Abstract
OBJECTIVE
The objective of this article is to provide a practical review of the incremental benefit of MRI in the assessment of adnexal masses in pregnancy.
CONCLUSION
MRI can assist sonographic assessment of adnexal masses in pregnancy by depicting the characteristic findings of exophytic leiomyoma, red degeneration of leiomyoma, endometrioma, decidualized endometrioma, and massive ovarian edema. Accordingly, MRI should be considered as a useful adjunct when sonography is inconclusive or insufficient to guide management of adnexal masses discovered in pregnancy.
Keywords: adnexal mass, fetal imaging, MRI, obstetrics, women’s imaging
A pathologic adnexal mass is found in 1–2% of pregnancies [1] (by definition, the physiologic corpusluteum cyst of early pregnancy is excluded). The relative frequency of the more common diagnoses encountered is illustrated by a sonographic series of 131 adnexal masses seen after 12 weeks of gestation in which 38% were functional cysts; 32%, dermoid cysts; 12%, benign cystic tumors; and 11%, endometriomas [1].
Only 1–3% of adnexal masses are malignant, but even benign masses can cause symptoms or obstetric complications. Sonography is the primary method of detection and evaluation, but findings may be nonspecific and then MRI may assist characterization [2]. The use of MRI in pregnancy has expanded because of improvements in rapid breath-hold sequences and because better imaging helps avoid the potential hazards of surgery during gestation. This pictorial essay aims to provide a practical review of the incremental benefit of MRI in the assessment of adnexal masses in pregnancy and consists of a description of MRI technique during pregnancy accompanied by a review of MRI findings of these masses categorized as mimics, nonneoplastic, and neoplastic.
Technique
Standard MRI safety screening should be performed. The patient should fast for 4 hours to reduce bowel peristalsis artifact and prevent postprandial fetal motion and should empty her bladder immediately before scanning. Written consent is not mandatory, although arguably it is advisable to explain to the patient the negligible nature of the risks posed by MRI in pregnancy [3] and document this discussion in either the chart or the radiology report. A pelvic surface coil will improve image quality, but it can be omitted if the scanner bore will not accommodate both patient and coil. Most pregnant patients can be scanned in the supine position, but left lateral decubitus positioning should be considered during later gestation to avoid caval compression by the gravid uterus.
After a localizer is acquired, rapid T1- and T2-weighted imaging, which will eliminate respiratory motion artifact and minimize fetal motion artifact, can be performed during a maternal breath-hold with multislice spoiled gradient-echo and single-shot RARE sequences, respectively. Axial images are usually adequate for T1-weighted evaluation. T1-weighted images with frequency-selective fat saturation should be obtained if an adnexal mass is of high T1 signal intensity, because this sequence can distinguish fat from blood.
Axial, sagittal, and coronal images are often helpful for T2-weighted assessment. Slower breathing-averaged RARE T2-weighted sequences may provide greater spatial and contrast resolution than T1-weighted sequences but have the disadvantages of longer imaging times and potential for greater motion artifact. TR and TE values used locally for nonpregnant patients can be used in pregnant patients to produce appropriately T1- and T2-weighted images. Slice thickness and matrix can be adjusted to optimize coverage and resolution while remaining within the breath-hold capacity of the patient. Typically, slice thickness would be 5–8 mm with an interslice gap of 0–1 mm and a matrix of 256 × 128–256.
Gadolinium is teratogenic in animal studies and crosses the placenta where it is presumably excreted by the fetal kidneys into the amniotic fluid. In the era of nephrogenic systemic fibrosis, this characteristic of gadolinium raises theoretic concerns of toxicity related to disassociation and persistence of free gadolinium. Gadolinium is classified as a category C drug by the U.S. Food and Drug Administration (FDA) and can be used if considered critical—that is, to be administered only “if the potential benefit justifies the potential risk to the fetus.” More stable macrocyclic agents (e.g., gadoteridol or gadobutrol) may be preferable to gadolinium [4]. In reality, contrast administration for adnexal masses is used primarily to assess for the presence of solid components in a cystic mass and is used to a lesser extent to evaluate nonenhancement in a torsed mass. Such information can generally be derived from gray-scale and Doppler sonography; thus, it is unlikely that IV gadolinium would be considered critical for MRI of an adnexal mass in pregnancy.
Mimics of Adnexal Masses
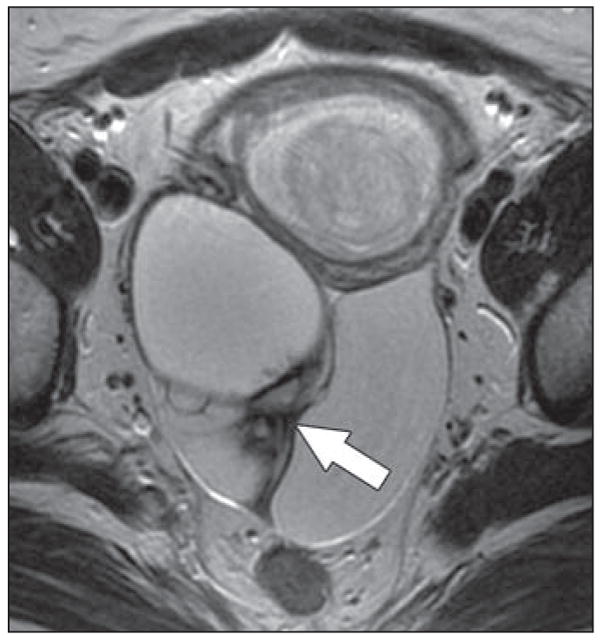
This category consists of masses that do not arise primarily from the ovaries or fallopian tubes and includes exophytic uterine leiomyoma and ectopic pregnancy. Exophytic leiomyomas are a common cause of an apparent adnexal mass at sonography. MRI is superior to sonography in differentiating leiomyomas from other masses [5], and the correct diagnosis is suggested when a well-circumscribed lesion with low-T2-signal-intensity solid components is seen to have a beak- or claw-shaped interface with the uterus (Fig. 1). Bridging vessels between the uterus and an apparent adnexal mass are also a useful sign of an exophytic leiomyoma. Occasionally during pregnancy, leiomyomas undergo spontaneous hemorrhagic infarction, known as “red degeneration,” or growth and can present with acute pain. There are no specific sonographic features of leiomyoma, but MRI characteristically shows a leiomyoma with uniform or peripheral high T1 signal intensity [6] (Fig. 2).
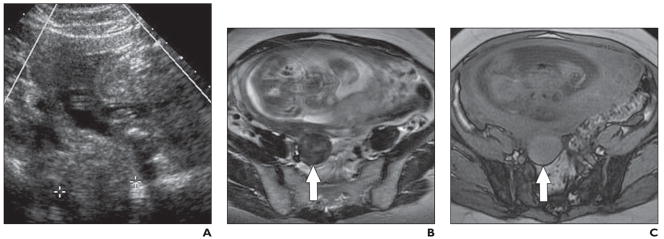
Fig. 1. 36-year-old pregnant woman who presented for routine early pregnancy sonography.
A, Routine early pregnancy transabdominal sonogram obtained at 7 weeks’ gestation shows solid mass (arrow) of indeterminate origin and nature in pelvis posterior to uterus (UT).
B, Sagittal single-shot RARE T2-weighted image shows large mixed solid and cystic pelvic mass inferoposterior to gravid uterus. Note that solid parts (arrow) of mass are of low T2 signal intensity.
C, Axial RARE T2-weighted image with fat saturation shows mass has beak- or clawlike interface with myometrium (arrows), consistent with uterine origin. Overall findings are those of cystic degeneration in exophytic uterine leiomyoma.
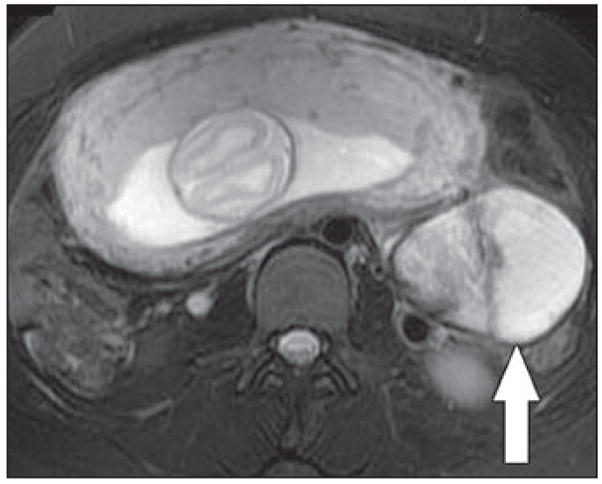
Fig. 2. 34-year-old pregnant woman who presented with lower abdominal pain.
A, Transvaginal sonogram obtained at 25 weeks’ gestation shows solid 3.8-cm mass (between calipers) thought to be of right adnexal origin.
B, Axial RARE T2-weighted image shows mass (arrow) arises from uterus and is of low T2 signal intensity; also, note “claw sign,” similar to Figure 1. Findings are those of exophytic uterine leiomyoma.
C, Axial spoiled gradient-echo T1-weighted MR image shows exophytic uterine leiomyoma (arrow) is of increased T1 signal intensity; this finding indicates red degeneration (i.e., spontaneous hemorrhagic infarction).
Ectopic pregnancy is usually diagnosed clinically and sonographically. MRI serves as an adjunct when sonography is occasionally limited by inadequate soft-tissue contrast, resolution, or field of view. The key MRI feature of ectopic pregnancy is a gestational sac that is outside the uterus [7] (Fig. 3), generally in the absence of an intrauterine pregnancy. The ectopic gestational sac typically appears as a cystic saclike structure that is frequently associated with surrounding acute hematoma of distinct low intensity on T2-weighted images.
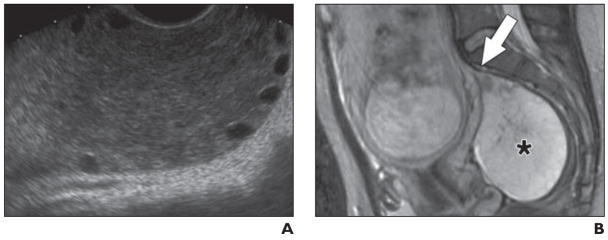
Fig. 3.
Sagittal single-shot RARE T2-weighted image in 29-year-old woman with ectopic pregnancy at 22 weeks’ gestation shows fetus in extrauterine location. Empty endometrial cavity (arrow) is seen anterior to large leiomyoma (Fibroid).
Nonneoplastic Adnexal Masses
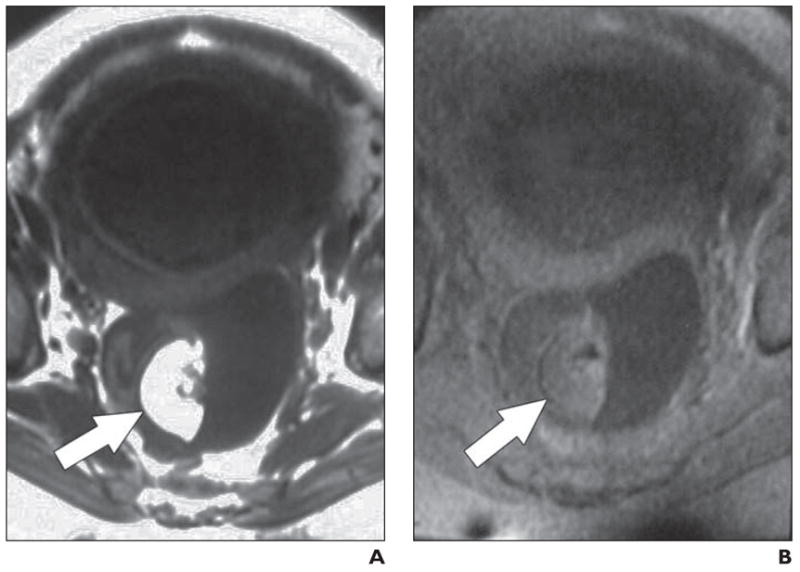
This category includes hemorrhagic cyst, endometrioma, theca lutein cyst (hyperreactio luteinalis), tuboovarian abscess, and massive ovarian edema. Hemorrhagic cysts may have a variable course and sonographic appearance, including internal heterogeneity, thickened rim, septations, and solid components thought to represent clot [8]. Although high T1 signal may suggest the diagnosis of hemorrhagic cyst, MRI may also be inconclusive in these difficult cases (Fig. 4).
Fig. 4.
Axial RARE T2-weighted image with fat saturation obtained at 24 weeks’ gestation in 29-year-old woman shows complex mixed solid and cystic left adnexal mass (arrow). No increased signal was seen on T1-weighted images (not shown). MRI appearances are nonspecific, although diagnostic considerations include cystic malignancy. Mass was resected and found to be benign hemorrhagic cyst.
On MRI, endometriomas are somewhat thick-walled cystic structures of characteristically high T1 and variably reduced T2 signal intensity (the latter is known as “T2 shading”). High T1 signal intensity is due to blood products and does not suppress with fat saturation [6] (Fig. 5). Solid components within an endometrioma can be due to the rare complication of malignant transformation but when seen in pregnancy may reflect ectopic decidualization (i.e., ectopic occurrence of the endometrial changes that normally form the vascular decidual lining of the uterus). Decidualized endometrioma can mimic ovarian malignancy during pregnancy, but a prospective diagnosis may be possible when solid smoothly lobulated nodules with prominent internal vascularity within an endometrioma are seen on sonography from early in pregnancy, and the nodules show marked similarity in signal intensity and texture to the decidualized endometrium in the uterus at MRI [9] (Fig. 6). That is, smooth lobulation and prominent vascularity on Doppler imaging and isointensity to decidualized endometrium on MRI are features of solid nodules in an endometrioma that suggest decidualization rather than malignant transformation.
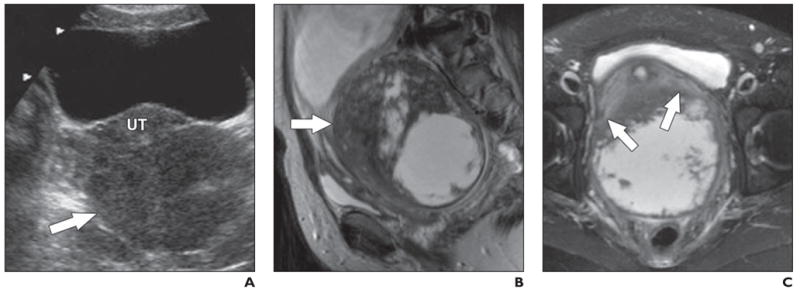
Fig. 5. 37-year-old pregnant woman.
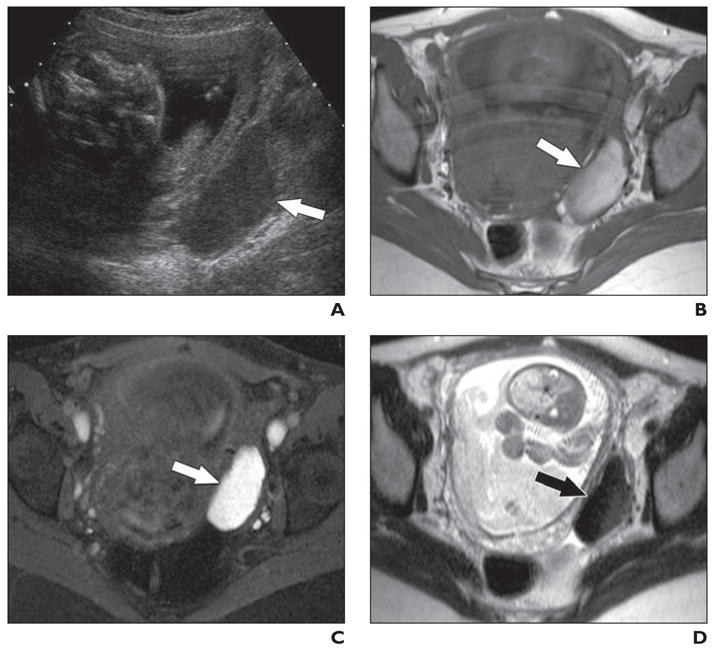
A, Transvaginal sonogram obtained at 21 weeks’ gestation shows uniformly hypoechoic left adnexal mass (arrow) of indeterminate nature.
B, Axial spin-echo T1-weighted MR image shows mass (arrow) is of increased T1 signal intensity.
C, Axial spin-echo T1-weighted MR image with fat saturation shows mass (arrow) remains of increased signal intensity, excluding macroscopic fat and suggesting blood.
D, Axial single-shot RARE T2-weighted MR image shows mass (arrow) of reduced T2 signal intensity (“T2 shading”). Overall findings are consistent with endometrioma.
Fig. 6. 34-year-old pregnant woman.
A, Axial Doppler sonography image obtained at 21 weeks’ gestation shows right adnexal mass (arrow) with smoothly lobulated mural nodules and prominent internal vascularity.
B, Axial T1-weighted spoiled gradient-echo MR image shows that fluid in cystic part of mass is of high T1 signal intensity (arrow), which is consistent with blood.
C, Axial RARE T2-weighted MR image shows solid component (white arrow) of mass is strikingly similar to decidualized endometrium (between black arrows) in uterus, both with respect to signal intensity and texture. Findings are considered consistent with decidualized endometrioma; postnatal resection confirmed diagnosis.
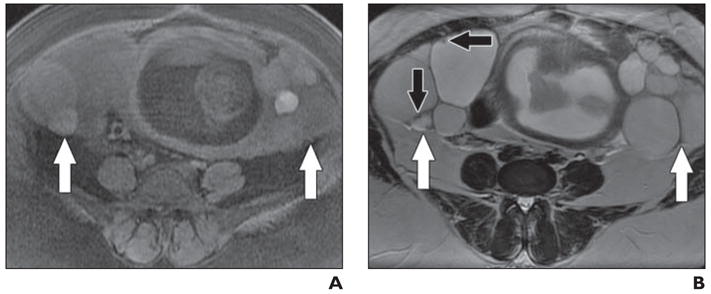
Theca lutein cysts (hyperreactio luteinalis) are rare functional ovarian masses that are due to overstimulation of the ovaries by endogenous or exogenous gonadotropins, usually in the setting of assisted fertility, gestational trophoblastic disease, or multiple gestation. Theca lutein cysts are large and have a typical multilocular cystic appearance across all imaging techniques, and there is usually little incremental benefit to MRI in diagnosis [6] (Fig. 7).
Fig. 7.
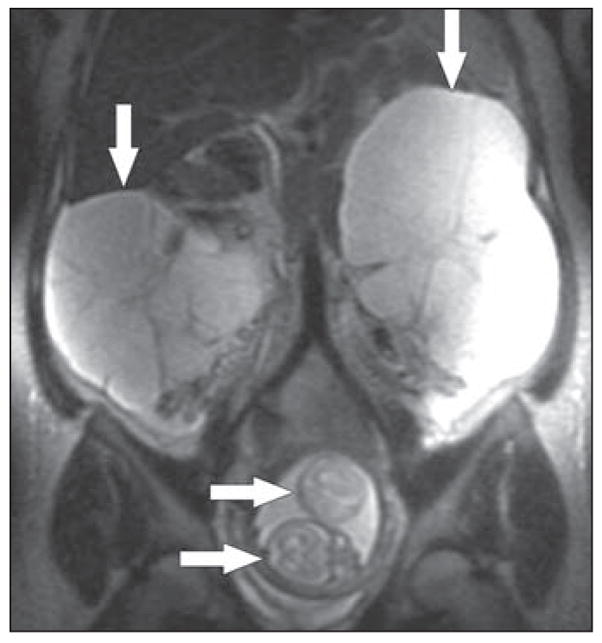
Coronal single-shot RARE T2-weighted MR image obtained at 22 weeks’ gestation in 31-year-old woman. Large bilateral multilocular adnexal masses (vertical arrows) are typical of theca lutein cysts, which in this case were associated with twin pregnancy; note two fetal heads (horizontal arrows) in uterus.
Tuboovarian abscess may complicate pregnancy, typically in patients presenting with fever, elevated WBC count, pelvic pain, and vaginal discharge. Patients with more severe symptoms or who are unresponsive to initial therapy may need to undergo imaging, and MRI is sometimes superior to transvaginal sonography for radiologic assessment [10]. An abscess appears as a thick-walled, fluid-filled mass in the adnexal region that is hypointense on T1-weighted images and hyperintense or heterogeneous on T2-weighted images. However, in practice, the workup of tuboovarian abscess usually begins with sonography and proceeds to CT if exclusion of other inflammatory or gastrointestinal abnormalities or if imaging-guided percutaneous drainage is required, so the incremental role of MRI is debatable. MRI may be helpful if sonography is inconclusive or nondiagnostic or when abscesses containing gas cannot be differentiated from gas within bowel.
Massive ovarian edema is characterized by marked enlargement of one ovary (rarely both) due to gross diffuse stromal edema that results in peripherally displaced follicles and may be due to subacute or chronic torsion without frank infarction [11]. MRI shows an enlarged ovary that is hyperintense on T2-weighted images. T2 hyperintensity may even suggest the lesion is cystic, but correlation with sonography will help avoid this pitfall (Fig. 8).
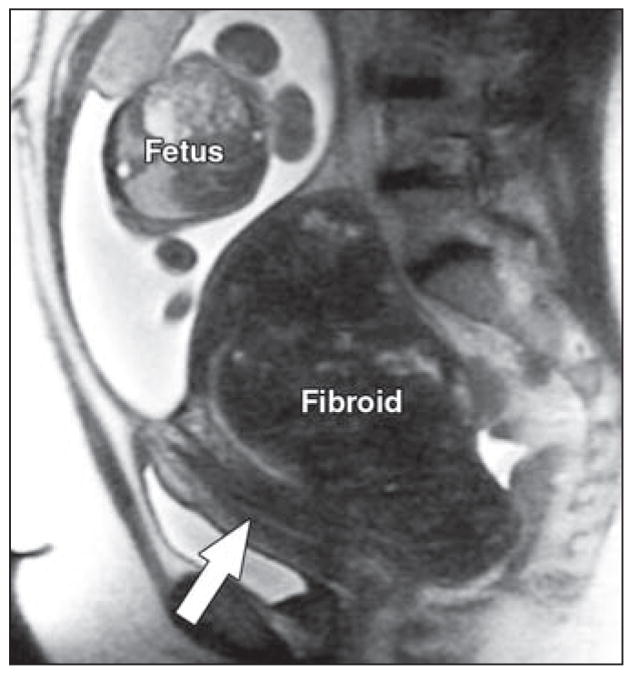
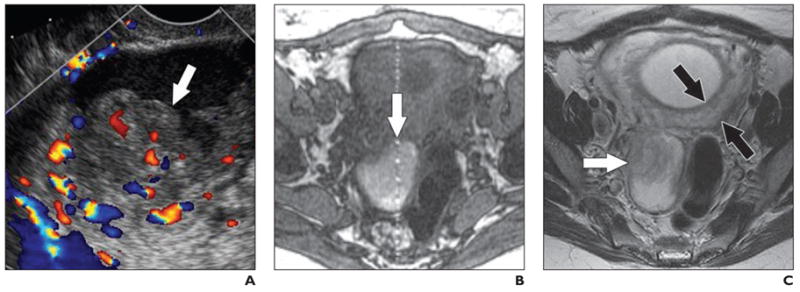
Fig. 8. 32-year-old woman with persistent right-sided pelvic pain.
A, Transvaginal sonogram obtained at 24 weeks’ gestation shows enlarged right ovary with preservation of peripheral follicles.
B, Sagittal RARE T2-weighted MR image shows right ovary (asterisk) is of markedly increased T2 signal intensity to degree that mass might be considered cystic if MRI findings had not been interpreted in conjunction with sonographic findings. Appearance is of massive ovarian edema. Cause of this condition is not well understood but may reflect chronic or subacute low-grade torsion. Beaklike pedicle (arrow) arising from superior aspect of ovary is compatible with this pathogenesis.
Neoplastic Adnexal Masses
This category includes cystadenoma, dermoid cyst, borderline tumor, primary ovarian cancer, and metastases to the ovary. Cystadenomas are typically benign-appearing cysts of variable size and MRI generally adds little to sonography (Fig. 9), although occasionally MRI may help in evaluation of the overall dimensions and site of origin of the mass by showing a displaced ovary not seen at sonography.
Fig. 9.
Axial RARE T2-weighted MR image obtained at 18 weeks’ gestation in 29-year-old woman shows large predominantly cystic right adnexal mass with somewhat thickened internal septae (arrow). Resection showed benign cystadenofibroma.
Dermoid cysts are also usually distinctive at sonography, but the diagnostic finding on MRI, if performed, is the presence of macroscopic fat (Fig. 10). It should be remembered that dermoid cysts may undergo torsion. Borderline tumors show a greater degree of complexity, with thickened walls or septae and internal solid components [6] (Fig. 11).
Fig. 10. 22-year-old pregnant woman.
A, Axial spin-echo T1-weighted MR image obtained at 24 weeks’ gestation shows adnexal mass is posterior to uterus and contains focus (arrow) of increased T1 signal intensity.
B, Axial spin-echo T1-weighted MR image with fat saturation shows that focus of increased T1 signal intensity in A is now of low signal intensity (arrow), confirming presence of macroscopic fat and indicating diagnosis of mature cystic teratoma (dermoid cyst).
Fig. 11. 24-year-old pregnant woman.
A, Axial T1-weighted spoiled gradient-echo MR image with fat saturation obtained at 25 weeks’ gestation shows bilateral cystic adnexal masses (arrows) with thick septations and stained-glass appearance due to variable signal intensity among different compartments of lesion.
B, Axial RARE T2-weighted MR image shows internal complexity in masses (white arrows) with thick septations (vertical black arrow) and solid nodules (horizontal black arrow). Findings are considered suggestive of malignancy. Resection showed bilateral mucinous cystic tumors of low malignant potential (borderline tumors).
Frank ovarian malignancies account for approximately 1% of pathologic ovarian masses in pregnancy [12] and are characterized by prominent solid components within a cystic mass, necrosis in a solid mass, or peritoneal metastases (Fig. 12). Any cystic mass should be carefully examined for mural or septal thickening or mural nodules, papillary excrescences, or other solid components because these findings may indicate malignancy. Although all these features within the primary tumor can be seen on both sonography and MRI, MRI has the advantages of depicting more distant findings, such as widespread ascites, peritoneal implants, and pelvic or retroperitoneal adenopathy, and of being more accurate overall than sonography in the distinction of benign from malignant ovarian masses [13].
Fig. 12. 34-year-old pregnant woman.
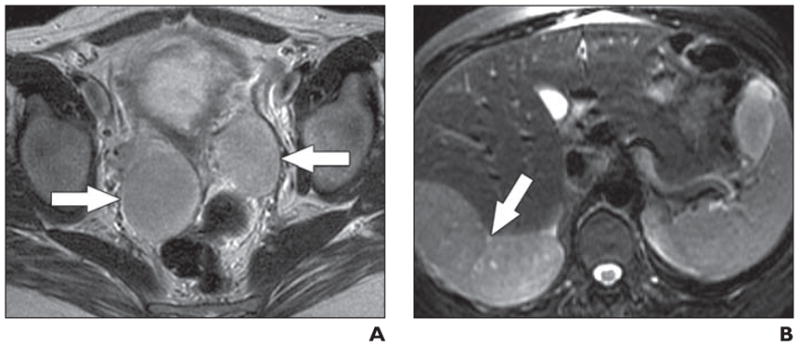
A, Axial RARE T2-weighted MR image obtained at 23 weeks’ gestation shows bilateral solid adnexal masses (arrows).
B, Axial RARE T2-weighted MR image through upper abdomen shows large tumor deposit (arrow) abutting liver. Appearances are considered indicative of malignancy. Cesarean hysterectomy and bilateral salpingo-oophorectomy were performed at 28 weeks’ gestation because of progression of subphrenic tumor with diaphragmatic irritation. Pathology results showed benign metastasizing leiomyoma. Masses spontaneously regressed after surgery and patient remains free of disease 3 years after surgery.
Conclusion
MRI can assist sonographic assessment of adnexal masses in pregnancy by showing the uterine origin and reduced T2 signal intensity of exophytic leiomyoma; the increased T1 signal intensity in red degeneration of leiomyoma; the increased T1 signal intensity of endometrioma; and the characteristic findings of dermoid cyst, decidualized endometrioma, and massive ovarian edema. The distinction and specific characterization of these different neoplastic and nonneoplastic abnormalities require close attention to lesion morphology and signal characteristics and are often aided by review of sonographic findings. Accordingly, MRI should be considered a useful adjunct when sonography is inconclusive or insufficient to guide management of adnexal masses discovered in pregnancy.
Acknowledgments
A. C. Westphalen was supported by the National Institute of Biomedical Imaging and Bioengineering (NIBIB T32 training grant no. 1 T32 EB001631).
References
- 1.Chiang G, Levine D. Imaging of adnexal masses in pregnancy. J Ultrasound Med. 2004;23:805–819. doi: 10.7863/jum.2004.23.6.805. [DOI] [PubMed] [Google Scholar]
- 2.Bromley B, Benacerraf B. Adnexal masses during pregnancy: accuracy of sonographic diagnosis and outcome. J Ultrasound Med. 1997;16:447–452. doi: 10.7863/jum.1997.16.7.447. [DOI] [PubMed] [Google Scholar]
- 3.Coakley FV, Glenn OA, Qayyum A, Barkovich AJ, Goldstein R, Filly RA. Fetal MRI: a developing technique for the developing patient. AJR. 2004;182:243–252. doi: 10.2214/ajr.182.1.1820243. [DOI] [PubMed] [Google Scholar]
- 4.The Royal College of Radiologists: Board of the Faculty of Clinical Radiology. Gadolinium-based contrast media and nephrogenic systemic fibrosis. London, UK: The Royal College of Radiologists; Nov, 2007. [Accessed November 24, 2007]. reference no. BFCR(07)14. www.rcr.ac.uk/docs/radiology/pdf/BFCR0714_gadolinium_NSF_guidanceNov07.pdfPublished November 2007. [Google Scholar]
- 5.Weinreb JC, Brown CE, Lowe TW, Cohen JM, Erdman WA. Pelvic masses in pregnant patients: MR and US imaging. Radiology. 1986;159:717–724. doi: 10.1148/radiology.159.3.3517956. [DOI] [PubMed] [Google Scholar]
- 6.Brown MA, Ascher SM, Semelka RC. Adnexa. In: Semelka RC, editor. Abdominal–pelvic MRI. 2. Hoboken, NJ: Wiley-Liss; 2006. pp. 1333–1382. [Google Scholar]
- 7.Tamai K, Koyama T, Togashi K. MR features of ectopic pregnancy. Eur Radiol. 2007;17:3236–3246. doi: 10.1007/s00330-007-0751-6. [DOI] [PubMed] [Google Scholar]
- 8.Baltarowich OH, Kurtz AB, Pasto ME, Rifkin MD, Needleman L, Goldberg BB. The spectrum of sonographic findings in hemorrhagic ovarian cysts. AJR. 1987;148:901–905. doi: 10.2214/ajr.148.5.901. [DOI] [PubMed] [Google Scholar]
- 9.Poder L, Coakley FV, Rabban JT, Goldstein RB, Sollitto RA, Chen L. Decidualized endometrioma during pregnancy: recognizing an imaging mimic of ovarian malignancy. J Comput Assist Tomogr. 2008 doi: 10.1097/RCT.0b013e31814685ca. (in press) [DOI] [PubMed] [Google Scholar]
- 10.Tukeva TA, Aronen HJ, Karjalainen PT, Molander P, Paavonen T, Paavonen J. MR imaging in pelvic inflammatory disease: comparison with laparoscopy and US. Radiology. 1999;210:209–216. doi: 10.1148/radiology.210.1.r99ja04209. [DOI] [PubMed] [Google Scholar]
- 11.Hall BP, Printz DA, Roth J. Massive ovarian edema: ultrasound and MR characteristics. J Comput Assist Tomogr. 1993;17:477–479. doi: 10.1097/00004728-199305000-00027. [DOI] [PubMed] [Google Scholar]
- 12.Sayar H, Lhomme C, Verschraegen CF. Malignant adnexal masses in pregnancy. Obstet Gynecol Clin N Am. 2005;32:569–593. doi: 10.1016/j.ogc.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Kurtz AB, Tsimikas JV, Tempany CM, et al. Diagnosis and staging of ovarian cancer: comparative values of Doppler and conventional US, CT, and MR imaging correlated with surgery and histopathologic analysis—report of the Radiology Diagnostic Oncology Group. Radiology. 1999;212:19–27. doi: 10.1148/radiology.212.1.r99jl3619. [DOI] [PubMed] [Google Scholar]