Abstract
Acute appendicitis is a common surgical condition that is usually managed with early surgery, and is associated with low morbidity and mortality. However, some patients may have atypical symptoms and physical findings that may lead to a delay in diagnosis and increased complications. Atypical presentation may be related to the position of the appendix. Ascending retrocecal appendicitis presenting with right upper abdominal pain may be clinically indistinguishable from acute pathology in the gallbladder, liver, biliary tree, right kidney and right urinary tract. We report a series of four patients with retrocecal appendicitis who presented with acute right upper abdominal pain. The clinical diagnoses at presentation were acute cholecystitis in two patients, pyelonephritis in one, and ureteric colic in one. Ultrasound examination of the abdomen at presentation showed subhepatic collections in two patients and normal findings in the other two. Computed tomography (CT) identified correctly retrocecal appendicitis and inflammation in the retroperitoneum in all cases. In addition, abscesses in the retrocecal space (n = 2) and subhepatic collections (n = 2) were also demonstrated. Emergency appendectomy was performed in two patients, interval appendectomy in one, and hemicolectomy in another. Surgical findings confirmed the presence of appendicitis and its retroperitoneal extensions. Our case series illustrates the usefulness of CT in diagnosing ascending retrocecal appendicitis and its extension, and excluding other inflammatory conditions that mimic appendicitis.
Keywords: Retrocecal appendicitis, Upper abdominal pain, Computed tomography
INTRODUCTION
The vermiform appendix may occupy several positions in relation to the cecum. The most common positions are descending intraperitoneal (31%-74%) and retrocecal (26%-65%)[1,2]. The location and spread of inflammation from acute appendicitis depends on the location of the appendix. If the appendix is located retrocecally, it may give rise to an abscess in the pararenal space and spread to bare area of the liver[3], or it may spread along the right paracolic gutter, and extend to the right posterior subhepatic and right subphrenic spaces[4]. More than half of the patients with ascending retrocecal appendicitis may have an atypical clinical presentation[5]. We present a case series of ascending retrocecal appendicitis with atypical clinical presentation, and highlight the utility of computed tomography (CT) in diagnosing the condition.
CASE REPORT
During the period January 2003 to December 2006, a computerized search for patients with surgically confirmed retrocecal appendicitis was made. Patients with retrocecal appendicitis and preoperative CT were selected. There were four patients who had atypical clinical presentation with right upper abdominal pain, who formed the study group. The hospital records were reviewed for clinical features, laboratory investigations, surgical findings and follow-up. Preoperative ultrasound and CT were reviewed.
Case 1
A 30-year-old woman presented with a 3-d history of right hypochondrial pain that was constant and radiated to the back. There was right hypochondrial tenderness with negative Murphy’s sign and renal punch. She had leukocytosis (13 200 cells/μL). A clinical diagnosis of acute cholecystitis was made. Ultrasound showed a normal liver and gallbladder with no significant abnormality. She was treated initially with antibiotics. A CT scan performed 2 d after presentation showed an inflamed appendix with inflammatory changes in the retrocecal and subhepatic regions (Figure 1). Open appendectomy revealed a moderately inflamed retrocecal appendix with no perforation. Postoperative recovery was uneventful.
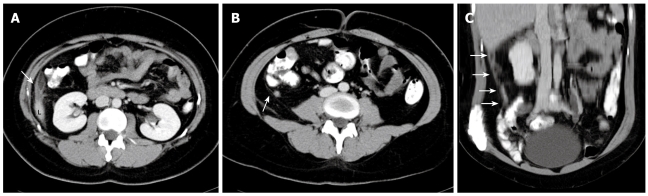
Figure 1.
A 30-year-old woman presenting with a clinical diagnosis of acute cholecystitis. A and B: Contrast-enhanced computed tomography (CT) sections showing inflammatory changes (arrow) adjacent to the inferior tip of the liver (L); B: Thickened appendix (arrow) with mild inflammatory changes in the retrocecal region; C: Coronal reconstruction showing the extent of inflammatory changes (arrows) from the retrocecal region to the tip of the liver.
Case 2
A 31-year-old woman presented with a 2-d history of right hypochondrial pain that radiated to the back and right shoulder tip, fever with chills, and vomiting. She also complained of foul-smelling urine and vaginal discharge. She had a termination of pregnancy 4 d earlier. The pain was increasing in severity and aggravated by movement and coughing. She was febrile with right hypochondrial rebound tenderness and a positive right renal punch. She had leukocytosis (14 080 cells/μL). The clinical impression was pelvic inflammatory disease with pyelonephritis and hepatobiliary sepsis. Focused assessment with sonography for trauma (FAST) showed no fluid collection in Morrison’s pouch, and pelvic ultrasound did not show any collections. CT (Figure 2) at 3 d after admission showed loculated collections adjacent to segment 6 of the liver. A long inflamed retrocecal appendix was seen with surrounding inflammation that extended to involve the hepatic flexure and anterior pararenal space. There was also consolidation of the right lung base. At surgery, there was retrocecal appendicitis with perforation that caused a subhepatic collection. The patient made a good recovery.
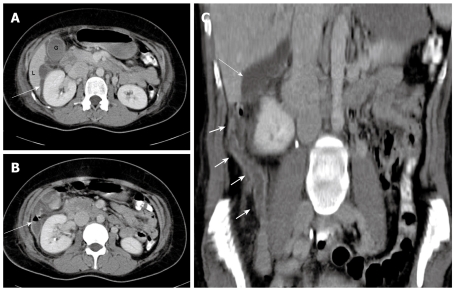
Figure 2.
A 31-year-old woman presenting with right hypochondrial pain and a clinical diagnosis of pelvic inflammatory disease and right pyelonephritis. A: Contrast-enhanced CT scan showing fluid collection (arrow) in the subhepatic region, extending anteriorly to the gallbladder fossa with inflammatory stranding; B: Note the air fluid level in the collection adjacent to the right kidney; C: Coronal reconstruction showing the long thickened and inflamed appendix (short arrows) reaching the subhepatic region, and the subhepatic collection (arrow) is seen extending more cranially.
Case 3
A 34-year-old man presented with right flank pain of 6 d duration. The pain was colicky and radiated to the back. There was no history of dysuria or urinary frequency, but he also had nausea and vomiting with loss of appetite for 2 d. He had leukocytosis (13 620 cells/μL). The abdomen was soft but the right renal punch was positive. The clinical impression was of right-sided ureteric colic and urinary tract infection. Ultrasound showed no urinary calculi but there was a subhepatic collection (Figure 3) with hyperechoic areas that were suggestive of an abscess. CT (Figure 3) performed on the next day showed the appendix to be swollen and inflamed. There were collections in the subhepatic, rectovesical and paravesical regions. Surgery on the same day confirmed an inflamed and perforated retrocecal appendix with extensive retrocecal collections and abscesses, and a hemicolectomy was performed. The patient recovered uneventfully.
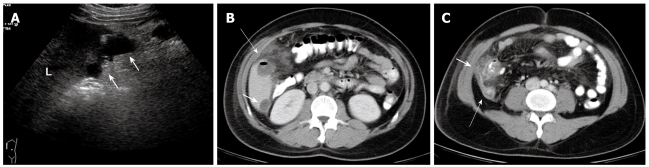
Figure 3.
A 34-year-old man with colicky right flank pain and clinical diagnosis of right ureteric colic. A: Ultrasound showed a subhepatic fluid collection (arrows) and no other significant abnormality; B: CT scan performed 2 d later showed the collection in the subhepatic region (short arrow). Note the air-fluid level in the anterior collection (long arrow) with inflammatory changes; C: The section at the level of the cecum and appendix shows inflammatory changes in the retrocecal region (short arrow) and thickened appendix (long arrow).
Case 4
A 27-year-old man presented with fever and right hypochondrial pain for 1 d. There was tenderness in the right hypochondrium. He was treated nonsurgically for acute cholecystitis but defaulted from treatment and follow-up. He presented again 2 mo later with fever, vomiting and right hypochondrial pain of 2 d duration. There was tenderness in the right hypochondrium with a positive right renal punch. The total white cell count was elevated at 24 700 cells/μL but liver function tests were normal. Ultrasound showed two abscesses in the right hepatic lobe and a thickened gallbladder wall, but no gallstones were seen. He was treated for liver abscesses with intravenous antibiotics and made an excellent recovery. Follow-up ultrasound scans showed resolution of the liver abscesses.
Four months later, he presented again with fever and right hypochondrial pain. Ultrasound showed no significant abnormality. He was treated with a further course of intravenous antibiotics and discharged. He was readmitted 5 mo later. CT showed subphrenic and subhepatic collections with a thickened inflamed appendix (Figure 4). In view of the recurrent collections, diverticulitis was suspected. Colonoscopy was normal and he was managed conservatively. Follow-up CT 3 mo later showed resolution of the collection, but the appendix was still thickened with periappendiceal inflammatory changes. Elective laparoscopic appendectomy was then performed. This showed a high retrocecal appendix with dense adhesions between the appendix and the liver. A final diagnosis of recurrent retrocecal appendicitis was made. The patient made a good recovery with no further episodes.
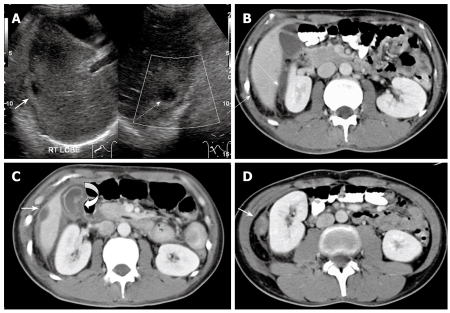
Figure 4.
A 27-year-old man with recurrent right upper abdominal pain. A: Ultrasound showed a hypoechoic area in the subphrenic (straight arrow) and subhepatic (broken arrow) region; B: Confirmation by contrast-enhanced CT; C: CT also showed a thickened gallbladder wall (curved arrow), subhepatic collection (white arrow) and inflammation in the perinephric region; D: Another caudal section shows a thickened appendix with inflammatory stranding in the perinephric region.
DISCUSSION
Acute appendicitis may be diagnosed easily and treated in children and adults if there is a classical history with typical clinical signs[5]. When the appendix is in the retrocecal position, the signs and symptoms of acute appendicitis may be atypical and mimic pathology in the right flank and hypochondrium, such as acute cholecystitis, diverticulitis, acute gastroenteritis, ureter colic, acute pyelonephritis, colon cancer and irritable bowel syndrome[6].
When the clinical impression is of gallbladder, hepatobiliary or urinary tract pathology, ultrasound is often performed. This may show liver abscesses and collections in the subhepatic and right flank regions. Although ultrasound is used frequently in the assessment of suspected acute appendicitis in young children, it requires expertise and dedicated techniques, such as graded compression. The appendix could be visualized in up to 99% of suspected cases of appendicitis in children in one series[7]. However, in adults, un-enhanced CT has been shown to be more sensitive in diagnosing acute appendicitis than ultrasound is[8]. In our series, acute appendicitis was not suspected in any of the patients, therefore, the ultrasound scan performed was not dedicated to rule out appendicitis.
CT is very sensitive for evaluating the appendix, and a thickened appendix, inflamed periappendiceal fat, collections, and presence of free gas in ruptured appendix are detected readily by CT. The inflammatory changes that result from an acutely inflamed ascending retrocecal appendix may extend to the perirenal, adrenal and subhepatic regions, and on rare occasions, inferior extension along the psoas muscle into the thigh has been reported[9,10]. The inflammatory changes are seen most commonly in the retrocolic space (88%), followed by paracolic gutter (30%), pararenal space (27%), mesentery (24%), perirenal space (18%), and less often, in the subhepatic space (3%)[6]. In a recently published series of 33 patients[6] with ascending retrocecal appendicitis who were investigated with CT, only one was found to have a subhepatic collection.
It is interesting that all four of our cases involve young adult patients rather than children. A retrocecal appendix is common and one series showed the appendix to be retrocolic and retrocecal in 58% of cases[1]. A retrocecal appendix has been described also in families and is thought to be inherited as a simple dominant unit character[11]. Studies of the fetal appendix, however, show that it is almost always subcycle during this period[12]. It is possible therefore that the appendix continues to grow during childhood, extending further from the cecum later in life, although there have been no published studies documenting this process. Therefore, retrocecal appendicitis with symptoms remote from the right iliac fossa may occur also in an older age group.
Our case series illustrated a spectrum of uncommon clinical and radiological manifestations of ascending retrocecal appendicitis. This emphasizes the importance of considering the possibility of ascending retrocecal appendicitis in cases in which the signs and symptoms are referred to areas along the possible location of a retrocecal appendix, especially when initial investigations like ultrasound do not support other diagnoses, such as cholecystitis, or hepatobiliary or urinary tract pathology. CT is helpful to establish rapidly the correct diagnosis, as delays in appendectomy for over 24-36 h have been shown to increase the complication rate[13,14].
In summary, CT is useful for evaluation of patients with atypical right upper abdominal pain and nonspecific clinical findings, to rule out the possibility of retrocecal appendicitis.
Peer reviewer: Dr. Andreas G Schreyer, Department of Radiology, University Hospital Regensburg, Franz-Josef-Strauss-Allee 11, Regensburg 93053, Germany
S- Editor Li LF L- Editor Kerr C E- Editor Ma WH
References
- 1.Collins DC. Acute retrocecal appendicitis: based on seven hundred and fifty-one instances. Arch Surg. 1938;36:729–743. [Google Scholar]
- 2.Wakeley CP. The Position of the Vermiform Appendix as Ascertained by an Analysis of 10,000 Cases. J Anat. 1933;67:277–283. [PMC free article] [PubMed] [Google Scholar]
- 3.Meyers MA, Oliphant M. Ascending retrocecal appendicitis. Radiology. 1974;110:295–299. doi: 10.1148/110.2.295. [DOI] [PubMed] [Google Scholar]
- 4.Feldberg MA, Hendriks MJ, van Waes PF. Computed tomography in complicated acute appendicitis. Gastrointest Radiol. 1985;10:289–295. doi: 10.1007/BF01893114. [DOI] [PubMed] [Google Scholar]
- 5.Lee SL, Ho HS. Acute appendicitis: is there a difference between children and adults? Am Surg. 2006;72:409–413. doi: 10.1177/000313480607200509. [DOI] [PubMed] [Google Scholar]
- 6.Kim S, Lim HK, Lee JY, Lee J, Kim MJ, Lee AS. Ascending retrocecal appendicitis: clinical and computed tomographic findings. J Comput Assist Tomogr. 2006;30:772–776. doi: 10.1097/01.rct.0000228151.73528.8f. [DOI] [PubMed] [Google Scholar]
- 7.Lee JH, Jeong YK, Park KB, Park JK, Jeong AK, Hwang JC. Operator-dependent techniques for graded compression sonography to detect the appendix and diagnose acute appendicitis. AJR Am J Roentgenol. 2005;184:91–97. doi: 10.2214/ajr.184.1.01840091. [DOI] [PubMed] [Google Scholar]
- 8.Gamanagatti S, Vashisht S, Kapoor A, Chumber S, Bal S. Comparison of graded compression ultrasonography and unenhanced spiral computed tomography in the diagnosis of acute appendicitis. Singapore Med J. 2007;48:80–87. [PubMed] [Google Scholar]
- 9.Dimofte G, Dubei L, Lozneanu LG, Ursulescu C, Grigora Scedil M. Right adrenal abscess -- an unusual complication of acute apendicitis. Rom J Gastroenterol. 2004;13:241–244. [PubMed] [Google Scholar]
- 10.Hsieh CH, Wang YC, Yang HR, Chung PK, Jeng LB, Chen RJ. Extensive retroperitoneal and right thigh abscess in a patient with ruptured retrocecal appendicitis: an extremely fulminant form of a common disease. World J Gastroenterol. 2006;12:496–499. doi: 10.3748/wjg.v12.i3.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shperber Y, Halevy A, Oland J, Orda R. Familial retrocaecal appendicitis. J R Soc Med. 1986;79:405–406. doi: 10.1177/014107688607900708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malas MA, Sulak O, Gokcimen A, Sari A. Development of the vermiform appendix during the fetal period. Surg Radiol Anat. 2004;26:202–207. doi: 10.1007/s00276-003-0208-9. [DOI] [PubMed] [Google Scholar]
- 13.Omundsen M, Dennett E. Delay to appendicectomy and associated morbidity: a retrospective review. ANZ J Surg. 2006;76:153–155. doi: 10.1111/j.1445-2197.2006.03673.x. [DOI] [PubMed] [Google Scholar]
- 14.Bickell NA, Aufses AH Jr, Rojas M, Bodian C. How time affects the risk of rupture in appendicitis. J Am Coll Surg. 2006;202:401–406. doi: 10.1016/j.jamcollsurg.2005.11.016. [DOI] [PubMed] [Google Scholar]