Abstract
We have succeeded in implementing ring-shaped light illumination ultrasound-modulated optical tomography (UOT) in reflection mode. The system used intense acoustic bursts and a charge-coupled device camera-based speckle contrast detection method. In addition, the implementation allows placing the tissue sample below (not within) an acoustic coupling water tank and scanning the tissue without moving the sample. Thus, the UOT system is more clinically applicable than previous transmission-mode systems. Furthermore, we have successfully imaged an ex vivo methylene-blue-dyed sentinel lymph node (SLN) embedded at a depth of 13 mm in chicken breast tissue. This UOT system offers several advantages: noninvasiveness, nonionizing radiation, portability, cost-effectiveness, and possibility of combination with ultrasound pulse-echo imaging and photoacoustic imaging. One potential application of the UOT system is mapping SLNs in axillary staging for breast cancer patients.
Keywords: Reflection-mode ultrasound-modulated optical tomography, ring-shaped light illumination, sentinel lymph node biopsy, breast cancer, axillary lymph node dissection
Imaging optical properties in the visible and near-infrared regions in biological tissues has become increasingly important because the optical properties are directly related to the functional and morphological parameters of tissues.1,2 However, owing to strong light scattering in tissue, keeping high spatial resolution in relatively deep tissue (beyond one transport mean free path) is still a challenge in pure optical imaging techniques such as diffuse optical tomography (DOT).3 Ultrasound-aided optical imaging techniques such as photoacoustic (PA) imaging2 and ultrasound-modulated optical tomography (UOT)4 overcome the drawback of pure optical imaging by taking advantage of optical contrast and ultrasonic spatial resolution. In spite of the great success of PA imaging, the optical contrast of PA imaging is mainly based on optical absorption. However, by supplying information about the optical scattering as well as the optical absorption parameters of tissue, UOT can potentially provide more biological information than PA imaging.5
In UOT, when diffuse light travels through the ultrasound focal spot in tissues under ultrasound insonification, the light is acoustically tagged by ultrasound-induced particle displacement and refractive index changes.6,7 By quantifying the intensity ratio of the tagged photons to the untagged photons at each scanned ultrasound focal spot, we can obtain images that represent the local optical heterogeneities of tissues. The principles of UOT have been theoretically modeled by Leutz and Maret8, Wang6, and Sakadžic' and Wang.7 The generally low signal-to-noise ratio (SNR) is a major challenge in UOT. Experimentally, a number of detection techniques have been explored to surmount the low SNR difficulty9-11. In addition to the low SNR, the practicability of current UOT systems for clinical application is also limited: most current UOT systems are in transmission modes, tissue samples still need to be immersed in water, and the samples are mechanically moved for scanning9-12. Therefore, there is a pressing need to develop a practical reflection-mode UOT system for clinical application.
In this Letter, for the first time to our knowledge, we have implemented a ring-shaped light illumination UOT system in reflection mode, using intense acoustic bursts and a charge-coupled device (CCD) camera-based speckle contrast detection technique.13 We can implement a portable and relatively economical UOT system by mounting the light source (a cw diode laser), the light detector (a CCD camera), and the ultrasonic transducer on a scanning stage. For more clinical practicability, the UOT system itself moves instead of the sample, and the sample is positioned below a water tank, rather than immersed in it. In a preliminary test for clinical applicability, we have successfully imaged an ex vivo methylene-blue-dyed sentinel lymph node (SLN) buried at a depth of 13 mm in chicken breast tissue (the mean depth of the top surface of human SLNs is 12 mm in ultrasound images).
Figure 1 shows the experimental setup for our reflection-mode UOT system, which is similar to the photoacoustic microscopy system in Ref [14]. We can build a compact and inexpensive UOT system by using a small diode laser (Melles Griot, 56ICS153/HS; 657-nm wavelength; 9 × 6 × 13 cm along the X, Y, and Z axes). The laser is coaxially positioned on a two-dimensional mechanical scanner with a focused ultrasonic transducer (Panametrics, A326S-SU; 5 MHz central frequency; 12.7 mm active aperture; 16.0 mm focal length). The bottom surface of the transducer, installed inside the optical condenser, is coupled with water inside a tank whose bottom opening is covered with a thin, clear plastic membrane. A tissue sample is located immediately underneath the water tank. Up to 2.5-MPa maximum pressure is achieved in the ultrasonic focal spot, so the mechanical index at this frequency is about 1.1, within the typical safety limit for diagnostic ultrasound.15 The donut-shaped light illumination is formed by a conical lens and then focused through an optical condenser. Unlike an optical condenser in Ref [12], this optical condenser composes of two plano-convex lenses to enhance the efficiency of diffusely reflected light collection from the sample. The line focus of the light is aligned with the ultrasonic focal zone in the water, forming a quasi-confocal configuration of optical illumination and ultrasound. Compared with a coaxial bright-field light illumination design,16 this configuration has the following advantages: First, the large area of donut-shaped illumination reduces the optical fluence on the sample surface to 8 mW/cm2, within the current safety limit.17 Second, thanks to the evenly distributed light illumination, the light shadow effect can be alleviated. Third, the dark-field ring-shaped illumination reduces unwanted surface modulation from outside the ultrasonic focal zone.
FIG. 1.
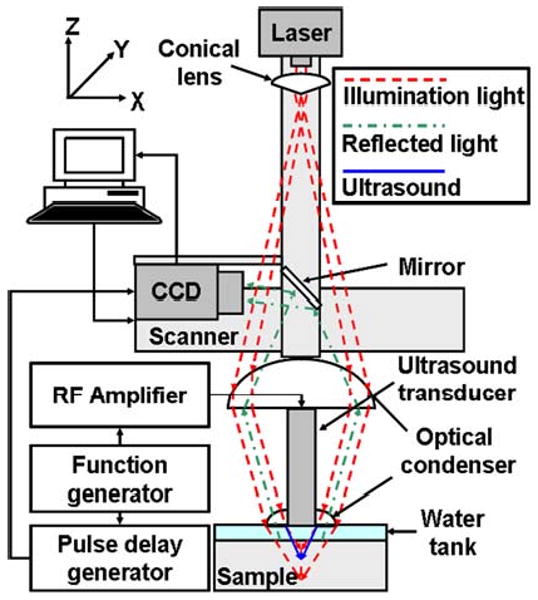
Experimental schematic of the reflection-mode ring-shaped light illumination UOT system
A CCD camera (Basler, A312f; 12-bit, 640×480 pixels) is also positioned on the scanner, so diffusely reflected light from the tissue sample first travels back through the optical condenser, is reflected by a mirror, and is collected by the CCD camera. The CCD camera captures the speckle pattern formed by diffusely reflected light from the sample. The automatic mechanical scanner is controlled by a computer for raster scanning, so the entire UOT system is moved instead of the sample. A function generator (Agilent, 33250A) synthesizes acoustic bursts and simultaneously triggers a pulse-delay generator (Stanford Research, DG535). Subsequently, the ultrasound tone bursts are amplified by an RF amplifier (Amplifier Research, 75A250) and drive the ultrasound transducer. The synchronized pulse-delay generator triggers the CCD camera twice for each burst; one burst-synchronized CCD frame is captured with ultrasound, and another one is captured without ultrasound shortly (600 ms) after. A low 0.83-Hz burst repetition rate is used to protect the transducer. Both the exposure time of the CCD camera and the duration of each ultrasonic burst are fixed at 2 ms. Two laser speckle contrasts are measured with ultrasound insonification and without. We define the difference in speckle contrasts between the ultrasound on and off conditions as the UOT signal. The signals are normalized by the maximum value in the image. Ten pairs of ultrasound on-off measurements are averaged to enhance SNRs in UOT signals.
To investigate the SNR, spatial resolution, and quality of cross-sectional images of the UOT system, we first imaged an optically absorptive target buried 6 mm deep in a tissue-mimicking phantom. The scattering medium was made of gelatin and intralipid with a reduced scattering coefficient of ∼9cm-1. Black India ink was added to the absorptive target. The target was 1.5 mm thick along the ultrasound propagation direction. The maximum acoustic pressure in the transducer focus was 2.3 MPa. The object in the photograph, Fig. 2(a), is clearly imaged using the UOT system in Fig. 2(b), whereas the unmodulated light intensity (DC) based image in Fig. 2(d) shows a widely broadened target. The images are in the XY plane and perpendicular to the Z direction. Figure 2(c) compares two 1D profiles taken from the UOT image and the DC image. The 1D image from the UOT image provides higher resolution and stronger contrast. In addition, the peak absorption position of the target in the DC image is off by about 2 mm from the original position. The spatial resolution, defined as the one-way distance between the 25% and 75% points of the edge spread function, is 1.16±0.23 mm (standard error). The SNR, defined as the ratio of the mean to the standard deviation of the UOT signals, is 32±3 (standard error). This SNR is about 6 times worse than the reported SNR from a transmission-mode ring-shaped light illumination UOT system (199±13 (standard error))12 since the collection of diffusely reflected light passing back through the optical condenser is much less efficient than the collection of diffusely transmitted light passing directly through the sample.
FIG. 2.
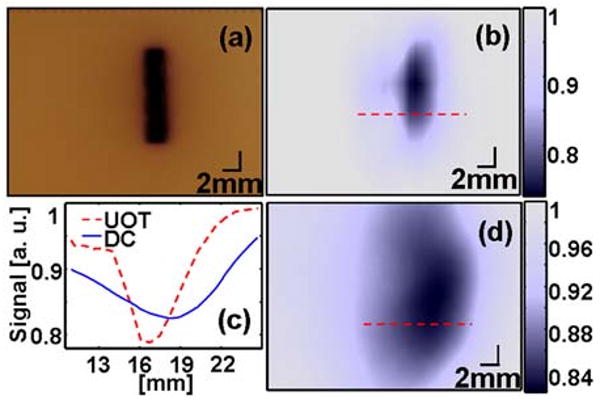
Cross-sectional UOT image of an optically absorptive object. (a) Photograph of the target. (b) UOT image based on change in speckle contrast. (c) 1D profiles along the cuts in Fig. 2(b) and 2(d). (d) Unmodulated light intensity based image (DC)
To examine the feasibility of this technology for in vivo axillary staging for breast cancer patients, we imaged an ex vivo methylene-blue-dyed SLN embedded 13 mm deep in chicken breast tissue, which is comparable with the mean depth of the top surface of human SLNs from the skin surface (∼12 mm) as measured by ultrasonography. All animal handling followed guidelines on the care and use of laboratory animals at Washington University in St. Louis. First, 0.25 ml of 1% methylene blue dye (10 mg/mL, American Regent, INC) was injected intradermally on the right forepaw pad of an adult male Sprague Dawley rat weighing 380 g. Fifteen minutes after the methylene blue injection, the animal was euthanized by administering an overdose of pentobarbital. The SLN dyed with methylene blue was removed from the right axilla of the animal, and one without any dye was excised from the other axilla. The two excised nodes (3 × 4 × 2 mm along the X, Y, and Z axes) were buried 13 mm below the tissue surface in chicken breast tissue (Figure 3(a) and 3(c)). The transparent membrane of the water tank was coupled with the top slice of chicken breast tissue. To reduce acoustic impedance mismatch, ultrasound coupling gel was used at the interface. Figure 3(c) shows the thickness of the top piece of chicken tissue, ∼13 mm. A needle was placed to indicate the middle interface between the two tissue slices. The UOT image shows only the methylene-blue-dyed node clearly in Fig. 3(b), and agrees well with the photograph in Fig. 3(a). Notably, the unmodulated light intensity based image in Fig. 3(d) does not provide any information about the localized methylene-blue-dyed SLN.
FIG. 3.
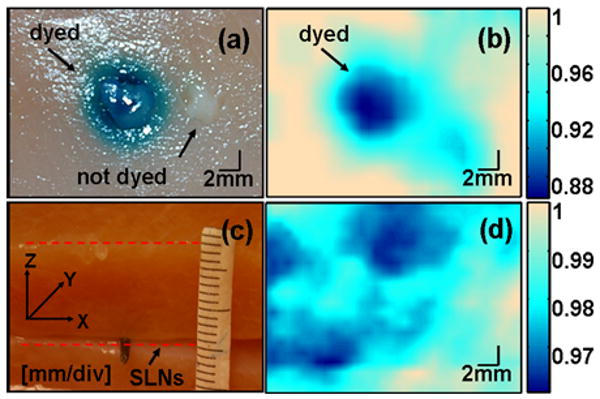
Ex vivo cross-sectional images of two sentinel lymph nodes at 13-mm depth in chicken breast tissue. (a) Photograph of two nodes; the left node is dyed with methylene blue and the right one is not. (b) UOT image. (c) Photograph of chicken tissues (d) Unmodulated light intensity based image
In conclusion, we have implemented a reflection-mode ring-shaped light illumination ultrasound-modulated optical tomography and applied the system to image an ex vivo methylene-blue-dyed SLN buried 13 mm deep in biological tissue. This UOT system has several advantages: 1. Compared to the previous transmission systems, this reflection-mode system is more practical for clinical applications. 2. Compared to the coaxial bright-field light illumination system, it has less light shadow effect due to the even light distribution, and it reduces unwanted surface modulation. 3. Compared to photoacoustic imaging, it is more portable and cheaper owing to the small and cheap light source. It also provides optical scattering information.5 4. It is nonionizing and noninvasive, unlike ionizing and intraoperative gamma radiation based detection techniques for mapping SLNs. 5. It offers the possibility of combining three imaging techniques: UOT, PA imaging, and single-element ultrasound pulse-echo imaging.12 Considering these features and the preliminary experimental results, it is expected that this technique can clinically and practically be tested to image methylene-blue dyed SLNs in humans in vivo.
Acknowledgments
This research was supported by NIH Grant Nos. R33 CA 094267.
References
- 1.Fujimoto JG. Optical coherence tomography for ultrahigh resolution in vivo imaging. Nat Biotechnol. 2003;21(11):1361–1367. doi: 10.1038/nbt892. [DOI] [PubMed] [Google Scholar]
- 2.Zhang HF, Maslov K, Stoica G, Wang LV. Functional photoacoustic microscopy for high-resolution and noninvasive in vivo imaging. Nat Biotechnol. 2006;24(7):848–851. doi: 10.1038/nbt1220. [DOI] [PubMed] [Google Scholar]
- 3.Zeff BW, White BR, Dehghani H, Schlaggar BL, Culver JP. Retinotopic mapping of adult human visual cortex with high-density diffuse optical tomography. Proc Natl Acad Sci USA. 2007;104(29):12169–12174. doi: 10.1073/pnas.0611266104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang L, Jacques SL, Zhao X. Continuous-wave ultrasonic modulation of scattered laser light to image objects in turbid media. Opt Lett. 1995;20(6):629–631. doi: 10.1364/ol.20.000629. [DOI] [PubMed] [Google Scholar]
- 5.Kothapalli SR, Sakadzic S, Kim C, Wang LV. Imaging optically scattering objects with ultrasound-modulated optical tomography. Opt Lett. 2007;32(16):2351–2353. doi: 10.1364/ol.32.002351. [DOI] [PubMed] [Google Scholar]
- 6.Wang LV. Mechanisms of ultrasonic modulation of multiply scattered coherent light: an analytic model. Phys Rev Lett. 2001;87(4):043903. doi: 10.1103/PhysRevLett.87.043903. [DOI] [PubMed] [Google Scholar]
- 7.Sakadzic S, Wang LV. Correlation transfer and diffusion of ultrasound-modulated multiply scattered light. Phys Rev Lett. 2006;96(16):163902. doi: 10.1103/PhysRevLett.96.163902. [DOI] [PubMed] [Google Scholar]
- 8.Leutz W, Maret G. Ultrasonic modulation of multiply scattered light. Physica B. 1995;204(14):14–19. [Google Scholar]
- 9.Leveque S, Boccara AC, Lebec M, Saint-Jalmes H. Ultrasonic tagging of photon paths in scattering media: parallel speckle modulation processing. Opt Lett. 1999;24(3):181–183. doi: 10.1364/ol.24.000181. [DOI] [PubMed] [Google Scholar]
- 10.Sakadžic' S, Wang LV. High-resolution ultrasound-modulated optical tomography in biological tissues. Opt Lett. 2004;29(23):2770–2272. doi: 10.1364/ol.29.002770. [DOI] [PubMed] [Google Scholar]
- 11.Murray TW, Sui L, Maguluri G, Roy RA, Nieva A, Blonigen F, DiMarzio CA. Detection of ultrasound-modulated photons in diffuse media using the photorefractive effect. Opt Lett. 2004;29(21):2509–2511. doi: 10.1364/ol.29.002509. [DOI] [PubMed] [Google Scholar]
- 12.Kim C, Song KH, Wang LV. Sentinel lymph node detection ex vivo using ultrasound-modulated optical tomography. J Biomed Opt. 2008;13(2):020507. doi: 10.1117/1.2907791. [DOI] [PubMed] [Google Scholar]
- 13.Kim C, Zemp RJ, Wang LV. Intense acoustic bursts as a signal-enhancement mechanism in ultrasound-modulated optical tomography. Opt Lett. 2006;31(16):2423–2425. doi: 10.1364/ol.31.002423. [DOI] [PubMed] [Google Scholar]
- 14.Maslov K, Stoica G, Wang LV. In vivo dark-field reflection-mode photoacoustic microscopy. Opt Lett. 2005;30(6):625–627. doi: 10.1364/ol.30.000625. [DOI] [PubMed] [Google Scholar]
- 15.Dalecki D. Mechanical bioeffects of ultrasound. Annu Rev Biomed Eng. 2004;6:229–248. doi: 10.1146/annurev.bioeng.6.040803.140126. [DOI] [PubMed] [Google Scholar]
- 16.Hisaka M. Ultrasound-modulated optical parallel speckle measurement with stroboscopic illumination in a coaxial reflection system. Appl Phys Lett. 2006;88(3):033901–3. [Google Scholar]
- 17.American national standard for the safe use of lasers, Standard Z136.1-2000. ANSI. Inc; New York: 2002. [Google Scholar]


