Abstract
Francisella tularensis, the etiologic agent of tularemia, can cause severe and fatal infection after inhalation of as few as 10-100 CFU. F. tularensis is a potential bioterrorism agent and, therefore, a priority for countermeasure development. Vaccination with the live vaccine strain (LVS), developed from a Type B strain, confers partial protection against aerosal exposure to the more virulent Type A strains and provides proof of principle that a live attenuated vaccine strain may be efficacious. However LVS suffers from several notable drawbacks that have prevented its licensure and widespread use. To address the specific deficiencies that render LVS a sub-optimal tularemia vaccine, we engineered F. tularensis LVS strains with targeted deletions in the guaA or guaB genes that encode critical enzymes in the guanine nucleotide biosynthetic pathway. F. tularensis LVSΔguaA and LVSΔguaB mutants were guanine auxotrophs and were highly attenuated in a mouse model of infection. While the mutants failed to replicate in macrophages, a robust proinflammatory cytokine response, equivalent to that of the parental LVS, was elicited. Mice vaccinated with a single dose of the F. tularensis LVSΔguaA or LVSΔguaB mutant were fully protected against subsequent lethal challenge with the LVS parental strain. These findings suggest the specific deletion of these target genes could generate a safe and efficacious live attenuated vaccine.
1. Introduction
Francisella tularensis is a Gram-negative facultative intracellular bacterium and the causative agent of tularemia in humans. Depending of the route of exposure and biotype of the infecting strain, the disease may occur in ulceroglandular, oculoglandular, oropharyngeal, pneumonic, or septic forms. Two subspecies of F. tularensis, F. tularensis subsp. tularensis (Type A), and the less virulent F. tularensis subsp. holarctica (Type B), cause the majority of cases of tularemia in humans [44]. These two biotypes differ in geographic distribution as well as pathogenic manifestations. F. tularensis subsp. holarctica is found primarily in Europe, Asia, and to a lesser extent, in North America and causes a disease with reduced severity. F. tularensis subsp. tularensis is found almost exclusively in North America and aerosal exposure to as few as 10 CFU has the capacity to cause severe morbidity and mortality [25;37]. Accordingly, the CDC has designated F. tularensis as a Category A pathogen and a biodefense priority for vaccine development.
Currently, there is no licensed vaccine for Francisella. In the 1950s, a live attenuated strain of F. tularensis subsp. holarctica (LVS) was developed in the Soviet Union and transferred to the United States [10]. Despite the ability of LVS to decrease the incidence of laboratory acquired tularemia [5] as well as to confer partial protection against wild-type challenge, several factors prevented its licensure and widespread use. Specifically, these include an unknown and undefined molecular basis of attenuation [47], phenotypic inconsistencies [12;23], and its ability to confer only partial protection against virulent Type A challenge [25;37].
While not an optimal vaccine, LVS serves as proof of principal that a live attenuated strain can be an effective tool to prevent human tularemia. A more valuable vaccine strain would contain precisely defined genetic mutations that render it safe for use in the general population and protective against virulent Type A challenge. Targeted mutations in genes composing metabolic pathways have been the basis of attenuating mutations in many bacterial pathogens. For example, the guaBA operon encodes two enzymes critical for guanine nucleotide biosynthesis. Deletions in the Shigella flexneri guaBA operon led to an attenuated auxotrophic strain that is both safe and immunogenic in volunteer studies [28;29]. As the synthesis of guanine nucleotides requires both IMP dehydrogenase, encoded by guaB, and GMP synthase, encoded by guaA, we hypothesized that deletion of either gene would render Francisella auxotrophic for guanine and attenuated for virulence. Interestingly, and unlike enteric organisms, the Francisella guaB and guaA genes are not contained within an operon, but rather, are present as independent loci separated by 312,613 bp.
Until recently, few tools were available for the genetic manipulation of F. tularensis [16]. In this report, we describe a system to generate precise deletions in chromosomal loci to construct F. tularensis LVS mutants that contained deletions in either the guaB or guaA genes. Here, we report characterization of two vaccine prototypes, LVSΔguaA and LVSΔguaB. Both are auxotrophic for guanine, attenuated for growth within macrophages, and exhibit reduced virulence in the mouse model. Most importantly, a single inoculation with either attenuated strain protected mice against a subsequent wild-type challenge.
2. Materials and Methods
2.1 Bacterial and growth conditions
Bacterial strains used in this study are listed in Table 1. F. tularensis LVS was kindly provided by Dr. Karen L. Elkins (CBER/FDA, Rockville, MD), and preserved in aliquots at −80°C. Mueller Hinton Broth (Becton Dickinson Microbiology Systems, Sparks, MD) supplemented with 1% IsoVitaleX (Becton Dickinson, Cockeysville, MD), 0.1% glucose and Ferric PPi (Sigma Chemical Co. St. Louis Mo.) was used for liquid cultures (MHB) and Mueller Hinton Agar containing 10% defibrinated sheep blood (MHA-B) was used for solid media when culturing Francisella strains. When needed, kanamycin (km) was added at a final concentration of 10 μg/ml and guanine added at a final concentration of 0.001%. The suicide plasmids used in this study were propagated in E. coli DH5α, grown in LB broth supplemented with ampicillin (Ap, 250 μg/ml) or Km (50 μg/ml). LVS vaccine stocks used for the animal studies were made from bacteria cultured in MHB and were stored in aliquots at −80°C. These were thawed for use, and viable bacteria were quantified by plating serial dilutions on MHA-B plates.
Table 1. Bacterial strains and plasmids used in this study.
| Strain or plasmid | Relevant characteristics | Reference or source |
|---|---|---|
| Strains | ||
| F. tularensis LVS | Attenuated F. tularensis vaccine strain | CBER/FDA |
| LVSΔguaA | F. tularensis LVS mutant in guaA locus | This study |
| LVSΔguaB | F. tularensis LVS mutant in guaB locus | This study |
| E coli DH5α | deoR, endA1, gyrA96, recA1, relA1, supE44 | Laboratory collection |
| Plasmids | ||
| pUC19 | Cloning vector (Ampr) | Laboratory collection |
| pBlue-ScriptKS+ | Cloning vector (Ampr) | Laboratory collection |
| pUCGA | Containing guaA5′-aphT-guaA3′ cassette | This study |
| pBSGB | Containing guaB5′-aphT-guaB3′ cassette | This study |
| pSacB | Containing the sacB gene | This study |
| pFT695 | guaA suicide plasmid | This study |
| pFT724 | guaB suicide plasmid | This study |
| pFT906 | Plasmid containing PguaB promoter | This study |
| PFT916 | Plasmid containing PguaB-guaA fragment | This study |
| pKK214 | Plasmid used to trans complement mutants | UTSA |
| pKK214guaA | pKK214 plasmid containing full-length guaA | This study |
| pKK214guaB | pKK214 plasmid containing full-length guaA | This study |
2.2 Construction of suicide vectors
The guaB and guaA genes were deleted by allelic exchange using the suicide plasmids, pFT724 and pFT695, respectively. Mutagenesis of both genes was accomplished by deletion of the locus and replacement with the aphT gene (encoding km resistance, Genbank accession #AY048743) amplified with primers AphTfor and AphTrev. Briefly, 500-bp flanking regions upstream and downstream of guaA (FTL_1071; location in the genome, 1023479 to 1025029) or guaB (FTL_1478; location in the genome, 1403186 to 1404646) were amplified from F. tularensis LVS using the primers listed in Table 2. Primers GuaA5for and GuaA5Arev amplified a 500 bp fragment upstream of guaA, and primers GuaA3for and GuaA3rev amplified a 500 bp fragment downstream of guaA. The fragments were cloned into pUC19 and the aphT gene was inserted in between the flanking fragments as a SmaI fragment to create pUCGA (guaA5′-aphT-guaA3′ cassette). Similarly, 500 bp fragments upstream and downstream of guaB were amplified using primer pairs GuaB5for - GuaB5rev and GuaB3for - GuaB3rev, respectively. The fragments were cloned into pBlue-Script SK (Stratagene), with restriction sites BamHI and HindIII and the aphT gene was inserted in between the 2 fragments via a SmaI site to create pBSGB (guaB5′-aphT-guaB3′ cassette).
Table 2. Oligonucleotides used in this study.
| Name | Oligonucleotide Sequences (5′ → 3′) | Combined primers and product size (bp) |
|---|---|---|
| Upstream guaA region | ||
| GuaA5for | CCC GGA TCC ATC TTT AGA GAT AAG TTT TCA CAT ATT GAG | GuaA5for-GuaA5rev (500) |
| GuaA5rev | GAT GAT ATC TTT TTA TAA AAA TAA ACA TTT TCT TAA AAG GTT ATT T | |
| Downstream guaA region | ||
| GuaA3for | GAT GAT ATC GCT ATG TCA AAA TAT ACT ATT TTA GAT AAA ATA A | GuaA3for-GuaA3rev (500) |
| GuaA3rev | CCC GTC GAC GCG GCC GCA GAT CTA TAC CGC CAG CAT GAT TTA AGG CTT CA | |
| Upstream guaB region | ||
| GuaB5for | CCC GGA TCC TAA ATA TAA GCC TAA GGC AGT GAT TGA TTT | GuaB5for-GuaB5rev (500) |
| GuaB5rev | GAT CCC CGA ATT CCT GCA GCC CGG GTT TTT GAT CTC CGT AAT TAA AAT CTA AAG AGT | |
| Downstream guaB region | ||
| GuaB3for | CCC GAA TTC CTG CAG AAC CTC TTA ATT ATG ATT TTA ATA AGT TAT AAT | GuaB3for-GuaB3rev (500) |
| GuaB3rev | CCC GTC GAC GCG GCC GCA ACA ACA CCG CTT ACA GCA AAC TTT TTA | |
| Km resistance cassette (aphT) | ||
| AphTfor | ATG CCC GGG GAA GTT CCT ATA CTT TCT AGA GAA TAG | AphTfor-AphTrev (1438) |
| AphTrev | ATG CCC GGG AGT TCC TAT TCC GAA GTT CCT ATT CT | |
| GroEL promoter (PgroEL) | ||
| GroELfor | GAA TTC CGG ATC CTT TCT TGA AAA TTT TTT TTT TGA CTC AAT AT | GroELfor-GroELrev (132) |
| GroELrev | GAA TTC CCC CGG GCA TAT GAA TCT TAC TCC TTT GTT AAA TTA | |
| Genotypic identification of LVS guaA mutant | ||
| OLIGA1 | GGA TAA AAT AAC CTT TTA AGA AAA TGT TT | OLIGA1-OLIGA2 (565) |
| OLIGA2 | GTT TCT GGG TGA AAC TGC ACA CC | OLIGA1-OLIGkm (855) |
| Genotypic identification of LVS guaB mutant | ||
| OLIGB1 | ACT CTT TAG ATT TTA ATT ACG GAG ATC | OLIGB1-OLIGB2 (550) |
| OLIGB2 | TCT TTT TAA TCG CTC CTT GAG AAG C | OLIGB1-OLIGkm (840) |
| aphT oligonucleotide | ||
| OLIGkm | ATG CAG CCG CCG CAT TGC ATC A | |
| Trans complementation of guaA gene | ||
| CompA1 | AGC TAG CTC CCG GGA TGA CAG ATA TAC ATA ATC ATA AGA TTT TGA TT | CompA1-CompA2 (1550) |
| CompA2 | AGC TAG CTG ATA TCG TCG ACT TAT TCC CAT TCA ATT GTT CCA GGT GGT T | |
| Trans complementation of guaB gene | ||
| CompB1 | GGG ACT AGT CTA GAG CGA AAT AGT AAA TTC TAA TAC TTA TTT C | CompB1-ComB2 (1570) |
| CompB2 | GGG ACT AGT CTA GAT TAA GAC TGG TAA TTA GG TGG TTC TTT AG | |
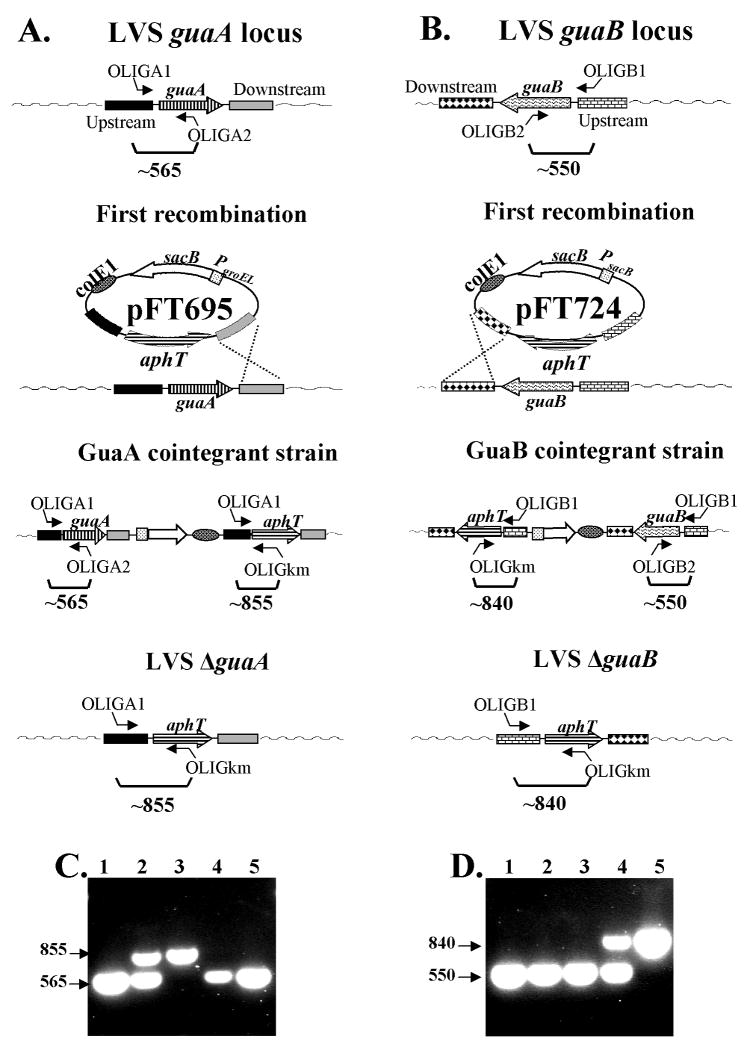
Subsequently, pFT695 (Figure 1A) was constructed by sub-cloning the guaA5′-aphT-guaA3′ cassette into pSacB plasmid as a SpeI/SalI fragment. pSacB is a pUC19 derivative plasmid that contains sacB (encoding levansucrase) to promote plasmid elimination during sucrose treatment. The efficiency of pFT695 in Francisella was improved by replacing the native sacB promoter (PsacB) with the Francisella PgroEL promoter [14] (5′-TTT CTT GAA AAT TTT TTT TTT GAC TCA ATA TCT AGA CTT GCA AGA GCT TGG AAC TTT GAG ATT GTT CTA AGA TGC ATA CAA ATT CAA AAT GCT TAA ACA AAA ATA ATT TAA CAA AGG AGT AAG ATT CAT ATG-3′) amplified with primers GroELfor and GroELrev. Similarly pFT724 (Figure 1B) was obtained by sub-cloning the guaB5′-aphT-guaB3′ cassette into pSacB plasmid as a SpeI/SalI fragment. pFT695 and pFT724 were electroporated into LVS.
Figure 1.
Deletion of guaA (panel A) or guaB (panel B) in F. tularensis LVS was generated by allelic exchange. F. tularensis LVS∷FTp695 and LVS∷pFT724 cointegrants were generated by recombination of pFT695 or pFT724 into the LVS genome. Second recombination events for plasmid curing were promoted by growing the strains in sucrose. Colonies auxotrophic for guanine were isolated on MHA-B plates and evaluated by PCR. The genotypic PCR analysis utilized isolated genomic DNA from parental LVS, lane 1; LVS∷pFT695 cointegrant, lane 2; LVSΔguaA mutant, lane 3; LVS∷pFT724 cointegrant, lane 4 and LVSΔguaB mutant strain, lane 5. Primers were specific for guaA (OLIGA1, OLIGA2, OLIGkm) in panel C, or specific for guaB (OLIGB1, OLIGB2, OLIGkm) in panel D.
2.3 Deletion of guaA and guaB loci
Cells from one plate of confluent LVS growth were resuspended in 1.5 ml of fresh sucrose wash buffer (0.5 M sucrose) and centrifuged at 14,000 rpm. The pellet was re-suspended in wash buffer and centrifuged again for a total of four washes. The final pellets resulting from two bacterial plates were suspended in wash buffer to a total volume of 300 μl and mixed with the suicide plasmid. Electroporation conditions were 1.75 Kv, 25 μF and 600Ω for a total of 3 pulses. The electroporation mix was transferred to 1.5 ml of MHB. The bacteria were incubated with shaking for 3 h at 37°C, and plated on MHA-B with 10 μg/ml of km. Isolated colonies were analyzed by PCR to confirm the suicide plasmid integration in the F. tularensis genome. A positive cointegrant colony was selected and grown in MHB with 10% sucrose. When the optical density (OD) was ∼0.4 at 600 nm, the bacteria were spread on MHA-B plates with guanine. Individual colonies were then replica plated onto MHA-B plates without guanine to identify guanine auxotrophs. Isolated guanine auxotrophic colonies were evaluated by PCR. Genomic DNA was isolated from colonies according to the Gnome®DNA KIT (Q-BIOgene, Carlsbad, CA) manufacturer's protocol and used as the PCR template. The primers used for genotype confirmation of the guaA mutation include OLIGA1, OLIGkm, and OLIGA2 (Table 2). The primers used for genotype confirmation of the guaB mutation include OLIGB1, OLIGkm, and OLIGB2 (Table 2).
2.4 Bacterial growth curves
The guanine auxotrophic phenotypes of F. tularensis LVSΔguaA and LVSΔguaB were evaluated in vitro. Isolated LVS derivatives were inoculated in 5 ml of MHB media supplemented with guanine and incubated overnight at 37° C. Aliquots containing 100 μl of the overnight inocula were transferred to 50 ml of fresh media that either contained or lacked guanine supplementation (at 0.01 μg/ml final concentration). Both cultures were incubated with shaking at 37° C and the OD at 600 nm was evaluated every hour.
Reversion to guanine prototrophy was assessed by growing LVSΔguaA and LVSΔguaB in 10 ml broth cultures with serial passage every 24 hours for 2 days. At 6 hours and every 24 hour time point, bacteria were plated on MHB plates with or without guanine. The total number of bacteria in the culture was calculated from colony counts of serial dilutions plated on MHB plus guanine on day 3 post plating. The reversion rate was calculated by dividing the number of bacteria growing on MHB plates without guanine by the total number of bacteria in the culture. No colonies of LVSΔguaA or LVSΔguaB grew on MHB plates without guanine (allowed to incubate 3-5 days post plating). The reversion rate for each mutant was calculated to be <10-10.
2.5 Intracellular Replication Assay
The intracellular replication of LVSΔguaA and LVSΔguaB mutants was evaluated in the murine macrophage cell line, J774 (American Type Culture Collection, Manassas, VA). Cells were cultivated in Dulbecco's modified essential medium (DMEM) (Cellgro® Herndon, VA), supplemented with 2 mM glutamine (Gibco, Grand Island, NY) and 10% heat-inactivated defibrinated fetal bovine serum (Gibco), and were maintained at 37° C in humidified air containing 5% CO2 throughout the assay. Intracellular replication of the various strains was assessed in duplicate wells in 12-well plates (Costar, Corning, NY). Wells containing 3 × 105 cells per well were infected with bacteria at a multiplicity of infection (MOI) of 100 for 2 hours. Following this period, cells were washed 3 times with PBS, and incubated in DMEM medium containing 50 μg/ml of gentamicin (Gibco) for 1 hour. After 1 hour, the cells were washed and incubated in DMEM medium with 2 μg/ml gentamicin. F. tularensis replication in macrophages was evaluated at 0 - 48 hours post-gentamicin treatment by lysis of cells with a PBS-SDS (0.02%) solution and plating 10-fold serial dilutions on MHA-B plates. To determine if the intracellular growth defect of the LVSΔguaA and LVSΔguaB strains was specifically due to a failure to synthesize GMP de novo rather than an inability to use preformed guanine molecules, J774 cells were infected with LVS derivatives and incubated in DMEM medium with guanine (0.5μg/ml) or without guanine. Intracellular bacterial replication was evaluated at 0, 24, and 48 hours after gentamicin treatment.
2.6 Complementation of LVS mutants
pKK214guaA and pKK214guaB were constructed to complement the corresponding gua mutant in trans. Both pKK214guaA and pKK214guaB plasmids were derived from pKEK612 (kindly provided by Dr. Karl E. Klose, UTSA) [32]. First, pKEK612 was digested with XbaI to release the fragment araC-PBAD-γβexo encoding λRed recombinase genes and re-ligated to obtain pKK214 [30]. The PguaB-guaB fragment including the guaB gene and its promoter was amplified by PCR with primers CompB1 and CompB2 and cloned in XbaI-digested pKK214 to generate pKK214guaB. Since a guaA promoter has not been identified, the guaB promoter was used to drive guaA expression in pKK214. Previously, we engineered pFT906 to drive expression of genes in Francisella. pFT906 has the Francisella guaB promoter, PguaB, (5′- TTT CTT GAA AAT TTT TTT TTT GAC TCA ATA TCT AGA CTT GCA AGA GCT TGG AAC TTT GAG ATT GTT CTA AGA TGC ATA CAA ATT CAA AAT GCT TAA ACA AAA ATA ATT TAA CAA AGG AGT AAG ATT CAT ATG-3′) followed by a multi-cloning site including SpeI, XmaI, Sal I, NdeI and EcoRV restriction sites.
The guaA gene was amplified by PCR using primers CompA1 and CompA2, digested with XmaI/SalI and cloned into pFT906 to generate pFT916. The PguaBguaA fragment was excised from pFT916 and subcloned into pKK214 as an EcoRV fragment to generate pKK214guaA. pKK214guaA and pKK214guaB were electroporated into the corresponding LVS mutant.
2.7 Real-time PCR
Peritoneal macrophages were isolated from 6-8 week old female BALB/c mice 4 days after intraperitoneal (i.p.) injection of sterile 3% thioglycollate. Macrophages were plated in 12-well plates (2 × 106 cells/well) (Costar, Corning, NY USA). All experiments were performed in triplicate. After overnight incubation, cells were washed with PBS to remove non-adherent cells. Cells were cultured in RPMI 1640 containing 2% FBS and 2 mM L-glutamine during all experiments. Cells were infected with either the parental LVS or the LVS ΔguaB mutant at an MOI of 100. After 2 hours, the cells were washed twice in sterile PBS then incubated for 45 min in RPMI 1640 containing 50 μg/ml gentamicin, followed by replacement with antibiotic-free media. Time 0 was defined as the time at which the gentamicin-containing medium was replaced with antibiotic-free medium. Total RNA was isolated from macrophage cultures using TRIzol (Invitrogen., Carlsbad), at 0, 4, 8 and 24 hours. Real-time PCR was performed in a Sequence Detector System (ABI Prism 7900 Sequence Detection System and software; Applied Biosystems, Foster City, CA). Levels of mRNA for specific murine genes are reported as relative gene expression over background levels detected in uninfected control samples. The primer sets and reagents used in these studies were previously described [7;11]. All cellular treatments were performed in triplicate and data are representative of a single experiment.
2.8 F. tularensis growth in organs of naïve mice
Bacterial replication of LVS, LVSΔguaA, and LVSΔguaB was analyzed in vivo. Groups of 9 to 10 BALB/c mice (Charles River, N.Y.) were housed in microisolator cages in a barrier environment at the University of Maryland, School of Medicine Animal Facility. All experiments were performed according to protocols approved by the UMB Institutional Animal Care and Use Committee. The mice were injected i.p. with 100 CFU of LVSΔguaA, 720 CFU of LVSΔguaB or 860 CFU of LVS in 1 ml of gelatin 1%-PBS. Bacterial recovery from the lungs, spleens, livers, and blood of infected mice was evaluated at 24, 48 and 72 h post-infection. At each time point, 3-4 mice were euthanized and 100 μl of blood collected from the heart was plated on MHA-B to assess the systemic bacterial burden. The organs were dissected aseptically and homogenized. The homogenates were serially diluted in PBS and spread on MHA-B plates. The plates were incubated at 37° C for 2 to 5 days and the CFU in each organ was determined.
2.9 Immunogenicity of the LVS derivatives in mice
The virulence of the LVS derivatives was evaluated in three individual animal experiments. In a preliminary experiment, groups of 5 BALB/c mice were injected i.p. with varying amounts of LVS, LVSΔguaA, or LVSΔguaB suspended in 1 ml of 0.1% gelatin-PBS. A control group of mice was injected with 1 ml gelatin-PBS. The mice were monitored daily and survival ratio was determined at day 28.
The ability of the LVSΔguaA and LVSΔguaB strains to protect against subsequent LVS challenge was also evaluated. Twenty-eight days after immunization with varying doses of either LVSΔguaA or LVSΔguaB or 1 ml of gelatin-PBS, mice were challenged i.p with 2.5 × 103 CFU of the parental LVS strain. Challenged mice were observed daily and survival ratio was determined at day 28.
In a second experiment, groups of 10 BALB/c mice were immunized with a single dose of 2.2 × 107 CFU LVSΔguaA, 3.6 × 107 CFU LVSΔguaB or 1ml of gelatin-PBS and challenged at day 28 with 2.8 × 105 CFU of LVS by the i.p. route. Survival ratios were determined at day 28.
In a third experiment, groups of 4 C57BL/6 mice were injected i.p. with approximately 104 CFU of LVS, or 107 or 108 CFU of LVSΔguaA, or or 107 or 108 CFU of LVSΔguaB suspended in 1 ml of 0.1% gelatin-PBS. The mice were monitored daily and the survival ratio was determined at day 11.
2.10 Statistical Methods
Linear regression modeling was used to assess associations of log10 counts with strains and experiments, separately for each time point (0, 24 hours, and 48 hours). In these models, LVS was taken as the reference strain, so that the p-value for each strain coefficient (LVSΔguaB or LVSΔguaA) indicated the statistical significance of that strain compared to LVS; p < 0.05 was considered statistically significant. The combined interaction terms (interactions of experiment with LVSΔguaB and LVSΔguaA) had p > 0.05 in all cases and p > 0.10 in all cases except one, so the final models had terms for strain and experiment, but not their interaction.
3.0 Results
3.1 Construction of F. tularensis LVSΔguaA and LVSΔguaB by allelic exchange
Because of their use as successful attenuating targets in enteric organisms, the guaB and guaA genes were selected for mutation in F tularensis. Using the sequences of the enteric guaB and guaA loci, homologues were identified in the genome sequence of F tularensis that were 62% and 60% identical to the respective enteric genes and separated in the chromosome by 312,613 bp. A deletion in each gene was generated independently using a two-step allelic exchange strategy. The LVS strain was used as the basis for genetic manipulation in order to allow refinement of genetic techniques without the need for high level containment.
The suicide system includes an oriE1 origin of replication that does not support plasmid replication in Francisella, the aphT gene encoding km resistance for selection of plasmid integration into the Francisella chromosome, and a sacB locus driven by the Francisella groEL promoter to allow plasmid counter-selection following resolution. Suicide plasmids pFT695 (Figure 1A) and pFT724 (Figure 1B) were constructed to catalyze complete deletion of the guaA and guaB genes, respectively. The suicide plasmids contain DNA fragments that flank each target gene which was replaced with the aphT gene (km resistance marker) (Figure 1). Each plasmid was independently electroporated into F. tularensis LVS. Transformants were observed after 5-6 days of incubation at 37° C in 5% CO2. Cointegrants were identified by PCR using a set of 3 primers in each reaction. For guaA, primers OLIGA1, OLIGA2, OLIGkm were used (Table 2). For guaB, primers OLIGB1, OLIGB2, OLIGkm were used (Table 2). Site-specific integration in the Francisella genome was confirmed in isolated guaA (LVS::pFT695) and guaB (LVS::pFT724) cointegrants. Using LVS::pFT695 genomic DNA as the template, amplification via PCR yielded two products corresponding to the native guaA gene (565 bp) and deleted guaA version (855 bp) (Figure 1C, lane 2). Similarly, PCR amplification of LVS::pFT724 genomic DNA resulted in two DNA fragments corresponding to the native guaB gene (550 bp) and the deleted guaB version (840 bp) (Figure 1D, lane 4).
Isolated, single cointegrant colonies were chosen for growth in the presence of sucrose to select for a second recombination event and excision of the plasmid from the chromosome. Colonies that were auxotrophic for guanine were evaluated by PCR using the 3 sets primers described above and in Table 2. A single DNA band, corresponding to the mutated allele, was amplified when LVSΔguaA (Figure 1C, lane 3) and LVSΔguaB (Figure 1D, lane 5) were analyzed via PCR. The integrity of guaB in LVSΔguaA and the guaA gene in LVSΔguaB was confirmed by PCR (Figure 1D, lane 3 or Figure 1C, lane 5 respectively). These results demonstrated that LVSΔguaA and LVSΔguaB strains contain specific deletions in the target gua genes.
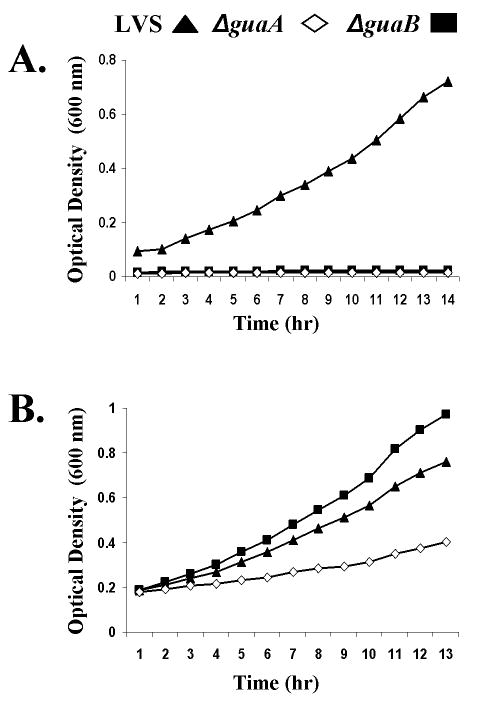
3.2 F. tularensis LVSΔguaA and LVSΔguaB are auxotrophic for guanine
Growth kinetics were measured for LVSΔguaA and LVSΔguaB in MHB in the presence or absence of guanine (Figure 2). While the parental LVS strain grew equally well in MHB with or without guanine supplementation, the LVSΔguaA and LVSΔguaB mutants were unable to grow in media without guanine. Addition of exogenous guanine fully restored the growth rate of LVSΔguaB to parental LVS levels, but only partially restored the growth rate of LVSΔguaA (Figure 2B). These results indicate that guaA and guaB encode essential enzymes that the bacteria use to synthesize guanine nucleotides de novo.
Figure 2.
Growth phenotypes of the LVS mutants were evaluated in vitro. F tularensis LVS (triangle), LVSΔguaA (rhombus) and LVSΔguaB (square) were grown in MHB (panel A) or MHB + guanine (panel B) and the optical density at 600 nm was recorded every hour.
The ability of the mutants to revert to guanine prototrophy was assessed by growing LVSΔguaA and LVSΔguaB in broth cultures with serial passage for 2 days. At various time points bacteria were plated on media with or without guanine and the number of revertants calculated per total number of bacteria. No colonies of LVSΔguaA or LVSΔguaB grew on MHB plates without guanine. The reversion rate for each mutant was calculated to be <10-10.
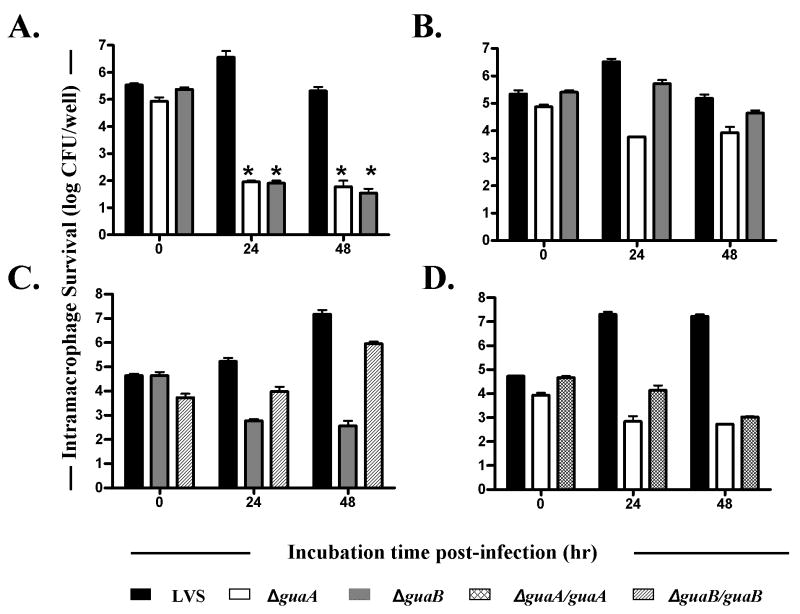
3.3 Mutations in guaA and guaB reduce bacterial growth in macrophages
A hallmark of the pathogenesis of Francisella infection is its ability to survive and replicate within macrophages. The ability of the guaB and guaA mutants to survive and replicate within J774 macrophages was compared to that of the parental strain, LVS. J774 murine macrophages were infected and intracellular growth was analyzed at 0, 24, and 48 hours post infection (Figure 3A). The initial uptake of bacteria was the same for all strains as evidenced by recovery of equal numbers of bacteria at time 0 post-infection. After 24 hours, the number of recovered guaB and guaA mutants significantly decreased (<102 CFU/well), while the parental LVS strain reached the highest levels of intracellular growth (>106 CFU/well). At the 48 hour time point, the number of mutant bacteria remained low and the number of LVS recovered was decreased due to the observed death of the macrophages at this late stage of infection. These findings demonstrate that the absence the metabolic genes guaA or guaB interferes with intracellular survival and replication within the J774 macrophage cell line.
Figure 3.
Survival of F. tularensis strains within macrophages. In panel A, J774 cells (3 × 105) were infected with F. tularensis LVS (black bars), LVSΔguaA (white bars), LVSΔguaB (grey bars), LVSΔguaA(pKK214guaA) (cross hatched bars), or LVSΔguaB(pKK214guaB) (diagonal lined bars) at a multiplicity of infection of 100 in duplicate wells. In panel B, the media was supplemented with guanine (0.05 μg/ml). In panel C, complementation of LVSΔguaB is evaluated. In panel D, complementation of LVSΔguaA is evaluated. The number of bacteria in the cell monolayer was determined at 0, 24, and 48 h post-infection. Data represent the median ± standard deviations of two wells from one representative experiment of three. * p<0.001 compared to parental LVS.
Addition of guanine to the cell culture media restored the ability of LVSΔguaB to survive and replicate (Figure 3B). In contrast, LVSΔguaA reached higher numbers of intracellular growth at both 24 and 48 hours with the addition of guanine, but bacterial recovery was not restored to the level of parental LVS. This observation is consistent with the incomplete complementation of LVSΔguaA growth in vitro even after the addition of guanine (Figure 2B).
Each mutant strain was transformed with a plasmid bearing the corresponding wild-type gene and tested for restoration of WT levels of intracellular replication. LVSΔguaB(pKK214guaB) was able to grow to greater levels than LVSΔguaB alone, but did not reach parental LVS levels at 24 or 48 hours post infection (Figure 3C). LVSΔguaA(pKK214guaA) grew to higher levels than LVSΔguaA at 24 hours, but did not reach parental LVS levels (Figure 3D). At 48 hours, LVSΔguaA(pKK214guaA) was recovered at levels that were the same as the mutant alone.
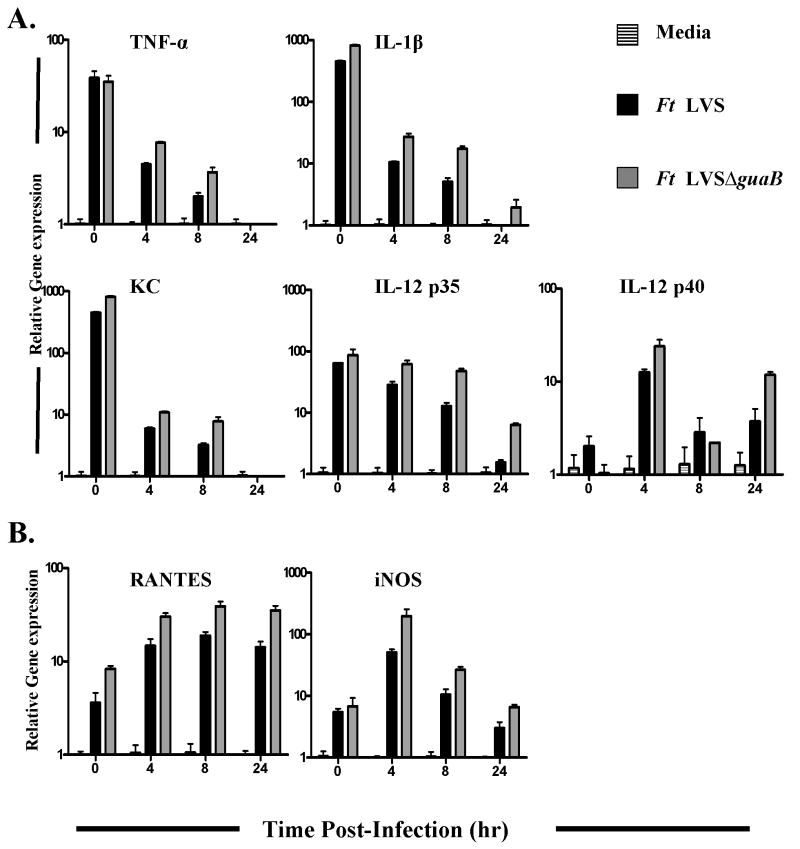
3.3 Francisella tularensis LVSΔguaB induces inflammatory cytokines by TLR2 activation
Despite the inability to replicate in macrophages, we previously demonstrated that LVSΔguaA continued to signal through TLR2 equivalently to parental LVS [9]. Here we compared induction of a large panel of cytokine genes following macrophage infection with LVS or LVSΔguaB using real-time PCR. Primary macrophages were infected with LVS or LVSΔguaB and mRNA levels for TNF-α, IL-1β, KC, IL-12p35, IL-12 p40, RANTES, and iNOS, were quantified at four time points. Expression of TLR2-dependent cytokines TNF-α, IL-1β, KC, and IL-12 p35, was increased at early time points following infection by both LVS and LVSΔguaB (Figure 4A). The importance of IL-12 p40 in the clearance of Francisella infection in mice has been recognized, despite the fact that its biological mechanism of action is not completely understood [13]. In this study, we found that infection of macrophages with both LVS and LVSΔguaB induced sustained mRNA expression of IL-12 p40 in the subsequent 24 hour post-infection period.
Figure 4.
Induction of proinflammatory cytokine gene expression in infected macrophages. Primary macrophages from BALB/c mice were exposed to media alone (lined bars), LVS (black bars) or LVSΔguaB (gray bars) for 0 to 24 hours. At the indicated time points, total mRNA was extracted from the macrophages and analyzed by real-time PCR. Gene expression is reported as relative gene expression compared with macrophages exposed to media alone. Data are presented as mean ± SEM. Data are of a single representative experiment.
In previous studies, we showed that there is a group of cytokines including RANTES and iNOS that required both TLR2 and as well as activation of an unknown intracellular sensor to activate IRF-3 to be induced by infected macrophages [8]. In agreement with that finding, we observed that both RANTES and iNOS mRNA peaked at later time points (≥4 hours post-infection) (Figure 4B). Again, no major differences in cytokine expression levels were observed between macrophages infected with LVSΔguaB or the parental LVS strain. While LVSΔguaB is attenuated for virulence in mice and unable to replicate in macrophages, it is still able to induce a potent proinflammatory cytokine response.
3.4 F. tularensis LVSΔguaA and LVSΔguaB are attenuated in mice
While LVS is attenuated for humans, it is virulent in mice and causes death with a very low inoculum (e.g., ∼10 organisms i.p.). Accordingly, mice serve as a valuable model for studying the attenuating capacity of LVS mutations. Groups of 5 BALB/c mice were inoculated i.p. with 102 to 107 CFU of LVS or the mutant derivatives. Mice inoculated with the LVS parental strain became overtly sick (ruffled fur and hunched gait) between days 2 to 7 post-inoculation depending on the challenge dose, and a dose of 170 CFU or higher was lethal to 100% of the mice (Table 3). In contrast, mice inoculated with 102 to 107 CFU of LVSΔguaA or LVSΔguaB remained healthy through day 28 post-infection. The lethal dose for LVSΔguaA delivered i.p. approached 9.0 × 107 as only 1/5 mice died after infection with this dose (Table 3).
Table 3. Virulence of F. tularensis derivatives in BALB/c mice.
| Experimental groupa | Bacterial inoculum (CFU) | Survival ratiob | Time to death of individual mice (days) |
|---|---|---|---|
| LVS | |||
| Group 1 | 1.7 × 101 | 3/5 | 5, 7, >28, >28, >28 |
| Group 2 | 1.7 × 102 | 0/5 | 5, 5, 6, 6, 8 |
| Group 3 | 1.7 × 103 | 0/5 | 4, 6, 6, 6, 7 |
| Group 4 | 1.7 × 104 | 0/5 | 3, 3, 4, 5, 5 |
| Group 5 | 1.7 × 105 | 0/5 | 3, 3, 3, 4, 6 |
| LVSΔguaA | |||
| Group 6 | 9.0 × 102 | 5/5 | >28, >28, >28, >28, >28 |
| Group 7 | 9.0 × 103 | 5/5 | >28, >28, >28, >28, >28 |
| Group 8 | 9.0 × 104 | 5/5 | >28, >28, >28, >28, >28 |
| Group 9 | 9.0 × 105 | 5/5 | >28, >28, >28, >28, >28 |
| Group 10 | 9.0 × 106 | 5/5 | >28, >28, >28, >28, >28 |
| Group 11 | 9.0 × 107 | 4/5 | 3, >28, >28, >28, >28 |
| LVSΔguaB | |||
| Group 12 | 1.05 × 102 | 5/5 | >28, >28, >28, >28, >28 |
| Group 13 | 1.05 × 103 | 5/5 | >28, >28, >28, >28, >28 |
| Group 14 | 1.05 × 104 | 5/5 | >28, >28, >28, >28, >28 |
| Group 15 | 1.05 × 105 | 5/5 | >28, >28, >28, >28, >28 |
| Group 16 | 1.05 × 106 | 5/5 | >28, >28, >28, >28, >28 |
| Group 17 | 1.05 × 107 | 5/5 | >28, >28, >28, >28, >28 |
| Gelatin 0.1%-PBS | |||
| Group 18 | None | 5/5 | >28, >28, >28, >28, >28 |
Groups of 5 BALB/c mice were inoculated by intraperitoneal route with 10-fold dilutions of LVS (groups 1 to 5); LVSΔguaA (groups 6 to 11) or LVSΔguaB (groups 12 to 17) derivatives in 1.0 ml of gelatin 0.1%-PBS. As a control, group 18 was inoculated with 1.0 ml of gelatin 0.1%-PBS.
Survival ratio, number of mice alive/total number of mice injected with the corresponding LVS derivative at day 28.
In order to confirm the attenuation of the guaB and guaA mutations, virulence was assessed in a second mouse strain. One hundred percent (4/4) of C57BL/6 mice inoculated with 104 CFU of parental LVS succumbed to infection within 4-7 days post inoculation. In contrast, inoculation with LVSΔguaB or LVSΔguaA did not cause death in any mouse at doses of 107 or 108 CFU.
3.5 Replication of F. tularensis LVSΔguaA and LVSΔguaB mutants in mouse organs
To determine the extent of proliferation of the LVS attenuated mutants in the organs of infected mice, the numbers of bacteria in the spleen, liver, lung, and blood were enumerated at 1, 2 and 3 days post-infection. Groups of 9-10 mice were inoculated i.p. with parental LVS, LVSΔguaB, or LVSΔguaA. Three mice from each group were sacrificed at the specified time points post-infection and bacteria in the organs enumerated (Table 4). Both LVSΔguaA and LVSΔguaB mutants were completely cleared from the lungs, livers, and blood by day 1 post-infection. It should be noted that the inoculum size for LVSΔguaA (100 CFU) was lower, than that of LVSΔguaB or parental LVS (720 CFU and 860 CFU respectively) and could account for differences in organ counts. The LVSΔguaA mutant was completely cleared from the spleen by day 1 post-infection; however, 2 out of 3 mice infected with LVSΔguaB showed low levels of bacteria in the spleen on day 1. In contrast, the parental LVS strain was recovered from the blood, spleens, livers, and lungs of all infected animals at all time points examined. The recovery of LVS increased daily and correlated with the increase in disease severity.
Table 4. Growth of F. tularensis in organs of naïve BALB/c mice.
| Group (No. mice) | F. tularensis straina | Mean ± SD CFU of Francisella (log 10) / organ | |||
|---|---|---|---|---|---|
| Spleen | Lung | Liver | Blood (ml) | ||
| 1 (n=3) | LVSΔguaA | BDLb | BDL | BDL | BDL |
| 2 (n=3) | LVSΔguaB | 1.03 ± 0.91 (2/3)c | BDL | BDL | BDL |
| 3 (n=3) | LVS | 4.31 ± 0.76 | 2.82 ± 1.18 | 4.48 ± 0.91 | 2.17 ± 0.96 |
| 4 (n=3) | LVSΔguaA | BDL | BDL | BDL | BDL |
| 5 (n=3) | LVSΔguaB | BDL | BDL | BDL | BDL |
| 6 (n=4) | LVS | 5.91 ± 0.78 | 3.82 ± 1.69 | 5.87 ± 0.90 | >2.00 d |
| 7 (n=3) | LVSΔguaA | BDL | BDL | BDL | BDL |
| 8 (n=4) | LVSΔguaB | BDL | BDL | BDL | BDL |
| 9 (n=4) | LVS | 6.77 ± 0.95 | 4.20 ± 0.95 | 6.92 ± 1.09 | >2.00 |
Groups 3 to 4 BALB/c mice were challenged with LVS derivatives in 1 ml of gelatin 1%-PBS. Groups 1, 4 and 7 were inoculated with 100 CFU of F. tularensis LVSΔguaA; Groups 2, 5 and 8 received 720 CFU of LVSΔguaB and groups 3, 6 and 9 were inoculated with 860 CFU of LVS by the intraperitoneal route. To determine bacterial burdens in lung, spleen and liver, inoculated mice were sacrificed on day 1 (groups: 1, 2, and 3), day 2 (groups: 4, 5 and 6) and day 3 of infection (groups: 7, 8 and 9). Tissue homogenates were serially diluted in PBS and plated on MHA-B plates, and the number of CFU per organ was calculated.
BDL, below detection limit (∼ 20 organisms/organ)
Bacteria only detected in two out of three organs
Bacteria detected in the organs is over 100 CFU/ml of blood
3.6 A single inoculation with LVSΔguaA and LVSΔguaB mutants protects against parental LVS challenge
The mice that survived challenge with a single dose F. tularensis LVSΔguaA or LVSΔguaB in the virulence assay above were assessed for their ability to survive a subsequent LVS challenge. Twenty-eight days following the initial inoculation, mice were challenged with a dose of 2.5 × 103 CFU of parental LVS. All mice that received a single inoculation containing 104 – 107 CFU of LVSΔguaA or LVSΔguaB were protected against LVS challenge (Table 5). The lower initial inoculation dose of 102 CFU of LVSΔguaA or LVSΔguaB protected 4/5 mice and 0/5 mice, respectively. Control, unimmunized mice succumbed to LVS challenge by day 5 following challenge. Similar findings were observed in a second high dose challenge experiment, where a single inoculation of either LVSΔguaA (2.2 × 107 CFU) or LVSΔguaB (3.6 × 107 CFU) conferred protection against a higher challenge dose of 2.8 × 105 CFU of LVS (Table 6). Unimmunized control mice did not survive LVS challenge. Taken together, these findings demonstrated that the vaccination of mice with a single dose of as few as 104 CFU LVSΔguaA or LVSΔguaB led to solid protection against systemic LVS challenge. All of the protected micesurvived without displaying any symptoms of disease.
Table 5. Protective immunity in vaccinated BALB/c mice to re-infection with F. tularensis LVS.
| Vaccine Strain | Immunization dose | Survival ratioa | Median time to death (days) |
|---|---|---|---|
| LVS ΔguaA | |||
| Group 6 | 9.0 × 102 | 4/5 | >28 |
| Group 8 | 9.0 × 104 | 5/5 | >28 |
| Group 10 | 9.0 × 106 | 5/5 | >28 |
| Group 11 | 9.0 × 107 | 4/4b | >28 |
| LVS ΔguaB | |||
| Group 12 | 1.05 × 102 | 0/5 | 5 |
| Group 14 | 1.05 × 104 | 5/5 | >28 |
| Group 16 | 1.05 × 106 | 5/5 | >28 |
| Group 17 | 1.05 × 107 | 5/5 | >28 |
| Gelatin 0.1%-PBS | |||
| Group 18 | None | 0/5 | 5 |
Groups of BALB/c mice pre-vaccinated (see table 3) with 10 fold dilutions of LVSΔguaA (groups 6 to 11); LVSΔguaB (groups 12 to 17) and gelatin 0.1% - PBS (group 18) were injected with 2.5 × 103 CFU of parental LVS strain by intraperitoneal route.
Survival ratio, number of survival animal/ total number of animals immunized at day 28.
One mouse dead after the immunization with LVSΔguaA derivative strain
Table 6. Protective immunity in vaccinated BALB/c mice to challenge with F. tularensis LVS.
| Vaccine Strain | Immunization dosea | Survival ratiob | Median time to death (days) |
|---|---|---|---|
| LVSΔguaA | |||
| Group 1 | 2.2 × 107 | 10/10 | >28 |
| LVSΔguaB | |||
| Group 2 | 3.6 × 107 | 9/9c | >28 |
| Gelatin 0.1%-PBS | |||
| Group 3 | None | 0/10 | 3.5 |
Groups of 10 BALB/c mice were immunized with a single dose of 2.2 × 107 LVSΔguaA (group 1); 3.6 × 107 LVSΔguaB (group 2) and gelatin 0.1%-PBS (group 3). The animals were challenged with 2.8 × 105 CFU of LVS by the i.p. route and survival was observed by 28 days.
Survival ratio, number of survival animal/ total number of animals immunized at day 28.
One mouse died after the immunization with the LVSΔguaB derivative strain.
4.0 Discussion
In the five years since its identification as a priority for biodefense countermeasure development in the United States, a surge of literature about Francisella tularensis has provided insights into mechanisms of pathogenesis and fostered efforts to develop vaccines against this pathogen [22;26]. Reports from studies performed in the 1960s on the protective efficacy of the LVS strain are proof of principal that a live attenuated strain can confer at least partial protection against tularemia in humans [25;37]. However LVS suffers from several shortcomings that prevent its licensure for broad use in the population including a lack of complete definition of the molecular basis of its attenuation despite the completion of genome sequences for Type A and B strains, phenotypic inconsistencies, and lack of complete protection against virulent Type A challenge [31;40;47]. Accordingly, an optimal live attenuated vaccine would possess precisely defined attenuating mutations, genetic stability, and the ability to confer robust protection against the most virulent strains of Francisella.
Towards the goal of constructing an improved vaccine, we created a set of genetic tools to allow precise genetic manipulation of chromosomal loci in F. tularensis. Earlier reports revealed a number of unique properties of Francisella genetics including the need for promoters native to Francisella to drive gene expression as well as the nonreplicative nature of oriE1 based plasmids [2;4;16;21;35;36]. Using this information we constructed a suicide plasmid system for allelic exchange in F. tularensis. Similar methods have recently been used by other investigators and are reported by Frank and Zahrt in a comprehensive review of genetic techniques used in Francisella [16]. We developed our system using the LVS strain as the template for mutagenesis so that molecular techniques could be refined without the need for high level containment. Using this suicide plasmid system, precise deletions in the guaA and guaB genes were introduced into the F. tularensis chromosome resulting in the guanine auxotrophic mutant derivatives LVSΔguaA and LVSΔguaB.
A key feature of Francisella pathogenesis is the ability to multiply to high levels within macrophages. While our LVS mutants were taken up into macrophages at levels equivalent to the parental LVS strain, the LVSΔguaA and LVSΔguaB mutant derivatives were unable to replicate intracellularly and decreased in numbers over time. By 24 hours post-infection, the parental LVS increased to levels that were 1-2 orders of magnitude greater than measured at time 0 h, whereas the LVSΔguaA and LVSΔguaB bacterial numbers were reduced 100- to 1,000-fold (Figure 3). Intracellular growth of LVSΔguaB was restored by the addition of guanine to the media or by expression of the WT guaB gene in trans. In contrast, guanine or trans expression of the WT guaA gene only partially complemented LVSΔguaA growth in vitro and in macrophages. The lack of full complementation of LVSΔguaA suggests that mutation of the guaA gene might be having unintended downstream polar effects. The next gene downstream from guaA is dxs. The dxs gene encodes 1-deoxy-D-xylulose-5-phosphate synthase, the loss of which could weaken the ability of LVS to grow in vitro and in vivo. As no promoter sequence is clearly defined for the dxs gene, it is possible that the guaA mutation disrupted an operon structure, thereby preventing full expression of the dxs gene. We subsequently constructed an unmarked nonpolar guaA deletion in a Type A strain. This new SCHU S4ΔguaA mutant was fully complemented with guanine supplementation as well as by introduction of the WT gene in trans (manuscript in preparation).
In concordance with the inability to replicate within macrophages, the mutant derivatives were also unable to replicate as effectively as LVS in mice following inoculation. Colony counts within livers, lungs, and blood of the infected mice confirmed a lack of replication of both mutant strains and only low level recovery of the LVSΔguaB mutant in the spleen at the 24 hour time point. In contrast, Ft LVS was recovered from all organs and blood at every time point examined (Table 4). Both mutant strains were highly attenuated, at least 10,000-fold, compared to parental LVS. LVS killed 100% of mice inoculated with 170 CFU by the i.p. route, whereas, both mutants were avirulent in the mouse model with LD50 values greater than 107 CFU.
Infection of mice with LVS results in a pronounced inflammatory response [7;15;19;20;45]. We previously demonstrated that despite an inability to replicate in macrophages and mouse organs, LVSΔguaA was able to activate NF-κB reporter activity in TLR2-transfected HEK293T cells comparably to parental LVS [9]. The proinflammatory cytokine response in infected macrophages has been shown to be TLR2-dependent [9;27]. We extended those studies by evaluating the ability of the replication-deficient LVSΔguaB mutant to induce a cytokine response in macrophages. By real-time PCR, we demonstrated that LVS and LVSΔguaB caused a rapid increase in the levels of transcription of TLR2-dependent cytokines including TNF-α, IL-1β, KC, and IL-12 p35 following infection of primary mouse macrophages. Expression of a second group of cytokines that are TLR2 and IRF-3-dependent was induced after 4 hours of infection, and included RANTES and iNOS. IL-12 p40 mRNA was induced later, but was expressed for a longer period of time than the other cytokine genes examined. All cytokines were induced by LVSΔguaB to levels that were equivalent to the LVS parental strain. While we have only reported changes in mRNA expression, past experiments have demonstrated that overall there is a strong correlation between mRNA and protein levels for the cytokines measured [8;9].
Following uptake into macrophages Francisella resides within the phagosome before escaping into the cytoplasm where it can replicate and induce IFN-β transcription and IL-1β secretion [1;6;17;18]. The fact that IFN-β dependent genes iNOS and RANTES were induced following infection with LVS or LVSΔguaB is an indirect indication that the bacteria escaped the phagosome and entered the cytosol [34]. Previously we demonstrated that LVSΔiglC, a mutant incapable of phagosome escape, induced significantly lower levels of iNOS and RANTES transcription due to a lack of phagosomal escape [8]. Furthermore, LVSΔiglC induced higher levels of a panel of TLR2-dependent cytokines as well as TLR2, TLR1, and TLR6, suggesting that retention within the phagosome allowed for enhanced and prolonged stimulation of TLR2 by the bacteria [8]. Taken together, these data suggest that while LVSΔguaB does not replicate in macrophages or in mouse organs this strain is as capable as parental LVS at stimulating the pro-inflammatory cytokine cascade.
Inoculation with a single dose of LVSΔguaB or LVSΔguaA was able to protect mice from both low and high dose lethal challenges. A dose as low as 104 CFU of LVSΔguaB or LVSΔguaA was able to protect against a lethal challenge dose of 2.5×103 CFU of LVS. Mice immunized with 107 CFU of either vaccine strain were fully protected against the more stringent high dose challenge of 2.8×105 CFU of LVS. This is in contrast to the LVSΔiglC mutant which is unable to protect against a lethal LVS challenge [43]. The failure of the attenuated LVSΔiglC mutant to provide protection against subsequent LVS challenge points to the importance of cytokine expression in the development of protective immunity. The LVSΔiglC mutant is unable to escape from the phagosome and LVSΔiglC infection of macrophages leads to little to no IFN-β and IFN-γ production and severely reduced activation of the inflammasome [8]. It has been postulated the activation of the inflammasome and type 1 IFN signaling pathways may be critical for priming protective responses [8;17;24;34;49]. Futhermore, cytokines have been shown previously to be important in the control of LVS infection; antibody neutralization of TNF-α or IFN-γ converts an otherwise non-lethal i.d. infection into one that is lethal and anti-cytokine treatment effectively abrogates the protective immunity provided by passive transfer of spleen cells from immune mice to naïve animals [33]. Therefore, it seems likely that any viable vaccine candidate cannot merely be attenuated. It must be able to induce an appropriate cytokine response. Accordingly, the generation of mutant strains that are avirulent, yet capable of inducing protective responses, provides models for further investigation of critical immune responses.
These two mutant strains have served as valuable tools for the elucidation of the immune response pathways of Francisella in the host. While these strains were protective against challenge with the homologous parental Type B LVS, we did not test their efficacy against Type A challenge. It has been hypothesized that an optimal live attenuated vaccine strain would be derived from a Type A strain in order to provide robust protection against the most virulent strains. This theory is supported by studies in rabbits, an arguably better model for Francisella, that established the superiority of Type A vaccination over LVS in protecting against a lethal Type A challenge [38]. While a few SchuS4 mutant strains have been reported to confer modest to no protective immunity against Type A challenge [39;41;46;48],a recent report by Qin and Mann described a dsbA-like mutant derivative of SchuS4 that was able to protect against i.n. challenge with SchuS4 in the stringent C57BL/6 mouse model [42]. These studies support the contention that an efficacious Type A derivative can be developed if the correct target genes are identified. Interestingly, Bakshi et al. demonstrated modest but significant short term protection against Type A challenge in C57BL/6 mice following immunization with a sodB mutant derivative of LVS [3]. This is remarkable in that parental LVS affords no protection in this model, and suggests potential for Type B-derived strains as well.
There may be multiple viable strategies for creating an attenuated Francisella vaccine that will protect against virulent Type A challenge. The guaB and guaA genes were chosen as targets for mutation based on the successful attenuating effects of their deletion in Shigella. In enteric organisms, the guaBA genes are contained within an operon and a single mutation deletes both genes. In F. tularensis, the guaB and guaA genes are widely separated in the chromosome. This arrangement proves beneficial for further development of Francisella vaccine candidates. Any live attenuated vaccine will require two independently attenuating mutations to ensure a high level of safety against the potential for reversion or repair to wild type. We observed similarly attenuated phenotypes and protective capacities for LVSΔguaB and LVSΔguaA and postulate that introduction of both mutations into a single strain will optimize safety by providing the requisite two independent mutations. It is expected that the combination of both guaB and guaA mutations would not result in additive attenuation since the encoded enzymes function consecutively in the terminal portion of the de novo pathway, both acting prior to the point of guanine entry into the salvage pathway. Finally, the genetic distance between the two loci makes the chance of repair of both genes minuscule. We have recently applied our genetic system to the SchuS4 prototype strain to create guaB and guaA mutant derivatives. Full characterization of these candidates will determine the protective efficacy and potential for advancement of these live attenuated candidates.
Acknowledgments
This work was supported by NIH Cooperative Agreement No. U54 AI57168 (ML, EB, SV). The authors thank Dr. Fernando Ruiz for assistance with the animal studies, Dr. William Blackwelder for statistical analysis, and Chris Grassel for technical assistance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Anthony LD, Burke RD, Nano FE. Growth of Francisella spp. in rodent macrophages. Infect Immun. 1991 Sep;59(9):3291–6. doi: 10.1128/iai.59.9.3291-3296.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anthony LS, Gu MZ, Cowley SC, Leung WW, Nano FE. Transformation and allelic replacement in Francisella spp. J Gen Microbiol. 1991 Dec;137(12):2697–703. doi: 10.1099/00221287-137-12-2697. [DOI] [PubMed] [Google Scholar]
- 3.Bakshi CS, Malik M, Mahawar M, et al. An improved vaccine for prevention of respiratory tularemia caused by Francisella tularensis SchuS4 strain. Vaccine. 2008 Sep 26;26(41):5276–88. doi: 10.1016/j.vaccine.2008.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baron GS, Myltseva SV, Nano FE. Electroporation of Francisella tularensis. Methods Mol Biol. 1995;47:149–54. doi: 10.1385/0-89603-310-4:149. [DOI] [PubMed] [Google Scholar]
- 5.Burke DS. Immunization against tularemia: analysis of the effectiveness of live Francisella tularensis vaccine in prevention of laboratory-acquired tularemia. J Infect Dis. 1977 Jan;135(1):55–60. doi: 10.1093/infdis/135.1.55. [DOI] [PubMed] [Google Scholar]
- 6.Clemens DL, Horwitz MA. Uptake and Intracellular Fate of Francisella tularensis in Human Macrophages. Ann N Y Acad Sci. 2007 Apr 13; doi: 10.1196/annals.1409.001. [DOI] [PubMed] [Google Scholar]
- 7.Cole LE, Elkins KL, Michalek SM, et al. Immunologic consequences of Francisella tularensis live vaccine strain infection: role of the innate immune response in infection and immunity. J Immunol. 2006 Jun 1;176(11):6888–99. doi: 10.4049/jimmunol.176.11.6888. [DOI] [PubMed] [Google Scholar]
- 8.Cole LE, Santiago A, Barry E, et al. Macrophage proinflammatory response to Francisella tularensis live vaccine strain requires coordination of multiple signaling pathways. J Immunol. 2008 May 15;180(10):6885–91. doi: 10.4049/jimmunol.180.10.6885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cole LE, Shirey KA, Barry E, et al. Toll-like receptor 2-mediated signaling requirements for Francisella tularensis live vaccine strain infection of murine macrophages. Infect Immun. 2007 Aug;75(8):4127–37. doi: 10.1128/IAI.01868-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cross AS, Calia FM, Edelman R. From rabbits to humans: the contributions of Dr. Theodore E. Woodward to tularemia research. Clin Infect Dis. 2007 Jul 15 15;45 1:S61–S67. doi: 10.1086/518150. [DOI] [PubMed] [Google Scholar]
- 11.Cuesta N, Salkowski CA, Thomas KE, Vogel SN. Regulation of lipopolysaccharide sensitivity by IFN regulatory factor-2. J Immunol. 2003 Jun 1;170(11):5739–47. doi: 10.4049/jimmunol.170.11.5739. [DOI] [PubMed] [Google Scholar]
- 12.Eigelsbach HT, Downs CM. Prophylactic effectiveness of live and killed tularemia vaccines. I. Production of vaccine and evaluation in the white mouse and guinea pig. J Immunol. 1961 Oct;87:415–25. [PubMed] [Google Scholar]
- 13.Elkins KL, Cooper A, Colombini SM, Cowley SC, Kieffer TL. In vivo clearance of an intracellular bacterium, Francisella tularensis LVS, is dependent on the p40 subunit of interleukin-12 (IL-12) but not on IL-12 p70. Infect Immun. 2002 Apr;70(4):1936–48. doi: 10.1128/IAI.70.4.1936-1948.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ericsson M, Golovliov I, Sandstrom G, Tarnvik A, Sjostedt A. Characterization of the nucleotide sequence of the groE operon encoding heat shock proteins chaperone-60 and -10 of Francisella tularensis and determination of the T-cell response to the proteins in individuals vaccinated with F. tularensis. Infect Immun. 1997 May;65(5):1824–9. doi: 10.1128/iai.65.5.1824-1829.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Forestal CA, Benach JL, Carbonara C, Italo JK, Lisinski TJ, Furie MB. Francisella tularensis selectively induces proinflammatory changes in endothelial cells. J Immunol. 2003 Sep 1;171(5):2563–70. doi: 10.4049/jimmunol.171.5.2563. [DOI] [PubMed] [Google Scholar]
- 16.Frank DW, Zahrt TC. Genetics and genetic manipulation in francisella tularensis. Ann N Y Acad Sci. 2007 Jun;1105:67–97. doi: 10.1196/annals.1409.008. [DOI] [PubMed] [Google Scholar]
- 17.Gavrilin MA, Bouakl IJ, Knatz NL, et al. Internalization and phagosome escape required for Francisella to induce human monocyte IL-1beta processing and release. Proc Natl Acad Sci U S A. 2006 Jan 3;103(1):141–6. doi: 10.1073/pnas.0504271103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Golovliov I, Baranov V, Krocova Z, Kovarova H, Sjostedt A. An attenuated strain of the facultative intracellular bacterium Francisella tularensis can escape the phagosome of monocytic cells. Infect Immun. 2003 Oct;71(10):5940–50. doi: 10.1128/IAI.71.10.5940-5950.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Golovliov I, Kuoppa K, Sjostedt A, Tarnvik A, Sandstrom G. Cytokine expression in the liver of mice infected with a highly virulent strain of Francisella tularensis. FEMS Immunol Med Microbiol. 1996 Mar;13(3):239–44. doi: 10.1111/j.1574-695X.1996.tb00244.x. [DOI] [PubMed] [Google Scholar]
- 20.Golovliov I, Sandstrom G, Ericsson M, Sjostedt A, Tarnvik A. Cytokine expression in the liver during the early phase of murine tularemia. Infect Immun. 1995 Feb;63(2):534–8. doi: 10.1128/iai.63.2.534-538.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Golovliov I, Sjostedt A, Mokrievich A, Pavlov V. A method for allelic replacement in Francisella tularensis. FEMS Microbiol Lett. 2003 May 28;222(2):273–80. doi: 10.1016/S0378-1097(03)00313-6. [DOI] [PubMed] [Google Scholar]
- 22.Griffin KF, Oyston PC, Titball RW. Francisella tularensis vaccines. FEMS Immunol Med Microbiol. 2007 Apr;49(3):315–23. doi: 10.1111/j.1574-695X.2007.00219.x. [DOI] [PubMed] [Google Scholar]
- 23.Hartley G, Taylor R, Prior J, et al. Grey variants of the live vaccine strain of Francisella tularensis lack lipopolysaccharide O-antigen, show reduced ability to survive in macrophages and do not induce protective immunity in mice. Vaccine. 2006 Feb 13;24(7):989–96. doi: 10.1016/j.vaccine.2005.08.075. [DOI] [PubMed] [Google Scholar]
- 24.Henry T, Brotcke A, Weiss DS, Thompson LJ, Monack DM. Type I interferon signaling is required for activation of the inflammasome during Francisella infection. J Exp Med. 2007 Apr 23; doi: 10.1084/jem.20062665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hornick RB, Eigelsbach HT. Aerogenic immunization of man with live Tularemia vaccine. Bacteriol Rev. 1966 Sep;30(3):532–8. doi: 10.1128/br.30.3.532-538.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Isherwood KE, Titball RW, Davies DH, Felgner PL, Morrow WJ. Vaccination strategies for Francisella tularensis. Adv Drug Deliv Rev. 2005 Jun 17;57(9):1403–14. doi: 10.1016/j.addr.2005.01.030. [DOI] [PubMed] [Google Scholar]
- 27.Katz J, Zhang P, Martin M, Vogel SN, Michalek SM. Toll-like receptor 2 is required for inflammatory responses to Francisella tularensis LVS. Infect Immun. 2006 May;74(5):2809–16. doi: 10.1128/IAI.74.5.2809-2816.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kotloff KL, Pasetti MF, Barry EM, et al. Deletion in the Shigella enterotoxin genes further attenuates Shigella flexneri 2a bearing guanine auxotrophy in a phase 1 trial of CVD 1204 and CVD 1208. J Infect Dis. 2004 Nov 15;190(10):1745–54. doi: 10.1086/424680. [DOI] [PubMed] [Google Scholar]
- 29.Kotloff KL, Simon JK, Pasetti MF, et al. Safety and Immunogenicity of CVD 1208S, a Live, Oral DeltaguaBA Deltasen Deltaset Shigella flexneri 2a Vaccine Grown on Animal-Free Media. Hum Vaccin. 2007 Jul 15;3(6) doi: 10.4161/hv.4746. [DOI] [PubMed] [Google Scholar]
- 30.Kuoppa K, Forsberg A, Norqvist A. Construction of a reporter plasmid for screening in vivo promoter activity in Francisella tularensis. FEMS Microbiol Lett. 2001 Nov 27;205(1):77–81. doi: 10.1111/j.1574-6968.2001.tb10928.x. [DOI] [PubMed] [Google Scholar]
- 31.Larsson P, Oyston PC, Chain P, et al. The complete genome sequence of Francisella tularensis, the causative agent of tularemia. Nat Genet. 2005 Feb;37(2):153–9. doi: 10.1038/ng1499. [DOI] [PubMed] [Google Scholar]
- 32.Lauriano CM, Barker JR, Nano FE, Arulanandam BP, Klose KE. Allelic exchange in Francisella tularensis using PCR products. FEMS Microbiol Lett. 2003 Dec 12;229(2):195–202. doi: 10.1016/S0378-1097(03)00820-6. [DOI] [PubMed] [Google Scholar]
- 33.Leiby DA, Fortier AH, Crawford RM, Schreiber RD, Nacy CA. In vivo modulation of the murine immune response to Francisella tularensis LVS by administration of anticytokine antibodies. Infect Immun. 1992 Jan;60(1):84–9. doi: 10.1128/iai.60.1.84-89.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li H, Nookala S, Bina XR, Bina JE, Re F. Innate immune response to Francisella tularensis is mediated by TLR2 and caspase-1 activation. J Leukoc Biol. 2006 Oct;80(4):766–73. doi: 10.1189/jlb.0406294. [DOI] [PubMed] [Google Scholar]
- 35.LoVullo ED, Sherrill LA, Perez LL, Pavelka MS., Jr Genetic tools for highly pathogenic Francisella tularensis subsp. tularensis. Microbiology. 2006 Nov;152(Pt 11):3425–35. doi: 10.1099/mic.0.29121-0. [DOI] [PubMed] [Google Scholar]
- 36.Maier TM, Havig A, Casey M, Nano FE, Frank DW, Zahrt TC. Construction and characterization of a highly efficient Francisella shuttle plasmid. Appl Environ Microbiol. 2004 Dec;70(12):7511–9. doi: 10.1128/AEM.70.12.7511-7519.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McCrumb FR. Aerosol Infection Of Man With Pasteurella Tularensis. Bacteriol Rev. 1961 Sep;25(3):262–7. doi: 10.1128/br.25.3.262-267.1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nutter JE, Myrvik QN. In vitro interactions between rabbit alveolar macrophages and Pasteurella tularensis. J Bacteriol. 1966 Sep;92(3):645–51. doi: 10.1128/jb.92.3.645-651.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pechous RD, McCarthy TR, Mohapatra NP, et al. A Francisella tularensis Schu S4 purine auxotroph is highly attenuated in mice but offers limited protection against homologous intranasal challenge. PLoS ONE. 2008;3(6):e2487. doi: 10.1371/journal.pone.0002487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Prior RG, Klasson L, Larsson P, et al. Preliminary analysis and annotation of the partial genome sequence of Francisella tularensis strain Schu 4. J Appl Microbiol. 2001 Oct;91(4):614–20. doi: 10.1046/j.1365-2672.2001.01499.x. [DOI] [PubMed] [Google Scholar]
- 41.Qin A, Scott DW, Mann BJ. Francisella tularensis subsp. tularensis Schu S4 disulfide bond formation protein B, but not an RND-type efflux pump, is required for virulence. Infect Immun. 2008 Jul;76(7):3086–92. doi: 10.1128/IAI.00363-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Qin A, Scott DW, Thompson JA, Mann BJ. Identification of an essential Francisella tularensis subsp. tularensis virulence factor. Infect Immun. 2009 Jan;77(1):152–61. doi: 10.1128/IAI.01113-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Santic M, Molmeret M, Klose KE, Jones S, Kwaik YA. The Francisella tularensis pathogenicity island protein IglC and its regulator MglA are essential for modulating phagosome biogenesis and subsequent bacterial escape into the cytoplasm. Cell Microbiol. 2005 Jul;7(7):969–79. doi: 10.1111/j.1462-5822.2005.00526.x. [DOI] [PubMed] [Google Scholar]
- 44.Sjostedt A. Tularemia: History, epidemiology, pathogen physiology, and clinical manifestations. Ann N Y Acad Sci. 2007 Mar 29;1105:1–29. doi: 10.1196/annals.1409.009. [DOI] [PubMed] [Google Scholar]
- 45.Stenmark S, Sunnemark D, Bucht A, Sjostedt A. Rapid local expression of interleukin-12, tumor necrosis factor alpha, and gamma interferon after cutaneous Francisella tularensis infection in tularemia-immune mice. Infect Immun. 1999 Apr;67(4):1789–97. doi: 10.1128/iai.67.4.1789-1797.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thomas RM, Titball RW, Oyston PC, et al. The immunologically distinct O antigens from Francisella tularensis subspecies tularensis and Francisella novicida are both virulence determinants and protective antigens. Infect Immun. 2007 Jan;75(1):371–8. doi: 10.1128/IAI.01241-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Titball RW, Petrosino JF. Francisella tularensis Genomics and proteomics. Ann N Y Acad Sci. 2007 Apr 13;1105:98–121. doi: 10.1196/annals.1409.015. [DOI] [PubMed] [Google Scholar]
- 48.Twine SM, Shen H, Kelly JF, Chen W, Sjostedt A, Conlan JW. Virulence comparison in mice of distinct isolates of type A Francisella tularensis. Microb Pathog. 2006 Mar;40(3):133–8. doi: 10.1016/j.micpath.2005.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weiss DS, Henry T, Monack DM. Francisella tularensis activation of the inflammasome. Ann N Y Acad Sci. 2007 Mar 29; doi: 10.1196/annals.1409.005. [DOI] [PubMed] [Google Scholar]