001 | .08 | <.001 | .046 | |
| Table 2b. Sensitivity Analysis: Primary Outcomes at 12 Months for All Patients Assuming Those Not Completing Follow-up Had Baseline Blood Pressure in e-BP Trial by Intervention Group, Then Stratified by Elevated Blood Pressure | ||||||||
|---|---|---|---|---|---|---|---|---|
| P valuese for Testing Difference Between Intervention Groups | ||||||||
| 12-Month BP Outcomes for All Patients, n = 778 | Usual Care (n = 258) | BPM-Web (n = 259) | BPM-Web-Pharm (n = 261) | Overall P valued | BPM-Web to Usual Care | BPM-Web-Pharm to Usual Care | BPM-Web-Pharm to BPM-Web | |
| Systolic BP (95% CI) | ||||||||
| Unadjusted, mean | 146.5 (144.7, 148.3) | 144.2 (142.4, 146.0) | 139.1 (137.3, 140.9) | <.001 | .08 | <.001 | <.001 | |
| Adjusted, mean changea | −5.1 (−6.9, −3.4) | −7.8 (−9.5, −6.1) | −12.9 (−14.6, −11.2) | .002 | .03 | <.001 | <.001 | |
| Diastolic BP (95% CI) | ||||||||
| Unadjusted, mean | 86.0 (84.9, 87.2) | 84.9 (83.7, 86.1) | 82.7 (81.5, 83.9) | <.001 | .17 | <.001 | <.001 | |
| Adjusted, mean changea | −3.3 (−4.3, −2.4) | −4.1 (−5.1, −3.2) | −6.2 (−7.2, −5.3) | <.001 | .26 | <.001 | .003 | |
| BP controlled (95% CI)b | ||||||||
| Unadjusted, Yes/No, % | 0.29 (0.24, 0.35) | 0.34 (0.29, 0.40) | 0.51 (0.45, 0.57) | <.001 | .23 | <.001 | <.001 | |
| Adjusted RR, Yes/Noc | 1 | 1.19 (0.93, 1.52) | 1.74 (1.39, 2.18) | <.001 | .18 | <.001 | <.001 | |
| Subanalysis of patients in trial whose systolic BP at baseline was ≥160 mm Hg, n = 162 | Usual Care (n = 54) | BPM-Web (n = 50) | BPM-Web-Pharm (n = 58) | Overall P valued | BPM-Web to Usual Care | BPM-Web-Pharm to Usual Care | BPM-Web-Pharm to BPM-Web | |
| Systolic BP (95% CI) | ||||||||
| Unadjusted, mean | 153.2 (149.0, 157.4) | 152.0 (147.6, 156.4) | 142.5 (138.4, 146.6) | <.001 | .71 | <.001 | <.001 | |
| Adjusted, mean changea | −13.9 (−18.1, −9.7) | −16.3 (−20.7, −11.9) | −25.0 (−29.1, −21.0) | <.001 | .46 | <.001 | .005 | |
| Diastolic BP (95% CI) | ||||||||
| Unadjusted, mean | 85.2 (82.4, 87.9) | 84.1 (81.2, 87.0) | 82.3 (79.6, 85.0) | .35 | .62 | .15 | .15 | |
| Adjusted, mean changea | −5.3 (−7.7, −3.0) | −5.9 (−8.3, −3.5) | −9.0 (−11.2, −6.8) | .06 | .75 | .03 | .07 | |
| BP controlled (95% CI)b | ||||||||
| Unadjusted, Yes/No, % | 0.19 (0.10, 0.31) | 0.24 (0.14, 0.38) | 0.48 (0.36, 0.61) | .001 | .40 | .001 | .01 | |
| Adjusted RR, Yes/Noc | 1 | 1.73 (0.85, 3.51) | 3.10 (1.73, 5.58) | <.001 | .13 | <.001 | .04 | |
Abbreviations: e-BP, Electronic Communications and Home Blood Pressure Monitoring; BPM-Web, home BP monitoring and secure patient Web services training; BPM-Web-Pharm, home BP monitoring and secure patient Web services training plus pharmacist care management delivered through Web communications; BP, blood pressure; CI, confidence interval; RR, relative risk.
Adjusted mean change is the estimated mean change in 12-month outcome from baseline value from a linear regression model adjusted for baseline outcome value, sex, already having a home BP monitor before trial, and clinic while assuming mean baseline covariate values.
BP controlled is defined as <140/90 mm Hg.
Adjusted controlled BP is the estimated relative risk (RR) comparing each intervention arm to usual care for the outcome of controlled BP in a modified Poisson regression model adjusted for body mass index, sex, already having a home BP before trial, baseline systolic BP, and clinic.
P-values from an F-test for continuous outcomes and chi-square test for binary outcomes comparing a difference between any of the 3 intervention groups.
P-values from a Wald T-test for continuous outcomes and Wald Z-test for binary outcomes comparing a difference between two intervention groups.
Abbreviations: e-BP, Electronic Communications and Home Blood Pressure Monitoring; BPM-Web, home BP monitoring and secure patient Web services training; BPM-Web-Pharm, home BP monitoring and secure patient Web services training plus pharmacist care management delivered through Web communications; BP, blood pressure; CI, confidence interval; RR, relative risk.
Adjusted mean change is the estimated mean change in 12-month outcome from baseline value from a linear regression model adjusted for baseline outcome value, sex, already having a home BP monitor before trial, and clinic while assuming mean baseline covariate values
BP controlled is defined as <140/90 mm Hg.
Adjusted controlled BP is the estimated relative risk (RR) comparing each intervention arm to usual care for the outcome of controlled BP in a modified Poisson regression model adjusted for body mass index, sex, already having a home BP before trial, baseline systolic BP, and clinic.
P values from an F-test for continuous outcomes and Likelihood Ratio Chi-square test for binary outcomes comparing a difference between any of the 3 intervention groups.
P values from a Wald T-test for continuous outcomes and Wald Z-test for binary outcomes comparing a difference between two intervention groups.
Secondary Outcomes
At baseline, patients took a mean of 1.6 antihypertensive medication classes. At 12 months, there was a stepped increase in mean number of antihypertensive medications classes filled, with BPM-Web (1.9, SD 0.9) significantly greater than UC (1.7, SD 0.9) (P <.01) and BPM-Web-Pharm (2.2, SD 0.9) significantly greater than both UC (P <.001) and BPM-Web (P <.01) (TABLE 3). Aspirin use for BPM-Web-Pharm significantly increased by 1.3 times and 1.2 times compared to UC and BPM-Web, respectively (RR 1.3 [95% CI, 1.1 to 1.5]; 1.2 [95% CI, 1.1 to 1.4]). Aspirin use did not significantly change for BPM-Web compared to UC. BMI, physical activity, health-related quality of life, and satisfaction with the health plan did not differ among the three groups.
Table 3.
Secondary Outcomes at 12 Months for All Patients Completing Follow-up in e-BP Trial by Intervention Group
| Assessing the Difference Between Intervention Groups |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Usual Care | BPM-Web | BPM-Web-Pharm | BPM-Web to Usual Care | BPM-Web-Pharm to Usual Care | BPM-Web-Pharm to BPM-Web | |||||
| Baseline | 12 Months | 12 Months | 12 Months | Ea | (95% CI) | E | (95% CI) | E | (95% CI) | |
| Number of HTN Med classes, mean (SD) | 1.64 (0.85) | 1.69 (0.91) | 1.94 (0.91) | 2.16 (0.93) | 0.3 | (0.1, 0.4)c | 0.5 | (0.3, 0.6) d | 0.2 | (0.1, 0.4) c |
| Aspirin use, Yes, No. (%) | 338 (48.8) | 124 (53.0) | 131 (56.0) | 149 (66.5) | 1.1 | (0.9, 1.2) | 1.3 | (1.1, 1.5) c | 1.2 | (1.0, 1.4) b |
| Missing | 38 | |||||||||
| BMI, mean (SD) | 32.3 (6.5) | 32.5 (6.5) | 32.5 (7.0) | 31.6 (6.2) | 0.0 | (−1.1, 1.2) | −0.9 | (−2.1, 0.3) | −0.9 | (−2.1, 0.3) |
| Missing | 34 | |||||||||
| Active, Yes, No. (%) | 464 (68.1) | 158 (68.4) | 173 (73.9) | 155 (71.8) | 1.1 | (1.0, 1.2) | 1.0 | (0.9, 1.2) | 1.0 | (0.9, 1.1) |
| Missing | 49 | |||||||||
| Quality of Life, SF2, 1–100 Scale | ||||||||||
| General health, SF1, mean (SD) | 67.1 (20.4) | 66.7 (20.4) | 66.6 (20.9) | 66.6 (22.2) | −0.1 | (−4.0, 3.7) | −0.1 | (−4.0, 3.8) | 0.0 | (−3.9, 3.9) |
| Missing | 38 | |||||||||
| Physical health, mean (SD) | 80.6 (27.0) | 78.1 (27.7) | 77.7 (30.3) | 81.0 (26.5) | −0.4 | (−5.6, 4.7) | 2.8 | (−2.3, 8.0) | 3.3 | (−1.9, 8.5) |
| Missing | 44 | |||||||||
| Emotional health, mean (SD) | 71.6 (16.8) | 71.5 (17.7) | 72.1 (16.8) | 71.7 (19.7) | 0.5 | (−2.7, 3.8) | 0.1 | (−3.2, 3.4) | −0.4 | (−3.7, 2.9) |
| Missing | 39 | |||||||||
| CAHPS, mean (SD), 0–10 Scale | 7.9 (1.5) | 8.1 (1.5) | 8.1 (1.5) | 8.3 (1.4) | 0.0 | (−0.3, 0.3) | 0.2 | (−0.1, 0.5) | 0.2 | (−0.0, 0.5) |
| Missing | 65 | |||||||||
Abbreviations: e-BP, Electronic Communications and Home Blood Pressure Monitoring; BPM-Web, home BP monitoring and secure patient Web services training (BPM-Web); BPM-Web-Pharm, home BP monitoring and secure patient Web services training plus pharmacist care management delivered through Web communications; CI, confidence interval; SD, standard deviation; BMI, body mass index; CAHPS, Assessment of Healthcare Providers and Systems.
E = estimate: stands for mean difference if outcome is continuous and RR if outcome is binary.
Significant at P <.05 level.
Significant at P <.01 level.
Significant at P <.001 level.
Secure Messages and Other Healthcare Utilization
In the 12 months after randomization, mean number of message threads (a secure message and subsequent responses) was higher in the BPM-Web-Pharm group (22.3, SD 10.2) than in the UC (2.4, SD 4.6) and BPM-Web (3.3 , SD 7.4) groups, because the pharmacists regularly initiated these threads. Patient-initiated threads increased significantly in the BPM-Web group compared to UC (P = .01) and in the BPM-Web-Pharm group compared to both UC (P <.01) and BPM-Web (P <.01) (mean number of patient initiated message threads: UC 1.8, SD 4.2; BPM-Web 2.7, SD 7.1; BPM-Web-Pharm 4.2, SD 6.0). At 12 months, with the one planned phone encounter excluded, phone encounters were also higher in the BPM-Web-Pharm (mean 7.5, SD 9.3) compared to the BPM-Web (3.8, SD 5.0) (P <.001) and UC groups (4.0, SD 4.8) (P <.001). Primary care visits did not differ between patients in the UC, BPM-Web, and BPM-Web-Pharm groups (with 3.2, 3.0, and 3.2 visits, respectively, over 12 months). There were also no significant differences among patients in any arm with respect to inpatient and urgent care/emergency use at 12 months. There was a modest but significant decrease in the percentage of patients in the BPM-Web-Pharm group with office visits to a specialist in 12 months (P = .04 ) relative to baseline and to patients in the other arms.
Serious Adverse Events
Three people died during the study: two in the BPM-Web group from cancer-related complications and a third in the BPM-Web-Pharm group from a cardiac arrest. Seven patients had non-fatal cardiovascular events: two in the UC, four in the BPM-Web, and three in the BPM-Web-Pharm group. The DSMB and investigators attributed none of the deaths, cardiovascular events, or other hospitalizations to study participation.
COMMENT
Summary
The results of this study indicate that Web-based pharmacy care improved BP control. Our intervention was particularly effective for those with higher systolic BP (≥160 mm Hg at baseline), which is typically more difficult to treat and associated with increased cardiovascular risk.35
Our study findings support previous research that demonstrates encouraging patients to participate more actively in their own care, combined with care management,36 including assisted patient review of paper medical records,37,38 leads to improved health outcomes. Our intervention extends this work by connecting patients and care managers through a shared EMR over the Web. In our study, providing home BP monitors and Web training alone did not significantly improve BP control, despite trends in that direction. These results are consistent with recent meta-analyses7,8,39,40 showing care delivered by an ancillary care provider, such as a nurse or pharmacist, resulted in larger decreases in BP than did home BP monitoring and patient education interventions alone.
Limitations
Our intervention was limited to those with uncontrolled essential hypertension, and patients were required to have computer, Internet, and email access. We sent letters to more than 9000 patients with a diagnosis of hypertension, but more than two thirds of them were ineligible. Patients without computer access (22%) were more likely to be older, belong to racial or ethnic minority groups, and have less education, suggesting a “digital divide”. This gap between persons with and without access to the Internet may narrow with time as the population ages, but some patients are likely to remain without access to care over the Web.41 Patients were also ineligible if they had diabetes, heart disease, or other serious diseases, as we wanted to keep medications protocols simple for this first test of Web-based care. Patients also had better BP control than expected, with 60.9% having controlled5,6 hypertension at the recruitment screening visits. These rates of control are better than those published in peer-reviewed literature,4 but similar to those reported by National Committee for Quality Assurance (NCQA) Health Plan Employer Data and Information Set (HEDIS®).42 The e-BP study began shortly after implementation of the EMR, and there were not enough clinic BP measurements in the EMR for us to use these to pre-identify patients more likely to have uncontrolled BP. However, now most Group Health adult patients have BP measurements in the EMR, and these could be used to refine recruitment strategies.
We also did not control for the greater attention BPM-Web-Pharm patients received; BPM-Web patients might have had similar reductions in BP if we had emailed them reminders to send BP measurements to their physician. We also do not know whether BP control will be maintained after the end of pharmacy support. Additionally, the health plan’s characteristics may have influenced results. Patients in this study received care in a large integrated group practice, where Group Health was both the insurance plan and the health care delivery system. Group Health medical centers were paperless; orders, laboratory test results, medications, and patient encounter notes were part of the EMR and already used clinical pharmacists for ”team-based” care management. Patients had prescription drug coverage and received medications for a co-payment from Group Health pharmacies. Independent group practices or those in an insurance plan network might have greater difficulties in providing these integrated services.
Strengths
To our knowledge, this is the first large randomized controlled trial to test the use of care management over the Web, including a pre-existing EMR shared between patients and providers and additional Web services, to improve chronic disease treatment outcomes. Use of patient websites is consistent with the Institute of Medicine Crossing the Quality Chasm report, which states that an essential element for the transformation of healthcare is “continuous access” (24/7) to healthcare.43
To our knowledge, this is also the first randomized controlled trial that has applied the Chronic Care Model to the care of hypertension. Systematic reviews have shown that use of this model can lead to improved health outcomes for other chronic conditions.44,45 Uncertainty persists regarding how best to deliver this model and whether all six domains are required.
In the e-BP study, a low intensity, self-care management intervention that did not include ongoing and planned care management support led to some increases in Web communications and number of classes of antihypertensive medications used, and a modest reduction in systolic BP. Adding pharmacy care allowed the Chronic Care Model to be integrated, with further increases in secure messaging, more antihypertensive medication classes being added, and larger reductions in both systolic and diastolic BP. We believe the pharmacists were successful because they provided planned care to a defined population, consistently applied stepped medication protocols, and used comprehensive information systems, a patient shared EMR, and Web communications to collaborate with patients and their physicians.
CONCLUSION
Our findings demonstrate the effectiveness of using home BP monitoring combined with pharmacy care over the Web to improve BP control for patients with essential hypertension. More studies are needed to determine whether similar care can be applied to other chronic diseases, be implemented in other settings, and decrease costs.
Acknowledgment
We wish to thank other people who have made significant contributions, including: Rebecca Hughes, BA (manuscript preparation and editing); Melissa Rabelhofer, BA (manuscript preparation and administrative support); Danette Feuling, RPH, Shannon Jewell, PharmD, and Jilene Winther, PharmD (clinical pharmacists); and Ted Eytan MD, MPH (study design and informatics support). We also specifically acknowledge Harold Goldberg, MD, MPH, deceased, for his role in the study design, study team participation, and mentorship of Drs. Green and Ralston
Funding/Support: This research was funded by a grant from the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH): Grant R01-HL075263; Electronic Communications and Blood Pressure Monitoring (e-BP).
Role of the Sponsor: The funding agency had no role in the study design, analysis, or interpretation of data; decision regarding publication; or preparation of this article.
Footnotes
Trial Registration www.clinicaltrials.gov or http://isrctn.org Identifier: NCT00158639
Financial Disclosures: Dr. Ralston has received grant funding from Sanofi Aventis. No other authors disclosed any financial interests.
References
- 1.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.Fields LE, Burt VL, Cutler JA, Hughes J, Roccella EJ, Sorlie P. The burden of adult hypertension in the United States 1999 to 2000: a rising tide. Hypertension. 2004;44(4):398–404. doi: 10.1161/01.HYP.0000142248.54761.56. [DOI] [PubMed] [Google Scholar]
- 3.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 4.Wang TJ, Vasan RS. Epidemiology of uncontrolled hypertension in the United States. Circulation. 2005;112(11):1651–1662. doi: 10.1161/CIRCULATIONAHA.104.490599. [DOI] [PubMed] [Google Scholar]
- 5.Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294(4):466–472. doi: 10.1001/jama.294.4.466. [DOI] [PubMed] [Google Scholar]
- 6.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290(2):199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 7.Walsh JM, McDonald KM, Shojania KG, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44(7):646–657. doi: 10.1097/01.mlr.0000220260.30768.32. [DOI] [PubMed] [Google Scholar]
- 8.Walsh JM, Sundaram V, McDonald K, Owens DK, Goldstein MK. Implementing effective hypertension quality improvement strategies: barriers and potential solutions. J Clin Hypertens (Greenwich) 2008;10(4):311–316. doi: 10.1111/j.1751-7176.2008.07425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pew Internet & American Life Project. [Accessed February 26, 2007];Demographics of Internet Users. 2006 December; http://www.pewinternet.org/trends/User_Demo_1.11.07.htm.
- 10.Adler KG. Web portals in primary care: an evaluation of patient readiness and willingness to pay for online services. J Med Internet Res. 2006;8(4):e26. doi: 10.2196/jmir.8.4.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Staessen JA, O'Brien ET, Thijs L, Fagard RH. Modern approaches to blood pressure measurement. Occup Environ Med. 2000–2000;57(8):510–520. doi: 10.1136/oem.57.8.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Green BB, Kaplan RC, Psaty BM. How do minor changes in the definition of blood pressure control affect the reported success of hypertension treatment? Am J Manag Care. 2003–2003;9(3):219–224. [PubMed] [Google Scholar]
- 13.Little P, Barnett J, Barnsley L, Marjoram J, Fitzgerald-Barron A, Mant D. Comparison of agreement between different measures of blood pressure in primary care and daytime ambulatory blood pressure. BMJ. 2002;325(7358):254–257. doi: 10.1136/bmj.325.7358.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosner B, Polk BF. The implications of blood pressure variability for clinical and screening purposes. J Chronic Dis. 1979;32(6):451–461. doi: 10.1016/0021-9681(79)90105-x. [DOI] [PubMed] [Google Scholar]
- 15.Baguet JP, Mallion JM. Self-monitoring of blood pressure should be used in clinical trials. Blood Press Monit. 2002–2002;7(1):55–59. doi: 10.1097/00126097-200202000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Green BB, Ralston JD, Fishman PA, et al. Electronic Communications and Home Blood Pressure Monitoring (e-BP) study: Design, delivery, and evaluation framework. Contemp Clin Trials. 2008;29(3):376–395. doi: 10.1016/j.cct.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wagner EH, Austin BT, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4(2):12–25. [PubMed] [Google Scholar]
- 18.Ralston JD, Carrell D, Reid R, Anderson M, Moran M, Hereford J. Patient web services integrated with a shared medical record: patient use and satisfaction. J Am Med Inform Assoc. 2007;14(6):798–806. doi: 10.1197/jamia.M2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coleman A, Freeman P, Steel S, Shennan A. Validation of the Omron 705IT (HEM-759-E) oscillometric blood pressure monitoring device according to the British Hypertension Society protocol. Blood Press Monit. 2006;11(1):27–32. doi: 10.1097/01.mbp.0000189788.05736.5f. [DOI] [PubMed] [Google Scholar]
- 20.O'Brien E, Waeber B, Parati G, Staessen J, Myers MG. Blood pressure measuring devices: recommendations of the European Society of Hypertension. BMJ. 2001;322(7285):531–536. doi: 10.1136/bmj.322.7285.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Verberk WJ, Kroon AA, Kessels AG, de Leeuw PW. Home blood pressure measurement: a systematic review. J Am Coll Cardiol. 2005;46(5):743–751. doi: 10.1016/j.jacc.2005.05.058. [DOI] [PubMed] [Google Scholar]
- 22.Farivar SS, Cunningham WE, Hays RD. Correlated physical and mental health summary scores for the SF-36 and SF-12 Health Survey, V.I. Health Qual Life Outcomes. 2007;5:54. doi: 10.1186/1477-7525-5-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cote I, Gregoire JP, Moisan J, Chabot I. Quality of life in hypertension: the SF-12 compared to the SF-36. Can J Clin Pharmacol. 2004;11(2):e232–e238. [PubMed] [Google Scholar]
- 24.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63(1):60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 25.Consumer Assessment of Healthcare Providers and Systems. [Accessed March 5, 2008];CAHPS health plan survey 4.0. https://www.cahps.ahrq.gov/cahpskit/files/1151a_engadultcom_40.doc.
- 26.Carrell D, Ralston J. Messages, strands, and threads: measuring electronic patient-provider messaging; Proceeding of the American Informatics Association Annual Session; Washington, D.C. [PMC free article] [PubMed] [Google Scholar]
- 27.Fienberg S. The analysis of cross-classified data. Cambridge, MA: MIT Press; 1980. [Google Scholar]
- 28.Seber GAF. Linear Regression Analysis. New York: John Wiley and Sons; 2007. [Google Scholar]
- 29.Searle S. Linear Models. New York: John Wiley & Sons, Inc; 1971. [Google Scholar]
- 30.Levin J, Serlin R, Seaman MA. A controlled, powerful multiple-comparison strategy for several situations. Psychological Bulletin. 1994;115:153–159. [Google Scholar]
- 31.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 32.Piegorsch WW. Multiple comparisons for analyzing dichotomous response. Biometrics. 1991;47(1):45–52. [PubMed] [Google Scholar]
- 33.R Development Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2007. [Google Scholar]
- 34.Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ. 1999;319(7211):670–674. doi: 10.1136/bmj.319.7211.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mancia G, Bombelli M, Lanzarotti A, et al. Systolic vs diastolic blood pressure control in the hypertensive patients of the PAMELA population. Pressioni Arteriose Monitorate E Loro Associazioni. Arch Intern Med. 2002;162(5):582–586. doi: 10.1001/archinte.162.5.582. [DOI] [PubMed] [Google Scholar]
- 36.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002–2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 37.Greenfield S, Kaplan S, Ware JE., Jr Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med. 1985;102(4):520–528. doi: 10.7326/0003-4819-102-4-520. [DOI] [PubMed] [Google Scholar]
- 38.Greenfield S, Kaplan SH, Ware JE, Jr, Yano EM, Frank HJ. Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3(5):448–457. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 39.Fahey T, Schroeder K, Ebrahim S. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2006;2 doi: 10.1002/14651858.CD005182.pub2. CD005182. [DOI] [PubMed] [Google Scholar]
- 40.Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ. 2004–2004;329(7458):145. doi: 10.1136/bmj.38121.684410.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McNeill LH, Puleo E, Bennett GG, Emmons KM. Exploring social contextual correlates of computer ownership and frequency of use among urban, low-income, public housing adult residents. J Med Internet Res. 2007;9(4):e35. doi: 10.2196/jmir.9.4.e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.National Committee for Quality Assurance, The state of health care quality 2007. Washington, D.C: National Committee for Quality Assurance; 2007. [Google Scholar]
- 43.Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press; 2001. Committee on Quality Health Care in America IoM. [PubMed] [Google Scholar]
- 44.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 45.Tsai AC, Morton SC, Mangione CM, Keeler EB. A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care. 2005;11(8):478–488. [PMC free article] [PubMed] [Google Scholar]